Abstract
In general practice, short films of the knee are used to assess component position and define the entry point for intramedullary femoral alignment in TKAs; however, whether it is justified to use the short film commonly used in research settings and everyday practice as a substitute for the whole leg view is controversial and needs clarification. In 138 long leg CT scanograms we measured the angle formed by the anatomic axis of the proximal fourth of the tibia and the mechanical axis of the tibia, the angle formed by the anatomic axis of the distal fourth of the femur and the mechanical axis of the femur, the “bow” of the tibia (as reflected by the offset of the anatomic axis from the center of the talus), and the “bow” of the femur (as reflected by the offset of the anatomic axis from the center of the femoral head). Because the angle formed by these axes and the bow of the tibia and femur have wide variability in females and males, a short film of the knee should not be used in place of the whole leg view when accurate assessment of component position and limb alignment is essential. A previous study of normal limbs found that only 2% of subjects have a neutral hip-knee-ankle axis, which can be explained by the wide variability of the bow in the tibia and femur and the lack of correlation between the bow of the tibia and femur in a given limb as shown in the current study.
Introduction
It generally is accepted that wear and loosening depend on proper alignment of the components and the limb, however, review of the methods of previous research of limb alignment in TKA has revealed two limitations that cause us to question the relationship between wear and loosening. These limitations include the use of a short film of the knee instead of a whole leg view to assess limb alignment, and the study of a knee component with size, shape, and fixation features that no longer are deemed desirable [1].
The use of the standard short knee film as a substitute for the whole leg view for assessing component and limb alignment is commonplace in everyday practice but controversial. Limb alignment in the coronal plane is quantified by the hip-knee-ankle axis. Neutral alignment is said to exist when the line connecting the center of the femoral head and center of the ankle passes through the center of the knee, and varus or valgus alignment is said to exist when this line passes medially or laterally, respectively, to the center of the knee [4, 25]. One study concluded short knee images cannot substitute for whole leg views when accurate assessment of the hip-knee-ankle axis is essential [30], whereas other studies suggested the anatomic axis of the knee on short knee film appears to be a valid alternative to the hip-knee-ankle axis of the limb on full leg radiographs [8, 16].
For the short knee film to accurately substitute for the whole leg view, the variability of the angle formed by the anatomic and mechanical axes in the tibia and femur and the variability of the bow of the tibia and femur should be small. Studies have qualitatively reported variability in the bow of the tibia and femur [15, 20, 24, 27, 28]; however, these studies did not describe a method for quantifying the bow. A previous study of normal limbs found that only 2% of subjects have a neutral hip-knee-ankle axis [7], which might be explained by variability in the angle formed by the anatomic and mechanical axes and the bow in the tibia and femur and a lack of correlation between the bow of the tibia and femur in a given limb.
Accordingly, we hypothesized (1) the angle formed by the anatomic axis of the proximal fourth of the tibia and the mechanical axis of the tibia and the angle formed by the anatomic axis of the distal fourth of the femur have wide variability; (2) the bow of the tibia and femur has wide variability; (3) there are no differences in the angle and bow between females and males; and (4) there is no correlation between the bow of the tibia and femur in a given limb.
Materials and Methods
We considered all patients who underwent TKAs from June 19 to December 1, 2007, for inclusion. The inclusion criterion was the presence of primary arthritis of the knee with or without previous open or arthroscopic meniscectomy or ligament reconstruction. We excluded patients with a treated leg with evidence of a hip disorder (ie, developmental dysplasia, Perthes, or slipped epiphysis), an osteotomy, a healed fracture, internal fixation, arthroplasty of the hip, knee, or ankle, or a malaligned computer tomogram of the leg. Four patients were excluded because of developmental dysplasia of the hip (N = 1), THA (N = 1), internal fixation of a femoral neck fracture (N = 1), and a malaligned computer tomogram of the leg (N = 1). Therefore, the study consisted of 138 patients (90 women, 48 men) with an average age of 68 ± 10 years. All patients received an unconstrained TKA (Vanguard; Biomet, Inc, Warsaw, IN). We obtained Institutional Review Board approval.
In accordance with a standard protocol, we acquired a postoperative, anteroposterior scanogram with a field of view from the hip to the ankle with use of CT (GE LightSpeed® 16; GE Healthcare, www.gehealthcare.com). Because simultaneous flexion of the knee and rotation of the leg causes large changes in projected angles [2, 15], we limited the projection error of the mechanical axis to approximately 1° by iteratively rotating the limb and repeating the scanogram until the two augment holes in the posterior condyles were at least partially visible on either side of the flange of the femoral component.
