Abstract
Distal tibial fractures are difficult to manage. Limited soft tissue and poor vascularity impose limitations for traditional plating techniques that require large exposures. The nature of the limitations for traditional plating techniques is intrinsic to the large exposure required to approach distal tibia, a bone characterized by limited soft tissue coverage and poor vascularity. The locking plate (LP) is a new device for treatment of fractures. We assessed the bone union rate, deformity, leg-length discrepancy, ankle range of motion, return to preinjury activities, infection, and complication rate in 21 selected patients who underwent minimally invasive osteosynthesis of closed distal tibia fractures with an LP. According to the AO classification, there were 12 Type A, 5 Type B, and 4 Type C fractures. The minimum followup was 2 years (average, 2.8 years; range, 2–4 years). Two patients were lost to followup. Union was achieved in all but one patient by the 24th postoperative week. Four patients had angular deformity less than 7°. No patient had a leg-length discrepancy more than 1.1 cm. Five patients had ankle range of motion less than 20° compared with the contralateral side. Sixteen patients had not returned to their preinjury sporting or leisure activities. Three patients developed a delayed infection. We judge the LP a reasonable device for treating distal tibia fractures. The level of physical activities appears permanently reduced in most patients.
Level of Evidence: Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Fractures of the distal tibia can be challenging to treat because of the limited soft tissue, the subcutaneous location, and poor vascularity. The best treatment remains controversial. Nonsurgical treatment is possible for stable fractures with minimal shortening, but malunion, shortening of affected leg, limitation of range of motion, and early osteoarthritis of the ankle have all been reported following treatment of these fractures particularly pilon fractures [36, 40]. Surgical fixation of distal tibia fractures can be difficult, and requires careful preoperative planning. Fracture pattern, soft tissue injury, and bone quality critically influence the selection of fixation technique [2]. Several surgical methods have been described, including external fixation, intramedullary nailing, and plate fixation. External fixation can be useful in open fractures with soft tissue injury which preclude nail or plate fixation, but may result in inaccurate reduction [1, 4], a relatively high rate of malunion (range, 5%–25%) [8, 47] or nonunion (range, 2%–17.6%) [1, 32], and pin tract infection (range, 10%–100%) [4, 47]. In diaphyseal fractures of the tibia, intramedullary nailing allows relatively atraumatic closed stabilization. It preserves the vascularity of the fracture site and integrity of the soft tissue envelope [3]. However, stable intramedullary nailing of the distal tibia may be difficult to achieve because the hourglass shape of the intramedullary canal prevents a tight endosteal fit and compromises torsional and angular stability [9]. Secondary displacement of the fracture on insertion of the nail, breakage of nails and locking screws (range, 5%–59%) [28], and malunion of the tibia (range, 0–29%) [10, 34] are potential risks. Classic open reduction and internal plate fixation require extensive soft tissue dissection and periosteal stripping even in expert hands, with high rates of complications, including infection (range, 8.3%–23%) [24, 26] and delayed union and nonunions (range, 8.3%–35%) [6, 24, 26, 46, 48]. Several minimally invasive plate osteosynthesis techniques have been developed, with union rates ranging between 80% and 100% [14, 21, 31, 44]. These techniques aim to reduce surgical trauma and to maintain a more biologically favorable environment for fracture healing. Nevertheless, complications, such as angular deformities greater than 7° (range, 7.1%–35%) [31, 46], hardware failure (range, 0–10%) [27, 31], and nonunions (range, 0–20%) [14, 21] have been reported.
A new advance in this field is represented by the “locked internal fixators.” These devices consist of plate-and-screw systems where the screws are locked in the plate at a fixed angle. Screw locking minimizes the compressive forces exerted by the plate on the bone because the plate does not need to be tightly pressed against the bone to stabilize the fracture. The claim of minimizing disturbance of the bone blood supply [13, 16, 17, 37] will require future confirmation. The system works as flexible elastic fixation that putatively stimulates callus formation. The anatomical shape prevents primary displacement of the fracture caused by inexact contouring of a normal plate, and allows a better distribution of the angular and axial loading around the plate [16, 17]. These biomechanical advantages as contrasted to other approaches have not been confirmed in clinical followup studies.
We therefore assessed the union rate, deformity, leg-length discrepancy, gait and ankle range of motion, return to preinjury daily and sports activities, and infections and other complications. We compared our results with those reported by other authors using the same technique to evaluate whether the LCP is a suitable device for surgical management of distal tibia fractures.
