Abstract
When evaluating the role of ankle arthrodesis in the treatment of severe ankle arthritis, postoperative infection, nonunion, and the development of arthritis at the adjacent joints are major issues when considering treatment alternatives. We evaluated the rate of complications, the functional outcome, and compensatory range of motion at the midtarsal joint at medium-term followup after ankle arthrodesis with four cancellous screws. We performed 94 ankle fusions in 92 patients; 12 patients were lost to followup and eight declined to participate, leaving 72 patients (76%) for evaluation. The minimum followup was 4.8 years (mean, 5.9; range, 4.8–7.8 years). No patient developed a deep infection; three patients developed postoperative hematoma which we operatively drained. Union occurred in 93 of the 94 patients (99%). The sagittal motion at the midtarsal joint averaged 24°. Secondary arthritis of the subtalar and talonavicular joints developed during the followup period in 17% and 11%, respectively. Progression of preexisting arthritis occurred in 13 of 43 patients (30%) at the subtalar joint and five of 26 patients (19%) at the talonavicular joint. None of these patients had fusion of an adjacent joint. The average American Orthopaedic Foot and Ankle Society score increased from 36 preoperatively to 85 at followup. Ankle arthrodesis with screws provides high rates of union, reliable pain relief, and favorable functional medium-term results.
Level of Evidence: Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
In 1878, the term “arthrodesis” was first used by the Austrian surgeon Eduard Albert when he performed a surgical procedure for fusion of both knees and ankles in a 14-year-old child who had severe palsy of the lower extremities [2]. At the end of the 19th century and the beginning of the 20th century, ankle and subtalar arthrodeses were used predominantly for paralytic foot deformities, especially after poliomyelitis [24]. In the 1930s, several authors recognized ankle fusion as an option for surgical reconstruction of malunited ankle fractures with a painful incongruent talocrural joint [23, 45]. In 1951, compression arthrodesis of the ankle was introduced for the first time without bone graft and using an external fixation device, which is known as the Charnley frame [9]. More recently, open joint débridement and internal three- to four-screw compression arthrodesis [15, 21, 47, 49, 55] or arthroscopic débridement with percutaneous screw fixation [34, 38, 53] became popular because of the higher fusion rates and the lower morbidity, compared to methods using plates or external fixators [28, 33, 49, 54]. External fixation is still widely used, predominately in cases of critical soft tissues and ongoing infections [37, 50, 55].
Historically, complication rates between 9% and 60% [14, 25, 28, 33, 35, 41], nonunion rates between 5% and 37% [1, 9, 35, 55], and limitations of the activities of daily life or occupation in 33% to 50% of patients [1, 17, 18, 25] have been reported after ankle arthrodesis. These studies looked at historical techniques and thus included a high proportion of patients who had been treated with external fixation, were fused in equinus or varus malalignment, and those who underwent simultaneous fusion of adjacent joints. More recent studies that employed screw fixation and strived for fusion in neutral position of the ankle reported substantially better functional outcomes and union rates between 87% and 100% [5–7, 16, 19, 30, 42, 46–48, 53].
Over the last 20 years, total ankle replacement has evolved as a treatment alternative to arthrodesis in end-stage ankle arthritis. While comparative studies are still missing, the complication rates and medium-term functional outcomes of both procedures seem similar [20, 44]. While aseptic loosening is the most frequent reason for failure after total ankle replacement [20, 44], the development or progression of arthritis at the talonavicular and subtalar joints remains a major concern after ankle arthrodesis [4, 6, 17, 44, 55]. Long-term studies with followup of more than 20 years revealed a high percentage (ie, 47% to 100%) of arthritis at the adjacent joints [11, 17, 51]. However, only few studies reported the amount of preexisting arthritis of these joints [5, 27, 43, 48] and the clinical relevance of radiographic signs of arthritis is not entirely clear [4, 37, 51].
Therefore, we report (1) the rate of major and minor complications; (2) the union rate after ankle arthrodesis with four cancellous screws and (3) medium-term followup with the functional scores; (4) compensatory range of motion at the midtarsal joint; (5) the development or progression of osteoarthritis at the subtalar and talonavicular joints; and (6) alignment of the ankle and hindfoot.
Patients and Methods
We retrospectively reviewed all 92 patients (94 ankles) treated with a uniform technique of ankle arthrodesis using internal fixation with four screws between January 1, 1994, and December 31, 2000. We included only patients who underwent isolated ankle arthrodesis. We excluded patients who underwent additional fusion of the subtalar and/or talonavicular joints, patients treated with external fixation because of critical soft tissue conditions or underlying infection, and patients with mild degree osteoarthritis after malunited malleolar fractures treated with joint-preserving corrective osteotomies. Mean patient age at the time of surgery was 53 years (range, 34–69 years). Eighty-three of the 92 patients (90%) were treated for posttraumatic arthritis of the ankle. In all patients, nonoperative measures, such as alteration of activity or shoe wear, pain medication, and physical therapy, had failed for a minimum of 6 months prior to surgery. Twelve of the 92 patients had moved to an unknown address and eight declined to attend followup examination because they had moved to distant locations. Thus, 72 patients (72 ankles) were available for followup at a minimum of 4.8 years (average, 5.9 years; range, 4.8–7.8 years). Sixty-five of the 72 patients (90.3%) had posttraumatic arthritis, five had primary osteoarthritis (6.9%), and two patients had Charcot-Marie-Tooth disease (2.8%). Fifty-six of the 72 patients (77.8%) had initial malalignment of the talocrural axis with varus deformity greater than 5° in 47 patients, a valgus deformity greater than 10° in 10 patients, and equinus of more than 10° in nine patients.
