Abstract
Background
Chondral lesions, peroneal tendon tears, and other disorders in patients with chronic ankle instability may not be detected by preoperative MRI. Also, MRI often is obtained and interpreted at the referring institution, leading to variability in reading.
Questions/Purposes
We assessed the accuracy of the radiologists’ and orthopaedic surgeon’s reading of preoperative MRI for diagnosing ankle lesions in patients with ankle instability warranting surgery.
Patients and Methods
We retrospectively reviewed 133 patients who underwent 135 surgeries for lateral ankle ligament reconstruction with concomitant ankle arthroscopy and who had preoperative MRI.
Results
We found 72 associated lesions in 66 of the 135 surgeries, including 38 chondral injuries, 18 peroneus brevis tears, seven loose bodies, and nine other miscellaneous abnormalities. Eliminating eight lesions for which the decision to operate was not based on operative findings, there were 127 surgeries with 64 associated lesions that required intraoperative confirmation or were detected intraoperatively. In the original reports, the radiologists identified 39% (15) of the chondral injuries, 56% (10) of the peroneal tears, and 57% (four) of the loose bodies. Radiologists’ MRI sensitivity for detecting lesions was 45%. The attending surgeon identified 47% (18) of the chondral injuries, 89% (16) of the loose bodies, 71% (five) of the peroneus brevis tears, and the posterior talus process lesion, with a sensitivity of 63%.
Conclusions
Our data suggest orthopaedic surgeons should review preoperative MRIs and also suggest the sensitivity of MRI may not be adequate to detect lesions in these patients before surgery.
Level of Evidence
Level IV, diagnostic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Ankle sprains are extremely common injuries [6, 7]. Although many patients are successfully treated nonoperatively, residual problems may occur [4, 8]. Twenty to 40% of patients with chronic instability have associated disorders, such as chondral lesions of the talus, peroneal tears, or loose bodies [2, 3, 7]. These lesions may contribute to morbidity after an ankle sprain [7, 10, 19, 24]. In the absence of definitive data, diagnosis and treatment at the time of reconstructive ligament surgery appear desirable.
To appropriately treat lesions associated with ankle instability, lesions must be diagnosed accurately. A thorough clinical examination is an important first step, but some lesions may be difficult to assess. One way to identify concomitant disorders is to obtain preoperative MRI. A previous report noted MRI accuracy of 80% in detecting talus osteochondral lesions and peroneal brevis tendon tears [2], but another study reported MRI detected cartilage lesions in only five of 26 (19%) patients with lesions confirmed at surgery [18]. Often patients arrive for surgical consultation with MR images obtained and read at outside institutions, which may add additional variability to the scenario. Some authors have recommended routine ankle arthroscopy to detect intraarticular disorders at the time of ligament reconstruction [3, 7, 10].
Given the reported variability of accuracy of MRI, we (1) determined the sensitivity of preoperative MRI by assessing the accuracy of community radiologists and an orthopaedic surgeon in identifying associated lesions found intraoperatively in patients undergoing ligament reconstruction and (2) assessed accuracy of detecting different types of lesions.
Patients and Methods
We retrospectively reviewed 133 patients who underwent 135 surgeries for lateral ankle ligament reconstruction and had preoperative MRI and ankle arthroscopy between 2003 and 2008. All patients first had a nonoperative course of immobilization that failed, activity modification, and physical therapy. Instability was noted by history, and all patients had ligamentous instability on examination. All patients had a positive anterior drawer sign, and no patients had interosseous tenderness. We did not include patients with syndesmotic instability. Two patients had an opposite-side surgery separated in time. Of the 135 surgeries, 134 were a primary Broström-Gould repair, and one was primary anatomic reconstruction with semitendinosus allograft. Mean patient age was 29 years (range, 13–64 years). There were 95 females and 38 males. This study was approved by our institutional review board.
