Introduction
Holistic concepts of health are rooted in ancient medical traditions with recent emergence of multiple perspectives from around the world for the need to pay greater attention to the totality of the person seeking care, the integration of health and social services, and to aspire towards personalized approach to care [1–8].
The person-centered integrative diagnosis model (PID) is the key diagnostic project of the Psychiatry for the Person Institutional Program of the World Psychiatric Association (WPA General Assembly, 2005) which proposes the whole person in context, as the center and goal of clinical care and public health [9]. The PID is the operational articulation of the psychiatry for the person diagnostic principles with the goal of developing a model applicable into regular clinical care settings [10].
Despite the repeated calls for the centeredness of the person seeking care and for the importance of a holistic approach to care, the effective application of these principles to regular clinical care has been hampered by the lack of adequate diagnostic models that can embodies these principles, yet be flexible, adaptable, and useful to the diverse clinical realities and needs. For example, the full implementation of the multiaxial diagnostic models into clinical practice has been limited due to their complexity and to the perceived lack of immediate utility of some of their domains [11]. Furthermore, these multi-axial models lack explicit attention to positive aspects of health deemed key in the recovery and health restoration process.
This manuscript presents key concepts, evolving multilevel domains of health status, structure and design of the person-centered diagnostic model (PID).
Key concepts for person-centered integrative diagnosis (PID)
The 20th century Spanish philosopher and humanist, Ortega y Gasset (1883–1955), dictum “I am I and my circumstance” cogently captures the overarching concept embodied in the person-centered integrative diagnosis and the psychiatry for the person's vision of considering “the whole person in context”, as the centre and goal of clinical care and public health. The key concept in the person-centered integrative diagnosis is its consideration of a broader and deeper notion of diagnosis (to include positive and ill aspects of health), which goes beyond the restricted concept of nosological diagnoses. The notion of diagnosis as a formulation of health status, and as a process involving the interactive participation and engagement of clinicians, patients, and families, represents a paradigm shift.
Diagnosis has a fundamental role in medicine as the basic unit in the process of medical care. It is essential for communication among health professionals and other stakeholders, it is fundamental for the process of clinical care and the identification and treatment of disorders, it is used for prevention and health promotion, for conducting research, testing interventions and understanding disease mechanisms. Diagnosis is needed for education and training and for a host of administrative purposes from quality improvement to reimbursement activities. The pivotal role of diagnosis in the clinicians' work was cogently expressed by Feinstein (Feinstein, 1967) [12] as “Diagnostic categories provide the locations where clinicians store the observations of clinical experience” and “The diagnostic taxonomy establishes the patterns, according to which clinicians observe, think, remember and act.”
It should also be recognized that diagnosis has had mixed role for patients. While for some diagnosis provide understanding and empowerment, for others diagnosis has been associated with illness adjudication, with a sense of suffering, loss, and damaged self. Diagnosis, especially in psychiatry, has also been associated with value judgments, labeling and stigma.
A broader perspective on the meaning of diagnosis may also be gleaned from its etymological roots. Diagnosis has been derived from two connotations. On the one hand, diagnosis is derived from the Greek word ‘dia’, which refers to elucidating a disorder, a meaning that is more consonant with the common etiopathogenic meaning of diagnosis. The other term, also from the Greek language is ‘diagignoskein’ which refers to the understanding of the person, reflecting the meaning of health (sanscrit hal) as wholeness. This latter definition is particularly suitable for chronic diseases, such as diabetes, HTN, or obesity, where behavioral components can assume significant role.
Reflecting on the meaning of diagnoses in medicine, the medical historian Lain-Entralgo stated that, “diagnoses is more than identifying disorders (nosological diagnoses)”, or “distinguishing one disorder from another (differential diagnoses); diagnoses is really understanding what is going on in the mind and body of the person who present for care” [13]. A broader understanding of diagnosis that goes beyond the ethiopathogenic understanding, has been reflected in ancient traditional medicine as well as in modern understanding of health. For example, in the ancient Chinese medicine, diagnostic indicators were always viewed holistically. The Indian medical tradition, Ayurveda, which means the science of living, views health as harmony between body, mind and spirit. Pointedly, in modern times, the World Health Organization Constitution defines health as “Health is a state of complete physical, emotional, and social well-being, and not merely the absence of disease” (WHO, 1946) [14].
The concept of diagnosis in the PID is to provide broader understanding of the person's health status, describing both positive and ill health (disorders and disabilities as classified by the International Classification of Diseases and its national and regional adaptations), and to also include an innovative focus on positive aspects of health, such as adaptive functioning, protective factors, and quality of life, deemed crucial for enhancing recovery and health restoration.
