Abstract
Background
Psychiatric advance directives are intended to enable self-determined treatment for patients who lose decisional capacity, and thus reduce the need for coercive interventions such as police transport, involuntary commitment, seclusion and restraints, and involuntary medications during mental health crises; whether PADs can help prevent the use of these interventions in practice is unknown.
Aims
This study examined whether completion of a Facilitated Psychiatric Advance Directive (F-PAD) was associated with reduced frequency of coercive crisis interventions.
Method
The study prospectively compared a sample of PAD completers (n=147) to non-completers (n=92) on the frequency of any coercive interventions, with follow-up assessments at 6, 12, and 24 months. Repeated-measures multiple regression analysis was used to estimate the effect of PADs. Models controlled for relevant covariates including a propensity score for initial selection to PADs, baseline history of coercive interventions, concurrent global functioning and crisis episodes with decisional incapacity.
Results
F-PAD completion was associated with lower odds of coercive interventions (adjusted OR=0.50; 95% CI=0.26-0.96; p < 0.05).
Conclusions
PADs may be an effective tool for reducing coercive interventions around incapacitating mental health crises. Less coercion should lead to greater autonomy and self-determination for people with severe mental illness.
Keywords: Ethics, law, psychiatry
Introduction
Psychiatric advance directives (PADs) provide a legal means for competent individuals to refuse or consent to future mental health treatment during periods of decisional incapacity (Appelbaum, 1991; Srebnik & Lafond, 1999). PADs typically comprise two types of legal devices - advance instructions for mental health treatment and proxy decision-makers (Keefe & Pinals, 2004; Winick, 1996). A major theoretical goal of PADs is to empower psychiatric patients by reducing coercive interventions during mental health crises; whether PADs can accomplish this effect in practice remains unknown (Swanson et al., 2000).
This study examined whether completing a Facilitated Psychiatric Advance Directive (F-PAD) would reduce the frequency of specific coercive crisis interventions (CCIs): transport by police for mental health evaluation, use of handcuffs during transport, involuntary commitment, use of locked seclusion, use of physical restraints in the hospital, and forced medication. The study prospectively assessed the frequency of any CCIs over a 24-month observational follow-up in the experimental group from a recent trial that was focused on the completion of F-PADs (Swanson et al., 2006a). In the present study, PAD completers (n=147) were compared to non-completers (n=92) using a propensity-score adjustment for initial selection to PADs.
Background
A substantial body of research has documented adverse effects of coercion on clinical outcomes and quality of life for persons with mental disorders (Bonsack & Borgeat, 2005; Eriksson & Westrin, 1995; Fisher, 1994; Greenberg et al., 1996; Haglund et al., 2003; Swanson et al., 2003). Whereas CCIs may be necessary in some cases to protect the parties involved, as routine practice these interventions can be counter-therapeutic and may contribute to stigma, trauma, and criminalization of the mentally ill.
The common use of law enforcement officers and vehicles to transport psychiatric patients in handcuffs (Dupont & Cochran, 2000; Kaufman 2007), the trappings of criminal arrest and the process of involuntary hospital admission may contribute to patients’ traumatic experiences of coercion (Hiday et al., 1997; Iversen, et al., 2002; Lidz et al., 1998; Monahan et al., 1996). Public psychiatric hospitals’ long reliance on seclusion, physical restraints, and involuntary psychotropic PRN (as needed) medication to manage patients’ behavior has detracted from the quality of care in these hospitals some scholars argue (Currier 2003; Dickson 2005; Donat, 2005; Gaskin et al., 2007; Fisher 1994). Understandably, mental health service providers as well as consumers would seek to avoid these practices whenever possible.
The expansion of psychiatric advance directives legislation and policy in the US - with new statutes being passed in 25 states since the early 1990s - has been driven in large part by emergent resistance to legal and de facto coercion in mental health care (Swartz & Swanson, 2002; Swanson et al., 2006b). Advocates have hoped that PADs would give persons with severe mental illness greater self-determination and control over their own lives, at a time when public mental health systems are often relying on legal and other forms of mandates in service delivery (Monahan et al., 2005). As an alternative to coercion, PADs are also being promoted as instruments of self-directed care to improve voluntary treatment engagement and thus promote long-term recovery (Backlar & McFarland, 1996; Fisher, 2000; Srebnik & La Fond, 1999; Srebnik, Russo, Sage et al, 2003). Still, the empirical question remains: What role can PADs actually play in achieving the recovery-oriented goals of an evolving mental health system? Can they work as intended and reduce coercive practices around psychiatric emergencies? The purpose of the current research was to assess the impact of PADs on the frequency of long-term objective coercion, particularly during mental health crises when patients may experience decisional incapacity.
Study design and methods
The original F-PAD intervention and parent study design are described in detail elsewhere (Swanson et al., 2006a). Briefly, we conducted a randomized controlled trial to study the effects of a manualized intervention to facilitate completion of psychiatric advance directives. All of the subjects in the current analysis were offered the opportunity, if they so chose, to complete a PAD with the assistance of a trained facilitator.