All patients were evaluated by one of the authors (TE) pre- and postoperatively using the American Orthopaedic Foot and Ankle Society (AOFAS) ankle/hindfoot scale [29], and weight-bearing anteroposterior (with both feet in 20° of internal rotation) and lateral radiographs of both ankles. To evaluate the amount of axial deviation, a hindfoot alignment view [10] of the lower leg was obtained and the hindfoot axis with respect to the tibia measured according to Saltzman and el-Khoury [40]. The degree of arthritis at the ankle, subtalar, and talonavicular joints was documented by one of us (TE) using the radiographic scale provided by Bargon and Henkemeyer [3] (Table 1). Data on interobserver variability of this radiographic scale are not available. We performed CT scanning of the ankle and/or subtalar joint in all patients with radiographic evidence of subtalar or talonavicular arthritis at the time of initial presentation because this could influence the management plan, indicating necessity to fuse adjacent joints. We obtained MRI in cases of suspected necrosis after talar or pilon fractures to determine the subsequent need of bone grafting. In 35 patients with malunited malleolar fractures and only mild signs of posttraumatic arthritis (Bargon grade 0 to I), we performed an initial arthroscopy or arthrotomy of the ankle to evaluate the quality of weight-bearing cartilage. In 29 of these 35 patients viable cartilage was still present, therefore peritalar osteotomies or anatomic repair of a chronic unstable distal tibiofibular syndesmosis were preferred as joint-preserving procedures [31, 36, 54]. These patients are not included in the present study.
Table 1.
Radiographic grading of ankle arthrosis according to Bargon and Henkemeyer [3]
| Grade | Description |
|---|---|
| 0 | No radiographic signs of arthritis |
| I | Subchondral sclerosis, osteophytes, mild joint space narrowing |
| II | Focal joint space narrowing and obliteration the subchondral bone lamella |
| III | Defects and cysts within the subchondral bone lamella, marked joint space narrowing |
All patients underwent an ankle arthrodesis with débridement and fusion using the four-screw fusion technique, first described by the senior author (HZ [55]). The patient was positioned supine with a thigh tourniquet that was inflated to between 200 and 300 mm Hg depending on the individual weight. We approached the ankle midline through a 6- to 8-cm-long longitudinal incision close to the medial border of the anterior tibial tendon (Fig. 1A–B). Care was taken to avoid injury to the medial dorsal cutaneous nerve, which may cross over the distal incision medially. We incised the proximal extensor retinaculum in a Z-shaped manner to allow easier reapproximation at the end of the operation. The anterior tibial artery and veins and the deep peroneal nerve were held away laterally with the extensor hallucis longus and extensor digitorum longus tendons (Fig. 2A–B). The anterior joint capsule and any existing osteophytes were resected. A generous débridement and removal of all sclerotic and nonviable bone was performed with osteotomes, curettes, and a rongeur. A midsized laminar spreader was placed between tibia and talus first laterally, then medially to allow complete débridement of the posterior aspect of the ankle, as well as the medial and lateral gutters. To determine adequate joint resection, we deflated the tourniquet at that time to ensure that a bleeding bone surface was exposed. Defects in 38 of 94 cases were grafted with autologous bone, especially in case of varus malposition of the talus or in the presence of avascular necrosis at the talar dome or lateral tibial plafond. A monocortical bone block was taken from the ipsilateral iliac crest and additional cancellous bone chips were interposed (Fig. 3A–B). In 21 cases of shortening of the distal tibia of more than 5 mm after correcting frontal malalignment, a shortening osteotomy of the distal fibula was performed to avoid calcaneofibular impingement. In 10 patients with marked equinus of more than 10° we performed percutaneous lengthening of the Achilles tendon to achieve correction. A roll of sheets below the distal tibia served as a fulcrum for forced reduction of the foot with respect to the tibial axis to avoid anteversion of the talus. The ankle was fixed temporarily with a 2.5-mm Kirschner wire (Fig. 4A–B). Proper positioning of the center of the talar body below the longitudinal axis of the tibia in both planes, correction of equines, and frontal (varus/valgus) malalignment were assessed fluoroscopically. The arthrodesis was fixed with four 6.5-mm cancellous lag screws as described previously [15, 55]. Two screws were inserted parallel from the anterior aspect of the distal tibia into the body of the talus (Fig. 5A–D). The third, mechanically most important, screw was inserted through a posteromedial stab incision approximately 3 cm proximal to the tip of the medial malleolus. The screw was inserted into the anterolateral portion of the talar head. The fourth screw was inserted percutaneously from the posterolateral aspect of the distal fibula approximately 1.5 cm proximal to the tip of the lateral malleolus into the dorsal portion of the talar body. In the presence of greater defects or osteopenic bone, fully threaded 6.5-mm screws were used. If a manifest syndesmotic instability was present at the time of fusion, a fifth screw was introduced as a tibiofibular set screw approximately 1.5 cm above and parallel to the tibial plafond. In four patients with a known or suspected allergy to components of surgical steel (cobalt, chromium, or nickel), we used titanium screws. Correct screw length and realignment of the ankle position was assessed by intraoperative anteroposterior and lateral radiographs of the ankle (Fig. 6A–D). The wound was closed in layers over a suction drain with reapproximation of the extensor retinaculum.
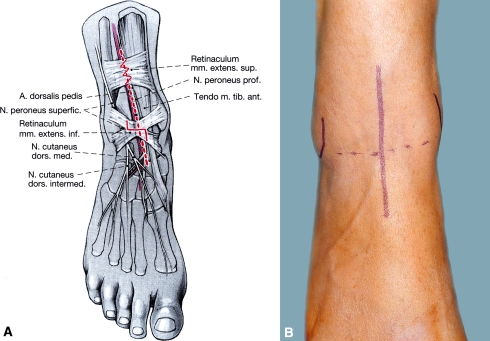
Fig. 1A–B.