One of us (KK) made measurements under a magnified view using screen measurement software (Screen Caliper, Compass, and Protractor; Iconico Inc, www.iconico.com; Adobe Photoshop, Adobe Inc, www.adobe.com) with a reported accuracy of 0.5° [26]. Because the short knee film often is used intraoperatively and postoperatively to assess component position, especially when access to full limb radiographs is limited [14, 16, 24, 30], and because the short knee film typically shows only the proximal fourth of the tibia and the distal fourth of the femur [8, 16], we defined the anatomic axes of the tibia and femur based on axes centered in the proximal fourth of the tibia and the distal fourth of the femur. The anatomic axis of the tibia was a line joining the midpoints of the tibia at the joint line and at the junction of the proximal one-fourth and distal three-fourths of the tibia [15, 16, 21, 26] (Fig. 1). The mechanical axis of the tibia was a line joining the midpoint of the tibia at the joint line and the center of the talus [12, 15, 16, 18, 21, 25, 27, 32]. The angle formed by the mechanical axis and the anatomic axis of the tibia was measured. We defined the bow of the tibia in the coronal plane as the offset in centimeters of the anatomic axis of the tibia and the center of the talus (Fig. 1). A positive value (+) indicated a valgus tibia with the apex of the bow pointing medial and with the anatomic axis passing medial to the center of the talus. A negative value (−) indicated a varus tibia with the apex of the bow pointing lateral and with the anatomic axis passing lateral to the center of the talus. The anatomic axis of the femur was a line joining the midpoints of the femur at the joint line and at the junction of the distal one-fourth and proximal three-fourths of the femur (Fig. 2). The mechanical axis of the femur was a line joining the midpoint of the femur at the joint line and the center of the femoral head [7]. The angle formed by the anatomic axis and the mechanical axis of the femur was measured. We defined the bow of the femur in the coronal plane as the offset in centimeters of the anatomic axis of the femur from the center of the femoral head. The larger the offset, the larger the bow with a positive value (+) indicating the anatomic axis passed lateral to the center of the femoral head and a negative value (−) indicating the anatomic axis passed medial to the center of the femoral head.
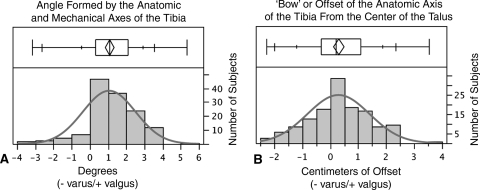
Fig. 1A–B.
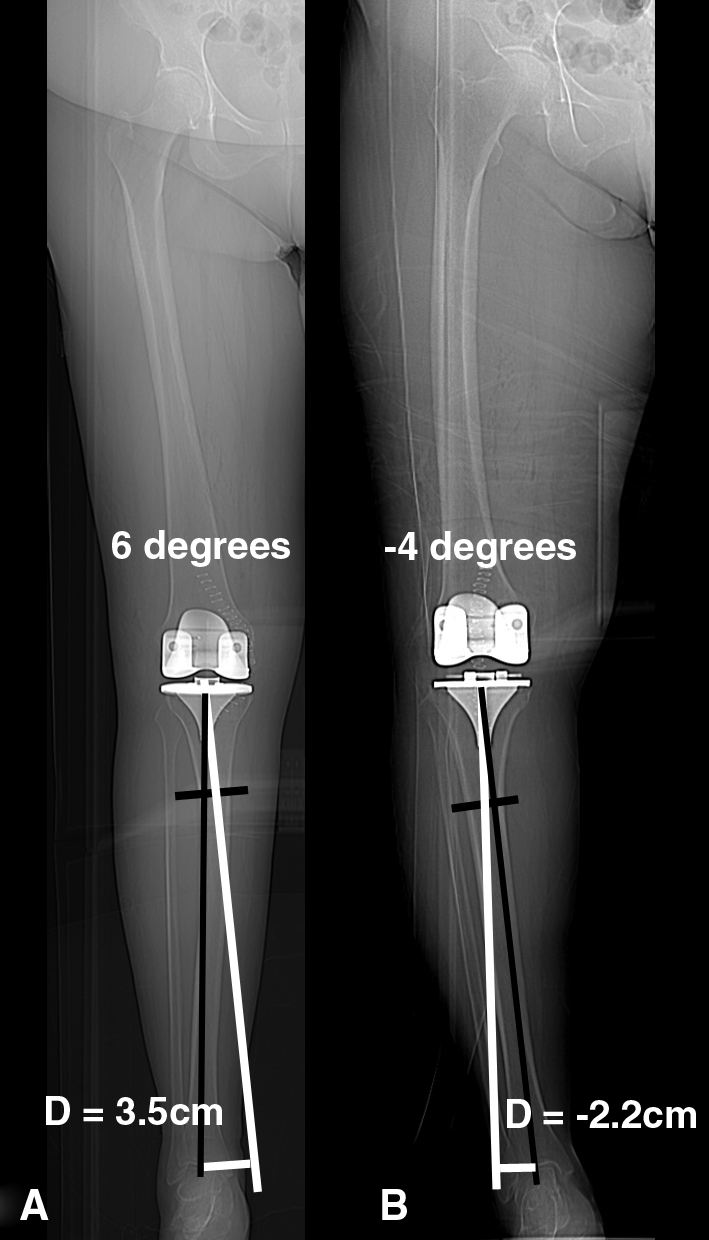
The anatomic axis of the tibia (longitudinal white line) was a line joining the midpoints of the tibia at the joint line and at the junction of the proximal one-fourth and distal three-fourths of the tibia (transverse black line). The mechanical axis of the tibia was a line joining the midpoint of the tibia at the joint line and the center of the talus (longitudinal black line). The angle formed by these two lines was measured. The bow of the tibia was quantified by the offset (D) measured from a line (transverse white line) drawn perpendicular from the anatomic axis of the tibia to the center of the talus. A positive value (+) indicated a valgus tibia with the apex of the bow pointing medial and with the anatomic axis passing medial to the center of the talus. (A) The offset of the tibia with the greatest valgus bow was 3.5 cm. A negative value (–) indicated a varus tibia with the apex of the bow pointing lateral and with the anatomic axis passing lateral to the center of the talus. (B) The offset of the tibia with the greatest varus bow was −2.2 cm. The use of an extramedullary tibia guide that references the ankle would place the tibial cut in six additional degrees of varus in the valgus tibia (left) and four additional degrees of valgus in the varus tibia (right) requiring lateral and medial soft tissue release to balance the knee, respectively.
