Abstract
Determining an older adult’s capacity to live safely and independently in the community presents a serious and complicated challenge to the health care system. Evaluating one’s ability to make and execute decisions regarding safe and independent living incorporates clinical assessments, bioethical considerations, and often legal declarations of capacity. Capacity assessments usually result in life changes for patients and their families, including a caregiver managing some everyday tasks, placement outside of the home, and even legal guardianship. The process of determining capacity and recommending intervention is often inefficient and highly variable in most cases. Physicians are rarely trained to conduct capacity assessments and assessment methods are heterogeneous. An interdisciplinary team of clinicians developed the capacity assessment and intervention (CAI) model at a community outpatient geriatrics clinic to address these critical gaps. This report follows one patient through the entire CAI model, describing processes for a typical case. It then examines two additional case reports that highlight common challenges in capacity assessment. The CAI model uses assessment methods common to geriatrics clinical practice and conducts assessments and interventions in a standardized fashion. Reliance on common, validated measures increases generalizability of the model across geriatrics practice settings and patient populations.
Keywords: capacity assessment and intervention (CAI) model, safety in independent-living
1. Introduction
Older adults commonly report living safely and independently in their own home as one of their major life goals (Naik et al., 2005). Assessment of one’s ability to live independently is an important priority for health care professionals caring for older adults, perhaps as important as managing medical comorbidities (Schulman-Green et al., 2006; Huang et al., 2007). Assessment is difficult, however, as living independently involves multiple functional domains. As people age, they face a variety of physical, mental, and social challenges. Even minor deficits in several domains can present as a significant functional disability (Naik et al., 2006). Cognitive function, affect and judgment are important for safe and independent living, and deficits in these domains are linked to impaired executive control function (the ability to perform complex, goal-directed behavior) (Workman et al., 2000). Impairments in executive control function limit one’s ability to implement plans of actions related to everyday living and execute choices that maintain one’s safety when encountering unexpected circumstances (Workman et al., 2000).
Assessing the capacity to make and execute decisions is a central aspect of deciding if an older adult can live independently. Lacking capacity is not synonymous with having disabilities or being dependent. A disabled older adult may be able to utilize assistive devices or services performed by others to ensure personal daily needs are met. The subset of older adults that lack capacity for safe and independent living are also different from those who rationally refuse to conform to social norms. Cooney et al. (2004) warns that “eccentric, risky, or even foolish decisions should not be confused with impaired capacity”.
Capacity determination is a complex, cross-disciplinary process that ideally involves a range of professionals. It requires knowledge of medicine, ethics, and the law (Moye and Marson, 2007). The legal definition of capacity is usually thought of as an all or nothing phenomena, which can be problematic as real world situations are rarely black and white (Moye et al., 2007a). Many court initiated determinations of capacity assess a limited set of functional domains, when all five domains of safe and independent living should be evaluated (Moye et al., 2007b). These domains consist of (1) personal needs and hygiene, including bathing, toileting, dressing, and feeding; (2) the condition of the home environment, including basic repair and maintenance and the physical structure of one’s living environment; (3) activities for independent living, including shopping, cooking, cleaning and laundry, using telephone and transportation; (4) medical self care, including medication management, wound care, and appropriate self illness monitoring and (5) financial affairs, including daily transactions like managing a checkbook and paying bills as well as judgment with basic financial decisions (Naik et al., 2008).
In contrast to the legal approach, clinicians usually view capacity as a gradient. A person may lack the capacity to manage her entire estate but be able to navigate everyday monetary responsibilities. Similarly, a person may retain capacity in one functional domain (personal care and hygiene), but lack capacity in another (medical self care). The lack of comprehensive and standardized procedures for capacity assessment and intervention represents a significant clinical and scientific gap.
The geriatrics team at Quentin Mease (QM) Community Hospital is part of the Harris County Hospital District (HCHD); a tax supported health care system in Harris County, Texas and affiliated with Baylor College of Medicine. Clinicians noted that 70–80% of all patients seen in the clinic or during home visits were vulnerable older adults with questionable capacity for safe and independent living. Clinicians expressed a need for developing a systematic process to evaluate vulnerable patients and to provide them with the services they needed. In addition, they were confronted by the reality that few geriatrics health care professionals receive adequate training in capacity assessment. To address these gaps in care, the geriatrics team at QM developed a standardized process to assess capacity for safe and independent living in vulnerable older adults.
