Abstract
Bacillus anthracis represents a formidable bioterrorism and biowarfare threat for which new vaccines are needed with improved safety and efficacy over current options. Toward this end, we created recombinant adeno-associated virus type 1 (rAAV1) vectors containing synthetic genes derived from the protective antigen (PA) or lethal factor (LF) of anthrax lethal toxin (LeTx) and tested them for immunogenicity and induction of toxin-neutralizing antibodies in rabbits. Codon-optimized segments encoding activated PA (PA63), or LF, were synthesized and cloned into optimized rAAV1 vectors containing a human cytomegalovirus (hCMV) promoter and synthetic optimized leader. Serum from rabbits immunized intramuscularly with rAAV1/PA (monovalent), rAAV1/LF (monovalent), rAAV1/PA + rAAV1/LF (bivalent), or rAAV1/enhanced green fluorescent protein (control) exhibited substantial PA- and LF-specific antibody responses at 4 weeks by both western blot (> 1:10,000 dilution) and enzyme-linked immunosorbent assay (ELISA) (mean end-point titer: 32,000–260,000), and contained anthrax LeTx–neutralizing activity in vitro, with peak titers approximating those of a rabbit hyperimmune antisera raised against soluble PA and LF. Compared to the monovalent groups (rAAV1/PA or rAAV1/LF), the bivalent group (rAAV1/PA + rAAV1/LF) exhibited marginally higher ELISA and neutralization activity with dual specificity for both PA and LF. The finding of robust neutralizing antibody responses after a single injection of these rAAV1-based vectors supports their further development as candidate anthrax vaccines.
Introduction
Bacillus anthracis has a long and storied history as the causative agent of anthrax in wildlife, livestock and human hosts. More recently, the easy distribution and extreme toxicity associated with inhalation of its endospores have positioned it as an accessible yet formidable bioweapon for use in warfare and terrorism. The real and present nature of the threat was made evident in the 2001 attacks exploiting the US postal system which resulted in 22 confirmed infections and 5 deaths.1 The pathogenesis of anthrax has been widely studied and important disease mechanisms worked out at the molecular level.2,3 The lethality of anthrax is caused by the production of the exotoxins lethal toxin (LeTx) and edema toxin during vegetative growth in the host.2,4 These toxins are classic A-B toxins with protective antigen (PA) serving as the “B” receptor–binding moiety in both toxins, and lethal factor (LF) or edema factor serving as the enzymatic “A” moiety in LeTx and edema toxin, respectively. The PA first binds to a host cell surface receptor, where a furin-like protease cleaves PA83 to release the PA20 fragment thereby enabling PA63 to associate with other PA molecules to form a heptamer. The heptamer subsequently binds to either LF or EF molecules to form the assembled holotoxin that ultimately results in translocation of the “A” moieties from an endosomal compartment into the cytoplasm of the cell.
PA-specific humoral immunity has been demonstrated to protect from inhalation anthrax even in the absence of LF and EF immunity.5,6 Nonetheless, LF and EF may contribute to toxin-directed vaccines by eliciting neutralizing antibody responses against the molecules themselves, and possibly by enhancing anti-PA responses.6 One study demonstrated substantial augmentation of the anti-PA immune responses through co-inoculation with DNA expressing PA63 and LFn, a truncated n-terminal LF fragment (LF domain 1 residues 10–254). Further, immunity to LFn alone was shown to provide protection against an intravenous LeTx challenge in mice.7 Edema factor–specific responses do not block LeTx intoxication, but could potentially contribute to vaccine efficacy by targeting edema toxin.6,8,9,10
The current licensed anthrax vaccine, anthrax vaccine adsorbed (AVA), is manufactured by preparing a filtrate of a nonencapsulated but toxigenic B. anthracis derivative, treating it with formaldehyde, and adsorbing it to aluminum hydroxide.11,12 Animal model studies have shown that AVA provides protection by stimulating antibodies against PA,13 and AVA has been shown to confer virtually complete protection from an inhalation spore challenge in rabbits and primates.12,13,14 An early trial evaluating AVA in anthrax-exposed industrial workers demonstrated an efficacy of 92.5% for protection against cutaneous and inhalation anthrax.15,16 The multiple injections and yearly boosts required for establishment and maintenance of immunity, however, and the reactogenicity and potential adverse reactions to AVA, have raised broad concern, and have motivated commitment to the development of next generation anthrax vaccines.17,18,19,20
Vectors based on recombinant adeno-associated virus (rAAV) have been widely applied as gene transfer vehicles for gene therapy.21,22,23 Recently, the potential of rAAV as viral-based vaccines has been recognized.24,25,26,27 In particular, the outstanding clinical safety record in humans, the simplicity of vector system, the ability to infect muscle cells, and the long-term expression are prominent features that make rAAV an attractive candidate as a vaccine vector.
In this article, we describe the development and testing of rAAV1 vector–based constructs containing codon-optimized PA63 or LF genes. The results demonstrate that a single intramuscular (IM) injection of rabbits with one or both rAAV1 constructs leads to the rapid onset of high-titered antibody responses capable of neutralizing LeTx in vitro.
Results
Construction of rAAV1 expressing PA, LF, or enhanced green fluorescent protein
To achieve high-level expression in human cells, we codon-optimized the sequences of PA63 and LF for human expression and placed them under the control of the cytomegalovirus (CMV) immediate-early promoter (Figure 1a,b). In addition, several cis modifications were made to ensure maximum gene expression, as follows: first, an intron derived from SV40 was included to increase mRNA processing stability and nuclear export;28 second, a synthetic leader was added for secretion of the protein; third, a consensus Kozak sequence (CCACC) was included as a translation initiation signal; and fourth, a SV40 polyadenylation signal was added for proper mRNA processing. To prevent toxicity in rabbits inoculated with both rAAV1/PA and rAAV1/LF, we created a point mutation at amino acid position 236 (Y236A) of LF, which has been shown to abolish LF binding to PA.29 A vector expressing enhanced green fluorescent protein (eGFP) was constructed for use as a negative control (Figure 1c). To assess protein production, C12 cells were infected with rAAV1/PA, rAAV1/LF, or rAAV1/eGFP, in the presence of pAdhelper which enhances second-strand synthesis through its E4 ORF6.30 The lysates from C12 cells infected with rAAV1/PA, rAAV1/LF, or rAAV1/eGFP were collected and assayed by western blotting and demonstrated specific reactivity with antibodies specific for PA, LF, and eGFP, respectively, at their predicted molecular masses (Figure 1d–f).