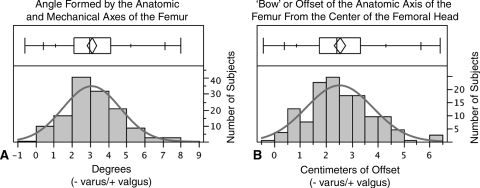
Fig. 2A–B.
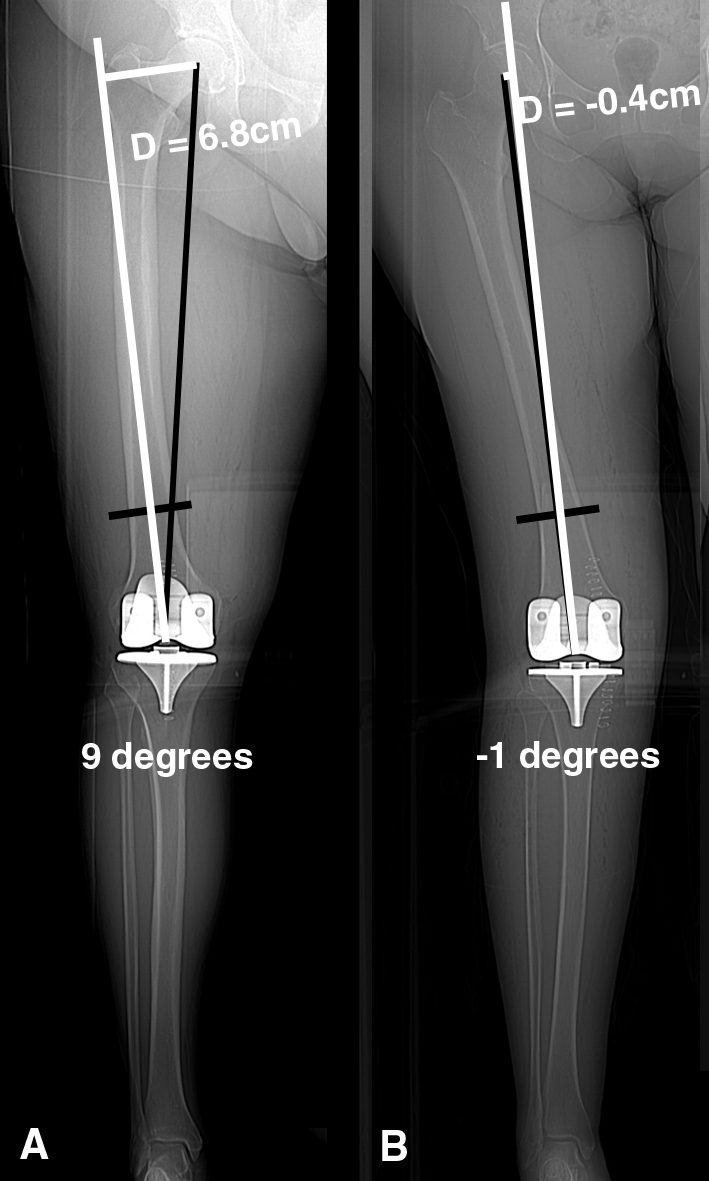
The anatomic axis of the femur (longitudinal white line) was a line joining the midpoints of the tibia at the joint line and at the junction of the distal one-fourth and proximal three-fourths of the femur (transverse black line). The mechanical axis of the femur was a line joining the midpoint of the femur at the joint line and the center of the femoral head (longitudinal black line). The angle formed by these two lines was measured. The bow of the femur was quantified by the offset (D) measured from a line (transverse white line) drawn perpendicular from the anatomic axis of the femur to the center of the femoral head. The larger the offset, the larger the bow with a positive value (+) indicating the anatomic axis passed lateral to the center of the femoral head and a negative value (−) indicating the anatomic axis passed medial to the center of the femoral head. (A) The offset of the femur with the greatest lateral bow was 6.4 cm. (B) The offset of the femur with the least lateral bow was −0.4 cm. Because of the variability in the lateral bow of the femur, the mechanical axis of the femur does not form a 5° to 6° angle with the anatomic axis of the distal fourth of the femur in either leg.
