Abstract
The consistency of neuropsychological outcome following circumscribed damage to the prefrontal cortex (PFC) in the first years of life has not been systematically investigated. On the basis of a single well-studied case, Ackerly and Benton (1948) postulated that the core profile involves development of a primary social defect in the context of generally normal intellectual abilities. We evaluated the consistency of this profile across all patients in our registry who had focal PFC damage acquired between the prenatal period and 62 months of age (N=7). Clinical ratings based on detailed evaluations, parental ratings, and neuropsychological testing confirmed this general profile in 5 of the 7 patients. The impairments of social function were evident in early childhood and persisted into adult life. Of the two patients who did not fit this profile, one had significant social impairment in the context of broader cognitive deficits, and one had no significant impairment of social or intellectual function. The profile was not observed in a comparison group with childhood-onset nonfrontal lesions. These findings support the notion that focal damage to PFC in the first years of life leads to the development of substantial impairment of social competencies, albeit with some variability in outcome. Further, the findings highlight the importance of emotional dysfunction and poor behavior regulation in the development of these impairments. Our studies recapitulate and confirm the core messages set forth by Ackerly and Benton more than a half-century ago.
At the 1947 meeting of the Association for Research in Nervous and Mental Disease, Spafford Ackerly and Arthur Benton presented their seminal report on the long-term developmental consequences of childhood-onset damage to prefrontal cortex (PFC) (Ackerly & Benton, 1948). This rich description of the life history, cognitive profile, and behavior of patient JP was especially important due to a rarity at the time – anatomical description of the lesion location – accomplished by means of pneumoencephalogram and an exploratory surgery. This report provided compelling support for a causal link between damage to the PFC early in life and subsequent abnormal development of social competencies, while retaining relatively normal development of most other aspects of cognition. Ackerly and Benton concluded that the frontal lobes are critical for the development of the abilities necessary for normal social functioning, and particularly for the integration of social experiences over the course of childhood, as required for normal personality development. The authors were careful to qualify their conclusions, however, noting that, “… not until more cases like this which have been damaged at birth or at early age are studied and reported with an eye to similarities, can it find a place in our neuropsychiatric classification” (p. 500). Despite the growing appreciation over the subsequent 60 years that early dysfunction in PFC likely plays a role in a number of developmental neuropsychiatric disorders, no study to date has attempted a systematic evaluation of the consistency or “similarities” of outcomes following early PFC damage. The current study was designed to address this charge.
To set the stage for the current report, it is worth revisiting the Ackerly and Benton case in some detail. JP was 35 years old at the time of the original report, and was described as giving “… the appearance of an alert, intelligent, responsive individual” (the identifying initials “JP” were not used in the original paper, but were introduced in 1964 follow-up report by Ackerly). JP was born in 1912 to “respectable parents of middle economic status,” and his family history was unremarkable. His birth involved prolonged labor and an instrumental delivery. He became severely jaundiced at 9 days of age and lost considerable weight, but then appeared to fully recover, and his early developmental milestones were achieved at a normal rate. His early medical history was notable for falling off a bed while playing at the age of four years. He struck his head on the floor, with no immediate consequences, but approximately one hour later began acting and talking strangely, followed by loss of consciousness and left side convulsions for approximately 4 hours. He then appeared to fully recover, and was discharged from the hospital the next morning. This event was considered as the possible cause of the prefrontal lesion which was detected 17 years later, although it was thought to be more likely that the lesion was congenital in nature, because of the minor nature of the fall and the fact that some aberrant behaviors appeared prior to this event.
The earliest behavioral abnormality noted was JP’s tendency to wander long distances, and as it turned out, wandering was one of JP’s most distinguishing traits. By the time he was 2-3 years old, he was repeatedly found long distances from home (more than 1 mile), showing no fear of being lost. Neither scoldings nor “relatively severe whippings” from his father had any impact on this behavior. This habit of wandering persisted into adulthood, with later trips of thousands of miles without clear destinations. Another notable behavior that appeared early and persisted into adulthood was JP’s tendency to employ overly polite and superficial manners (“Chesterfieldian manners”), particularly when dealing with adults or authority figures. However, he was “heartily disliked” by his peers, and noted to be boastful and bossy with other children. He would generally deny any wrongdoing, no matter how strong the evidence, and was quick to blame others for his misdeeds.
