Abstract
Medical interactions between Black patients and nonBlack physicians are usually less positive and productive than same-race interactions. We investigated the role that physician explicit and implicit biases play in shaping physician and patient reactions in racially discordant medical interactions. We hypothesized that whereas physicians’ explicit bias would predict their own reactions, physicians’ implicit bias, in combination with physician explicit (self-reported) bias, would predict patients’ reactions. Specifically, we predicted that patients would react most negatively when their physician fit the profile of an aversive racist (i.e., low explicit-high implicit bias). The hypothesis about the effects of explicit bias on physicians’ reactions was partially supported. The aversive racism hypothesis received support. Black patients had less positive reactions to medical interactions with physicians relatively low in explicit but relatively high in implicit bias than to interactions with physicians who were either (a) low in both explicit and implicit bias, or (b) high in both explicit and implicit bias.
Although there has been dramatic improvement in the health of all people living in the United States over the past 50 years, the level of disparities between Black and White Americans for several key indicators of health remains essentially unchanged (National Center for Health Statistics, 2006). Among the suggested contributors to this disparity are health providers’ racial prejudice and stereotypes (Institute of Medicine, 2003; van Ryn, Burgess, Malat, & Griffin, 2006). The potential impact of such provider bias on the health care that Black patients receive is substantial: Approximately 75% of all medical interactions for Black patients in the US are “racially discordant”–that is, they involve nonBlack health care providers (Penner, Albrecht, Coleman, & Norton, 2007). Moreover, relative to racially concordant medical interactions, racially discordant interactions are characterized by less patient trust (Cooper, Roter, Johnson, Ford, Steinwachs, & Powe, 2003), less positive affect (Johnson, Roter, Powe & Cooper, 2004), fewer attempts at relationship building (Siminoff, Graham, & Gordon; 2006), and less joint decision-making (Koerber, Gajendra, Fulford, BeGole, & Evans, 2004). Although provider bias has been proposed as a contributor to such outcomes in racially discordant interactions, it has not, as far as we know, been directly investigated. Thus, the present research investigated the impact of physicians’ explicit and implicit racial bias on medical encounters with Black patients.
Behavior toward Blacks is influenced by both explicit racial attitudes, traditionally assessed with self-reports, and by implicit attitudes, which are automatically activated typically without conscious awareness (Greenwald, Poehlman, Uhlmann, & Banaji, 2009). Moreover, explicit and implicit measures of bias tend to predict different responses (Dovidio, Kawakami, Smoak, & Gaertner, 2009). Explicit measures predict blatant discrimination, whereas implicit measures predict more subtle expressions of discrimination that often occur unintentionally, such as nonverbal behavior and negative decisions in complex situations in which bias could be attributed to factors other than race (McConnell & Leibold, 2001; Son Hing, Chung-Han, Hamilton, & Zanna, 2008). For instance, Green Carney, Pallin, Ngo, Iezzoni, and Banaji (2008) found that when presented with vignettes about patients with symptoms of a myocardial infarction, physicians higher in implicit bias were less likely to recommend appropriate drugs for Black patients.
Whereas people are aware of their overt and deliberative (e.g., verbal) behaviors, which relate to explicit measures of their attitudes, they may be unaware of their subtly biased and spontaneous (e.g., nonverbal) behaviors, which relate to implicit measures (Dovidio, Kawakami, & Gaertner, 2002; McConnell & Leibold, 2001). As targets of these behaviors, however, Blacks and members of other disadvantaged groups attend closely to these subtly biased behaviors, which critically shape their impressions of intergroup interactions (Dovidio, Kawakami, & Gaertner, 2002). The inconsistency between positive overt expressions and negative subtle displays may be particularly problematic because this kind of mismatch is generally perceived to reflect deceitfulness (beyond even a mismatch between negative overt and positive subtle behaviors; Eskritt & Lee, 2003), which can be especially detrimental in interracial interactions that are often characterized by intergroup mistrust (Dovidio, Gaertner, Kawakami, & Hodson, 2002).