All patients underwent ankle arthroscopy before ligament reconstruction by the senior author (GPG). Standard anteromedial and anterolateral portals were made, with caution to avoid surrounding structures. A standard posterolateral portal was made only if necessary to access posteromedial lesions for débridement. This portal was used three times in the study. A careful inspection of the ankle was performed at the time of surgery by one observer, and any identified abnormality in the surgical field was treated if judged appropriate by the surgeon.
Of the 135 surgeries, we observed 72 lesions in 66 surgeries (48%) treated separately from the ligament reconstruction, including 38 chondral lesions, one of which was on the tibia; 18 peroneus brevis tears; seven loose bodies; four symptomatic os trigona with bone edema; one talar exostosis; one posterior tibial tendon tear; one medial malleolus stress fracture; one lateral malleolus stress fracture; and one large posterior impingement lesion. The decision to surgically address the four os trigona, one posterior tibial tendon tear, the stress fractures, and the posterior impingement lesion was not based on intraoperative findings. This left 127 surgeries and 64 lesions that required intraoperative detection or confirmation before treatment. Five patients had two lesions. In these five surgeries, the first lesion was a chondral lesion and the second was a peroneal tear (four) or a second chondral lesion (one). Only the chondral lesion was counted in the total of 64 lesions detected intraoperatively. All patients had ankle instability by examination under anesthesia.
As is typical in our referral foot and ankle practice, MRI was obtained by most patients from various community radiology providers and read at that institution before consultation with the orthopaedic surgeon. Patients without MR images at consultation were referred for MRI noting history of ankle instability and requesting evaluation for osteochondral lesion or peroneal tear. All patients had MRI. All magnets used in MRI were 1.0 to 1.5 T, and MRI scans were performed without contrast or arthrogram. We reviewed the original radiologist’s MRI report (regardless of the institution) and recorded any mention of associated ankle abnormalities, such as chondral lesions, peroneal tendon tears, and loose bodies. We reviewed the attending surgeon’s reading of the MRI noted in the chart and recorded any mention of these ankle abnormalities.
We compared findings from the radiologist’s and attending surgeon’s MRI readings with operative findings of lesions. Lesions not detected by MRI by either the radiologist or the attending surgeon but detected at surgery were counted as missed. We also noted lesions reported as present based on MRI by the reader but not found during surgery. Because of possible subjectivity in assessment, chondral lesions were counted as missed only if a microfracture, drilling, or substantial débridement was performed. We excluded consideration of lesions of the anterior talofibular ligament or the calcaneofibular ligament because we believed diagnosis of these lesions by MRI is not sufficiently reliable, and our decision for ligament reconstruction was based on history and clinical examination. Also excluded were tenosynovitis of the peroneal tendons and synovitis of the ankle. Sensitivity values were calculated separately for radiologists’ and the orthopaedic surgeon’s MRI readings, based on the total number of lesions found intraoperatively. For patients with more than one lesion, only the first chondral lesion observed in that patient was counted for sensitivity calculations.
Results
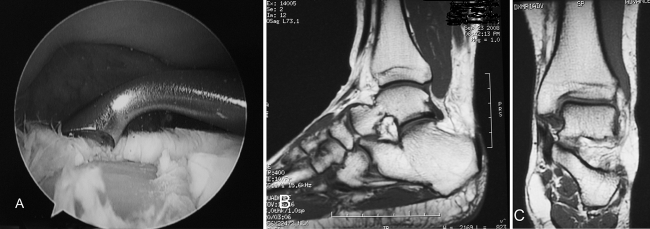
With 64 true positives and 29 read as positive by the radiologists, sensitivity of the radiologists’ MRI readings was 45% (Table 1). Sensitivity of the orthopaedic surgeon’s MRI readings, based on 40 identified lesions of 64 actual lesions, was 63% (Table 1). Radiologists detected one of the five additional lesions in patients who had two lesions. In one patient with two chondral lesions, the attending surgeon did not detect any lesions by MRI. Specificity was high for the radiologists’ (97%) and the orthopaedic surgeon’s (100%) MRI readings. Two chondral lesions identified by the radiologist on MRI were not found during surgery. Of the 20 chondral lesions not identified by the attending surgeon on MRI, 10 (50%) were on the medial side and five (25%) were posterior. We observed cases with extensive medial chondral injury without extension into the subchondral bone but unremarkable MRI findings (Fig. 1).
