Abstract
Abnormal reactions accompanied by bone formation in the osteoarticular region induced by long-term administration of etretinate have been reported. We treated a patient who received continuous treatment of psoriatic erythroderma with etretinate for 7 years, and who had an osseous bridge that extended across the acetabulum over the femur on both sides. The patient experienced a major gait disturbance and eventually was unable to walk. Functional gait was restored by resecting the ossified regions and radiotherapy. Histologic sections of the ossified lesions showed enchondral ossification in the ligament attachment site in the joint margin, with advancing ossification along the articular capsule; the pattern was similar to that in diffuse idiopathic skeletal hyperostosis. This is the first report of an osseous bridge associated with long-term administration of etretinate extending across the acetabulum over the femur on both sides.
Introduction
The retinoic acid preparation (synthetic vitamin A analog), etretinate, is effective for treatment of psoriasis vulgaris and pustular psoriasis. However, abnormal reactions accompanied by bone formation in the osteoarticular region induced by long-term administration of etretinate have been reported [1, 2, 9–12]. We encountered a patient who received continuous treatment of psoriatic erythroderma with etretinate for 7 years, in whom an osseous bridge extended across the acetabulum over the femur on both sides and caused gait disturbance. Gait function was restored by resection of the ossified regions and radiotherapy, and the resected bone was histologically examined.
Case Report
A 78-year-old man presented to our hospital with a chief complaint of bilateral hip pain and gait disturbance. He had the hip pain for 1 year, and range of motion of his hip had become progressively limited.
His family medical history was noncontributory. His medical history included epididymitis at 27 years of age, cervical vertebral ossification of the posterior longitudinal ligament at 55 years of age, and pulmonary emphysema at 72 years of age.
When he was 71 years old, erythema accompanied by scales appeared on the his scalp and extremities. Psoriasis vulgaris was diagnosed by a dermatologist, and administration of 30 mg/day oral etretinate (Tigason®; Chugai Pharmaceutical Co, Ltd, Tokyo, Japan) and external treatment were initiated. One year later, the patient visited the dermatology department of our hospital, and topical treatment with vitamin D3 and steroids, administration of 10 mg/day oral etretinate, and psoralen and ultraviolet A bath therapy were initiated for treatment of psoriatic erythroderma. Two years later, the dose of oral etretinate was increased to 20 mg/day because of poor control of skin eruptions.
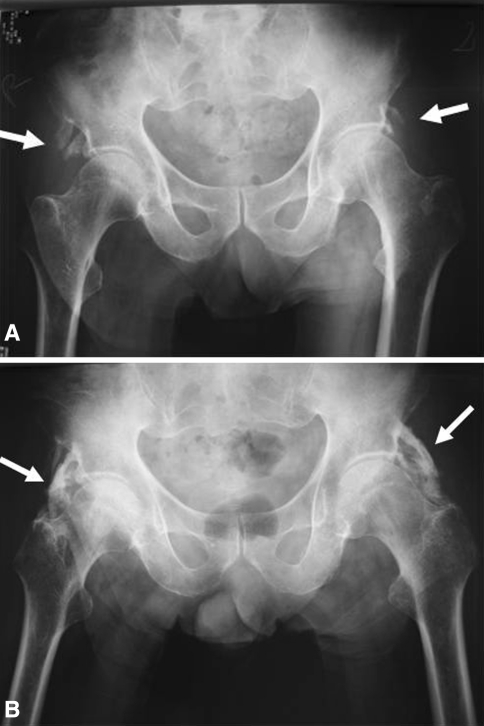
Six years after onset of the psoriasis, the patient was referred to the orthopaedics department of our hospital. Plain radiographs of the pelvis revealed ossification extending from the bilateral anterior-inferior iliac spines toward the distal direction (Fig. 1A). We recommended the patient stop the medicine but it was not practical owing to his psoriasis; we did not recommend any other treatment at that time.
Fig. 1A–B.
(A) Bilateral soft tissue ossification extending inferiorly from the anterior-inferior iliac spines on the acetabular side (arrows) extending from the right anterior-inferior iliac spine toward the distal direction was observed on plain radiographic examination. (B) One year later, bilateral ossification extended toward the distal direction along the articular capsule and bridged the acetabulum and trochanter (arrows).
During the following year, the patient became unable to walk owing to contracture in flexion, external rotation, and abduction and limited bilateral extension of the knees. He had no deformity of the distal interphalangeal joints characteristic of psoriatic arthropathy. The range of motion of both hips was limited. In addition, the bilateral extension of the knees was markedly limited owing to the contracture of the hips in flexion (Table 1).