2. Overview of the CAI model
The CAI model represents this effort. The CAI model consists of a stepwise process (Figure 1) to guide health care professionals through a comprehensive capacity assessment. First, health care providers, family members, or social services agencies such as adult protective services (APS), refer patients to the QM geriatrics program. Second, one or more trained clinicians conduct a comprehensive assessment (Step 2 of Figure 1) by examining the older adult’s ability to make and execute decisions in the five domains critical to safe and independent living. Ideally, assessments are performed in the patient’s home but may also occur in the clinic or skilled nursing facility. The third step involves an interdisciplinary team meeting of providers representing medical, nursing, social work, and rehabilitation disciplines. The team examines all aspects of the case history and assessment and recommends appropriate interventions. The next step consists of a meeting to discuss the assessment and recommendations for intervention with the older adult and family members and social services professionals (when warranted). As a final step, a follow up assessment is conducted to ensure that intervention recommendations have been implemented and their interval effectiveness validated. The intervention plan will often include contingencies to address ongoing declines observed during follow up assessments (Figure 1).
Figure 1.
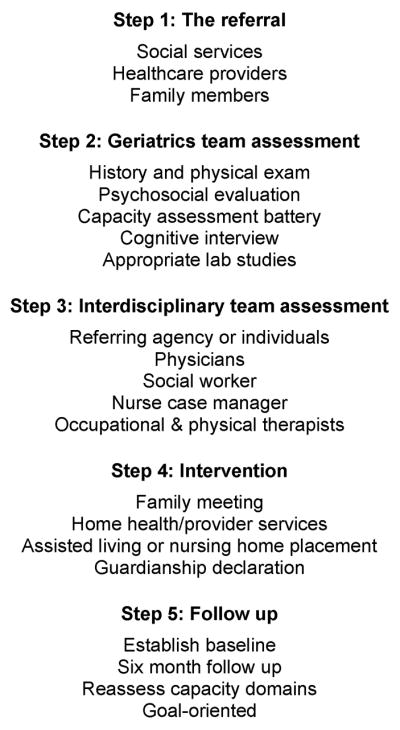
The flow chart of the CAI model
3. Results
3.1. Case of Mr. B
3.1.1. Step 1: the referral
Mr. B. is an 80 year old African American male referred by APS for a capacity assessment. Home health providers assisted Mr. B. daily, but did not fulfill all of his needs. His three children occasionally provided additional assistance with Instrumental Activities of Daily Living (IADLs) and other aspects of his care. More recently, Mr. B. had become increasingly aggressive towards the family, often using foul language. In addition, he was increasingly reliant on family and friends with even basic daily activities. A referral was eventually made to APS. Mr. B. possessed several risk factors that increased his vulnerability. He was of advanced age, lived alone and exhibited self-neglecting behavior. Other factors commonly associated with vulnerability include repeated hospital admissions for acute illness and exacerbations of chronic illnesses and prior reports of elder abuse and exploitation. (Naik et al., 2008)
3.1.2. Step 2: geriatrics assessment
Once a patient is referred to the CAI program, a complete medical and social assessment is scheduled. The assessment is usually completed within two weeks after the referral is received, and sooner for more acute situations. Ideally, clinicians travel to the patients’ home and conduct the assessment. Family members and social services professionals may accompany the assessment team as appropriate. The assessment team usually includes one or more geriatricians or nurse practitioners and a clinical geriatrics social worker, and takes approximately one and a half hours to complete, with additional transit time. The social worker spends additional time on background research in preparation for the visit. Mr. B’s children were present during his evaluation and gave most of the history as he is a poor historian. The assessment began with a comprehensive history and physical. Mr. B. was alert but disoriented to time. He suffered from visual hallucinations and was argumentative throughout the initial assessment. Mr. B. denied medical problems, but his family had noticed a steady cognitive decline over the past two-three years. He was recently diagnosed with dementia by a primary care physician, but reportedly declined further treatment. His physical exam was unremarkable except for poor hygiene, and a strong smell of urine. His social history revealed that he completed high school, was a widower of 10 years, and had four children.