Table 1.
Comparison of lesions detected by radiologist and attending surgeon
| Lesion | Number of lesions | Number of lesions detected | |
|---|---|---|---|
| Radiologist | Attending surgeon | ||
| Chondral | 38 | 15 (40%) | 18 (47%) |
| Peroneus brevis tear | 18 | 10 (56%) | 16 (89%) |
| Loose body | 7 | 4 (57%) | 5 (71%) |
| Other | 1 | 0 (0%) | 1 (100%) |
Fig. 1A–C.
(A) An ankle arthroscopy image shows a large, full-thickness chondral lesion down to subchondral bone. (B) A sagittal MR image for this patient shows no evidence of the lesion with no change in the bone marrow signal. (C) A coronal MR image for the same patient similarly shows no evidence of a lesion.
The lowest detection rate for radiologists and the attending surgeon was for chondral lesions (40% and 47%, respectively) (Table 1). Detection of peroneus brevis tears and loose bodies was substantially higher for the radiologists and the attending surgeon, with the surgeon’s detection rate also substantially higher than that of the radiologists.
Discussion
Chondral lesions, peroneal tears, and other disorders occur relatively frequently in patients with chronic ankle instability [2, 7, 9, 20]. These associated lesions may be an important potential cause of long-term problems [7, 10, 15, 19, 24], and appropriate treatment depends on accurate diagnosis. Although studies have not established the long-term effect of chondral lesions and other disorders in ankle instability, it seems reasonable to assume diagnosis and treatment of these lesions are warranted in the absence of data to the contrary. Some of these associated lesions may be difficult to assess. To determine whether typical MRI could be relied on to establish the presence of these lesions, we assessed the accuracy of preoperative MRI as read by community radiologists and by an orthopaedic surgeon for detecting concomitant disorders.
This study is limited by several factors. First, MR images for most patients in this study were taken and read at various institutions, and the original reading was used in the study. The relatively low-powered magnets, multiple MRI sources, and possible variation in radiologists’ skills are limitations of the study, but this scenario also represents the clinical situation encountered by the practicing orthopaedist. Although a prospective study with one musculoskeletal radiologist and a 3-T magnet might alter the findings, these resources currently are not available to the general orthopaedic community. Also, although sensitivity of the radiologists’ detection of lesions was low, sensitivity of the orthopaedic surgeon’s MRI readings also was lower than would be desirable to detect lesions preoperatively. Only anterior ankle arthroscopy was performed on a routine basis, and therefore some medial and posterior lesions may have been missed on arthroscopy. Our surgical technique may not have detected all lesions because only one observer performed the arthroscopic procedure and only lesions in the surgical field could be observed. However, we believe a high rate of accuracy was obtained using arthroscopy in the area surrounding the ankle. No studies have reported on whether treatment of moderate cartilaginous injury affects long-term outcome. In the absence of published data, we believe prudence warrants diagnosis and treatment when possible.
There was an evident discrepancy between the radiologists and the attending surgeon in detecting lesions on preoperative MRI. Some of these differences, particularly with the less common diagnoses, may result from the clinician’s advantage in being able to take a history and perform an examination, which can guide scrutiny of the MRI. Also, the experienced orthopaedic surgeon is likely more attuned to disorders of the foot and ankle than the community radiologist, who often reads MR images of various parts of the body. A specialized musculoskeletal radiologist may have access to various imaging sequences and may have an extensive background in reading images of musculoskeletal tissue. The high MRI detection accuracy rate in a previous study may be partly attributable to the fact that 60% of the MRIs in that study were performed at the host institution with access to a musculoskeletal radiologist [2].
