Abstract
Muscle disorders such as Duchenne muscular dystrophy (DMD) still need effective treatments, and mesenchymal stem cells (MSCs) may constitute an attractive cell therapy alternative because they are multipotent and accessible in adult tissues. We have previously shown that human multipotent adipose–derived stem (hMADS) cells were able to restore dystrophin expression in the mdx mouse. The goal of this work was to improve the myogenic potential of hMADS cells and assess the impact on muscle repair. Forced expression of MyoD in vitro strongly induced myogenic differentiation while the adipogenic differentiation was inhibited. Moreover, MyoD-expressing hMADS cells had the capacity to fuse with DMD myoblasts and to restore dystrophin expression. Importantly, transplantation of these modified hMADS cells into injured muscles of immunodepressed Rag2−/−γC−/− mice resulted in a substantial increase in the number of hMADS cell–derived fibers. Our approach combined the easy access of MSCs from adipose tissue, the highly efficient lentiviral transduction of these cells, and the specific improvement of myogenic differentiation through the forced expression of MyoD. Altogether our results highlight the capacity of modified hMADS cells to contribute to muscle repair and their potential to deliver a repairing gene to dystrophic muscles.
Introduction
Novel cell therapy perspectives have emerged over the past few years with respect to characterization of mesenchymal stem cells (MSCs). These cells can be easily expanded in vitro and differentiated into osteoblasts, adipocytes, chondrocytes, and even myoblasts. Initially, bone marrow MSCs treated with 5-azacytidine were found to differentiate in vitro into multinucleated myotubes.1 The myogenic potential of bone marrow MSCs was then demonstrated in vitro in coculture assays with myoblasts and in vivo by injection in mouse regenerating muscles.2,3 MSCs have also been found in other tissues including the abundant and easily accessible adipose tissue. The plasticity of adipose-derived stem cells was first reported in 2001 by Zuk and colleagues, who showed that populations of human adipose-derived stem cells can differentiate in vitro into adipogenic, chondrogenic, osteogenic, and myogenic lineages.4 It should be noted that most of the data indicate that MSC myogenic differentiation requires either DNA demethylation treatments, coculture with myoblasts or in vivo muscle engraftment.5,6,7,8,9 MSCs do not differentiate into the myogenic lineage as efficiently as into the other lineages. However, the myogenic differentiation capacity of MSCs has a special therapeutic potential. Indeed, many muscle disorders still remain incurable and much effort is devoted, for instance, to the lethal Duchenne muscular dystrophy (DMD), caused by a lack or severe deficiency of dystrophin.10 Dystrophin is a subsarcolemmal protein that connects cytoskeletal actin to sarcolemma and extracellular matrix through a large protein complex. Various therapeutic strategies have been developed including gene or cell therapy, but no treatment protocol is yet available. Thus, identification of any cell population that could efficiently regenerate muscle would be very useful to assess alternative cell therapy strategies. MSCs are considered potential candidates, but, to date no high-yield cell engraftment in animal skeletal muscle has been obtained with most of the unfractioned MSC populations. As the therapeutic impact is very limited in such conditions, different strategies can be addressed to overcome these limitations tentatively. For instance, very recently promising results have been obtained in vitro as well as in vivo with the forced expression of key regulators of the embryonic myogenic program such as MyoD1 (MyoD)11,12,13 and Pax3.14
Our laboratory has isolated cell populations from young donor adipose tissues that exhibit stem cell properties at the clonal level and were named human multipotent adipose-derived stem (hMADS) cells.15 These cells participate in muscle regeneration and induce human dystrophin expression after injection into skeletal muscle of mdx mice (a classical murine model for DMD that displays intense muscle regeneration).9 More recently, human adipose–derived stem cells have also been found to contribute to muscle regeneration in the SJL mouse model for limb–girdle muscular dystrophies.16 However, under myogenic in vitro culture conditions, hMADS cells fail to fuse into myotubes reproducibly, although myogenic markers are expressed to some extent.9 Thus, hMADS cells cannot autonomously fully differentiate into the myogenic lineage.
In the study herein, it was postulated that overexpression of key myogenic genes may overcome the limitations observed in the myogenic differentiation of hMADS cells. As an initial approach to increase their myogenic potential tentatively, expression of MyoD was forced with lentiviral vector transduction. The results demonstrate that the myogenic potential of hMADS cells was drastically increased in vitro and in vivo, and importantly, had promising muscle repair capacities.
Results
Characterization of hMADS cells transduced with mouse MyoD lentiviral vector
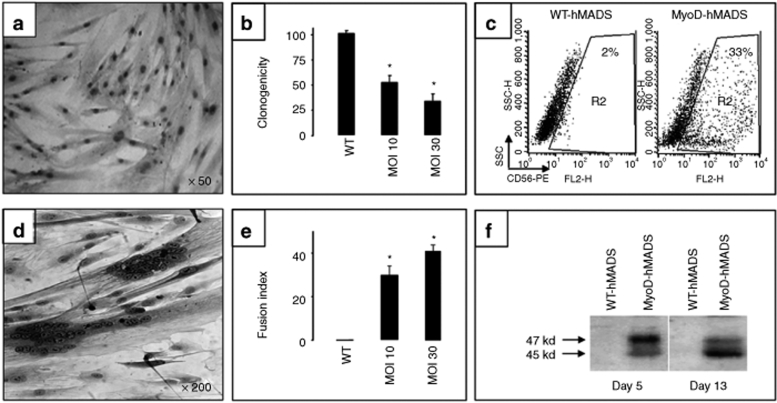
MyoD expression was forced in hMADS cells by transduction with a mouse MyoD lentiviral vector. A LacZ lentiviral vector was used as a negative control. All the following results were identical with LacZ-hMADS cells and wild-type hMADS (WT-hMADS) cells and therefore, only WT-hMADS cell results are shown. Two days after transduction, >95% of the hMADS cells expressed MyoD at the expected nuclear position, as shown with an anti-MyoD antibody (Figure 1a), while no MyoD expression was seen in wild-type cells without the lentiviral vector (WT-hMADS cells) (data not shown). As it should be expected because MyoD withdraws cells from cell cycle, MyoD-hMADS cells grew more slowly than the WT-hMADS cells. The doubling time of the MyoD-hMADS cells was approximately twofold higher than that of the WT-hMADS cells using the mulitplicity of infection (MOI) 30 transduction. This was confirmed at the clonal level because the MyoD-hMADS cell clones were much smaller than the WT-hMADS clones. In addition, clonogenicity was impaired by MyoD expression (Figure 1b). The number of clones decreased with an increase in MOI. MyoD had no effect on the expression of various cell surface markers. Like the WT-hMADS cells, proliferating MyoD-hMADS cells were found positive by flow cytometry analysis for CD13, CD90, and CD105, and negative for CD15, CD117, and STRO-1 (data not shown). However, a clear difference of expression was found for CD56, which is an important marker for myogenesis process.17 More than 30% of MyoD-hMADS cells transduced with a MOI 30 were systematically found positive for CD56, while this percentage was only ~2% for WT-hMADS cells (Figure 1c).
Figure 1.