Figure 1.
Vaccine construction and transgene expression. The rAAV1/PA63, rAAV1/LF, and rAAV1/eGFP vaccine constructs were engineered as depicted in a–c to express PA63, lethal factor (LF), or enhanced green fluorescent protein (eGFP), respectively. For each construct, expression was confirmed by infection of HeLa cells and subsequent analysis of cell lysates by western blot using anti-PA, anti-LF, or anti-eGFP antisera as shown in d–f for rAAV1/PA63, rAAV1/LF, and rAAV1/eGFP, respectively. Lysates from cells infected with vaccine constructs (+) were run in lanes adjacent to lysates from cells infected with irrelevant control vector (–). CMV, cytomegalovirus immediate-early promoter; ITR, inverted terminal repeat; intron, an SV40 derived intron; Opt L, a synthetic optimized leader sequence; PA, protective antigen; rAAV1, recombinant adeno-associated virus type 1; SV40pA, an SV40 polyadenylation signal.
Serum antibody response following IM immunization
All rabbits received a single inoculation in each quadriceps of their hind legs with rAAV1 expressing either PA, LF, or eGFP as outlined in Table 1, and were then bled at 2, 4, 8, 12, and 16 weeks after inoculation. Serum anti-PA and anti-LF reactivity were assessed by enzyme-linked immunosorbent assay (ELISA) as described in the Materials and Methods section. As seen in Figure 2a, most rabbits inoculated with rAAV1/PA (group 1, monovalent immunization) had very low titers to immobilized PA at the 2-week time point, but demonstrated robust antibody production by the 4-week time point. Group 1 peak anti-PA antibody titers were attained by week 8 and were sustained at a high level through the week 16 time point. Bivalently immunized rabbits (group 3), which received a single inoculation with rAAV1/PA, and in the opposite leg, a single inoculation with rAAV1/LF, demonstrated a more rapidly developing anti-PA response with significant titers among some rabbits as early as 2 weeks after inoculation (Figure 2b). Like the group 1 rabbits, the bivalently inoculated group 3 rabbits reached peak anti-PA titers at the 8-week time point. There was no evidence from the analysis of the anti-PA responses from group 3 rabbits that the concomitant inoculation in the opposite leg with rAAV/LF and/or the subsequent immune response to LF, had any inhibitory effect on the induction of anti-PA immunity. Indeed, the group 1 and 3 peak anti-PA titers were comparable with reciprocal geometric mean titers (GMTs) of 185,364 and 208,064 at 8 weeks and 92,682 and 104,032 at 16 weeks, respectively. Both groups also evidenced good durability in their anti-PA titers as demonstrated by reciprocal GMTs of 131,072 at the time of killing, 5 months after inoculation (data not shown).
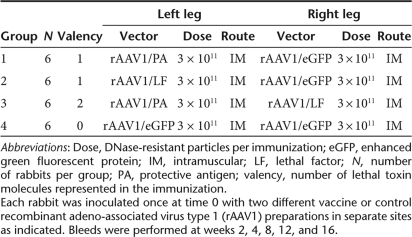
Table 1.
Vaccine groups
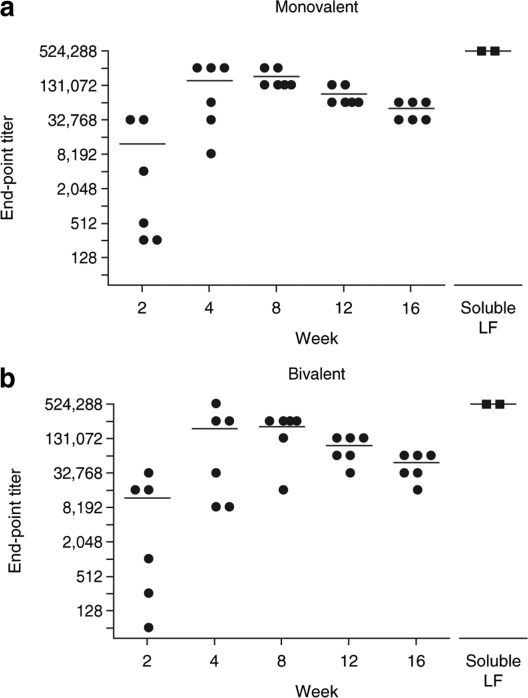
Figure 2.
Protective antigen (PA)-specific serum antibody responses in rabbits after monovalent and bivalent vaccination. Serum from rabbits immunized (a) with rAAV1/PA (group 1, monovalent immunization), or (b) with both rAAV1/PA and rAAV1/LF (group 3, bivalent immunization) was tested for anti-PA reactivity by enzyme-linked immunosorbent assay at 2, 4, 8, 12, and 16 weeks after immunization. Prebleed serum and serum from group 4 rabbits inoculated with recombinant adeno-associated virus type 1 (rAAV1) expressing enhanced green fluorescent protein were negative (<64, data not shown). Each circle represents the response of an individual rabbit and the horizontal lines represent geometric mean end-point titers. Squares represent individual rabbit antibody titers from two positive control rabbits immunized four times with soluble PA83 in an emulsion with Freund's adjuvant. LF, lethal factor.
High-titer LF-specific antibody responses were seen in monovalently inoculated group 2 rabbits and bivalently inoculated group 3 rabbits. Many of the group 2 and 3 rabbits demonstrated anti-LF responses as early as 2 weeks, and a number of rabbits reached near peak titers at the 4-week time point. As shown in Figure 3a, group 2 rabbits reached a peak LF-specific titer of 165,140 at 8 weeks, which declined to 46,341 at 16 weeks. Group 3 rabbits reached a peak LF titer of 147,123 at 8 weeks followed by a decline to 41,285 at week 16 (Figure 3b). At the time of killing, 5 months after inoculation, antiserum from groups 2 and 3 demonstrated reciprocal GMTs of 41,285 and 46,341, respectively (data not shown). Control group 4 rabbits inoculated with rAAV1/eGFP had no detectable antibody specific for PA or LF at any time point (data not shown).