Entering his school years, JP “… was in difficulties from the day school began,” with frequent conduct problems and inappropriate behaviors such as public masturbation and confrontations with his schoolmates. These behaviors led to expulsion from public school and referral to mental health professionals at age 13. He remained under frequent professional observation and evaluation from that time on. The common conclusion from these evaluations was that his “social adjustment was extremely poor,” and that his problem behaviors were refractory to treatment. Multiple psychological and neuropsychological evaluations revealed generally average level intellectual abilities and an absence of typical “organic” signs, although there was some impairment in planning capacity and the ability to organize behavior to obtain long-term goals. Overall, JP’s real-world behavioral impairments greatly exceeded the relatively minor cognitive deficits suggested by the psychometric evidence. In school, he demonstrated generally good competencies in academic subjects, but required near constant supervision if he was to remain on task.
As an adolescent and young adult, he repeatedly stole cars (for joyrides, not for profit), was unable to hold a job for more than a few months, and remained socially isolated. Personality evaluation at age 20 showed:
“… the same over-polite, boastful, somewhat overtalkative individual, with no evidence of anxiety, conversion symptoms, hallucinations, delusions, illusions or bizarre ideas. He showed no memory difficulty. He planned poorly for the future and was quite definitely impulsive. He spent money unwisely, had ‘big ideas’ (none of which reached even the planning stage). He showed a poorly developed sense of responsibility.” (p. 489)
JP was noted to be “quick to flare up,” but he also “quickly recovered from disappointments and showed no lasting resentments.” Ackerly (1964) described general stability in his basic personality profile throughout adulthood, up to at least 50 years of age.
Because of the history of head trauma followed by convulsions in childhood, a pneumoencephalographic study was conducted upon his admission to the Psychopathic Ward of the Louisville General Hospital in 1933. The pneumonencephalogram showed ventricular enlargement, particularly in the anterior horn of the left lateral ventricle, and “a large area of destruction in the left frontal lobe.” Two weeks later, an exploratory surgery provided a more detailed view of the injury. The surgeon, Dr. R. Glen Spurling, entered through a left frontal bone flap, noting that “the cortex of the left frontal lobe was found to be markedly compressed by an adherent type of arachnoiditis.” However, when he pulled back the atrophied left frontal lobe, “… a bulging mass from the right frontal fossa was opened. Much to my surprise, the right frontal fossa was entirely devoid of cortical tissue. It was occupied by a large collection of fluid which was distinctly yellow. I was never able to identify cortical tissue on the right of the midline through my exposure from the left frontal region. Undoubtedly there was an absence or a tremendously atrophied frontal lobe on the right side” (p. 480).
Although the similarities between JP and patients with documented adult-onset PFC damage (particularly Brickner’s patient A) provided some support for the validity of Ackerly and Benton’s conclusions, for many years the case of JP stood alone as the only detailed evidence that early damage to PFC appeared to have a devastating impact on the development of personality, emotion, and social behavior. When Benton (1991) revisited this issue more than four decades after the initial report, he noted the continued absence of new case reports, but predicted, “It is reasonable to expect that the extreme paucity of informative case material found in the literature will be alleviated with the advent of neurodiagnostic procedures such as CT scan, magnetic resonance imaging, cerebral blood flow determinations, and electrophysiologic measures.”
Showing his characteristic perseverance, Benton again revisited the issue in 2004, in a literature review co-authored with his student Paul Eslinger and Claire Flaherty-Craig (Eslinger et al., 2004). As Benton had predicted, the situation had improved, with 9 new cases of childhood-onset frontal lobe injury described in the literature. The combined findings from these reports lent considerable support to the notion that early PFC damage is followed by impaired development of social competencies, and also pointed to a particularly important role of anterior, orbital, and medial PFC regions in these deficits.
Although the number of well-studied cases of circumscribed childhood-onset PFC damage remains limited, and much remains to be learned about the course of development and underlying neuropsychological mechanisms following such damage, there now is little question that early dysfunction in this region can have major implications for social and emotional development. To date, however, no study has specifically addressed the consistency of the core findings of the Ackerly and Benton report in a series of comparably studied patients.
The purpose of the present study was to determine the extent to which the neuropsychological profile described by Ackerly and Benton would be replicated in a systematically studied series of comparable patients with focal damage in the PFC acquired in the first years of life. Taking all patients in our registry who met this core criterion, we focused on the 6 behavioral characteristics of JP highlighted by Benton (1991): 1) generally normal intellectual development, 2) lack of anxiety and concern, 3) impulsivity and emotional instability, 4) inappropriate sexual conduct, 5) empty and inappropriate boastfulness, and 6) superficial politeness and proper manners. The criteria for inclusion in this study were designed to match the essential characteristics of patient JP, namely: a) damage to PFC acquired during the first years of life, b) no significant damage to other brain regions, and c) no family history of serious mental illness. It was further required that a parent be available for interview and to complete questionnaires. No requirement was made regarding the patients’ current age. Thus, certain of the behavioral characteristics (e.g., sexual conduct) could not be evaluated in the younger patients.