Characterization of MyoD-hMADS cells. (a–c) Transduction of hMADS cells with the lentiviral vector HIV PGK-MyoD. (a) hMADS cells were labeled with an anti-MyoD antibody revealed with peroxydase staining 2 days after transduction. Note the positive nuclear staining of almost all cells. (b) Effect of MyoD on hMADS clonogenicity expressed as the percentage of clones compared to that obtained with WT-hMADS cells (WT). MOI, multiplicity of infection; n = 7 independent experiments and *P = 0.001. (c) Flow cytometry analysis comparing the percentage of CD56+ cells in WT- and MyoD-hMADS cells. In this representative experiment, cells were used one passage after viral transduction and MyoD expression enhanced the percentage of CD56+ cells from 2% in WT-hMADS cells to 33% in MyoD-hMADS cells. (d–f) Myogenic differentiation of MyoD-hMADS cells. (d) The microscope phase-contrast view shows a typical field of MyoD-hMADS cells 10 days after the switch in myogenic differentiation medium. Multinucleated myotube-like structures are clearly visible on a background of mononucleated cells. (e) Abundance of the cellular elongated syncitia varied according to the MOI levels. The histogram indicates the fusion index of three independent experiments and *P = 0.05. The fusion index was calculated as the ratio of the number of nuclei inside myotubes to the number of total nuclei × 100 at day 8 of myogenic differentiation. The number of nuclei was estimated by the average of nuclei counted in 20 independent and randomly chosen microscope fields. A myotube was defined by the presence of at least three nuclei within a continuous cell membrane. (f) Comparison by western blot of MyoD phosphorylation status between WT- and MyoD-hMADS cells after 5 and 13 days in myogenic differentiation medium. Total cellular extracts were stained with an anti-MyoD antibody (1/200) for phosphorylated (47 kd) and dephosphorylated (45 kd) MyoD protein. A clear shift toward dephosphorylated MyoD was reproducibly found. Lanes were normalized according to protein bands labeled with an anti-tubulin antibody (not shown). hMADS, human multipotent adipose-derived stem.
MyoD-hMADS cells differentiate into myotubes in vitro
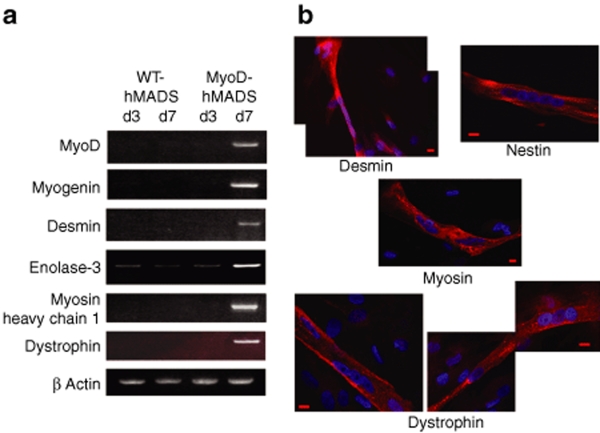
Under myogenic conditions, many elongated multinucleated myotube-like structures were found dispersed among mononucleated MyoD-hMADS cells (Figure 1d). To the contrary, no such cellular structures were visible with WT- or LacZ-hMADS cells. The nuclei were clustered at both the center and the periphery of the cellular structures, which contained up to 80 nuclei. The number and rate of formation of these structures were found to be dependent on the MOI values (Figure 1e). MyoD was detected in the physiological phosphorylated (47 kd) and unphosphorylated (45 kd) forms, as reported to occur under myogenic differentiation culture conditions (Figure 1f). The balance between the two forms shifted toward the dephosphorylated 45 kd form during myogenic differentiation as it is the case in genuine myoblasts. Indeed, the dephosphorylated form is the more stable form because the phosphorylated form is targeted for degradation by the ubiquitin pathway.18 The observed syncitia expressed early and late differentiation markers characteristic of skeletal muscle, and therefore, can be considered as skeletal myotubes. Muscle regulatory factors as well as the terminal differentiation markers, such as desmin, enolase-3, myosin heavy chain, and dystrophin, were found clearly upregulated in the MyoD-hMADS cells (Figure 2a). The same experimental conditions failed to amplify any of these transcripts in WT-hMADS cells. It is interesting to note that the human endogenous MyoD, detected with specific primers, was upregulated as a consequence of the transduction of mouse MyoD, similarly to the autoactivation of MyoD occurring in genuine myoblasts.19 The differentiation of MyoD-hMADS cells in skeletal myotubes was also validated by immunofluorescence studies (Figure 2b). The two intermediate filament proteins, desmin and nestin, were mainly found in the cytoplasm of multinucleated myotubes, but also in some mononucleated cells. Both are early markers of skeletal myogenic lineage and their expression in mononucleated cells indicates a myogenic commitment before any fusion event, as occurs in genuine myoblasts.6 Myosin and dystrophin, which are terminal muscle markers, were only detected in myotubes. Myosin was evenly distributed over the entire myotube and could also be seen with the typical striated pattern due to its sarcomeric localization (data not shown). Dystrophin was essentially observed lining the plasma membrane at its proper localization.
Figure 2.
Muscle differentiation markers expressed in MyoD-hMADS cells. (a) Comparative expression by RT-PCR between WT- and MyoD-hMADS cells after 3 and 7 days in myogenic differentiation medium. Many markers could be amplified at day 7 for MyoD-hMADS cells. PCR was run for 30 cycles, which gave sufficient amplification signal for MyoD-hMADS cells at day 7 without any amplification for other cDNAs under comparison. All the primers were human sequence specific. (b) Immunofluorescence analysis of MyoD-hMADS cells in myogenic differentiation medium. The muscle proteins desmin, nestin, skeletal myosin, and dystrophin were detected using specific antibodies revealed with Rhodamin fluorochrome (red). Nuclei were counterstained with Hoechst 34580 (blue) to detect multinucleated myotubes. Note the presence of mononucleated hMADS cells also expressing desmin beside the desmin positive myotubes. Skeletal myosin is detected with an anti-myosin heavy chain. Dystrophin could be observed in some myotubes at its expected membrane localization. Bar = 20 µm. cDNA, complementary DNA; RT-PCR, reverse transcriptase-PCR; WT-hMADS, human multipotent adipose-derived stem.
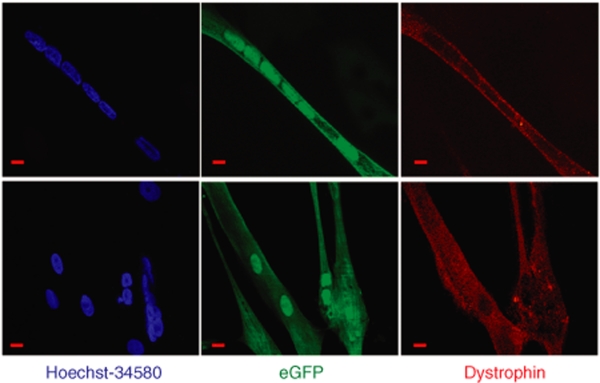
MyoD-hMADS cells fuse with human DMD myoblasts and restore dystrophin
From a human cell therapeutic perspective, the question is whether the strong effect of MyoD expression in hMADS cells is compatible with fusion with myoblasts, and particularly myoblasts isolated from patients suffering of muscular dystrophies. MyoD-hMADS cells were mixed with eGFP-transduced DMD myoblasts in myogenic culture conditions. As expected, no dystrophin was observed in the DMD cell cultures. In cocultures, many DMD myotubes were found as eGFP-positive but dystrophin-negative myotubes, whereas eGFP-negative MyoD-hMADS myotubes stained positive for dystrophin. Importantly, some eGFP-positive myotubes were clearly labeled with the anti-dystrophin antibody (Figure 3). These myotubes were, therefore, hybrid myotubes generated by fusion between hMADS cells and DMD myoblasts. Such hybrid myotubes were exclusively observed with MyoD-hMADS cells that had been transduced with an MOI of 30. In cocultures using WT- or LacZ-hMADS cells, no dystrophin staining was visible under the experimental conditions.