Indeed, Dovidio and Gaertner (2004; Gaertner & Dovidio, 1986) proposed that a subtle form of bias, “aversive racism,” can have a particularly detrimental influence on interracial interactions. An aversive racist is a person who is low in explicit bias but who harbors implicit racial biases against Blacks. Aversive racism research has traditionally focused on Whites, but it also applies to the orientations of members of other groups (e.g., Asians; Kawakami, Dunn, Karmali, & Dovidio, 2009) toward Blacks. The mixed messages conveyed by aversive racists during interracial interactions can interfere with effective social coordination and jointly affect Blacks and nonBlacks’ abilities to work together successfully. For example, dyads consisting of a Black participant and a White aversive racist performed less effectively than dyads involving Blacks with Whites who had consonant explicit and implicit attitudes and ironically, even those with high explicit and high implicit bias (Dovidio, 2001).
Recently laboratory work on implicit bias has been extended to health providers, but whereas prior studies of physician bias focused on treatment decisions using retrospective or vignette methodologies, we investigated the relationship of nonBlack (i.e., Asian and White) physicians’ implicit and explicit racial bias to both physicians’ and Black patients’ responses to actual medical interactions in an inner-city primary care clinic. We predicted that physicians’ perceptions of their own behavior (involving the patient in the treatment decision and feeling on the “same team”) would relate primarily to physicians’ explicit (self-reported) prejudice. By contrast, we hypothesized that patients’ perceptions of the encounter would relate to physicians’ implicit bias, unintended activation of biased attitudes measured using the Implicit Association Test (IAT; Greenwald, Nosek, & Banaji, 2003), in combination with their level of explicit prejudice. Drawing on previous work demonstrating that dyads involving Blacks with Whites who fit the aversive racism profile perform particularly poorly on a cooperative task (Dovidio, 2001), we predicted a Physician Implicit Bias x Physician Explicit Bias interaction for Black patients’ perceptions of their involvement in the treatment decision as well as their personal responses to the medical encounter (perceptions of physician warmth and friendliness, feeling on the same team, and satisfaction with the visit). Patients’ reactions were expected to be least positive when physicians were low in explicit prejudice and high in implicit bias.
Method
Participants
The patients were 150 Black patients (112 women, 38 men; average age, 43.63) at an inner-city primary care clinic in the Midwest. (There were no White patients at the clinic during 18 months of data collection.) Participants, who received $20.00 gift cards, were recruited consecutively. Seventy-three percent of the patients asked to participate agreed to do so; the sample closely matched the demographics of the clinic patient population.
The physicians, who received a $50.00 incentive for participating, were 15 (7 female, 8 male) residents in Family Medicine (average age=30.87 years), representing 83% of those asked to participate. Three physicians self-identified as White and the remainder as Indian, Pakistani, or Asian. This high percentage of International Medical Graduates from Asia is typical of primary care clinics in low socioeconomic status urban neighborhoods (Mertz, Jain, Breckler, Chen, & Grumbach, 2007).
Procedure
Physicians completed a 25-item (1=strongly disagree to 5=strongly agree) explicit measure of racial prejudice (α=.89; M = 2.08; SD = .34; Brigham, 1993; McConahay, 1986) and a race IAT measure of implicit bias several weeks before the medical interactions. In the present study, the race concept was Blacks versus Whites and the attributes were Good (e.g., happy, loving) versus Bad (e.g., unpleasant, tragic). IAT responses were scored with the procedures recommended by Greenwald et al. (2003), producing a D measure. Overall, the physicians showed a slight, nonsignificant preference on the IAT for Blacks over Whites (D=.097, p=.138). Physicians’ implicit and explicit prejudice scores were positively correlated, r(15)=.54, p=.029.
After each interaction, both physicians and patients privately completed two items that assessed feelings of being on the same Team, which previous work has shown is associated with more positive intergroup relationships (Gaertner & Dovidio, 2000): (a) “The patient (doctor) and I worked together as a team to solve his/her (my) medical problems,” and (b) “I felt like the patient (doctor) and I were members of the same team, trying to solve his/her (my) medical problems” (1=Strongly Disagree to 5=Strongly Agree). The items were positively correlated for physicians and for patients (r = .79, .70, respectively). Therefore, these two items were averaged to produce a single score for physicians (M=4.16) and for patients (M=4.37). A measure of physicians’ and patients’ perceptions of the extent to which the physician consulted the patient on the final treatment decision, Treatment Consultation, was adapted from Degner, Sloan, and Venkatesh’s (1997) Control Preferences Scale: “I (the doctor) made the decision about which treatment the patient (I) would receive without really considering the patient’s [my] opinion” (1=Strongly Disagree to 5=Strongly Agree: physician M = 3.92; patient M=4.21).