METHODS
Patients
Seven patients from the Patient Registry at the Department of Neurology at the University of Iowa Carver College of Medicine met the aforementioned criteria, and were selected for participation (Table 1). The 7 patients (4M/3F) ranged in age from 4 to 32 years at the time of their most recent evaluation in our laboratory, and all were evaluated on at least two occasions separated by at least one year. The time of onset of damage to PFC ranged from the prenatal period to 62 months of age. All were right-handed. A comparison group included 7 patients (6M/1F), ranging in age from 5 to 51 years, with non-frontal brain damage acquired in childhood. It was required that no involvement of the frontal lobes was evident on MRI. The injuries were caused by stroke, herpes simplex encephalitis, trauma, and resection of a benign tumor, and variously involved the temporal, parietal, and occipital regions (3 right hemisphere, 2 left, and 2 bilateral).
Table 1. Demographic and clinical characteristics.
| Patient # | Etiology |
Age at Onset |
Current Age (yrs.) |
Sex |
|---|---|---|---|---|
| 1 | stroke | prenatal | 30 | M |
| 2 | resection (angioma) |
birth | 4 | M |
| 3 | resection (abscess) |
7 days | 6 | F |
| 4 | resection (benign tumor) |
3 mo. | 32 | M |
| 5 | trauma | 16 mo. | 28 | F |
| 6 | trauma | 56 mo. | 17 | M |
| 7 | resection (AVM) |
62 mo | 9 | F |
Note. Patients are listed according to age at the time of lesion onset. AVM=arteriovenous malformation.
Neuroanatomical analysis of the lesions
The neuroanatomical analysis was based on magnetic resonance (MR) data. For five of the seven participants with PFC damage, as part of the research protocol, thin-cut, contiguous T1-weighted coronal cuts were obtained either in a General Electric scanner operating at 1.5 Tesla using the 3D SPGR sequence or in a Siemens Trio scanner operating at 3.0 Tesla using the 3D MPRAGE sequence. These data were then used to generate a 3-dimensional reconstruction of each participant’s brain using Brainvox (Damasio and Frank, 1992; Frank et al., 1997). For the two youngest subjects (2 and 3) MR data obtained for clinical purposes were utilized as research scans could not be obtained due to the need for sedation.
Two investigators with anatomical expertise and who were blind to the neuropsychological data visually inspected each MR data set to determine the lesion boundaries and extent of involvement within 10 subregions of the frontal cortex (see Figure 1). Notably, in their original paper, Ackerly and Benton did not discuss the precise locus of damage within the prefrontal cortex; however, subsequent research has highlighted the importance of prefrontal regions such as the ventromedial and polar regions (e.g., Anderson et al., 1999), and thus we chose to code lesion damage with regard to these key subregions. For each patient, the extent of damage in these 10 subregions was coded as having no damage, partial damage (less than 75% damaged), or severe damage (75% or greater).
Figure 1. Anatomical subdivisions of the frontal cortex.
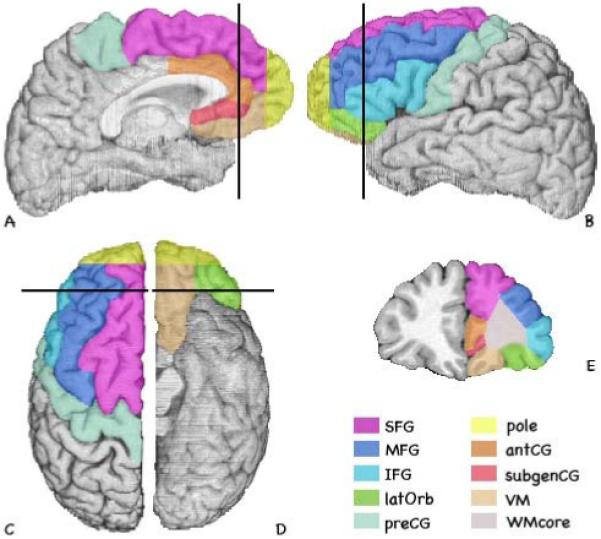
Note: SFG = superior frontal gyrus; pole = frontal pole; MFG = middle frontal gyrus; antCG = anterior cingulate gyrus; IFG = inferior frontal gyrus; subgenCG = subgenu cingulate gyrus; latOrb = orbital gyrus (lateral portion); VM = orbital gyrus (medial portion) and gyrus rectus (including the aspect on the medial surface), considered together; preCG = precentral gyrus; WMcore = prefrontal white matter core.