(A) The ankle is approached through an anterior midline approach, 6 to 8 cm in length. (Reprinted with permission from Endres T, Grass R, Rammelt S, Zwipp H. Ankle arthrodesis with four cancellous lag screws [in German]. Oper Orthop Traumatol. 2005;17:345–360.) (B) The superior extensor retinaculum is incised in a Z-shaped manner. The skin incision extends further proximally from the joint level (dotted line) than distally.
Fig. 2A–B.
(A) The joint is exposed between the anterior tibial and extensor hallucis longus tendons. (Reprinted with permission from Endres T, Grass R, Rammelt S, Zwipp H. Ankle arthrodesis with four cancellous lag screws [in German]. Oper Orthop Traumatol. 2005;17:345–360.) (B) The intraoperative aspect of the ankle displays end-stage arthrosis with only a minimum amount of cartilage left (*).
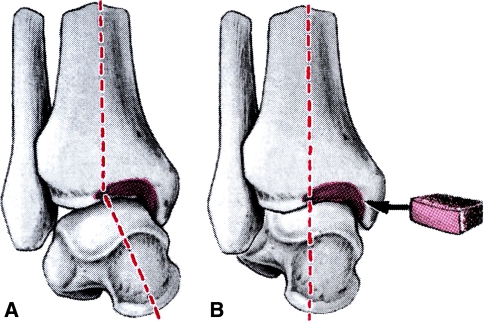
Fig. 3A–B.
(A) Preoperative varus malposition of the talus must be corrected. (B) This may necessitate the interposition of a monocortical bone graft. (Reprinted with permission from Endres T, Grass R, Rammelt S, Zwipp H. Ankle arthrodesis with four cancellous lag screws [in German]. Oper Orthop Traumatol. 2005;17:345–360.)
Fig. 4A–B.
(A) Anterior translation of the talus is regularly found. (B) It must be corrected intraoperatively by shifting the talar center back into the longitudinal axis of the tibia. The position is held temporarily with a 2.5-mm Kirschner wire and controlled fluoroscopically. (Reprinted with permission from Endres T, Grass R, Rammelt S, Zwipp H. Ankle arthrodesis with four cancellous lag screws [in German]. Oper Orthop Traumatol. 2005;17:345–360.)
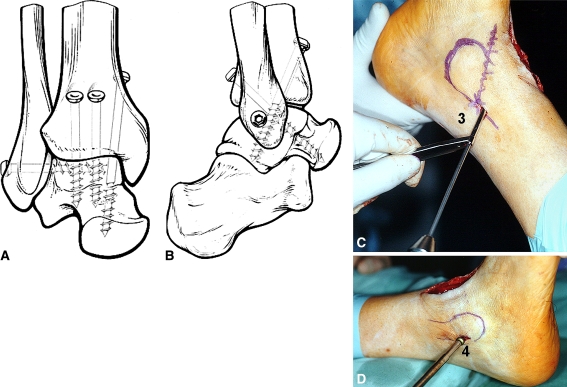
Fig. 5A–D.
(A) Fixation of the arthrodesis is achieved with four-screws. (Reprinted with permission and ©Springer from Fig. 2A in Zwipp H, Grass R, Rammelt S, Dahlen C. Arthrodese—Pseudarthrosen am Sprunggelenk. Die fehlgeschlagene Arthrodese [in German]. Chirurg. 1999;70:1216–1224.) (B) The two anterior screws (1, 2) are inserted from the open approach. (Reprinted with permission and ©Springer from Fig. 2B in Zwipp H, Grass R, Rammelt S, Dahlen C. Arthrodese—Pseudarthrosen am Sprunggelenk. Die fehlgeschlagene Arthrodese [in German]. Chirurg. 1999;70:1216–1224.) (C) The posterior-medial screw (3) is inserted percutaneously from behind the medial malleolus. (D) The lateral screw (4) is inserted percutaneously from the distal fibula.
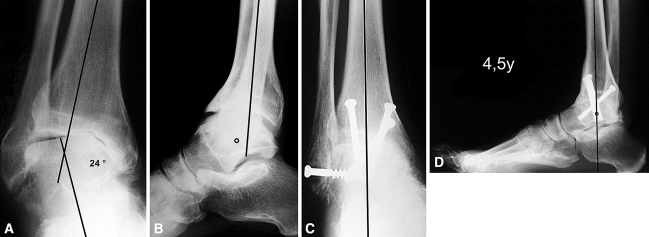
Fig. 6A–D.
A 57 year old patient presented with idiopathic ankle arthritis and gradually developing pain and malalignment. (A) The preoperative radiographs show a severe varus malposition in the coronal plane and (B) a considerable anterior translation of the talus with respect to the tibia. (C) AP and (D) lateral weightbearing radiographs at a followup of 4.5 years after corrective ankle arthrodesis show solid fusion and reorientation of the talus in both planes without signs of subtalar or talonavicular arthritis.
The postoperative management aimed at early functional rehabilitation. The suction drain was typically removed after 2 days. Active and passive motion of the subtalar and midtarsal joints was begun on the second postoperative day while temporarily removing the cast. A split short-leg cast was applied for the period of wound healing only, typically 5 to 9 days. Following that time, 60 of 92 patients were treated postoperatively with an arthrodesis boot with rigid medial and lateral struts and a flexible sole (Variostabil®, Adidas, Herzogenaurach, Germany) allowing early full weight bearing as tolerated, usually after 2 to 3 weeks; otherwise, partial weightbearing of 20 kg was recommended for 6 to 8 weeks, the longer period being necessary after bone grafting. Ten patients were treated with partial weightbearing of 20 kg in their regular shoes. Twenty-two patients were placed in a short-leg cast for 6 weeks with partial weight bearing because of osteopenic bone quality or extensive bone grafting. Weightbearing was increased gradually after removal of the cast. All patients were given daily injections of low-molecular-weight heparin (eg, dalteparin, enoxaparin) until full weight bearing was achieved.