Mr. B. was then subjected to a battery of standardized screening tools including the mini-mental state examination (MMSE) (Folstein et al., 1975), the geriatric depression scale (GDS) (Yesavage et al., 1982), the Kohlman evaluation of living skills (KELS) (Thomson, 1992), used to assess the patient’s ability to adequately perform activities necessary for living in the community, the CLOX executive clock drawing test (Royall et al., 1998), and a standardized assessment of activities of daily living (ADLs) and instrumental ADLs, performed by an experienced team member. Mr. B’s mental status at the time of the initial assessment made it difficult to complete the battery; however, his MMSE score was 13/30 (24 or greater is considered normal), GDS score was 2/15 (less than 5 is considered normal), and CLOX I and II scores were 1 and 9 (normal values are 10 or above for CLOX I and 12 or above for CLOX II) (Royall et al., 1998), respectively. He would not cooperate with performance of the KELS assessment.
Next, a physician conducts an interview evaluating capacity within the five domains crucial to safe and independent living (Table 1). Within each of the five functional domains, two facets of capacity are explored: decisional (the capacity to make informed decisions) and executive (the capacity to implement one’s decisions). There are four components of decisional capacity: understanding, appreciation, reasoning, and expressing a choice, first delineated by Grisso et al. (2008). Individuals must understand the basic information being presented to them. This is often elucidated by asking the patient to paraphrase and repeat back the facts or instructions that were just given to them. Secondly, individuals must appreciate how particular information or situations relate to them; this is demonstrated by a description of how they function daily within a given domain of safe and independent living. Individuals who have problems with appreciation do not provide accurate self-reports of their functioning. The next evaluative criterion requires the patient reason through a given problem and a related set of options by comparing the options and predicting the consequences of each. Asking patients questions such as what would happen if they did not take their medications correctly or how they would go about procuring necessary services are routine aspects of an evaluation of reasoning. Lastly the patient must choose one option; the inability to make a definite choice is a simple but required step for informed decision making (Grisso et al., 2008). Focused questions are asked to elicit a patient’s response, with probing and redirecting techniques used to further evaluate decision making skills.
Table 1.
Assessing the self care and protection domains to determine capacity
| ASSESSMENT OF MEDICAL SELF CARE |
|---|
| Decisional capacity |
| Understanding: |
| Can the patient tell the interviewer about their medical conditions? |
| Upon explaining a new medication or procedure, can the patient recite the explanation in their own words? |
| Appreciation |
| Can the patient describe how the medical problem relates to their own life? |
| Does the patient deny having a medical problem and offer a rational and coherent explanation to why they disagree? |
| Reasoning |
| Comparative: Can the patient identify the differences between choice A and choice B? |
| Example: “Choice A makes me stay longer in the hospital than choice B.” |
| Consequential: Does the patient understand how either choice will affect his/her life? |
| Example: “I have to make a lot of changes in my diet if I pick Choice A.” |
| Making a choice |
| Patients states a clear choice; does not make multiple reversals of choice. |
| Executive capacity |
| Past performance: |
| Missed refills, emergency room visits due to adverse drug reactions. |
| Present performance: |
| Can patient demonstrate how they take their medication, or give themselves insulin injections? |
| Future performance: |
| Prospective home medication assessment. |
Mr. B. exhibited several deficits in decision-making capacity. His understanding of his situation was intact, but he lacked all appreciation of his obvious difficulty in managing personal hygiene, medical conditions and IADLs. He displayed severe limitations in comparative and consequential reasoning, often coming to illogical conclusions about how to manage his affairs and sparse explanations of his choices.