Figure 3.
hMADS and DMD cell cocultures. Dystrophin-deficient DMD myoblasts were transduced with an eGFP lentiviral vector (>90% efficiency measured 2 days after transduction) and cocultured with MyoD-hMADS cells (MOI 30). Cells were cultured on glass to allow microscopic examination and were stained at the end of the longest survival time, ~18 days under such conditions. Immunostaining of dystrophin was observed with an Alexa Fluor 594-conjugated secondary antibody. The figure shows two views of myotubes positive for both eGFP (green) and dystrophin (red) which are hybrid myotubes formed from DMD and MyoD-hMADS cells. Nuclei were labeled in blue with Hoechst-34580 and show the multinucleated structure of myotubes. Myotubes were often found isolated in the cultures because of the plating on glass, which was required for the immunostaining. Bar = 20 µm. DMD, Duchenne muscular dystrophy; eGFP, enhanced green fluorescent protein; hMADS, human multipotent adipose-derived stem; MOI, multiplicity of infection.
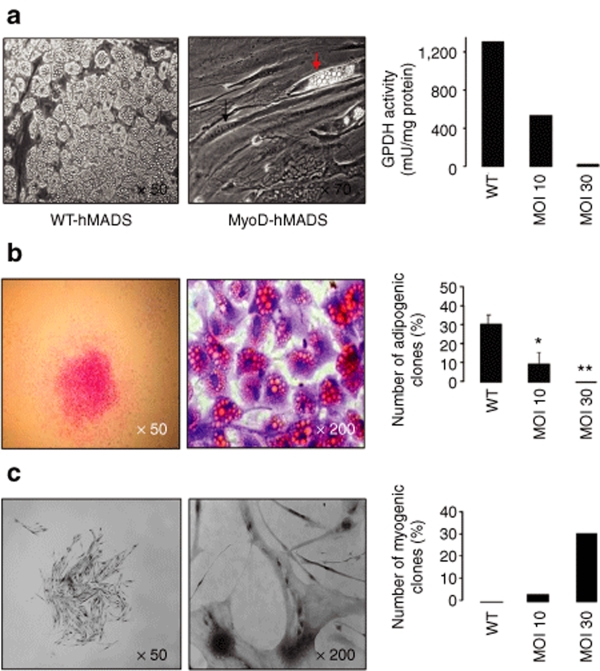
MyoD expression blocks adipogenesis of hMADS cells
We investigated whether MyoD expression alters hMADS cell multipotency and in particular, the adipogenic potential. MyoD-hMADS cells were subjected to adipogenic culture conditions and representative results are presented in Figure 4a. Although robust differentiation into adipocytes filled with lipid vesicles was obtained with WT- or LacZ-hMADS cells, only very few adipocytes could be found in the MyoD-hMADS cells transduced with an MOI of 30. Adipogenesis inhibition was confirmed by a dramatic decrease in the activity of glycerol-3-phosphate dehydrogenase, a key triglyceride synthesis enzyme and a marker of terminal differentiation in adipocytes. Similar observations were made from clonal analysis. MyoD-hMADS cell clones were cultured in adipogenic differentiation medium. For comparison purposes, clones were also cultured in myogenic differentiation medium. A strong decrease in the percentage of adipogenic clones was correlated with the increase of MOIs (Figure 4b). Conversely, MyoD expression gave rise to the development of myogenic clones in correlation with MOI levels (Figure 4c). The direct implication of MyoD was confirmed by finding that no MyoD was detected by immunocytochemistry in the adipogenic clones while MyoD was observed in all the myogenic clones (Figure 4c, high magnification view).
Figure 4.
Differentiation potential of MyoD-hMADS cells. (a) The adipogenic differentiation potential was compared between WT- and MyoD-hMADS cells. The phase-contrast microscope views show typical fields of WT- and MyoD-hMADS cells (MOI 30) subjected to adipogenic culture conditions for 2 weeks. Adipocytes are characterized by the presence of tiny lipid droplets in their cytoplasm. They cover the entire culture dish with WT-hMADS cells, while they are very rare with MyoD-hMADS cells (red arrow). The MyoD-hMADS cells could also be found as multinucleated myotubes (black arrow), in accordance with the very close adipogenic and myogenic culture conditions. The histogram visualizes a representative experiment comparing the GPDH adipocyte marker activity between WT- and MyoD-hMADS cells at the indicated MOI. (b) A single clone in adipogenic differentiation medium is shown at low and high magnification after Oil Red O staining for triglycerides. The histogram compares the percentage of adipogenic clones in WT- and MyoD-hMADS cells according to MOI; n = 5; *P = 0.05 and **P = 0.001. (c) For comparison, the same clonal analysis as in b is shown in myogenic differentiation medium. The low magnification picture is a phase-contrast view of a single myogenic clone and the high magnification picture shows nuclei labeled with an anti-MyoD antibody revealed by peroxydase staining. As opposed to the adipogenic clones, the histogram of this representative experiment shows that the percentage of myogenic clones drastically increases with the MOI level. hMADS, human multipotent adipose-derived stem; MOI, multiplicity of infection; GPDH; glycerol-3-phosphate dehydrogenase; WT, wild type.
MyoD-hMADS cells actively contribute to muscle repair in vivo
As MyoD expression confers to hMADS cells the interesting in vitro capacities described earlier, we speculated that MyoD-hMADS cells may participate in muscle regeneration more efficiently than WT-hMADS cells. We tested this hypothesis in immunodeficient RAG2−/−γC−/− mice whose the tibialis anterior muscles were cryoinjured, to give rise to massive tissue regeneration, and injected with the three types of hMADS cells, i.e., LacZ- or WT- or MyoD-hMADS cells.
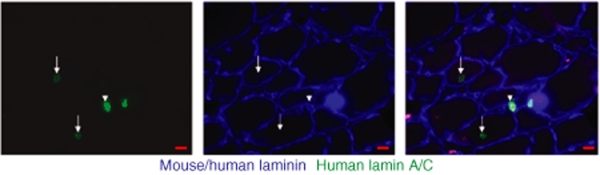
To assess the survival of hMADS cells in mouse muscles, hMADS cells–derived nuclei were examined with a human specific anti-lamin A/C antibody. Up to >200 positive nuclei could be counted per section of injected muscles. For the three types of hMADS cells, lamin A/C positive nuclei were found either scattered within or among the muscle fibers or in clusters between fibers, showing that hMADS cells survived in the mouse muscles in different locations. Most of these nuclei were present in the interstitial spaces (Figure 5 arrow head). Others were found as central nuclei integrated in the regenerated fibers (Figure 5 arrows). Much more MyoD-hMADS cells–derived nuclei than LacZ- or WT-hMADS cells–derived nuclei were found integrated in muscle fibers. Serial sections showed that human nuclei were always detected among mouse nuclei within the same fiber, indicating that hMADS cells fused with mouse regenerating fibers, as could be expected from the in vitro results.
Figure 5.
Detection of hMADS cells–derived nuclei in mouse muscles. The presence of hMADS cells–derived nuclei was assessed 1 month after injection of hMADS cells in the tibialis anterior muscles of Rag2−/− γC−/− mice. hMADS cells–derived nuclei were labeled on transverse cryostat sections with a human specific anti-lamin A/C antibody conjugated to Alexa Fluor 488 (green). The basal lamina was labeled with an antibody crossreacting with both human and mouse laminin and detected with Alexa Fluor 405 (blue). Human positive nuclei were found as central nuclei in regenerated fibers (arrow) or in cells located in interstitial spaces (arrowhead). Nuclei derived from MyoD-hMADS cells are presented. The same immunofluorescent pattern was observed for the different types of hMADS cells, except that MyoD-hMADS cell–derived nuclei were more often observed integrated in the muscle fibers than nuclei derived from LacZ- or WT-hMADS cells. Bar = 10 µm. hMADS, human multipotent adipose-derived stem; WT, wild type.