Patients also responded to two items that measured physician warmth and physician friendliness (r =.58) (1=not at all to 4=completely), which were aggregated and averaged to produce a single score (M=3.73). Lastly, patients completed a 14-item measure of Patient Satisfaction (PCC; Stewart et al., 2000), plus one additional item that directly asked patients how satisfied they were with the interaction (1=not at all to 4=completely; α=.93, M=3.66). PCC scores are significantly associated with health outcomes and efficient use of health services (Stewart et al., 2000).
Results
Because physicians interacted with more than one patient (i.e., patients are nested within physicians), to control for non-independence we used the General Estimating Equation (GEE) procedure, a form of multilevel modeling (Hanley, Negassa, Edwardes, & Forrester, 2003; Hardin & Hilbe, 2003). We included implicit bias and explicit prejudice as main effects and their interaction in all equations. Also, all the measures in the equations were standardized by converting them to z scores; thus, the parameter estimates (β) indicate effect size. Physician gender, patient gender, and physician race were not included in the main analyses because they did not moderate any of the effects reported. The correlations among all the outcome measures are presented in Table 1.
Table 1.
Correlations among Ratings of Interactions by Physicians and Patients1
| Patient Team |
Warmth/Friendliness (by Patients) |
Patient Satisfaction |
Physician Treatment Consultation |
Physician Team |
|
|---|---|---|---|---|---|
| Patient Treatment Consultation |
.25** | .26** | .28** | .05 | .19** |
| Patient Team | .45** | .60** | .07 | .06 | |
| Warmth/Friendliness (by Patients) |
.61** | .12 | .15 | ||
| Patient Satisfaction | .17* | .11 | |||
| Physician Treatment Consultation |
.25** |
p < .05
p < .01
There were 15 physicians and 150 patients in the sample. However, for all correlations the n is the number of interactions (150) that were rated by the physicians and the patients
Table 2 presents the relationships between the bias measures and the outcome measures. For physician responses, greater explicit prejudice tended to predict less physician involvement in of the patient in decision making (β=−.31, p=.058), and greater implicit bias tended to predict lower Team ratings (β=−.28, p=.065).
Table 2.
Tests of the effects (standardized coefficients) of Physician Explicit Bias, Implicit Bias and Their Interaction on Physician and Patient Ratings of Interactions
| Effect | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Physician Explicit Bias | Physician Implicit Bias | Interaction | ||||||||||
| β (Std. Error) Wald χ2(1) p | β (Std. Error) Wald χ2(1) p | β (Std. Error) Wald χ2(1) p | ||||||||||
| Physician Ratings | ||||||||||||
| Team | .039 | (.284) | .018 | .892 | −.279 | (.151) | 3.40 | .065 | .265 | (.167) | 2.50 | .114 |
| Treatment Consultation | −.310 | (.163) | 3.60 | .058 | .022 | (.098) | 0.05 | .824 | .088 | (.125) | 0.50 | .480 |
| Patient Ratings | ||||||||||||
| Composite | .203 | (.143) | 2.00 | .157 | −.258 | (.137) | 3.51 | .061 | .260 | (.104) | 6.28 | .012 |
| Team | .194 | (.187) | 1.08 | .299 | −.180 | (.168) | 1.14 | .286 | .335 | (.133) | 6.33 | .012 |
| Treatment Consultation | −.106 | (.147) | .52 | .471 | −.080 | (.131) | 0.38 | .538 | .078 | (.075) | 1.09 | .297 |
| Physician Warmth/Friendliness | .255 | (.153) | 2.76 | .097 | −.285 | (.121) | 5.55 | .018 | .239 | (.103) | 5.37 | .020 |
| Satisfaction | .116 | (.183) | 0.40 | .529 | −.305 | (.233) | 1.72 | .189 | .206 | (.116) | 3.13 | .077 |
Because of the relatively high intercorrelations (between .45 and .61; Table 1) among the patients’ ratings of physician Warmth/Friendliness, Team, and Satisfaction, we created a composite measure that was the standardized aggregated score for the three measures. The Chronbach’s alpha for the composite measure was .79. Treatment Consultation, which correlated less than .30 with the other measures, was analyzed separately.