Table 1.
Hip and knee range of motion
| Joint | Movement | Range of motion (preoperative/followup) | |
|---|---|---|---|
| Right side | Left side | ||
| Hip | Flexion | 40°/85° | 45°/90° |
| Extension | −30°/−10° | −40°/0° | |
| Adduction | −10°/10° | −10°/20° | |
| Abduction | 20°/10° | 20°/15° | |
| Internal rotation | −20°/0° | −20°/0° | |
| External rotation | 30°/40° | 30°/45° | |
| Knee | Flexion | 130°/125° | 130°/130° |
| Extension | −40°/−20° | −30°/−15° | |
The rheumatoid factor was negative, and C-reactive protein was 0.15, showing a slight increase, but the leukocyte count, calcium, phosphorus, and alkaline phosphatase were normal. The human leukocyte antigen type was A-24/B-52.
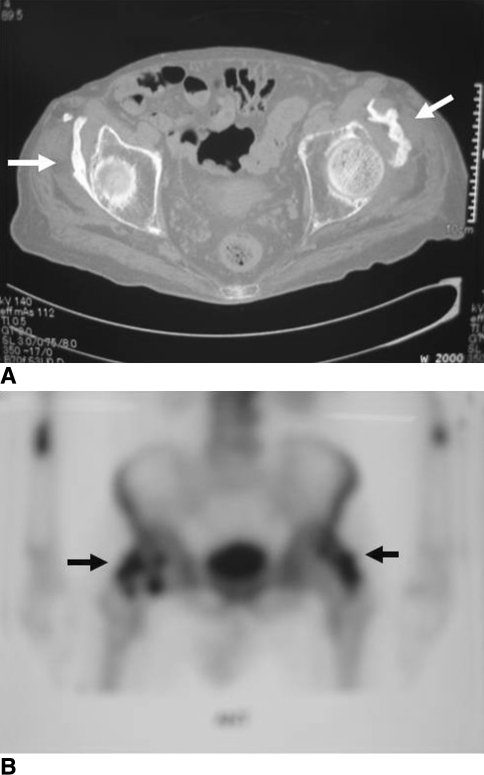
Radiographically, ossification extended toward the distal direction along the articular capsule and bridged the acetabulum and trochanter on both sides (Fig. 1B). On CT, the bilateral acetabula were ossified over the trochanters in contact with the lateral sides of the bilateral hip capsules (Fig. 2A). Moreover, the lumbar vertebrae showed ankylosing spinal hyperostosis (ASH), whereas the sacroiliac joint was normal. Bone scintigraphy detected abnormal accumulation in the bilateral hip regions (Fig. 2B).
Fig. 2A–B.
(A) A CT scan shows bridging soft tissue ossification extending from the superior lateral acetabulum to the greater trochanter over the trochanters in contact with the lateral sides of the bilateral hip capsules (arrows). (B) Bone scintigraphy detected an abnormal accumulation in the bilateral hip regions (arrows).
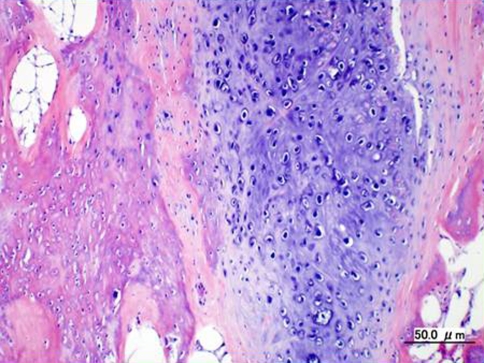
Based on these findings, we diagnosed etretinate-induced hyperplastic ossification of the bilateral hip regions. The ossified lesions in the bilateral hip regions were resected 1 year after onset of the hip symptoms. We used a posterolateral approach. In both hips, the ossified lesion covered the lateral side of the articular capsule and was partially continuous to the intertrochanteric crest. The ossified lesions were hard, appeared similar to cortical bone, and were mostly continuous to the lateral side of the articular capsule. On pathologic examination of the surgically excised ossified lesions, hyaline cartilage suggesting enchondral ossification and immature new bone was evident in the marginal region of the ossified lesions, and mature lamellar bonelike tissue was in contact with the articular capsule in its center (Fig. 3).
Fig. 3.
On pathologic examination of the surgically excised ossified lesions, hyaline cartilage suggesting enchondral ossification and immature new bone were evident in the marginal region of the ossified lesions, and mature lamellar bonelike tissue was in contact with the articular capsule in its center (Stain, hematoxylin and eosin; original magnification, ×100).
