Abstract
Background
Radiofrequency-generating energy devices have been used clinically in musculoskeletal procedures to provide hemostasis and capsular shrinkage (thermal capsulorrhaphy). However, the dose-effects are not well known.
Questions/Purposes
We therefore determined dosage effects of radiofrequency energy on bone, skin incisions, and joint capsule in sheep.
Methods
Five mature sheep had six 2.5-cm2 tibial periosteal defects and six 1.0-cm skin incisions assigned to six treatments varying by watts and fluence (f = watts · seconds/cm2): (1) untreated control, (2) 50 W for 9.5 seconds (190f; n = 5), (3) 110 W for 4.3 seconds (190f; n = 5), (4) 170 W for 2.8 seconds (190f; n = 5), (5) 170 W for 5.6 seconds (380f; n = 5), or (6) 170 W for 8.4 seconds (570f; n = 5). Outcomes included hemostasis, contraction, healing, and histomorphometry for inflammation and necrosis at 2 weeks.
Results
Radiofrequency energy application on skin at 190f or greater had more than 80% hemostasis and dose-dependent contraction, inflammation, and necrosis. Radiofrequency energy application on bone had good (70%) hemostasis at 190f and complete (> 95%) hemostasis at 380f and 570f, without histologic or clinically detectable necrosis.
Conclusions
Hemostasis can be achieved with radiofrequency energy at 190f in skin and bone. Bone necrosis was not detected at up to 570f. Using fluence greater than 190f in skin achieved dose-dependent necrosis and incisional contraction.
Clinical Relevance
Radiofrequency energy can be used on bone and skin for hemostasis, but potential incisional complications, such as necrosis and an atypical firm and desiccated surface, should be expected.
Introduction
Radiofrequency-generating energy devices have been used clinically in musculoskeletal procedures, such as chondroplasty [9, 13, 35, 39, 41], arthroscopic treatment of intraarticular tissues [1, 3, 14, 21, 26, 29, 31, 33, 43], meniscectomy [16, 25], and treatment of musculoskeletal tumors [8, 12, 23, 24, 27, 34, 37], to provide hemostasis and thermal capsulorrhaphy.
The potential clinical consequences from surgical blood loss for patients undergoing these procedures include (1) decreased intraoperative visualization, (2) increased risk of blood transfusion, and (3) high incidence of postoperative complications, such as development of postoperative hematomas [19, 35], swelling and pain [19, 35], risk of infection [19, 35, 38], and potentially delayed rehabilitation, including second surgery [19, 35]. Surgeons and operating room personnel are at risk for blood-borne diseases potentially transmitted on blood splash during total arthroplasty [38], such as hepatitis B virus (HBV) and HIV. In orthopaedics, from 3239 healthcare workers tested, 13% had HBV infections develop [11]. After occupational exposure to HIV-infected blood, the risk of infection after percutaneous exposure has been estimated at approximately 0.3% and 0.09% after membrane mucous exposure [11]. Physical barriers, such as visor masks, to block blood exposure events fail to protect the surgeon from splash [38]. Use of radiofrequency energy (RFE) would decrease the risk of exposure to blood and thus reduce the peril of acquired blood-borne diseases [18].
RFE is a form of electromagnetic energy that, when applied to tissues with a high collagen content, causes the heat-labile intramolecular cross-links to break and the protein to undergo a transition from a highly organized crystalline structure to a random, gel-like state [3]. The level of energy, duration of treatment, and nature of the tissues determine this thermal effect. The bipolar electrode size and shape influences the extent of thermal modification of tissues, as does the pattern of operator use [3]. When temperature rises above 65°C [2, 15, 17], collagen denatures regardless of the source of thermal energy [3]. Electromagnetic energy can be applied between two points on the tip of a probe (bipolar) or between one electrode tip and a grounding plate (monopolar). In monopolar devices, the molecular friction created in the tissues adjacent to the probe produces heat. Thus, the actual source of heat is the frictional resistance of the tissues rather than the probe. With bipolar probes, the electromagnetic energy follows a much shorter path through a conductive irrigating solution or through the tissues between the tips of the probe. Less current is required with a bipolar device than with a monopolar device to achieve the same effect because the current passes through a much smaller volume of tissue. In addition, the depth of tissue damage relative to the probe tip may be less with a bipolar device [3]. Saline-coupled bipolar sealing technology uses bipolar RFE combined with an automated, adjustable, but continuous, saline flow at the electrode tip to control the increase in tissue temperature and thus control alterations to the tissue. Bipolar RFE offers advantages for hemostasis by reducing the tissue carbonization and necrosis that occurs with electrocautery. Specifically, use of a bipolar RFE device with conductive fluid avoids bone necrosis on CT and histology when used on cortical and cancellous bone in vivo with 92% hemostasis and applied at a modest dose of 50 W for 11 seconds in an area of 2.9 cm2 (190 fluence [f = watts · seconds/cm2]) [6]. However, the dosage effects of RFE are not well known.
We determined dosage effects of RFE on bone, skin incisions, and joint capsule in sheep. We hypothesized: (1) all dosages of RFE would produce hemostasis with minimal necrosis in cortical bone and (2) increasing fluence greater than 190f, specifically 380f and 570f, would cause a dose-dependent necrosis and contraction in soft tissue.