We selected a random sample from de-identified client files at two county-based mental health systems, both in racially diverse areas of north-central North Carolina. Potential participants from the client cases were pre-screened for study eligibility. Study participants were required to be age 18-65; have a chart diagnosis of schizophrenia, schizoaffective disorder, other psychotic disorder, or major mood disorder with psychotic features; be currently receiving mental health treatment services from one of the two designated county programs; and be able to provide informed consent to participate in the study.
A total of 239 patients were assigned to be offered the F-PAD session; about 60% completed PADs as a result. The F-PAD consists of a semi-structured, guided discussion of treatment decision-making and planning for future mental health treatment, incorporating the statutory elements of PADs in the state of North Carolina (www.nrc-pad.org). If the participant wished to prepare the relevant legal PAD documents, the trained facilitator provided assistance with completing these forms. The sections of the Advance Instruction for Mental Health Treatment and Health Care Power of Attorney (NC Gen Stat §122C-73-77, NC Gen Stat 32A-25) statutory forms (e.g., including medication choices, hospital preferences, powers granted to, or withheld from, the health care agent) were used to organize and guide discussion of the participant’s choices and preferences. Facilitators also assisted the participant in obtaining witnesses, notarization, and filing forms in the medical record and an electronic registry. Participants completing PADs were given a PAD identification card for their wallet and a stainless steel bracelet or necklace engraved to indicate that the person had a PAD and how to access it. The intervention allowed the facilitator to contact, with participants’ consent, the individuals designated as health care proxies, to explain the process and answer any questions they had about their role and what to do during a crisis.
A content analysis of the completed PADs is described elsewhere (Swanson et al., 2006a). Virtually all PADs in the study included both assents and refusals in the same document - i.e., assent to treatment with certain medications, admission to certain preferred facilities, and refusal of others. No participant used a PAD to refuse all treatment.
Regarding the type of PAD completed, 13% chose a stand-alone advance instruction, 5% opted for a stand-alone health care power of attorney, and 43% completed both legal documents. Results of follow-up of these patients at 6, 12, and 24 months are presented here.
Measures
The outcome variable was measured by self-report interview items that asked participants whether they had experienced each of 6 CCIs: (1) being picked up by the police and transported to an emergency room or other facility for psychiatric treatment or evaluation; (2) being placed in handcuffs; (3) being involuntarily committed to a hospital for psychiatric treatment; (4) being placed in seclusion in a locked hospital room; (5) being placed in physical restraints; and (6) receiving forced medications. Two indices were created for analysis: a continuous score comprised the sum of positive (yes vs. no) responses to these items, and a dichotomous score measured whether any of these experiences were reported.
Decisional incapacity was measured by retrospective self-report at each of the follow-up assessments, using the following question from a section of the interview on PADs and mental health crisis situations: “Since your last interview, has there been any time when you became ill and were not able to think clearly enough to make your own decisions about treatment or let others know what you wanted?” (As a clinical and legal matter, patients could have experienced a mental health crisis and been hospitalized - voluntarily or involuntarily - without having decisional incapacity.)
Whereas almost all PAD documents in the study both requested and rejected different types of treatment, the relative emphasis of the PAD in terms of the participant’s intent and priority could be more or less “proscriptive” vs. “prescriptive”. The patient’s focus on avoiding unwanted treatment vs. obtaining recommended treatment was measured by attitudinal Likert-scale items rating the importance of various purposes of the PAD. Participants were coded as having a proscriptive-emphasis PAD if they gave the highest preference rating to “avoiding treatment I don’t want”, and a lower preference rating to “getting the treatment my doctor thinks is best” and “having a family member make decisions for me when I am very ill”. PADs with the reverse pattern were considered to have a prescriptive emphasis.
Several other scale scores were used to measure salient covariates and to create a propensity score for PAD completion (as described below). To measure competence to complete a PAD, we used the Decisional Competence Assessment Tool for Psychiatric Advance Directives (D-CAT-PAD), which is an abbreviated, simplified version of a previously developed instrument, the Competence Assessment Tool for Psychiatric Advance Directives (Elbogen et al., 2007). The anchored version of the Brief Psychiatric Rating Scale (BPRS) (Moerner et al., 1988) was used to assess current psychiatric symptoms. The Global Assessment of Functioning scale (GAF) (Endicott et al., 1976) was used to measure functional impairment. Substance abuse was assessed with questions adapted from the Michigan Alcoholism Screening Test (Selzer, 1971) and the Drug Abuse Screening Test (Skinner, 1982). Motivation to enter and participate in treatment was measured by the Treatment Motivation Questionnaire (Deci & Ryan, 1985; Ryan et al., 1995) as adapted for persons with severe mental illness. The Drug Attitude Inventory (Awad, 1993) was used to assess participants’ attitudes toward taking psychotropic medications.
Sample size and attrition
Sample attrition was 20.5% over the first 6 months (retained n=190); 8.8% between 6 and 12 months (retained n=169); and 24.6% between 12 and 24 months (retained n=110). Combining these waves for longitudinal analysis produced a total of n=469 person-period observations - n=324 with PADs and n=145 without PADs. Completion of PADs was not significantly associated with attrition between 1 and 6 months, but did significantly predict greater sample retention after 6 months.