Postoperatively, the patient was treated prophylactically with radiotherapy and drug therapy. He received radiotherapy of the resected regions of both hips with 10 Gy (2 Gy × 5 treatments) beginning 2 days after surgery. We observed no skin changes after irradiation. Etidronate disodium (Didronel®; Procter & Gamble Pharmaceuticals, Inc, Cincinnati, OH; 800 mg/day) was given to the patient the day after surgery but the drug was discontinued 1 month later owing to his gastrointestinal symptoms. To control the primary disease (psoriatic erythroderma), administration of etretinate was continued at a reduced dose (15 mg/day).
At last followup 3.5 years after surgery, the patient was able to walk using two canes, and range of motion in both hips was improved. The range of the knees in extension was −20° on the right and −15° on the left, indicating limitation of extension remained in both knees (Table 1). On plain radiographic examination, a mild recurrent ossified lesion was seen in the hip region for which we have continued followups of the patient (Fig. 4).
Fig. 4.
At last followup 3.5 years after surgery, a mild recurrent ossified lesion was seen in the hip region on plain radiographic examination (arrow).
Discussion
Excessive ossification of the vertebral bodies and bones of the extremities (diffuse idiopathic skeletal hyperostosis or DISH) after administration of isotretinoin (13-cis-retinoic acid) at a high dose for 1 year was reported by Pennes et al. [11] in 1984. Osteophyte formation and ligament calcification induced by long-term oral etretinate administration was reported by Burge and Ryan [1]. Tendon and ligament calcification induced by long-term administration of isotretinoin for cystic acne also has been reported by DiGiovanna et al. [2]. Okada et al. [10] reported osteophyte formation and calcification of the vertebral anterior ligament occurred at a high frequency in a group of patients treated with etretinate for psoriasis vulgaris for 30 months on average. Although two studies [4, 13] suggest a causal relation between retinoid therapy and ossification of the vertebral bodies and bones of the extremities, such a relationship has not been established.
Retinoic acid preparations, such as etretinate, are effective for dermatologic diseases, such as psoriasis vulgaris, pustular psoriasis, and cystic acne, but attention should be paid to long-term administration-induced abnormal reactions accompanied by bone formation in the osteoarticular region, ligament, and tendon. However, early diagnosis is difficult because subjective symptoms, such as arthralgia and limited range of motion of joints, typically are minor [2, 11], and the blood calcium, phosphorus, and alkaline phosphatase levels are not abnormal on blood chemistry in many cases [12]. Thus, periodic examination of bone and joint abnormalities by radiography is necessary. Glover et al. [3] reported bone scintigraphy is useful for early discovery of bone and joint abnormalities during the early stage, when no ossifying bone is shown on radiography.
The cause of retinoic acid-induced ossification is unclear, but retinoids reportedly promote differentiation of undifferentiated mesenchymal cells into osteoblasts [5], and subsequent induction of proteoglycan release in bone induces changes in cartilage matrix [7], suggesting retinoic acid is closely involved in the promotion of bone formation. DiGiovanna et al. [2] reported ossification occurred in 84% of 38 patients with cystic acne who were treated with etretinate for 5 years or longer, and among nonvertebral regions, ossification occurred most frequently in the calcaneus (76%), followed by the pelvis in 53% and knee in 42%, whereas the incidence in the vertebrae was low, unlike the ossification occurring in DISH. Kilcoyne [6] described DISH and osteophyte development and progression after acitretin administration for 1 to 2 years in 11 (5%) of 240 patients with psoriasis (thoracic vertebrae in five and cervical vertebrae in four) and encouraged physicians to remain cognizant of the potential for cervical and thoracic vertebral lesions.
Histopathologically, cartilage metaplasia and enchondral ossification occur after fibrous vascular tissue hyperplasia in tendon/ligament attachment sites in DISH, and then vascular buds generated from the new bone penetrate the tidemark at the ligament attachment site to induce bone union [8]. In the histologic sections of the ossified lesions from our patient, hyaline cartilage, suggesting enchondral ossification and immature new bone, were present in the marginal region of the ossified lesions, and mature bone tissue was present in contact with the articular capsule in the central region. These observations are consistent with the theory that enchondral ossification occurs in the ligament attachment site in the joint margin and that ossification advances along the articular capsule, exhibiting an ossification mechanism similar to that in DISH.