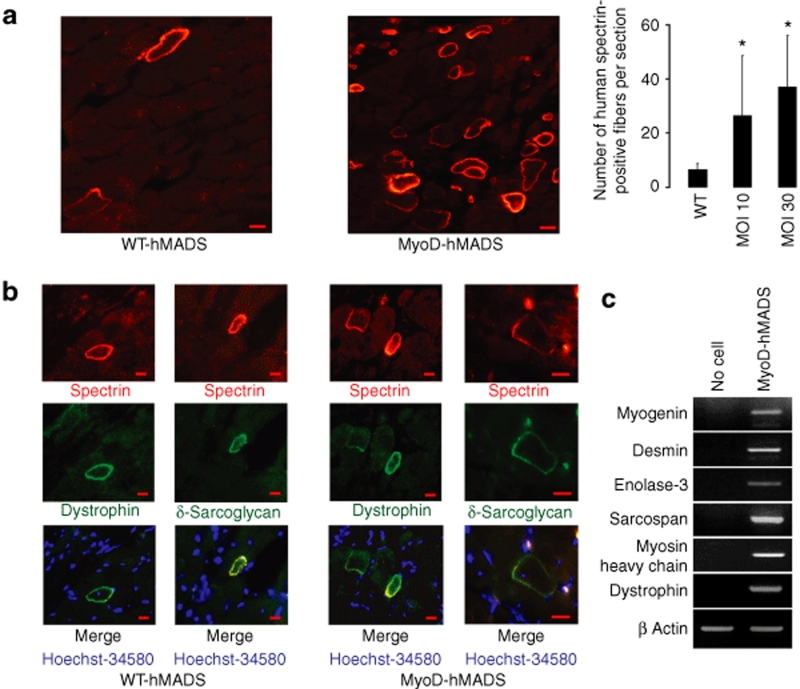
Then, the presence of hMADS cells–derived fibers was studied by the expression of human specific muscle markers. Human spectrin was clearly detected at the membrane of many fibers (Figure 6a). Positive fibers were found mainly concentrated in some areas, likely close to the point of injection, and always in regenerated regions displaying human lamin A/C-positive nuclei scattered in and among fibers. These ranged from very small to large fibers. The proportion of large fibers was variable. The human spectrin labeling was used to quantify the in vivo effect of modification of hMADS cells by MyoD. Thus, the total number of human spectrin-positive fibers was definitively higher with MyoD-hMADS cells than with WT- or LacZ-hMADS cells. This was observed for MOIs of 30 and even 10 (Figure 6a). The presence of hMADS cells–derived muscle fibers was further confirmed by the colabeling of most of the human spectrin-positive fibers with human specific anti-dystrophin and anti-δ-sarcoglycan antibodies. This was observed for muscle fibers derived from MyoD-hMADS cells and from LacZ- or WT-hMADS cells (Figure 6b). Finally, expression of additional human muscle markers was assessed by reverse transcriptase–PCR on pools of cryostat sections of the same muscles analyzed by immunofluorescence. All the human transcripts tested were found to be expressed in mouse muscles injected with the three types of hMADS cells (Figure 6c). The transcripts included early muscle differentiation markers (myogenin and desmin), as well as late markers (dystrophin, myosin heavy chain, sarcospan, and enolase-3).
Figure 6.
Detection of hMADS cells–derived muscle fibers in mouse muscles. The presence of hMADS cells–derived muscle fibers was assessed 1 month after injection of hMADS cells in the tibialis anterior muscles of Rag2−/− γC−/− mice. (a) Assembled representative views of transverse cryostat sections from muscles transplanted with MyoD-and WT-hMADS cells. The sections were immunolabeled with a human specific anti-spectrin β-chain antibody conjugated with Alexa Fluor 594. Note the variations in muscle fiber calibers. The histogram shows the quantification of human spectrin-positive fibers per section found for WT- and MyoD-hMADS cells at MOI 10 and 30; n = 18, 3, and 6 muscles, respectively, and *P = 0. 05. (b) Double staining of muscle fibers derived from hMADS cells. Sections found positive for anti-spectrin antibody were colabeled with human specific anti-dystrophin or anti-δ-sarcoglycan antibodies to ascertain whether the hMADS cells–derived muscle fibers were expressing characteristic human muscle proteins. All antibodies gave the expected membrane labeling of muscle fibers. Spectrin was labeled with Alexa Fluor 594 fluorochrome (red), dystrophin and δ-sarcoglycan with FITC fluorochrome (green), and nuclei with Hoechst-34580 (blue). (c) Expression of human muscle markers in mouse muscles analyzed by RT-PCR. RNA was extracted from 6 to 8 pools of 50 cryostat sections cut along the tibialis anterior muscles. All the amplifications were performed at 30 cycles with human specific primers. PCR amplifications are illustrated with cDNAs from muscles transplanted with MyoD-hMADS cells. Human cDNAs obtained from noninjected muscles were used for negative control (no cell). Equilibrium of cDNA quantities was verified with mouse β-actin. Bar = 20 µm. cDNA, complementary DNA; hMADS; human multipotent adipose-derived stem; MOI, multiplicity of infection; RT-PCR, reverse transcriptase-PCR; WT, wild type.
Discussion
In recent years, several cell populations have been tested for potential clinical applications in muscle pathologies. In the first studies, the cells logically originated from the skeletal muscle itself and myoblast-based therapies constitute a very active field of investigation.20 Besides these cells, mesoangioblasts are very promising clinical candidates based on several studies in dystrophic mice and dogs. They gave rise to >50% of recipient's muscle fibers derived from donor cells.21,22 However, results of transplantation of human mesoangioblasts are not available. Other highly interesting cells are the less characterized human peripheral blood AC133+ cells which gave rise to an average of >30% of human-derived fibers in scid/mdx mouse muscles.23 Finally, MSCs are also obvious candidates due to their multipotency and their important properties of expansion. In this context, progenitor cells found in adipose tissue are of great interest because they meet the requirements for convenient therapeutic use. They come from a tissue that is abundant and easily accessible without damage. The existence of multipotent cells derived from adipose tissue has been documented by several laboratories including ours, prompting the study of their characterization and therapeutic potential. We have already reported that hMADS cells can contribute to muscle regeneration in the mdx mouse.9 Similar results have been now reported with human adipose–derived stem cells in the SJL dystrophic mice in association with an improvement in muscle function.16 The data herein extend our previous mdx mouse results in another murine model. The Rag2−/− γC−/− mouse has no muscle dystrophy and, therefore, has intact regenerative capacities involving its own muscle progenitor cells, which fully compete against injected donor cells after muscle injury unlike mdx mice.24
Cell myogenic conversion by MyoD was initially reported almost 20 years ago in several differentiated cells.25,26 The spectacular differentiation of MyoD-hMADS cells into myotubes proves that MyoD can orchestrate a myogenic programming also in human multipotent stem cells. MyoD transgenic expression clearly showed that MyoD-hMADS cells acquire a high capacity to fuse together to form myotubes, like myoblasts but unlike WT-hMADS cells. The cocultures performed with DMD cells indicate that MyoD-hMADS cells have also the capacity to fuse with human myoblasts and to restore dystrophin expression. This complementation strongly suggests that the hMADS cell gene expression programmed by MyoD is as functional in hybrid myoblasts—hMADS cell myotubes as in hMADS cell myotubes. In addition, the formation of the hybrid myotubes indicates that the fusion of hMADS cells into DMD myotubes does not disturb the myogenic differentiation program of DMD myoblasts, which is a necessary condition for potential clinical use.
