Abstract
Percutaneous treatment of calcaneal fractures is intended to reduce soft tissue complications and postoperative stiffness of the subtalar joint. We assessed the complications, clinical hindfoot alignment, motion, functional outcome scores, and radiographic correction of percutaneous arthroscopically assisted reduction and screw fixation of selected, less severe fractures. We performed percutaneous reduction and screw fixation in 61 patients with Type II (Sanders et al.) calcaneal fractures. In 33 of 61 patients with displaced intraarticular fractures (types IIA and IIB), anatomic reduction of the subtalar joint was confirmed arthroscopically; these patients form the basis of this report. We observed no wound complications or infections. In two patients, one prominent screw was removed after 1 and 3 years, respectively. In one patient, arthroscopic arthrolysis was performed 1 year after the index procedure. Twenty-four of 33 patients (73%) were followed a minimum of 24 months (mean, 29 months; range, 24–67 months). The average American Orthopaedic Foot and Ankle Society ankle-hindfoot score at last followup was 92.1 (range, 80–100). Böhler’s angle and calcaneal width were reduced close to the values of the uninjured side. We believe percutaneous fixation is a reasonable alternative for moderately displaced Type II fractures provided adequate control over anatomic joint reduction with either subtalar arthroscopy or high-resolution (3-D) fluoroscopy.
Level of Evidence: Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
The ideal choice of treatment for displaced intraarticular calcaneal fractures has generated controversy for more than a century [5, 18, 31, 32]. There is evidence from numerous studies with large patient cohorts that anatomic restoration of the calcaneal shape and joint congruity predict higher functional scores [2–4, 10, 29, 32, 37, 41, 46] and a lower incidence of posttraumatic subtalar arthritis with potentially less need of secondary subtalar fusion [4, 24, 29, 31, 33, 45] when treating these injuries. However, minor and major wound complications remain a major concern because of the thin and vulnerable skin over the lateral calcaneal wall, which is exposed during surgery. The reported rates of wound edge necrosis vary between 2% and 11% and those of soft tissue infections vary between 1.3% and 7% after plate fixation via an extended lateral approach [1–3, 19, 29, 46]. The cumulative rate of wound complications reportedly approaches 25% of patients, with 21% of patients having further surgery in a cohort of 190 patients [13].
Therefore, a number of authors have proposed closed reduction and minimally invasive fixation to minimize soft tissue problems in the treatment of calcaneal fractures [12, 14, 16, 30, 38, 39]. These approaches are not new. In a review compiled in 1938, C.W. Goff of Hartford, Conn., described and illustrated more than 40 different operative treatment methods for displaced calcaneal fractures, most of which included some form of percutaneous reduction and skeletal traction [18]. The method of closed reduction with percutaneous pin leverage and subsequent plaster immobilization was introduced by the German surgeon Westhues in 1934 [42, 43]. It was later modified and popularized by Gissane [17] and Essex-Lopresti [11] in the English-speaking literature. More recently, this method has been advocated for tongue-type fractures with the posterior calcaneal facet to the subtalar joint being displaced as a whole [38, 39]. Because closed reduction of intraarticular calcaneus fractures carries the risk of inaccurate restoration of the posterior facet, we supplemented percutaneous fixation with subtalar arthroscopy for intraarticular fracture patterns [16]. In 2002, we reported favorable short-term results (1 year) with an average AOFAS score of 94 in a preliminary series of 16 selected patients with less severe fractures [30].
We now report a minimum followup of 2 years on 13 of those 16 patients and an additional 20 patients subsequently treated. The purpose of this study was (1) to determine whether with select patients we could achieve anatomical percutaneous reduction combined with arthroscopic control of the posterior joint facet in displaced intraarticular calcaneal fractures; (2) to determine the rate of soft tissue complications with this minimally invasive approach; (3) to evaluate hindfoot alignment, hindfoot motion, and the functional scores [21] at medium-term followup; and (4) to assess anatomical restoration of the calcaneus with radiographic measurements.