Patients and Methods
We retrospectively analyzed prospectively collected data on 21 adult patients with closed distal tibia and fibula fractures without previous or present ipsilateral leg fracture treated from 2003 to 2006. We excluded patients with pathological fractures, lower limbs with preexisting neurological deficit, autoimmune disease, or vascular disease. Five patients sustained their fracture as a result of a fall, 10 in a motor vehicle accident, and six during sports activities (three soccer, one rugby, one running, one mountain biking). Seven patients were smokers. None had a polytrauma or an open fracture. Depending on the skin condition, surgery was planned when the ankle swelling subsided, and the “wrinkle sign” was present. In the wrinkle sign, the ankle is dorsiflexed while the anterior aspect of the ankle is observed; the absence of a skin crease or wrinkle suggests severe swelling [45]. The time between trauma and surgery was 6.5 ± 4.3 days (range, 5–14 days). There were nine women and 12 men, ranging in age from 25 to 66 years (mean age for all patients, 43 ± 7 years; mean age, men, 42 ± 12 years, age range, men, 26–66 years; mean age, women, 44 ± 7 years, range, women, 25–65 years). In all patients, the distal tibia was affected. In 17 of 21 patients, the fibula was fractured as well. The minimum followup was 2 years (average, 2.8; range, 2–4 years) after surgery. Two patients were lost to final followup, but their fracture was clinically and radiographically healed at 9 months, and they had returned to their work. They had not returned to their leisure activities. These two patients were not included in the final evaluation, leaving 19 patients for evaluation. All the procedures described in this investigation were approved by our local ethics committee. All the patients gave written informed consent to be included in the present study.
All patients had plain radiographs. We obtained CT scans in 9 patients with extension of the fracture to the joint. All the fractures were evaluated by the surgeon (NM) and classified according to the AO comprehensive classification system [35]. The AO classification arose from efforts to produce a comprehensive system for fractures of the long bones. The distal segment of the tibia is classified as ‘43’ and divided into three types as follows: Type A, extraarticular fractures; Type B, partial articular fractures, which maintain some continuity between the shaft and the articular surface; and Type C, complete articular fractures. There were 12 AO 43A fractures, 5 AO 43B fractures, and 4 AO 43C fractures.
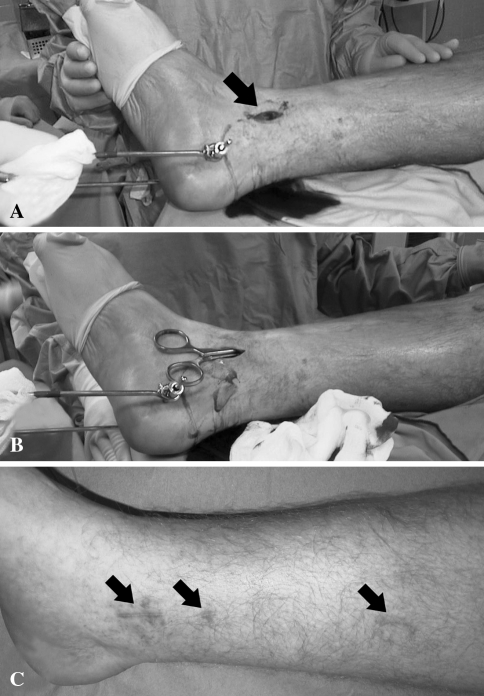
Immediate skeletal stabilization was achieved by splints with an above-knee back slab or a spanning external fixator in nine instances. All procedures were performed by a single surgeon (NM) with a special interest in these techniques using a previously described approach [41]. Briefly, with the patient supine on a radiolucent table, antibiotic prophylaxis was administered (cefuroxime, 1.5 g intravenously) and standard intraoperative fluoroscopy used throughout the procedure. Both the injured and the noninjured limb were prepped and draped above the knee, thus allowing intraoperative alignment to be checked against the normal limb. The joint line of both the knee and the ankle was identified with fluoroscopy control and marked on the skin. Using manual traction at the ankle or through a single Steinmann pin inserted into the calcaneus, the fracture was gently reduced, restoring limb length, alignment, and rotation (Fig. 1A). Most often, we internally fixed the tibial fracture first when a fibular fracture was present. However, if normal length, axis, and rotation of the tibial fracture were not achieved, a fibula fracture, if present, was plated first using a one-third tubular plate to provide lateral stability, restore the correct length, and avoid overdistraction at the tibial fracture site. Thus, in two patients we first stabilized the fibula using a one-third tubular plate. In seven patients, accurate reduction and stable fixation of the fibular fracture was achieved after tibial fixation using a minimally invasive approach. In the five patients in whom reduction and/or stable fixation of the fibula was not possible using a minimally invasive approach, we converted the fixation of the fibular fracture to an open method. In the other three patients in whom the fibula was fractured, this was internally fixed after minimally invasive fixation of the tibial fracture having planned an open approach from the start. The main fracture fragments of the distal tibia were aligned and reduced percutaneously or through separate stab incisions using a periosteal elevator, clamps, or Kirschner wires as joysticks, and then fixed with individual lag screws. In the four patients with fractures with intraarticular extension in whom we thought that a combined approach would have been helpful, we performed arthroscopy through conventional anteromedial and anterolateral portals to assess the reduction of the articular surface and to address any associated joint lesions. At arthroscopy, we found loose bodies or chondral defects in three of these patients. The loose bodies were removed, and the chondral defects were débrided. A transverse incision about 1 cm distal to the medial malleolus was performed in 13 patients. The transverse incision remained in the superficial subcutaneous layers, and did not penetrate the sheath of the tendon of tibialis posterior. In the remaining eight patients, we used a longitudinal incision over the medial malleolus. A subcutaneous tunnel was produced using forceps (Fig. 1B) or a periosteum elevator. Following appropriate reduction of the fracture, a locking compression plate-distal tibial plate (LCP-DTP, Synthes, Stratec Medical, Oberdorf, Switzerland) is inserted to bridge the fracture site. We chose a plate long enough to bridge the metaphyseal zone and allow the insertion of at least two bicortical screws insertions proximal to the fracture. More than two screws in each fracture fragment may cause increased stress at the plate for small bridging lengths and small fracture gap sizes [43]. On the other hand, additional screws increase the implant stress since higher loads are needed to achieve bone contact in tibial fractures [43].