Materials and Methods
Five mature sheep had six 2.5-cm2 circular periosteal defects, three per tibia, made and assigned to treatment using a commercially available bipolar RFE device clinically introduced in 2005 and designed to accept a saline (0.9% NaCl) drip. Treatment of the tibial periosteal defects was as follows: (1) untreated control (n = 5), (2) 50 W for 9.5 seconds (190f; n = 5), (3) 110 W for 4.3 seconds (190f; n = 5), (4) 170 W for 2.8 seconds (190f; n = 5), (5) 170 W for 5.6 seconds (380f; n = 5), or (6) 170 W for 8.4 seconds (570f; n = 5). Additionally, on the same sheep, three 1.0-cm skin incisions were made with a scalpel in tandem at the seventh intercostal space bilaterally (six incisions/sheep) and the incisions were treated with RFE of (1) 190f (n = 10), (2) 380f (n = 10), or (3) 570f (n = 10) (Fig. 1). Treatments were assigned to the proximal, middle, or distal incision sites such that each of the three RFE dosages occurred at each site an equal number of times. Power calculations were made based on assuming a 5% alpha error level and a power greater than 0.8 for our outcomes based on clinically meaningful effects. In Marulanda et al. [30], bipolar sealer decreased total blood loss by 40% and transfusions from 52% to 20% in patients having hip arthroplasty. The power calculation was made by using this effect size (a minimum of 40% bleeding reduction), a SD of the hemostasis variables from our previous work [6], and a 5% alpha error level (95% confidence level). Based on this power analysis, the n = 5 sample size was estimated to be sufficient to show at least a 40% reduction in blood loss with high power (> 0.98). Power-based SDs from published work of histomorphometry on tibia cortical bone [5], using adult sheep of the same size and age and the same dose of RFE on the same site in the tibia, estimated a sample size of n = 5 would be overpowered (power = 0.9–1.0) to observe differences among our treatments for necrosis. Procedures performed for this study were reviewed and approved by the Institutional Animal Care and Use Committee at The Ohio State University.
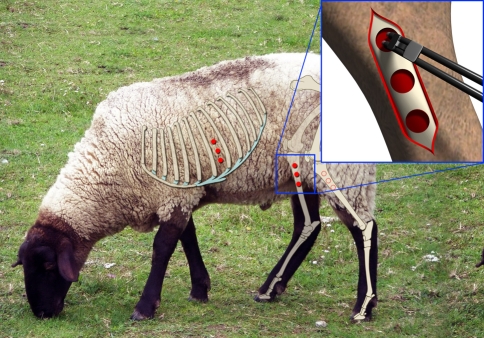
Fig. 1.
An illustration of the surgical sheep model shows the periosteal defects on the tibial cortical bone and intercostal skin incisions to be treated with the bipolar RFE device.
We used an Aquamantys™ System generator and hand piece (Salient Surgical Technologies, Inc, Portsmouth, NH) to apply RFE to the defects, varying watts (50 W, 110 W, or 170 W) or fluence (190f, 380f, or 570f). The Aquamantys™ System is automated to vary the flow rate (0.5–36 mL/minute) depending on power setting (20–200 W) to maintain the surface probe temperature at less than 100°C [16].
The sheep were induced with a combination of xylazine hydrochloride (0.1 mg/kg dose; xylazine, 20 mg/mL) and ketamine hydrochloride (2-mg/kg dose; Ketaset®; Fort Dodge Animal Health, Madison, NJ) and maintained under general anesthesia with isofluorane (1.5%; Isoflo®; Abbott Laboratories, North Chicago, IL). Under general anesthesia, the sheep were placed in dorsal recumbency. Both tibiae and intercostal spaces were clipped and aseptically prepared. On the midmedial tibia, a 12-cm scalpel incision was made, extending to the periosteum. A sterile, plastic template was used to trace the defects (2.5 cm2) and standardize the distance between them (1.5 cm apart). A Number 15 scalpel blade was used to cut the periosteum to bone using the template. The template was removed. The periosteum was stripped from the surface of the tibia cortical bone 1 minute before application of the assigned RFE. Subcutaneous tissue was closed using 2-0 polyglycolic sutures in a simple continuous pattern. Staples were used on skin. A bandage was applied on each tibia. The intercostal skin incisions (1 cm in length) were made using a Number 10 scalpel blade full-thickness through the epidermis and dermis. A template was used to determine size and distance between incisions. Simple interrupted 2-0 nylon sutures were used in the skin after RFE application.
After surgery, the animals were allowed unrestricted activity in a 4- by 8-foot cage; sheep were seen daily postoperatively by one author (MM) to assess lameness, drainage, and swelling. There were no intraoperative or postoperative complications. Animals were euthanized by overdose of barbiturate (100 mg/kg; Euthasol™; Virbac Corp, Fort Worth, TX) at 2 weeks.
The outcome measurement for hemostasis in cortical bone and skin incisions was the percentage of surface without bleeding immediately and 1 minute after device application. A 1-mm grid template was placed over the bone and incision surface and the intersections were counted as bleeding or not bleeding for the entire surface and expressed as a percent. The outcome measure for skin incision contraction was the percentage of reduction in incision area 1 minute after device application. Estimates were made by two blinded investigators (AB, MM). Skin incisions also were quantified objectively in a blinded fashion by two of us (MM, AB) daily for swelling (measurement of swelling in centimeters from the incision at the widest point) [5]. Final skin incision healing was assessed blindly (AB, MM) as a score of 0 to 4 at 2 weeks (0 = primary healing; 1 = minimal atypical surface; 2 = mild atypical surface; 3 = moderate atypical surface; 4 = marked atypical surface [4]).