Patients and Methods
From March 1998 to August 2006 we performed percutaneous reduction and screw fixation in 61 patients with less severe calcaneal fractures: Type II fractures as classified by Sanders et al. [33] (hereinafter referred to simply by “Type”) with one coronal fracture line at the level of the subtalar joint and moderate displacement and Grade I to II soft tissue damage as described by Tscherne and Oestern [40]. We considered the following contraindications to this specific procedure: patients younger than 16 years, patients with open fractures and Type II fractures with deep impaction of the posterior facet fragment, and polytraumatized or noncompliant patients (eg, substance abusers, patients with dementia) [31, 45]. On occasion we have also performed percutaneous reduction of calcaneal fractures in patients with more severe fracture patterns in whom open reduction and lateral plate fixation carried an excessive risk of infection, such as patients with severe neurovascular insufficiency, poorly controlled insulin-dependent diabetes mellitus, or critical soft tissue conditions [28, 45]; these patients were excluded from this series. We furthermore considered percutaneous reduction as a first-line treatment in polytraumatized or multiply injured patients with severely displaced fractures [28, 44]. However, because the patient characteristics and the treatments differed, we excluded these cases from the study. During the study period, anatomic reduction of the joint could not be achieved percutaneously in another five patients because of deep impaction of the lateral fragment, interposition of debris, or further fragmentation with manipulation. In these patients, we proceeded with open joint reduction via a direct anterolateral approach to the subtalar joint (modified Palmer approach) [25], ideally including the arthroscopic portals, and fixed with a screw or plate. These five patients were excluded from the study because they have not been treated with percutaneous reduction. Twenty-eight of the 61 patients had Type IIC (Sanders et al. [33]) fractures with the posterior facet being displaced as a whole. In 33 patients with Type IIA and IIB fractures, who had a displaced fracture of the posterior facet, the procedure was assisted arthroscopically. Mean patient age of the 33 patients at the time of surgery was 43 years (range, 22–76 years). The predominant injury mechanism was a fall from a height of 1.5 to 3 m on hard ground in 48% (16 of 33) followed by motor vehicle accidents in 36% (12 of 33). Four of the 33 patients were seen at less than 1 year and then moved away. Five of the 33 patients were lost to followup because they could not be located. This left 24 patients (three women and 21 men) with arthroscopically evaluated reductions for reevaluation at a minimum of 24 months (mean, 29 months; range, 24–67 months).
Surgery was performed within 1 to 19 days after the injury. Thirty of 33 patients were operated within 10 days after the injury. In general, surgery was scheduled as early as possible to allow for anatomical percutaneous reduction. The relatively wide range results from the time of patient referral from other hospitals.
Patients were placed in a lateral decubitus position with a tourniquet placed around the thigh. We introduced a 6.5-mm Schanz screw with T-handle via stab incision centrally into the main portion of the tongue fragment parallel to the superior border of the calcaneal body (Fig. 1). The screw was directed toward the most distal aspect of the displaced posterior facet. We mobilized the fragments and grossly reduced the tuberosity with leverage at the handle under fluoroscopic guidance. In cases of patients who were operated more than 10 days after injury, mobilization of the fragments was difficult and achieved with the percutaneous introduction of a sharp elevator into the fracture plane. In Type IIC fractures with the posterior facet being displaced as a whole, we checked restoration of the calcaneal height and correction of any varus or valgus malalignment fluoroscopically with lateral, axial, and Brodén views and followed by percutaneous screw fixation.
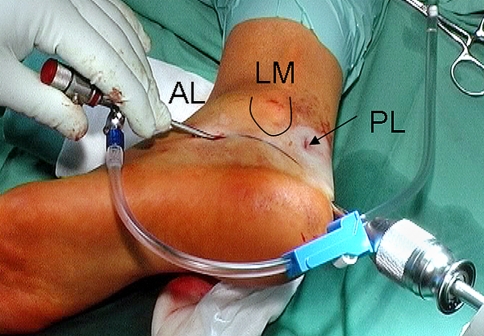
Fig. 1.
The method of percutaneous leverage with a pin introduced into the calcaneal tuberosity as first described by Westhues in 1934 and employed today together with subtalar arthroscopy. Note the arthroscope in the anterolateral portal (AL), the position of the posterolateral portal (PL) with respect to the lateral malleolus (LM) and the line of the tuberosity-joint angle drawn with skin marker.