A second key concept of the PID is its emphasis on an inclusive and participatory process, highlighting the importance of all protagonists of the clinical encounter into the diagnostic process. Diagnostic formulation in the PID is also considered as an ongoing process constructed through interactive partnership involving a dialogue between the primary stakeholders and evaluators. This partnership of equals includes the clinician (the conventional expert), the patient (the protagonist, informationally and ethically), the family (crucial support group), and community members (teachers, social workers, etc.) Thus, the PID, through this process upholds the dignity, values, and aspirations of the person seeking care.
The multilevel person-centered integrative diagnosis model
The development and structure of the proposed PID model is anchored in the well established record of the World Psychiatric Association's experience in the development of diagnostic models and contributions to the central issue of international diagnoses in psychiatry [15–18]. The current organizational schema of the developing multilevel PID model proposes to assess the health status of the person presenting for care, as opposed to a predominant focus on pathology. Thus, the two broad domains covered are ill health and positive aspects of health. In each of these domains, the PID schema provides for a standardized component and for a narrative, idiographic personalized component. The integration of these domains and components aims at forming the informational bases for intervention and care, such as developing treatment plans to guide recovery and health restoration, in addition to providing the informational bases for education, public health planning and for administrative functions.
The evolving PID model has currently three main levels within each health status domain (Ill health versus positive health status domains) [19–21]. Within the ill health status domain, the first level is ill health and its burden. This is further divided into two sublevels: the first sublevel corresponds to clinical disorders, both mental and general health. The second sublevel corresponds to disabilities (regarding self-care, occupational functioning, functioning with family and participation in community activities). The second ill health domain level corresponds to the idiographic personalized narrative covering the experience of illness. This includes topics, such as sufferings, values and cultural experience of illness and care. The third level within the ill health domain covers risk factors and contributors to ill health. These include inner risk factors, such as genetic vulnerability and external risk factors, such as stressors. Factors in this domain may also be conceptualized using a bio-psycho-social framework.
Wellness is the first level of the positive health status domain. This is further divided into two sublevels: the first sublevel corresponds to remission/recovery (health restoration and growth), while the second sublevel corresponds to functioning. The second level of positive health domain corresponds to the idiographic personalized narrative covering the experience of health. This includes topics, such as quality of life, values and cultural formulation of identity and context. The third level in the positive health status domain covers protective factors and contributors to positive health. These may include inner protective factors, such as resilience, and external protective factors, such as social support. These factors may also be conceptualized in a bio-psycho-social framework (Figure 1).
Figure 1.
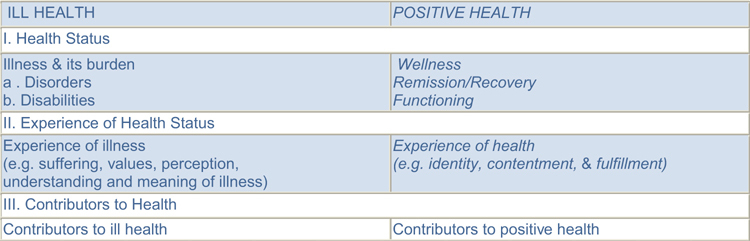
Schema of the person-centered integrative diagnosis domains.
The PID will avail of all relevant descriptive tools, including categorical, dimensional, and narrative approaches. These approaches will allow for capturing quantitative and categorical assignments above a certain threshold level and the use of narrative would offer the possibility of a deeper and richer personalized description of a relevant domain. Within the PID, the evaluators' role has been elaborated as ‘Trialogs’ among patients, families and health professionals [8] who would jointly undertake the diagnostic process and formulate planned interventions.
Conclusion
The person-centered integrative diagnosis (PID) is the diagnostic model endeavored through the psychiatry for the person program, a major World Psychiatric Association (WPA) initiative. The person-centered integrative diagnosis (PID) is a novel model of conceptualizing the process and formulation of clinical diagnosis. It proposes to implement into regular clinical practice the principles and vision of person-centered psychiatry proposing the whole person in context, as the center and goal of clinical care and public health. The PID entails a broader and deeper notion of diagnosis, beyond the restricted concept of nosological diagnoses. It involves a multilevel formulation of health status (both ill and positive aspects of health) through interactive participation and engagement of clinicians, patients, and families using all relevant descriptive tools (categorization, dimensions, and narratives). The development of the PID model has been a reiterative process with continuing refinements. The fully developed and validated model is intended to be used in diverse settings across the world and to serve multiple needs in clinical care, education, research, and public health.
Contributor Information
Ihsan M Salloum, University of Miami Miller School of Medicine, Miami, Florida, USA.