Lameness was scored by one investigator (MM) as 0 to 5 for each hind limb (0 = no lameness, 1 = minimal, 2 = mild, 3 = moderate, 4 = marked, 5 = nonweightbearing [22]). At termination of the study at 2 weeks, the cortical bone and skin incisions were harvested in cross section from the center of the lesion for a measurement (in millimeters) of visible depth of tissue change and cross-sectional histologic analysis. Joint capsule contraction was assessed ex vivo immediately after euthanasia by two blinded investigators (MM, AB). Four 2-cm2 joint capsule specimens were harvested from the caudal femorotibial joint capsule of all five sheep (n = 20) for 0, 190f, 380f, or 570f RFE application to the synovial surface. Objective measurement of the width and length of the synovial surface before and after device application was made by MM and verified by AB in a blinded fashion.
After gross evaluation and measurements, we fixed the cross-sectioned blocks of the dorsomedial half of the tibial cortical bone, skin incisions, and joint capsule in 10% neutral-buffered formalin and sectioned en bloc. Tibia specimens were decalcified in 10% EDTA. Paraffin-embedded sections (10 μm) were prepared and stained with hematoxylin and eosin. Sections from each tibial sample were evaluated by three investigators (SW, AB, MM) for extracellular matrix staining, cellular morphology, and distribution. We considered normal osteocytes to have dark staining nuclei and lie within lacunae from which canaliculi radiate. Fine cytoplasmatic processes of osteocytes occupied the canaliculi and communicated with adjacent osteocytes [44].
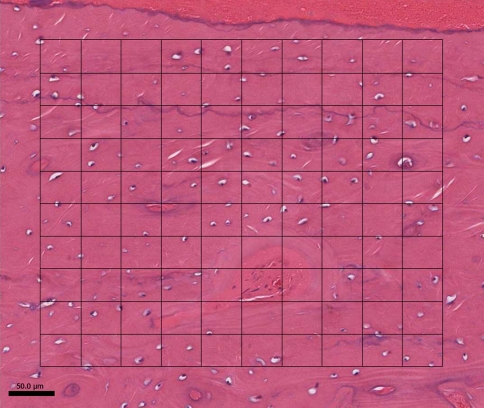
Of multiple sections, all three investigators selected the best and most representative from each tibial sample to be analyzed by histomorphometry by one investigator (MM) without knowledge of the groups. We used a point-counting grid (250 μm) at ×20 magnification to count the number of total and empty lacunae at the periosteal zone (grid on the dorsal surface of the tibia near the middle of the periosteal defect) and endosteal zone (grid on the inner layer of compact bone directly under the sites of measurement of the periosteal zone) and expressed as a percentage of empty lacunae (number of empty lacunae/number of total lacunae × 100) (Fig. 2). Bone necrosis is represented histologically as areas of completely empty lacunae in bone [42]. Necrotic bone may be replaced without any clinical implications or may sequester if infection is present [42].
Fig. 2.
A representative histologic section of the periosteal zone in tibial cortical bone treated with 570f RFE, showing the microscope grid (250 μm) and the field counted, shows the evenly distributed lacunae containing morphologically normal osteocytes (Stain, hematoxylin & eosin; original magnification, ×20 magnification).
Skin incisions were scored blindly by two of us (AB, SW) for amount of inflammatory cells and edema (0–4; 0 = none, 4 = marked) and necrosis (0–4; 0 = none, 4 = marked [32]). Inflammatory cells were monocyte/macrophage cells. Proteinaceous fluid, noted as diffuse light pink or unstained nonfibrillar, acellular material in between tissues planes was scored for presence and amount of edema. Intracapsular femorotibial joint sections were scored for presence of coagulation (dark pink amorphous nonfibrillar appearance on polarized light within the fibrillar extracellular matrix [ECM]) as 0 to 4 (0 = fibrillar ECM; 1 = minimal amorphous nonfibrillar ECM; 2 = mild amorphous nonfibrillar ECM; 3 = moderate amorphous nonfibrillar ECM; 4 = marked amorphous nonfibrillar ECM [6]).
Descriptive variables included treatments, sheep, and sides (eg, left versus right hind limbs or skin incisions), whereas the treatments and sides were considered nested in sheep. The intraobserver consistency when counting cells under the microscope was assessed by counting the number of total lacuna five times in the same defined 250-μm region of the same section. This represents approximately 200 lacunae per counting session. The coefficient of variation (CV) was calculated among the five measurements in the same site to estimate the repeatability of outcomes by one observer. The intraobserver CV value was 2.90% in the number of total lacunae outcome, confirming a low variation. Additionally, the total lacunae were counted among three adjacent regions in the periosteal and endosteal zones (total six regions) in the same section for 10 of control and 10 of 170 W for 8.4 seconds (570f) groups to determine a variability of outcomes in the treated sites of the bone specimens. The CV value was 5.29% in the number of total lacunae outcome.
We used a repeated-measures ANOVA to perform multiple comparisons between the treatment groups with PROC MIXED statistical models for continuous outcomes (ie, percent hemostasis, percent contraction, skin incision wound swelling, and percent empty lacunae) and GENMOD statistical models for categorical outcomes (ie, scored data such as histologic coagulation and inflammation). Multiple comparisons were made among the three treatments (170 W for 2.8 seconds [190f], 170 W for 5.6 seconds [380f], and 170 W for 8.4 seconds [570f]) for percent contraction, skin incision swelling, and skin incision histologic scores. For skin incision swelling, the comparisons were made in each time (eg, 5–15 postoperative days). In bone, multiple comparisons were made among the five treatments (50 W for 9.5 seconds [190f], 110 W for 4.3 seconds [190f], 170 W for 2.8 seconds [190f], 170 W for 5.6 seconds [380f], and 170 W for 8.4 seconds [570f]) for percent hemostasis or the six treatments (control, 50 W for 9.5 seconds [190f], 110 W for 4.3 seconds [190f], 170 W for 2.8 seconds [190f], 170 W for 5.6 seconds [380f], and 170 W for 8.4 seconds [570f]) for the number of empty lacunae. A commercial software program (SAS® Version 8.2; SAS Institute Inc, Cary, NC) was used for data analysis.