Patients were routinely seen at 6 weeks, and at 3, 6, and 12 months postoperatively for a complete physical examination, to assess bony union and determine weight-bearing status individually as detailed above. Union was verified by obliteration of the joint space and trabecular continuity from the tibia to the talus on lateral and anteroposterior weight-bearing radiographs of the ankle.
Nonunion was defined as radiographic evidence of incomplete fusion more than 9 months after surgery. All postoperative complications were noted. We defined major complications as deep soft tissue infection, osteomyelitis, and malunion or nonunion. Minor complications included superficial wound dehiscence, wound edge necrosis, or hematoma without signs of infection.
At final followup, patients were examined clinically for alignment and range of motion in the midtarsal (Chopart) joint. The functional results were evaluated by one of the authors (TE) with the AOFAS ankle/hindfoot scale [29]. Anteroposterior and lateral weight-bearing radiographs of the ankle and a hindfoot alignment view of the lower leg [10] were obtained to evaluate bone healing, the amount of arthritis in the adjacent joints as graded on the Bargon scale [3], and tibiotalar alignment. We measured sagittal motion at the midtarsal joint with lateral radiographs with the foot in dorsiflexion and plantarflexion (Fig. 7A−J).
Fig. 7A–J.
A 44-year-old woman presented with severe posttraumatic arthritis 2 years after an operatively treated trimalleolar fracture-dislocation. On preoperative radiographs she had (A) varus malunion of the talus with (B) anterior translation. (C) The intraoperative anteroposterior and (D) lateral radiographs show correct alignment and screw position at the time of ankle arthrodesis. Stress radiographs at followup display a (E) dorsiflexion of 8° and (F) plantar flexion of 36° at the midtarsal (Chopart) joint. Clinical followup shows (G) the compensatory dorsiflexion and (H) plantarflexion of the midtarsal joint in the sagittal plane. There is also (I) near-normal eversion and (J) inversion of the hindfoot at the triple joint complex in the coronal plane.
Results
Minor wound healing problems, such as superficial wound dehiscence or wound edge necrosis, were seen in five of 94 cases (5%). All responded to nonoperative measures, such as observation, rest, and antiseptic dressings. Three patients (3%) had a postoperative hematoma for which we performed a single drainage with subsequent resolution. We observed no deep soft tissue infections and no patient with subsequent osteomyelitis.
Union was achieved in 93 of the 94 patients (99%). One patient with nonunion had repeat arthrodesis with bone grafting 9 months after surgery and healed uneventfully.
At final followup at an average of 5.9 years, the mean AOFAS ankle/hindfoot score [29] had increased to 85 from a mean preoperative value of 36. Sixty-nine of 72 (96%) patients stated that given the same circumstances as before the arthrodesis they would undergo surgery again.
The mean sagittal arc of motion at the midtarsal (Chopart) joint as measured radiographically was 24° (standard deviation 16°).
At last followup, radiographic signs of arthritis had developed or progressed in 25 of 72 patients (35%) at the subtalar joint and in 13 of 72 patients (18%) at the talonavicular joint. Among those, secondary arthritis at the subtalar joint had developed during the followup period in 12 patients (17%) and in eight patients (11%) at the talonavicular joint. Progression of preexisting arthritis by at least one grade on the Bargon scale [3] was noted in 13 of 43 patients (30%) at the subtalar joint and five of 26 patients (19%) at the talonavicular joint. None of these patients had fusion of either of these joints.
One patient with Charcot-Marie-Tooth disease developed loss of correction. At final followup at 5 years postoperatively he had a malalignment in varus of 10°. The patient declined further surgery because he was relatively pain free, probably due to his underlying neuropathic disease. Seven of the 72 patients had a mild residual varus deformity of up to 5°, three patients had a hindfoot valgus up to 10°, and one patient had 10° of equinus at the time of followup. The AOFAS scores in these patients did not differ from the other patients and all except the patient with a residual equinus were satisfied with the clinical result.
Discussion
Ankle arthrodesis is an established treatment method for end-stage symptomatic ankle arthritis with many internal and external fixation techniques being described. When evaluating the value of ankle fusion compared with alternative treatment options, infection and nonunion rates in the short term and the development of arthritis in adjacent joints in the medium to long term are major issues. We therefore evaluated the rates of complications and union after a standardized isolated ankle arthrodesis with internal fixation using four screws. We report the functional outcome, patient satisfaction, compensatory range of motion at the midtarsal joint, the development or progression of osteoarthritis at the subtalar and talonavicular joints, and realignment of the ankle and hindfoot at a minimum of 4.8 years followup.
Readers should be aware of the limitations of our study. First is the medium-term followup. While a longer followup period would have been desirable, long-term studies necessarily include many patients treated with historical methods that may lead to less satisfactory results [11, 17]. Although there is evidence from one longitudinal study, that long-term outcome (23 years) does not differ from medium-term outcome (7 years) in the same patient population [51], arthritis at the adjacent joints may develop or further progress over time. Second is the loss to followup in 22% of patients (20 of 92). Loss to followup is unavoidable with many patients being referred to our center from distant locations. Nonetheless, we report one of the largest cohorts in the literature treated with a single method of fixation (Table 2).
Table 2.