We used the arithmetic mean, standard deviation, 95% confidence interval, frequency distribution, and quantile box plot to describe the variability of the angle formed by the anatomic and mechanical axes of the tibia and femur and the bow of the tibia and femur. The quantile box plot summarizes the distribution of data points. The line across the middle of the box identifies the median. The ends of the box indicate the 25th and 75th quantiles. The small ticks indicate the 10% and 90% quantiles, the intermediate ticks indicate the 2.5% and 97.5% quantiles, and the large ticks indicate the 0% and 100% quantiles. An unpaired t-test was used to determine whether the angle formed by the anatomic and mechanical axes of the tibia and femur and the bow of the tibia and femur were different between females and males. A correlation coefficient was computed to assess the correlation between the bow of the tibia and the bow of the femur. Each analysis was performed with software (Version 7.0.2, JMP for MacIntosh; SPSS, Chicago, IL; www.jmp.com).
Results
The angle formed by the anatomic axis and the mechanical axis of the tibia and the bow of the tibia varied widely (Fig. 3). The angle formed by the anatomic axis and the mechanical axis of the femur and the bow of the femur also varied widely (Fig. 4). The angle formed by the anatomic and mechanical axes of the tibia varied 11° from −4° to 6° and averaged 1.1° ± 1.4° (valgus tibia). The angle was less than −1° or greater than 1° in 61%, less than −2° or greater than 2° in 34%, and less than −3° or greater than 3° in 13% of the subjects. The angle formed by the anatomic and mechanical axes of the femur varied 10° from −1° to 8°, averaged 3° ± 1.6°, and the 95% confidence interval (2.8°–3.4°) did not include 5° or 6°.
Fig. 3A–B.
Frequency distributions of the (A) angle formed by the anatomic and mechanical axes of the tibia and (B) bow of the tibia as quantified by the offset of the anatomic axis from the center of the talus are shown. Descriptive statistics include the quantile plot and the number of patients in each column.
Fig. 4A–B.
Frequency distributions of the (A) angle formed by the anatomic and mechanical axes of the femur and (B) bow of the femur as quantified by the offset of the anatomic axis of the femur from the center of the femoral head are shown. Descriptive statistics include the quantile plot and the number of patients in each column.
The bow of the tibia, defined by the offset of the anatomic axis from the center of the talus, varied 5.7 cm from 2.2 cm medial to 3.5 cm lateral to the center of the talus and averaged 0.3 ± 1.1 cm. The bow of the femur, defined by the offset of the anatomic axis from the center of the femoral head, varied 7.2 cm from 6.8 cm lateral to −0.4 cm medial to the center of the femoral head and averaged 2.5 ± 1.3 cm.
We observed no difference in the angle formed by the anatomic and mechanical axes of the tibia (p = 0.8784) and femur (p = 0.7706) and the bow of the tibia (p = 0.8578) and femur (p = 0.8101) between females and males (Table 1).
Table 1.
Comparison of the angle formed by the anatomic and mechanical axes and the bow
| Dependent variable | Female (n = 90) | Male (n = 48) | p Value |
|---|---|---|---|
| Angle of the anatomic and mechanical axes in the tibia | −1.2° ± 1.5° | −0.9° ± 1.4° | 0.8784, NS |
| Angle of the anatomic and mechanical axes in the femur | 3.0° ± 1.5° | 3.2° ± 1.7° | 0.7706, NS |
| Bow of the tibia (ie, offset of the anatomic axis from the center of the talus) | −0.4 ± 1.1 cm | −0.2 ± 1.1 cm | 0.8578, NS |
| Bow of the femur (ie, offset of the anatomic axis from the center of the femoral head) | 2.5 ± 1.2 cm | 2.7 ± 1.4 cm | 0.8101, NS |
NS = nonsignificant.
We found no correlation between the bow of the tibia and femur in a given limb (r = 0.0185, p = 0.8286), which means the degree and direction of the bow in the tibia is not related to the degree of bow of the femur in a given limb.