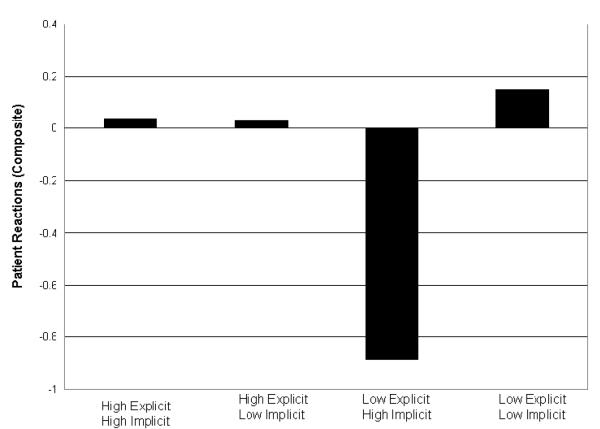
There were no significant effects for Treatment Consultation (see Table 2). However, as predicted, the Physician Implicit x Explicit Bias interaction for the composite measure was significant, Waldχ2(1)= 6.28, β=.26, p=.0121 (see Figure 1). Because the implicit and explicit bias measures are continuous, the plots in Figure 1 represent predicted estimates (the predicted means of patients’ responses to physicians relatively high or low in implicit and explicit bias) rather than actual group means (see Aiken & West, 1991).
Figure 1.
Predicted mean composite patient responses to four groups of physicians: High-explicit-high implicit, high explicit-low implicit, low explicit-high implicit (aversive racist profile) and low explicit-low implicit.
In further analyses, we examined the extent to which patients had more negative reactions, based on the composite measure, to physicians with the aversive racism profile (low explicit-high implicit bias) than to physicians either (a) low in both explicit and implicit bias, or (b) high in both explicit and implicit bias. Consistent with our predictions, when physician explicit bias was relatively low (i.e., 1 SD below the mean), greater physician implicit bias predicted less positive patient responses, Waldχ2(1)= 6.57, β=−.52, p=.010.2 That is, patients responded more negatively to aversive racists than to physicians low in both explicit and implicit bias. Also consistent with predictions, when physician implicit bias was high (i.e., 1 SD above the mean), greater explicit bias predicted patients’ more positive perceptions of physicians, Waldχ2(1)=3.70, β=.46, p=.054.3 Patients responded generally more negatively to physicians low in explicit bias but high in implicit bias (aversive racists) than even to physicians high in explicit and high in implicit bias. Parallel analysis for physicians high in explicit bias (i.e., 1 SD above the mean) showed no effect for implicit bias on the composite (p= .99).
Discussion
Provider bias has been suggested as a contributor to health care interactions (Institute of Medicine, 2003), but there is only limited, indirect evidence for this hypothesis. In addition, although there is some evidence that physicians’ implicit bias predicts physician treatment decisions for Black patients (Green et al., 2008), no previously published research to our knowledge has directly linked physicians’ racial bias to reactions of both doctors and patients following medical interactions. The present research found that Black patients responded particularly negatively to medical encounters with physicians relatively high in implicit bias and relatively low in explicit prejudice–the profile of an aversive racist–relative to all other combinations of implicit bias and explicit prejudice. Thus, whereas most previous research on implicit bias has attempted to link it to an individual’s particular actions, our research demonstrates, in a very consequential setting, the hypothesized significant interpersonal impact implicit bias, especially the impact of aversive racism.
We note, however, the unexpected finding that, in contrast to other results with general populations (Nosek, Banaji, & Greenwald, 2002) and other studies with physicians (Green et al., 2008; Sabin, Rivara, & Greenwald, 2008), overall, the nonblack physicians in the present study did not display implicit racial bias. One possible explanation for these different findings involves the context in which we conducted our study, an inner-city clinic, and the related nature of our sample of physicians. Physicians who choose to practice in such settings may be those who have low levels of bias, implicit as well as explicit. In addition, a large portion of physicians in our sample were born outside of the US and may not have been exposed to the same degree to the socialization influences that create implicit bias (Rudman, 2004) or that suppress correlations between implicit and explicit measures (Hofmann, Gawronski, Geschwender, Le, & Schmitt, 2005). The absence of moderation by physician race/ethnicity for our effects, which would argue against this interpretation, might be attributable in part to the small proportion of White physicians. Future research might pursue these self-selection and cultural socialization explanations. Nevertheless, the findings from this sample have direct practical relevance. Asian physicians represent a substantial portion of primary care physicians practicing in the US and are especially common in clinics that serve inner-city low-income minorities (Mertz et al., 2007).
