Abstract
Oxidative stress, implicated in the etiology of cancer, results from an imbalance in the production of reactive oxygen species (ROS) and cell’s own antioxidant defenses. ROS deregulate the redox homeostasis and promote tumor formation by initiating an aberrant induction of signaling networks that cause tumorigenesis. Ultraviolet (UV) exposures, γ-radiation and other environmental carcinogens generate ROS in the cells, which can exert apoptosis in the tumors, thereby killing the malignant cells or induce the progression of the cancer growth by blocking cellular defense system. Cancer stem cells take the advantage of the aberrant redox system and spontaneously proliferate. Oxidative stress and gene-environment interactions play a significant role in the development of breast, prostate, pancreatic and colon cancer. Prolonged lifetime exposure to estrogen is associated with several kinds of DNA damage. Oxidative stress and estrogen receptor-associated proliferative changes are suggested to play important roles in estrogen-induced breast carcinogenesis. BRCA1, a tumor suppressor against hormone responsive cancers such as breast and prostate cancer, plays a significant role in inhibiting ROS and estrogen mediated DNA damage; thereby regulate the redox homeostasis of the cells. Several transcription factors and tumor suppressors are involved during stress response such as Nrf2, NFκB and BRCA1. A promising strategy for targeting redox status of the cells is to use readily available natural substances from vegetables, fruits, herbs and spices. Many of the phytochemicals have already been identified to have chemopreventive potential, capable of intervening in carcinogenesis.
Key words: ROS, antioxidants, cancer stem cells, NRF2, NFκB, BRCA1, phase II, detoxification enzymes
Introduction
Death resulting from cancer has not changed significantly for last three decades although US government has given a lot of stress in search for the cure of cancer. In the beginning, cancer cells are more vulnerable to chemotherapy and radiotherapy than normal cells, but, as the disease progresses, they lose their preferential sensitivity to the same treatments. All these therapeutic approaches as well as exposure to environmental carcinogens like ionizing radiations (IR), ultraviolet (UV) exposures and other environmental carcinogens generate reactive oxygen species (ROS) in the cells, which can act in both beneficial and detrimental ways. ROS exerts oxidative stress in the cells which deregulate the body’s cellular defense system leading to genomic instability and cancer.1–3 Moreover, oxidative stress can result from a number of endogenous sources, including the production of oxygen-free radicals by mitochondrial oxidative phosphorylation. Mitochondria are the significant source of ROS as they are the major consumers of molecular oxygen in cells.4,5 Cellular defense system is comprised of several Phase II detoxification enzymes such as glutathione-S-transferases (GSTs), NADP(H) quinone oxidoreductase (NQO1), Glutathione peroxidases (GPx), Catalase, superoxide dismutases (SODs), epoxide hydrolase, heme oxygenase (HO-1), UDP-glucuronosyl transferases (UGTs), gamma-glutamylcysteine synthetase and many others. Expression of these proteins protects cells from oxidative damage and can prevent mutagenesis and cancer.6–11 Apart from cancer, oxidative stress has been implicated in several chronic diseases and natural process such as aging, atherosclerosis, diabetes mellitus, arthritis and neurodegenerative disease including Alzheimer’s and Parkinson’s disease.12–17 Due to scope and limitation, this review will focus on the (1) Role of ROS in pathophysiological implications of altered redox regulation in breast, prostate, colon and pancreatic cancer; (2) Involvement of BRCA1, as a protectant against oxidative stress; (3) Modulation of redox environment in cancer stem cells; (4) Targeting redox system by phytochemicals for therapeutic interventions; (5) Function of antioxidants, antioxidation enzymes and transcription factors in the maintenance of cellular defense system; (6) Finally we will discuss the future perspectives on addressing the question; ‘Where are we leading to with these innovations and what should be done so that everybody can lead a better and relaxed life in this hazardous environment?’
Reactive Oxygen Species (ROS) Mediated Carcinogenesis
Oxidative stress promotes damage to the cell structure including proteins, lipids, membranes and DNA, that plays a key role in the development of cancer.2,12–15,18 Mitochondrial electron-transport chain and other oxidizing agents are the prime pathways that generate excess ROS in vivo, leading to several types of DNA damage, including depurination and depyrimidination, singleand double-stranded DNA breaks, base and sugar modifications and DNA-protein crosslinks.19–21 Permanent modification of genetic material resulting from the oxidative damage is one of the vital steps involved in mutagenesis that leads to carcinogenesis. Stimulation of DNA damage can either arrest or induce transcription, signal transduction pathways, replication errors and genomic instability, all of which are associated with carcinogenesis.18,22,23 The most frequent DNA mutations caused during oxidative stress, initiated by ionizing radiation and other environmental carcinogens are 7,8-dihydro-8-oxoguanine (8-Oxo-G) and Thymine Glycol (TG). Thymine glycol blocks transcription and causes cell death both in cancer and non-cancer cells. These oxidized DNA products are relatively easy to generate during oxidative stress and are both mutagenic and carcinogenic. Thus they are considered as useful markers of oxidative stress and potential biomarkers of carcinogenesis.24–26 To counterbalance the oxidative damage from ROS, aerobic organisms have created a variety of antioxidant mechanisms to maintain their genomic stability. These mechanisms include phase II detoxification and other antioxidation enzymes that act in cellular defense such as catalase and SOD, GPx, GST, other constitutive and inducible antioxidants, DNA repair enzymes, and other cellular mechanisms of genomic surveillance, such as cell cycle checkpoint control systems. 27 Moreover, several growth factors such as serum, insulin like growth factor I, or fibroblast growth factor 2 generates ROS in MIA PaCa-2 and PANC-1 cells, which are human pancreatic adenocarcinoma cells that promotes cell survival. Inhibiting ROS generation with the antioxidants or NADPH oxidase (Nox4) antisense, or MnSOD overexpression would stimulate apoptosis in PaCa-2 and PANC-1 cells. This mechanism might play an important role in pancreatic cancer resistance for treatment and thus represent a novel therapeutic target.28 In gastrointestinal and colon cancer, oxidative pentose pathway (OPP) and the glutathione (GSH) antioxidant defense system play an important role in the regulation of cell growth and apoptosis. The OPP modulate intracellular redox status and provides NADPH for the synthesis of GSH, which is responsible for the inactivation of intracellular ROS that induce apoptosis and cell injury. Depletion of GSH increases the sensitivity of cells to ROS. Therapeutic inhibition of the OPP and/or the GSH defense system might increase the sensitivity of gastric and colon cancer cells to anti-cancer therapy.29 Recent studies have shown that the enzymatic product of thymidine phosphorylase (TP) generated ROS within cancer cells that help in maintaining the growth of colon cancer cells thus may provide improved therapeutic results as well as a preventative effect on carcinogenesis of the colorectum.30 Emerging evidence also suggests that supranutritional doses of selenite could induce typical apoptosis in colorectal cancer cells in vitro and in xenograft tumors by inducing ROS. It indicates that selenite can activate the apoptotic machinery through redox-dependent activation and could be useful in cancer therapy.31
BRCA1 Functions in Oxidative Stress Responses
The breast cancer susceptibility gene, BRCA1, encodes a tumor suppressor protein, mutations of which account for about 40–50% of hereditary breast cancers.32,33 In sporadic (non-hereditary) breast cancers, BRCA1 expression is absent or decreased in about 30–40% of cases. Environmental and genetic factors are the important contributors of the neoplastic transformation leading to breast cancer. BRCA1 has several important functions and one of them is to render protection to the cells during oxidative stress. BRCA1 upregulates the expression of multiple genes involved in the cytoprotective antioxidant response, including GST, GPx, Oxidoreductases, and other antioxidant genes. Consistent with these findings, ectopic expression of BRCA1 conferred resistance while BRCA1 deficiency conferred sensitivity to several different oxidizing agents (hydrogen peroxide and paraquat).34,35 Evidences collected from the BRCA1 mouse model where mice are homozygous for full-length breast cancer-associated gene-1 (Brca1) deletion and heterozygous for a p53-null mutation (Brca1Δ11/Δ11p53+/−), display high frequency of spontaneous lymphoma and mammary tumor formation.36 Brca1 mutant mice also exhibite increased expression of Redd1, which is a developmentally regulated transcriptional target of p63 and p53, during regulation of ROS. Additionally, the same mice demonstrate elevated levels of ROS and subsequently they are more sensitive to oxidative stress induced lethality.35 In addition, in the setting of oxidative stress (due to hydrogen peroxide), BRCA1 shifts the cellular redox balance to a higher ratio of reduced to oxidized glutathione (GSH).34,37 Higher content of reduced glutathione functions in favor of redox maintenance. The identification of transcriptional target of several antioxidant genes that are elevated during BRCA1 overexpression led to the findings that BRCA1 regulates the activity of the antioxidant response transcription factor Nrf2 and NFκB and protects cells against oxidative stress.34,38 This function would be consistent with the postulated role of BRCA1 as a caretaker gene in preserving genetic integrity via regulating the redox maintenance of the cells.