Fig. 1A–C.
(A) A calcaneal Steinmann pin is applied to reduce the fracture and to maintain the length and alignment of the limb. Small longitudinal incision is distal to the medial malleolus (arrow). (B) Through the small incision, the subcutaneous tunnel is created using an artery forceps. (C) Final scars (arrows) show the minimal nature of the exposure.
Distal to the metaphyseal fracture, we inserted bicortical or unicortical screws using as many of the distal plate holes as possible (maximum, nine holes). We used Kirschner wires to secure, through holes of the plate, the latter to the bone before screw insertion. At this stage, we assessed limb alignment by comparison with the other limb. We established the correct rotation evaluating the alignment of the proximal and distal cortices of the distal tibia and comparing at 90° of knee flexion the axis between the tibial tuberosity and the intermetatarsal spaces. Screws were then inserted percutaneously through stab wounds as necessary. The ratio between screws inserted and holes used was 0.65 (range, 0.6–0.8). The screening radiation time was 81.3 ± 33.4 seconds (range, 41–118 seconds). The stab incisions were irrigated and closed with routine skin sutures, the wound dressed. The mean hospital stay was 11.4 days (range, 6–22 days).
All limbs were immobilized in a below-knee synthetic cast for 6 weeks. The patients who had previous external fixation received two other doses of prophylactic antibiotics (cefuroxime, 1.5 g intravenously), one 8 hours and another 16 hours after the dose at induction. We did not routinely use postoperative venous thromboembolism prevention, except for the two patients who were already on anticoagulant drugs for underlying comorbidities. We instituted non-weight bearing crutch walking while still in hospital, following recovery from the anesthesia. At 2 weeks, we changed the below-knee synthetic cast to another short-leg lightweight cast after inspection of the wound and removal of the sutures (Fig. 1C). The weight-bearing status was dependent on the individual fracture pattern, but most patients could at least partially weight bear at 6 weeks. If the fracture was intraarticular, we kept the patients non-weight bearing for the first 2 weeks, and asked them to start toe-touch weight bearing starting from the 4th postoperative week. Outpatient physiotherapy was instituted to maximize the range of motion of the foot and ankle immediately after definitive removal of the cast.
We scheduled clinical, functional, and radiographic (plain anteroposterior and lateral radiographs) evaluations at 6, 12, 24 weeks, 1 year from the index procedure, and then annually. All the evaluations were performed by the surgeon. The functional outcomes were based on four parameters: substantial limp, range of motion of the ankle, inactivity (unemployment because of the leg injury or inability to return to daily activities because of the leg injury), infection, and complication rate. We defined a late skin infection as one that occurred at least 2 months after complete wound healing.
We evaluated three radiographic parameters: union (bridging of at least three of four cortices on two orthogonal views), deformity (< 7°), and leg-length discrepancy (< 2.5 cm in the tibia) on standard long-leg radiographs. We considered a healing time less than 6 months normal and between 6 and 9 months as a delayed union. Fractures not healed within 9 months were considered a nonunion according to the 1988 FDA guidance document definition for tibial fracture, requiring 9 months duration of the nonunited fracture with no evidence of progressive healing over the previous 3 months [15, 18].