The findings from the present research can help guide the development of practical interventions designed to reduce bias in medical encounters. In response to 2003 IOM report on “Unequal Treatment”, many physicians argued that overt racism is relatively rare among people who choose a career in health care (e.g., Epstein, 2005). However, it seems that the potential role of implicit bias is largely unrecognized among providers (Lurie et al., 2005). Thus, as Burgess, van Ryn, Dovidio, and Saha (2007) suggested, interventions directed at physicians may be especially productive if they address the subtle, often unintentional, nature of racial bias. Specifically, research suggests that making physicians aware of how implicit bias can influence outcomes of medical encounters and sensitizing them to their own potential for bias can help them “correct” for potential bias in the short-term (Dovidio & Gaertner, 2004) and motivate them to engage in self-regulatory process that can inhibit even subtle expression of bias in the longer term (see Monteith, Arthur, & Flynn, in press).
Acknowledgments
This research was supported by a grant from the National Institute of Child Health and Development (1R21HD050445001A1) to Louis A. Penner, Principal Investigator, and a grant from the National Cancer Institute (U01CA114583) to Terrance L. Albrecht and Peter Lichtenberg, Principal Investigators, and by a grant from the National Science Foundation (BCS-0613218) to Samuel L. Gaertner and John F. Dovidio.
We thank Professor Brian Nosek and members of his laboratory at the University of Virginia for providing us with the codes needed to create a Black-White IAT and advice as we constructed it. We are also grateful for the comments and suggestions offered by the editor and reviewers.
Footnotes
When patients’ perception of Treatment Consultation was added to the composite measure, the interaction was similar, Waldχ2(1)= 5.13, β=.22, p= .024.
Effects for individual components were: (a) Team: Waldχ2(1)=3.96, β=−.53, p=.047; (b) Warmth/Friendliness: Waldχ2(1)=8.12, β=−.54, p=.004; (c) Patient Satisfaction: Waldχ2(1)= 2.93, β=−.52, p=.087.
Effects for individual components were: (a) Team: Waldχ2 (1)=2.87, β=.54, p=.091; (b) Warmth/Friendliness: Waldχ2(1)=4.15, β=.50, p=.042; (c) Satisfaction: Waldχ2(1)=1.22, β=.32., p=.27.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Louis A. Penner, Karmanos Cancer Institute and Department of Family Medicine and Public Health Sciences Wayne State University Research Center for Group Dynamics University of Michigan
John F. Dovidio, Department of Psychology Yale University
Tessa V. West, Department of Psychology New York University
Samuel L. Gaertner, Department of Psychology University of Delaware
Terrance L. Albrecht, Karmanos Cancer Institute and Department of Family Medicine and Public Health Sciences Wayne State University
Rhonda K. Dailey, Department of Family Medicine and Public Health Sciences
Tsveti Markova, Department of Family Medicine and Public Health Sciences.