We have studied the antioxidant property of BRCA1 by either over- and or under-expression of BRCA1 in breast cancer cells. We have demonstrated that wild-type BRCA1 (but not a cancer-associated mutant) significantly reduced ROS levels, determined by DCF fluorescence assays using flow cytometry and confocal microscopy.37 Figure 1 demonstrates the cellular protection function of BRCA1 during oxidative stress. MCF-7 breast cancer cells were transfected with either wt BRCA1 or the background vector (pcDNA3) and simultaneously all the experimental cells were treated with tert-butyl hydroperoxide (TBHP) (Molecular Probes; Carlsbard, CA) to artificially generate cellular ROS, which is detected by using Carboxy-H2DCFDA (Green) (Molecular probes (I36007), Carlsbard, CA). This figure demonstrates that ectopic expression of BRCA1 significantly reduces the formation of ROS triggered by TBHP (third column) when compared to vehicle and pcDNA3 plasmid transfection (first and second column). Furthermore, expression of redox factor 1/AP endonucleases 1 (Ref1/APE1) in breast cancer cells, which has a dual role of redox regulation in cells and lyase activity in stimulating base excision repair (BER) pathway, inhibits the generation of ROS and promotes cell survival against oxidative stress, rendered by either stress producing agents.39,40 The BRCA1 and Ref1/APE1 pathways for reduction of ROS levels appear to exhibit cross-talk in protecting the cells from stress. BRCA1 also reduced the levels of protein nitration that exerts nitrative stress in the cells by forming harmful 3-Nitrotyrosine during H2O2-induced oxidative damage to proteins.37 H2O2 caused modest but detectable increases in the levels of 8-oxo-G and thymine glycol (TG) modification in DNA. Wt BRCA1 reduced, while BRCA1-siRNA further increased the 8-oxo-G and TG levels in H2O2-treated cells indicating BRCA1 involves in stimulating DNA repair process to repair the oxidative lesions.37
Figure 1.
Wt BRCA1 downregulates the production of ROS in MCF-7 breast cancer cells. Cells were transfected either with background vector (pcDNA3) or with wt BRCA1 plasmid. Forty-eight hours post transfection all the cells were treated with 100 µM of ROS producing agent TBHP (tert-butyl hydroperoxide) in a serum free medium. Levels of ROS were detected through confocal microscopy using carboxy-H2DCF-DA fluorescence (first row). Second row is the phase picture of all the cells that are used for confocal staining. Decrease in the stain intensity in BRCA1 transfected cells compared to vehicle and background vector transfected cells depicts an important function of BRCA1 in protecting cells from oxidative damages.
Oxidative Stress Mediated Estrogen Receptor Activity in Breast Cancer
Estrogens play a crucial role in the development and evolution of human breast cancer. Epidemiological evidence indicates that prolonged lifetime exposure to estrogen is associated with elevated breast cancer risk in women. Estrogen is converted by cytochrome P450 1B1 to 4-hydroxyestradiol (4-OHE2), a putative carcinogenic metabolite of estrogen.41 This catechol estrogen metabolite is oxidized further to produce a reactive quinone via semiquinone. Oxidative stress and estrogen receptor-associated proliferative changes are suggested to play important roles in estrogen-induced breast carcinogenesis.42–44 Treatment of the immortalized human breast epithelial cells (MCF-10F) with 17β-estradiol (E2), 4-hydroxyestradiol (4-OHE2) or 2-hydroxyestradiol (2-OHE2) induces phenotypical changes indicative of neoplastic transformation.45 Although the precise molecular mechanisms by which E2 induces breast cancer have not been completely understood, the estrogen implication in breast cancer has been associated mostly with the estrogen receptor46,47 that mediates cell proliferation. The direct role of estrogens as tumor initiators has been supported by the evidence that E2, catechol estrogens (CEs) and their quinone derivatives exerts oxidative stress that lead to various types of DNA damage, including single strand breaks as well as stable and depurinating DNA adducts.48,49 2-OHE2 and 4-OHE2 are the two catechol metabolites of estrogens that could be oxidized to CE quinones (CE-Q) that may react with DNA. Physiologic concentrations of estradiol (E2) have also been reported to cause a decrease in catalase activity followed by an increase in glutathione peroxidase (GPx) activity, in MCF-10A breast epithelial cells.50,51 Moreover, thioredoxin (Trx) and thioredoxin reductase (TrxR) are shown to modulate H2O2 levels and the activity of estrogen in estrogen responsive breast cancer cells.52 Oxidative stress can change the structure and function of estrogen receptor and progesterone receptor (PR), altering the biology and clinical outcome of endocrine responsive (ER-positive) breast cancer.53,54 A subset of estrogen/ER-responsive breast cancer genes that are linked to cell growth and invasion pathways were identified and associated with loss of PR.55,56 Intracellular proteins that are most susceptible to oxidant-induced structural and functional damage are redox-sensitive zinc finger transcription factors such as Sp1 and ER. Zinc finger cysteine residues of ER are readily oxidized during stress, eliminating their DNA-binding activity. Failure of DNA-binding activity of ER has been found in up to 30–35% of all ER-positive breast cancers and that correlated with loss of PR expression. Both, Sp1 and ER-α DNA-binding and transactivating functions are needed for optimal estrogenic stimulation of genes such as PR and Bcl2. ER-positive breast cancers would exhibit suppressed expression of these estrogen-inducible genes during oxidative stress.