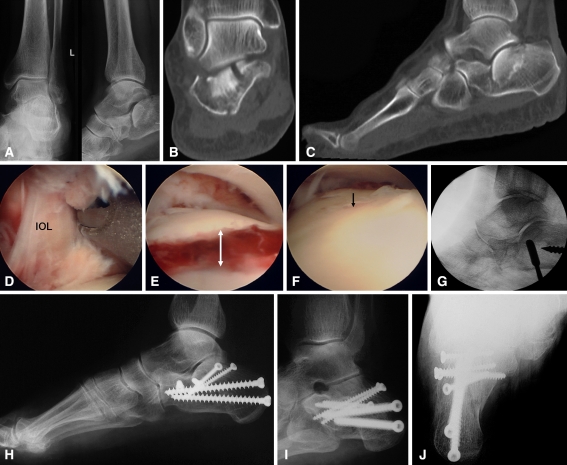
In Type IIA and IIB fractures (Fig. 2A–C), we judged the quality of the reduction of the posterior facet arthroscopically. A small-diameter ankle arthroscope (2.7 mm, 30°) was introduced into the subtalar joint via the standard anterolateral or posterolateral portal (Fig. 1) and sometimes an additional middle portal from lateral [15, 26], depending on the fracture anatomy. After irrigation, we cleared the joint and fracture of loose fragments or clots (Fig. 2D). If residual step-offs were detected arthroscopically after screw leverage (Fig. 2E), fine corrections were carried out under direct vision (Fig. 2F). We employed leverage with the Schanz screw to mobilize impacted fragments. The separate lateral posterior facet fragment was elevated and aligned percutaneously with an additional Kirschner wire, pestle, and smooth or sharp elevator (Fig. 2G). The amount of correction of the overall anatomic shape of the calcaneus was checked fluoroscopically. The fragments were fixed with 3.5- or 4.5-mm screws introduced percutaneously via stab incisions under fluoroscopic guidance (Fig. 2H). Generally, one or two screws were introduced parallel to the posterior facet into the sustentacular fragment, engaging the medial cortex to keep the lateral facet fragment in its anatomic position. Fixation of the tuberosity fragment to the anterior process fragment was carried out according to the individual fracture pattern. Anatomic reduction and screw position was checked intraoperatively with a 20° Brodén view (Fig. 2I), lateral, and axial (Fig. 2J) radiographs.
Fig. 2A–J.
(A) Radiographs, (B) coronal and (C) axial CT scans of an active 76-year-old woman show a Type IIB fracture of the right calcaneus sustained after falling from a ladder in her home. Surgery was performed 3 days after injury. Arthroscopy was employed (D) to remove minor bone fragments from the subtalar joint, (E) to assess displacement and (F) control percutaneous reduction that was achieved with the Westhues method and (G) a sharp elevator introduced percutaneously and controlled fluoroscopically. Fixation was achieved with 3.5- and 4.5-mm cancellous screws. Restoration of the calcaneal shape and adequate screw placement was controlled with intraoperative (H) lateral, (I) 20° Brodén, and (J) axial views.
Postoperatively, we applied an elastic dressing but no cast. Physical therapy was initiated the day after surgery with active and passive range-of-motion exercises at the ankle, subtalar, and midtarsal joints, as well as isotonic and isometric exercises of the lower leg. Exercises were supervised for 15 to 30 minutes and the patients were advised to continue active exercises at least two times for 30 minutes every day. They were put on continuous passive motion (CPM) for 2 hours daily. Patients were restricted to partial weightbearing of 20 kg at the affected limb in their own shoes for 6 to 8 weeks, depending on the type of fracture and bone quality.
Two of the treating surgeons (SR, MA) and one independent reviewer (SB) followed all patients at 6, 26, and 52 weeks with a clinical examination for signs of wound healing problems or infection, hindfoot range of motion and gait function tests such as toe and heel gait, squatting, jumping, etc. At last followup we used the American Orthopaedic Foot and Ankle Society (AOFAS) ankle-hindfoot scale [21] to quantify functional outcome. This score assigns a maximum of 40 points for pain, 45 for function, and 15 for alignment resulting in a total maximum of 100 points.
At 1 year and at last followup, we obtained a hindfoot alignment view [9], lateral and dorsoplantar weightbearing radiographs of both feet [45], and a 20° Brodén view [6] of the formerly injured foot. Two of us (SR, SB) assessed the following radiographic parameters at last followup to judge reduction of the calcaneal shape: Böhler’s tuberosity joint angle, heel width, and axial alignment of the hindfoot with respect to the tibia [5, 9].
Differences in complication rates, time off work, AOFAS score, and subtalar range of motion at followup between patients with Type IIA and those with Type IIB fractures were compared with Student’s t-test. Furthermore, the same parameters were compared to a historic matched cohort of 20 patients with Type II fractures that had been treated at our institution with open reduction and plate fixation via an extended lateral approach. We used SPSS for Windows (SPSS Inc. Chicago, IL) for statistical analysis.
Results
Anatomic reduction of the posterior calcaneal facet could be achieved as judged arthroscopically in 33 patients with less severe Type IIA and IIB fractures. During the same timeframe, anatomic percutaneous reduction was impossible in five patients. In three patients, surgery had been delayed more than 10 days after the injury due to late referral and fibrous union had already begun. In two patients the posterior facet fragment was deeply impacted and could not be reduced percutaneously without risking further fragmentation. In four of these five patients, open reduction was performed immediately. In one patient, open reduction was postponed because of the soft tissue swelling after percutaneous reduction attempts and arthroscopy.