Figure 3.
Lethal factor (LF)-specific serum antibody responses in rabbits after monovalent and bivalent vaccination. Serum from rabbits immunized (a) with rAAV1/LF (group 2, monovalent immunization) or (b) with both rAAV1/PA and rAAV1/LF (group 3, bivalent immunization) was tested for anti-LF reactivity by enzyme-linked immunosorbent assay at 2, 4, 8, 12, and 16 weeks after immunization. Prebleed serum and serum from group 4 rabbits inoculated with recombinant adeno-associated virus type 1 (rAAV1) expressing enhanced green fluorescent protein were negative (<64, data not shown). Each circle represents the response of an individual rabbit and the horizontal lines represent geometric mean end-point titers. Squares represent individual rabbit antibody titers from two positive control rabbits immunized four times with soluble LF in an emulsion with Freund's adjuvant. PA, protective antigen.
Anthrax LeTx neutralization responses
PA- and LF-specific antiserum from rabbit groups 1–4 were analyzed for LeTx neutralization as described in the Materials and Methods section. Anthrax LeTx neutralization assays were configured to examine either PA- or LF-specific neutralization. In these assays, the target molecule of interest was present at concentrations representing 2.5–3.5 multiples of the amount needed to kill 50% of the RAW264 cells (TD50) as determined by a contemporaneous titration.
Monovalent group 1 rabbits demonstrated evidence of PA LeTx neutralization at week 8, which increased to a peak activity observed at week 12 with a reciprocal GMT of 60% of control anti-PA neutralization (Figure 4a). Thereafter, titers declined marginally to 54% of control at the 16-week time point, and to 32% of control at the time of killing ~5 months after inoculation (data not shown). Bivalent group 3 rabbits demonstrated more rapidly developing and higher overall levels of PA LeTx neutralization compared to group 1 rabbits, with a peak response of 81% of control at the 8-week time point (Figure 4b). Group 3 PA LeTx neutralization remained almost unchanged at this level through the 12-week time point with 80% of control anti-PA neutralization, and then declined to 52% of control at 16 weeks. At the time of killing, 5 months after inoculation, antiserum from group 3 rabbits demonstrated neutralization that was 38% of control (data not shown). None of the negative control group 4 rabbits inoculated with rAAV1/eGFP had any detectable PA or LF LeTx neutralization at any time point (Figures 4 and 5).
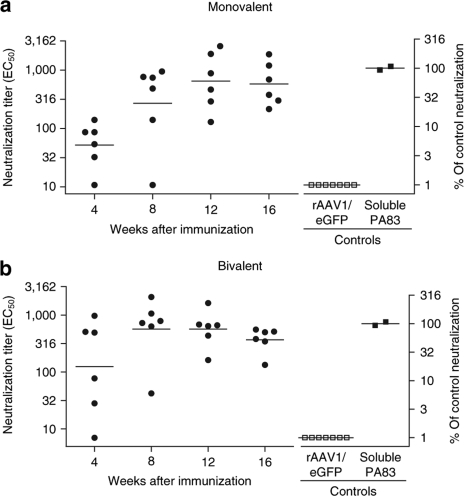
Figure 4.
Anthrax lethal toxin neutralization by protective antigen (PA)-specific antibodies after monovalent and bivalent vaccination. Serum from rabbits immunized (a) with rAAV1/PA (group 1, monovalent immunization) or (b) with both rAAV1/PA and rAAV1/LF (group 3, bivalent immunization) was tested for PA-specific lethal toxin neutralization at 4, 8, 12, and 16 weeks as described in Materials and Methods. Each circle represents the response of an individual rabbit and the horizontal lines represent geometric mean neutralization. The left y-axis corresponds to 50% effective concentration (EC50) neutralization titers and the right y-axis denotes the EC50 titers normalized to the geometric mean neutralization titers from the serum of the two control rabbits (closed squares) which were immunized four times with soluble PA83 in Freund's adjuvant as described in the Materials and Methods section. Also shown are the results from analysis of 8-week serum from rabbits inoculated with rAAV1/eGFP (group 4, open squares). Serum from group 4 rabbits also had no detectable neutralization at the 4-, 12-, and 16-week time points (data not shown). eGFP, enhanced green fluorescent protein; LF, lethal factor; rAAV1, recombinant adeno-associated virus type 1.
Figure 5.
Anthrax lethal toxin neutralization by lethal factor (LF)-specific antibodies after monovalent and bivalent vaccination. Serum from rabbits immunized (a) with rAAV1/LF (group 2, monovalent immunization), or (b) with both rAAV1/PA and rAAV1/LF (group 3, bivalent immunization) was tested for LF-specific lethal toxin neutralization at 4, 8, 12, and 16 weeks as described in Materials and Methods. Each circle represents the response of an individual rabbit, and the horizontal lines represent geometric mean neutralization. The left y-axis corresponds to 50% effective concentration (EC50) neutralization titers and the right y-axis denotes the EC50 titers normalized to the geometric mean neutralization titers from the serum of the two control rabbits (closed squares) which were immunized four times with soluble LF in Freund's adjuvant as described in the Materials and Methods section. Also shown are the results from analysis of 8-week serum from rabbits inoculated with rAAV1/eGFP (group 4, open squares). Serum from group 4 rabbits also had no detectable neutralization at the 4-, 12-, and 16-week time points (data not shown). eGFP, enhanced green fluorescent protein; PA, protective antigen; rAAV1, recombinant adeno-associated virus type 1.