Discussion
For the short film of the knee to accurately substitute for the whole leg view, the variability of the angle formed by the anatomic and mechanical axes in the tibia and femur and the variability of the bow of the tibia and femur should be small. We hypothesized (1) the angle formed by the anatomic axis of the proximal fourth of the tibia and the mechanical axis of the tibia and the angle formed by the anatomic axis of the distal fourth of the femur has wide variability; (2) the bow of the tibia and femur has wide variability; (3) there are no differences in the angles and bows between females and males; and (4) there is no correlation between the bow of the tibia and femur in a given limb.
We examine several limitations that might have affected the observed variability of the angle formed by the anatomic and mechanical axes and the bow of the tibia and femur. First, while we used nonweightbearing, rotationally controlled CT scanograms obtained in knees with osteoarthritis after TKA instead of weightbearing scanograms of normal limbs, we believe this unlikely affected the variability because the weightbearing status, presence or absence of components, and removal of osteophytes back to the normal edge of the joint at the time of surgery do not affect the shape of the tibia and femur. Second, the variability from our study of a Western population is likely to be different from the variability of an Occidental population, which has a high prevalence of tibias with a varus bow and a high prevalence of femurs with a large lateral bow [26].
The wide variability of the angle formed by the anatomic and mechanical axes of the tibia and femur in our study agrees with some previous studies [18, 21, 27, 28], but does not agree with the historic, pioneering principles in TKA [13, 15, 19, 29, 32]. In terms of the tibia, the principle of aligning the varus/valgus osteotomy of the proximal tibia in TKA was based on an idealized depiction of the tibia in which the shaft of the tibia was straight and the mechanical and anatomic axes of the tibia were assumed to be the same [13, 15, 19, 29, 32]. We found only 11% (16 of 138) of the tibias were straight with 34% of the subjects having an anatomic axis that diverged greater than 2° varus or valgus from the mechanical axis of the tibia. In terms of the femur, the principle of aligning the varus/valgus osteotomy of the distal femur in TKA was based on the assumption that the angle formed by the anatomic and mechanical axes of the femur is consistently between 5° and 6° [15, 19, 31]. In contrast to these previous studies, we found the angle averaged 3° with only 6% of the femurs having an angle of 5° to 6°. The difference might be explained by our use of the distal one-fourth of the femoral shaft to define the anatomic axis, which is a shorter linear length for defining the anatomic axis of the femur than used in other studies [3, 4, 12, 19]. The clinical consequences of this variability are the use of a short knee film to check the varus/valgus osteotomy intraoperatively and component alignment and to predict the hip-knee-ankle axis postoperatively is unreliable because of the inconsistent relationship between the anatomic and mechanical axes of the tibia and femur (Fig. 5) [30].
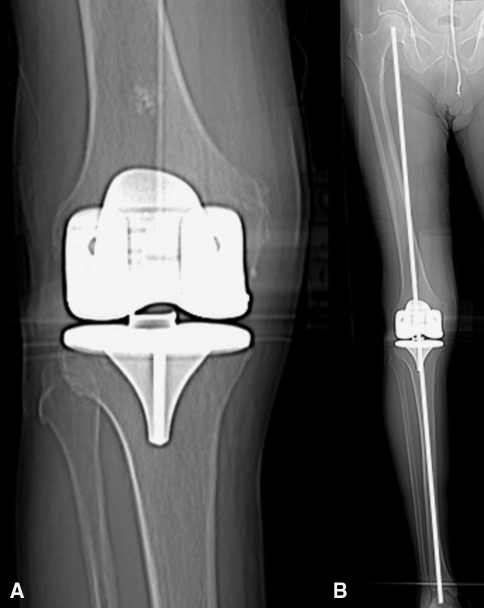
Fig. 5A–B.
(A) The short view of the knee suggests the tibial component is malaligned in varus. (B) However, the long leg view shows the limb has a neutral hip-knee-ankle axis. The use a short knee radiograph to assess component and limb alignment is not recommended.
The offset of the anatomic axis of the tibia and femur from the center of the talus and femoral head, respectively, is a new method for quantifying the degree of bow of these two bones. In the tibia, the bow typically starts at the junction of the proximal one-fourth and distal three-fourths of the tibia (Fig. 1). The extramedullary tibial guide strives to reproduce the mechanical axis of the tibia by referencing the ankle and making a classic tibial osteotomy that centers the ankle on the knee. Making a classic tibial osteotomy with an extramedullary guide only maintains the normal plane between the knee and ankle when there is no bow in the tibia (ie, anatomic and mechanical axes of the tibia are the same), which occurred in only 11% of the patients in our study. The use of an intramedullary tibial guide results in a less than ideal cut in a bowed tibia because aligning the intramedullary tibial guide parallel to the mechanical axis of the tibia is impossible [27]. In the femur, the factors determining the level of the bow are more complex than in the tibia. The bow in the femur is affected by variations in the bow of the shaft of the femur, the neck-shaft angle, and the length of the femoral neck (Fig. 2). Much has been written about how the degree of bow affects the starting point for insertion of the intramedullary rod and the accuracy of alignment of the varus/valgus osteotomy of the distal femur [17, 23, 24, 26, 28]. The wide variability of the bow of the femur in our patients further underscores the need to determine, for each patient, the best angle for making the distal femur varus/valgus osteotomy. Determining the best angle for each patient is a challenge because guidelines for placing the starting point for insertion of the intramedullary rod in the distal femur and selecting the angle, although available, lack agreement [24].