Main findings in relevant studies during the last 10 years after ankle arthrodesis that employed at least partly internal fixation with screws
| Author | Number of ankles followed | Method of fixation | Average followup (years, months) | Union rate (%) | Wound healing problems (%) | Deep infection rate (%) | Functional outcome assessment (score with a maximum of 100) | Alignment, remarks |
|---|---|---|---|---|---|---|---|---|
| Ben Amor et al. [4] | 36 | 80% internal fixation, 20% external fixation | 8 years, 6 months | 97 | 56.2 (Duquennoy) | Significantly more subtalar pain with fusion in equinus >5° (12 patients) | ||
| Takakura et al. [46] | 43 | Anterior sliding bone graft, internal fixation | 7 years, 2 months | 93 | 7 | 0 | 77.9 (Takakura) | Hindfoot fixed in varus in 34 ankles (81%) |
| Coester et al. [11] | 23 | Arthrodesis by external or internal fixation | 22 years | # | Fusion in varus/valgus malalignment in 74%, mean equinus of 4° (versus unaffected side) | |||
| Bertrand et al. [5] | 23 | 84% internal fixation, 16% external fixation | 12 years, 9 months | 87 | 69.7 (Duquennoy) | Inferior results with fusion in equinus or valgus >5° | ||
| Kopp et al. [30] | 41 | Internal fixation with staples and screws | 7 years, 3 months | 93 | 4.9 | 2.4 | 72.8 (Mazur) | |
| Fuchs et al. [17] | 18 | 22% internal fixation, 78% external fixation | 20 years | 95 | † | 59.4 (Olerud & Molander) | 15/18 feet in > 5° equinus, 8/18 with varus/valgus | |
| Buchner & Sabo [6] | 45 | 38% internal fixation, 62% external fixation | 9 years, 3 months | 92 | 23 | 8 | 73.6 (AOFAS) | Fusion in more than 5° of equinus (38 patients) associated with worse outcome |
| Winson et al. [53] | 105 | Arthroscopic arthrodesis, followup by telephone interview | 5 years, 5 months | 92.4 | 3 | 1 | One stress fracture with fusion in equinus | |
| Ferkel & Hewitt [16] | 35 | Arthroscopic arthrodesis | 6 years | 97 | 0 | 0 | 73.9 (Mazur) | |
| Kennedy et al. [27] | 41 | Internal fixation with screws | 8 years 7 months | 95 | 2.4 | 0 | 80.6 (AOFAS) | One tibial stress fracture, one CRPS, 38 of 41 ankles with correct alignment |
| Thomas et al. [48] | 26 | Internal fixation with transfibular approach | 3 years, 8 months | 100 | 74 (AOFAS) | Mean tibiotalar angle 103° (range, 93° to 115°) | ||
| Trichard et al.[51] | 25 | 60% internal fixation, 40% external fixation | 23 years | # | 64.7 (Duquennoy) | 13 ankles with some degree of malalignment | ||
| Smith & Wood [42] | 25 | Internal fixation | 1 year, 10 months | 96 | 4 | 0 | 43.7 (AOFAS) | Residual varus or valgus deformity of >5° in seven ankles |
| Colman & Pomeroy [12] | 48 | Transfibular approach with onlay grafting | 3 years, 9 months | 96 | 6 | 0 | 69 (AOFAS) | 24 ankles with preoperative deformity were corrected |
| Zwipp et al. [current study] | 72 | Standard screw technique | 5 years, 11 months | 98.9 | 5.3 | 0 | 84.7 (AOFAS) | Varus malalignment in one case (1.3%) |
# Not explicitly stated, but no non-unions reported.
† Seven infections overall; four patients had been treated with ankle arthrodesis for chronic infections.
With the reported technique, using an anterior midline approach and a four-screw technique with two screws introduced percutaneously, only minor complications occurred in 12% patients. All went on to uneventful healing. The still frequently cited historic complication rates after ankle arthrodesis have varied considerably between 9% and 60%. They stem from earlier studies in the 1960s and ’70s that reported ankle fusion with external fixation and included infected cases at the time of fusion [25, 28, 33, 35, 41]. Recent studies with open and percutaneous techniques of internal fixation report substantially lower complication rates that compare with our study (Table 2).
Union rate with our technique was 99% which is in keeping with the recent literature with union rates ranging from 87% to 100% (Table 2). We agree with other authors that judicious resection of remaining cartilage, sclerotic and nonviable bone while preserving the bone contours results in a highly stable fusion and avoids rotational malalignment [27, 34, 47, 55].
Patients with ankle arthritis usually seek care for pain and disability. Sixty-nine of our 72 patients (96%) stated that given the same circumstances as preoperatively they would undergo surgery again. The functional results as measured with the AOFAS score improved substantially as compared to the preoperative values and compare well to the recent literature (Table 2). Similarly, other authors have reported that between 88% and 98% of patients would undergo ankle arthrodesis again [11, 27]. This probably reflects the patients’ subjective relief of long-standing pain and disability despite residual functional restrictions. This effect has also been observed in corrective fusion of the subtalar joint [39].
Residual function after ankle fusion greatly depends on compensatory motion of the adjacent joints. In the present study, the total sagittal motion of the foot at the midtarsal (Chopart) joint averaged 24°. Several studies have described residual sagittal motion between 13° and 24° over the medium to long term [1, 5, 32, 34, 46] while others have noted stiffness at the subtalar and midtarsal joints, at least in a proportion of patients, after ankle arthrodesis [4, 6, 7, 25, 46]. We concur with Takakura et al. [46] that shorter periods of immobilization (about 6 weeks) after ankle arthrodesis will lead to increased range of motion at the subtalar and midtarsal joints as compared with longer immobilization times of 12 to 15 weeks [5, 6, 42]. The arthrodesis boot used in our study protects the ankle against varus and valgus stress with rigid struts while allowing some sagittal motion of the midfoot with partial or full weight bearing because of the flexible sole. Early weight bearing after 2 to 3 weeks as tolerated in compliant patients without extensive bone grafting and with normal bone quality does not prevent a high rate of union [8]. In addition, we advocate early active and passive motion of the midtarsal and subtalar joints.