Another important issue is the risk of differentiation into undesirable lineages, a potential pitfall with multipotent cells. In many muscle dystrophies, muscles are infiltrated by fat cells, which aggravate muscle dysfunction and create an adipogenic environment.27 It was therefore crucial to observe that myogenic differentiation of the MyoD-hMADS cells inhibited the adipogenic differentiation potential of hMADS cells. This is in accordance with a mutual exclusivity of myogenic differentiation with adipogenic differentiation already observed for many cells of mesenchymal origin.28
On the basis of the very positive assessment of the in vitro requirements for in vivo efficient muscle repair, MyoD-hMADS cells were transplanted into regenerating muscles of immunodeficient mice. These cells were much more efficient than WT-hMADS cells in contribution to muscle repair. The next step will be to optimize the procedure of engraftment. Considering that we counted ~1,800 fibers in the injected tibialis anterior muscles, the percentage of fibers expressing MyoD-hMADS cell proteins was ~2%. This amount is in the same range than found in other studies with genuine human myoblasts in similar conditions.29 However, many improvements can be considered. Notably, high-density injections in muscles and heat shock treatments of the cells before use have been shown to increase the graft success of myoblasts in DMD patient and mouse muscles, respectively.30,31,32,33 The heat shock treatment of myoblasts induces the overexpression of heat-shock proteins which reduces apoptosis and consequently improves the myoblast survival. Indeed, a great majority of hMADS cells do not survive after transplantation. On the basis of the counting of hMADS cells–derived nuclei detected with the human specific anti-lamin A/C antibody, we assume than a maximum of 60,000–70,000 hMADS cells was still present 6 days after transplantation (data not shown). This represents 12–14% of the quantity of injected cells. No investigation was performed on the origin of the massive lost of hMADS cells, but if we can show an involvement of apoptosis, it will be appropriate to test the effect of heat shock treatment of hMADS cells. Also, the use of immunosuppressed mdx or scid/mdx mice would provide a dystrophic muscle mouse model. Only one round of muscle regeneration was triggered by cryoinjury in the Rag2−/− γC−/− mouse muscles instead of the continuous regeneration occurring in the mdx mouse muscles. We can thus speculate that the yield of engraftment could be higher in mdx mouse muscles. In addition, important increases in muscle repair capacities may still be expected on the basis of the dramatic increase of myogenic conversion observed in vitro after MyoD expression in hMADS cells. These improvements will allow to really compare the efficiency of MyoD-hMADS cells with other cell-based therapies that are mentioned earlier.
A decade ago, several labs converted the easily available human dermal fibroblasts to myogenic cells by the forced expression of MyoD.34,35 Such modified human fibroblasts were shown to integrate into mouse regenerating muscles but they did not give rise to many new fibers. MyoD-hMADS cells are clearly more efficient than shown in these reports. It can be speculated that hMADS cells have a better plasticity; as undifferentiated cells they can enter different lineages, and consequently, they may develop a more complete differentiation program than differentiated fibroblasts. This highlights the advantage of using genetically modified human multipotent cells over differentiated cells for muscle repair. It should be noted that the situation may be different in mice. Mouse fibroblasts were very recently found to contribute efficiently to muscle regeneration in mouse after MyoD transduction.13 However, the number of mouse donor-derived fibers decreased strongly between 2 and 4 weeks after cell injection into the muscle.
From a potential therapeutic point of view, an important issue is the use of viral vectors to transduce hMADS cells. Lentiviral vectors are very efficient for gene therapy because they are integrating vectors able to transduce nondividing cells.36 They have already been successfully used to express microdystrophin in human and monkey muscle precursor cells, even allowing allogeneic expression in monkey muscles.37 The clinical safety of lentiviral vectors has still to be fully proven, but these vectors have been estimated safe enough to start a few clinical trials for instance for human immunodeficiency virus treatments.38 In this study, we did not find any evidence of side effects but further long-term studies will be needed to draw any firm conclusion. Another issue to address will be the age of adipose tissue donors. hMADS cells are derived from young donors. The oldest donor we have is a 12-year-old boy. No difference in hMADS cell proliferation was observed among the donors at least until 15 passages in culture. We do not have experience in the properties of equivalent cells from older donors. This will be relevant in a potential perspective of autologous transplantation in DMD patients.
In conclusion, hMADS cells have been shown to be efficiently committed to myogenic lineage by the forced expression of MyoD. In accordance with two recent in vitro investigations, it is thus demonstrated that MSCs also are very receptive to myogenic commitment triggered by key myogenic regulatory factors.13,14 An important finding in this report is that the forced myogenic commitment of hMADS cells is highly beneficial in a perspective of muscle transplantation. Finally, stem cells from adipose tissue present several advantages. They are now rather well characterized through many studies. They can be prepared from an abundant and easily accessible tissue. They have interesting immunosuppressive properties.9,16,39,40,41 Thus, optimization of hMADS cell genetic modifications may create a useful alternative tool to contribute to regeneration and even to delivering gene repair to dystrophic muscles.
Materials and Methods
Cell culture and immunolabeling materials. Culture media were from Lonza Verviers (Verviers, Belgium). The anti-dystrophin (NCL-DYS3), anti-δ-sarcoglycan (NCL-d-SARC), anti-β chain of spectrin (NCL-SPEC1), and anti-lamin A/C (NCL-LAM-A/C) mouse monoclonal antibodies were from Novocastra (Newcastle upon Tyne, UK). The anti-nestin mouse monoclonal antibody was from Millipore (Molsheim, France). These antibodies recognize human antigens without crossreaction with mouse proteins. The anti-laminin (L9393) polyclonal antibody was from Sigma-Aldrich Chimic (Saint-Quentin Fallavier, France). The anti-desmin (D3) and anti-myosin heavy chain (A4.1025) mouse monoclonal antibodies were purchased from Developmental Studies Hybridoma Bank (University of Iowa, Iowa City, Iowa). The rabbit anti-MyoD polyclonal antibody (SC-304) was purchased from Santa Cruz Biotechnology (Heidelberg, Germany). Zenon mouse IgG labeling kits, Alexa Fluor 594- and 405-conjugated secondary antibodies, anti-Alexa Fluor 488, and Hoechst-34580 were purchased from Invitrogen (Cergy Pontoise, France). Biotin-conjugated secondary antibodies were from Jackson ImmunoResearch Europe (Newmarket, UK). The HRP-ABC kit and DAB detection kit were from Vector Laboratories (Peterborough, UK). All the other products were purchased from Sigma-Aldrich.
hMADS cells. Establishment, characterization, and culture of hMADS cells have been described previously by Rodriguez et al.9 hMADS-2 and-3 cells used in this sudy were isolated from fat pads of the pubic and prepubic regions of 5-year and 4-month-old male donors, respectively. However, transduction with hMADS-3 cells consistently gave better results than with hMADS-2 cells and all the quantitative data presented in this study came from hMADS-3 cell results. hMADS cells were used between passages 12 and 21. Isolated cellular clones were obtained by low-density plating, i.e., 500 cells in culture dishes of 100 mm diameter.