The results from this analysis are are provided in Table 2 and Figure 1. Four participants had bilateral damage to PFC, and 3 had unilateral right PFC damage. For five of the seven participants, the damage was limited to prefrontal regions described in Table 2; however, two participants had additional limited damage outside of the frontal lobe. This included patient 6, who had partial damage involving the temporal pole on the right, and patient 7, who had partial damage involving the anterior sector of the extreme and external capsules on the right. Across all of the participants, the regions that were most frequently damaged were the frontal pole and the white matter core, with most participants incurring damage to both (at least within a single hemisphere) and no participant without damage to either region.
Table 2. Neuroanatomical Data.
The extent of damage in each region of the frontal lobe is reported for each patient
| Frontal Pole |
Lateral | White Matter (core) |
Mesial | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Precentral | SFG | MTG | IFG | Orbital | SFG | Anterior Cingulate |
Subgenual Cingulate |
Ventral -medial |
||||||||||||||
| R | L | R | L | R | L | R | L | R | L | R | L | R | L | R | L | R | L | R | L | R | L | |
| 1 | 2 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 1 | 1 | 1 | 0 | 2 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 1 | 0 |
| 2 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 3 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 4 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 1 | 0 | 1 | 0 | 1 | 0 | 1 | 0 | 1 | 0 | 1 | 0 | 0 | 0 |
| 5 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 |
| 6 | 2 | 1 | 0 | 0 | 1 | 0 | 1 | 0 | 2 | 0 | 2 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 0 |
| 7 | 2 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 1 | 0 | 1 | 0 | 1 | 0 | 1 | 0 | 2 | 0 |
Note: 0 = no damage; 1 = partial damage (less than 75% by visual inspection); 2 = severe damage (75% or greater by visual inspection). SFG = Superior Frontal Gyrus; MTG = Middle Frontal Gyrus; IFG = Inferior Frontal Gyrus; Orbital = Orbital Gyrus (lateral portion); Ventral-medial = Orbital Gyrus (medial portion) and Gyrus Rectus (including the aspect on the medial surface), considered together.
Intellectual assessment
Intellectual abilities were assessed with the age-appropriate versions of the Wechsler Intelligence Scales (WIPPSI-III, WISC-II or III, or WAIS-III).
Behavioral assessment
A clinical neuropsychologist aware of the purpose of this study rated each patient on the behavioral characteristics described below. The rater was familiar with each case and had access to detailed evaluations and interviews with the patient and with at least one parent of each patient, as well as medical, academic, and mental health records, This information included records of behavioral observations by several examiners (neuropsychologists and neuropsychological technicians). The rated behavioral characteristics included overall social function, in accord with Ackerly and Benton’s main conclusion of a “primary social defect”, and the six behavioral characteristics highlighted by Benton (1991). Each of these characteristics was rated as either: 0= no evidence of impairment, 1= evidence of mild impairment, or 2= evidence of severe impairment.
Overall impairment of social function: this is a summary rating of the patient’s ability to: a) fulfill normal expected age-appropriate societal roles, b) not put undue burden on his or her family or other persons, and c) comply with the laws, rules, and moral standards in effect in his or her daily environment.
Lack of anxiety and concern: this rating took into account observable physiological signs of anxiety (e.g., sweating, twitching), behavioral indications of anxiety (e.g., fidgeting, restlessness), and self-report of anxiety during evaluation, as well as reports of behavior outside of the laboratory.
Impulsivity: this rating took into account behavior that indicated a tendency to act or respond quickly and before a situation could be adequately appraised. Consideration was giving to behavior during neuropsychological testing and during interviews, as well as reports of behavior outside of the laboratory.
Emotional instability: this was defined as the expression of affect that changed quickly and/or frequently in intensity and valence, e.g., rapid onset of giddiness or sadness, easy irritability.
Inappropriate sexual conduct: this included lewd public behavior, as emphasized in the report of JP’s behavior, as well as other sexual behaviors that put the patient or others at risk, or were clearly in conflict with broadly accepted moral standards.
Inappropriate boastfulness: this was defined as expressions of grandiosity, fantastic plans for his/her personal future, and bragging of exploits and exceptional skills.
Superficial politeness: this included any excessive display of manners, politeness beyond what might be expected in a situation, or other gratuitous behavior.
In addition, parental behavior ratings were available for 3 of these traits: level of anxiety, impulsivity, and emotional instability. These characteristics were rated on the Iowa Scales of Personality Development (Anderson et al., 2006), which is a version of the Iowa Rating Scales for Personality Change (Barrash et al., 2000) modified for use with individuals with childhood-onset brain damage.