Results
Union was achieved in all but one of the 21 patients by the 24th postoperative week, with one patient being classified as a nonunion (Figs. 2A–D and 3A–B) (Table 1). The one patient with a nonunion is still undergoing nonoperative treatment, as he does not wish to undergo a further operation. Four patients (21%) had angular deformities, all less than 7°: one patient had a valgus deformity; three patients had a varus deformity, and two of these four patients had anterior bowing (6° and 7° respectively) of the tibia at the fracture site. No patient had a leg-length discrepancy greater than 1.1 cm.
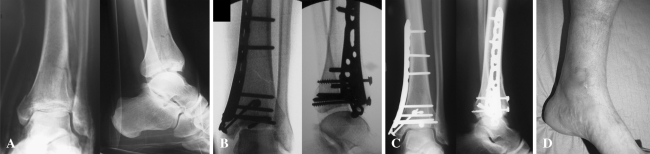
Fig. 2A–D.
(A) AO 43 B fracture, (B) postoperative radiographs, (C) 6-month followup, and (D) clinical appearance after 6 months are shown. The patient is fully weight bearing with no walking aids and no limp. Note the well-healed, barely visible scars.
Fig. 3A–B.
(A) AO 43 C fracture and (B) plain radiographs after 1 year are shown. The fracture united with no limb shortening and the patient reports no use of walking aids and no limp.
Table 1.
Overall results according bone and functional parameters
| Variable | Number of patients |
|---|---|
| Bone results | |
| Union | 18/19 (95%) |
| Angular deformities < 7° | 4/19 (21%) |
| Leg-length discrepancy > 1.1 cm | 0/19 (0%) |
| Functional results | |
| Limp | 8/19 (42%) |
| Range of motion of ankle > 20° | 5/19 (26%) |
| Return to preinjury activities | 3/19 (16%) |
| Deep infection | 3/19 (16%) |
At the last followup, eight of the 19 patients (excluding the two lost to followup) had a limp, but none of them used walking aids. The range of motion of the ankle was reduced more than 20° compared with the contralateral side in five patients. In six patients, the plate was palpable in the subcutaneous tissues at the time of the latest clinic visit, but did not produce any discomfort that interfered with the patients’ daily activities. Sixteen of the 19 patients had not returned to their preinjury sporting or leisure activities.
The wounds healed without further wound problems in 12 of the 21 patients (Fig. 1C). Three patients developed a late infection around the proximal or distal screws 13, 15, and 17 weeks, respectively, after the index operation. None of these three infections resolved with local wound care and 6 weeks of oral antibiotics and we therefore removed the tibial locked plate at 6, 7, and 8 months, respectively, from the original operation. Two of these three patients had undergone transient external fixation for less than 10 days before definitive fixation. Six patients experienced minor wound dehiscence or superficial cellulitis within 3 months of the index operation, and were treated with local wound care and oral antibiotics (500 mg of flucloxacyllin four times a day for 7 days); the wound problems resolved in all six patients. One female patient developed complex regional pain syndrome that was managed with intensive rehabilitation and resolved after 9 months. Four patients (21%) reported deep venous thrombosis between 4 and 6 weeks after surgery, and were managed with oral anticoagulants for 3 months with no adverse effects. There were no complications related to the arthroscopic approach.
Discussion
The treatment of distal tibia fractures can be challenging because of the limited soft tissue, the subcutaneous location of the bone, and poor vascularity. Minimally invasive plating techniques reduce iatrogenic soft tissue injury and damage to bone vascularity, as well as preserve the osteogenic fracture hematoma [11, 12]. Initial clinical series using these methods demonstrated favorable results with low rates of infection and nonunion [7, 21, 31, 39], but several complications such as angular deformities greater than 7° and hardware failure have been reported [14, 21, 31]. Locking plates have been developed to overcome these limits. We therefore evaluated a selected group of patients with closed distal tibia fracture, the bone union rate, deformity, leg-length discrepancy, range of motion of the ankle, return to preinjury daily and sports activities, and infection or other complications rate after locking plating.
Our study presents several limitations. First, the relatively small number of patients and the lack of a control group do not allow the formulation of definitive statements and guidelines. As closed distal tibial fractures are uncommon, it would be difficult for a single hospital to collect a large enough number of patients to perform a randomized study. Several authors using locking tibial plates reported, in series of between 20 and 48 patients, a percentage of open fracture of 19% to 40% [7, 19–21, 29]. Second, our cohort involves both intraarticular and extraarticular fractures, all managed in a standard fashion. Unfortunately, the numbers involved are too small to allow meaningful subcohort comparisons.
We used distal tibial locking plates (LCP-DTP) instead of metaphyseal locking plates (LCP-MP) because LCP-DTP afford better control strain during neutral (decreased 39%–47% versus 6.4%–41.5%), flexion (increased 0.2%–18% versus 34%–109%), and extension (increased 13%–21% versus 25%–60%) moments [42]. Also, the LCP-DTP has greater versatility to insert distal screws, with has nine distal holes instead of the four holes of the LCP-MP, allowing more precise modulation of the rigidity of fixation [42]. Borg et al. reported as a limitation of the conventional low contact plate the number of screws that can be placed in a short distal fragment [5].
