Abstract
Background
Although assays for detecting Yersinia pestis using TaqMan probe-based real-time PCR have been developed for years, little is reported on room-temperature-stable PCR reagents, which will be invaluable for field epidemic surveillance, immediate response to public health emergencies, counter-bioterrorism investigation, etc. In this work, a set of real-time PCR reagents for rapid detection of Y. pestis was developed with extraordinary stability at 37°C.
Methods/Principal Findings
TaqMan-based real-time PCR assays were developed using the primers and probes targeting the 3a sequence in the chromosome and the F1 antigen gene caf1 in the plasmid pMT1of Y. pestis, respectively. Then, carbohydrate mixtures were added to the PCR reagents, which were later vacuum-dried for stability evaluation. The vacuum-dried reagents were stable at 37°C for at least 49 days for a lower concentration of template DNA (10 copies/µl), and up to 79 days for higher concentrations (≥102 copies/µl). The reagents were used subsequently to detect soil samples spiked with Y. pestis vaccine strain EV76, and 5×104 CFU per gram of soil could be detected by both 3a- and caf1-based PCR reagents. In addition, a simple and efficient method for soil sample processing is presented here.
Conclusions/Significance
The vacuum-dried reagents for real-time PCR maintain accuracy and reproducibility for at least 49 days at 37°C, indicating that they can be easily transported at room temperature for field application if the machine for performing real-time PCR is available. This dry reagent is of great significance for routine plague surveillance.
Author Summary
Plague, caused by Yersinia pestis, is one of the oldest and most dangerous diseases in human history, and has claimed millions of lives in the three major historical pandemics. Although panic caused by the Black Death is fading, the threat of the reemergence of plague pandemics still exists, with the additional potential of misuse in biowarfare or bioterrorism. Rapid on-site detection and identification of the pathogen is of paramount significance for timely implementation of effective countermeasures. TaqMan probe-based real-time PCR assays can give quick and accurate identification; however, the need for cold delivery and storage prevents its potential on-site application. The objective of this study was to develop a stable PCR system for easy delivery and storage under room temperature, which is vital for conventional plague surveillance and for preparedness in public health emergencies. We present a solution to this particular issue, hoping that it is helpful to future applications.
Introduction
Yersinia pestis, the causative pathogen of the plague, mainly resides in rodents and can be transmitted to humans by infected fleas [1]. As Y. pestis is highly virulent and infectious, it has always been recognized as one of the classical biological warfare agents [2] and was classified as a Category A pathogen by the U. S. Center for Disease Control and Prevention (http://www.bt.cdc.gov/agent/agentlist-category.asp) [3].
Y. pestis was traditionally identified by bacterial isolation and microscopy observation [4], the phage lysis assay [5] and animal experiments, which was termed as a “four-step” protocol in China. Although it is time-consuming and laborious, this protocol is still a gold standard for laboratory confirmation of Y. pestis infections. Immunological methods were also developed for the detection of F1 antigen and antibodies against Y. pestis [6],[7],[8]. Immunological biosensors, based on fiber optics, magnetic and up-converting phosphor technology, were recently applied in detection of antigen and antibodies of Y. pestis as well [9],[10],[11]. These methods have played important roles in fighting plague, however, nucleic acid-based detection techniques could be an even powerful alternative for detecting Y. pestis.
Conventional PCR-gel electrophoresis method has been developed for detecting Y. pestis in fleas and other specimens [12],[13],[14]. A handful of real-time quantitative PCR assays in various formats were also established for detecting and identifying Y. pestis [15],[16],[17],[18],[19],[20],[21],[22] [23]. Real-time PCR assays provide greater specificity, and they require less time and labor to complete than conventional PCRs. The techniques applied include SYBR Green [24], molecular beacon [25], TaqMan probes [18],[20] and minor groove binding (MGB) probes [22] ect., targeting specific sequences on the chromosome and (or) plasmids. Although real-time PCR has been successfully used in detecting and identifying Y. pestis, the relevant reagents need to be transported under low temperature in dry ice in order to keep the activities of enzymes and labeled probes. In this report we developed a room-temperature stable reagent for real-time PCRs which targeted the 3a sequence [26] in chromosome and the caf1 gene [14] in the plasmid pMT1. This reagent could be stable during transportation at room temperature and thus be reliably applied for on site detection of target microorganisms if the thermal cycler is available.
Materials and Methods
Genomic DNAs
Genomic DNAs of four biovars (Microtus, Orientalis, Antiqua and Mediaevalis) of Y. pestis were stored in our lab. Closely related or other genomic DNAs used in this study include 9 species of Yersinia (Y. enterocolitica, Y. intermedia, Y. aldovae, Y. bercovieri, Y. frederiksenii, Y. kristensenii, Y. mollaretii, Y. rohdei, Y. ruckeri), 16 different serotypes of Y. pseudotuberculosis, Brucella, Francisella tularensis, Bacillus anthracis, and E. coli DH5α; and DNAs from human blood and mouse. All bacterial strains used in this study were listed in Table 1.