Redox Status in Cancer Stem Cells
Studies have shown that redox balance plays an important role in the maintenance of stem cell self-renewal and in differentiation. Very little is known about the redox status in cancer stem cells. Normal haemopoietic stem cells and normal mammary epithelial stem cells maintained lower levels of ROS than their mature progeny to prevent cellular differentiation and maintain longterm self-renewal.57–59 A newly identified subpopulation of cells, known as ‘cancer stem cells’, are responsible for the reoccurrence of tumor following chemotherapy. These cells are highly drug resistance and one can hypothesize that these cells use redox regulatory mechanisms to escape the cell death by several anticancer agents.60–65 Cancer stem cells actually maintain both the stemness nature and cancer cell characteristics for growth and survival and probably they share some very common characteristics like normal stem cells in redox regulation. Evidences are that subsets of cancer stem cells in human and murine breast tumors contain lower ROS levels, similar to normal stem cells, than the corresponding non-tumorigenic cells.57 This low level of ROS seems to be associated with elevated expression of ROS-scavenging molecules, which may contribute to tumor radioresistance. We believe BRCA1 has a role in modulating cancer stem cells. The major transcription factor responsible for the stemness nature of the cells is the Forkhead Box Os (FoxOs) that upregulates the expression of SOD and catalase.66,67 Biological properties of the cancer stem cells renders that these cells might have an elevated antioxidation enzymes pool to maintain reduced levels of ROS like normal stem cells. On the other hand, this high antioxidant capacity also favors the survival of the cancer stem cells and drug resistance. Moreover, some stem cells reside in a relatively low oxygen microenvironment that might also limit the endogenous ROS production. Thus cancer stem cells in a hypoxic microenvironment may be relatively resistant to radiotherapy and chemotherapy with redox-cycling agents since their cytotoxicity requires the availability of local oxygen. It is thus crucial to first determine the redox status in cancer stem cells compared with normal stem cells and with cancer cells in tumors.57,68 Discovery of the main molecular signaling pathway that maintains the redox nature in cancer stem cells might provide a possibility to abrogate the survival mechanisms in these cancer stem cells and allow the eradication of the root of cancer.
Targeting Redox Mediated Signaling Cascade Leading to Cell Death in Cancer
Cancer cells have been found to be in a state of redox imbalance, an alteration in the homeostasis between oxidants and antioxidants, resulting in increased oxidants within the cell. Oxidative stress due to the chronic over-exposure to ROS is thought to contribute to a variety of processes, including aging, degenerative diseases, and cancer.12–16 On the other hand, ROS also play an essential role as secondary messengers in the normal regulation of a variety of physiological processes, suggesting that their production is a double-edged sword. Oxidative stress can induce positive responses such as cellular proliferation or activation, as well as negative responses such as growth inhibition or cell death. Cellular redox status is maintained by several intracellular redox-regulating molecules, including thioredoxins (TRX).69 TRX is one of the key regulators of signaling in the cellular responses against various stresses. TRX demonstrates a cytoprotective action against oxidative stress-induced apoptosis as well as induces growth-promoting effect as an autocrine growth factor. Moreover, TRX is involved in the regulation of protein-protein or protein-nucleic acid interactions through its redox nature of the cysteine residues. TRX translocates from the cytosol into the nucleus due to a variety of cellular stresses, to regulate the expression of various genes through the redox factor-1 (Ref-1/APEX1).70 Glutathione (GSH)/Glutaredoxin (GRX) system also maintains the redox homeostasis in the cells but it is dependent on the TRX redox regulation.71 GRX is a small dithiol protein involved in various cellular functions, including the redox regulation of certain enzyme activities via its disulfide exchange reaction. Overexpression of GRX, protect cells from hydrogen peroxide (H2O2)-induced apoptosis by regulating the redox state of the cell. Thus molecules or enzymes that can penetrate the redox environment of the cancer cells will be beneficial for killing the same. Incidentally stress levels in some tumor cells are actually masked by the activation of anti-oxidation/anti-apoptotic signaling. If this molecular shield can be removed in the cancer cells, death signals can be reinstated by inducing stress and cells can be forced to undergo apoptosis again. A number of examples imply that this can be achieved. For example, non-small-cell lung carcinoma cells become more resistant to cytotoxic agents such as cisplatin, doxorubicin and etoposide due to the elevated levels of Her-2/neu expression but when Her-2/neu signaling was inhibited, these cells become re-sensitized to these agents.72 Similarly, the ectopic expression of a mutated EGFR, in advanced glioma, exhibit resistance to cisplatin due to reduced apoptosis. Blocking EGFR signaling in these cells restores their cisplatin sensitivity.73 Blocking Her-2 with Herceptin (Trastuzumab) sensitizes highly drug-resistant breast cancer cells to cytotoxic drugs.74 In fact, the combination of chemotherapy with cellular redox system modifiers has shown promising results in clinical trials. How these combined therapies modulate ROS and stress kinase pathways at the cellular level has not been determined yet. The study of stress signaling has proved to be instructive in explaining recent advances in cancer therapy and should facilitate the development of improved anticancer strategies.
Phytochemicals as Anti-Cancer Chemopreventive Compounds that Targets Redox Regulations
Considering the burden of health-care cost as a major global concern, dietary chemoprevention provides an inexpensive, readily applicable and easily accessible approach to cancer control and management and at present it is a hot area of research. Strengthening of cellular defense mechanism or restoration of stress-response signaling by administrating dietary phytonutrients provides an important strategy for cancer chemoprevention. Currently antioxidant activity is the most common in vitro parameter used to assess or predict potential benefits of plant derived compounds. However, correlations between in vitro antioxidant activity and actual health benefits are unknown. Such in vitro antioxidant data ignore other potentially beneficial or harmful effects of phytochemicals like modification of enzyme activity and/or cell signaling pathways. There are several compounds we are working with, that target the redox system of the cancer cells either by inducing ROS-mediated apoptosis or prevent the cells from exogenous or endogenous sources of ROS by upregulating cellular defense system and inhibiting the cancerous growth.