Monovalent group 2 rabbits were tested in a LF-specific toxin-neutralizing antibody (TNA) as shown in Figure 5a. The kinetics of the neutralization response mirrored that of the anti-LF antibody results in that neutralization was observed at week 4 with a reciprocal GMT of 18% of control anti-LF neutralization, and peak titers were attained at week 8 with 71% of control. Thereafter, neutralization responses declined to 61 and 45% of control at the 12- and 16-week time points, respectively. At the time of killing, ~5 months after inoculation, serum from group 2 rabbits demonstrated neutralization that was 24% of the LF control levels. As shown in Figure 5b, bivalently inoculated group 3 rabbits demonstrated similar LF neutralization kinetics, but attained a higher overall LF neutralization titer, compared to the monovalently inoculated group 2 rabbits with 4-week responses of 22% of control and peak neutralization at 8 weeks of 91% of control. Group 3 LF-specific neutralization declined slightly to 87% of control at 12 weeks and then to 63% of control at 16 weeks. At the time of killing, 5 months after inoculation, serum from the bivalently inoculated group 3 rabbits demonstrated neutralization that was 41% of the LF control levels.
As seen with the antibody responses to PA and LF in bivalently inoculated group 3 rabbits, there was no evidence from the neutralization results of interference associated with the simultaneous induction of immunity against both the PA and LF components comprising the binary LeTx. On the contrary, bivalent inoculation resulted in higher peak levels of neutralization compared to monovalent inoculation, though the results did not reach statistical significance.
Discussion
Aerosolized B. anthracis continues to present a major threat for use as a biological weapon. It is therefore imperative that effective countermeasures be in place to neutralize or mitigate this potential threat. Safety and delivery concerns associated with the current AVA vaccine, which requires six injections over 18 months and then yearly booster immunizations, have motivated substantial research toward developing new and improved vaccines. While much of this work has focused on soluble PA, alternative expression platforms and alternative targets for humoral immunity have attracted interest. Expression vaccines traditionally included live-attenuated or live-related viruses (e.g., vaccinia), but now include several viral and microbial platforms for expression of recombinant protein antigens, as well as DNA vaccines. AAV has also emerged as an attractive vaccine platform. Some of the advantages of AAV include the relative lack of pathogenicity and its wide range of infectivity including postmitotic target cells like skeletal muscle, which is an ideal vaccine target. Most importantly, rAAV vectors have been shown to induce strong cellular and humoral immune responses to foreign transgenes.24,31,32,33,34,35 We previously demonstrated that a single IM dose of macaques with rAAV/simian immunodeficiency virus vaccines elicits simian immunodeficiency virus–specific T cells and antibodies. Furthermore, immunized macaques were able to significantly restrict replication of a live, virulent simian immunodeficiency virus challenge.26 Though rAAV vectors have been shown to elicit robust immune responses following a single injection, the immune responses could potentially be enhanced with the use of adjuvants, or through use of a prime-boost strategy using a heterologous rAAV serotype or recombinant protein for the booster immunization.27,34,36,37,38 The relative safety of rAAV vectors, coupled with their ability to induce robust humoral immunity26,27,37 makes rAAV a particularly attractive vaccine delivery platform for anthrax, because a preponderance of data suggests that antibody neutralization is sufficient to lead to protection in rabbit anthrax spore inhalation challenges.39,40
In the current studies, we sought to develop a rAAV-based anthrax vaccine targeting both PA and LF. Though the currently licensed vaccine for anthrax, AVA, and the majority of vaccine approaches currently under development for anthrax target PA, an efficacious vaccine targeting LF could enhance the protection afforded by an anthrax vaccine, especially in the event of a malicious attempt to reengineer the bacterium so as to escape protection conferred by PA-directed vaccines. Experimental vaccines targeting LF or LF fragments, have demonstrated protective immunity in mouse and rabbit models.7,41 To avoid potential toxicity in vivo associated with the coexpression of both LF and PA as occurs in the bivalently inoculated rabbits, we introduced an in-frame mutation previously demonstrated to eliminate LF binding to PA.29 Because the rAAV does not replicate and there is no selective pressure in vivo, there is no risk of back mutations.
We proceeded to test the vaccine constructs in both monovalent and bivalent immunization formats, where rabbits received a single inoculation of either the rAAV1/PA or rAAV1/LF or separate inoculations with both vectors. Monovalent immunization resulted in the development of significant neutralizing responses as early as 8 weeks after inoculation in rabbits immunized with rAAV1/PA and at 4 weeks in rabbits inoculated with rAAV1/LF. Peak neutralization responses were observed at 12 and 8 weeks, respectively. Bivalent inoculation of group 3 rabbits, like the monovalent group 2 rabbits, demonstrated more rapid kinetics compared to group 1 rabbits, with considerable PA and LF neutralization apparent in the 4-week serum and peak PA and LF neutralization at the 8-week time point. It is unclear why the group 1 rabbits demonstrate some delay in development of neutralization compared to group 2 and 3 rabbits, though the expression of LF in both of the latter groups may be important. Previous work in mice has demonstrated that DNA inoculation with plasmids encoding fragments of both LF and PA yielded greater PA- and LF-specific immunogenicity than inoculation with either plasmid alone.7 A second study showed that mucosal immunization with PA63 and LF stimulated higher PA and LF-specific antibody than either protein alone.42 The PA expressed in the rAAV1/PA, is the activated PA63, and not the PA83 form. We utilized PA63 because this moiety could be expected to express at higher levels compared to PA83, may display antibody epitopes that are not exposed in the PA83 molecule, and has demonstrated effectiveness in prior studies.43 It has been suggested, however, that PA83 may be more immunogenic than PA63.44
Bivalently inoculated rabbits demonstrated levels of neutralization that were higher in comparison to the levels observed in monovalent-inoculated rabbits, though the differences did not reach the level of statistical significance. Both monovalent and bivalently inoculated groups demonstrated some reduction of antibody and neutralization titers from their peak levels to the end of the time period examined in the study, though significant antibody and neutralization titers were still evident in both monovalent and the bivalent groups at the time of killing ~5 months after inoculation with rAAV1. This suggests durability of the immune response engendered through inoculation with rAAV1 expressing PA or LF, which may be an advantage compared to alternative immunization modalities. If determined to be necessary for the promotion of more durable immunity, a strategy for boosting the immune responses could include a boost with either soluble PA and/or LF or a re-inoculation with a different serotype of rAAV expressing the respective transgenes.