Table 1. Strains used in this study.
| Species | Strain* | Biovar or Serotype |
| Yersinia pestis | 49006 | Antiqua |
| 47004 | Mediaevalis | |
| 82009 | Orientalis | |
| 18014 | Microtus | |
| Yersinia pseudotuberculosis | ATCC 29833 | O:1a |
| PTB1 | O:1b | |
| Kuratani | O:1c | |
| 53519 | O:2 | |
| 1134 | O:3 | |
| CBSLAM1684 | O:4a | |
| 53522 | O:5 | |
| DD110 | O:6 | |
| 141 | O:7 | |
| 151 | O:8 | |
| R708Ly | O:9 | |
| 6088 | O:10 | |
| R80 | O:11 | |
| MW864-2 | O:12 | |
| CBSLAM1695 | O:13 | |
| 93422 | O:15 | |
| Y.aldovae | ATCC 35236 | |
| Y.bercovieri | ATCC 43970 | |
| Y.enterocolitica | ATCC 9610 | |
| Y.frederiksenii | ATCC 33641 | |
| Y.intermedia | ATCC 29909 | |
| Y.kristensenii | ATCC 33638 | |
| Y.mollaretii | ATCC 43969 | |
| Y.rohdei | ATCC 43380 | |
| Y.ruckeri | ATCC 29473 | |
| Brucella.melitensis | 28411 | |
| Francisella tularensis | 410101 | |
| Bacillus anthracis | Sterne | |
| E. coli | DH5α |
*All strains were collected in our lab.
Primers and probes
The primers and probes for real-time PCR were designed based on the 3a sequence in the chromosome [26] and caf1 in plasmid pMT1 using Primer Express 2.0 (PE Corporation,USA). Other primers were also designed for cloning the target 3a and calf1 sequences into pGEM-T Easy Vector (Promega, USA). The primers and probes used in this study were listed in Table 2.
Table 2. List of primers and probes used in this study.
| Primers and probes | Sequence( 5′- 3′)d | Locatione | Length of the Amplicon(bp) | Comments |
| 3a-CFa | TGTAGCCGCTAAGCACTACCATCC | 15–38 | 275 | This pair of primers are used to clone sequence containing 3a sequence |
| 3a-CR | GGCAACAGCTCAACACCTTTGG | 268–289 | ||
| 3a-Fb | GGACGGCATCACGATTCTCT | 192–211 | 67 | This set of primers and probe are used in real-time PCR reaction of 3a. |
| 3a-R | CCTGAAAACTTGGCAGCAGTT | 238–258 | ||
| 3a-Tc | Fam-AAACGCCCTCGAATCGCTGGC-Tamra | 216–236 | ||
| caf1-CF | TTCCGTTATCGCCATTGCAT | 15–34 | 451 | This pair of primers are used to clone sequence containing caf1 sequence |
| caf1-CR | TGCAAGTTTACCGCCTTTGG | 446–465 | ||
| caf1-F | AGGTAAACGGTGAGAACCTTGTG | 365–387 | 78 | This set of primers and probe are used in real-time PCR reaction of caf1. |
| caf1-R | CAATTGAGCGAACAAAGAAATCC | 420–442 | ||
| caf1-T | Fam-ATGACGTCGTCTTGGCTACGGGCA-Tamra | 392–415 |
CF/CR:short for clone forward primer and clone reverse primer.
F/R:forward primer and reverse primer.
T:TaqMan probe.
FAM: 6-carboxy fluorescein; TAMRA: 6-carboxy-tetra-methylrhodamine.
Refererring to the positions in the corresponding sequences.
Real-time PCR and cycling parameters
The PCR system (20µl) contained 2µl of 10×buffer (500 mM KCl, 100 mM Tris-HCl, 25 mM MgCl2, 1mg/ml glutin), 1µl of each forward (F) and reverse (R) primer (5µM), 1µl of TaqMan probe (5µM), 1.6 µl of dNTPs (2. 5 mM), 0.2µl of Taq DNA polymerase (5U/µl), 5µl of DNA template, 5µl of enzyme stabilizer mixture (40% trehalose and 20% dextran), and 3.2µl of ddH2O. Real-time PCRs were all performed on the Roche LightCycler 1.0 with the optimized cycling parameters of pre-denaturation at 94°C for 5 min, 40 cycles of denaturation at 95°C for 5 s, annealing and extension at 60°C for 30 s, and finally cooled at 40°C for 10 s. Signal acquisition mode is “single” at each cycle end of amplification.