Statistical analysis
We used propensity scores (Rubin, 1997; Skeem et al., 2002) to factor out any variance in the outcome that might have been associated with nonrandom selection to PADs; the goal of the propensity score adjustment was to render the two groups statistically comparable with respect to baseline predictors of PAD completion. Propensity scores were generated as predicted probabilities from a multistage logistic regression model of PAD completion (Swanson et al., 2006a). Potential baseline predictors were organized into topical domains (e.g., demographics, patient clinical characteristics, attitudes, service utilization), and separate logistic regression models were estimated for each domain as a method for variable reduction. Next, a final multivariable logistic model was derived using stepwise selection at p < 0.10 to identify statistically significant predictors of completing a facilitated PAD. In effect, the final propensity score provides a control for significant net predictors of PAD completion: older than median age, competence to complete PADs, adverse medication experiences, evidence of independent help-seeking motivation, and absence of recent violent victimization. The model is described in further detail in Swanson et al. (2006a.)
We used Generalized Estimating Equations (GEE) multivariable regression analysis to test the intervention effect on CCIs over time, controlling for relevant fixed and time-variant covariates. These models are designed to account for multiple correlation and non-constant variability in clustered, repeated-measures data (Diggle, Liang, & Zeger, 1994; Stokes, Davis, & Koch, 1995). Resulting beta coefficients are exponentiated and presented as odds ratios.
Two types of regression models were tested using PROC GENMOD in SAS (version 9.1). The first was a Poisson model estimating effects on the continuous (but skewed) CCI score, and the second was a logistic regression model predicting a dichotomized index of any CCIs vs. none. The second (dichotomous) model was used to generate mean predicted probabilities for participants within subgroups defined by the presence or absence of decisional incapacity within periods. Both models were tested with controls for a range of salient demographic and clinical covariates. Nonsignificant covariates with p values greater than 0.10 were excluded from the final models. Time and PAD propensity were forced in the models. Final models controlled for the following reduced set of covariates: time, PAD propensity, incapacity, and Global Assessment of Functioning. Mean predicted probabilities were calculated for each service category according to PAD completion status.
The study was conducted according to ethical principles of research and complied with all applicable regulations concerning research involving human subjects. The study protocol was reviewed and approved by the Duke University Medical Center Institutional Review Board.
Results
Sample characteristics
Mean age of the analytic sample was 41.9 years (SD=10.64). Fifty-nine percent of respondents were female. Sixty percent were African American, 38% were white, and 2.7% were persons of other racial/ethnic backgrounds. Only 11% were currently married, while 39% were separated or divorced and 46% were never married. Twenty-seven percent had less that high school education. Only 24% had worked for pay in the past month. Regarding diagnosis, 63.8% had schizophrenia spectrum diagnosis 19% had depression, 33% had bipolar disorder. Eleven percent had co-occurring diagnoses of substance use disorder. Regarding history of hospitalization, 41% had been admitted for inpatient psychiatric treatment within the past year, and 21% had been hospitalized more than once within the year. Baseline mean score on the Global Assessment of Functioning (GAF) scale was 40.0 (SD=10.3), with a median and modal GAF score=35. Baseline mean total score on the Brief Psychiatric Response (BPRS) was 34.0 (SD=9.5). Thirty-three percent of participants had a recent history of self-harm; 26% had experienced recent violent victimization. Twenty-three percent had engaged in some minor or serious violent behavior toward others in the past 6 months, and 8% been arrested in the past 6 months. Based on previous studies, the characteristics of the sample are fairly representative of the patient population with severe mental illness receiving services in the public-sector mental health system central North Carolina.
Frequency of Coercive Crisis Interventions (CCI)
Table I presents lifetime prevalence rates for 6 types of CCIs that were assessed. The most commonly reported experiences were being transported by the police to a treatment facility (68%) and being involuntarily committed (61%). Fifty percent had experienced being placed in seclusion in a locked unit of a treatment facility. The least frequent type of coercive crisis intervention was receiving forced medications; still, one in three participants (34%) had been involuntarily medicated. Overall, the vast majority of study participants (82%) had experienced at least one of these types of interventions in their lifetime. However, these were relatively infrequent events within the context of the study’s 24-month observational period; the prevalence of any CCI in 6 months was 11%, with the cumulative 2-year prevalence doubling to 22%. (The denominator for cumulative prevalence is the sample interviewed at 6, 12 or 24 months, with last-observation-carried-forward for participants who missed interviews at 12 or 24 months.)
Table I.