Indole-3-carbinol (I3C), a phytochemical from cruciferous vegetables, is of interest because a diet rich in cruciferous vegetables is associated with a reduced risk of several tumor types, such as breast cancer. In the acidic environment of the stomach, I3C undergoes hydrolysis to a number of products, including a dimeric product, 3,3′-diindolylmethane (DIM), its major active metabolite.75 Both these phytochemicals stimulate BRCA1 in breast and prostate cancer cells and has been shown to protect cells against oxidative stress mediated by H2O2 and γ-radiation.75,76 Genistein (4,5,7-trihydroxyisoflavone) was identified as the predominant isoflavone in soybean enriched foods, which comprises a significant portion of the Asian diet, has been shown to inhibit prostate carcinogenesis in animal models. Genistein has antioxidant effects and protects cells against ROS by scavenging free radicals, inhibiting the expression of stress-response related genes.76 Furthermore, genistein is a powerful inhibitor of NFκB, Akt and PTK signaling pathways, all of which are important for cell survival.77 Curcumin, on the other hand, is a diferuloylmethane, derived from the rhizomes of turmeric. Curcumin targets the Nrf2-ARE signaling pathway to induce phase II detoxifying enzymes on an event of oxidative stress.38,78 Addition of curcumin disrupts the Nrf2-Keap1 complex, leading to elevated Nrf2 binding to ARE and subsequent increase in the expression and activity of HO-1 in porcine renal epithelial proximal tubule (LLC-PK1) cells and/or rat kidney epithelial (NRK-52E) cells via activation of p38 MAP kinase. UDP-glucuronosyltransferase (UGT) isozymes catalyze detoxification of numerous chemical toxins present in our daily diet and environment, which give rise to ROS, by conjugation to glucuronic acid. Curcumin modulates the activity of cellular UGT1A7 and UGT1A10 and increases the bioavailability of other compounds such as Genistein or Diadzein in the cells that has an inhibitory effect on cancer.79–81
Whole food and spices demonstrate excellent source of mixture of compounds that targets the redox system of the cells and are known for their high therapeutic potential for ages. Spices are now receiving increasing attention as many of them have been shown to have anti-carcinogenic properties. Saffron, Clove, Cardamom and Cinnamon are highly aromatic spices, commonly used in Asian, Arab and some Scandinavian cuisines. We and others have demonstrated several anti-carcinogenic activities of these spices against several cancers by upregulating several phase II detoxification enzymes, antioxidants and reducing the lipid peroxides in the cells.82–87 Additionally, garlic, which is whole food used all over the world demonstrates a formidable prophylactic and therapeutic medicinal property.85 Garlic extracts inhibits the oxidative modification of lipids induced by DMBA, thus protecting cells from injury by the oxidized molecules.85 Oral administration with aqueous infusion of garlic and cardamom in addition to the DMBA treatment to the swiss albino mice demonstrate downregulation of COX2 and p53 (tumor suppressor) expression when compared to the DMBA treated mice only indicating reduction of inflammation related abnormalities in the phytocompounds treated mice. These phytocompounds delayed the formation of skin papillomas in animals and simultaneously decreased the size and number of papillomas demonstrating their beneficial effects.84,85
Redox Sensitive Transcription Factors Involved in Oxidative Stress
The concept of “Redox Regulation” in the field of cancer prevention is emerging to understand the mechanisms behind the pathogenesis of several disorders including tumor initiation and malignant transformation.88,89 Redox sensitive transcription factors are the key players in regulating several pathways that lead to carcinogenesis. Transcription factors/activators are a group of proteins that bind to specific consensus sequences (cis elements) in the promoter regions of downstream target/effector genes and either transactivate or repress effector gene expression. The change in the expression of the effector genes eventually leads to several biological modifications such as proliferation, growth suppression, differentiation or senescence. Furthermore, redox-induced biochemical alterations sometimes lead to change in the biological functions of these proteins. Therefore, differential regulation of these transcriptional activators, which in turn, regulate many target/effector genes, may provide an additional mechanism by which small antioxidant molecules play protective roles in anti-cancer processes and thus have an important impact on drug discovery and therapy for the inhibition of cancer. This section will focus on the redox regulation of transcription factors/ activators with emphasis on Nrf2 and NFκB that modulate during oxidative stress.
Nrf2
The role of the activation of Nuclear factor-erythroid-2-related factor 2 (Nrf2) transcription factor and its repression by Kelchlike ECH-associated protein 1 (Keap1) during oxidative stress has been well established.90–92 The basal expression as well as the induction of genes encoding phase II enzymes are mediated by means of the antioxidant response element (ARE).93 ARE is a cis-acting enhancer sequence that transcriptionally regulates these genes, to maintain the cellular redox status and to protect against oxidative damage. Several studies have demonstrated that Nrf2 is involved in the regulation of ARE-mediated gene expression.90,94 Nrf2 is a member of basic leucine zipper transcription factors and is essential for the coordinated induction of genes that encodes stress-responsive or cytoptotective enzymes and related proteins, such as NQO1, SODs, GSTs, GPx, HO-1, glutamate cysteine ligase (GCL), catalase and thioredoxin. Nrf2 plays an essential role in maintaining cellular homeostasis and hence represents a critical target for prevention of oxidative stress- or inflammation-associated carcinogenesis. Under normal physiological conditions, Nrf2 forms an inactive complex with the negative regulator, Keap1 which controls the subcellular localization and steady-state levels of Nrf2. Cysteine residues present in Keap1 function as redox sensors. Oxidation or chemical modification of some of the highly reactive cysteine residues facilitates the dissociation of Nrf2 from Keap1 and subsequent nuclear translocation.95–97 Therefore, Nrf2 constitutes a unique redox regulator that can be modulated in response to redox imbalance caused by oxidative and electrophilic stresses. Evidences gathered from the Nrf2-deficient mice, demonstrate a strong redox imbalanced system that failed to induce genes responsible for carcinogen detoxification and protection against oxidative stress.98 In addition, levels of pro-inflammatory mediators, such as cyclooxygenase-2 (COX-2), inducible nitric oxide synthase (iNOS), interleukin (IL)-1β, IL-6, and tumor necrosis factor alpha (TNFα), were significantly elevated in the colonic tissues of Nrf2−/− mice as compared to their wild-type counterparts. 99 All of these conditions described above induce generation of ROS in the cells. Thus, it would be highly advantageous to explore the cytoprotective gene expression induced by anticancer compounds with the Nrf2-Keap1 system as a prime molecular target.