The lesion detection rate of the orthopaedic surgeon in our study was higher than the radiologists’ rate but inadequate to allow preoperative assessment of lesions that may require treatment, especially for chondral lesions. The low detection rate for chondral lesions was similar to that found previously with preoperative MRI in a study of athletes with symptomatic ankle lesions, where chondral lesions were detected in five of 26 patients (19%). Other investigators have reported a higher detection rate of chondral lesions on preoperative MRI, with 11 of 14 (79%) chondral lesions observed [2]. However, in that study, ankle exploration was performed without arthroscopy through an anterolateral incision. This method may limit detection of medial or posterior lesions, of which a relatively high number were observed in our study and previous investigations [7, 10, 15, 18, 20, 24]. In another report, eight of 21 (38%) chondral lesions were missed by preoperative MRI [25], similar to the rate found for the orthopaedic surgeon in the current study.
Our low detection rate of chondral lesions by MRI support a previous report suggesting these lesions are difficult to observe in the ankle [26] and in the knee using conventional MRI techniques [5, 13, 14, 22]. Although meniscus and ligament injuries are easily imaged, arthroscopy is required to see articular cartilage injuries in the knee [5, 14]. Also, almost all lesions missed on MRI in our study were full thickness and warranted microfracture, but the lesions were not large or deep. Because MRI detects subchondral changes, more superficial lesions are less likely to be imaged [25]. Other MRI factors that may affect accuracy include the type of sequence [5, 16, 17, 27], power of the magnet [11, 12, 26], and positioning [21]. The articular cartilage in the ankle is thinner than in the knee [23], there is close tibiotalar apposition, and the bony anatomy is more complex, all of which could complicate accurate observation of chondral lesions by MRI in the ankle as compared with the knee.
The rate of detection of peroneus brevis tears by the attending surgeon on preoperative MRI was 89%, similar to that found previously [2]. Although this finding shows MRI was relatively reliable at detecting peroneal tears, two tears were missed in our study. MRI may miss some of these lesions because of the location of the tear and orientation of the tendons as they turn the corner at the distal fibula. Radiologists were less able to detect a peroneal tear than the attending surgeon, but this may represent an advantage of the clinician who can examine the patient. The tendons should be inspected routinely during the ligament reconstruction, as suggested by others [1, 2].
We believe MRI is warranted in treatment of ankle instability for which surgery is considered, but our data suggest certain caveats. Although preoperative MRI sensitivity was not high for detecting lesions, many lesions were detected. Also, MRI is useful for incision planning, determination of equipment needed, and managing patients’ postoperative expectations. The current data suggest orthopaedic surgeons should evaluate preoperative MR images personally in addition to reading the radiologist’s report to ensure maximum value of MRI in a clinical scenario where imaging may be obtained in variable settings. The clinical importance of chondral and other associated lesions is not yet established, but prudence dictates detection and treatment whenever possible. Our findings suggest ankle arthroscopy may be needed for the most accurate diagnosis possible in patients undergoing ligament reconstruction for ankle instability.