References
- Aiken L, West S. Multiple regression: Testing and interpreting interactions. Sage; Newbury Park CA: 1991. [Google Scholar]
- Burgess D, van Ryn M, Dovidio J, Saha S. Reducing racial bias among health care providers: lessons from social-cognitive psychology. Journal of General Internal Medicine. 2007;22:882–887. doi: 10.1007/s11606-007-0160-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brigham JC. College students’ racial attitudes. Journal of Applied Social Psychology. 1993;23:1933–1967. [Google Scholar]
- Cooper LA, Roter DL, Johnson RL, Ford DE, Steinwachs DM, Powe NR. Patient-centered communication, ratings of care, and concordance of patient and physician race. Annals of Internal Medicine. 2003;139:907–915. doi: 10.7326/0003-4819-139-11-200312020-00009. [DOI] [PubMed] [Google Scholar]
- Degner LF, Sloan JA, Venkatesh P. The control preferences scale. Canadian Journal of Nursing Research. 1997;29:21–43. [PubMed] [Google Scholar]
- Dovidio JF. On the nature of contemporary prejudice: The third wave. Journal of Social Issues. 2001;57:829–849. [Google Scholar]
- Dovidio JF, Gaertner SL. Aversive racism. In: Zanna MP, editor. Advances in experimental social psychology. Vol. 36. Academic Press; San Diego, CA: 2004. pp. 1–52. [Google Scholar]
- Dovidio JF, Gaertner SL, Kawakami K, Hodson G. Why can’t we just get along? Interpersonal biases and interracial distrust. Cultural Diversity & Ethnic Minority Psychology. 2002;8:88–102. doi: 10.1037/1099-9809.8.2.88. [DOI] [PubMed] [Google Scholar]
- Dovidio JF, Kawakami K, Gaertner SL. Implicit and explicit prejudice and interracial interaction. Journal of Personality and Social Psychology. 2002;82:62–68. doi: 10.1037//0022-3514.82.1.62. [DOI] [PubMed] [Google Scholar]
- Dovidio JF, Kawakami K, Smoak N, Gaertner SL. The roles of implicit and explicit processes in contemporary prejudice. In: Petty RE, Fazio RH, Brinol P, editors. Attitudes: Insights from the new implicit measures. Psychology Press; New York: 2009. pp. 165–192. [Google Scholar]
- Epstein RA. Disparities and discrimination in health care coverage: A critique of the Institute of Medicine study. Perspectives in Biology and Medicine. 2005;48(Suppl):S26–S41. [PubMed] [Google Scholar]
- Eskritt M, Lee K. Do actions speak louder than words? Preschool children’s use of the verbal-nonverbal consistency principle during inconsistent communications. Journal of Nonverbal Behavior. 2003;27:25–41. [Google Scholar]
- Gaertner SL, Dovidio JF. The aversive form of racism. In: Dovidio JF, Gaertner SL, editors. Prejudice, discrimination, and racism. Academic Press; Orlando, FL: 1986. pp. 61–89. [Google Scholar]
- Gaertner SL, Dovidio JF. Reducing intergroup bias: The Common Ingroup Identity Model. Psychology Press; Philadelphia, PA: 2000. [Google Scholar]
- Green AR, Carney DR, Pallin DJ, Ngo LH, Raymond KL, Iezzoni LI, Banaji MR. The presence of implicit bias in physicians and its predictions of thrombolysis for Black and White patients. Journal of General Internal Medicine. 2008;22:1231–1238. doi: 10.1007/s11606-007-0258-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenwald AG, Nosek BA, Banaji MR. Understanding and using the Implicit Association Test: I. An improved scoring algorithm. Journal of Personality and Social Psychology. 2003;85:197–216. doi: 10.1037/0022-3514.85.2.197. [DOI] [PubMed] [Google Scholar]
- Greenwald AG, Poehlman TA, Uhlmann EL, Banaji MR. Understanding and using the Implicit Association Test: III. Meta-analysis of predictive validity. Journal of Personality and Social Psychology. 2009;97:17–41. doi: 10.1037/a0015575. [DOI] [PubMed] [Google Scholar]
- Hanley JA, Negassa A, Edwardes MD, Forrester JE. Statistical analysis of correlated data using generalized estimating equations: An orientation. American Journal of Epidemiology. 2003;157:364–375. doi: 10.1093/aje/kwf215. [DOI] [PubMed] [Google Scholar]
- Hardin JW, Hilbe JM. Generalized estimating equations. Chapman & Hall/CRC; Boca Raton, FL: 2003. [Google Scholar]
- Hofmann W, Gawronski B, Gschwendner T, Le H, Schmitt M. A meta-analysis on the correlation between the Implicit Association Test and explicit self-report measures. Personality and Social Psychology Bulletin. 2005;31:1369–1385. doi: 10.1177/0146167205275613. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine . In: Unequal treatment: Confronting racial and ethnic disparities in health care. Smedley BD, Stith AY, Nelson AR, editors. National Academies Press; Washington, DC: 2003. [PubMed] [Google Scholar]