Results
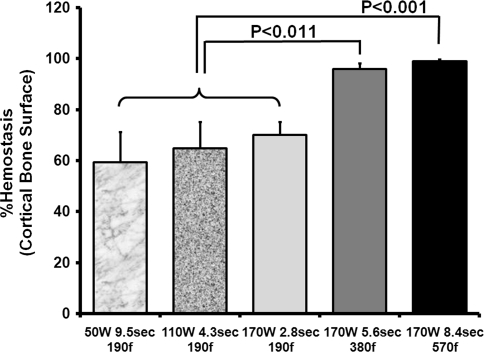
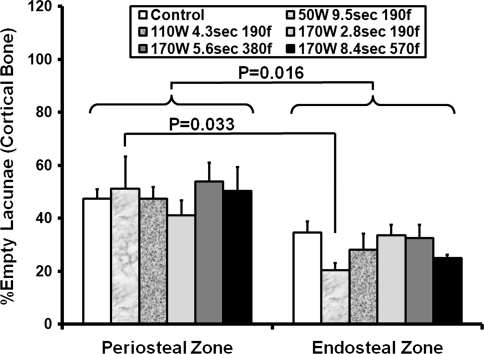
RFE application on bone produced increased hemostasis with greater fluence (380f and 570f), without histologic or clinically detectable necrosis. Specifically, tibial cortical bone hemostasis was greater (p < 0.01) at 380f (96% ± 2.1%) and 570f (99% ± 0.7%) than at 190f (70% ± 5.1%) (Table 1; Fig. 3). All tibial incisions healed primarily without drainage or swelling. Histologically, on the periosteal and endosteal zones, there was no increase in empty lacunae among treatments. The empty lacunae were distributed evenly in the bone, and no patches of empty lacunae were seen. Many cells (mean 112 cells/250-μm grid at x20 magnification ± 5) were morphologically normal and housed in lacunae in all groups (Fig. 2). Contrary to expectation, on the endosteal zone, in the 50 W, 190f RFE treatment group, there were fewer (p < 0.02) empty lacunae than in the untreated control group. In all tibiae, the periosteal zone had more (p < 0.03) empty lacunae than the endosteal zone, regardless of energy application (Fig. 4).
Table 1.
Clinical and histologic variables
| Site | Outcome | Control | 50 W 9.5 seconds 190f | 110 W 4.3 seconds 190f | 170 W 2.8 seconds 190f | 170 W 5.6 seconds 380f | 170 W 8.4 seconds 570f |
|---|---|---|---|---|---|---|---|
| Tibia | Hemostasis (%) | 0 | 59 ± 12* | 65 ± 10* | 70 ± 5* | 96 ± 2*,† | 99 ± 1*,† |
| Skin incision | Hemostasis (%) | NA | NA | NA | 84 ± 4 | 92 ± 3 | 97 ± 2‡ |
| Healing score | NA | NA | NA | 4 (3.5–4) | 2.5 (0.5–4)‡ | 2 (0–4)‡ | |
| Joint capsule | Coagulation score | 0 (0) | NA | NA | 1 (1–2)* | 4 (0–4)* | 0 (0–4) |
Values are expressed as mean ± standard error of the mean or mean, with range in parentheses; *different from control (p < 0.03); †different from all three 190f treatments (50 W 9.5 seconds, 110 W 4.3 seconds, 170 W 2.8 seconds) (p < 0.04); ‡different from 170 W 2.8 seconds 190f treatment (p < 0.02); NA = not applicable.
Fig. 3.
A graph shows the percentage of hemostasis of cortical bone. Tibial cortical bone hemostasis was greater (p < 0.01) at 380f and 570f than at 190f.
Fig. 4.
A graph shows the percentage of empty lacunae on the periosteal and endosteal zones in the tibial cortical bone. On the endosteal zone, in the 50 W, 190f RFE treatment group, there were fewer (p < 0.02) empty lacunae than in the untreated control group. In all tibiae, the periosteal zone had more (p < 0.03) empty lacunae than the endosteal zone, regardless of energy application.
RFE application on skin at 190f or greater produced more than 84% hemostasis and a dose-dependent necrosis of skin and subcutaneous tissues. Specifically, in the skin incisions, hemostasis was 84% or greater for all fluences (190–570f). Skin incision contraction and joint capsule contraction increased (p < 0.03) with increased fluence (Fig. 5). There was no drainage from the skin incisions after 72 hours. The 570f had a sustained and greater (p < 0.04) skin incisional swelling for the 2 weeks of the study. None of the incisions were painful on palpation. Eight of 10 190f skin incisions healed by primary apposition of skin edges. Variably, but more frequently (p < 0.01) than 190f, the 380f and 570f incisions developed a firm, dry, fleeceless surface, scored as atypical healing. After skin and subcutaneous tissue harvest, a dose-dependent increase (p < 0.02) in depth of visibly abnormal tissue was measured (Fig. 6). On histologic evaluation, an increase (p < 0.04) in inflammation and necrosis was observed with increased fluence in the skin incisions (Fig. 7). Sheep were clinically normal in health and gait throughout the study, except one sheep, which had intermittent, 2 hours’ duration lameness after recovery from anesthesia in the hind limb treated with the higher fluence levels.