The percentage of union, delayed union, and nonunion is comparable to studies that included only patients with closed fracture [5, 39]. Three preliminary retrospective studies using an LCP-DTP to manage closed and open distal tibia fractures reported a union rate similar to our study (range, 90%–100%) (Table 2) [7, 19, 20]. However, two of these three studies reported several supplementary procedures (range, 2–9 procedures) performed to obtain union.
Table 2.
Clinical series of distal tibia fractures treated with percutaneous LCP-DTP
| Study | Frature type | Open fracture | Outcome | Deep infections |
|---|---|---|---|---|
| Collinge et al. [7] | 26 distal tibia | 14 | 26 union in 35 weeks (range, 12–112); 9 required supplementary procedures; no deformity ≥ 5° or shortening ≥ 1 cm; 1 implant failure | 2 (1 in closed fracture) |
| Hasenboehler et al. [19] | 32 diaphyseal and distal tibial fracture | 8 | 29 union in 27.7 weeks (range, 24–60); 2 nonunion; no deformity ≥ 5° or shortening ≥ 1 cm; 1 plate bending (18°) | 1 |
| Hazarika et al. [20] | 20 distal tibia | 8 | 18 union in 28.5 weeks (range, 9–68); 2 required supplementary procedures; 2 nonunion; 1 implant failure | 2 (closed fractures) |
| Ronga et al. [current study] | 19 distal tibia | 0 | 18 union in 22.3 weeks (range, 12–24); no deformity ≥ 7° or shortening ≥ 1.1 cm | 3 |
No patients had angular deformities greater than 7° or leg discrepancy greater than 1.1 cm, although we acknowledge that two of four patients each had deformities in two planes. This result can be attributed to the experience of the surgeon, to the contour of the anatomic plate, and to the fixed angle stability of the holes. These findings are comparable to other studies using an LCP-DTP (Table 2) [7, 19, 20]. Before fixing the plate, given the possibility of a discrepancy between the anatomical axis of the tibia and the contour of the plate, we assessed limb alignment by comparison with the other limb. Then we inserted Kirschner wires through the holes of the plate to secure the latter to the bone before screw insertion. The fixed angle stability of the holes avoids the need of tightly pressing the plate against the bone to stabilize the fracture. This prevents primary dislocation of the fracture caused by inexact contouring of a plate. In a previous study, the same surgeon (NM), using a dynamic compression plate precontoured before undertaking the procedure, reported that seven of 20 patients (35%) had angular deformities greater than 7° [31]. The design of the implant is also important. The LC-DCP has a better fatigue resistance than earlier AO plates [38]. These mechanical properties of the LC-DCP may be the reason why no plates broke in this series compared to previous studies (2.7%–10% of the plates) [14, 31, 46]. However, in the other three studies using an LCP-DTP there were two cases of plate breakage and one case of plate bending. One of the two plate failures involved a man with diabetic neuropathy and questionable compliance whose plate broke 4 months after injury while excessive weight bearing determined the plate bending of more than 18° [7, 19].
Five patients (26%) experienced restriction in ankle motion greater than 20° and 16 patients (84%) had not returned to their preinjury sporting or leisure activities. We cannot be certain that no problems related to ankle osteoarthritis will arise in the future in patients with intraarticular involvement who reported satisfactory functional and radiographic results. However, Collinge et al. reported the only variable that influenced functional outcomes was the occurrence of a secondary surgery (34% of patients), which was associated with poorer function results [7]. Associated lower-extremity fracture, other injuries, intraarticular extension, bone loss, open fracture, or the time to union were not associated with poorer function on limb-specific assessments.
We identified late infections in three patients. This complication was also observed by other authors using the same plates, and was attributed to the possible plate prominence in the distal region of the tibia rather than to open fractures (Table 2) [7, 19, 20]. In our patients, bone healing was not affected by the infection. The resistance to superficial infection and good bony union rate may be due to the preservation of bony vascularity with the use of the minimally invasive technique [29].
The arthroscopic approach allows visualization of the reduction of the articular surface, to assess and to treat any joint lesions. Several authors reported an incidence of intraarticular pathology in ankle fractures ranging between 63% and 79.2% [22, 30]. Based on the minimal added time and morbidity to the surgical procedure, we use arthroscopy on a regular basis in intraarticular fractures [23, 25, 33].