Ankle fusion puts greater strain on the adjacent joints which may lead to the development or progression of arthritis [7, 26, 32]. During the followup period, we observed development of arthritis at the subtalar joint in 16.6% and at the talonavicular joint in 11.1% of patients and progression of preexisting arthritis 30% and 19%, respectively. Our observations confirm those of Sheridan et al. [43] who reported a high percentage (96%) of subtalar and midfoot arthritis was preexisting due to ankle malfunction in end-stage arthritis. Progression of preexisting arthritis has been reported in between 0 and 70% [5, 27, 30, 48]. Several long-term studies have reported high overall rates of subtalar arthritis of between 47% and 100% [4, 6, 11, 17]. All of these studies included a substantial portion of ankles that were fused in either varus/valgus or equinus. There is consensus in the literature that a neutral position in the sagittal plane and neutral to slight valgus in the coronal plane is essential for a satisfactory functional outcome and puts less strain on adjacent joints including the knee [1, 7, 32, 52]. Conti and Walter observed a correlation of arthritic changes at the midfoot and fusion in plantar flexion [13].
The clinical relevance of radiographic signs of arthritis at the subtalar and talonavicular joints is not well-established [37]. While some authors [6, 17] noted a worse clinical outcome in the presence of subtalar arthritis, patient satisfaction was still high in these studies. Trichard et al. [51] reported less than 1/3, Kennedy et al. [27] found one in seven, and Ben Amor et al. [4] found none of them clinically relevant. Consequently, only a small proportion of the patients with radiographic subtalar arthritis [27, 51]—and none of our patients—had an additional fusion of either of these joints.
Several clinical studies have reported a correlation between radiographic alignment of the fused ankle and functional outcome [1, 5, 6, 13, 35, 46]. We believe that the favorable outcomes in our study are partly attributable to alignment. The one patient with residual equinus of 10° had a low outcome score and another patient with loss of correction was relatively pain-free probably because of his neuropathy. We presumed the best position for ankle arthrodesis was neutral flexion of the foot in the sagittal plane, neutral to slight valgus (5°) in the coronal plane, and 5° to 10° external rotation in the horizontal plane with the talus centered exactly below the tibia [7, 22, 32, 48]. These recommendations from clinical outcome studies could be substantiated by a wealth of studies employing further measurements like gait analyses and pressure measurements of the subtalar joint [7, 15, 34, 47, 52, 55]. It is assumed that less favorable outcomes and high rates of subtalar arthritis in historical and long-term studies result from fusion in malalignment [1, 4–7, 11, 17, 32].
We conclude from our data and the literature that ankle arthrodesis with screws in neutral alignment provides a reasonable treatment for symptomatic ankle arthritis with high rates of union, low complication rates, and favorable functional outcome in the medium-term. Despite some development and progression of arthritis in the subtalar and talonavicular joints there was no need for subsequent fusions. Hypermobility of the midtarsal joint can partially compensate for the loss of sagittal motion.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
References
- 1.Abdo RV, Wasilewski SA. Ankle arthrodesis: a long-term study. Foot Ankle. 1992;13:307–312. doi: 10.1177/107110079201300602. [DOI] [PubMed] [Google Scholar]
- 2.Albert E. Zur Resektion des Kniegelenkes. Wien Med Press. 1879;20:705–708. [Google Scholar]
- 3.Bargon G, Henkemeyer H. Long-term radiological and clinical observations following surgery for injuries to the tibio-fibular syndemosis after malleolar fractures [in German] Fortsch Röntgenstr. 1977;126:543–545. doi: 10.1055/s-0029-1230633. [DOI] [PubMed] [Google Scholar]
- 4.Ben Amor H, Kallel S, Karray S, Saadaoui F, Zouari M, Litaiem T, Douik M. Consequences of tibiotalar arthrodesis on the foot. A retrospective study of 36 cases with 8.5 years of followup [in French] Acta Orthop Belg. 1999;65:48–56. [PubMed] [Google Scholar]
- 5.Bertrand M, Charissoux JL, Mabit C, Arnaud JP. Tibio-talar arthrodesis: long term influence on the foot [in French] Rev Chir Orthop Reparatrice Appar Mot. 2001;87:677–684. [PubMed] [Google Scholar]
- 6.Buchner M, Sabo D. Ankle fusion attributable to posttraumatic arthrosis: a long-term followup of 48 patients. Clin Orthop Relat Res. 2003;406:155–164. doi: 10.1097/00003086-200301000-00025. [DOI] [PubMed] [Google Scholar]