In breast cancer cells (MCF-7, T47D and MCF-10A), Nrf2 plays an important role in suppressing oxidative stress rendered by either paraquat or H2O2 by upregulating several phase II detoxification enzymes. On the other hand ectopic expression of wtBRCA1 also stimulate the expression of Nrf2 in the same cells thus indicate an important function of Nrf2 in breast cancer. 34,75,100 Additionally, retinoic acid (RA), which is an analogue of Vitamin A, has been shown to inhibit breast cancer cell growth101 although it is clinically hindered by toxicity possibly related to oxidative stress. At relatively low concentrations RA inhibits Nrf2 and the expression of its target antioxidation enzymes, thus possibly raises the toxicity. Nrf2 enhancement as a therapeutic target of retinoid toxicity awaits further investigation.102 Gammatocopherol (γ-T) alone or in combination with alpha-tocopherol diet to mice [murine prostate cancer model (TRAMP)] has been shown to suppress prostate carcinogenesis by significantly upregulating the expression of Nrf2 and its related detoxifying and antioxidant enzymes, thereby suppressing prostrate intraepithelial neoplasia (PIN) and tumor development.7 More evidences of Nrf2 involvement in prostate cancer is demonstrated by multiple human prostate cancer microarray data sets that revealed that Nrf2 and members of the glutathione-S-transferase (GST) mu family are extensively decreased in human prostate cancer. Loss of Nrf2 initiates a detrimental cascade of reduced GST expression, elevated ROS levels and ultimately DNA damage associated with initiation of cellular transformation in the prostate gland.103
NFκB
The NFκB family of redox transcription factors has been activated in many malignancies including breast, prostate, pancreas, colon, leukemia, lymphoma etc. NFκB activation results in development and/or progression of cancer by regulating the expression of genes involved in cell growth and proliferation, anti-apoptosis, angiogenesis and metastasis.104–108 The NFκB transcription factors are composed of homodimers or heterodimers of Rel proteins, which interact with inhibitory proteins, members of the IκB family. As a consequence of binding to cytoplasmic IκBs, the nuclear localization signal of the NFκB dimer is masked and NFκB is sequestered in the cytoplasm. In response to proinflammatory cytokines such as tumor necrosis factor (TNF) and interleukin-1 (IL-1), bacterial lipopolysaccharide (LPS) or viral double-strand RNA (dsRNA), the IκBs are rapidly phosphorylated and then undergo ubiquitination and proteolysis by the 26S proteasome, resulting in release and translocation of NFκB to the nucleus, where it activates transcription of specific target genes. It is suggested that NFκB activity is regulated by intracellular ROS levels, but the exact molecular mechanism involved in this regulation remains to be elucidated.25,109,110 For example it was shown that ROS overproduced by 4-OHE2 increased the nuclear translocation of NFκB and its DNA binding through induction of IκB kinase alpha and IKKβ activities that contribute to neoplastic transformation of human mammary epithelial cells (MCF-10A).110 Similar effect has been observed with sodium arsenite that mimics the effects of estradiol and induces cell proliferation in the estrogen responsive breast cancer cell line MCF-7. Sodium arsenite stimulate ROS generation followed by oxidative DNA damage. It also induces HO-1 and c-Myc proteins as well as NFκB activation and cell proliferation in human breast cancer MCF-7 cells.111
In certain cell types, such as Wurzburg subclone of T cells, L6 skeletal muscle myotubes, human breast MCF-7 and 70Z/3 pre-B cells, hydrogen peroxide (H2O2) was shown to be an effective inducer of NFκB activation, but in other cell types it does not.112,113 Intracellular level of reduced glutathione (GSH), which may differ from one cell type to another, may be crucial for H2O2-induced NFκB response during oxidative stress. GSH is the major intracellular thiol and an exellent ROS scavenger. N-acetyl-L-cysteine (NAC) is a nontoxic compound that protects cells from oxidative damage and Buthionine-Sulfoximine (BSO) is a drug that causes GSH depletion since it selectively inhibits glutamylcysteine synthetase, the enzyme responsible for GSH synthesis. Preincubation with NAC abolished H2O2-induced NFκB activation in the Wurzburg T cells, while preincubation with BSO demonstrate detectable H2O2-induced NFκB activation in HeLa cells.114,115 Several indirect lines of evidence suggest a role for ROS as a common and critical intermediate for various NFκB-activating signals.25,109,110,116 This conclusion is based largely on the inhibition of NFκB activation by a variety of antioxidants and by overexpression of antioxidant enzymes.117 These reagents have been reported to block NFκB activation in many instances, although the extent of inhibition appears to vary depending on cell type and duration of the stimulus. Overexpression of manganese superoxide dismutase (MnSOD) or GPx abolished NFκB activation induced by TNF, LPS, PMA and H2O2. AP-1 activity, JNK activation and apoptosis induced by TNF were also suppressed by overexpression of MnSOD.118 Molecularly, oxidative stress stimulate the formation of the slow migrating ubiquitinated forms of the NFκB subunit, IκBα, in SDS-polyacrylamide gel, which rapidly degrades unless cells were treated with the proteasome inhibitor.119 Addition of antioxidants or overexpression of peroxidases in the same stressed cells blocked IκBα degradation induced by TNF, PMA and LPS. Taken together, these data suggested that post translational modification of IκBα and subsequent degradation might be the step that is responsive to oxidative stress.
In prostate cancer cells, a constitutive NFκB activity was reported either due to increase in activity of IκB kinase complex or by regulating the expression of c-myc, cyclin D1 and IL6 in the same cells that deregulate the redox homeostasis in the cells. Additionally, expression of androgen receptor was found to be inversely proportional with the activity of NFκB. Several natural products have been successfully tested against prostate cancer progression but the most effective ones are the soy isoflavones such as, genistein and daidzein. Genistein acts as antioxidant and simultaneously inhibits the TNFα induced activation of the redox-sensitive transcription factor, NFκB, in these cells as well as in human lymphocytes. Surprisingly both anti apoptotic and pro apoptotic function of NFκB have been reported in prostate cancer cells that make it difficult to understand the role of NFκB in prostate cancer cells. Similarly, activation of NFκB signaling is responsible in ROS mediated pancreatic cancer progression. Pancreatic stellate cells (PSC) play a pivotal role in the development of pancreatic fibrosis, which is a characteristic feature of chronic pancreatitis and of desmoplastic reaction associated with pancreatic cancer. PSCs activation is important for the development of anti-fibrosis therapy. Recent studies have identified key mediators of stimulatory and inhibitory signals such as peroxisome proliferator-activated receptor-gamma (PPAR-γ), Rho/Rho kinase, NFκB, MAP kinases, phosphatidylinositol 3 kinase (PI3K) and reactive oxygen species (ROS) might be candidates for the development of anti-fibrosis therapy targeting PSCs.120 In human leukemic cells (HL-60) and colon adenocarcinoma cells (LS-174 and WiDr), β-carotene alone or in combination with α-tocopherol or NAC, is associated with significant increase in ROS production and in oxidized glutathione (GSSG) content. These effects were always accompanied by a sustained elevation of NFκB and by a significant inhibition of cell growth that suggests that NFκB induced by β-carotene is involved in the growth-inhibitory and proapoptotic effects of the carotenoid in leukemia and colon adenocarcinoma cells.121 Moreover, diallyl sulfide (DAS), an organosulfur component of garlic, induces apoptosis in colon cancer cells by stimulating the expression of NFκB and Caspase 3. It also suppresses the expression of extracellular regulatory kinase-2 (ERK-2) and inhibits the expression of ROS in the same colon cancer cells.122 Isothiocyanates that are found in cruciferous vegetables such as broccoli, brussels sprouts, cauliflower and cabbage, suggest that cruciferous vegetable intake may lower overall cancer risk generated during oxidative stress, including colon and prostate cancer due to inactivation of NFκB signaling pathway.