For myogenic differentiation, the medium was replaced by 1.5 g/l glucose Dulbecco's modified Eagle's medium supplemented with 10 µg/ml insulin and 5 µg/ml transferrin when the cells reached 90% confluence. Adipogenic differentiation and glycerol-3-phosphate dehydrogenase enzymatic activity were performed as described previously.15
DMD cells. A human DMD myoblastic cell line was kindly provided by D. Trono (Geneva, Switzerland). Cells were grown in Ham's F10 medium supplemented with 20% fetal calf serum. For cocultures, eGFP-transduced DMD myoblasts were seeded with hMADS cells at a 1:1 ratio on glass coverslips. Four days later, growth medium was replaced by hMADS cell myogenic differentiation medium for 18 days.
Viral transductions. PGK-nlsLacZ and PGK-eGFP lentiviral vectors were prepared as described.42,43 Recombinant HIV PGK-MyoD lentiviral vector was kindly provided by Genethon (Evry, France). hMADS cells were transduced with the recombinant HIV PGK-MyoD lentiviral vector, encoding mouse MyoD (MyoD-hMADS cells), at 10 and 30 MOIs or with recombinant PGK-nlsLacZ lentiviral vector (LacZ-hMADS cells) at MOI 30 as a negative control. All the results were identical with LacZ-hMADS cells and WT-hMADS cells. DMD cells were transduced with recombinant PGK-eGFP lentiviral vector at MOI 10.
CD56 flow cytometry analysis. 105 cells were incubated for 30 minutes at 4 °C with a phycoerythrin-conjugated anti-CD56 antibody (1:50 dilution; BD Biosciences, 555516) or an IgG1κ-phycoerythrin control isotype (1:100 dilution; BD Biosciences, 555749). Analyses were performed with a FACScan flow cytometer (BD Biosciences).
hMADS cell transplantation in mice. All animal experiments were done in accordance with our institutional ethic committee guidelines (Comité régional d'éthique en matière d'expérimentation animale—Côte d'Azur). Immunodeficient RAG2−/− γC−/− mice were maintained under pathogen-free conditions. MyoD transduced hMADS cells were injected into mice three passages after transduction with a minimum of 80% of cells positive for anti-MyoD staining. Two- to three-month-old RAG2−/− γC−/− mice were anesthetized with intraperitoneal injection of 250 µl of a solution 10% Imalgène1000 (Ketamin), 0.1% Rompun (Xylazine). The skin over tibialis anterior muscles was slightly cut and cryoinjury was performed by applying a liquid nitrogen–cooled metal rod twice for 10 seconds. Approximately 500,000 hMADS cells suspended in 15 µl Hank's balanced salty solution were injected into the center of the muscle, with a 300 ml insulin syringe. The skin was stitched and cleaned with Betadine solution. The mice were euthanized 4 weeks later. Cross cryosections of the tibialis anterior muscles were collected at 6–7 levels along the muscle for hematoxylin/eosin and immunofluorescence analyses. The intermediate sections were pooled for RNA preparation. Regeneration was checked on the hematoxylin/eosin-stained sections. In all tests, ~80–90% of transversal section areas were occupied by fibers with central nuclei, which is the signature of regenerated fibers.
Immunocytochemistry. Cells plated on coverslips were fixed in 4% paraformaldehyde or in 100% methanol for MyoD staining, and permeabilized with 0.1% Triton X100. Nonspecific reactions were blocked with 1% bovine serum albumin. Cells were then incubated with primary antibodies, at the dilutions recommended by the manufacturer, overnight at 4 °C, and then incubated with secondary antibodies 45 minutes at room temperature. Alexa Fluor 594-conjugated secondary antibodies were used for immunofluorescence, and biotin-conjugated secondary antibodies for immunoperoxydase staining. This latter was observed using a streptavidin-coupled HRP-ABC signal amplification kit followed by DAB detection. Coverslips were mounted on slides using Mowiol 4.88 (Calbochem) solution with 0.5 µg/ml Hoechst-35840.
Immunohistochemistry. To optimize the signal/background ratio for human specific anti-dystrophin (1:20), anti-δ-sarcoglycan (1:20), anti-spectrin (1:100), and anti-lamin A/C (1:100) mouse monoclonal antibodies, antibodies were conjugated with Alexa Fluor fluorochromes using Zenon mouse IgG labeling kits. The anti-spectrin antibody was conjugated with Alexa Fluor 594. For the anti-dystrophin and anti-δ-sarcoglycan antibodies, the fluorescent signal was amplified as follows. Antibodies were first conjugated with Alexa Fluor 488 and unfixed sections were labeled according to manufacturer's recommendations. Sections were then successively incubated with an anti-Alexa Fluor 488 (1:300) rabbit antibody and an anti-rabbit IgG (1:100) coupled to fluorescein isothiocyanate. For colabeling, the anti-spectrin antibody was incubated at the same time as the anti-dystrophin or anti-δ-sarcoglycan antibody. To localize hMADS cells–derived nuclei, anti-lamin A/C antibody was conjugated with Alexa Fluor 488 and incubated at the same time as nonconjugated rabbit anti-laminin polyclonal (1:25) antibody which was observed with a goat anti-rabbit IgG coupled to Alexa Fluor 405. Sections were mounted as described earlier.
Microscopy image capture. Fluorescent immunostained cells and sections were viewed on a Zeiss microscope using ×40 and ×63 oil-immersion objectives. Images were optimized for contrast and brightness using Adobe Photoshop software.
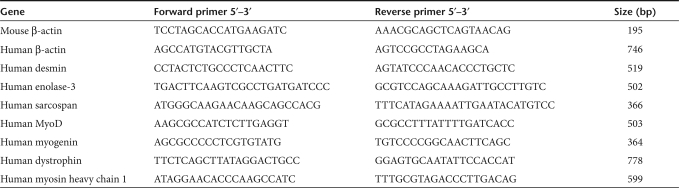
Semiquantitative reverse transcriptase–PCR. Total RNA was extracted using TRI-Reagent according to manufacturer's instructions (Euromedex, Souffelweyersheim, France). Reverse transcription was carried out with Superscript II reverse transcriptase (Invitrogen) and random primers (Promega, Charbonnieres Les Bains, France) on 1 µg RNA treated with RQ1 RNase-free DNase (Promega). PCRof the complementary DNA was performed with GoTaq DNA polymerase (Promega) in a total volume of 25 µl. Cycle numbers were optimized for each primer pair (Table 1) to be in the linear range amplification and amounts of complementary DNA under comparison were carefully adjusted to give the same quantity of amplified complementary DNA with human or mouse β-actin primers. The forward and reverse PCR primers were designed from different exon sequences, except for the human specific MyoD and myogenin primers. The absence of genomic DNA was checked for each PCR primer pairs using the DNAse-treated RNAs as a template for PCR amplification (data not shown).
Table 1.
PCR primers
Western blotting. Cells were detached mechanically from culture dishes at 4 °C, sonicated and placed in 0.05 mol/l Tris–HCl pH 6.8, 4% sodium dodecyl sulfate (0.01% bromophenol blue, 30% glycerol, 1% DTT, and boiled for 5 minutes. Protein concentration was determined using a BCA protein assay kit (Interchim, Montluçon, France). Samples were processed as previously described using Immobilon membranes and HRP substrate (Millipore) visualized with a Fujifilm-LAS-3000-Imager.44
Statistical analyses. All data are expressed as means ± SEM and are representative of at least three separate experiments. The statistical significance of the difference between groups was determined by a Student's t-test. A value of P < 0.05 was considered significant.