Finally, while the co-inoculation of rabbits with rAAV1 expressing PA and LF may broaden the potential for protective immunity by including LF as an additional target, it is also possible that LF-specific antibodies may synergize with PA-specific antibodies in ways currently undetectable by the in vitro toxin-neutralization assay. Any potential synergies associated with bivalent inoculation compared to monovalent inoculation might be manifested as greater than additive protection in anthrax spore inhalation challenge experiments.
In conclusion, the results presented here demonstrate that rAAV1-based anthrax vaccines targeting PA63 and LF, singly or in combination, induce prompt, sustained neutralizing antibody responses following a single IM immunization. The current study demonstrates that rAAV can be successfully employed for the vaccination of rabbits to induce high-titered neutralizing antibody responses against the LeTx of B. anthracis and support further testing of these vaccines in the anthrax spore inhalation challenge.
Materials and Methods
Cell lines. C12 is a HeLa-derived cell engineered to expresses AAV helper functions (rep and cap) upon induction by adenovirus helper functions.45 HEK293 is derived from human embryonic kidney transformed by adenovirus type 5 DNA, and RAW264.7 is a mouse macrophage cell line derived from Abelson murine leukemia virus–induced tumor in BALB/c mice (American Type Culture Collection, Manassas, VA).
Gene construction. The protein sequences of PA63, the C-terminal fragment resulting from proteolytic cleavage of B. anthracis PA (GenBank P13423, residues 197–764), and LF (GenBank P15917) were reverse-translated with codon usage optimized for human expression, and were synthesized commercially (GenScript, Piscataway, NJ). The LF sequence contains a substitution of alanine for tyrosine at residue 236 (Y236A), which eliminates the ability for LF to bind to PA.29 Each gene includes a consensus Kozak sequence and synthetic leader. These constructs were cloned between AAV2 inverted terminal repeats using flanking NotI restriction enzyme sites in a plasmid derived from pCMVβ (Clontech Laboratories, Mountain View, CA). SmaI restriction enzyme digestion was used to confirm inverted terminal repeat integrity. eGFP was cloned into pCMVβ in the same manner. Expression of DNA plasmids was tested by transient transfection of C12 cells using SuperFect transfection reagent (Qiagen, Valencia, CA).46 Cell lysate was collected 48 hours after transfection and analyzed by western blotting.
rAAV vector production. A modified cross-packaging method was used to produce the rAAV vectors.47 This approach allows the AAV2 vector genome to be packaged into different AAV capsid serotypes. rAAV vectors were produced by using HEK293 cells with a standard triple plasmid DNA/CaPO4 precipitation method. HEK293 cells were maintained in Dulbecco's modified Eagle's medium (Mediatech, Manassas, VA) with 10% fetal bovine serum, penicillin, and streptomycin at 37 °C with 5% CO2. The plasmids used in production were: pCMV-PA, pCMV-LF, or pCMV-eGFP, each encoding an immunogen of interest; rep2-capX modified AAV helper plasmid encoding the serotype 1 capsid protein; and an adenovirus type 5 helper plasmid (pAdhelper) bearing the adenovirus E2A, E4 ORF6, and VA I/II RNA genes. Vector genome titer was determined by a quantitative real-time PCR method using Prism 7500 TaqMan detector system (Applied Biosystems, Foster City, CA),48 using a primer pair and fluorescent probe targeting the CMV promoter as described.49 To confirm expression of the immunogens in mammalian cells, C12 cells were infected with rAAV1/ PA, LF, or eGFP in the presence of pAdhelper. The cell lysates were collected and assayed by western blotting.
Western blot analysis. Samples were boiled at 95°C for 5 minutes, run in a 7.5 or 12% polyacrylamide Tris–Acetate gel (Bio-Rad, Carlsbad CA) and then electroblotted at 4 °C to a polyvinylidene fluoride membrane (GE Healthcare, Piscataway, NJ) for 1 hour at 100 V. After blocking in 5% nonfat dry milk in TBST (100 mmol/l Tris–HCl, pH 8.0, 167 mmol/l NaCl, 0.1% Tween) at room temperature for 1 hour, the membrane was incubated with diluted primary antibody in TBST/5% dry milk overnight at 4 °C. Primary antibodies included PA- and LF-specific rabbit antiserum used at 1:5,000 and rabbit anti-eGFP used at 1:200 (BioVision, Mountain View, CA). Peroxidase-labeled anti-rabbit IgG antibody was used for ECL immunodetection in accordance with the manufacturer's instructions (GE Healthcare, Piscataway, NJ).
Immunization of animals and sample collection. Female New Zealand White rabbits, six animals per group, were immunized on day 0 with rAAV1 expressing PA63, LF, or eGFP as shown in Table 1. Rabbits were anesthetized prior to immunization and the skin surface at the targeted leg area shaved. Each inoculation was administered IM in the quadriceps of the hind leg of rabbits and consisted of 3 × 1011 DNA resistant particles in a volume of 200 µl. Serum samples were collected prior to the first immunization (day 0) and then at 2-, 4-, 8-, 12-, and 16-week time points. For the procurement of positive control hyperimmune anti-PA and anti-LF serum for use in the western blotting and as positive controls for the LeTx neutralization assays, rabbits were immunized with 250 µg of either soluble PA83 or LF in an emulsion with CFA (List Biological Laboratories, Campbell, CA). Rabbits were then boosted three times at 2–3-week intervals with 125 µg of the respective immunogens in an emulsion with incomplete Freund's adjuvant (Covance Research Products, Denver, PA). Both PA-immune rabbits had end-point ELISA titers of 262,144 and both LF-immune rabbits had end-point ELISA titers of 524,288. All animal procedures were approved by the Institutional Animal Care and Use Committee and were performed in facilities accredited by the Association for the Assessment and Accreditation of Laboratory Animal Care, International.