Standard curve
DNA fragments flanking amplicons of 3a and caf1 were amplified using primers CF and CR (Table 2), respectively, from the 91001 genomic DNA for cloning into the pGEM-T Easy Vector according to the standard protocols reported elsewhere [18],[27]. The ligation products were transformed into DH5α and positive clones were identified by PCR and sequencing. Plasmids containing target fragments were purified separately and linearized by Sal I digestion. The concentration of linearized plasmid solution was then determined by UV spectrophotometer for calculating the copy numbers of the target DNAs. The quantified plasmid solution was serially diluted by 10-fold to prepare the standard templates with known copy numbers of target DNAs. Therefore, the real-time PCR was performed using these templates for obtaining the standard curves of Ct-Log concentration for 3a and caf1, respectively [18],[27]. Ct, the cycle threshold, refers to the cycle at which the fluorescence from a sample crosses the threshold.
Sensitivity and specificity
Y. pestis live attenuated strain EV76 was cultivated in Luria-Bertani broth overnight at 26°C and then serially diluted by 10-fold. The number of viable cells was determined by counting colony forming unit (CFU) on the HBI (Heart Brain Infusion) agar plate. Five µl of each sample were directly applied to PCR amplification for evaluating the sensitivity of the PCR systems. All experiments were performed in duplicate. Genomic DNAs listed in Table 1, human and mouse DNAs were employed to evaluate the specificity of the PCR systems.
Stability of real-time PCR reagent
All reagents needed for real-time PCR were mixed up at appropriate proportion and dispensed into 200 µl microcentrifuge tubes with 15 µl each for a single reaction. The dispensed reaction mixture was then vacuum-dried. For stability evaluation, the dry reagents were kept away from lights at 37°C up to 79 days and the reagents were taken out at different time points to perform PCR by the following method. The reagents were reconstituted by adding 10 µl of ddH2O, and then, 5 µl of plasmid templates containing 101, 103, 105 and 107 copies/µl were separately added. The real-time PCRs were performed according to the protocol mentioned above. Only the real-time PCR system for 3a primers and probe was evaluated in this experiment. The stability of the real-time PCR reagent is assessed in terms of accuracy and reproducibility.
A standard curve of the PCR system was made using the plasmid templates as mentioned above, and the “log10 concentration” of the freshly prepared reagents was chosen as reference values. Results of “log10 concentration” of the reagents kept at 37°C for different periods were compared with the reference ones for accuracy evaluation.
Four plasmid templates (101, 103, 105, and 107copies/µl) were used to perform PCR in triplicate in parallel. The coefficient of variation (CV) of Ct values was used to evaluate the reproducibility of the 3a PCR systems.
Detection of Y. pestis in spiked soil samples
A culture of Y. pestis EV76 was serially diluted by 10-fold, and the number of viable cells was determined. For each of serial dilutions, 100 µl was added to 0.2 g soil samples, and the spiked samples were inoculated at 4°C over night for complete adsorption of the bacteria to soil. The soil samples were collected from the yard of our institute, and they were air dried at room temperature. The dried soil samples were directly spiked with dilution of Y. pestis cultures without any pretreatment for mimicking the real situation that is usually confronted in practice.
The spiked soil samples were vortexed thoroughly and centrifuged at 2, 000 rpm for 4 min and the supernatants were collected. Then, 1 ml of dH2O was added to the pellet, and the mixture was vortexed completely and centrifuged again at 2, 000 rpm for 4 min. The supernatant was transferred to the tube containing the supernatants collected in the first step. This washing step was repeated once for collecting as many bacteria in the soil as possible. The supernatants collected above were mixed together for centrifuging at 8,000 rpm for 5 min to collect the target bacteria. The pellets were washed by dH2O once, and 100 µl of dH2O was added to each sample to resuspend the pellet for boiling in a water bath for 5 min. Five microlitres of this solution were used as templates for real-time PCR. We evaluated the sensitivity and specificity of the PCR system for detecting Y. pestis in the spiked soil samples and a blind experiment was performed for evaluating the feasibility of applying this technique in detection of Y. pestis directly from soil samples.
Sensitivity and specificity for detecting Y. pestis in soil samples
The spiked soil samples with different concentrations of Y. pestis were prepared and processed following the procedures described above, and the washed supernatants were used for sensitivity evaluation. As for the specificity test, genomic DNA (100 µg each) of the four biovars of Y. pestis, and other bacterial genomic DNAs listed in Table 1 (100 µg each) were all spiked into soil samples separately, and the real-time PCR was performed to test the specificity of the primers and probes. All experiments were performed in triplicates.
Blind detection of Y. pestis in the spiked soil samples
Soil samples spiked with different concentrations of EV76 were prepared by our colleague 1, and disordered and renumbered by our colleague 2, and then, the real-time PCR were performed by the first two authors of this article. After reporting the results by the first two authors, the three sides involved in this blind experiment sat together for evaluating agreement of the results to the original preparations. The blind test was performed in triplicates.