Prevalence of coercive crisis interventions
| Lifetime prevalence (%) (Baseline N=239) |
|
|---|---|
| Police transport to treatment | 67.78 |
| Placed in handcuffs | 41.84 |
| Involuntary commitment | 61.09 |
| Seclusion on locked unit | 49.79 |
| Physical restraints used | 37.66 |
| Forced medications | 33.89 |
| Any coercive crisis intervention (lifetime) | 82.43 |
| Cumulative summary indices | Cumulative prevalence at follow-up (%) (Retained n=197) |
|
| |
| Any coercive crisis intervention: 1-6 months | 11.05 |
| Any coercive crisis intervention: 1-12 months | 15.98 |
| Any coercive crisis intervention: 1-24 months | 21.65 |
The summary Coercive Crisis Interventions (CCI) scale ranged from 0 to 6. The lifetime version had a fairly normal distribution, with mean=2.87, mode=3, and SD=1.91. The follow-up version of the CCI was skewed due to infrequency of index events within a 6-month period, with mean=0.22, mode=0, and SD=0.72. All involuntary hospitalizations and hospital-based CCI that were recorded occurred in the local region within the jurisdiction covered by the PAD.
Did clinicians view the PAD?
Among participants with PADs who experienced episodes of decisional incapacity, 35% reported being aware that a clinician had read their PAD, or an outpatient case manager reported that the patient’s PAD was viewed. Most of the remaining participants were uncertain as to whether clinicians had actually read their PAD; however, it is not necessarily to be expected that a patient who was in an acute episode of psychiatric illness would have known whether or not a treating clinician read their PAD.
Did PAD have an impact on CCIs?
During the first 6 months of the study, PAD completers experienced CCIs significantly less often than noncompleters did (6.5% vs. 19.7%; p <0.001; Fisher’s exact test p <0.01). The mean difference in the continuous CCI score was also significant between PAD and no-PAD group at 6 months (mean=0.13 vs. mean=0.48; p < 0.01). However, the group differences in CCI rate were attenuated somewhat over the long-term follow-up. By 24-months, the cumulative rate of CCIs reached 18.8% in the PAD group, compared to 27.3% in the no PAD group. Likewise the mean group difference in CCI score was also attenuated: mean=0.16 in the PAD group vs. mean=0.47 for those without PADs at 24 months; these long-term cumulative differences did not achieve statistical significance.
Multivariable regression for repeated measures analysis provided a more powerful and appropriate test of PAD longitudinal effects on CCIs; Table II displays the results. The adjusted model shows that PAD completers had significantly lower odds of experiencing CCIs compared to the no-PAD group over 24 months, controlling for PAD propensity and relevant covariates. Specifically, PAD completers had, on average, approximately half the odds of achieving any given CCI score or higher, compared to their counterparts without PADs (adjusted OR=0. 50; 95% CI=0.26-0.98; p < 0.05). As might have been expected, CCIs were also significantly predicted by baseline history of CCIs, the occurrence of decisional incapacity around mental health crises, and poorer Global Assessment of Functioning scores. However, even controlling for these strong predictors, PADs apparently exerted a significant net effect in reducing CCIs.
Table II.
Longitudinal effects of PADs on frequency of coercive crisis interventions (CCIs) over 24 months: General Estimating Equations (GEE) repeated-measures Poisson regression analysis
| Odds of Coercive Crisis Interventions |
||||
|---|---|---|---|---|
| Bivariate associations |
Adjusted multivariate model2 |
|||
| OR | 95% CI | OR | 95% CI | |
| Independent variables | ||||
| Time (month) | 0.99 | (0.95-1.03) | 1.00 | (0.96-1.04) |
| Baseline history of coercive crisis interventions | 1.36 | (1.14-1.63)*** | 1.21 | (1.04-1.40)* |
| Baseline PAD selection propensity score1 | 0.20 | (0.06-0.74)* | 0.77 | (0.19-3.12) |
| Completed Facilitated PAD | 0.38 | (0.20-0.74)** | 0.50 | (0.26-0.98)* |
| Time variant covariates | ||||
| Episode of decisional incapacity within period | 3.61 | (1.84-7.09)*** | 2.61 | (1.43-4.75)** |
| Global assessment of functioning (GAF) score in period | 0.92 | (0.87-0.97)** | 0.95 | (0.91-0.99)* |
| Statistical significance: *p <0.05; **p <0.01; ***p <0.001 | Model information: N=446 person-period observations DF=439 Log likelihood=-206.57 |
|||
Baseline variables in the propensity score included: age, D-CAT-PAD reasoning scale, DAI medication problem subscale, TMQ internal motivation subscale, and history of victimization. Propensity variables were selected by conducting a staged multivariable logistic regression analysis predicting PAD completion.
Other covariates were tested but eliminated from the model as nonsignificant. These included demographics (race, sex), diagnosis, and substance abuse.
The PAD propensity score had a significant bivariate association with CCIs (OR=0.20; 95% CI=0.06-0.74; p < 0.05), but the propensity effect was rendered nonsignificant in the multivariable analysis with PAD completion in the model (OR=0.77; 95% CI=0.19-3.12; NS). This pattern in the data is consistent with a causal effect for PADs, rather than indicating a favorable selection bias associated with baseline PAD propensity.