The second facet of capacity involves the planning and execution of decisions, either independently or by delegating responsibility to caregivers. Evaluation of this area comes through reports of past performance in the five functional domains including physical examination, medication bottle and pill checks, reviewing prior bank statements and examination of the home environment itself, either through proxy or home visits (Table 1). Mr. B’s children noted his penchant for poor personal hygiene, mentioning he would often urinate around the house and refuse to change his clothing. He had a history of burning food while attempting to cook. When past performance is in question, a standardized performance test can be used to evaluate executive functions. Assessments such as KELS can be performed in a clinic or home setting to directly observe how individuals perform activities related to financial management, medical self-care, and tasks related to independent living.
For standardized tools like the MMSE, instructions must be given verbatim with no elaboration. The capacity interview, however, is highly individualized and interactive; it demands probing on the part of the examiner to get to the core of the patient’s true capacity. It also allows the examiner to observe other qualitative measures of impaired executive function such as impulsivity, apathy, distractability, or lack of initiative (Cooney et al., 2004). In addition, if the CAI team requires legal documentation declaring the incapacity of a patient in the future, the interview provides context and details about the limitations in an individual’s decision making and real-world functioning.
After the capacity battery is completed, any relevant laboratory studies are performed to obtain a medical baseline for the patient and to rule out physiological causes of impairment. Based on all of these results additional testing may be performed, including further examination by a geropsychiatrist or neuropsychologist, as well as neuroimaging.
3.1.3. Step 3: interdisciplinary team assessment
An interdisciplinary team (IDT) meeting is initiated as soon as possible after completing a patient assessment, rarely occurring more than a week after the assessment. Meetings last for one hour, and are completed by phone conference call if all members cannot be physically present. Physicians, social workers, nurse practitioners, and nurse case managers from the geriatrics team provide their impressions based on the details of the assessment and make suggestions about the best plan of care for the patient. Occasionally, family members are invited to the discussion. The social worker then prepares a summary of the assessment findings, diagnoses, and recommendations for intervention to present to the referring clinician or agency. The interdisciplinary team concluded that Mr. B’s impairments in decision-making, especially with appreciation and reasoning, vividly impacted his capacity to perform everyday tasks related to safe and independent living. The assessment battery was consistent with the capacity interview suggesting moderate dementia and significant executive cognitive impairment. It was determined that he should not continue living independently without significant assistance.
3.1.4. Step 4: intervention
Once an assessment of the patient has been made, the next step in the process is to enact a plan of care. The philosophy of the CAI model is that the best intervention is one that allows for maximum autonomy while assuring safety. Each health care professional works with the patient and family to carry out the recommendations made at the IDT meeting. In the case of Mr. B. the geriatrics team recommended disconnecting the gas supply to the stove. They also initiated guardianship proceedings, filed by the physician. With the assent of Mr. B. and his family, he began receiving medial care in the QM geriatrics clinic. The team also recommended various provider services that the family could utilize to ensure that he had supervision at home until the guardianship was authorized.
The CAI model utilizes an assortment of interventions to meet individualized needs and support patients’ ability to live safely and independently in the community. Interventions include prescription of assistive devices (hearing aids, walkers, canes, glasses, etc) and environmental modifications that may support functional capacity (Naik and Gill, 2005). Furthermore, the CAI model’s social worker ensures that eligible patients are enrolled in Medicare and Social Security.
3.1.5. Step 5: follow-up
Follow-up may be the most crucial step in ensuring long-term benefits. Often first line interventions are enacted on a trial basis, with second line interventions planned if the individual still displays deficits in safe and independent living. Effective and consistent communication between families and the CAI team guide the timing of intervention implementation. In Mr. B’s case, CAI clinicians established clear understanding of his baseline capacity and described goals for the follow-up assessment. Secondary interventions are considered at follow-up if predefined goals are not met. At the follow-up assessment, Mr. B’s capacity for independent living continued to decline with ongoing complaints from family members.
Several weeks after the CAI assessment, the probate court authorized guardianship with one of Mr. B’s sons designated as his legal guardian. After failing to achieve the goals elaborated at the initial IDT assessment, placement in a long-term care facility was agreed upon by the team clinicians and Mr. B’s guardian. He continues to receive care from QM geriatricians and his hallucinations due to dementia have subsided. He is happy with his current living situation and thankful for the support of his family and the geriatrics team.