We identified no difference in the variability of the angle formed by the anatomic and mechanical axes and the bow in the tibia and femur between females and males. The lack of a gender difference between the angle formed by the anatomic and mechanical axes in the femur has been confirmed in the Chinese population [26].
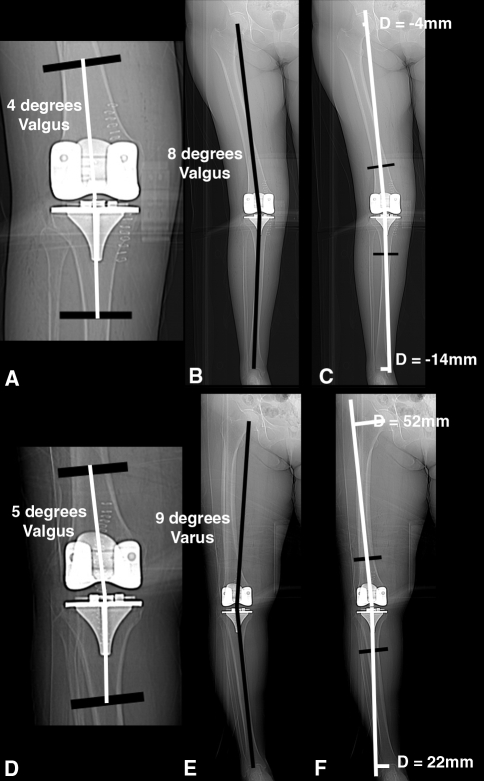
A previous study of normal limbs found that only 2% of subjects have a neutral hip-knee-ankle axis [7], which can be explained by the wide variability of the bow in the tibia and femur and the lack of correlation between the bow of the tibia and femur in a given leg observed in the current study. A leg with a valgus hip-knee-ankle axis typically has a tibia with a medial bow combined with a femur with a small lateral bow (ie, offset). A leg with a varus hip-knee-ankle axis typically has a tibia with a lateral bow combined with a femur with a large lateral bow (ie, offset) (Fig. 6). The independent pairing of any shaped tibia with any shaped femur does not agree with the classic assumption that the bow of the tibia and femur compensate for each other to form a neutral hip-knee-ankle axis of the limb [13, 22, 29].
Fig. 6A–F.
(A, D) The anatomic axis (longitudinal white lines) of the knee measured on the radiographic view of these two knees are similar; however, (B, E) the hip-knee-ankle axis of these two limbs are dissimilar. (C, F) The reason the anatomic axis of the knee does not predict the hip-knee-ankle axis of the limb is because of the wide variability in the bow of the tibia of the femur and because of the lack of correlation between the bow of a tibia and femur in a given limb.
The variability in the angle formed by the anatomic and mechanical axes and bow in the tibia and femur has changed our method for choosing the correct angle for making the proximal tibia and distal femoral cut. Because few normal limbs have a neutral hip-knee-ankle axis (ie, 2%) [7], and because changing the hip-knee-axis from normal to neutral changes the three kinematic axes of the knee from normal and requires collateral ligament and retinacular releases that can lead to instability, we align the components kinematically [6, 7, 10, 11]. Three interrelated axes, none of which share any relationship to the center of the femoral head or the center of the ankle, describe the kinematics of the knee [5, 6, 9]. The primary axis is a tibial-femoral axis in the femur about which the tibia flexes and extends and is nonorthogonal to the three anatomic planes (ie, sagittal, coronal, and axial) [5–7, 9]. One secondary axis is the patellofemoral axis in the femur about which the patella flexes and extends that is aligned parallel to the primary axis [5]. The other secondary axis is a tibial-femoral axis in the tibia about which the tibia internally and externally rotates on the femur that is perpendicular to the tibial-femoral axis and the patellofemoral flexion axis in the femur [5, 9]. Therefore, the foundation for restoring normal kinematics in TKA is aligning the axis of the femoral component coincident with the axis in the femur about which the tibia flexes and extends [5–7, 9].
Virtual, preoperative planning is used to align the axis of the femoral component coincident with the tibial-femoral axis in the femur by shape-matching the articular surface of the femoral component to the articular surface of the normal femur. A three-dimensional model of the normal femur is reconstructed from MR images of the patient’s knee, which are each restored by filling in areas of focal wear. The surgical technique uses custom-made tibial and femoral cutting guides machined to the topography of the patient’s knee to position the femoral and tibial components in all six degrees of freedom. This technique, which surface-matches the components to a knee that virtually has been restored to normal, adheres to the measured resection principle of TKA and restores the hip-knee-ankle axis to the natural prearthritic alignment of the limb the subject had before arthritis and deformity developed [10, 11].