- 7.Buck P, Morrey BF, Chao EY. The optimum position of arthrodesis of the ankle. J Bone Joint Surg Am. 1987;69:1052–1062. [PubMed] [Google Scholar]
- 8.Cannon LB, Brown J, Cooke PH. Early weightbearing is safe following arthroscopic ankle arthrodesis. Foot Ankle Surg. 2004;10:135–139. doi: 10.1016/j.fas.2004.06.001. [DOI] [Google Scholar]
- 9.Charnley J. Compression arthrodesis of the shoulder and ankle. Orthop Clin North Am. 1951;20:709–721. [Google Scholar]
- 10.Cobey JC. Posterior roentgenogram of the foot. Clin Orthop Relat Res. 1976;118:202–207. [PubMed] [Google Scholar]
- 11.Coester LM, Saltzman CL, Leupold J, Pontarelli W. Long-term results following ankle arthrodesis for post-traumatic arthritis. J Bone Joint Surg Am. 2001;83:219–228. doi: 10.2106/00004623-200102000-00009. [DOI] [PubMed] [Google Scholar]
- 12.Colman AB, Pomeroy GC. Transfibular ankle arthrodesis with rigid internal fixation: an assessment of outcome. Foot Ankle Int. 2007;28:303–307. doi: 10.3113/FAI.2007.0303. [DOI] [PubMed] [Google Scholar]
- 13.Conti RJ, Walter JH. Effects of ankle arthrodesis on the subtalar and midtarsal joints. J Foot Ankle Surg. 1990;29:334–336. [PubMed] [Google Scholar]
- 14.Davis RJ, Millis MB. Ankle arthrodesis in the management of traumatic ankle arthrosis: a long-term retrospective study. J Trauma. 1980;20:674–678. doi: 10.1097/00005373-198008000-00007. [DOI] [PubMed] [Google Scholar]
- 15.Endres T, Grass R, Rammelt S, Zwipp H. Ankle arthrodesis with four cancellous lag screws [in German] Oper Orthop Traumatol. 2005;17:345–360. doi: 10.1007/s00064-005-1147-x. [DOI] [PubMed] [Google Scholar]
- 16.Ferkel RD, Hewitt M. Long-term results of arthroscopic ankle arthrodesis. Foot Ankle Int. 2005;26:275–280. doi: 10.1177/107110070502600402. [DOI] [PubMed] [Google Scholar]
- 17.Fuchs S, Sandmann C, Skwara A, Chylarecki C. Quality of life 20 years after arthrodesis of the ankle. A study of adjacent joints. J Bone Joint Surg Br. 2003;85:994–998. doi: 10.1302/0301-620X.85B7.13984. [DOI] [PubMed] [Google Scholar]
- 18.Fuller JE, Rostrup O, Huckell JR. Ankle arthrosis—a clinical review. In: Proceedings of the Canadian Orthopaedic Association. J Bone Joint Surg Br. 1974;56:587.
- 19.Glick JM, Morgan CD, Myerson MS, Sampson TG, Mann JA. Ankle arthrodesis using an arthroscopic method: long-term follow-up of 34 cases. Arthroscopy. 1996;12:428–434. doi: 10.1016/s0749-8063(96)90036-5. [DOI] [PubMed] [Google Scholar]
- 20.Haddad SL, Coetzee JC, Estok R, Fahrbach K, Banel D, Nalysnyk L. Intermediate and long-term outcomes of total ankle arthroplasty and ankle arthrodesis. A systematic review of the literature. J Bone Joint Surg Am. 2007;89:1899–1905. doi: 10.2106/JBJS.F.01149. [DOI] [PubMed] [Google Scholar]
- 21.Hansen ST., Jr . Functional Reconstruction of the Foot and Ankle. Philadelphia: Lippincott Williams & Wilkins; 2000. [Google Scholar]
- 22.Hefti FL, Baumann JU, Morscher EW. Ankle joint fusion: determination of optimal position by gait analysis. Arch Orthop Trauma Surg. 1980;96:187–195. doi: 10.1007/BF00457782. [DOI] [PubMed] [Google Scholar]
- 23.Henderson MS, Stuck WG. Fractures of the ankle: recent and old. J Bone Joint Surg. Am. 1933;15:882–888. [Google Scholar]
- 24.Hohmann G. Foot and Leg [in German] München, Germany: Bergmann; 1948. [Google Scholar]
- 25.Johnson EW, Boseker EH. Arthrodesis of the ankle. Arch Surg. 1968;97:766–773. doi: 10.1001/archsurg.1968.01340050106015. [DOI] [PubMed] [Google Scholar]
- 26.Jung H-G, Parks BG, Nguyen A, Schon LC. Effect of tibiotalar joint arthrodesis on adjacent tarsal joint pressure in a cadaver model. Foot Ankle Int. 2007;28:103–108. doi: 10.3113/FAI.2007.0019. [DOI] [PubMed] [Google Scholar]
- 27.Kennedy JG, Hodgkins CW, Brodsky A, Bohne WH. Outcomes after standardized screw fixation technique of ankle arthrodesis. Clin Orthop Relat Res. 2006;447:112–118. doi: 10.1097/01.blo.0000203480.04174.0e. [DOI] [PubMed] [Google Scholar]
- 28.Kitaoka HB, Anderson PJ, Morrey BF. Revision of ankle arthrodesis with external fixation for malunion. J Bone Joint Surg Am. 1992;74:1191–1198. [PubMed] [Google Scholar]
- 29.Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. Clinical rating systems for the ankle, hindfoot, midfoot, hallux and lesser toes. Foot Ankle Int. 1994;15:349–353. doi: 10.1177/107110079401500701. [DOI] [PubMed] [Google Scholar]
- 30.Kopp FJ, Banks MA, Marcus RE. Clinical outcome of tibiotalar arthrodesis utilizing the chevron technique. Foot Ankle Int. 2004;25:225–230. doi: 10.1177/107110070402500406. [DOI] [PubMed] [Google Scholar]
- 31.Marti RK, Raaymakers ELFB, Rammelt S. Reconstruction of malunited malleolar fractures [in German] Fuß und Sprunggelenk. 2009;7:78–87. doi: 10.1016/j.fuspru.2009.03.014. [DOI] [Google Scholar]