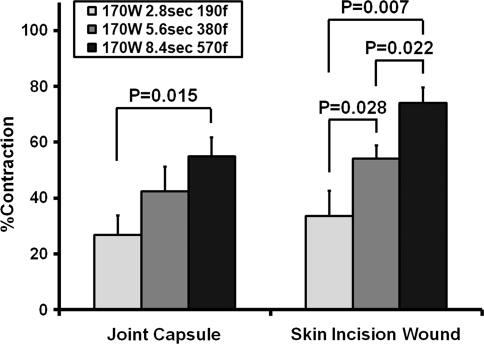
Fig. 5.
A graph shows the percentage of contraction of skin incisions (in vivo) and the percentage of contraction of the femorotibial joint capsule (ex vivo) after RFE device application. Skin incision contraction and joint capsule contraction increased (p < 0.03) with increased fluence.
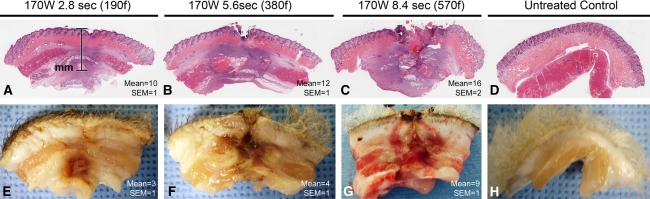
Fig. 6A–H.
Necrosis depth (mm; mean ± standard error of the mean [SEM]) is shown at (A) 10 ± 1 m, 170 W for 2.8 seconds, 190f (B) 12 ± 1 m, 170 W for 5.6 seconds, 380f, (C) 16 ± 2 m, 170 W fir 8.4 seconds, 570 w, and in the (D) untreated control (Stain, hematoxylin & eosin). In the gross cross sections from the skin incisions at 2 weeks of healing, necrosis depth is shown at (E) 3 ± 1 mm, 170 W for 2.8 seconds, 190f; (F) 4 ± 1 mm, 170 W for 5.6 seconds, 380f; (G) 9 ± 1 mm, 170 W for 8.4 seconds, 570f; and in the (H) untreated control. A dose-dependent increase (p < 0.02) in depth of visibly abnormal tissue can be seen.
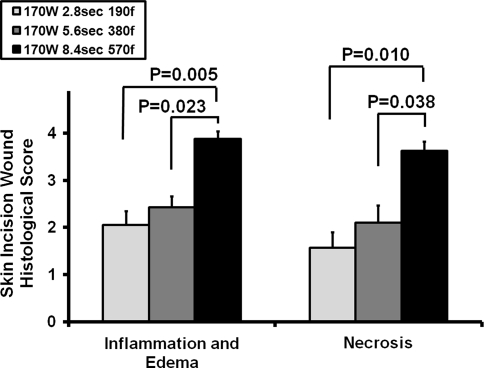
Fig. 7.
A graph shows the histomorphology scores of the intercostal space skin incisions for inflammation, edema, and necrosis. An increase (p < 0.04) in inflammation and necrosis can be seen with increased fluence.
Discussion
RFE devices are used clinically in musculoskeletal procedures to make incisions, control hemorrhage in bone, and reduce joint laxity by inducing contraction of the joint capsule and surrounding joint soft tissues (thermal capsulorrhaphy). We aimed to determine if a range of dosages of RFE would produce hemostasis with minimal necrosis in cortical bone and if increasing fluence greater than 190f, specifically 380f and 570f, would cause a dose-dependent necrosis and contraction in soft tissue.
Our study has several limitations. First, the power analysis for our sample size was based on statistical calculations for many of the parameters, such as histomorphometry for osteonecrosis. Experimental studies rely on histomorphometry as a highly rigorous and sensitive assessment of bone necrosis, but the clinical correlations to bone pain, drainage, or failed surgeries are not published. In an animal study of subchondral bone in naturally occurring osteoarthritis, correlative sections of bone histomorphometry and clinical CT showed excellent correlation for bone density, bone sclerosis, and bone resorption [45]. In a previous publication in sheep using RFE on bone, the CT correlated to histology [5]. Second, we do not have a control using another device. In previous work using similar RFE on sheep bone, electrocautery induced char and less hemostasis [5]. In patients undergoing joint arthroplasty, RFE on bone reportedly produces less blood loss, smoke, and tissue damage than electrocautery, including less decrease in hemoglobin postoperatively [30]. Our focus was to compare dosages of RFE for clinical use. Previous work provides sufficient evidence that RFE is superior to electrocautery for hemostasis [5, 30]. Third, numerous key outcome variables were semiquantitative and may have some inherent bias. Assigned scores were used for outcome variables believed to be important but difficult to quantify, such as bleeding intensity, swelling, and limb pain. Assignment of scores at surgery was performed by multiple individuals and the dosage used was not announced, but the duration of application would be apparent to the surgeon and provide some insight regarding the treatment. However, multiple investigators were used in the scoring, one without any knowledge of application.
All dosages (190f, 380f, and 570f) of RFE induced hemostasis with minimal necrosis in cortical bone. Our data on bone hemostasis correspond to clinical data presented by Marulanda et al. [30] that showed a substantial reduction in the total blood loss and postoperative drainage in primary hip arthroplasties. Our data on bone necrosis correspond to clinical data by Bonutti et al. [7]. In 2386 patients who underwent knee arthroplasties, osteonecrosis occurred in 24 patients or 1% [7]. Of the 24 patients, 10 had a history of arthroscopic débridement with RFE. They reported osteonecrosis on postarthroscopic MRI, whereas preoperative MRI was normal. Cetik et al. [13], in a study of 50 patients who underwent arthroscopic chondroplasties and bipolar RFE, detected subchondral osteonecrosis in two (4%) on the postoperative MRI performed 6 months after the arthroscopy. Our data supported these clinical findings and showed lack of necrosis at as much as 570f of RFE on cortical bone. This low incidence of necrosis of RFE on bone may be related to the high mineral content (hydroxyapatite) and lower collagen content in cortical bone compared with soft tissue and skin [30].