Results
Standard curves
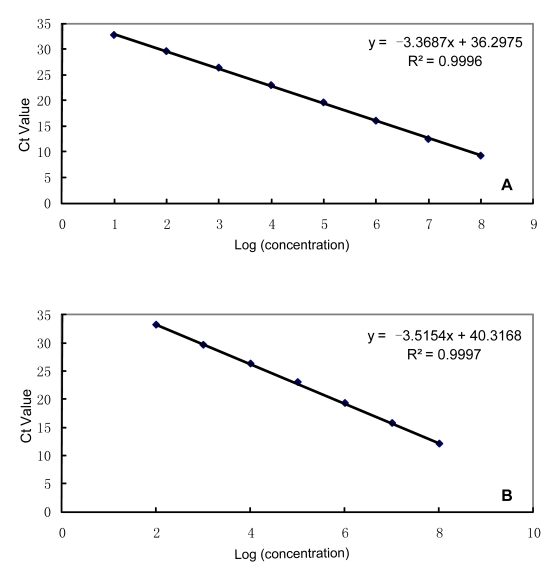
As shown in Fig. 1A and Fig. 1B, standard curves of both 3a and caf1 sequences, based on 10-fold serial dilutions of 10–108 copies/µl, have a linear relationship between the log10 concentration and the Cts, with slopes of −3.3687 and −3.5154, respectively. The efficiency of each reaction is 98% and 93%, and Y-intercepts of 36.298 and 40.317, respectively, indicating a good quantitative determination of the PCR system. The r2 (coefficient of determination) are 0.9996 and 0. 9997, for 3a- and caf1-based PCRs, respectively, implying the accuracy of serial dilution and the precision of sampling, and the ideal linearity of our PCR system as well.
Figure 1. Standard curves for the two targets.
Standard curve of using linearized plasmid containing 3a sequence (A) and caf1 sequence (B) as template. The X-axis represents the log10 concentrations of serially diluted template (10–108 copies/µl) and the Y-axis stands for the Ct values. Please see the text for detail.
Sensitivity and specificity
The sensitivity of real-time PCR system based on the 3a and the caf1 sequences is 1.5 and 15 CFU per system, respectively, using dilutions of EV76 as template (Table 3). For both 3a and caf1 primers and probes, all four biovars of Y. pestis gave positive signals, and the other genomic DNAs in Table 1, human and mouse DNAs gave negative results, indicating the good specificity of these PCR systems.
Table 3. Sensitivity test for 3a and caf1 using live bacteria as template.
| Ct | Live bacteria concentration (CFU/µl) | |
| Sensitivity test for 3a | 34.91 | 3.03×10−1 |
| 31.89 | 2.81 | |
| 27.87 | 3.14×10 | |
| 24.96 | 3.22×102 | |
| 21.75 | 2.95×103 | |
| 18.60 | 2.85×104 | |
| Sensitivity test for caf1 | 32.23 | 3.23 |
| 29.36 | 3.25×10 | |
| 25.79 | 2.86×102 | |
| 22.98 | 2.92×103 | |
| 19.27 | 3.16×104 | |
| 16.83 | 3.31×105 |
Ct: threshold cycle; values <35 are considered to be positive.
Stability of real-time PCR reagent
The vacuum-dried reagents were put in a 37°C incubator and taken out at different time points. We used the ratio of “log10 concentration” of them against the original “log10 concentration” of the standards as a criterion to evaluate the stability of the reagents. A value close to 1 indicates good stability of the reagents, and we set the ratio of 0.900∼1.100 as the standard of acceptable stability. As shown in Table 4, only the results at the days 18 and 79 for lower concentration (10 copies/µl) were beyond this threshold. However, for the days 23, 32 and 49 at this concentration, the results were good enough to indicate the stability of the reagents. Therefore, we could reasonably attribute the biased results at day 18 for the lower concentration to the experimental errors. For concentration of template higher than 10 copies/µl, the vacuum-dried real-time PCR reagents could remain effective for at least 79 days at 37°C.
Table 4. Ratio of every time test results vs. the first test result.
| Log10CET/ Log10CFT* | |||||||||||||
| concentration | Day1 | Day3 | Day5 | Day7 | Day9 | Day11 | Day13 | Day15 | Day18 | Day23 | Day32 | Day49 | Day79 |
| 10 | 1 | 1.03 | 1.02 | 1.09 | 0.94 | 1.05 | 0.99 | 0.97 | 1.21 | 1.08 | 0.95 | 1.05 | 1.57 |
| 103 | 1 | 0.96 | 0.99 | 0.97 | 1.03 | 0.96 | 0.93 | 0.94 | 0.91 | 1.00 | 0.96 | 0.94 | 0.90 |
| 105 | 1 | 0.99 | 0.99 | 1.00 | 1.01 | 0.96 | 0.98 | 1.00 | 0.97 | 0.99 | 0.97 | 0.98 | 0.95 |
| 107 | 1 | 0.98 | 0.97 | 0.99 | 0.98 | 0.97 | 0.98 | 0.96 | 0.94 | 0.95 | 0.96 | 0.92 | 0.92 |
*As the experiments proceeded, a calculated concentration was obtained at each time point for each of the four theoretical concentrations, then, the ratio of Log10(concentration measured at each time, CET)/ Log10(concentration measured at the first time, CFT) are calculated, each concentration was measured three times. The unit of concentration is copies/µl.