Given the small numbers of patients in our study, we cannot draw any definitive conclusions. The high percentage of unions and the low rate of complications, comparable to previous studies using the same plates, suggest the LCP-DTP may be a reasonable alternative for treating distal tibia fractures. The cost of the locking plates, the technically demanding nature of the procedure, and the increased exposure to radiation during the procedure should be considered when comparing the efficacy of this device to the normal plates. Only future prospective randomized studies may be able to clarify these issues.
Acknowledgments
We thank Stefano Turino, MD, for his assistance in preparing the pictures.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution has approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at Centre for Sports and Exercise Medicine, Barts and The London School of Medicine and Dentistry, Mile End Hospital—275 Bancroft Road, London E1 4DG, United Kingdom.
References
- 1.Anglen JO. Early outcome of hybrid external fixation for fracture of the distal tibia. J Orthop Trauma. 1999;13:92–97. doi: 10.1097/00005131-199902000-00004. [DOI] [PubMed] [Google Scholar]
- 2.Bedi A, Le TT, Karunakar MA. Surgical treatment of nonarticular distal tibia fractures. J Am Acad Orthop Surg. 2006;14:406–416. doi: 10.5435/00124635-200607000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Blachut PA, O’Brien PJ, Meek RN, Broekhuyse HM. Interlocking intramedullary nailing with and without reaming for the treatment of closed fractures of the tibial shaft. A prospective, randomized study. J Bone Joint Surg Am. 1997;79:640–646. doi: 10.2106/00004623-199705000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Bone L, Stegemann P, McNamara K, Seibel R. External fixation of severely comminuted and open tibial pilon fractures. Clin Orthop Relat Res. 1993;292:101–107. [PubMed] [Google Scholar]
- 5.Borg T, Larsson S, Lindsjo U. Percutaneous plating of distal tibial fractures. Preliminary results in 21 patients. Injury. 2004;35:608–614. doi: 10.1016/j.injury.2003.08.015. [DOI] [PubMed] [Google Scholar]
- 6.Bourne RB. Pylon fractures of the distal tibia. Clin Orthop Relat Res. 1989;240:42–46. [PubMed] [Google Scholar]
- 7.Collinge C, Sanders R, DiPasquale T. Treatment of complex tibial periarticular fractures using percutaneous techniques. Clin Orthop Relat Res. 2000;375:69–77. doi: 10.1097/00003086-200006000-00009. [DOI] [PubMed] [Google Scholar]
- 8.Court-Brown CM, Walker C, Garg A, McQueen MM. Half-ring external fixation in the management of tibial plafond fractures. J Orthop Trauma. 1999;13:200–206. doi: 10.1097/00005131-199903000-00008. [DOI] [PubMed] [Google Scholar]
- 9.Drosos G, Karnezis IA, Bishay M, Miles AW. Initial rotational stability of distal tibial fractures nailed without proximal locking: the importance of fracture type and degree of cortical contact. Injury. 2001;32:137–143. doi: 10.1016/S0020-1383(00)00157-1. [DOI] [PubMed] [Google Scholar]
- 10.Fan CY, Chiang CC, Chuang TY, Chiu FY, Chen TH. Interlocking nails for displaced metaphyseal fractures of the distal tibia. Injury. 2005;36:669–674. doi: 10.1016/j.injury.2004.10.018. [DOI] [PubMed] [Google Scholar]
- 11.Farouk O, Krettek C, Miclau T, Schandelmaier P, Guy P, Tscherne H. Minimally invasive plate osteosynthesis and vascularity: preliminary results of a cadaver injection study. Injury. 1997;28(Suppl 1):A7–A12. doi: 10.1016/S0020-1383(97)90110-8. [DOI] [PubMed] [Google Scholar]
- 12.Farouk O, Krettek C, Miclau T, Schandelmaier P, Guy P, Tscherne H. Minimally invasive plate osteosynthesis: does percutaneous plating disrupt femoral blood supply less than the traditional technique? J Orthop Trauma. 1999;13:401–406. doi: 10.1097/00005131-199908000-00002. [DOI] [PubMed] [Google Scholar]
- 13.Field JR, Hearn TC, Caldwell CB. Bone plate fixation: an evaluation of interface contact area and force of the dynamic compression plate (DCP) and the limited contact-dynamic compression plate (LC-DCP) applied to cadaveric bone. J Orthop Trauma. 1997;11:368–373. doi: 10.1097/00005131-199707000-00013. [DOI] [PubMed] [Google Scholar]
- 14.Francois J, Vandeputte G, Verheyden F, Nelen G. Percutaneous plate fixation of fractures of the distal tibia. Acta Orthop Belg. 2004;70:148–154. [PubMed] [Google Scholar]
- 15.Friedlaender GE, Perry CR, Cole JD, Cook SD, Cierny G, Muschler GF, Zych GA, Calhoun JH, LaForte AJ, Yin S. Osteogenic protein-1 (bone morphogenetic protein-7) in the treatment of tibial nonunions. J Bone Joint Surg Am. 2001;83(Suppl 1):S151–S158. [PMC free article] [PubMed] [Google Scholar]
- 16.Frigg R. Locking Compression Plate (LCP). An osteosynthesis plate based on the Dynamic Compression Plate and the Point Contact Fixator (PC-Fix) Injury. 2001;32(Suppl 2):63–66. doi: 10.1016/S0020-1383(01)00127-9. [DOI] [PubMed] [Google Scholar]
- 17.Frigg R. Development of the Locking Compression Plate. Injury. 2003;34(Suppl 2):B6–B10. doi: 10.1016/j.injury.2003.09.020. [DOI] [PubMed] [Google Scholar]
- 18.Guidance Document for the Preparation of Investigational Device Exemptions and Pre-market Approval Applications for Bone Growth Stimulator Devices. Rockville MD, United States Food and Drug Administration, 1988.