To examine whether PADs’ effect on CCIs would vary according to the patient’s intended purpose for the PAD, we also ran the analysis separating out high proscriptive-emphasis PADs from other PADs. We found that PAD completers who gave the highest preference rating to avoiding unwanted treatment did not significantly differ on frequency of CCIs compared to those with PADs emphasizing receipt of treatment recommended by their doctor or having a family member act as a proxy decision maker. Both groups of patients, those with proscriptive-emphasis PADs (OR=0.32; 95% CI=0.09-1.12) and prescriptive-emphasis PADs (OR=0.52; 95% CI=0.26-1.05), showed negative odds ratios compared to the no-PAD group with respect to occurrence of CCIs over the two-year period. (However, splitting the PAD completers into these two groups diminished statistical power for showing an overall PAD effect.)
Figure 1 illustrates the longitudinal impact of PADs in preventing CCIs over the follow-up period, for participants who reported episodes of incapacity around mental health crises, as well as those who did not experience such episodes. The points on the lines indicate predicted probabilities of any CCIs assessed at each of the three follow-up time points. The graphed probabilities were generated from a multivariable logistic regression model with the same specifications as the Poisson model shown in Table II, but predicting a dichotomized version of the dependent variable (1 or more CCIs vs. none).
Figure 1.
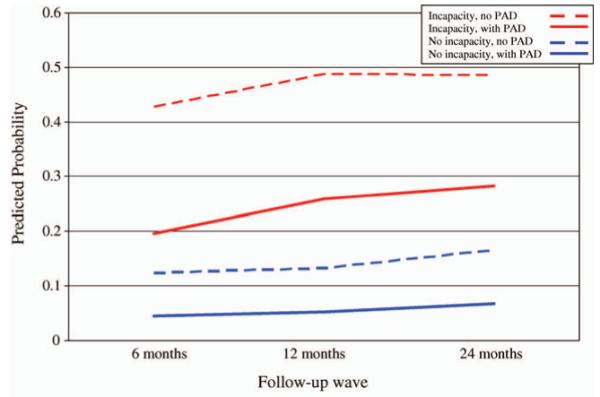
Adjusted predicted probability1 of any coercive crisis interventions at follow-up for psychiatric advance directive (PAD) completers and noncompleters, by any episode of decisional incapacity within period.
1Estimates produced from GEE regression model (see Table 2).
In the presence of incapacity, the estimated chance of any CCIs ranged from 43-49% in participants without PADs, but was substantially reduced in PAD completers - to the range of 20-28%. CCI rates were much lower overall in participants who did not report incapacity during a mental health crisis; still, even in those individuals, the pattern of estimated effects for PADs, as derived from the statistical model, was essentially similar.
Attrition from the study was quite high especially in the second year, with 24% of participants dropping out between 12 and 24 months; PAD completion was a significant predictor of sample retention. Unfortunately, since the outcome is based on self-report, there is no way to know whether the participants who dropped out would have experienced CCIs had they been available to be interviewed at long-term follow-up. To address the possibility that selective attrition may have biased the longitudinal results, we re-ran the models for the 6-month wave alone, i.e., at the point when 80% of the sample remained in the study. In both models - for continuous and dichotomous versions of the dependent variable - the effect of PAD completion was statistically significant, controlling for PAD propensity.
What was the subjective experience behind these numbers? What does prevention of CCIs via PADs actually look like in human terms? The following excerpt from a narrative interview with one of the participants in the study illustrates qualitatively how a PAD might reduce CCIs (Kim et al., 2007):
[In the hospital] we talked about what was in the PAD . . . I did not receive any treatments that I did not want. They were very respectful . . . I really felt like the hospital took better care of me because I had my PAD. In fact, I think it’s the best care that I’ve ever received . . . The doctor didn’t treat me like a nut case because some hospitals do. You know what the doctor said to me? [He said] ‘You’ve got rights and it’s great that you know you have them.’ That’s what he said. He said to me, ‘Now you know your rights and we’ll try to respect those completely . . . And he did a lot for my health too . . . I never take [PAD wrist bracelet] off. My other wrist has my dialysis bracelet. I never take either of these off because I hope this doesn’t happen but if I’m in a situation where I’m out of my mind, at least people can just look at my wrist and see that I’ve got a PAD and that I better not get that ECT and that they better contact [health care proxy] before doing anything to me. I haven’t taken this bracelet off since I got it.
Discussion
This study examined the long-term effects of completing a facilitated psychiatric advance directive on reducing coercive crisis interventions. We find that F-PAD completion was significantly associated with fewer coercive crisis interventions, lowering the adjusted odds by about half compared to those without PADs. The effect remained significant in the presence of appropriate statistical controls, including baseline history of CCIs and initial propensity to complete PADs.
These findings are important because they relate specifically to the core purpose for which PADs were designed. PADs have always been conceived as a legal mechanism for patients to retain some control over treatment decision making, rather than to have the state forcibly intervene. Underlying the design of this legal tool - and the specific legislative intent behind the statutes authorizing PADs - was the expectation that the advance directive would be of most value to patients during episodes of mental health crisis.
How might PADs actually accomplish reduction of coercion? In theory, PADs could prevent the use of CCIs in several ways. First, the experience of legally documenting one’s preferences and choices for future treatment could motivate the consumer to become more actively engaged in regular treatment; this could, in turn, help prevent the recurrence of mental health crises when CCIs might otherwise be applied.