Increasing fluence greater than 190f, specifically to 380f and 570f, caused a dose-dependent necrosis and contraction in soft tissue, specifically for the skin and joint capsule. Hecht et al. [20] reported increased stiffness of RFE-treated joint capsular tissue returned to a normal value by 6 weeks. However, Lopez and Markel [28] reported canine ACLs treated with monopolar RFE were torn approximately 55 days after treatment. In addition, Scheffler et al. [36] reported the effect of RFE shrinkage on the structural properties of the elongated ACL in a sheep model. They reported the initial reduction of knee laxity after RFE treatment could not be maintained at 24 weeks. The literature supports RFE shrinkage of soft tissue, but persistence and necrosis were not fully evaluated. Our study showed dose-dependent necrosis was associated with the contracture of soft tissue, at least skin and joint capsule. This could result in an undesirable joint capsule contracture and thus reduce joint mobility and delay rehabilitation.
Additional and longer-term investigation of the biologic response to thermal modification after cumulative dosages of RFE using in vivo models is needed. The factors that lead to capsular tissue failure, cellular death, and subchondral osteonecrosis after thermal alteration, and the threshold at which tissue becomes irreparable by biologic processes, need to be defined. RFE, in combination with complementary blood management strategies such as preoperative autologous blood donation [10, 40], allogenic blood transfusion [10, 40], hypotensive anesthesia [10, 40], acute normovolemic hemodilution [10, 40], and recombinant human erythropoietin [10, 40], may help to mitigate surgical and postoperative bleeding. Reducing the need for transfusion and delayed rehabilitation will decrease morbidity and medical and financial costs.
Acknowledgments
We thank the Wiseman Hall ULAR Staff and Facilities and Drs Kelly Santangelo, Päivi Rajala-Schultz, Famke Aeffner, and Elijah Hothem for professional assistance and Tim Vojt for illustrations.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Footnotes
The institution of one or more authors (AB, SW) received a contract for partial support of this study from Salient Surgical Technologies, Inc, Portsmouth, NH.
Each author certifies that his or her institution approved the animal protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Alemdaroğlu KB, Cimen O, Aydoğan NH, Atlihan D, Iltar S. Early results of arthroscopic lateral retinacular release in patellofemoral osteoarthritis. Knee. 2008;15:451–455. doi: 10.1016/j.knee.2008.06.003. [DOI] [PubMed] [Google Scholar]
- 2.Allain JC, Le Lous M, Cohen-Solal L, Bazin S, Maroteaux P. Isometric tensions developed during the hydrothermal swelling of rat skin. Connect Tissue Res. 1980;7:127–133. doi: 10.3109/03008208009152104. [DOI] [PubMed] [Google Scholar]
- 3.Arnoczky SP, Aksan A. Thermal modification of connective tissues: basic science considerations and clinical implications. J Am Acad Orthop Surg. 2000;8:305–313. doi: 10.5435/00124635-200009000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Barber FA, Iwasko NG. Treatment of grade III femoral chondral lesions: mechanical chondroplasty versus monopolar radiofrequency probe. Arthroscopy. 2006;22:1312–1317. doi: 10.1016/j.arthro.2006.06.008. [DOI] [PubMed] [Google Scholar]
- 5.Bertone A, Lipson D, Kamei J, Litsky A, Weisbrode S. Effective bone hemostasis and healing using radiofrequency and conductive fluid. Clin Orthop Relat Res. 2006;446:278–285. doi: 10.1097/01.blo.0000201163.97937.1a. [DOI] [PubMed] [Google Scholar]
- 6.Bertone AL, Goin S, Kamei SJ, Mattoon JS, Litsky AS, Weisbrode SE, Clarke RB, Plouhar PL, Kaeding CC. Metacarpophalangeal collateral ligament reconstruction using small intestinal submucosa in an equine model. J Biomed Mater Res A. 2008;84:219–229. doi: 10.1002/jbm.a.31432. [DOI] [PubMed] [Google Scholar]
- 7.Bonutti PM, Seyler TM, Delanois RE, McMahon M, McCarthy JC, Mont MA. Osteonecrosis of the knee after laser or radiofrequency-assisted arthroscopy: treatment with minimally invasive knee arthroplasty. J Bone Joint Surg Am. 2006;88(suppl 3):69–75. doi: 10.2106/JBJS.F.00533. [DOI] [PubMed] [Google Scholar]
- 8.Buy X, Basile A, Bierry G, Cupelli J, Gangi A. Saline-infused bipolar radiofrequency ablation of high-risk spinal and paraspinal neoplasms. AJR Am J Roentgenol. 2006;186(5 suppl):S322–S326. doi: 10.2214/AJR.05.0265. [DOI] [PubMed] [Google Scholar]