- 19.Hasenboehler E, Rikli D, Babst R. Locking compression plate with minimally invasive plate osteosynthesis in diaphyseal and distal tibial fracture: a retrospective study of 32 patients. Injury. 2007;38:365–370. doi: 10.1016/j.injury.2006.10.024. [DOI] [PubMed] [Google Scholar]
- 20.Hazarika S, Chakravarthy J, Cooper J. Minimally invasive locking plate osteosynthesis for fractures of the distal tibia–results in 20 patients. Injury. 2006;37:877–887. doi: 10.1016/j.injury.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 21.Helfet DL, Shonnard PY, Levine D, Borrelli J., Jr Minimally invasive plate osteosynthesis of distal fractures of the tibia. Injury. 1997;28(Suppl 1):A42–A47. doi: 10.1016/S0020-1383(97)90114-5. [DOI] [PubMed] [Google Scholar]
- 22.Hintermann B, Regazzoni P, Lampert C, Stutz G, Gachter A. Arthroscopic findings in acute fractures of the ankle. J Bone Joint Surg Br. 2000;82:345–351. doi: 10.1302/0301-620X.82B3.10064. [DOI] [PubMed] [Google Scholar]
- 23.Holt ES. Arthroscopic visualization of the tibial plafond during posterior malleolar fracture fixation. Foot Ankle Int. 1994;15:206–208. doi: 10.1177/107110079401500409. [DOI] [PubMed] [Google Scholar]
- 24.Im GI, Tae SK. Distal metaphyseal fractures of tibia: a prospective randomized trial of closed reduction and intramedullary nail versus open reduction and plate and screws fixation. J Trauma. 2005;59:1219–1223. doi: 10.1097/01.ta.0000188936.79798.4e. [DOI] [PubMed] [Google Scholar]
- 25.Imade S, Takao M, Nishi H, Uchio Y. Arthroscopy-assisted reduction and percutaneous fixation for triplane fracture of the distal tibia. Arthroscopy. 2004;20:e123–e128. doi: 10.1016/j.arthro.2004.10.001. [DOI] [PubMed] [Google Scholar]
- 26.Janssen KW, Biert J, Kampen A. Treatment of distal tibial fractures: plate versus nail: a retrospective outcome analysis of matched pairs of patients. Int Orthop. 2007;31:709–714. doi: 10.1007/s00264-006-0237-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Khoury A, Liebergall M, London E, Mosheiff R. Percutaneous plating of distal tibial fractures. Foot Ankle Int. 2002;23:818–824. doi: 10.1177/107110070202300908. [DOI] [PubMed] [Google Scholar]
- 28.Kneifel T, Buckley R. A comparison of one versus two distal locking screws in tibial fractures treated with unreamed tibial nails: a prospective randomized clinical trial. Injury. 1996;27:271–273. doi: 10.1016/0020-1383(95)00116-6. [DOI] [PubMed] [Google Scholar]
- 29.Lau TW, Leung F, Chan CF, Chow SP. Wound complication of minimally invasive plate osteosynthesis in distal tibia fractures. Int Orthop. 2007;32:697–703. doi: 10.1007/s00264-007-0384-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Loren GJ, Ferkel RD. Arthroscopic assessment of occult intra-articular injury in acute ankle fractures. Arthroscopy. 2002;18:412–421. doi: 10.1053/jars.2002.32317. [DOI] [PubMed] [Google Scholar]
- 31.Maffulli N, Toms AD, McMurtie A, Oliva F. Percutaneous plating of distal tibial fractures. Int Orthop. 2004;28:159–162. doi: 10.1007/s00264-004-0541-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Marsh JL, Bonar S, Nepola JV, Decoster TA, Hurwitz SR. Use of an articulated external fixator for fractures of the tibial plafond. J Bone Joint Surg Am. 1995;77:1498–1509. doi: 10.2106/00004623-199510000-00004. [DOI] [PubMed] [Google Scholar]
- 33.Miller MD. Arthroscopically assisted reduction and fixation of an adult Tillaux fracture of the ankle. Arthroscopy. 1997;13:117–119. doi: 10.1016/s0749-8063(97)90220-6. [DOI] [PubMed] [Google Scholar]
- 34.Mosheiff R, Safran O, Segal D, Liebergall M. The unreamed tibial nail in the treatment of distal metaphyseal fractures. Injury. 1999;30:83–90. doi: 10.1016/S0020-1383(98)00213-7. [DOI] [PubMed] [Google Scholar]
- 35.Muller ME, Nazarian S, Koch P, Schatzker J. The Comprehensive Classification of Fractures of Long Bones. Berlin, Germany: Springer-Verlag; 1990.