ELISA analysis. Individual rabbit antisera were analyzed in duplicate by ELISA as described previously.50 For analysis of antibodies specific for the PA or LF proteins, wells of microtiter plates (Immulon 2; Thermo Labsystems, Franklin MA) were coated overnight at 4°C with 100 ng of PA83 or LF (List Biological Laboratories, Campbell, CA) in a 0.05 mol/l carbonate buffer pH 9.5. Bound antibody was detected with secondary biotinylated antibody specific for rabbit IgG (Southern Biotechnology, Birmingham, AL) followed by streptavidin–alkaline phosphatase and 4-nitrophenylphosphate (Roche, Indianapolis, IN). Absorbance at 405 nm minus absorbance at 650 nm was determined using an ELISA reader (Emax microplate reader; Molecular Devices, Menlo Park, CA). End-point titers were defined as the highest dilution yielding twice the absorbance of an irrelevant immune serum at the same dilution.
Anthrax LeTx-neutralizing assay (TNA). The ability of antibody to block LeTx action in vitro was assessed using RAW264.7 cells. Cells were grown in culture in Dulbecco's modified Eagle's medium with 10% fetal bovine serum, Penicillin–Streptomycin, and 50 µmol/l 2-mercaptoethanol (complete medium) in a humidified 6.5% CO2 incubator. Complete medium was used for dilution of all assay reagents. For each experiment, cells were harvested using 3 mmol/l EDTA, washed with Dulbecco's modified Eagle's medium, and plated at 30 × 103 cells/well in 96-well flat-bottom plates for overnight culture (Costar 3596; Corning, Corning, NY). The following day, heat-denatured rabbit antisera were serially diluted in polypropylene round-bottom 96-well plates in a final volume of 50 µl per well. LeTx reagent containing PA83 and LF in complete medium was prepared at a twice-final (2×) concentration, with the final concentration representing 2.5–3.5 multiples of the amount needed to kill 50% of the RAW264 cells. The second component of the binary LeTx complex was included in excess. Each TNA assay was validated by a contemporaneous PA or LF titration. For PA neutralization studies, 110 ng/ml PA83 was used along with 150 ng of LF. For LF neutralization studies, 20 ng/ml LF and 150 ng/ml PA were used. The diluted rabbit antiserum was added to the LeTx and the mixture was incubated for 30 minutes before transferring to the RAW 264 cells in exchange for the preexisting medium. Following a 4-hour incubation, 20 µl of MTS reagent was added to each well (CellTiter96 AQ; Promega, Madison, WI), and after an additional 2-hour incubation, the absorbance at 405 nm minus absorbance at 650 nm was determined for each plate using a Vmax plate reader. The 50% effective concentration was determined for each serum by using nonlinear regression to fit a variable slope sigmoidal equation to the serial dilution data set using Prism 4.0 (GraphPad Software, San Diego, CA). All assays were performed using hyperimmune rabbit sera raised against either full length PA83 or LF as a control. TNA results are expressed as a percentage of the control anti-PA or anti-LF neutralization, which was determined to be the mean TNA titer from the two soluble PA- or LF-immune rabbits.
Statistics. Geometric mean antibody and LeTx neutralization titers from monovalent and bivalently inoculated rabbits were compared at each serum time point using the two-tailed Student's t-test and differences were considered significant at P < 0.05 (Prism software 5.0; GraphPad, San Diego, CA).
Acknowledgments
This work was supported by the National Institutes of Health U01-AI56480. This work was also supported in part with resources and the use of facilities at the Veterans Administration Healthcare System, Ann Arbor.
REFERENCES
- Hudson MJ, Beyer W, Bohm R, Fasanella A, Garofolo G, Golinski R, et al. Bacillus anthracis: balancing innocent research with dual-use potential. Int J Med Microbiol. 2008;298:345–364. doi: 10.1016/j.ijmm.2007.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collier RJ., and , Young JA. Anthrax toxin. Annu Rev Cell Dev Biol. 2003;19:45–70. doi: 10.1146/annurev.cellbio.19.111301.140655. [DOI] [PubMed] [Google Scholar]
- Moayeri M., and , Leppla SH. The roles of anthrax toxin in pathogenesis. Curr Opin Microbiol. 2004;7:19–24. doi: 10.1016/j.mib.2003.12.001. [DOI] [PubMed] [Google Scholar]
- Dixon TC, Meselson M, Guillemin J., and , Hanna PC. Anthrax. N Engl J Med. 1999;341:815–826. doi: 10.1056/NEJM199909093411107. [DOI] [PubMed] [Google Scholar]
- Turnbull PC, Leppla SH, Broster MG, Quinn CP., and , Melling J. Antibodies to anthrax toxin in humans and guinea pigs and their relevance to protective immunity. Med Microbiol Immunol. 1988;177:293–303. doi: 10.1007/BF00189414. [DOI] [PubMed] [Google Scholar]
- Pezard C, Weber M, Sirard JC, Berche P., and , Mock M. Protective immunity induced by Bacillus anthracis toxin-deficient strains. Infect Immun. 1995;63:1369–1372. doi: 10.1128/iai.63.4.1369-1372.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Price BM, Liner AL, Park S, Leppla SH, Mateczun A., and , Galloway DR. Protection against anthrax lethal toxin challenge by genetic immunization with a plasmid encoding the lethal factor protein. Infect Immun. 2001;69:4509–4515. doi: 10.1128/IAI.69.7.4509-4515.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taft SC., and , Weiss AA. Role of vaccine-induced antibodies to anthrax lethal and edema toxin. Clin Vaccine Immunol. 2007;15:71–75. doi: 10.1128/CVI.00321-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherer K, Li Y, Cui X., and , Eichacker PQ. Lethal and edema toxins in the pathogenesis of Bacillus anthracis septic shock: implications for therapy. Am J Respir Crit Care Med. 2007;175:211–221. doi: 10.1164/rccm.200608-1239CP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cui X, Li Y, Li X, Laird MW, Subramanian M, Moayeri M, et al. Bacillus anthracis edema and lethal toxin have different hemodynamic effects but function together to worsen shock and outcome in a rat model. J Infect Dis. 2007;195:572–580. doi: 10.1086/510856. [DOI] [PubMed] [Google Scholar]