We observed no patients with postoperative wound edge necrosis, hematoma, or infection. No postoperative complications related to surgery were seen, most notably compartment syndrome or any other complications attributable to subtalar arthroscopy such as fluid extravasation (Fig. 3A).
Fig. 3A–H.
Clinical photographs illustrate 3-year followup of the same patient as shown in Fig. 2. The patient here is 79 years old and has no pain or limitations during activities of daily living. She enjoys Nordic walking and smaller hikes. (A) The soft tissues have healed without complications and the sites of the stab incisions for the arthroscopic portals and screws are barely visible. A plantigrade foot with no soft tissue swelling is seen (B) clinically and (C) on pedogram. Active range of motion of the (D) hindfoot is close to the uninjured side while (E) ankle motion is normal. Weight-bearing (F) lateral and (G) axial radiographs show good hindfoot alignment despite some subsidence of the thalamic portion; (H) the Brodén view reveals a slight irregularity but no step-off in the posterior joint facet.
At last followup, the AOFAS mean ankle-hindfoot scale in the 24 patients was 92 (Table 1). All patients had a stable plantigrade foot (Fig. 3B) without signs of axial deviation or chronic swelling (Fig. 3C). Coronal hindfoot motion (eversion/inversion) averaged 42° (range, 20°–55°) on the affected side (Fig. 3D); ankle motion was the same as on the uninjured side (Fig. 3E). With the numbers available, we found no differences between patients with Type IIA and Type IIB fractures. We did not routinely remove hardware although we did so in two patients with a symptomatic prominent screw head at 1 and 3 years postoperatively. In one patient, arthroscopic arthrolysis was carried out 1 year after screw fixation because of residual pain and restricted motion at the subtalar joint. This patient received worker’s compensation and was improved with respect to both pain and function at 2 years but still complained about subfibular pain while walking on uneven ground.
Table 1.
Results of the present study compared to a historic group of patients treated with open reduction and plate fixation via an extended lateral approach at our institution
| Variable | Percutaneous reduction and screw fixation | Open reduction and plate fixation | Significance (t-test) |
|---|---|---|---|
| Number of patients | 33 | 18 | — |
| Mean age (years) | 42 (22–76) | 43 (25–68) | — |
| Wound dehiscence | 0 | 1 (5%) | N.S. |
| Deep infection | 0 | 0 | N.S. |
| Time off from work (weeks) | 11 (8–14) | 16 (11–23) | p < 0.001 |
| Followup (months) | 29 (24–67) | 23 (15–53) | N.S. |
| AOFAS score | 92 (80–100) | 88 (74–100) | N.S. |
| Böhler’s angle at followup (°) | 25 (16–35) | 26 (14–42) | N.S. |
| Coronal hindfoot range of motion (°) | 42 (20–55) | 34 (5–45) | p = 0.041 |
N.S. = not significant.
Radiographic parameters (Böhler’s angle, calcaneal width) at followup were near normal, as compared to the uninjured side in the weightbearing radiographs (Fig. 3F). No step-offs were seen in the subtalar joint (Fig. 3G) and no patient required a secondary subtalar fusion. Böhler’s angle improved from 12° (range, 0°–22°) preoperatively to 25° (range, 16°–35°) postoperatively compared to 28° (range, 22°–34°) on the uninjured side. Patients returned to work at an average of 11 weeks after the injury. Calcaneal width averaged 110% of uninjured side in the hindfoot alignment view (Fig. 3H). No discernible varus or valgus malalignment was observed.
Discussion
The development of major and minor wound complications is a major concern in the treatment of displaced intraarticular calcaneal fractures with extensile approaches [1–3, 13, 19, 29, 46]. A wide range of percutaneous treatment methods has been employed for different indications to reduce soft tissue problems associated with calcaneal fracture treatment [8, 12, 14, 22, 23, 27, 35, 36, 38, 41]. We therefore (1) determined whether with select patients one could achieve anatomical percutaneous reduction combined with arthroscopic control of the posterior joint facet in displaced intraarticular calcaneal fractures; (2) determined the rate of soft tissue complications with this minimally invasive approach; (3) evaluated hindfoot alignment, hindfoot motion, and the functional scores at medium-term followup; and (4) assessed anatomical restoration of the calcaneus with radiographic measurements.