Conventional instrumentation and the current iterations of surgical navigation systems do not account for the wide intrasubject and intersubject variations in the angle formed by the anatomic and mechanical axes and the bow of the tibia and femur that are important in the selection of the ideal surgical planes in TKA [24]. Use of the short knee film to judge placement of intramedullary and extramedullary rods, component alignment, and predict the hip-knee-ankle axis of the limb cannot be justified [30].
Acknowledgments
We thank the imaging staff at Methodist Hospital for obtaining well-aligned scout CT scans of the limb.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Footnotes
One of the authors (SMH) is a paid consultant for and receives royalties from Biomet Sports Medicine, Inc; one of the authors (SMH) is a co-founder, stockholder, and unpaid consultant for OtisMed.
Each author certifies that his or her institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at the University of California at Davis, Davis, CA.
References
- 1.Alden KJ, Pagnano MW. Computer-assisted surgery: a wine before its time. Orthopedics. 2008;31:936–939. doi: 10.3928/01477447-20080901-02. [DOI] [PubMed] [Google Scholar]
- 2.Brouwer RW, Jakma TS, Brouwer KH, Verhaar JA. Pitfalls in determining knee alignment: a radiographic cadaver study. J Knee Surg. 2007;20:210–215. doi: 10.1055/s-0030-1248045. [DOI] [PubMed] [Google Scholar]
- 3.Cooke D, Scudamore A, Li J, Wyss U, Bryant T, Costigan P. Axial lower-limb alignment: comparison of knee geometry in normal volunteers and osteoarthritis patients. Osteoarthritis Cartilage. 1997;5:39–47. doi: 10.1016/S1063-4584(97)80030-1. [DOI] [PubMed] [Google Scholar]
- 4.Cooke TD, Sled EA, Scudamore RA. Frontal plane knee alignment: a call for standardized measurement. J Rheumatol. 2007;34:1796–1801. [PubMed] [Google Scholar]
- 5.Coughlin KM, Incavo SJ, Churchill DL, Beynnon BD. Tibial axis and patellar position relative to the femoral epicondylar axis during squatting. J Arthroplasty. 2003;18:1048–1055. doi: 10.1016/S0883-5403(03)00449-2. [DOI] [PubMed] [Google Scholar]
- 6.Eckhoff D, Hogan C, DiMatteo L, Robinson M, Bach J. Difference between the epicondylar and cylindrical axis of the knee. Clin Orthop Relat Res. 2007;461:238–244. doi: 10.1097/BLO.0b013e318112416b. [DOI] [PubMed] [Google Scholar]
- 7.Eckhoff DG, Bach JM, Spitzer VM, Reinig KD, Bagur MM, Baldini TH, Flannery NM. Three-dimensional mechanics, kinematics, and morphology of the knee viewed in virtual reality. J Bone Joint Surg Am. 2005;87(suppl 2):71–80. doi: 10.2106/JBJS.E.00440. [DOI] [PubMed] [Google Scholar]
- 8.Hinman RS, May RL, Crossley KM. Is there an alternative to the full-leg radiograph for determining knee joint alignment in osteoarthritis? Arthritis Rheum. 2006;55:306–313. doi: 10.1002/art.21836. [DOI] [PubMed] [Google Scholar]
- 9.Hollister AM, Jatana S, Singh AK, Sullivan WW, Lupichuk AG. The axes of rotation of the knee. Clin Orthop Relat Res. 1993;290:259–268. [PubMed] [Google Scholar]
- 10.Howell SM, Hodapp EE, Kuznik K, Hull ML. In vivo adduction and reverse axial rotation (external) of the tibial component can be minimized. Orthopedics. 2009;32:319. doi: 10.3928/01477447-20090501-04. [DOI] [PubMed] [Google Scholar]
- 11.Howell SM, Kuznik K, Hull ML, Siston RA. Results of an initial experience with custom-fit positioning total knee arthroplasty in a series of 48 patients. Orthopedics. 2008;31:857–863. doi: 10.3928/01477447-20080901-15. [DOI] [PubMed] [Google Scholar]
- 12.Hsu RW, Himeno S, Coventry MB, Chao EY. Normal axial alignment of the lower extremity and load-bearing distribution at the knee. Clin Orthop Relat Res. 1990;255:215–227. [PubMed] [Google Scholar]
- 13.Hungerford DS, Krackow KA. Total joint arthroplasty of the knee. Clin Orthop Relat Res. 1985;192:23–33. [PubMed] [Google Scholar]