Second, the socially-interactive process of preparing a PAD and discussing it with a clinician could help improve working alliance with the clinician. Indeed, our original study found that participants assigned to F-PADs had a statistically significant improvement in working alliance with their clinicians as compared to control group participants, and were more likely to report that their mental health treatment needs had been met (Swanson, 2006b). If the clinician knows the client and is familiar with what the PAD document says, the clinician might also be in a good position to advocate for the consumer’s PAD preferences during a crisis and thus help the consumer avoid unwanted crisis interventions.
Third, PAD documents that authorize a proxy decision maker and agree in advance to specific future treatment could provide a legally sufficient substitute for contemporaneous consent to treatment when needed; this, too, in some cases could eliminate the need for an involuntary commitment order. In our study, PADs typically contained advance consent to hospitalization; indicated a preference for specific medications over others; and included advice to inpatient staff about how to help them avoid the use of physical restraints and seclusion during a future mental health crisis (Swanson et al., 2006a).
Fourth, and finally, PADs typically provide useful information to clinicians - emergency contacts, treatment history, and interventions that have been helpful during past crises. Such information, on its face, may give clinicians a warrant to treat the patient without unduly invoking CCIs. In theory, a person with a PAD, or a family member, could also provide the PAD document to law enforcement officers who are transporting the patient or responding during a crisis. While designed to be invoked when the patient cannot communicate, it can also become in some situations a vehicle for communication between the patient and clinician. Insofar as the PAD gives the patient a “voice” and a sense of being respected - especially in situations when the patient is otherwise most powerless and vulnerable - the PAD may contribute directly to the quality of “procedural justice” which many previous studies have shown to be important in mitigating coercion (Tyler, 1992; Lidz et al., 1998; Watson & Angell, 2007). If read and appropriately followed then competently-prepared PADs can help foster treatment alternatives that do not rely on CCIs.
There are several limitations to this study. First, insofar as there was a PAD effect on reducing CCIs, we are unable to distinguish between any direct effect of the legal document itself, and the perhaps indirect effect of the social process of producing the document. Also, the study analyses included only participants who were in treatment and willing to consent to research; therefore, these results may not be generalizable to all people with severe mental illness who might have completed PADs, had they been offered the chance to do so. Sample attrition was quite high in the second year of follow-up, with 24% dropping out between 12 and 24 months. PAD completers were significantly more like to be retained. However, having CCIs in the first wave did not predict subsequent attrition differentially in the PAD and no PAD groups. Moreover, the adjusted effect of PADs on CCIs was statistically significant even in the first wave considered alone, i.e., before substantial attrition.
Another limitation is that, because participants could not be randomly assigned to complete a PAD, the findings, like the results of any naturalistic observational study of an intervention, are subject to potential self-selection bias. Indeed, we found a significant negative bivariate association between the CCI outcome and baseline propensity to complete PADs. However, the potential for bias was substantially mitigated by controlling for PAD propensity in a multivariable regression analysis. The fact that PAD completion remained statistically significant in the final model, while PAD propensity became nonsignificant, lends credence to a causal interpretation of the results, rather than indicating a methodological artifact resulting from favorable selection bias.
Conclusion
In conclusion, these study findings amount to the first promising evidence that PADs can actually do what 25 state legislatures in the USA drafted them to do: give psychiatric patients more control over their own treatment during mental health crisis, by reducing the use of coercive crisis interventions. In the long run, less coercion should lead to greater autonomy and self-determination for people with severe mental illness. PADs are a tool for empowerment now in the hands of mental health consumers. Clinicians can help to maximize the benefits of PADs by asking patients about PADs, reading what these documents say, and following their instructions and preferences as much as possible.
Acknowledgements
The study was funded by grants from the National Institute of Mental Health (R01-MH063949, K02-MH67864) and the John D. and Catherine T. MacArthur Foundation Research Network on Mandated Community Treatment.