- 32.Mazur JM, Schwartz E, Simon SR. Ankle arthrodesis. Long-term follow-up with gait analysis. J Bone Joint Surg Am. 1979;61:964–975. [PubMed] [Google Scholar]
- 33.Moeckel BH, Patterson BM, Inglis AE, Sculco TP. Ankle arthrodesis. A comparison of internal and external fixation. Clin Orthop Relat Res. 1991;268:78–83. [PubMed] [Google Scholar]
- 34.Morgan CD, Henke JA, Bailey RW, Kaufer H. Long-term results of tibiotalar arthrodesis. J Bone Joint Surg Am. 1985;67:546–550. [PubMed] [Google Scholar]
- 35.Morrey BF, Wiedemann GP. Complications and long-term results of ankle arthrodesis following trauma. J Bone Joint Surg Am. 1980;62:777–784. [PubMed] [Google Scholar]
- 36.Neumann HW, Lieske S, Schenk K. Supramalleolar, subtractive valgus osteotomy of the tibia in the management of ankle joint degeneration with varus deformity [in German] Oper Orthop Traumatol. 2007;19:511–526. doi: 10.1007/s00064-007-1025-7. [DOI] [PubMed] [Google Scholar]
- 37.Nihal A, Gellman RE, Embil JM, Trepman E. Ankle arthrodesis. Foot Ankle Surg. 2008;14:1–10. doi: 10.1016/j.fas.2007.08.004. [DOI] [PubMed] [Google Scholar]
- 38.Ogilvie-Harris DJ, Lieberman I, Fitsialos D. Arthroscopically assisted arthrodesis for osteoarthrotic ankles. J Bone Joint Surg Am. 1993;75:1167–1174. doi: 10.2106/00004623-199308000-00006. [DOI] [PubMed] [Google Scholar]
- 39.Rammelt S, Grass R, Zawadski T, Biewener A, Zwipp H. Foot function after subtalar distraction bone block arthrodesis—a prospective study. J Bone Joint Surg Br. 2004;86:659–668. doi: 10.1302/0301-620X.86B5.14205. [DOI] [PubMed] [Google Scholar]
- 40.Saltzman CL, el-Khoury GY. The hindfoot alignment view. Foot Ankle Int. 1995;16:572–576. doi: 10.1177/107110079501600911. [DOI] [PubMed] [Google Scholar]
- 41.Scranton PE, Fu FH, Brown TD. Ankle arthrodesis: a comparative clinical and biomechanical evaluation. Clin Orthop Relat Res. 1980;151:234–243. [PubMed] [Google Scholar]
- 42.Smith R, Wood PL. Arthrodesis of the ankle in the presence of a large deformity in the coronal plane. J Bone Joint Surg Br. 2007;89:615–619. doi: 10.2106/JBJS.F.00615. [DOI] [PubMed] [Google Scholar]
- 43.Sheridan BD, Robinson DE, Hubble MJ, Winson IG. Ankle arthrodesis and its relationship to ipsilateral arthritis of the hind- and mid-foot. J Bone Joint Surg Br. 2006;88:206–207. doi: 10.1302/0301-620X.88B2.17065. [DOI] [PubMed] [Google Scholar]
- 44.SooHoo NF, Zingmond DS, Ko CY. Comparison of reoperation rates following ankle arthrodesis and total ankle arthroplasty. J Bone Joint Surg Am. 2007;89:2143–2149. doi: 10.2106/JBJS.F.01611. [DOI] [PubMed] [Google Scholar]
- 45.Speed JS, Boyd MB. Operative reconstruction of malunion about the ankle joint. J Bone Joint Surg. 1936;18:270–278. [Google Scholar]
- 46.Takakura Y, Tanaka Y, Sugimoto K, Akiyama K, Tamai S. Long-term results of arthrodesis for osteoarthritis of the ankle. Clin Orthop Relat Res. 1999;361:178–185. doi: 10.1097/00003086-199904000-00023. [DOI] [PubMed] [Google Scholar]
- 47.Thermann H, Hüfner T, Roehler A, Tscherne H. Screw arthrodesis of the ankle joint. Technique and outcome [in German] Orthopäde. 1996;25:166–176. [PubMed] [Google Scholar]
- 48.Thomas R, Daniels TR, Parker K. Gait analysis and functional outcomes following ankle arthrodesis for isolated ankle arthritis. J Bone Joint Surg Am. 2006;88:526–535. doi: 10.2106/JBJS.E.00521. [DOI] [PubMed] [Google Scholar]
- 49.Thordarson DB, Markolf K, Cracchiolo A. Stability of an ankle arthrodesis fixed by cancellous-bone screws compared with that fixed by an external fixator. J Bone Joint Surg Am. 1992;74:1050–1055. [PubMed] [Google Scholar]
- 50.Trepman E, Nihal A, Pinzur MS. Charcot neuropathy of the foot and ankle. Foot Ankle Int. 2005;26:46–63. doi: 10.1177/107110070502600109. [DOI] [PubMed] [Google Scholar]
- 51.Trichard T, Remy F, Girard J, Soenen M, Duquennoy A, Migaud H. Long-term behavior of ankle fusion: assessment of the same series at 7 and 23 years (19–36 years) follow-up [in French] Rev Chir Orthop Reparatrice Appar Mot. 2006;92:701–707. doi: 10.1016/s0035-1040(06)75931-1. [DOI] [PubMed] [Google Scholar]
- 52.Wang CL, Cheng CK, Chen CW, Lu CM, Hang YS, Liu TK. Contact areas and pressure distributions in the subtalar joint. J Biomech. 1995;28:269–279. doi: 10.1016/0021-9290(94)00076-G. [DOI] [PubMed] [Google Scholar]
- 53.Winson IG, Robinson DE, Allen PE. Arthroscopic ankle arthrodesis. J Bone Joint Surg Br. 2005;87:343–347. doi: 10.1302/0301-620X.87B3.15756. [DOI] [PubMed] [Google Scholar]
- 54.Zwipp H. Foot Surgery [in German] Vienna, Austria: Springer Verlag; 1994. [Google Scholar]
- 55.Zwipp H, Grass R, Rammelt S, Dahlen C. Arthrodesis–non-union of the ankle. Arthrodesis failed [in German] Chirurg. 1999;70:1216–1224. doi: 10.1007/s001040050773. [DOI] [PubMed] [Google Scholar]