4. Barrier to consider: delays in delivering care
There are several obstacles that must be overcome in order to ensure successful treatment of patients using the CAI model. Most assessments are initially conducted in the patient’s home, so the situation can be quite variable. Often little to no past medical history is available. Family members may be reluctant or unable to implement new plans of care. Patients often do not share treatment goals with clinicians and family members, which can undermine the intervention process. Even if the family is willing to obtain further treatment, transportation and health insurance may present barriers to effective intervention.
Health care providers often find it difficult to authorize life-altering decisions, especially when the relationship with the patient is limited or new. Beginning legal proceedings to declare someone incapacitated may lead to a near complete loss of rights for the patient to make decisions involving her life. Many clinical and social details must be clarified before such a decision can be made. Consider the next case report as an example of how these complex issues are often addressed by the CAI model team.
4.1. The case of Mrs. S
Mrs. S. is a 75 year-old black female enrolled in the QM geriatrics clinic since 1999. Although she appeared to be highly functional, Mrs. S. had been involved in several incidents that raised suspicion about her ability to live safely and independently. She lost Medicare coverage due to her inability to keep up with the changes in her plan. In 2007, she was hospitalized several times for exacerbations of diabetes and chronic obstructive pulmonary disease (COPD). At that point a local physician decided to initiate a capacity assessment, referring her to the CAI model clinic.
Mrs. S’s assessment revealed a past medical history of type II diabetes mellitus, Parkinson’s disease, COPD, hypertension and partial blindness. As her health declined she began receiving in-home provider services for ADLs and skilled nursing services for insulin dosing. On physical exam, Mrs. S. exhibited poor personal hygiene and weight loss. Her chronic medical conditions were uncontrolled along with the presence of several geriatric syndromes, such as urinary incontinence and falls. A few days prior to her assessment, her home health nurse was unable to make a regular appointment for insulin dosing, and she had not made alternative arrangements. Psychosocial history revealed that Mrs. S. had a college degree and served in the military. She was a consultant and planner until 1985 when she retired and moved in with her ailing mother until her death. Her personality was secretive and standoffish and she didn’t talk about her personal life. Her only known relatives were an ex-husband and cousin.
Standardized testing included the following: MMSE was 30/30, CLOX I and II were within normal limits, GDS was 0 out of 15, and KELS score was a 5.5 (suggesting some difficulty living safely and independently). During the capacity interview Mrs. S. demonstrated difficulties with appreciation of the declines in her daily functioning, and problems with consequential reasoning as it related to managing medications and household finances.
Mrs. S’s sister, unknown to any of team clinicians previously, was located by the CAI social worker. Furthermore, an old family friend and attorney reached out to the CAI team because of concerns about financial discrepancies in Mrs. S’s estate. The attorney also recalled Mrs. S’s mother acting very similarly towards the end of her life.
As a result of the IDT meeting, a family meeting was recommended in order to identify: (1) a support system to manage her medial care and affairs; and (2) help for Mrs. S. to maintain a safe living environment. Interventions included granting general power of attorney to her sister and drafting advance directives. Closer supervision and monitoring by a safety network of willing friends was recommended to promote further independence. Physical therapy was also prescribed to improve mobility. Furthermore, repairs and home modifications were made to her home to accommodate functional needs. The follow-up assessment demonstrated improved control of her chronic medical morbidities, appropriate weight gain and personal care management, and enhanced mobility.
5. Barrier to consider: the importance of determining capacity beyond guardianship
There is great variability in the scope and format of clinician capacity assessments (Moye et al., 2007a,b). While appointing a legal guardian is one possible outcome of a capacity assessment, it should not be considered the only outcome. In actuality, guardianship is a low effectiveness but high resource option, and should be considered as a last resort. If guardianship proves to be the best course of action, however, the CAI model will provide a consistent, valid, and reliable method of documentation during legal proceedings to assist the probate court. Capacity assessments provided to the court should contain adequate information regarding the following: (1) decision making capacity, (2) capacity to carry out a plan and live independently, (3) any dangerous activities resulting from living alone at home, and (4) any activities that may endanger others. (Cooney et al., 2004) Concerns about guardianship include limited due process, poor communication between clinicians and the court, and overly paternalistic interventions. (Moye et al., 2007b) Family dynamics often play an important role in deciding whether or not guardianship is appropriate, clearly exemplified by the next clinical vignette.