Acknowledgments
We thank Lyn Camire, MA, ELS, of our department for editorial support.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Bonnin M, Tavernier T, Bouysset M. Split lesions of the peroneus brevis tendon in chronic ankle laxity. Am J Sports Med. 1997;25:699–703. doi: 10.1177/036354659702500520. [DOI] [PubMed] [Google Scholar]
- 2.DiGiovanni BF, Fraga CJ, Cohen BE, Shereff MJ. Associated injuries found in chronic lateral ankle instability. Foot Ankle Int. 2000;21:809–815. doi: 10.1177/107110070002101003. [DOI] [PubMed] [Google Scholar]
- 3.Ferkel RD, Chams RN. Chronic lateral instability: arthroscopic findings and long-term results. Foot Ankle Int. 2007;28:24–31. doi: 10.3113/FAI.2007.0005. [DOI] [PubMed] [Google Scholar]
- 4.Freeman MA. Instability of the foot after injuries to the lateral ligament of the ankle. J Bone Joint Surg Br. 1965;47:669–677. [PubMed] [Google Scholar]
- 5.Friemert B, Oberlander Y, Schwarz W, Haberle HJ, Bahren W, Gerngross H, Danz B. Diagnosis of chondral lesions of the knee joint: can MRI replace arthroscopy? A prospective study. Knee Surg Sports Traumatol Arthrosc. 2004;12:58–64. doi: 10.1007/s00167-003-0393-4. [DOI] [PubMed] [Google Scholar]
- 6.Garrick JG. The frequency of injury, mechanism of injury, and epidemiology of ankle sprains. Am J Sports Med. 1977;5:241–242. doi: 10.1177/036354657700500606. [DOI] [PubMed] [Google Scholar]
- 7.Hintermann B, Boss A, Schafer D. Arthroscopic findings in patients with chronic ankle instability. Am J Sports Med. 2002;30:402–409. doi: 10.1177/03635465020300031601. [DOI] [PubMed] [Google Scholar]
- 8.Karlsson J, Bergsten T, Lansinger O, Peterson L. Lateral instability of the ankle treated by the Evans procedure: a long-term clinical and radiological follow-up. J Bone Joint Surg Br. 1988;70:476–480. doi: 10.1302/0301-620X.70B3.3372575. [DOI] [PubMed] [Google Scholar]
- 9.Kibler WB. Arthroscopic findings in ankle ligament reconstruction. Clin Sports Med. 1996;15:799–804. [PubMed] [Google Scholar]
- 10.Komenda GA, Ferkel RD. Arthroscopic findings associated with the unstable ankle. Foot Ankle Int. 1999;20:708–713. doi: 10.1177/107110079902001106. [DOI] [PubMed] [Google Scholar]
- 11.Kuikka PI, Kiuru MJ, Niva MH, Kroger H, Pihlajamaki HK. Sensitivity of routine 1.0-Tesla magnetic resonance imaging versus arthroscopy as gold standard in fresh traumatic chondral lesions of the knee in young adults. Arthroscopy. 2006;22:1033–1039. doi: 10.1016/j.arthro.2006.06.021. [DOI] [PubMed] [Google Scholar]
- 12.Mori R, Ochi M, Sakai Y, Adachi N, Uchio Y. Clinical significance of magnetic resonance imaging (MRI) for focal chondral lesions. Magn Reson Imaging. 1999;17:1135–1140. doi: 10.1016/S0730-725X(99)00033-8. [DOI] [PubMed] [Google Scholar]
- 13.Munk B, Madsen F, Lundorf E, Staunstrup H, Schmidt SA, Bolvig L, Hellfritzsch MB, Jensen J. Clinical magnetic resonance imaging and arthroscopic findings in knees: a comparative prospective study of meniscus anterior cruciate ligament and cartilage lesions. Arthroscopy. 1998;14:171–175. doi: 10.1016/s0749-8063(98)70036-2. [DOI] [PubMed] [Google Scholar]
- 14.Ochi M, Sumen Y, Kanda T, Ikuta Y, Itoh K. The diagnostic value and limitation of magnetic resonance imaging on chondral lesions in the knee joint. Arthroscopy. 1994;10:176–183. doi: 10.1016/s0749-8063(05)80090-8. [DOI] [PubMed] [Google Scholar]