- 9.Caffey S, McPherson E, Moore B, Hedman T, Vangsness CT., Jr Effects of radiofrequency energy on human articular cartilage: an analysis of 5 systems. Am J Sports Med. 2005;33:1035–1039. doi: 10.1177/0363546504271965. [DOI] [PubMed] [Google Scholar]
- 10.Callaghan JJ, O’Rourke MR, Liu SS. Blood management: issues and options. J Arthroplasty. 2005;20(4 suppl 2):51–54. [DOI] [PubMed]
- 11.Cardo DM, Bell DM. Bloodborne pathogen transmission in health care workers: risks and prevention strategies. Infect Dis Clin North Am. 1997;11:331–346. doi: 10.1016/S0891-5520(05)70359-7. [DOI] [PubMed] [Google Scholar]
- 12.Carrafiello G, Lagana D, Ianniello A, Nicotera P, Fontana F, Dizonno M, Cuffari S, Fugazzola C. Radiofrequency thermal ablation for pain control in patients with single painful bone metastasis from hepatocellular carcinoma. Eur J Radiol. 2009;71:363–368. doi: 10.1016/j.ejrad.2008.04.019. [DOI] [PubMed] [Google Scholar]
- 13.Cetik O, Cift H, Comert B, Cirpar M. Risk of osteonecrosis of the femoral condyle after arthroscopic chondroplasty using radiofrequency: a prospective clinical series. Knee Surg Sports Traumatol Arthrosc. 2009;17:24–29. doi: 10.1007/s00167-008-0604-0. [DOI] [PubMed] [Google Scholar]
- 14.Diab MA, Fernandez GN, Elsorafy K. Time and cost savings in arthroscopic subacromial decompression: the use of bipolar versus monopolar radiofrequency. Int Orthop. 2009;33:175–179. doi: 10.1007/s00264-008-0541-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Edwards RB, Lu Y, Cole BJ, Muir P, Markel MD. Comparison of radiofrequency treatment and mechanical debridement of fibrillated cartilage in an equine model. Vet Comp Orthop Traumatol. 2008;21:41–48. doi: 10.3415/VCOT-07-01-0004. [DOI] [PubMed] [Google Scholar]
- 16.Figueroa D, Calvo R, Vaisman A, Gallegos M, Carrasco MA, Mardones R, Delgado I. Bipolar radiofrequency in the human meniscus: comparative study between patients younger and older than 40 years of age. Knee. 2007;14:357–360. doi: 10.1016/j.knee.2007.05.006. [DOI] [PubMed] [Google Scholar]
- 17.Flory PJ, Garrett RR. Phase transitions in collagen and gelatin systems. J Am Chem Soc. 1958;80:4836–4845. doi: 10.1021/ja01551a020. [DOI] [Google Scholar]
- 18.Fry DE. Occupational risks of blood exposure in the operating room. Am Surg. 2007;73:637–646. [PubMed] [Google Scholar]
- 19.Galat DD, McGovern SC, Hanssen AD, Larson DR, Harrington JR, Clarke HD. Early return to surgery for evacuation of a postoperative hematoma after primary total knee arthroplasty. J Bone Joint Surg Am. 2008;90:2331–2336. doi: 10.2106/JBJS.G.01370. [DOI] [PubMed] [Google Scholar]
- 20.Hecht P, Hayashi K, Lu Y, Fanton GS, Thabit G, 3rd, Vanderby R, Jr, Markel MD. Monopolar radiofrequency energy effects on joint capsular tissue: potential treatment for joint instability: an in vivo mechanical, morphological, and biochemical study using an ovine model. Am J Sports Med. 1999;27:761–771. doi: 10.1177/03635465990270061301. [DOI] [PubMed] [Google Scholar]
- 21.Horstman CL, McLaughlin RM. The use of radiofrequency energy during arthroscopic surgery and its effects on intraarticular tissues. Vet Comp Orthop Traumatol. 2006;19:65–71. [PubMed] [Google Scholar]
- 22.Ishihara A, Reed SM, Rajala-Schultz PJ, Robertson JT, Bertone AL. Use of kinetic gait analysis for detection, quantification, and differentiation of hind limb lameness and spinal ataxia in horses. J Am Vet Med Assoc. 2009;234:644–651. doi: 10.2460/javma.234.5.644. [DOI] [PubMed] [Google Scholar]
- 23.Kastler B, Jacamon M, Aubry S, Barral FG, Hadjidekov G, Sarliève P, Saguet O, Lerais JM, Cadel G, Kovacs R, Boulahdour H, Pereira P. Combined bipolar radiofrequency and cementoplasty of bone metastases [in French]. J Radiol. 2007;88(9 pt 2):1242–1247. [DOI] [PubMed]
- 24.Khan SA, Thulkar S, Shivanand G, Kumar A, Varshney MK, Yadav CS, Rastogi S, Sharma DN. Computed tomography-guided radiofrequency ablation of osteoid osteomas. J Orthop Surg (Hong Kong) 2008;16:179–181. doi: 10.1177/230949900801600210. [DOI] [PubMed] [Google Scholar]
- 25.King JS, Green LM, Bianski BM, Pink MM, Jobe CM. Shaver, bipolar radiofrequency, and saline jet instruments for cutting meniscal tissue: a comparative experimental study on sheep menisci. Arthroscopy. 2005;21:844–850. doi: 10.1016/j.arthro.2005.03.018. [DOI] [PubMed] [Google Scholar]
- 26.Kondo E, Yasuda K, Kitamura N, Kudoh T, Minami A, Tohyama H. The effect of electrothermal shrinkage on the biomechanical properties of the anterior cruciate ligament: an experimental study. Arthroscopy. 2005;21:448–456. doi: 10.1016/j.arthro.2004.11.017. [DOI] [PubMed] [Google Scholar]