The relatively low number of patients, the absence of a present control group, and the use of a nonvalidated outcome score [21] are limitations to our study. The number of patients is a result of careful patient selection to fully exploit the benefits of the method of percutaneous fixation without overstretching the indications to its application. For the same reason, we can only compare these patients to a historical cohort treated with open reduction and internal fixation for similar fracture patterns. We do not believe these limitations jeopardize the conclusions drawn regarding this select group because the selection led to a homogenous patient cohort treated according to a uniform protocol. For the same reason we did not include the results of patients with Type IIC fractures, ie, with the posterior facet being displaced as a whole because these patients may be treated without arthroscopic control and do generally have a favorable prognosis [30, 39]. The AOFAS ankle/hindfoot scale [21] is universally used and although not validated allows comparison to other studies and to our historic cohort.
Percutaneous reduction of displaced intraarticular calcaneal fractures was achieved as judged fluoroscopically in 61 patients with Type II fractures and moderate displacement. As has been suggested in earlier studies [28, 30], we found subtalar arthroscopy a useful tool in assessing anatomic reduction in 33 of these patients that had a displaced fracture through the posterior calcaneal facet (Types IIA and IIB). Anatomic reduction of the joint could not be achieved percutaneously in five additional patients because of deep impaction of the lateral fragment, interposition of debris, or fibrous union after late referral more than 10 days after the injury. In one of these patients, open reduction was postponed because of the soft tissue swelling after percutaneous reduction attempts and arthroscopy. Therefore, we believe one should not be overly zealous to achieve closed reduction. After three unsuccessful trials of percutaneous reduction, surgery should be converted to open reduction. In any case, patients should be made aware not only of possible conversion but also the need of a second surgery in case of severe soft tissue swelling. Because of our experience we have limited the method of percutaneous reduction to patients who are referred to us less than 10 days after the injury. We concur with Tornetta [39] that reduction is best achieved shortly after the injury and surgery should be ideally performed within 3 to 5 days. Several authors have reported on percutaneous reduction and fixation of displaced intraarticular calcaneal fractures regardless of the type of fracture. Methods include external fixation with a three-point distractor [14, 22, 23, 35], Steinmann pin, and Kirschner wire fixation [7, 8, 27, 36, 41]. Because almost all of the authors use their own followup scores, it is difficult to draw any general conclusions. Historically, Kirschner wire fixation resulted in residual articular step-offs in plain radiographs in 37% and some loss of reduction in 71% of cases [7]. These numbers could be reduced in more recent series [35, 36, 41]. Percutaneous reduction of severely displaced and more complex intraarticular calcaneal fractures (types III and IV) carries the considerable risk of residual joint incongruity with an inferior functional outcome [10, 28, 41].
We observed no wound complications and no soft tissue problems related to arthroscopy in our series. If practical, screw fixation via stab incisions reduces the risk of postoperative wound healing complications and the amount of scar formation resulting in postoperative stiffness of the subtalar joint that regularly occurs after open reduction and lateral plate fixation despite careful preparation and anatomic reduction [1, 13, 19, 29, 32, 46]. Even after percutaneous reduction, the use of external fixators or Kirschner wire fixation with the wires extruding through the skin invariably leads to pin tract infections that may develop into deep infections in up to 3.5% of cases [8, 27, 36]. Tornetta [38] changed his fixation regimen after percutaneous reduction of Type IIC fractures from Steinmann pins to screws because of complaints related to shoe wear and drainage from the pin sites in four of 17 patients.
We found percutaneous reduction and screw fixation of displaced calcaneal fractures yielded an average AOFAS score of 92/100 points in patients with Type II fractures with moderate displacement. Average hindfoot motion in the coronal plane averaged 42.7° at last followup. When comparing these outcomes to a historic group of 18 previously unreported patients treated at our institution with open reduction and internal fixation via a standard extended lateral approach for Type II calcaneal fractures, we observed no differences in AOFAS scores (Table 1). However, the patients from the percutaneous treatment group had less time off from work and a better range of hindfoot motion in the coronal plane. When using a similar method of percutaneous leverage, Tornetta [39] reported good to excellent results with the Maryland Foot Score [33] in 85% of 41 patients followed for an average of 3.4 years. His series consisted of 36 Type IIC and only five Type IIB fractures. The latter reportedly had slightly inferior results although the basis for this conclusion was not explained [39]. Our group has expanded this reduction method to Type IIA and IIB fractures with the additional use of subtalar arthroscopy to control joint reduction [16, 30] in order to reduce the risk of inadequate reduction of the posterior facet with all its potential drawbacks. As biomechanical and clinical studies have consistently shown, even minor step-offs in the joint surface of 1 to 2 mm lead to load redistribution within the posterior joint facet of the calcaneus [24, 34], inferior functional scores, and a higher rate of posttraumatic subtalar arthritis [2, 4, 10, 29, 33, 41]. In our experience, anatomic reduction cannot be achieved with percutaneous methods alone in the majority of calcaneal fractures due to the deep impaction of the posterior facet fragment into the calcaneal body, multiple fragmentation, and interposition of debris and small fragments. Over the last 10 years, approximately 10% of patients with displaced intraarticular calcaneal fractures have been treated with this method at our institution. Joint reduction should be controlled intraoperatively either with subtalar arthroscopy or with 3-D fluoroscopy in all intraarticular fractures [20].