- Johnson RL, Roter DL, Powe NR, Cooper LA. Patient race and the quality of patient-physician communication during medical visits. American Journal of Public Health. 2004;94:2084–2090. doi: 10.2105/ajph.94.12.2084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawakami K, Dunn E, Karmali F, Dovidio JF. Mispredicting affective and behavioral responses to racism. Science. 2009;323:276–279. doi: 10.1126/science.1164951. [DOI] [PubMed] [Google Scholar]
- Koerber A, Gajendra S, Fulford RL, BeGole E, Evans CA. An exploratory study of orthodontic resident communication by patient race and ethnicity. Journal of Dental Education. 2004;68:553–562. [PubMed] [Google Scholar]
- Lurie N, Fremont A, Jain AK, Taylor SL, McLaughlin R, Peterson E, Kong BW, Ferguson TB., Jr. Racial and ethnic disparities in care: The perspectives of cardiologists. Circulation. 2005;111:1264–1269. doi: 10.1161/01.CIR.0000157738.12783.71. [DOI] [PubMed] [Google Scholar]
- McConahay JB. Modern racism, ambivalence, and the modern racism scale. In: Dovidio JF, Gaertner SL, editors. Prejudice, discrimination, and racism. Academic Press; Orlando, FL: 1986. pp. 91–125. [Google Scholar]
- McConnell AR, Leibold JM. Relations among the Implicit Association Test, discriminatory behavior, and explicit measures of racial attitudes. Journal of Experimental Social Psychology. 2001;37:435–442. [Google Scholar]
- Mertz E, Jain R, Breckler J, Chen E, Grumbach K. Foreign versus domestic education of physicians for the United States: A case study of physicians of south Asian ethnicity in California. Journal of Health Care for the Poor and Underserved. 2007;18:984–993. doi: 10.1353/hpu.2007.0100. [DOI] [PubMed] [Google Scholar]
- Monteith M, Arthur SA, Flynn SM. Self-regulation and bias. In: Dovidio JF, Hewstone M, Glick P, Esses VM, editors. Handbook of prejudice, stereotyping, and discrimination. Sage; Thousand Oaks, CA: (in press) [Google Scholar]
- National Center for Health Statistics U.S. Government Printing Office; Hyattsville, MD: Health United States 2006 with chartbook on trends in the health of Americans. 2006 [PubMed]
- Nosek BA, Banaji MR, Greenwald AG. Harvesting implicit group attitudes and beliefs from a demonstration web site. Group Dynamics: Theory, Research, and Practice. 2002;6:101–115. [Google Scholar]
- Penner LA, Albrecht TL, Coleman DK, Norton WE. Interpersonal perspectives on Black-White health disparities: Social policy implications. Social Issues and Policy Review. 2007;1:63–98. [Google Scholar]
- Rudman LA. Sources of implicit attitudes. Current Directions in Psychological Science. 2004;13:79–82. [Google Scholar]
- Sabin JA, Rivara FP, Greenwald AG. Physician implicit attitudes and stereotypes about race and quality of medical care. Medical Care. 2008;46:678–685. doi: 10.1097/MLR.0b013e3181653d58. [DOI] [PubMed] [Google Scholar]
- Simonoff LA, Graham GC, Gordon NH. Cancer communication patterns and the influence of patient characteristics: Disparities in information-giving and affective behaviours. Patient Education and Counseling. 2006;62:355–360. doi: 10.1016/j.pec.2006.06.011. [DOI] [PubMed] [Google Scholar]
- Son Hing LS, Chung-Yan GA, Hamilton LK, Zanna MP. A two-dimensional model that employs explicit and implicit attitudes to characterize prejudice. Journal of Personality and Social Psychology. 2008;94:771–987. doi: 10.1037/0022-3514.94.6.971. [DOI] [PubMed] [Google Scholar]
- Stewart M, Brown JB, Donner A, McWhinney IR, Oates J, Weston WW, et al. The impact of patient-centered care on outcomes. Journal of Family Practice. 2000;49:796–804. [PubMed] [Google Scholar]
- Street RL, Jr., O’Malley KJ, Cooper LA, Haidet P. Understanding concordance in patient-physician relationships: personal and ethnic dimensions of shared identity. Annals of Family Medicine. 2008;6:198–205. doi: 10.1370/afm.821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Ryn M, Burgess D, Malat J, Griffin J. Physicians’ perception of patients’ social and behavioral characteristics and race disparities in treatment recommendations for men with coronary artery disease. American Journal of Public Health. 2006;96:351–357. doi: 10.2105/AJPH.2004.041806. [DOI] [PMC free article] [PubMed] [Google Scholar]