5.1. The Case of Mr. K
Mr. K. is an 85 year old white male, widowed for 5 years, who was referred to the CAI team by APS for suspicion of financial exploitation. Some of his children were extremely concerned about an unjustified depletion in the value of Mr. K’s estate. He had written several checks to a female companion, including one for $65,000. When confronted by his children about his spending he became angry and “didn’t want to be told what to do”. A dispute among the children about Mr. K’s ability to handle his affairs resulted in tension, hostility and alienation. One of his daughters, fearing her father was being financially exploited, reported the case to APS.
The geriatrics assessment revealed Mr. K’s past medical history included a hip replacement, urinary incontinence, and a family history of dementia. Mr. K. has a college degree and worked for the FBI for many years. Residing in an affluent neighborhood, he has three children, including a daughter in the same city. He is in excellent physical condition, exercises daily, and functions independently in his ADLs.
Mr. K’s standardized testing is as follows: his MMSE score was 27/30, CLOX I and II were 3 and 4, respectively, and GDS scale was 2/15. He received a score of 7 on the KELS, which was alarming, suggesting the need for significant assistance to support community living. During the capacity interview he also exhibited other subtle signs of impaired executive functioning. Lab tests further revealed a significant vitamin B12 deficiency.
The IDT meeting determined that Mr. K. most likely suffered from early Alzheimer’s dementia. The IDT recommended a family meeting to discuss these findings. Interventions included donepezil for dementia treatment and vitamin B12 supplementation. Plans were also implemented to designate a power of attorney over his estate and generate advanced directives. Mr. K. was also enrolled in adult day care.
At a follow-up visit eight months later, Mr. K. agreed to move in with his daughter. He was excited about the decision and seems more relieved and content in his new environment.
6. Conclusion
The CAI model provides a systematic approach to initiating, conducting, and following through an assessment of an older adult’s capacity to make and execute decisions regarding safe and independent living in the community. The need for assessing the capacity for safe and independent living is surprisingly common among vulnerable community-living older adults. Guardianship should be an option of last resort as many patients see significant improvements in their quality of life with less invasive intervention. Questions still remain as to the best method to assess capacity in this context. Formal training on capacity assessment remains a challenge for new clinicians. Consistency of training and proficiency in assessment skills remains an important quality measure.
The CAI model is different and more comprehensive then standard capacity assessments because of the addition of the capacity interview. The capacity interview is essential to the capacity assessment because it provides information that the quantitative scores of exams such as MMSE, GDS and KELS cannot. Interviewing the patient in their home gives the health care providers better insight into the patient’s life, but is also a challenging aspect of the model due to unpredictability. Coordination amongst all the members of the team can also pose a problem. The CAI model is practical to reproduce, requiring minimal additional personnel or resources to existing geriatrics clinic models. All of the participants are staff of the HCHD, either independently or through their affiliation with Baylor College of Medicine, and perform the assessments as a part of their weekly duties. Currently, more than thirty patients have been evaluated using the CAI model, resulting in placement outside of the home for only twelve cases. Through working with patients and their families using the objective framework of the CAI model, other solutions have been found to keep older adults as independent as possible. Validation of the CAI model is currently in process.
Acknowledgments
This study was supported by a bioethics project grant from the Greenwall Foundation (Naik, PI), the Practice Change Fellows Program (Regev) supported by the Hartford Foundation and Atlantic Philanthropies. The Capacity Assessment and Intervention model receives ongoing support from the Harris County Hospital District and the Houston VA HSR&D Center of Excellence (HFP90-020). Dr. Naik is also supported by an NIA K23 grant (5K23AG027144). Felicia Skelton was supported by a medical student training in aging research (MSTAR) grant from the American Foundation on Aging Research. None of the funding agencies played a role in the design and conduct of the study, analysis and interpretation of the data, or the preparation and approval of the manuscript.