In our series, radiographic parameters like Böhler’s angle and calcaneal width were corrected to near normal at followup indicating anatomical restoration of the calcaneal shape. Tornetta [38, 39], who used a similar method but without arthroscopy in a series of 36 Type IIC and five Type IIB fractures, reported axial alignment of the tuberosity to be restored within 10° and calcaneal width within 19% as compared to the uninjured side. Further studies have reported substantial restoration of Böhler’s and Gissane’s angles with other percutaneous reduction methods [14, 35, 36].
In summary, percutaneous treatment minimizes soft tissue complications and postoperative scar formation and therefore appears preferable to open reduction and plate fixation via an extended lateral approach in properly selected cases of mildly displaced Type II fractures. The quality of joint reduction should be visualized properly in all displaced intraarticular fractures. We do not encourage a uniform application of percutaneous reduction and fixation methods to all types of calcaneal fractures because we believe there is a considerable risk of inadequate joint reconstruction and redisplacement in fractures not filling our selection criteria.
Acknowledgments
We thank Mr. T. Albrecht, DGPh, for the clinical photographs in Figures 2 and 3.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved or waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Abidi NA, Dhawan S, Gruen GS, Vogt MT, Conti SF. Wound-healing risk factors after open reduction and internal fixation of calcaneal fractures. Foot Ankle Int. 1998;19:856–861. doi: 10.1177/107110079801901211. [DOI] [PubMed] [Google Scholar]
- 2.Benirschke SK, Sangeorzan BJ. Extensive intraarticular fractures of the foot: surgical management of calcaneal fractures. Clin Orthop Relat Res. 1993;292:128–134. [PubMed] [Google Scholar]
- 3.Bezes H, Massart P, Delvaux D, Fourquet JP, Tazi F. The operative treatment of intraarticular calcaneal fractures: indications, technique, and results in 257 cases. Clin Orthop Relat Res. 1993;290:55–59. [PubMed] [Google Scholar]
- 4.Boack DH, Wichelhaus A, Mittlmeier T, Hoffmann R, Haas NP. Therapy of dislocated calcaneus joint fracture with the AO calcaneus plate [in German] Chirurg. 1998;69:1214–1223. doi: 10.1007/s001040050559. [DOI] [PubMed] [Google Scholar]
- 5.Böhler L. Behandlung der Fersenbeinbrüche. Arch Klin Chir. 1929;157:723–732. [PubMed] [Google Scholar]
- 6.Brodén B. Roentgen examination of the subtaloid joint in fractures of the calcaneus. Acta Radiol. 1949;31:85–88. doi: 10.3109/00016924909136638. [DOI] [PubMed] [Google Scholar]
- 7.Buch J. Bohrdrahtosteosynthese des Fersenbeinbruches. Akt Chir. 1980;15:285–296. [Google Scholar]
- 8.Buch J, Blauensteiner W, Scherafati T, Vischer HM, Fischer W. Conservative treatment of calcaneus fracture versus repositioning and percutaneous bore wire fixation. A comparison of 2 methods [in German] Unfallchirurg. 1989;92:595–603. [PubMed] [Google Scholar]
- 9.Cobey JC. Posterior roentgenogram of the foot. Clin Orthop Relat Res. 1976;118:202–207. [PubMed] [Google Scholar]
- 10.Crosby LA, Fitzgibbons T. Intraarticular calcaneal fractures: results of closed treatment. Clin Orthop Relat Res. 1993;290:47–54. [PubMed] [Google Scholar]
- 11.Essex-Lopresti P. The mechanism, reduction technique, and results in fractures of the os calcis. Br J Surg. 1952;39:395–419. doi: 10.1002/bjs.18003915704. [DOI] [PubMed] [Google Scholar]
- 12.Fernandez DL, Koella C. Combined percutaneous and “minimal” internal fixation for displaced articular fractures of the calcaneus. Clin Orthop Relat Res. 1993;290:108–116. [PubMed] [Google Scholar]
- 13.Folk JW, Starr AJ, Early JS. Early wound complications of operative treatment of calcaneus fractures: analysis of 190 fractures. J Orthop Trauma. 1999;13:369–372. doi: 10.1097/00005131-199906000-00008. [DOI] [PubMed] [Google Scholar]
- 14.Forgon M, Zadravecz G. Closed reduction and percutaneous osteosynthesis: technique and results in 265 calcaneal fractures. In: Tscherne H, Schatzker J, eds. Major Fractures of the Pilon, the Talus and the Calcaneus. Berlin, Germany: Springer Verlag; 1993:207–213.