Acknowledgments
We thank Gérard Ailhaud (Institute of Developmental Biology and Cancer) for helpful discussions and Cynthia Bottema (The University of Adelaide) for comments on the manuscript. We are grateful to Olivia Cochet (Institute of Developmental Biology and Cancer) and Albert Villageois (Institute of Developmental Biology and Cancer) for efficient technical assistance, and Cendrine Dubaud (Institute of Developmental Biology and Cancer) for help with the mouse experiments. This work was supported by “Association Française contre les Myopathies” and S.G. was a recipient of a postdoctoral fellowship from the Centre National de la Recherche Scientifique.
REFERENCES
- Wakitani S, Saito T., and , Caplan AI. Myogenic cells derived from rat bone marrow mesenchymal stem cells exposed to 5-azacytidine. Muscle Nerve. 1995;18:1417–1426. doi: 10.1002/mus.880181212. [DOI] [PubMed] [Google Scholar]
- Gonçalves MA, de Vries AA, Holkers M, van de Watering MJ, van der Velde I, van Nierop GP, et al. Human mesenchymal stem cells ectopically expressing full-length dystrophin can complement Duchenne muscular dystrophy myotubes by cell fusion. Hum Mol Genet. 2006;15:213–221. doi: 10.1093/hmg/ddi438. [DOI] [PubMed] [Google Scholar]
- Shi D, Reinecke H, Murry CE., and , Torok-Storb B. Myogenic fusion of human bone marrow stromal cells, but not hematopoietic cells. Blood. 2004;104:290–294. doi: 10.1182/blood-2003-03-0688. [DOI] [PubMed] [Google Scholar]
- Zuk PA, Zhu M, Mizuno H, Huang J, Futrell JW, Katz AJ, et al. Multilineage cells from human adipose tissue: implications for cell-based therapies. Tissue Eng. 2001;7:211–228. doi: 10.1089/107632701300062859. [DOI] [PubMed] [Google Scholar]
- Bacou F, el Andalousi RB, Daussin PA, Micallef JP, Levin JM, Chammas M, et al. Transplantation of adipose tissue-derived stromal cells increases mass and functional capacity of damaged skeletal muscle. Cell Transplant. 2004;13:103–111. [PubMed] [Google Scholar]
- Lee JH., and , Kemp DM. Human adipose-derived stem cells display myogenic potential and perturbed function in hypoxic conditions. Biochem Biophys Res Commun. 2006;341:882–888. doi: 10.1016/j.bbrc.2006.01.038. [DOI] [PubMed] [Google Scholar]
- Di Rocco G, Iachininoto MG, Tritarelli A, Straino S, Zacheo A, Germani A, et al. Myogenic potential of adipose-tissue-derived cells. J Cell Sci. 2006;119:2945–2952. doi: 10.1242/jcs.03029. [DOI] [PubMed] [Google Scholar]
- Vieira NM, Brandalise V, Zucconi E, Jazedje T, Secco M, Nunes VA, et al. Human multipotent adipose-derived stem cells restore dystrophin expression of Duchenne skeletal-muscle cells in vitro. Biol Cell. 2008;100:231–241. doi: 10.1042/BC20070102. [DOI] [PubMed] [Google Scholar]
- Rodriguez AM, Elabd C, Amri EZ, Ailhaud G., and , Dani C. Transplantation of a multipotent cell population from human adipose tissue induces dystrophin expression in the immunocompetent mdx mouse. J Exp Med. 2005;201:1397–1405. doi: 10.1084/jem.20042224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffman EP, Brown RH Jr., and , Kunkel LM. Dystrophin: the protein product of the Duchenne muscular dystrophy locus. Cell. 1987;51:919–928. doi: 10.1016/0092-8674(87)90579-4. [DOI] [PubMed] [Google Scholar]
- Morosetti R, Mirabella M, Gliubizzi C, Broccolini A, De Angelis L, Tagliafico E, et al. MyoD expression restores defective myogenic differentiation of human mesoangioblasts from inclusion-body myositis muscle. Proc Natl Acad Sci USA. 2006;103:16995–17000. doi: 10.1073/pnas.0603386103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonçalves MA, Swildens J, Holkers M, Narain A, van Nierop GP, van de Watering MJ, et al. Genetic complementation of human muscle cells via directed stem cell fusion. Mol Ther. 2008;16:741–748. doi: 10.1038/mt.2008.16. [DOI] [PubMed] [Google Scholar]
- Kimura E, Han JJ, Li S, Fall B, Ra J, Haraguchi M, et al. Cell-lineage regulated myogenesis for dystrophin replacement: a novel therapeutic approach for treatment of muscular dystrophy. Hum Mol Genet. 2008;17:2507–2517. doi: 10.1093/hmg/ddn151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gang EJ, Bosnakovski D, Simsek T, To K., and , Perlingeiro RC. Pax3 activation promotes the differentiation of mesenchymal stem cells toward the myogenic lineage. Exp Cell Res. 2008;314:1721–1733. doi: 10.1016/j.yexcr.2008.02.016. [DOI] [PubMed] [Google Scholar]
- Rodriguez AM, Elabd C, Delteil F, Astier J, Vernochet C, Saint-Marc P, et al. Adipocyte differentiation of multipotent cells established from human adipose tissue. Biochem Biophys Res Commun. 2004;315:255–263. doi: 10.1016/j.bbrc.2004.01.053. [DOI] [PubMed] [Google Scholar]
- Vieira NM, Bueno CR, Jr, Brandalise V, Moraes LV, Zucconi E, Secco M, et al. SJL dystrophic mice express a significant amount of human muscle proteins following systemic delivery of human adipose-derived stromal cells without immunosuppression. Stem Cells. 2008;26:2391–2398. doi: 10.1634/stemcells.2008-0043. [DOI] [PubMed] [Google Scholar]
- Capkovic KL, Stevenson S, Johnson MC, Thelen JJ., and , Cornelison DD. Neural cell adhesion molecule (NCAM) marks adult myogenic cells committed to differentiation. Exp Cell Res. 2008;314:1553–1565. doi: 10.1016/j.yexcr.2008.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song A, Wang Q, Goebl MG., and , Harrington MA. Phosphorylation of nuclear MyoD is required for its rapid degradation. Mol Cell Biol. 1998;18:4994–4999. doi: 10.1128/mcb.18.9.4994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thayer MJ, Tapscott SJ, Davis RL, Wright WE, Lassar AB., and , Weintraub H. Positive autoregulation of the myogenic determination gene MyoD1. Cell. 1989;58:241–248. doi: 10.1016/0092-8674(89)90838-6. [DOI] [PubMed] [Google Scholar]
- Peault B, Rudnicki M, Torrente Y, Cossu G, Tremblay JP, Partridge T, et al. Stem and progenitor cells in skeletal muscle development, maintenance, and therapy. Mol Ther. 2007;15:867–877. doi: 10.1038/mt.sj.6300145. [DOI] [PubMed] [Google Scholar]
- Sampaolesi M, Blot S, D'Antona G, Granger N, Tonlorenzi R, Innocenzi A, et al. Mesoangioblast stem cells ameliorate muscle function in dystrophic dogs. Nature. 2006;444:574–579. doi: 10.1038/nature05282. [DOI] [PubMed] [Google Scholar]
- Sampaolesi M, Torrente Y, Innocenzi A, Tonlorenzi R, D'Antona G, Pellegrino MA, et al. Cell therapy of α-sarcoglycan null dystrophic mice through intra-arterial delivery of mesoangioblasts. Science. 2003;301:487–492. doi: 10.1126/science.1082254. [DOI] [PubMed] [Google Scholar]