Oxidative Stress Signaling through MAP Kinases
Mitogen-activated protein kinases (MAPKs) are the key players of kinase cascades that connect extracellular signals to specific transcription factors, thereby converting these signals into cellular responses. In mammalian systems, there are three subgroups of MAPKs: ERKs (extracellular signal-regulated kinases), JNKs (c-Jun N-terminal kinases) and p38 MAPKs. Growth factors and mitogens use the Ras/Raf/MEK/ERK signaling cascade to transmit signals from their receptors to regulate gene expression and prevent apoptosis in normal condition.123,124 The MAPK signaling cascade is activated by a wide variety of receptors involved in growth and differentiation including receptor tyrosine kinases (RTKs), integrins and ion channels. This pathway has been reported to be activated in over 50% of acute myelogenous leukemia, acute lymphocytic leukemia and are frequently activated in breast, prostate cancers and other cancer types.124–126 Under optimal growth conditions, transiently elevated ROS levels confer a growth advantage to tumor cells. However, exposure of these cells to anticancer agents induces a prolonged increase in ROS levels resulting in potentiation of apoptosis. Thus ROS modulates the ability of stress kinases to stimulate cell growth or cell death and it depends on signal intensity and signal duration.127,128 This idea has been nurtured to explain the complex nature of ERK signaling in cell cycle regulation and in stress activated protein kinase signaling (SAPK). Transient, reduced activity of SAPK promotes cell proliferation, whereas persistent, increased activity results in cell killing.129,130 Conversely, in drug-resistant tumors, phase II enzymes or other antioxidant defenses are often upregulated, shielding cells from apoptosis. ASK1, an upstream regulator of SAPKs, is inhibited in normal cells through its association with thioredoxin, which is an antioxidant capable of metabolizing ROS. Increased levels of ROS lead to the dissociation of this complex and thereby facilitate the activation of ASK1 and subsequently SAPKs.131,132 A similar redox control has been identified for JNK where increased level of ROS triggers the detachment of JNK associated glutathione-S-transferase-π (GSTp) and thereby facilitating JNK activation.133 Moreover, ROS-dependent activation of JNK may also lead to knock down of a JNK phosphatase via an unknown mechanism linking ROS and stress induced kinases an important player in cancer cell growth. Recently it was demonstrated that mammalian stanniocalcin-1 (STC1), which is a glycoprotein, has been implicated in various biological processes including angiogenesis and its aberrant expression has been reported with hormone responsive cancers such as breast, prostate and ovarian cancer. During oxidative stress the expression of STC1 increased several folds that are associated with decrease in ERK1/2 activation in mouse MEFs.134
Several natural phytochemicals exploit the signaling cascades of MAP kinases to exert its effects on the modulation of cancer initiation and progression. Kaempferol is a flavonoid that reduces the cell viability of breast cancer cells by inducing ROS mediated apoptosis and ERK activation as demonstrated by 3D culture conditions.135,136 On the other hand, Acacetin, which is a natural flavone, and stimulate apoptosis in MCF-7, breast cancer cells that is mediated by activation of caspases, ROS generation, mitochondria-mediated cell death signaling and the induction of SAPK/JNK1/2-c-Jun signaling pathway.137 Exposure of MCF-7 and MDA-MB-231 breast cancer cells to kotomolide A (KTA), a new butanolide constituent, resulted in cellular GSH reduction and ROS generation, accompanied by JNK activation and apoptosis.138 When comes to pancreatic cancer, it is very aggressive and unresponsive to treatments due to its resistance to apoptosis. Growth inhibition of pancreatic cells is dependent on the efficiency of scavenging ROS as well as effective inhibition of ERK1/2 signaling pathway activation as demonstrated by using the free radical scavenger NAC or the MEK/ERK1/2 inhibitor (PD98059). Moreover, ERK1/2 induction is dependent on ROS production as demonstrated by a complete removal of ERK1/2 phosphorylation by NAC.139 Thus ROS act as prosurvival, antiapoptotic factor in pancreatic cancer cells. Moreover, treatment of SW620 (colon cancer cells) with berberine, which is a major constituents of Coptidis Thizoma, resulted in activation of apoptosis by phosphorylation of JNK and p38 MAPK, as well as generation of the ROS.140 Furthermore, proline oxidase (POX), that often considered as a ‘housekeeping enzyme’, induce apoptosis through both intrinsic and extrinsic pathways and is involved in nuclear factor of activated T cells (NFAT) signaling and regulation of the MEK/ERK pathway in colon cancer cells. It is suggested that, as a nutrition factor, POX may modulate apoptosis signals induced by p53 or other anti-cancer agents and enhance apoptosis in stress situations.141
Activating Map kinase pathways in prostate cancer cells is often beneficial to stimulate apoptosis and inhibition of growth. Melatonin, the main secretory product of the pineal gland, inhibits the growth of prostate cancer cells (LNCaP) and promotes apoptosis via MAPKs, which are closely associated with apoptosis and survival. Melatonin also activates JNK and p38 kinase whereas extracellular signal-regulated kinase (ERK) was not responsive to melatonin. Thus, melatonin may be of promise for anti-prostate cancer strategies that will utilize the MAP kinase pathways.142 Moreover the well known AKT/mammalian target of rapamycin (AKT/mTOR) and ERK MAPK signaling pathways have been shown to participate in prostate cancer progression. A combinatorial therapy using rapamycin, an inhibitor of mTOR, and PD0325901, an inhibitor of MAPK kinase 1 (MEK; the kinase directly upstream of ERK), inhibits cell growth in cultured prostate cancer cells. Furthermore, analyses of human prostate cancer tissue microarrays demonstrated that AKT/mTOR and ERK MAPK signaling pathways are often deregulated during prostate cancer progression in humans.143 In androgen-independent prostate cancer (PC-3) cells, natural phytochemical, Capsaicin, originated from Red Pepper that has anticarcinogenic, antimutagenic or chemopreventive properties, inhibits cell growth and induces apoptosis through ROS generation. Capsaicin also stimulated the MAP kinase cascades, ERK, JNK and p38 MAPK, to demonstrate its antiproliferative effect but it does not activate p38 MAPK.144 Lastly a new ionic Pd(II) complex, with the metal center coordinated to two different chelating ligands, the pure curcumin (from turmeric) and the 4,4′-dinonyl-2,2′-bipyridine, has been shown to inhibit both cell growth and apoptosis in several human prostate cancer cells, (LnCaP, PC3, and DU145) through the production of ROS and JNK phosphorylation associated with GSTp1 downregulation.145 Thus exploiting the MAP kinase pathway could be an important step towards inhibition of the occurrences of prostate cancer.