Footnotes
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Appelbaum PS. Advance directives for mental health treatment. Hospital and Community Psychiatry. 1991;42:983–984. doi: 10.1176/ps.42.10.983. [DOI] [PubMed] [Google Scholar]
- Awad AG. Subjective response to neuroleptics in schizophrenia. Schizophrenia Bulletin. 1993;19:609–618. doi: 10.1093/schbul/19.3.609. [DOI] [PubMed] [Google Scholar]
- Backlar P, McFarland BH. A survey on use of advance directives for mental health treatment in Oregon. Psychiatric Services. 1996;47:1387–1389. doi: 10.1176/ps.47.12.1387. [DOI] [PubMed] [Google Scholar]
- Bonsack C, Borgeat F. Perceived coercion and need for hospitalization related to psychiatric admission. International Journal of Law and Psychiatry. 2005;28:342–347. doi: 10.1016/j.ijlp.2005.03.008. [DOI] [PubMed] [Google Scholar]
- Currier GW. The controversy over “chemical restraint” in acute care psychiatry. Journal of Psychiatric Practice. 2003;9:59–70. doi: 10.1097/00131746-200301000-00006. [DOI] [PubMed] [Google Scholar]
- Deci EL, Ryan RM. Intrinsic motivation and self-determination in human behavior. Plenum Press; New York: 1985. [Google Scholar]
- Dickson DT. Involuntary medication of the mentally ill: Continuing controversy, changing scene. In: Kirk SA, editor. Mental disorders in the social environment: Critical perspectives. Columbia University Press; New York: 2005. pp. 443–460. [Google Scholar]
- Diggle PJ, Liang K-Y, Zeger SL. Analysis of longitudinal data. Clarendon Press; Oxford: 1994. [Google Scholar]
- Donat DC. Special section on seclusion and restraint: Encouraging alternatives to seclusion, restraint, and reliance on PRN drugs in a public psychiatric hospital. Psychiatric Services. 2005;56:1105–1108. doi: 10.1176/appi.ps.56.9.1105. [DOI] [PubMed] [Google Scholar]
- Dupont R, Cochran S. Police response to mental health emergencies: Barriers to change. Journal of the American Academy of Psychiatry and the Law. 2000;28:338–344. [PubMed] [Google Scholar]
- Elbogen EB, Swanson JW, Appelbaum P, Swartz MS, Ferron J, Van Dorn RA, Wagner HR. Competency to complete psychiatric advance directives: Effects of facilitated decision making. Law and Human Behavior. 2007;31:275–289. doi: 10.1007/s10979-006-9064-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Endicott J, Spitzer RL, Fleiss JL, Cohen J. The Global Assessment Scale: A procedure for measuring overall severity of psychiatric disturbances. Archives of General Psychiatry. 1976;33:766–771. doi: 10.1001/archpsyc.1976.01770060086012. [DOI] [PubMed] [Google Scholar]
- Eriksson KI, Westrin CG. Coercive measures in psychiatric care: Reports and reactions of patients and other people. Acta Psychiatrica Scandinavica. 1995;92:225–230. doi: 10.1111/j.1600-0447.1995.tb09573.x. [DOI] [PubMed] [Google Scholar]
- Fisher D. Making advance directives work for you. National Empowerment Center Newsletter. 2000 Available at: www.power2u.org/selfhep/directive_work.html.
- Fisher WA. Restraint and seclusion: A review of the literature. American Journal of Psychiatry. 1994;151:1584–1591. doi: 10.1176/ajp.151.11.1584. [DOI] [PubMed] [Google Scholar]
- Gaskin C, Elsom SJ, Happell B. Interventions for reducing the use of seclusion in psychiatric facilities. British Journal of Psychiatry. 2007;191:298–303. doi: 10.1192/bjp.bp.106.034538. [DOI] [PubMed] [Google Scholar]
- Greenberg WM, Moore-Duncan L, Herron R. Patients’ attitudes toward having been forcibly medicated. Bulletin of American Academy Psychiatry Law. 1996;24:513–524. [PubMed] [Google Scholar]
- Haglund K, Von Knorring L, Von Essen L. Forced medication in psychiatric care: patient experiences and nurse perceptions. Journal of Psychiatric and Mental Health Nursing. 2003;10:65–72. doi: 10.1046/j.1365-2850.2003.00555.x. [DOI] [PubMed] [Google Scholar]
- Hiday VA, Swartz MS, Swanson J, Wagner HR. Patient perceptions of coercion in mental hospital admission. International Journal of Law and Psychiatry. 1997;20:227–241. doi: 10.1016/s0160-2527(97)00004-6. [DOI] [PubMed] [Google Scholar]
- Iversen K, Hoyer G, Sexton H, Gronli OK. Perceived coercion among patients admitted to acute wards in Norway. Nordic Journal of Psychiatry. 2002;56:433–439. doi: 10.1080/08039480260389352. [DOI] [PubMed] [Google Scholar]
- Kaufman AR. Should we use law enforcement for emergency transportation of people with mental illness? American Journal of Psychiatry [Residents Journal] 2007;164:3. [Google Scholar]
- Keefe B, Pinals DA. Durable power of attorney for psychiatric care. Journal of the American Academy of Psychiatry and the Law. 2004;32:202–204. [Google Scholar]
- Kim MM, Van Dorn RA, Scheyett A, Elbogen E, Swanson JW, Swartz MS, McDaniel LA. Understanding the personal and clinical utility of Psychiatric Advance Directives: A qualitative perspective. Psychiatry. 2007;70:19–29. doi: 10.1521/psyc.2007.70.1.19. [DOI] [PubMed] [Google Scholar]
- Lidz CW, Mulvey EP, Hoge SK, Kirsch BL, Monahan J, Eisenberg M, et al. Factual sources of psychiatric patients’ perceptions of coercion in the hospital admission process. American Journal of Psychiatry. 1998;155:1254–1260. doi: 10.1176/ajp.155.9.1254. [DOI] [PubMed] [Google Scholar]
- Moerner MG, Mannuzza S, Kane JM. Anchoring the BPRS: An aid to improved reliability. Pychopharmacology Bulletin. 1988;24:112–117. [PubMed] [Google Scholar]
- Monahan J, Hoge SK, Lidz CW, Eisenberg MM, Bennett NS, Gardner WP, et al. Coercion to inpatient treatment: Initial results and implications for assertive treatment in the community. In: Dennis DL, Monahan JE, editors. Coercion and aggressive community treatment: A new frontier in mental health law. Plenum Press; New York: 1996. pp. 13–28. [Google Scholar]
- Monahan J, Redlich A, Swanson JW, Robbins PC, Appelbaum PS, Petrila J, Steadman HJ, Swartz MS, Angell B, McNiel DE. Use of leverage to improve adherence to psychiatric treatment in the community. Psychiatric Services. 2005;56:37–44. doi: 10.1176/appi.ps.56.1.37. [DOI] [PubMed] [Google Scholar]
- NC Gen Stat §32A-25. Health Care Power of Attorney.