- 36.Othman M, Strzelczyk P. Results of conservative treatment of “pilon” fractures. Ortop Traumatol Rehabil. 2003;5:787–794. [PubMed] [Google Scholar]
- 37.Perren SM. Evolution of the internal fixation of long bone fractures. The scientific basis of biological internal fixation: choosing a new balance between stability and biology. J Bone Joint Surg Br. 2002;84:1093–1110. doi: 10.1302/0301-620X.84B8.13752. [DOI] [PubMed] [Google Scholar]
- 38.Perren SM, Klaue K, Pohler O, Predieri M, Steinemann S, Gautier E. The limited contact dynamic compression plate (LC-DCP) Arch Orthop Trauma Surg. 1990;109:304–310. doi: 10.1007/BF00636166. [DOI] [PubMed] [Google Scholar]
- 39.Redfern DJ, Syed SU, Davies SJ. Fractures of the distal tibia: minimally invasive plate osteosynthesis. Injury. 2004;35:615–620. doi: 10.1016/j.injury.2003.09.005. [DOI] [PubMed] [Google Scholar]
- 40.Sarmiento A, Latta LL. 450 closed fractures of the distal third of the tibia treated with a functional brace. Clin Orthop Relat Res. 2004;428:261–271. doi: 10.1097/01.blo.0000137550.68318.f8. [DOI] [PubMed] [Google Scholar]
- 41.Shanmugam C, Rahmatalla A, Maffulli N. Percutaneous fixation of distal tibial fractures using locking plates. Tech Orthop. 2007;22:162–166. doi: 10.1097/BTO.0b013e318149fc3e. [DOI] [Google Scholar]
- 42.Shanmugam C, Rahmatalla A, Maffulli N. Strain in distal tibial osteotomy stabilized with metaphyseal and distal tibial locking compression plates. Tech Orthop. 2007;22:162–166. doi: 10.1097/BTO.0b013e318149fc3e. [DOI] [Google Scholar]
- 43.Stoffel K, Dieter U, Stachowiak G, Gachter A, Kuster MS. Biomechanical testing of the LCP–how can stability in locked internal fixators be controlled? Injury. 2003;34(Suppl 2):B11–B19. doi: 10.1016/j.injury.2003.09.021. [DOI] [PubMed] [Google Scholar]
- 44.Toms AD, McMurtie A, Maffulli N. Percutaneous plating of the distal tibia. J Foot Ankle Surg. 2004;43:199–203. doi: 10.1053/j.jfas.2004.03.005. [DOI] [PubMed] [Google Scholar]
- 45.Tull F, Borrelli J., Jr Soft-tissue injury associated with closed fractures: evaluation and management. J Am Acad Orthop Surg. 2003;11:431–438. doi: 10.5435/00124635-200311000-00007. [DOI] [PubMed] [Google Scholar]
- 46.Vallier HA, Le TT, Bedi A. Radiographic and clinical comparisons of distal tibia shaft fractures (4 to 11 cm proximal to the plafond): plating versus intramedullary nailing. J Orthop Trauma. 2008;22:307–311. doi: 10.1097/BOT.0b013e31816ed974. [DOI] [PubMed] [Google Scholar]
- 47.Watson JT, Moed BR, Karges DE, Cramer KE. Pilon fractures. Treatment protocol based on severity of soft tissue injury. Clin Orthop Relat Res. 2000;375:78–90. doi: 10.1097/00003086-200006000-00010. [DOI] [PubMed] [Google Scholar]
- 48.Yang SW, Tzeng HM, Chou YJ, Teng HP, Liu HH, Wong CY. Treatment of distal tibial metaphyseal fractures: Plating versus shortened intramedullary nailing. Injury. 2006;37:531–535. doi: 10.1016/j.injury.2005.09.013. [DOI] [PubMed] [Google Scholar]