- 15.Frey C, Gasser S, Feder K. Arthroscopy of the subtalar joint. Foot Ankle Int. 1994;15:424–428. doi: 10.1177/107110079401500804. [DOI] [PubMed] [Google Scholar]
- 16.Gavlik JM, Rammelt S, Zwipp H. Percutaneous, arthroscopically-assisted osteosynthesis of calcaneus fractures. Arch Orthop Trauma Surg. 2002;122:424–428. doi: 10.1007/s00402-002-0397-4. [DOI] [PubMed] [Google Scholar]
- 17.Gissane W. News notes: Proceedings of the British Orthopedic Association. J Bone Joint Surg Am. 1947;29:254–258. [Google Scholar]
- 18.Goff CW. Fresh fracture of the os calcis. Arch Surg. 1938;36:744–765. [Google Scholar]
- 19.Harvey EJ, Grujic L, Early JS, Benirschke SK, Sangeorzan BJ. Morbidity associated with ORIF of intra-articular calcaneus fractures using a lateral approach. Foot Ankle Int. 2001;22:868–873. doi: 10.1177/107110070102201102. [DOI] [PubMed] [Google Scholar]
- 20.Kendoff D, Citak M, Gardner M, Kfuri M, Jr, Thumes B, Krettek C, Hüfner T. Three-dimensional fluoroscopy for evaluation of articular reduction and screw placement in calcaneal fractures. Foot Ankle Int. 2007;28:1165–1171. doi: 10.3113/FAI.2007.1165. [DOI] [PubMed] [Google Scholar]
- 21.Kitaoka H, Alexander I, Adelaar R, Nunley J, Myerson M, Sanders M. Clinical rating systems for the ankle, hindfoot, midfoot, hallux and lesser toes. Foot Ankle Int. 1994;15:349–353. doi: 10.1177/107110079401500701. [DOI] [PubMed] [Google Scholar]
- 22.Magnan B, Bortolazzi R, Marangon A, Marino M, Dall’Oca C, Bartolozzi P. External fixation for displaced intra-articular fractures of the calcaneum. J Bone Joint Surg Br. 2006;88:1474–1479. doi: 10.2106/JBJS.E.00897. [DOI] [PubMed] [Google Scholar]
- 23.McGarvey WC, Burris MW, Clanton TO, Melissinos EG. Calcaneal fractures: indirect reduction and external fixation. Foot Ankle Int. 2006;27:494–499. doi: 10.1177/107110070602700703. [DOI] [PubMed] [Google Scholar]
- 24.Mulcahy DM, McCormack DM, Stephens MM. Intra-articular calcaneal fractures: effect of open reduction and internal fixation on the contact characteristics of the subtalar joint. Foot Ankle Int. 1998;19:842–848. doi: 10.1177/107110079801901209. [DOI] [PubMed] [Google Scholar]
- 25.Palmer I. The mechanism and treatment of fractures of the calcaneus. J Bone Joint Surg Am. 1948;30:2–8. [PubMed] [Google Scholar]
- 26.Parisien JS, Vangsness T. Arthroscopy of the subtalar joint: an experimental approach. Arthroscopy. 1985;1:53–57. doi: 10.1016/s0749-8063(85)80079-7. [DOI] [PubMed] [Google Scholar]
- 27.Poigenfürst J, Buch J. Treatment of severe fractures of the calcaneus with repositioning and percutaneous wire fixation [in German] Unfallchirurg. 1988;91:493–501. [PubMed] [Google Scholar]
- 28.Rammelt S, Amlang M, Barthel S, Zwipp H. Minimally-invasive treatment of calcaneal fractures. Injury. 2004;35(Suppl 2):SB55–SB63. doi: 10.1016/j.injury.2004.07.012. [DOI] [PubMed] [Google Scholar]
- 29.Rammelt S, Barthel S, Biewener A, Gavlik JM, Zwipp H. Calcaneus fractures: open reduction and internal fixation [in German] Zbl Chir. 2003;128:517–528. doi: 10.1055/s-2003-40627. [DOI] [PubMed] [Google Scholar]
- 30.Rammelt S, Gavlik JM, Barthel S, Zwipp H. The value of subtalar arthroscopy in the management of intra-articular calcaneus fractures. Foot Ankle Int. 2002;23:906–916. doi: 10.1177/107110070202301004. [DOI] [PubMed] [Google Scholar]