For evaluating the reproducibility of the PCR reagents, four concentrations of standard templates (10, 103, 105, 107copies/µl) were chosen for performing real-time PCR in triplicates. As illustrated in Table 5, the coefficients of variations (CV) of Ct value for all concentrations were less than 3% in the 79-day's storage at 37°C, indicating an excellent reproducibility.
Table 5. Ct value for PCR reagent stored at 37°C for different days.
| Ct valuea | CVb | |||||||||||||
| concentration | Day1 | Day3 | Day5 | Day7 | Day9 | Day11 | Day13 | Day15 | Day18 | Day23 | Day32 | Day49 | Day79 | |
| 10 | 31.65 | 31.5 | 31.56 | 31.27 | 31.92 | 31.41 | 31.71 | 31.76 | 30.75 | 31.3 | 31.86 | 31.43 | 29.14 | 2.40 |
| 103 | 28.1 | 28.45 | 28.19 | 28.3 | 27.84 | 28.44 | 28.67 | 28.54 | 28.79 | 28.11 | 28.42 | 28.6 | 28.9 | 1.05 |
| 105 | 22.77 | 22.93 | 22.94 | 22.73 | 22.68 | 23.27 | 23.02 | 22.83 | 23.13 | 22.95 | 23.16 | 23.08 | 23.44 | 0.95 |
| 107 | 15.07 | 15.49 | 15.78 | 15.37 | 15.55 | 15.74 | 15.4 | 15.82 | 16.41 | 16.13 | 15.97 | 16.74 | 16.66 | 2.97 |
Ct: threshold cycle;values<35 are considered to be positive. Each Ct value is the mean result of the three values obtained each time point.
CV: coefficients of variations.
The results above suggest that the vacuum-dried real-time PCR reagent could be transported at room temperature by normal post or express mailing system.
Detection of Y. pestis in artificially contaminated soil samples
For the spiked soil with different concentrations of Y. pestis EV76 for evaluating sensitivity of our PCR system, the results demonstrated that 5×104 CFU per gram of soil could be detected by both 3a- and caf1-based PCR systems when Ct>35 was considered as a negative result. Genomic DNAs of four biovars of Y. pestis and its closely related and non-related bacterial genomic DNAs were all spiked separately into soil samples for evaluating the specificity of the PCR systems, and only the samples spiked with the four biovars of Y. pestis DNA showed positive results while all the samples spiked with other DNAs gave negative results. In the blind test, all the spiked samples with different amount of Y. pestis EV76 were detected correctly. As expected, the CFU values determined by the real-time PCR were 10 to 100 times lower than the ones spiked into the soil samples. These results implied that the real-time PCR systems could detect Y. pestis sensitively and specifically from soil samples.
Discussion
In vitro amplification of nucleic acids by PCR has been widely used for both research and clinical diagnosis. Although quantitative real-time PCR of the TaqMan technology has been developed and applied in detection of pathogenic microorganisms from different clinical samples for many years, the reagents or diagnostic kits should be transported under dry ice for protecting enzymes from activity loss. The reverse-transcriptase PCR kit for detecting dengue virus was once evaluated by storing at room temperature, refrigerator and freezer, and the results indicated that the test kits could only be stored above its recommended storage temperature of −20°C for no more than 3 days [28]. Ramanujam et al. reported that the PCR reaction mixtures could be stabilized in carbohydrate polymers by forming glassy matrices that provide room-temperature stability [29]. This kind of stabilized reagent could be stable at 22°C for 6 weeks. Wolff et al. modified a nested PCR system using single-tube, preformulated mixes embedded in a trehalose matrix, which allowed the reagents to be stored for >6 months at ambient temperature [30]. Carbohydrates (trehalose, inulin or dextran) were also employed to stabilize influenza subunit vaccine in the dry state, making the vaccine stable for at least 26 weeks at room temperature [31]. It has been recognized that some yeast cells tend to accumulate high concentrations of trehalose when submitted to heat shock, which can lead to a more heat-stable conformation of the enzyme in yeast [32]. Trehalose has been used to stabilize methanol dehydrogenase for the detection of methanol [33]. In this study, we initially wanted to compare different kinds of carbohydrates in PCR mixture for their ability in stabilizing the PCR reagents. Fortunately, when we tested our first mixture of carbohydrates (10% trehalose and 5% dextran in PCR mixture, final concentration), we obtained very stable PCR reagents as mentioned in the result. Then, we gave up more comparisons between different kinds of carbohydrates and turned to evaluate how stability of this fortunate formulation. During the development of this ambient-stable PCR reagent, we once compared the dried reagents with or without stabilizers. The results showed that the dried reagents without stabilizers could give positive amplifications for higher concentrations of DNA template for the first two days at 37°C (data not shown), however, the one with stabilizers, as shown in this report, could be stable for a much longer period at 37°C. This result indicated the stabilizing effect of the added carbohydrates on PCR reagents.