- Puziss M., and , Wright GG. Studies on immunity in anthrax. X Gel-adsorbed protective antigen for immunization of man. J Bacteriol. 1963;85:230–236. doi: 10.1128/jb.85.1.230-236.1963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ivins BE, Pitt ML, Fellows PF, Farchaus JW, Benner GE, Waag DM, et al. Comparative efficacy of experimental anthrax vaccine candidates against inhalation anthrax in rhesus macaques. Vaccine. 1998;16:1141–1148. doi: 10.1016/s0264-410x(98)80112-6. [DOI] [PubMed] [Google Scholar]
- Pitt ML, Little SF, Ivins BE, Fellows P, Barth J, Hewetson J, et al. In vitro correlate of immunity in a rabbit model of inhalational anthrax. Vaccine. 2001;19:4768–4773. doi: 10.1016/s0264-410x(01)00234-1. [DOI] [PubMed] [Google Scholar]
- Fellows PF, Linscott MK, Ivins BE, Pitt ML, Rossi CA, Gibbs PH, et al. Efficacy of a human anthrax vaccine in guinea pigs, rabbits, and rhesus macaques against challenge by Bacillus anthracis isolates of diverse geographical origin. Vaccine. 2001;19:3241–3247. doi: 10.1016/s0264-410x(01)00021-4. [DOI] [PubMed] [Google Scholar]
- Brachman PS, Gold H, Plotkin SA, Fekety FR, Werrin M., and , Ingraham NR. Field evaluation of a human anthrax vaccine. Am J Public Health Nations Health. 1962;52:632–645. doi: 10.2105/ajph.52.4.632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- FDA Biological products; bacterial vaccines and toxoids; implementation of efficacy review; anthrax vaccine adsorbed; final order. Fed Regist. 2005;70:75180–75198. [PubMed] [Google Scholar]
- Demicheli V, Rivetti D, Deeks JJ, Jefferson T., and , Pratt M. The effectiveness and safety of vaccines against human anthrax: a systematic review. Vaccine. 1998;16:880–884. doi: 10.1016/s0264-410x(98)00023-1. [DOI] [PubMed] [Google Scholar]
- Sever JL, Brenner AI, Gale AD, Lyle JM, Moulton LH., and , West DJ. Safety of anthrax vaccine: a review by the Anthrax Vaccine Expert Committee (AVEC) of adverse events reported to the Vaccine Adverse Event Reporting System (VAERS) Pharmacoepidemiol Drug Saf. 2002;11:189–202. doi: 10.1002/pds.712. [DOI] [PubMed] [Google Scholar]
- Pittman PR, Kim-Ahn G, Pifat DY, Coonan K, Gibbs P, Little S, et al. Anthrax vaccine: immunogenicity and safety of a dose-reduction, route-change comparison study in humans. Vaccine. 2002;20:1412–1420. doi: 10.1016/s0264-410x(01)00462-5. [DOI] [PubMed] [Google Scholar]
- Joellenbeck JM, Zwanziger LL, Durch JS., and , Strom BL. The Anthrax Vaccine: Is it safe? Does it work. National Academies Press: Washington, DC; 2002. [PubMed] [Google Scholar]
- Grimm D., and , Kay MA. From virus evolution to vector revolution: use of naturally occurring serotypes of adeno-associated virus (AAV) as novel vectors for human gene therapy. Curr Gene Ther. 2003;3:281–304. doi: 10.2174/1566523034578285. [DOI] [PubMed] [Google Scholar]
- Tenenbaum L, Lehtonen E., and , Monahan PE. Evaluation of risks related to the use of adeno-associated virus-based vectors. Curr Gene Ther. 2003;3:545–565. doi: 10.2174/1566523034578131. [DOI] [PubMed] [Google Scholar]
- Coura Rdos S., and , Nardi NB. The state of the art of adeno-associated virus-based vectors in gene therapy. Virol J. 2007;4:99. doi: 10.1186/1743-422X-4-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manning WC, Paliard X, Zhou S, Pat Bland M, Lee AY, Hong K, et al. Genetic immunization with adeno-associated virus vectors expressing herpes simplex virus type 2 glycoproteins B and D. J Virol. 1997;71:7960–7962. doi: 10.1128/jvi.71.10.7960-7962.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu X, Voulgaropoulou F, Chen R, Johnson PR., and , Clark KR. Selective Rep-Cap gene amplification as a mechanism for high-titer recombinant AAV production from stable cell lines. Mol Ther. 2000;2:394–403. doi: 10.1006/mthe.2000.0132. [DOI] [PubMed] [Google Scholar]
- Johnson PR, Schnepp BC, Connell MJ, Rohne D, Robinson S, Krivulka GR, et al. Novel adeno-associated virus vector vaccine restricts replication of simian immunodeficiency virus in macaques. J Virol. 2005;79:955–965. doi: 10.1128/JVI.79.2.955-965.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuck D, Lau T, Leuchs B, Kern A, Muller M, Gissmann L, et al. Intranasal vaccination with recombinant adeno-associated virus type 5 against human papillomavirus type 16 L1. J Virol. 2006;80:2621–2630. doi: 10.1128/JVI.80.6.2621-2630.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palmiter RD, Sandgren EP, Avarbock MR, Allen DD., and , Brinster RL. Heterologous introns can enhance expression of transgenes in mice. Proc Natl Acad Sci USA. 1991;88:478–482. doi: 10.1073/pnas.88.2.478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lacy DB, Mourez M, Fouassier A., and , Collier RJ. Mapping the anthrax protective antigen binding site on the lethal and edema factors. J Biol Chem. 2002;277:3006–3010. doi: 10.1074/jbc.M109997200. [DOI] [PubMed] [Google Scholar]