To our knowledge, there has been no previous report of etretinate-induced ossification that progressed to bridge the bilateral hips, as seen in our patient. The progression of ossification to osseous bridging may have been attributable to the presence of cervical vertebral ossification of the posterior longitudinal ligament and ASH, strong predispositions of the wide definition of DISH, which may have responded excessively to etretinate. Based on our patient, we consider predisposition toward DISH should be investigated by radiography of the vertebrae (cervical, thoracic, and lumbar vertebrae), pelvis, and calcaneus before initiating administration of retinoic acid and vitamin A-related substances.
Acknowledgments
We thank Dr. Takanobu Nakase (Department of Orthopaedic Surgery, Hoshigaoka Koseinenkin Hospital Osaka, Japan) for help in preparing the original manuscript.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution waived the reporting of this case report, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at Nissay Hospital.
References
- 1.Burge S, Ryan T. Diffuse hyperostosis associated with etretinate. Lancet. 1985;2:397–398. doi: 10.1016/S0140-6736(85)92546-2. [DOI] [PubMed] [Google Scholar]
- 2.DiGiovanna JJ, Helfgott RK, Gerber LH, Peck GL. Extraspinal tendon and ligament calcification associated with long-term therapy with etretinate. N Engl J Med. 1986;315:1177–1182. doi: 10.1056/NEJM198611063151901. [DOI] [PubMed] [Google Scholar]
- 3.Glover MT, Peters AM, Atherton DJ. Surveillance for skeletal toxicity of children treated with etretinate. Br J Dermatol. 1987;116:609–614. doi: 10.1111/j.1365-2133.1987.tb05892.x. [DOI] [PubMed] [Google Scholar]
- 4.Halverstam CP, Zeichner J, Lebwohl M. Lack of significant skeletal changes after long-term, low-dose retinoid therapy: case report and review of the literature. J Cutan Med Surg. 2006;10:291–299. doi: 10.2310/7750.2006.00065. [DOI] [PubMed] [Google Scholar]
- 5.Katagiri T, Yamaguchi A, Ikeda T, Yoshiki S, Wozney JM, Rosen V, Wang EA, Tanaka H, Omura S, Suda T. The non-osteogenic mouse pluripotent cell line, C3H10T1/2, is induced to differentiate into osteoblastic cells by recombinant human bone morphogenetic protein-2. Biochem Biophys Res Commun. 1990;172:295–299. doi: 10.1016/S0006-291X(05)80208-6. [DOI] [PubMed] [Google Scholar]
- 6.Kilcoyne RF. Effects of retinoids in bone. J Am Acad Dermatol. 1988;19:212–216. doi: 10.1016/S0190-9622(88)70167-X. [DOI] [PubMed] [Google Scholar]
- 7.Kistler A. Retinoic acid-induced cartilage resorption: induction of specific changes in protein synthesis and inhibition by tunicamycin. Differentiation. 1982;21:168–174. doi: 10.1111/j.1432-0436.1982.tb01210.x. [DOI] [PubMed] [Google Scholar]
- 8.McCarthy EF, Frassica FJ. Pathology of Bone and Joint Disorders with Clinical and Radiographic Correlation. Philadelphia, PA: WB Saunders Co; 1998. pp. 294–298. [Google Scholar]
- 9.Melnik B, Glück S, Jungblut RM, Goerz G. Retrospective radiographic study of skeletal changes after long-term etretinate therapy. Br J Dermatol. 1987;116:207–212. doi: 10.1111/j.1365-2133.1987.tb05813.x. [DOI] [PubMed] [Google Scholar]
- 10.Okada N, Higashiyama M, Morimoto S, Yoshikawa K. Skeletal alterations associated with long-term etretinate therapy] [in Japanese. Nippon Hifuka Gakkai Zasshi. 1991;101:547–552. [PubMed] [Google Scholar]
- 11.Pennes DR, Ellis CN, Madison KC, Voorhees JJ, Martel W. Early skeletal hyperostoses secondary to 13-cis-retinoic acid. AJR Am J Roentgenol. 1984;142:979–983. doi: 10.2214/ajr.142.5.979. [DOI] [PubMed] [Google Scholar]
- 12.Seishima M, Aoyama Y, Mori S, Kikuie A. A case of pustular psoriasis with hyperostosis induced by etretinate] [in Japanese. Nippon Hifuka Gakkai Zasshi. 1992;102:569–576. [Google Scholar]
- 13.Dooren-Greebe RJ, Lemmens JA, Boo T, Hangx NM, Kuijpers AL, Kerkhof PC. Prolonged treatment with oral retinoids in adults: no influence on the frequency and severity of spinal abnormalities. Br J Dermatol. 1996;134:71–76. doi: 10.1111/j.1365-2133.1996.tb07842.x. [DOI] [PubMed] [Google Scholar]