As shown by our results, this set of reagents can be stable at 37°C for up to 79 days when the concentration of template is higher than 10 copies/µl. For lower concentration, it can be stable at least for 49 days at 37°C. These results reveal that the stabilized PCR reagent can be transported by normal post mailing or express mailing system without dry-ice protection. To test its feasibility of delivering the reagents to different places without cold preservation, we mailed this reagent to different labs in Xinjiang, Shanghai, Tibet, Sichuan, Liaoning, Guangdong, Hubei Provinces by domestic couriers. It usually took 2 to 4 days for the receivers to get the reagent. The receivers tested them and confirmed that the sensitivity of the reagent met the requirement (data not shown).
Plague is one of the most important natural focus-related zoonotic diseases. Routine surveillances are of paramount significance for disease case reporting and controlling. In some of the surveillance stations, dead animals without any information of its dead time and reason and their spoiled soil in the natural plague foci are common samples for detecting and isolating Y. pestis. It usually takes 10 to 20 days to get final results. If PCR could be used in routine surveillances, it would improve the surveillance efficiency [12],[34]. However, the surveillance stations are usually set up in the field, some of which even do not have freezers or refrigerators. A room-temperature-stable PCR reagent is therefore urgently demanded. After developing such a kind of reagent and testing its stability at 37°C, we chose the spiked soils as clinical samples to develop a protocol for detecting Y. pestis because contaminated soils by dead animals are common samples for Y. pestis detection [35] and Y. pestis could be persisted in soils for a long time, up to 40 weeks [36]; and also because soils contain rich compounds that inhibit enzymes, including Taq polymerase used in PCR [37],[38],[39],[40]. A protocol for soil processing can be readily modified to treat the animal specimens by adding a step of proteinase K digestion. During soil treatment, we once compared the different lysis methods of direct heating lysis and NaI lysis. Direct heating method gave a better sensitivity than NaI lysis and hence we employed the former in our final protocol.
In the future application, we will distribute these reagents to different plague surveillance stations in China for their evaluation of its feasibility in field.
Acknowledgments
We want to express our appreciation to Ms. Jin Wang and many others who gave us instructions and help to our work, and to Dr. Yajun Song from University College Cork, Ireland, for his help in revising this manuscript.
Footnotes
The authors have declared that no competing interests exist.
This work was supported by the National Key Program for Major Infectious Diseases of China (2009ZX10004-103). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Perry RD, Fetherston JD. Yersinia pestis–etiologic agent of plague. Clin Microbiol Rev. 1997;10:35–66. doi: 10.1128/cmr.10.1.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Inglesby TV, Dennis DT, Henderson DA, Bartlett JG, Ascher MS, et al. Plague as a biological weapon: medical and public health management. Working Group on Civilian Biodefense. Jama. 2000;283:2281–2290. doi: 10.1001/jama.283.17.2281. [DOI] [PubMed] [Google Scholar]
- 3.Greenfield RA, Bronze MS. Prevention and treatment of bacterial diseases caused by bacterial bioterrorism threat agents. Drug Discov Today. 2003;8:881–888. doi: 10.1016/s1359-6446(03)02847-2. [DOI] [PubMed] [Google Scholar]
- 4.Gaval SR, Shrikhande SN, Makhija SK, Tankhiwale NS, Pathak AA, et al. Study of suspected plague cases for isolation and identification of Yersinia pestis. Indian J Med Sci. 1996;50:335–338. [PubMed] [Google Scholar]
- 5.Nunes MP, Suassuna I. Bacteriophage specificity in the identification of Yersinia pestis as compared with other enterobacteria. Rev Bras Pesqui Med Biol. 1978;11:359–363. [PubMed] [Google Scholar]
- 6.Chanteau S, Rahalison L, Ratsitorahina M, Mahafaly, Rasolomaharo M, et al. Early diagnosis of bubonic plague using F1 antigen capture ELISA assay and rapid immunogold dipstick. Int J Med Microbiol. 2000;290:279–283. doi: 10.1016/S1438-4221(00)80126-5. [DOI] [PubMed] [Google Scholar]