RESULTS
Intellectual assessment
Verbal (VIQ), Performance (PIQ), and Full Scale (FSIQ) IQ scores for the PFC patients are presented in Table 3. Most scores fell within the average range (6 of 7 patients on VIQ, 5 of 7 patients on PIQ, and 5 of 7 patients on FSIQ). One patient (Case 3) had significant impairments on both verbal and performance scales, and one patient (Case 1) had PIQ in the borderline range, in the context of average level verbal intellectual test performances. All patients in the comparison group had FSIQ scores in the average range or better.
Table 3. Wechsler Intelligence Scales.
| Patient | VIQ | PIQ | FSIQ |
|---|---|---|---|
| 1 | 91 | 77 | 84 |
| 2 | 104 | 87 | 96 |
| 3 | 75 | 63 | 71 |
| 4 | 94 | 104 | 98 |
| 5 | 92 | 106 | 99 |
| 6 | 104 | 107 | 106 |
| 7 | 85 | 94 | 93 |
Behavioral assessment
The behavioral ratings are presented in Table 4, and parental ratings on the ISPD are presented in Table 5.
Table 4. Behavioral ratings.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
|---|---|---|---|---|---|---|---|
| Social function | 2 | 2 | 2 | 2 | 2 | 2 | 0 |
| Lack of anxiety | 1 | 2 | 0 | 2 | 1 | 2 | 0 |
| Impulsivity | 2 | 2 | 2 | 2 | 2 | 2 | 0 |
| Emotional instability | 1 | 2 | 2 | 2 | 2 | 2 | 1 |
| Inapprop. sexual conduct | 1 | -- | -- | 2 | 2 | 1 | -- |
| Inapprop. Boastfulness | 0 | 0 | 0 | 2 | 2 | 0 | 0 |
| Superficial politeness | 1 | 0 | 0 | 1 | 0 | 0 | 0 |
Note: 0= no evidence of impairment, 1= evidence of mild impairment, or 2= evidence of severe impairment. Sexual behavior was not rated for pre-adolescents.
Table 5. Iowa Scales of Personality Development.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
|---|---|---|---|---|---|---|---|
| Anxiety | 3 | 2 | 5 | 1 | 4 | 3 | 5 |
| Impulsivity | 6 | 4 | 7 | 7 | 7 | 6 | 3 |
| Emotional instability | 5 | 7 | 7 | 7 | 7 | 6 | 4 |
Note: Each trait is rated on a 7-point scale, with 1 indicating the lowest level of that characteristic (i.e., less than what is characteristic of the hypothetical “average” or typical person) and 7 indicating the highest, most severely disturbed level.
Overall impairment of social function: Six of the 7 PFC patients had severe impairments of social function, whereas 1 patient (Case 7) had relatively normal social function. The degree of social impairment in the 6 patients who were rated as defective was such that none of the 3 adults were able to live independently, and the school-age children required behavioral intervention programs. The one PFC patient rated as unimpaired had displayed infrequent acts of aggression and threat toward her siblings, but otherwise appeared to function well in school and other social settings. In contrast, none of the comparison patients had severe impairments of social function. The 2 adults had obtained college degrees, were married, and were employed. The 5 comparison subjects in school required special educational services due to academic or perceptual difficulties; none had severe behavioral problems, but 3 of these were rated as having mild impairments of social function.
Lack of anxiety and concern: Three PFC patients were rated as showing a significant absence of anxiety, and 4 were rated as showing normal or mildly reduced anxiety. Parental ratings of anxiety on the ISPD largely concurred, with a notable lack of anxiety for 2 patients (also rated as low anxiety on clinician ratings), and relatively normal levels of anxiety for 5 patients. None of the comparison subjects showed reduced anxiety; 6 were rated as normal, and 1 had significantly elevated anxiety.
Impulsivity: Six PFC patients were rated as highly impulsive by both clinicians and their parents. These are the same 6 patients rated as having overall social impairment. Of note, 5 of these patients received ratings of 6 or 7 from their parents (with 7 indicating the highest level of impulsivity). None of the comparison patients were rated as highly impulsive. Three were rated as mildly impulsive.
Emotional instability: Five patients were rated as having severe emotional instability, and 2 with mild emotional instability. Parental ratings were highly consistent with this, with 6 of the patients being rated as having greater than normal emotional instability, and 4 of these receiving the highest possible rating. None of the comparison patients were rated as having severe emotional instability, but 2 were rated as having mild emotional instability.
Inappropriate sexual conduct: None of the patients engaged in the type of publicly lewd behavior displayed by JP. However, 2 PFC patients had clearly inappropriate sexual behavior, characterized by high-risk sexual behaviors, sex partners deemed inappropriate by their families, and undesired pregnancies. Two additional PFC patients were suspected of risky sexual behaviors, but without confirmation. Three PFC patients were pre-adolescent and were not known to engage in sexual behaviors. None of the comparison patients had inappropriate sexual behavior.