- 15.Okuda R, Kinoshita M, Morikawa J, Yasuda T, Abe M. Arthroscopic findings in chronic lateral ankle instability: do focal chondral lesions influence the results of ligament reconstruction? Am J Sports Med. 2005;33:35–42. doi: 10.1177/0363546504271058. [DOI] [PubMed] [Google Scholar]
- 16.Potter HG, Linklater JM, Allen AA, Hannafin JA, Haas SB. Magnetic resonance imaging of articular cartilage in the knee: an evaluation with use of fast-spin-echo imaging. J Bone Joint Surg Am. 1998;80:1276–1284. doi: 10.2106/00004623-199809000-00005. [DOI] [PubMed] [Google Scholar]
- 17.Recht MP, Kramer J, Marcelis S, Pathria MN, Trudell D, Haghighi P, Sartoris DJ, Resnick D. Abnormalities of articular cartilage in the knee: analysis of available MR techniques. Radiology. 1993;187:473–478. doi: 10.1148/radiology.187.2.8475293. [DOI] [PubMed] [Google Scholar]
- 18.Rolf CG, Barclay C, Riyami M, George J. The importance of early arthroscopy in athletes with painful cartilage lesions of the ankle: a prospective study of 61 consecutive cases. J Orthop Surg Res. 2006;1:4. doi: 10.1186/1749-799X-1-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sammarco GJ, DiRaimondo CV. Surgical treatment of lateral ankle instability syndrome. Am J Sports Med. 1988;16:501–511. doi: 10.1177/036354658801600513. [DOI] [PubMed] [Google Scholar]
- 20.Schafer D, Hintermann B. Arthroscopic assessment of the chronic unstable ankle joint. Knee Surg Sports Traumatol Arthrosc. 1996;4:48–52. doi: 10.1007/BF01565998. [DOI] [PubMed] [Google Scholar]
- 21.Schneck CD, Mesgarzadeh M, Bonakdarpour A, Ross GJ. MR imaging of the most commonly injured ankle ligaments. Part I. Normal anatomy. Radiology. 1992;184:499–506. doi: 10.1148/radiology.184.2.1620855. [DOI] [PubMed] [Google Scholar]
- 22.Speer KP, Spritzer CE, Goldner JL, Garrett WE., Jr Magnetic resonance imaging of traumatic knee articular cartilage injuries. Am J Sports Med. 1991;19:396–402. doi: 10.1177/036354659101900414. [DOI] [PubMed] [Google Scholar]
- 23.Sugimoto K, Takakura Y, Tohno Y, Kumai T, Kawate K, Kadono K. Cartilage thickness of the talar dome. Arthroscopy. 2005;21:401–404. doi: 10.1016/j.arthro.2004.12.005. [DOI] [PubMed] [Google Scholar]
- 24.Taga I, Shino K, Inoue M, Nakata K, Maeda A. Articular cartilage lesions in ankles with lateral ligament injury: an arthroscopic study. Am J Sports Med. 1993;21:120–126. doi: 10.1177/036354659302100120. [DOI] [PubMed] [Google Scholar]
- 25.Takao M, Uchio Y, Naito K, Fukazawa I, Ochi M. Arthroscopic assessment for intra-articular disorders in residual ankle disability after sprain. Am J Sports Med. 2005;33:686–692. doi: 10.1177/0363546504270566. [DOI] [PubMed] [Google Scholar]
- 26.Tan TC, Wilcox DM, Frank L, Shih C, Trudell DJ, Sartoris DJ, Resnick D. MR imaging of articular cartilage in the ankle: comparison of available imaging sequences and methods of measurement in cadavers. Skeletal Radiol. 1996;25:749–755. doi: 10.1007/s002560050173. [DOI] [PubMed] [Google Scholar]
- 27.Verhaven EF, Shahabpour M, Handelberg FW, Vaes PH, Opdecam PJ. The accuracy of three-dimensional magnetic resonance imaging in the diagnosis of ruptures of the lateral ligaments of the ankle. Am J Sports Med. 1991;19:583–587. doi: 10.1177/036354659101900605. [DOI] [PubMed] [Google Scholar]