- 7.Chanteau S, Rahalison L, Ralafiarisoa L, Foulon J, Ratsitorahina M, et al. Development and testing of a rapid diagnostic test for bubonic and pneumonic plague. Lancet. 2003;361:211–216. doi: 10.1016/S0140-6736(03)12270-2. [DOI] [PubMed] [Google Scholar]
- 8.Thullier P, Guglielmo V, Rajerison M, Chanteau S. Short report: Serodiagnosis of plague in humans and rats using a rapid test. Am J Trop Med Hyg. 2003;69:450–451. [PubMed] [Google Scholar]
- 9.Anderson GP, King KD, Cao LK, Jacoby M, Ligler FS, et al. Quantifying serum antiplague antibody with a fiber-optic biosensor. Clin Diagn Lab Immunol. 1998;5:609–612. doi: 10.1128/cdli.5.5.609-612.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yan Z, Zhou L, Zhao Y, Wang J, Huang L, et al. Rapid quantitative detection of Yersinia pestis by lateral-flow immunoassay and up-converting phosphor technology-based biosensor. Sensors and Actuators B. 2006;119:656–663. doi: 10.1016/j.snb.2006.01.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wei H, Zhao K, Bi Y, Liu H, Guo Z, et al. Direct detection of Yersinia pestis from the infected animal specimens by a fiber optic biosensor. Sensors and Actuators B. 2007;123:204–210. [Google Scholar]
- 12.Hinnebusch J, Schwan TG. New method for plague surveillance using polymerase chain reaction to detect Yersinia pestis in fleas. J Clin Microbiol. 1993;31:1511–1514. doi: 10.1128/jcm.31.6.1511-1514.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Norkina OV, Kulichenko AN, Gintsburg AL, Tuchkov IV, Popov Yu A, et al. Development of a diagnostic test for Yersinia pestis by the polymerase chain reaction. J Appl Bacteriol. 1994;76:240–245. doi: 10.1111/j.1365-2672.1994.tb01622.x. [DOI] [PubMed] [Google Scholar]
- 14.Tsukano H, Itoh K, Suzuki S, Watanabe H. Detection and identification of Yersinia pestis by polymerase chain reaction (PCR) using multiplex primers. Microbiol Immunol. 1996;40:773–775. doi: 10.1111/j.1348-0421.1996.tb01140.x. [DOI] [PubMed] [Google Scholar]
- 15.Higgins JA, Ezzell J, Hinnebusch BJ, Shipley M, Henchal EA, et al. 5′ nuclease PCR assay to detect Yersinia pestis. J Clin Microbiol. 1998;36:2284–2288. doi: 10.1128/jcm.36.8.2284-2288.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Iqbal SS, Chambers JP, Goode MT, Valdes JJ, Brubaker RR. Detection of Yersinia pestis by pesticin fluorogenic probe-coupled PCR. Mol Cell Probes. 2000;14:109–114. doi: 10.1006/mcpr.2000.0295. [DOI] [PubMed] [Google Scholar]
- 17.Lindler LE, Fan W, Jahan N. Detection of ciprofloxacin-resistant Yersinia pestis by fluorogenic PCR using the LightCycler. J Clin Microbiol. 2001;39:3649–3655. doi: 10.1128/JCM.39.10.3649-3655.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Loiez C, Herwegh S, Wallet F, Armand S, Guinet F, et al. Detection of Yersinia pestis in sputum by real-time PCR. J Clin Microbiol. 2003;41:4873–4875. doi: 10.1128/JCM.41.10.4873-4875.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tomaso H, Reisinger EC, Al Dahouk S, Frangoulidis D, Rakin A, et al. Rapid detection of Yersinia pestis with multiplex real-time PCR assays using fluorescent hybridisation probes. FEMS Immunol Med Microbiol. 2003;38:117–126. doi: 10.1016/S0928-8244(03)00184-6. [DOI] [PubMed] [Google Scholar]
- 20.Chase CJ, Ulrich MP, Wasieloski LP, Jr, Kondig JP, Garrison J, et al. Real-time PCR assays targeting a unique chromosomal sequence of Yersinia pestis. Clin Chem. 2005;51:1778–1785. doi: 10.1373/clinchem.2005.051839. [DOI] [PubMed] [Google Scholar]
- 21.Woron AM, Nazarian EJ, Egan C, McDonough KA, Cirino NM, et al. Development and evaluation of a 4-target multiplex real-time polymerase chain reaction assay for the detection and characterization of Yersinia pestis. Diagn Microbiol Infect Dis. 2006;56:261–268. doi: 10.1016/j.diagmicrobio.2006.06.009. [DOI] [PubMed] [Google Scholar]
- 22.Skottman T, Piiparinen H, Hyytiainen H, Myllys V, Skurnik M, et al. Simultaneous real-time PCR detection of Bacillus anthracis, Francisella tularensis and Yersinia pestis. Eur J Clin Microbiol Infect Dis. 2007;26:207–211. doi: 10.1007/s10096-007-0262-z. [DOI] [PubMed] [Google Scholar]
- 23.Tomaso H, Jacob D, Eickhoff M, Scholz HC, Al Dahouk S, et al. Preliminary validation of real-time PCR assays for the identification of Yersinia pestis. Clin Chem Lab Med. 2008;46:1239–1244. doi: 10.1515/CCLM.2008.251. [DOI] [PubMed] [Google Scholar]