Inappropriate boastfulness: Two PFC patients displayed frequent boastful or grandiose behavior, but this was not observed or reported in the other five. None of the comparison patients showed inappropriate boastfulness.
Superficial politeness and proper manners: None of the PFC or comparison patients displayed the “Chesterfieldian manners” described by Ackerly and Benton. One PFC patient inconsistently acted in an obviously ingratiating manner to authority figures and another was considered excessively charming toward women.
DISCUSSION
Sixty years ago, Ackerly and Benton described the development of a relatively isolated social deficit following damage to PFC in early childhood. Their main conclusion, that healthy neural systems within the PFC during childhood are necessary for development of the behavioral competencies required to function in society, had major implications for understanding the neural basis of a host of developmental neuropsychiatric disorders involving problems of conduct, impulse control, and emotional regulation. Yet, their supporting data were derived from the study—detailed, to be sure—of a single remarkable case, and their conclusions were both presented and received with due caution.
The findings of the current study indicate that, although there is some variability in outcome, several important aspects of the profile of development following childhood damage to PFC, as described by Ackerly and Benton (1948), occur with high consistency. The core profile of a “primary social defect” in the context of generally normal intellectual development was found in 5 of the 7 patients in our study. Of the two patients who did not fit this profile, one also had a severe impairment of social behavior, but in the context of intellectual impairments, and one had relatively normal social and intellectual functioning. In our sample, the presence or absence of a social defect appeared to be entirely unrelated to intellectual abilities. The one patient without social impairment had a lower FSIQ than most of the socially-impaired patients. The most consistent deficits occurred in the realms of impulsivity and emotional instability. Inappropriate sexual behavior and inappropriate boastfulness were apparent in some patients, but were not consistent features. There also was variability in level of anxiety. Two patients had notable lack of anxiety, and the others had relatively normal levels of anxiety, with two of the latter group rated by their parents as having somewhat more anxiety than most children. Superficial proper manners were generally not observed.
These findings can provide additional context for considering two controversies associated with the case of JP. The first issue, raised in the discussion following presentation of the case [see box] is whether or not JP’s brain injury was confined to the frontal lobe. Although modern MRI does not eliminate the possibility of undetected minor structural abnormalities, we can speak with considerably more confidence regarding the boundaries of the lesions in our cases. All had well-defined lesions that appeared to be entirely confined to the frontal lobes (5 cases) or showed only minor extension into other brain regions (2 cases). In 2 cases, the PFC lesions resulted from trauma, raising the possibility of damage to other brain regions. However, beyond the extension into the right temporal pole in Case 6, no additional damage was evident in these cases on high resolution MRI, and they had normal cognitive abilities outside the realms of social and executive functions. It is quite clear that the primary social deficit exhibited by JP can arise from damage confined to the PFC. This behavioral profile did not occur in the non-frontal comparison group, suggesting it may be specific to early PFC damage. Although some mild but significant difficulties with social function were observed in some of the comparison patients, on the whole, this group was remarkable for their relatively normal social development despite childhood brain injuries and often significant cognitive impairments. These findings are consistent with recent findings regarding the outcome of traumatic brain injury in children, where damage to the frontal lobes, but not other brain regions, was associated with personality change (Max et al., 2006) and worse psychosocial outcome (Levin et al., 2004).
Box: Excerpt from discussion following presentation of the case of JP at the 1947 meeting of the ARNMD.
Dr. Leo. M. Davidoff (New York, N.Y.): “I should like to ask Dr. Ackerly how much gas was used in the performance of that pneumoencephalogram. It seems to me this is a most interesting case psychologically, but if enough gas had been used, the pathological process could be shown to include not only the frontal lobes, but the entire brain, including the cerebellum, and I believe that it is unsafe on the basis of this kind of case to draw conclusions as to the functions of the frontal lobes.”
The second point of uncertainty in this case is JP’s age at the time of onset of the lesion. As stated by Ackerly and Benton in their introduction, “This defect is either congenital in origin or has existed since early childhood” (p. 479), with the weight of the evidence believed to support congenital onset. Our findings are consistent with the notion that this basic neuropsychological profile can arise from damage present at birth (see the first 3 cases in Table 1). Furthermore, we have found that subtle behavioral impairments following perinatal PFC injury can be detected as early as 14 months of age, although the earliest expression of PFC damage can be difficult to discriminate from the normal emotional instability and limited behavioral regulation of early childhood (Anderson et al., 2007). Our findings also are not incompatible with the notion that JP’s deficits may have arisen from brain damage acquired at four years of age. Our patient 6, with onset at 56 months of age, displayed a similar profile to JP, and we have studied other individuals (not reported here) with PFC lesion onset in later childhood who subsequently developed a primary social defect. There are too few cases with focal PFC damage acquired during childhood reported in the literature to yet draw any firm conclusions regarding the effects of age of onset on outcome. It is clear, however, that severe social impairments may persist into adulthood from even very early PFC damage (Anderson et al., 1999), and that similar impairments may also arise from PFC injury in later childhood (Eslinger et al., 2004).