The authors would like to thank Laurence McCullough, PhD and Carmel B. Dyer, MD for their support and insights in the early development of the capacity assessment and intervention model, and Kristin Cassidy, BS, for her careful editing of the final manuscript.
Footnotes
Conflict of interest statement: None.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Cooney LM, Jr, Kennedy GJ, Hawkins KA, Hurme SB. Who can stay at home? Assessing the capacity to choose to live in the community. Arch Intern Med. 2004;164:357–360. doi: 10.1001/archinte.164.4.357. [DOI] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Grisso T, Applebaum PS. MacArthur Competence Assessment Tool-Treatment (MacCAT-T) Manual. Professional Resource Press; Sarasota, FL: 2008. [Google Scholar]
- Huang ES, Brown SE, Ewigman BG, Foley EC, Meltzer DO. Patient perceptions of quality of life with diabetes-related complications and treatments. Diabetes Care. 2007;30:2478–2483. doi: 10.2337/dc07-0499.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moye J, Marson DC. Assessment of decision-making capacity in older adults: an emerging area of practice and research. J Gerontol B: Psychol Sci Soc Sci. 2007;62:S3–S11. doi: 10.1093/geronb/62.1.p3. [DOI] [PubMed] [Google Scholar]
- Moye J, Butz SW, Marson DC, Wood E. A conceptual model and assessment template for capacity evaluation in adult guardianship. Geronto-logist. 2007a;47:591–603. doi: 10.1093/geront/47.5.591. [DOI] [PubMed] [Google Scholar]
- Moye J, Wood S, Edelstein B, Armesto JC, Bower EH, Harrison JA, Wood E. Clinical evidence in guardianship of older adults is inadequate: findings from a tri-state study. Gerontologist. 2007b;47:604–612. doi: 10.1093/geront/47.5.604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naik AD, Gill TM. Underutilization of environmental adaptations for bathing in community-living older persons. J Am Geriatr Soc. 2005;53:1497–1503. doi: 10.1111/j.1532-5415.2005.53458.x. [DOI] [PubMed] [Google Scholar]
- Naik AD, Schulman-Green D, McCorkle R, Bradley EH, Bogardus ST., Jr Will older persons and their clinicians use a shared decision-making instrument? J Gen Intern Med. 2005;20:640–643. doi: 10.1111/j.1525-1497.2005.0114.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naik AD, Pickens S, Burnett J, Lai JM, Dyer CB. Assessing capacity in the setting of self-neglect: development of a novel screening tool for decision-making capacity. J Elder Abuse Negl. 2006;18:79–91. doi: 10.1300/j084v18n04_08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naik AD, Lai JM, Kunik ME, Dyer CB. Assessing capacity in suspected cases of self-neglect. Geriatrics. 2008;63:24–31. [PMC free article] [PubMed] [Google Scholar]
- Royall DR, Cordes JA, Polk M. CLOX: an executive clock drawing task. J Neurol Neurosurg Psychiatry. 1998;64:588–594. doi: 10.1136/jnnp.64.5.588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulman-Green DJ, Naik AD, Bradley EH, McCorkle R, Bogardus ST. Goal setting as a shared decision making strategy among clinicians and their older patients. Patient Educ Couns. 2006;63:145–151. doi: 10.1016/j.pec.2005.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomson LK. The Kohlman Evaluation of Living Skills. 3. American Occupational Therapy Association; Bethesda, MD: 1992. [Google Scholar]
- Workman RH, Jr, McCullough LB, Molinari V, Kunik ME, Orengo C, Khalsa DK, Rezabek P. Clinical and ethical implications of impaired executive control functions for patient autonomy. Psychiatr Serv. 2000;51:359–363. doi: 10.1176/appi.ps.51.3.359. [DOI] [PubMed] [Google Scholar]
- Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, Adev M, Leirer VO. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res. 1982;17:37–49. doi: 10.1016/0022-3956(82)90033-4. [DOI] [PubMed] [Google Scholar]