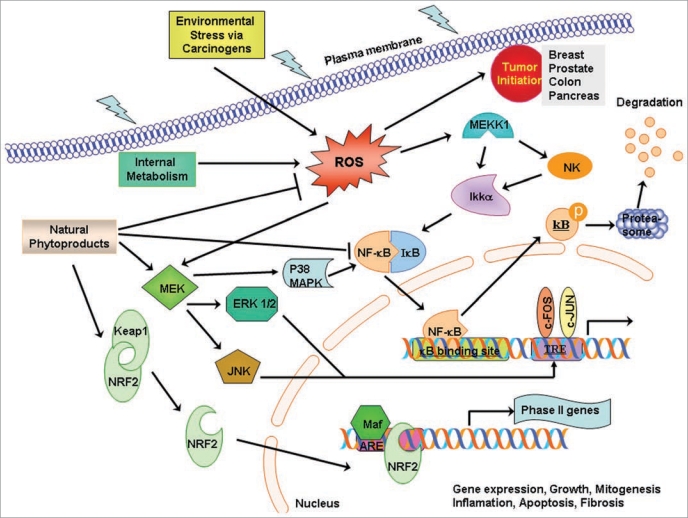
On the basis of what discussed above in regards to the role of oxidative stress in carcinogenesis with emphasis to breast, prostate, colon and pancreatic cancer we generated a pictorial model (Fig. 2) using Motifolio Tool kit (www.motifolio.com). We tried to demonstrate the crosstalk between the molecular mechanisms that occur during the anti-carcinogenic actions of several compounds by exploiting Nrf2, NFκB or MAP kinase pathways when the cells are under oxidative stress.
Figure 2.
A putative model for oxidative stress induced interactions in carcinogenesis. Reactive oxygen species (ROS) mediated oxidative stress either by environmental carcinogens such as UV and ionizing radiation or by mitochondrial metabolism exerts several effects on DNA damage and generation of oxidative lesions, gene expression, growth regulation mitogenesis, inflammation, apoptosis and fibrosis leading to genomic instability and cancer progression. Chemical signals generated by dietary chemopreventive agents, anticancer agents, antioxidants and antioxidation enzymes, cause Nrf2 nuclear translocation that sets in motion a dynamic machinery of coactivators and corepressors that might form a multimolecular complex with Nrf2 for modulating transcriptional response through the antioxidant response element, ARE producing several phase II detoxification enzymes as stimulation of cellular defense system during stress. Oxidative stress might also cause release of NFκB from IκB and stimulate NFκB nuclear translocation to modulate transcriptional response through the NFκB response element. Several members of the MAPK family may act in concert with Nrf2 and NFκB with multiple interactions between the members of the putative complex to elicit the chemopreventive and pharmacotoxicological events against carcinogenesis.
Concluding Remarks and Future Perspectives
Redox adaptation is an important concept that cancer cells undertake to survive, under persistent endogenous ROS stress and become resistant to certain anticancer agents. Redox-modulating strategies to target these biochemical properties of cancer cells will be a feasible therapeutic approach that may enable therapeutic selectivity and to overcome drug resistance. One of the best strategies is to increase the ROS metabolizing capacity of the agents (antioxidants and antioxidation enzymes) that subsequently suppress the tumor growth. But, there are reports that using antioxidants in clinical trials are associated with increased cancer incidences, probably due to the inhibition of ROS mediated apoptosis of cancer cells. In addition, there is experimental evidence that antioxidants (e.g.,: paclitaxel and bortezomib) and radiation therapy, could actually decrease the ROS-mediated anti-tumor activity of the anticancer agents.146,147 An alternative approach is to treat cancer cells with pharmacological agents that have pro-oxidant properties, which increase ROS generation or abrogate the cellular antioxidant systems in the tumor itself. Cancer stem cells are highly resistant to anticancer drugs and might use the same redox adaptation as normal stem cells, for their survival. An approach that can break this redox adaptation by depleting the main antioxidant pool from the cells might be beneficial to eliminate the cancer stem cells. Studies showing that a compound known as TDZD-8 (4-benzyl-2-methyl- 1,2,4-thiadiazolidine-3,5-dione) can induce the depletion of thiols, leading to a rapid accumulation of ROS and selectively kill leukaemic cells expressing stem-cell markers with minimal toxicity to normal haemopoietic stem cells,148 highlights this as an important research direction.
Molecularly, it has become clear that cancer results from alterations and aberrations in several hundred genes, indicating that a tumor cell uses multiple pathways to survive and thrive. A definitive role of selected dietary naturally occurring products for prevention and treatment of cancer is now getting high popularity. The challenge is how best to use this information for cancer prevention in populations with differing cancer risk. One way to address this problem is to design potent mixture of several phytochemicals from plant and fruit sources that could have an additive and synergistic effect to inhibit several molecular pathways required by cancer cells to survive. Such cocktails will have greater likelihood for producing cancer chemopreventive effects in humans than individual components. Bioavailability is one of the critical issues to be discussed even before considering the beneficial effects of several phytochemicals because metabolism of the dietary phytochemicals and their biological properties depends on their presence at the time and site of the damage. Another issue of concern is whether purified phytochemicals have the same protective effects, as do the whole food or mixture of foods in which these compounds are present. The current knowledge base teaches us that they are generally more effective when consumed as whole foods.
Acknowledgements
T.S. is thankful to American Cancer Society (IRG #97-152-16-2), Fisher Center for Familial Cancer Center, Lombardi Comprehensive Cancer Center, Georgetown University for financial support.