Juan E Mezzich, International Center for Mental Health and Division of Psychiatric Epidemiology, Mount Sinai School of Medicine, New York University, USA.
References
- 1.Herrman H, Saxena S, Moodie R. Promoting mental health: concepts, emerging evidence, practice. Geneva: WHO; 2005. [Google Scholar]
- 2.World Health Organization. WHO's new global strategies for mental health. Geneva: WHO; 1999. (Factsheet 217) [Google Scholar]
- 3.U.S. Presidential Commission on Mental Health. Achieving the promise: transforming mental health care in America. Final Report. Rockville, Maryland: Department of Health and Human Services; 2003. (DHHS Pub N: SMA-03-3832) [Google Scholar]
- 4.World Health Organization European Ministerial Conference on Mental Health. Mental health action plan for Europe: facing the challenges, building solutions. Helsinki, Finland, 12–15 January 2005. (EUR/04/5047810/7) [PubMed]
- 5.Patwardhan B, Warude D, Pushpangadan P, Bhatt N. Ayurveda and traditional Chinese medicine: a comparative overview. Evidence-based Complementary and Alternative Medicine. 2005;2:465–73. doi: 10.1093/ecam/neh140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Christodoulou GN, editor. Psychosomatic medicine. New York: Plenum Press; 1987. [Google Scholar]
- 7.Anthony W. Recovery from mental illness. The guiding vision of the mental health service systems in the 1990s. Psychosocial Rehabilitation Journal. 1993;16:11–23. [Google Scholar]
- 8.Amering M, Schmolke M. Recovery – Das Ende der Unheilbarkeit Recovery – the end of incurability. Bonn: Psychiatrie-Verlag; 2007. [Google Scholar]
- 9.Mezzich JE. Psychiatry for the person: articulating medicine's science and humanism. World Psychiatry. 2007 Jun;6(2):65–7. [PMC free article] [PubMed] [Google Scholar]
- 10.Mezzich JE, Salloum IM. Towards a person-centered integrative diagnosis. In: Salloum IM, Mezzich JE, editors. Psychiatric diagnosis: context and prospects. Oxford: Wiley-Blackwell; 2009. Chapter 30. [Google Scholar]
- 11.Banzato EM, Jorge MR, Kastrup M. Multiaxial schemas for psychiatric diagnosis. In: Salloum IM, Mezzich JE, editors. Psychiatric diagnosis: context and prospects. Oxford: Wiley-Blackwell; 2009. Chapter 28. [Google Scholar]
- 12.Feinstein AR. Clinical judgment. Huntington, NY: Robert E. Krieger; 1967. [Google Scholar]
- 13.Laın-Entralgo P. El Diagnostico Medico: Historia y Teoria. [Medical diagnostics: history and theory]. Barcelona: Salvat; 1982. [in Spanish] [Google Scholar]
- 14.World Health Organization. WHO constitution. Geneva: WHO; 1946. [Google Scholar]
- 15.Mezzich JE, Ustun TB. International classification and diagnosis: critical experience and future directions. Proceedings of a symposium. London, United Kingdom, July 2001. Psychopathology. 2002 Mar-Jun;35(2–3):59–201. doi: 10.1159/000065119. [DOI] [PubMed] [Google Scholar]
- 16.Banzato CEM, Mezzich JE, Berganza CE, editors. Philosophical and methodological foundations of psychiatric diagnosis. Psychopathology. 2005 Jul-Aug;38(4) doi: 10.1159/000086082. Special Issue. [DOI] [PubMed] [Google Scholar]
- 17.World Psychiatric Association. Essentials of the World Psychiatric Association's International Guidelines for Diagnostic Assessment (IGDA) British Journal of Psychiatry. 2003;182(Supp. 45):s37–s66. [PMC free article] [PubMed] [Google Scholar]
- 18.APAL. Guia Latinoamericana de Diagnostico Psiquiatrico (GLADP) [Latin American Guide of Psychiatric Diagnosis]. Mexico: Editorial de la Universidad de Guadalajara; 2004. [in Spanish] [Google Scholar]
- 19.Cloninger CR. Feeling good: the science of well-being. New York: Oxford University Press; 2004. [Google Scholar]
- 20.Cox J, Campbell A, Fulford KWM. Medicine of the person. London: Kingsley Publishers; 2007. [Google Scholar]
- 21.Mezzich JE. Positive health: conceptual place, dimensions and implications. Psychopathology. 2005 Jul-Aug;38(4):177–9. doi: 10.1159/000086086. [DOI] [PubMed] [Google Scholar]