- 27.Kondo E, Yasuda K, Tohyama H. In vivo effects of partial electrothermal shrinkage on mechanical properties of the anterior cruciate ligament in rabbits. Clin Biomech (Bristol, Avon). 2007;22:1037–1044. [DOI] [PubMed]
- 28.Lopez MJ, Markel MD. Anterior cruciate ligament rupture after thermal treatment in a canine model. Am J Sports Med. 2003;31:164–167. doi: 10.1177/03635465030310020201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mahnken AH, Tacke JA, Wildberger JE, Günther RW. Radiofrequency ablation of osteoid osteoma: initial results with a bipolar ablation device. J Vasc Interv Radiol. 2006;17:1465–1470. doi: 10.1097/01.RVI.0000235737.22496.6A. [DOI] [PubMed] [Google Scholar]
- 30.Marulanda GA, Ulrich SD, Seyler TM, Delanois RE, Mont MA. Reductions in blood loss with a bipolar sealer in total hip arthroplasty. Expert Rev Med Devices. 2008;5:125–131. doi: 10.1586/17434440.5.2.125. [DOI] [PubMed] [Google Scholar]
- 31.Massoud SN, Levy O, de los Manteros OE, Musa F, Even T, Sinha J, Copeland SA. Histologic evaluation of the glenohumeral joint capsule after radiofrequency capsular shrinkage for atraumatic instability. J Shoulder Elbow Surg. 2007;16:163–168. doi: 10.1016/j.jse.2006.06.008. [DOI] [PubMed] [Google Scholar]
- 32.Moses VS, Hardy J, Bertone AL, Weisbrode SE. Effects of anti-inflammatory drugs on lipopolysaccharide-challenged and unchallenged equine synovial explants. Am J Vet Res. 2001;62:54–60. doi: 10.2460/ajvr.2001.62.54. [DOI] [PubMed] [Google Scholar]
- 33.Nho SJ, Freedman KB, Bansal SL, Romeo AA, Bach BR, Jr, Bush-Joseph CA, Turner DA, Cole BJ. The effect of radiofrequency energy on nonweight-bearing areas of bone following shoulder and knee arthroscopy. Orthopedics. 2005;28:392–399. doi: 10.3928/0147-7447-20050401-16. [DOI] [PubMed] [Google Scholar]
- 34.Proschek D, Mack MG, Kurth AA, Proschek P, Martin B, Hansmann ML, Vogl TJ. Radiofrequency ablation of experimental bone metastases in nude rats. Anticancer Res. 2008;28:879–885. [PubMed] [Google Scholar]
- 35.Rosenberg AG. Reducing blood loss in total joint surgery with a saline-coupled bipolar sealing technology. J Arthroplasty. 2007;22(4 suppl 1):82–85. [DOI] [PubMed]
- 36.Scheffler S, Chwastek H, Schonfelder V, Unterhauser F, Hunt P, Weiler A. The impact of radiofrequency shrinkage on the mechanical and histologic properties of the elongated anterior cruciate ligament in a sheep model. Arthroscopy. 2005;21:923–933. doi: 10.1016/j.arthro.2005.05.008. [DOI] [PubMed] [Google Scholar]
- 37.Siegel HJ, Sparks DR, Casillas MA Jr, Hong H, Dunham WH. The use of bipolar hemosealing technology in orthopaedic oncology: safety and clinical impact. Orthopedics. 2008;31(10):pii: orthosupersite.com/view.asp?rID=32078. [DOI] [PubMed]
- 38.Singh VK, Kalairajah Y. Splash in elective primary knee and hip replacement: are we adequately protected? J Bone Joint Surg Br. 2009;91:1074–1077. doi: 10.1302/0301-620X.91B8.22079. [DOI] [PubMed] [Google Scholar]
- 39.Spahn G, Kahl E, Muckley T, Hofmann GO, Klinger HM. Arthroscopic knee chondroplasty using a bipolar radiofrequency-based device compared to mechanical shaver: results of a prospective, randomized, controlled study. Knee Surg Sports Traumatol Arthrosc. 2008;16:565–573. doi: 10.1007/s00167-008-0506-1. [DOI] [PubMed] [Google Scholar]
- 40.Stulberg BN, Zadzilka JD. Blood management issues using blood management strategies. J Arthroplasty. 2007;22(4 suppl 1):95–98. [DOI] [PubMed]
- 41.Voloshin I, Morse KR, Allred CD, Bissell SA, Maloney MD, DeHaven KE. Arthroscopic evaluation of radiofrequency chondroplasty of the knee. Am J Sports Med. 2007;35:1702–1707. doi: 10.1177/0363546507304328. [DOI] [PubMed] [Google Scholar]
- 42.Wilson JW. Blood supply to developing, mature, and healing bone. In: Sumner-Smith G, ed. Bone in Clinical Orthopedics. Ed 2. Dübendorf, Germany: AO Publishing; 2002:50–51.
- 43.Wolf BR, Heiner AD, Albright JP, Nepola JV. Excessive radiofrequency application: effects on capsular tissue in an animal model. J Shoulder Elbow Surg. 2005;14:149–156. doi: 10.1016/j.jse.2004.06.009. [DOI] [PubMed] [Google Scholar]
- 44.Young B, Lowe JS, Stevens A, Heath JW. Wheater’s Functional Histology: A Text and Colour Atlas. Ed 5. Edinburgh, UK: Elsevier Ltd; 2006:193–194.
- 45.Young BD, Samii VF, Mattoon JS, Weisbrode SE, Bertone AL. Subchondral bone density and cartilage degeneration patterns in osteoarthritic metacarpal condyles of horses. Am J Vet Res. 2007;68:841–849. doi: 10.2460/ajvr.68.8.841. [DOI] [PubMed] [Google Scholar]