- 31.Rammelt S, Zwipp H. Calcaneus fractures: facts, controversies and recent developments. Injury. 2004;35:443–461. doi: 10.1016/j.injury.2003.10.006. [DOI] [PubMed] [Google Scholar]
- 32.Sanders R. Displaced intra-articular fractures of the calcaneus. J Bone Joint Surg Am. 2000;82:225–250. doi: 10.2106/00004623-200002000-00009. [DOI] [PubMed] [Google Scholar]
- 33.Sanders R, Fortin P, DiPasquale T, Walling A. Operative treatment in 120 displaced intraarticular calcaneal fractures: results using a prognostic computed tomography scan classification. Clin Orthop Relat Res. 1993;290:87–95. [PubMed] [Google Scholar]
- 34.Sangeorzan BJ, Ananthakrishnan D, Tencer AF. Contact characteristics of the subtalar joint after a simulated calcaneus fracture. J Orthop Trauma. 1995;9:251–258. doi: 10.1097/00005131-199506000-00012. [DOI] [PubMed] [Google Scholar]
- 35.Schepers T, Vogels LM, Schipper IB, Patka P. Percutaneous reduction and fixation of intraarticular calcaneal fractures. Oper Orthop Traumatol. 2008;20:168–175. doi: 10.1007/s00064-008-1239-5. [DOI] [PubMed] [Google Scholar]
- 36.Stulik J, Stehlik J, Rysavy M, Wozniak A. Minimally-invasive treatment of intra-articular fractures of the calcaneum. J Bone Joint Surg Br. 2006;88:1634–1641. doi: 10.1302/0301-620X.88B12.17379. [DOI] [PubMed] [Google Scholar]
- 37.Thordarson DB, Krieger LE. Operative vs. nonoperative treatment of intra-articular fractures of the calcaneus: a prospective randomized trial. Foot Ankle Int. 1996;17:2–9. doi: 10.1177/107110079601700102. [DOI] [PubMed] [Google Scholar]
- 38.Tornetta P., III The Essex-Lopresti reduction for calcaneal fractures revisited. J Orthop Trauma. 1998;12:469–473. doi: 10.1097/00005131-199809000-00007. [DOI] [PubMed] [Google Scholar]
- 39.Tornetta P., III Percutaneous treatment of calcaneal fractures. Clin Orthop Relat Res. 2000;375:91–96. doi: 10.1097/00003086-200006000-00011. [DOI] [PubMed] [Google Scholar]
- 40.Tscherne H, Oestern HJ. A new classification of soft-tissue damage in open and closed fractures [in German] Unfallheilkunde. 1982;85:111–115. [PubMed] [Google Scholar]
- 41.Walde TA, Sauer B, Degreif J, Walde HJ. Closed reduction and percutaneous Kirschner wire fixation for the treatment of dislocated calcaneal fractures: surgical technique, complications, clinical and radiological results after 2–10 years. Arch Orthop Trauma Surg. 2008;128:585–591. doi: 10.1007/s00402-008-0590-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Westhues H. Eine neue Behandlungsmethode der Calcaneusfrakturen. Arch Orthop Unfallchir. 1934;35:121. doi: 10.1007/BF02581879. [DOI] [Google Scholar]
- 43.Westhues H. Eine neue Behandlungsmethode der Calcaneusfrakturen: Zugleich ein Vorschlag zur Behandlung der Talusfrakturen. Zentralbl Chir. 1935;35:995–1002. [Google Scholar]
- 44.Zwipp H. Chirurgie des Fußes. Wien, Austria: Springer; 1994. [Google Scholar]
- 45.Zwipp H, Rammelt S, Barthel S. Calcaneal fractures—open reduction and internal fixation (ORIF) Injury. 2004;35(Suppl 2):SB46–SB54. doi: 10.1016/j.injury.2004.07.011. [DOI] [PubMed] [Google Scholar]
- 46.Zwipp H, Tscherne H, Thermann H, Weber T. Osteosynthesis of displaced intraarticular fractures of the calcaneus: results in 123 cases. Clin Orthop Relat Res. 1993;290:76–86. [PubMed] [Google Scholar]