Four of our patients had bilateral PFC lesions, and all of these had substantial social impairments. The other three patients had unilateral right PFC lesions. Of these, the two males had social impairments generally comparable to those expressed by the patients with bilateral lesions. However, the remaining subject – a girl with a unilateral right PFC lesion – was the lone exception to the profile of substantial social impairment. It is possible that gender-related asymmetries in the neural systems underlying behavioral regulation conferred protection for this patient with regard to developing a primary social defect. Tranel et al. (2005) proposed that whereas the right PFC provides critical neural substrate for social/emotional function in males, it is the left PFC that is most important for these functions in females. The findings of the current study suggest that these asymmetries may be present already in early childhood.
Although the findings of the present study regarding the key outcome of a relatively isolated impairment of social function are clear, there are many interesting and important aspects of JP’s profile not considered in this analysis. We chose to follow the lead of Benton (1991) when he looked back on JP’s case four decades after the initial report, and focus on six specific behavioral characteristics in addition to the primary social defect. These six features identified in JP reflect the expression of early PFC damage in one particular individual, with the influences of factors such as his gender, home environment, and cultural context. These factors may have been particularly important in his display of Chesterfieldian manners, a characteristic not observed in any of our patients. In the modern era of more relaxed manners and decreased emphasis on formality, there would seemingly be little opportunity for most children, with or without brain injury, to learn such behaviors.
It is clear that Benton did not intend for these six features to be a definitive or comprehensive description of JP’s profile. In the same writing, he also emphasized JP’s lack of foresight, absence of depression, lack of response to punishment, and impaired self-awareness. In addition, the main concept of a primary social deficit reflects a conflation of several relatively specific behaviors, including lack of lasting friendships, blatant deception of others, disruptive behavior in school and unstable employment, and impaired moral behavior. Many of these characteristics also occur with high frequency in our patients.
As noted above, the most consistent impairments occurred in the realms of impulsivity and emotional instability. The linkage of PFC damage to poor impulse control is potentially relevant to understanding the etiology of attention-deficit/hyperactivity disorder (ADHD). PFC dysfunction plays a prominent role in most conceptualizations of the neural basis of ADHD, and it has previously been shown that damage to PFC caused by childhood trauma or stroke is associated with the development of ADHD symptomatology (Max et al., 2005a, 2005b).
A key advance in recent decades in the understanding of behavioral impairments of the type displayed by JP is growing recognition of the centrality of emotional dysfunction in the mental processes underlying the aberrant social behavior. Consistent with this, emotional dysfunction was a common and prominent feature of the patients in the present study. Their emotional dysfunction primarily involved poorly regulated and unstable emotions, and should be distinguished from emotional dysfunction in the sense of mood disorders (anxiety and depression) – which these patients were noteworthy for not having, despite major persistent problems that might be expected to elicit emotional distress.
In a series of publications beginning in the 1980s Antonio Damasio proposed the somatic marker hypothesis as a critical mechanism by which emotional information, encoded primarily as representations of body states, could become linked with memory for specific behaviors, events, people, and other stimuli on the basis of one’s learning history (for review see Damasio 1994). The PFC, particularly the orbital and medial sectors, provides essential neural infrastructure for this process. When this system is damaged in early childhood, the process of socialization, of learning right from wrong, and generally benefiting form one’s experiences with punishment and reward over the course of development is fundamentally disrupted. Emotional dysfunction (both diminished experience of emotion and emotional over-reactivity) is a strong predictor of real-world social dysfunction in patients with PFC damage (Anderson et al., 2006). Although the acquisition of social skills and social knowledge can and does advance to some extent over the course of development in persons with early PFC damage, this development is usually far from normal. Unfortunately, much as in JP’s generation, it remains the case that the impairments stemming from childhood PFC damage often persist into adulthood despite well-intended intervention, at considerable personal and societal cost.