- Ferrari FK, Samulski T, Shenk T., and , Samulski RJ. Second-strand synthesis is a rate-limiting step for efficient transduction by recombinant adeno-associated virus vectors. J Virol. 1996;70:3227–3234. doi: 10.1128/jvi.70.5.3227-3234.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brockstedt DG, Podsakoff GM, Fong L, Kurtzman G, Mueller-Ruchholtz W., and , Engleman EG. Induction of immunity to antigens expressed by recombinant adeno-associated virus depends on the route of administration. Clin Immunol. 1999;92:67–75. doi: 10.1006/clim.1999.4724. [DOI] [PubMed] [Google Scholar]
- Xin KQ, Urabe M, Yang J, Nomiyama K, Mizukami H, Hamajima K, et al. A novel recombinant adeno-associated virus vaccine induces a long-term humoral immune response to human immunodeficiency virus. Hum Gene Ther. 2001;12:1047–1061. doi: 10.1089/104303401750214276. [DOI] [PubMed] [Google Scholar]
- Xin KQ, Ooki T, Mizukami H, Hamajima K, Okudela K, Hashimoto K, et al. Oral administration of recombinant adeno-associated virus elicits human immunodeficiency virus-specific immune responses. Hum Gene Ther. 2002;13:1571–1581. doi: 10.1089/10430340260201662. [DOI] [PubMed] [Google Scholar]
- Xin KQ, Mizukami H, Urabe M, Toda Y, Shinoda K, Yoshida A, et al. Induction of robust immune responses against human immunodeficiency virus is supported by the inherent tropism of adeno-associated virus type 5 for dendritic cells. J Virol. 2006;80:11899–11910. doi: 10.1128/JVI.00890-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logan GJ, Wang L, Zheng M, Cunningham SC, Coppel RL., and , Alexander IE. AAV vectors encoding malarial antigens stimulate antigen-specific immunity but do not protect from parasite infection. Vaccine. 2007;25:1014–1022. doi: 10.1016/j.vaccine.2006.09.072. [DOI] [PubMed] [Google Scholar]
- Mueller C., and , Flotte TR. Clinical gene therapy using recombinant adeno-associated virus vectors. Gene Ther. 2008;15:858–863. doi: 10.1038/gt.2008.68. [DOI] [PubMed] [Google Scholar]
- Du L, Zhao G, Lin Y, Sui H, Chan C, Ma S, et al. Intranasal vaccination of recombinant adeno-associated virus encoding receptor-binding domain of severe acute respiratory syndrome coronavirus (SARS-CoV) spike protein induces strong mucosal immune responses and provides long-term protection against SARS-CoV infection. J Immunol. 2008;180:948–956. doi: 10.4049/jimmunol.180.2.948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallez-Hawkins G, Li X, Franck AE, Thao L, Lacey SF, Diamond DJ, et al. DNA and low titer, helper-free, recombinant AAV prime-boost vaccination for cytomegalovirus induces an immune response to CMV-pp65 and CMV-IE1 in transgenic HLA A*0201 mice. Vaccine. 2004;23:819–826. doi: 10.1016/j.vaccine.2004.06.048. [DOI] [PubMed] [Google Scholar]
- Little SF, Ivins BE, Fellows PF., and , Friedlander AM. Passive protection by polyclonal antibodies against Bacillus anthracis infection in guinea pigs. Infect Immun. 1997;65:5171–5175. doi: 10.1128/iai.65.12.5171-5175.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pitt ML, Little S, Ivins BE, Fellows P, Boles J, Barth J, et al. In vitro correlate of immunity in an animal model of inhalational anthrax. J Appl Microbiol. 1999;87:304. doi: 10.1046/j.1365-2672.1999.00897.x. [DOI] [PubMed] [Google Scholar]
- Hermanson G, Whitlow V, Parker S, Tonsky K, Rusalov D, Ferrari M, et al. A cationic lipid-formulated plasmid DNA vaccine confers sustained antibody-mediated protection against aerosolized anthrax spores. Proc Natl Acad Sci USA. 2004;101:13601–13606. doi: 10.1073/pnas.0405557101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu Q., and , Zeng M. Detoxified lethal toxin as a potential mucosal vaccine against anthrax. Clin Vaccine Immunol. 2008;15:612–616. doi: 10.1128/CVI.00402-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gu ML, Leppla SH., and , Klinman DM. Protection against anthrax toxin by vaccination with a DNA plasmid encoding anthrax protective antigen. Vaccine. 1999;17:340–344. doi: 10.1016/s0264-410x(98)00210-2. [DOI] [PubMed] [Google Scholar]
- Galloway D, Liner A, Legutki J, Mateczun A, Barnewall R., and , Estep J. Genetic immunization against anthrax. Vaccine. 2004;22:1604–1608. doi: 10.1016/j.vaccine.2003.09.043. [DOI] [PubMed] [Google Scholar]
- Clark KR, Voulgaropoulou F., and , Johnson PR. A stable cell line carrying adenovirus-inducible rep and cap genes allows for infectivity titration of adeno-associated virus vectors. Gene Ther. 1996;3:1124–1132. [PubMed] [Google Scholar]
- Clark KR, Voulgaropoulou F, Fraley DM., and , Johnson PR. Cell lines for the production of recombinant adeno-associated virus. Hum Gene Ther. 1995;6:1329–1341. doi: 10.1089/hum.1995.6.10-1329. [DOI] [PubMed] [Google Scholar]
- Rabinowitz JE, Rolling F, Li C, Conrath H, Xiao W, Xiao X, et al. Cross-packaging of a single adeno-associated virus (AAV) type 2 vector genome into multiple AAV serotypes enables transduction with broad specificity. J Virol. 2002;76:791–801. doi: 10.1128/JVI.76.2.791-801.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark KR, Liu X, McGrath JP., and , Johnson PR. Highly purified recombinant adeno-associated virus vectors are biologically active and free of detectable helper and wild-type viruses. Hum Gene Ther. 1999;10:1031–1039. doi: 10.1089/10430349950018427. [DOI] [PubMed] [Google Scholar]
- Schnepp BC, Clark KR, Klemanski DL, Pacak CA., and , Johnson PR. Genetic fate of recombinant adeno-associated virus vector genomes in muscle. J Virol. 2003;77:3495–3504. doi: 10.1128/JVI.77.6.3495-3504.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oscherwitz J, Hankenson FC, Yu F., and , Cease KB. Low-dose intraperitoneal Freund's adjuvant: toxicity and immunogenicity in mice using an immunogen targeting amyloid-beta peptide. Vaccine. 2006;24:3018–3025. doi: 10.1016/j.vaccine.2005.10.046. [DOI] [PubMed] [Google Scholar]