- NC Gen Stat §122C-73-77. Advance Instruction for Mental Health Treatment.
- Rubin D. Estimating causal effects from large datasets using propensity scores. Annals of Internal Medicine. 1997;127:757–763. doi: 10.7326/0003-4819-127-8_part_2-199710151-00064. [DOI] [PubMed] [Google Scholar]
- Ryan RM, Plant RW, O’Malley S. Initial motivations for alcohol treatment: Relations with patient characteristics. Addictive Behaviors. 1995;20(3):279–297. doi: 10.1016/0306-4603(94)00072-7. [DOI] [PubMed] [Google Scholar]
- Selzer ML. The Michigan alcoholism screening test: The quest for a new diagnostic instrument. American Journal of Psychiatry. 1971;127:1653–1658. doi: 10.1176/ajp.127.12.1653. [DOI] [PubMed] [Google Scholar]
- Skeem JL, Monahan J, Mulvey EP. Psychopathy, treatment involvement, and subsequent violence among civil psychiatric patients. Law and Human Behavior. 2002;26:577–603. doi: 10.1023/a:1020993916404. [DOI] [PubMed] [Google Scholar]
- Skinner HA. The Drug Abuse Screening Test. Addictive Behaviors. 1982;7:363–371. doi: 10.1016/0306-4603(82)90005-3. [DOI] [PubMed] [Google Scholar]
- Srebnik D, LaFond J. Advance directives for mental health services: Current perspectives and future directions. Psychiatric Services. 1999;50:919–925. doi: 10.1176/ps.50.7.919. [DOI] [PubMed] [Google Scholar]
- Srebnik D, Russo J, Sage J, Peto T, Zick E. Interest in psychiatric advance directives among high users of crisis services and hospitalization. Psychiatric Services. 2003;54:981–986. doi: 10.1176/appi.ps.54.7.981. [DOI] [PubMed] [Google Scholar]
- Stokes ME, Davis C, Koch GG. Categorical data analysis using the SAS system. SAS Institute, Inc.; Cary, NC: 1995. [Google Scholar]
- Swanson JW, Swartz MS, Elbogen E, Wagner HR, Burns BJ. Effects of involuntary outpatient commitment on subjective quality of life in persons with severe mental illness. Behavioral Sciences and the Law. 2003;21:473–491. doi: 10.1002/bsl.548. [DOI] [PubMed] [Google Scholar]
- Swanson JW, Swartz MS, Elbogen EB, Van Dorn RA, Ferron J, Wagner HR, McCauley BJ, Kim M. Facilitated psychiatric advance directives: A randomized trial of an intervention to foster advance treatment planning among persons with severe mental illness. American Journal of Psychiatry. 2006a;163:1943–1951. doi: 10.1176/appi.ajp.163.11.1943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swanson JW, Swartz MS, Ferron J, Elbogen EB, Van Dorn RA. Psychiatric advance directives among public mental health consumers in five U.S. cities: Prevalence, demand, and correlates. Journal of the American Academy of Psychiatry and Law. 2006b;34:43–57. [PubMed] [Google Scholar]
- Swanson JW, Tepper MC, Backlar PB, Swartz MS. Psychiatric advance directives: An alternative to coercive treatment? Psychiatry. 2000;63:160–172. doi: 10.1080/00332747.2000.11024908. [DOI] [PubMed] [Google Scholar]
- Swartz MS, Swanson JW. Involuntary outpatient commitment in the United States: Practice and controversy. In: Buchanan A, editor. Care for the mentally disordered offender in the community. Oxford University Press; Oxford: 2002. [Google Scholar]
- Tyler TR. Psychological consequences of judicial procedures: Implications for civil commitment hearings. Southern Methodist University Law Review. 1992;46:433–444. [Google Scholar]
- Winick BJ. Advance directive instruments for those with mental illness. University of Miami Law Review. 1996;51:57–95. [PubMed] [Google Scholar]
- Watson AC, Angell B. Applying procedural justice theory to law enforcement’s response to persons with mental illness. Psychiatric Services. 2007;58(6):787–793. doi: 10.1176/ps.2007.58.6.787. [DOI] [PubMed] [Google Scholar]