Acknowledgments
Supported by NINDS P019632 and NIDA R01 DA022549
References
- Ackerly SS. A case of paranatal bilateral frontal lobe defect observed for thirty years. In: Warren JM, Akert K, editors. The frontal granular cortex and behavior. McGraw-Hill; New York: 1964. [Google Scholar]
- Ackerly SS, Benton AL. Report of a case of bilateral frontal lobe defect; The Frontal Lobes; Proceedings of the Association for Research in Nervous and Mental Disease 1947; Baltimore: Williams & Wilkins Co.. 1948; pp. 479–504. [PubMed] [Google Scholar]
- Anderson SW, Aksen N, Kochanska G, Damasio H, Wisnowski J, Afifi A. The earliest behavioral expression of focal damage to human prefrontal cortex. Cortex. 2007;43:806–816. doi: 10.1016/s0010-9452(08)70508-2. [DOI] [PubMed] [Google Scholar]
- Anderson SW, Barrash J, Bechara A, Tranel D. Impairments of emotion and real-world complex behavior following childhood- or adult-onset damage to ventromedial prefrontal cortex. Journal of the International Neuropsychological Society. 2006;12:224–235. doi: 10.1017/S1355617706060346. [DOI] [PubMed] [Google Scholar]
- Anderson SW, Bechara A, Damasio H, Tranel D, Damasio AR. Impairment of social and moral behavior related to early damage in the human prefrontal cortex. Nature Neuroscience. 1999;2:1032–1037. doi: 10.1038/14833. [DOI] [PubMed] [Google Scholar]
- Barrash J, Tranel D, Anderson SW. Acquired personality disturbances associated with bilateral damage to the ventromedial prefrontal region. Developmental Neuropsychology. 2000;18:355–381. doi: 10.1207/S1532694205Barrash. [DOI] [PubMed] [Google Scholar]
- Benton AL. Prefrontal injury and behavior in children. Developmental Neuropsychology. 1991;7:275–281. [Google Scholar]
- Damasio AR. Descartes’ error: Emotion, reason, and the human brain. Grosset/Putnam; New York: 1994. [Google Scholar]
- Damasio H, Frank RJ. Three-dimensional in vivo mapping of brain lesions in humans. Archives of Neurology. 1992;49:137–143. doi: 10.1001/archneur.1992.00530260037016. [DOI] [PubMed] [Google Scholar]
- Eslinger PJ, Flaherty-Craig CV, Benton AL. Developmental outcomes after early prefrontal cortex damage. Brain and Cognition. 2004;55:84–103. doi: 10.1016/S0278-2626(03)00281-1. [DOI] [PubMed] [Google Scholar]
- Frank RJ, Damasio H, Grabowski TJ. Brainvox: an interactive, multimodal visualization and analysis system for neuroanatomical imaging. Neuroimage. 1997;5:13–30. doi: 10.1006/nimg.1996.0250. [DOI] [PubMed] [Google Scholar]
- Levin HS, Zhang L, Dennis M, Ewing-Cobbs L, Schachar R, Max J, Landis JA, Roberson G, Scheibel RS, Miller DL, Hunter JV. Psychosocial outcome of TBI in children with unilateral frontal lesions. Journal of the International Neuropsychological Society. 2004;10:305–316. doi: 10.1017/S1355617704102129. [DOI] [PubMed] [Google Scholar]
- Max JE, Levin HS, Schachar RJ, Landis J, Saunders AE, Ewing-Cobbs L, Chapman SB, Dennis M. Predictors of personality change due to traumatic brain injury in children and adolescents six to twenty-four months after injury. Journal of Neuropsychiatry and Clinical Neuroscience. 2006;18:21–32. doi: 10.1176/jnp.18.1.21. [DOI] [PubMed] [Google Scholar]
- Max JE, Manes FF, Robertson BA, Mathews K, Fox PT, Lancaster J. Prefrontal and executive attention network lesions and the development of attention-deficit/hyperactivity symptomatology. Journal of the American Academy of Child and Adolescent Psychiatry. 2005;44:443–450. doi: 10.1097/01.chi.0000156661.38576.0f. [DOI] [PubMed] [Google Scholar]
- Max JE, Schachar RJ, Levin HS, Ewing-Cobbs L, Chapman SB, Dennis M, Saunders A, Landis J. Predictors of attention-deficit/hyperactivity disorder within 6 months after pediatric traumatic brain injury. Journal of the American Academy of Child and Adolescent Psychiatry. 2005;44:1032–1040. doi: 10.1097/01.chi.0000173293.05817.b1. [DOI] [PubMed] [Google Scholar]
- Tranel D, Damasio H, Denburg NL, Bechara A. Does gender play a role in functional asymmetry of ventromedial prefrontal cortex? Brain. 2005;128:2872–2881. doi: 10.1093/brain/awh643. [DOI] [PubMed] [Google Scholar]