- Torrente Y, Belicchi M, Sampaolesi M, Pisati F, Meregalli M, D'Antona G, et al. Human circulating AC133(+) stem cells restore dystrophin expression and ameliorate function in dystrophic skeletal muscle. J Clin Invest. 2004;114:182–195. doi: 10.1172/JCI20325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reimann J, Irintchev A., and , Wernig A. Regenerative capacity and the number of satellite cells in soleus muscles of normal and mdx mice. Neuromuscul Disord. 2000;10:276–282. doi: 10.1016/s0960-8966(99)00118-2. [DOI] [PubMed] [Google Scholar]
- Weintraub H, Tapscott SJ, Davis RL, Thayer MJ, Adam MA, Lassar AB, et al. Activation of muscle-specific genes in pigment, nerve, fat, liver, and fibroblast cell lines by forced expression of MyoD. Proc Natl Acad Sci USA. 1989;86:5434–5438. doi: 10.1073/pnas.86.14.5434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi J, Costa ML, Mermelstein CS, Chagas C, Holtzer S., and , Holtzer H. MyoD converts primary dermal fibroblasts, chondroblasts, smooth muscle, and retinal pigmented epithelial cells into striated mononucleated myoblasts and multinucleated myotubes. Proc Natl Acad Sci USA. 1990;87:7988–7992. doi: 10.1073/pnas.87.20.7988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wren TA, Bluml S, Tseng-Ong L., and , Gilsanz V. Three-point technique of fat quantification of muscle tissue as a marker of disease progression in Duchenne muscular dystrophy: preliminary study. Am J Roentgenol. 2008;190:W8–W12. doi: 10.2214/AJR.07.2732. [DOI] [PubMed] [Google Scholar]
- Filvaroff EH., and , Derynck R. Induction of myogenesis in mesenchymal cells by MyoD depends on their degree of differentiation. Dev Biol. 1996;178:459–471. doi: 10.1006/dbio.1996.0231. [DOI] [PubMed] [Google Scholar]
- Vilquin JT, Marolleau JP, Sacconi S, Garcin I, Lacassagne MN, Robert I, et al. Normal growth and regenerating ability of myoblasts from unaffected muscles of facioscapulohumeral muscular dystrophy patients. Gene Ther. 2005;12:1651–1662. doi: 10.1038/sj.gt.3302565. [DOI] [PubMed] [Google Scholar]
- Bouchentouf M, Benabdallah BF., and , Tremblay JP. Myoblast survival enhancement and transplantation success improvement by heat-shock treatment in mdx mice. Transplantation. 2004;77:1349–1356. doi: 10.1097/01.tp.0000121503.01535.f5. [DOI] [PubMed] [Google Scholar]
- Riederer I, Negroni E, Bigot A, Bencze M, Di Santo J, Aamiri A, et al. Heat shock treatment increases engraftment of transplanted human myoblasts into immunodeficient mice. Transplant Proc. 2008;40:624–630. doi: 10.1016/j.transproceed.2008.01.026. [DOI] [PubMed] [Google Scholar]
- Skuk D, Roy B, Goulet M, Chapdelaine P, Bouchard JP, Roy R, et al. Dystrophin expression in myofibers of Duchenne muscular dystrophy patients following intramuscular injections of normal myogenic cells. Mol Ther. 2004;9:475–482. doi: 10.1016/j.ymthe.2003.11.023. [DOI] [PubMed] [Google Scholar]
- Skuk D, Goulet M, Roy B, Piette V, Cote CH, Chapdelaine P, et al. First test of a “high-density injection” protocol for myogenic cell transplantation throughout large volumes of muscles in a Duchenne muscular dystrophy patient: eighteen months follow-up. Neuromuscul Disord. 2007;17:38–46. doi: 10.1016/j.nmd.2006.10.003. [DOI] [PubMed] [Google Scholar]
- Huard C, Moisset PA, Dicaire A, Merly F, Tardif F, Asselin I, et al. Transplantation of dermal fibroblasts expressing MyoD1 in mouse muscles. Biochem Biophys Res Commun. 1998;248:648–654. doi: 10.1006/bbrc.1998.8995. [DOI] [PubMed] [Google Scholar]
- Lattanzi L, Salvatori G, Coletta M, Sonnino C, Cusella De Angelis MG, Gioglio L, et al. High efficiency myogenic conversion of human fibroblasts by adenoviral vector-mediated MyoD gene transfer. An alternative strategy for ex vivo gene therapy of primary myopathies. J Clin Invest. 1998;101:2119–2128. doi: 10.1172/JCI1505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neschadim A, McCart JA, Keating A., and , Medin JA. A roadmap to safe, efficient, and stable lentivirus-mediated gene therapy with hematopoietic cell transplantation. Biol Blood Marrow Transplant. 2007;13:1407–1416. doi: 10.1016/j.bbmt.2007.09.014. [DOI] [PubMed] [Google Scholar]
- Quenneville SP, Chapdelaine P, Skuk D, Paradis M, Goulet M, Rousseau J, et al. Autologous transplantation of muscle precursor cells modified with a lentivirus for muscular dystrophy: human cells and primate models. Mol Ther. 2007;15:431–438. doi: 10.1038/sj.mt.6300047. [DOI] [PubMed] [Google Scholar]
- Cohen J. Building an HIV-proof immune system. Science. 2007;317:612–614. doi: 10.1126/science.317.5838.612. [DOI] [PubMed] [Google Scholar]
- McIntosh K, Zvonic S, Garrett S, Mitchell JB, Floyd ZE, Hammill L, et al. The immunogenicity of human adipose-derived cells: temporal changes in vitro. Stem Cells. 2006;24:1246–1253. doi: 10.1634/stemcells.2005-0235. [DOI] [PubMed] [Google Scholar]
- Yanez R, Lamana ML, Garcia-Castro J, Colmenero I, Ramirez M., and , Bueren JA. Adipose tissue-derived mesenchymal stem cells have in vivo immunosuppressive properties applicable for the control of the graft-versus-host disease. Stem Cells. 2006;24:2582–2591. doi: 10.1634/stemcells.2006-0228. [DOI] [PubMed] [Google Scholar]
- Bochev I, Elmadjian G, Kyurkchiev D, Tzvetanov L, Altankova I, Tivchev P, et al. Mesenchymal stem cells from human bone marrow or adipose tissue differently modulate mitogen-stimulated B-cell immunoglobulin production in vitro. Cell Biol Int. 2008;32:384–393. doi: 10.1016/j.cellbi.2007.12.007. [DOI] [PubMed] [Google Scholar]
- Rouas R, Uch R, Cleuter Y, Jordier F, Bagnis C, Mannoni P, et al. Lentiviral-mediated gene delivery in human monocyte-derived dendritic cells: optimized design and procedures for highly efficient transduction compatible with clinical constraints. Cancer Gene Ther. 2002;9:715–724. doi: 10.1038/sj.cgt.7700500. [DOI] [PubMed] [Google Scholar]
- Naldini L, Blomer U, Gallay P, Ory D, Mulligan R, Gage FH, et al. In vivo gene delivery and stable transduction of nondividing cells by a lentiviral vector. Science. 1996;272:263–267. doi: 10.1126/science.272.5259.263. [DOI] [PubMed] [Google Scholar]
- Pisani DF, Cabane C, Derijard B., and , Dechesne CA. The topoisomerase 1-interacting protein BTBD1 is essential for muscle cell differentiation. Cell Death Differ. 2004;11:1157–1165. doi: 10.1038/sj.cdd.4401479. [DOI] [PubMed] [Google Scholar]