- 14.Issa SN, Dunlop D, Chang A, Song J, Prasad PV, Guermazi A, Peterfy C, Cahue S, Marshall M, Kapoor D, Hayes K, Sharma L. Full-limb and knee radiography assessments of varus-valgus alignment and their relationship to osteoarthritis disease features by magnetic resonance imaging. Arthritis Rheum. 2007;57:398–406. doi: 10.1002/art.22618. [DOI] [PubMed] [Google Scholar]
- 15.Jiang CC, Insall JN. Effect of rotation on the axial alignment of the femur: pitfalls in the use of femoral intramedullary guides in total knee arthroplasty. Clin Orthop Relat Res. 1989;248:50–56. [PubMed] [Google Scholar]
- 16.Kraus VB, Vail TP, Worrell T, McDaniel G. A comparative assessment of alignment angle of the knee by radiographic and physical examination methods. Arthritis Rheum. 2005;52:1730–1735. doi: 10.1002/art.21100. [DOI] [PubMed] [Google Scholar]
- 17.Lam LO, Shakespeare D. Varus/valgus alignment of the femoral component in total knee arthroplasty. Knee. 2003;10:237–241. doi: 10.1016/S0968-0160(02)00098-4. [DOI] [PubMed] [Google Scholar]
- 18.Matsuda S, Mizu-uchi H, Miura H, Nagamine R, Urabe K, Iwamoto Y. Tibial shaft axis does not always serve as a correct coronal landmark in total knee arthroplasty for varus knees. J Arthroplasty. 2003;18:56–62. doi: 10.1054/arth.2003.50002. [DOI] [PubMed] [Google Scholar]
- 19.Moreland JR, Bassett LW, Hanker GJ. Radiographic analysis of the axial alignment of the lower extremity. J Bone Joint Surg Am. 1987;69:745–749. [PubMed] [Google Scholar]
- 20.Novotny J, Gonzalez MH, Amirouche FM, Li YC. Geometric analysis of potential error in using femoral intramedullary guides in total knee arthroplasty. J Arthroplasty. 2001;16:641–647. doi: 10.1054/arth.2001.23714. [DOI] [PubMed] [Google Scholar]
- 21.Oswald MH, Jakob RP, Schneider E, Hoogewoud HM. Radiological analysis of normal axial alignment of femur and tibia in view of total knee arthroplasty. J Arthroplasty. 1993;8:419–426. doi: 10.1016/S0883-5403(06)80042-2. [DOI] [PubMed] [Google Scholar]
- 22.Paley D, Tetsworth K. Mechanical axis deviation of the lower limbs: preoperative planning of uniapical angular deformities of the tibia or femur. Clin Orthop Relat Res. 1992;280:48–64. [PubMed] [Google Scholar]
- 23.Reed SC, Gollish J. The accuracy of femoral intramedullary guides in total knee arthroplasty. J Arthroplasty. 1997;12:677–682. doi: 10.1016/S0883-5403(97)90141-8. [DOI] [PubMed] [Google Scholar]
- 24.Shakespeare D. Conventional instruments in total knee replacement: what should we do with them? Knee. 2006;13:1–6. doi: 10.1016/j.knee.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 25.Sikorski JM. Alignment in total knee replacement. J Bone Joint Surg Br. 2008;90:1121–1127. doi: 10.1302/0301-620X.90B9.20793. [DOI] [PubMed] [Google Scholar]
- 26.Tang WM, Zhu YH, Chiu KY. Axial alignment of the lower extremity in Chinese adults. J Bone Joint Surg Am. 2000;82:1603–1608. doi: 10.2106/00004623-200011000-00014. [DOI] [PubMed] [Google Scholar]
- 27.Teter KE, Bregman D, Colwell CW., Jr Accuracy of intramedullary versus extramedullary tibial alignment cutting systems in total knee arthroplasty. Clin Orthop Relat Res. 1995;321:106–110. [PubMed] [Google Scholar]
- 28.Teter KE, Bregman D, Colwell CW., Jr The efficacy of intramedullary femoral alignment in total knee replacement. Clin Orthop Relat Res. 1995;321:117–121. [PubMed] [Google Scholar]
- 29.Townley CO. The anatomic total knee resurfacing arthroplasty. Clin Orthop Relat Res. 1985;192:82–96. [PubMed] [Google Scholar]
- 30.van Raaij TM, Brouwer RW, Reijman M, Bierma-Zeinstra SM, Verhaar JA. Conventional knee films hamper accurate knee alignment determination in patients with varus osteoarthritis of the knee. Knee. 2009;16:109–111. doi: 10.1016/j.knee.2008.10.003. [DOI] [PubMed] [Google Scholar]
- 31.Yoshioka Y, Siu D, Cooke TD. The anatomy and functional axes of the femur. J Bone Joint Surg Am. 1987;69:873–880. [PubMed] [Google Scholar]
- 32.Yoshioka Y, Siu DW, Scudamore RA, Cooke TD. Tibial anatomy and functional axes. J Orthop Res. 1989;7:132–137. doi: 10.1002/jor.1100070118. [DOI] [PubMed] [Google Scholar]