- 24.Saikaly PE, Barlaz MA, de Los Reyes FL, 3rd Development of quantitative real-time PCR assays for detection and quantification of surrogate biological warfare agents in building debris and leachate. Appl Environ Microbiol. 2007;73:6557–6565. doi: 10.1128/AEM.00779-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Varma-Basil M, El-Hajj H, Marras SAE, Hazbon MH, Mann JM, et al. Molecular Beacons for Multiplex Detection of Four Bacterial Bioterrorism Agents. Clinical Chemistry. 2004;50:1060–1063. doi: 10.1373/clinchem.2003.030767. [DOI] [PubMed] [Google Scholar]
- 26.Radnedge L, Gamez-Chin S, McCready PM, Worsham PL, Andersen GL. Identification of nucleotide sequences for the specific and rapid detection of Yersinia pestis. Appl Environ Microbiol. 2001;67:3759–3762. doi: 10.1128/AEM.67.8.3759-3762.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Scheurer ME, Dillon LM, Chen Z, Follen M, Adler-Storthz K. Absolute quantitative real-time polymerase chain reaction for the measurement of human papillomavirus E7 mRNA in cervical cytobrush specimens. Infect Agent Cancer. 2007;2:8. doi: 10.1186/1750-9378-2-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ooi CP, Rohani A, Zamree I, Lee HL. Temperature related storage evaluation of an RT-PCR test kit for the detection of dengue infection in mosquitoes. Trop Biomed. 2005;22:73–76. [PubMed] [Google Scholar]
- 29.Ramanujam R, Koelbl J, Ting E, Jolly J, Burdick B. Room-temperature-stable PCR reagents. PCR Methods Appl. 1993;3:75–76. doi: 10.1101/gr.3.1.75. [DOI] [PubMed] [Google Scholar]
- 30.Wolff C, Hornschemeyer D, Wolff D, Kleesiek K. Single-tube nested PCR with room-temperature-stable reagents. PCR Methods Appl. 1995;4:376–379. doi: 10.1101/gr.4.6.376. [DOI] [PubMed] [Google Scholar]
- 31.Amorij JP, Meulenaar J, Hinrichs WL, Stegmann T, Huckriede A, et al. Rational design of an influenza subunit vaccine powder with sugar glass technology: preventing conformational changes of haemagglutinin during freezing and freeze-drying. Vaccine. 2007;25:6447–6457. doi: 10.1016/j.vaccine.2007.06.054. [DOI] [PubMed] [Google Scholar]
- 32.Felix CF, Moreira CC, Oliveira MS, Sola-Penna M, Meyer-Fernandes JR, et al. Protection against thermal denaturation by trehalose on the plasma membrane H+-ATPase from yeast. Synergetic effect between trehalose and phospholipid environment. Eur J Biochem. 1999;266:660–664. doi: 10.1046/j.1432-1327.1999.00916.x. [DOI] [PubMed] [Google Scholar]
- 33.Argall ME, Smith GD. The use of trehalose-stabilized lyophilized methanol dehydrogenase from Hyphomicrobium X for the detection of methanol. Biochem Mol Biol Int. 1993;30:491–497. [PubMed] [Google Scholar]
- 34.Engelthaler DM, Gage KL. Quantities of Yersinia pestis in fleas (Siphonaptera: Pulicidae, Ceratophyllidae, and Hystrichopsyllidae) collected from areas of known or suspected plague activity. J Med Entomol. 2000;37:422–426. doi: 10.1093/jmedent/37.3.422. [DOI] [PubMed] [Google Scholar]
- 35.Wong D, Wild MA, Walburger MA, Higgins CL, Callahan M, et al. Primary pneumonic plague contracted from a mountain lion carcass. Clin Infect Dis. 2009;49:e33–38. doi: 10.1086/600818. [DOI] [PubMed] [Google Scholar]
- 36.Ayyadurai S, Houhamdi L, Lepidi H, Nappez C, Raoult D, et al. Long-term persistence of virulent Yersinia pestis in soil. Microbiology. 2008;154:2865–2871. doi: 10.1099/mic.0.2007/016154-0. [DOI] [PubMed] [Google Scholar]
- 37.Whitehouse CA, Hottel HE. Comparison of five commercial DNA extraction kits for the recovery of Francisella tularensis DNA from spiked soil samples. Mol Cell Probes. 2007;21:92–96. doi: 10.1016/j.mcp.2006.08.003. [DOI] [PubMed] [Google Scholar]
- 38.Braid MD, Daniels LM, Kitts CL. Removal of PCR inhibitors from soil DNA by chemical flocculation. J Microbiol Methods. 2003;52:389–393. doi: 10.1016/s0167-7012(02)00210-5. [DOI] [PubMed] [Google Scholar]
- 39.Kramer F, Vollrath T, Schnieder T, Epe C. Improved detection of endoparasite DNA in soil sample PCR by the use of anti-inhibitory substances. Vet Parasitol. 2002;108:217–226. doi: 10.1016/s0304-4017(02)00199-1. [DOI] [PubMed] [Google Scholar]
- 40.Watson RJ, Blackwell B. Purification and characterization of a common soil component which inhibits the polymerase chain reaction. Can J Microbiol. 2000;46:633–642. doi: 10.1139/w00-043. [DOI] [PubMed] [Google Scholar]