Abbreviations
- DMBA
7-12 dimethylbenz [a] anthracene
- GPx
glutathione peroxidase
- GST
glutathione-S-transferase
- SOD
superoxide dismutase
- HO-1
heam oxygenase 1
- ER
estrogen receptor
- PR
progesterone receptor
- LPS
lipopolysaccharide
- TNF
tumor necrosis factor
- GCL
glutamate cysteine ligase
- SAPK
stress-activated protein kinase
- JNK
Jun-amino-terminal kinase
- PMA
phorbol 12-myristate 13-acetate
- NQO1
NAD(P)H quinone oxidoreductase 1
- ARE
antioxidant response element
- TRX
thioredoxins
- GRX
glutaredoxins
Footnotes
Previously published online: www.landesbioscience.com/journals/oximed/article/10095
References
- 1.Burhans WC, Weinberger M. DNA replication stress, genome instability and aging. Nucleic Acids Res. 2007;35:7545–7556. doi: 10.1093/nar/gkm1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Khandrika L, Kumar B, Koul S, Maroni P, Koul HK. Oxidative stress in prostate cancer. Cancer Lett. 2009;282:125–136. doi: 10.1016/j.canlet.2008.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Khansari N, Shakiba Y, Mahmoudi M. Chronic inflammation and oxidative stress as a major cause of age-related diseases and cancer. Recent Pat Inflamm Allergy Drug Discov. 2009;3:73–80. doi: 10.2174/187221309787158371. [DOI] [PubMed] [Google Scholar]
- 4.Addabbo F, Montagnani M, Goligorsky MS. Mitochondria and reactive oxygen species. Hypertension. 2009;53:885–892. doi: 10.1161/HYPERTENSIONAHA.109.130054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Archer SL, Gomberg-Maitland M, Maitland ML, Rich S, Garcia JG, Weir EK. Mitochondrial metabolism, redox signaling and fusion: a mitochondria-ROS-HIF-1alpha-KV1.5 O2-sensing pathway at the intersection of pulmonary hypertension and cancer. Am J Physiol Heart Circ Physiol. 2008;294:570–578. doi: 10.1152/ajpheart.01324.2007. [DOI] [PubMed] [Google Scholar]
- 6.Pool-Zobel B, Veeriah S, Bohmer FD. Modulation of xenobiotic metabolising enzymes by anticarcinogens—focus on glutathione S-transferases and their role as targets of dietary chemoprevention in colorectal carcinogenesis. Mutat Res. 2005;591:74–92. doi: 10.1016/j.mrfmmm.2005.04.020. [DOI] [PubMed] [Google Scholar]
- 7.Barve A, Khor TO, Nair S, Reuhl K, Suh N, Reddy B, et al. Gamma-tocopherol-enriched mixed tocopherol diet inhibits prostate carcinogenesis in TRAMP mice. Int J Cancer. 2009;124:1693–1699. doi: 10.1002/ijc.24106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kumaraguruparan R, Seshagiri PB, Hara Y, Nagini S. Chemoprevention of rat mammary carcinogenesis by black tea polyphenols: modulation of xenobioticmetabolizing enzymes, oxidative stress, cell proliferation, apoptosis and angiogenesis. Mol Carcinog. 2007;46:797–806. doi: 10.1002/mc.20309. [DOI] [PubMed] [Google Scholar]
- 9.Lee SB, Kim CY, Lee HJ, Yun JH, Nho CW. Induction of the Phase II Detoxification Enzyme NQO1 in Hepatocarcinoma Cells by Lignans from the Fruit of Schisandra chinensis through Nuclear Accumulation of Nrf2. Planta Med. 2009;18:18. doi: 10.1055/s-0029-1185685. [DOI] [PubMed] [Google Scholar]
- 10.Nair S, Li W, Kong AN. Natural dietary anti-cancer chemopreventive compounds: redox-mediated differential signaling mechanisms in cytoprotection of normal cells versus cytotoxicity in tumor cells. Acta Pharmacol Sin. 2007;28:459–472. doi: 10.1111/j.1745-7254.2007.00549.x. [DOI] [PubMed] [Google Scholar]
- 11.Naithani R. Organoselenium compounds in cancer chemoprevention. Mini Rev Med Chem. 2008;8:657–668. doi: 10.2174/138955708784567368. [DOI] [PubMed] [Google Scholar]
- 12.Fearon IM, Faux SP. Oxidative stress and cardiovascular disease: novel tools give (free) radical insight. J Mol Cell Cardiol. 2009;47:372–381. doi: 10.1016/j.yjmcc.2009.05.013. [DOI] [PubMed] [Google Scholar]
- 13.Okamura DM, Himmelfarb J. Tipping the redox balance of oxidative stress in fibrogenic pathways in chronic kidney disease. Pediatr Nephrol. 2009;7:7. doi: 10.1007/s00467-009-1199-5. [DOI] [PubMed] [Google Scholar]
- 14.Reddy VP, Zhu X, Perry G, Smith MA. Oxidative stress in diabetes and Alzheimer’s disease. J Alzheimers Dis 2. 2009;16:763–774. doi: 10.3233/JAD-2009-1013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wells PG, McCallum GP, Chen CS, Henderson JT, Lee CJ, Perstin J, et al. Oxidative stress in developmental origins of disease: teratogenesis, neurodevelopmental deficits and cancer. Toxicol Sci. 2009;108:4–18. doi: 10.1093/toxsci/kfn263. [DOI] [PubMed] [Google Scholar]
- 16.Wu D, Cederbaum AI. Oxidative stress and alcoholic liver disease. Semin Liver Dis. 2009;29:141–154. doi: 10.1055/s-0029-1214370. [DOI] [PubMed] [Google Scholar]
- 17.Zawia NH, Lahiri DK, Cardozo-Pelaez F. Epigenetics, oxidative stress and Alzheimer disease. Free Radic Biol Med. 2009;46:1241–1249. doi: 10.1016/j.freeradbiomed.2009.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Valko M, Rhodes CJ, Moncol J, Izakovic M, Mazur M. Free radicals, metals and antioxidants in oxidative stress-induced cancer. Chem Biol Interact. 2006;160:1–40. doi: 10.1016/j.cbi.2005.12.009. [DOI] [PubMed] [Google Scholar]
- 19.Bartsch H, Nair J. Chronic inflammation and oxidative stress in the genesis and perpetuation of cancer: role of lipid peroxidation, DNA damage and repair. Langenbecks Arch Surg. 2006;391:499–510. doi: 10.1007/s00423-006-0073-1. [DOI] [PubMed] [Google Scholar]
- 20.Barzilai A, Yamamoto K. DNA damage responses to oxidative stress. DNA Repair. 2004;3:1109–1115. doi: 10.1016/j.dnarep.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 21.Tsutsui H, Ide T, Kinugawa S. Mitochondrial oxidative stress, DNA damage and heart failure. Antioxid Redox Signal. 2006;8:1737–1744. doi: 10.1089/ars.2006.8.1737. [DOI] [PubMed] [Google Scholar]
- 22.Cooke MS, Evans MD, Dizdaroglu M, Lunec J. Oxidative DNA damage: mechanisms, mutation and disease. Faseb J. 2003;17:1195–1214. doi: 10.1096/fj.02-0752rev. [DOI] [PubMed] [Google Scholar]
- 23.Marnett LJ. Oxyradicals and DNA damage. Carcinogenesis. 2000;21:361–370. doi: 10.1093/carcin/21.3.361. [DOI] [PubMed] [Google Scholar]
- 24.Bailey DT, DeFedericis HC, Greene KF, Iijima H, Budzinski EE, Patrzyc HB, et al. A novel approach to DNA damage assessments: measurement of the thymine glycol lesion. Radiat Res. 2006;165:438–444. doi: 10.1667/rr3534.1. [DOI] [PubMed] [Google Scholar]
- 25.Mambo E, Nyaga SG, Bohr VA, Evans MK. Defective repair of 8-hydroxyguanine in mitochondria of MCF-7 and MDA-MB-468 human breast cancer cell lines. Cancer Res. 2002;62:1349–1355. [PubMed] [Google Scholar]
- 26.Valavanidis A, Vlachogianni T, Fiotakis C. 8-hydroxy-2′-deoxyguanosine (8-OHdG): A critical biomarker of oxidative stress and carcinogenesis. J Environ Sci Health C Environ Carcinog Ecotoxicol Rev. 2009;27:120–139. doi: 10.1080/10590500902885684. [DOI] [PubMed] [Google Scholar]
- 27.Sheweita SA, Tilmisany AK. Cancer and phase II drug-metabolizing enzymes. Curr Drug Metab. 2003;4:45–58. doi: 10.2174/1389200033336919. [DOI] [PubMed] [Google Scholar]
- 28.Vaquero EC, Edderkaoui M, Pandol SJ, Gukovsky I, Gukovskaya AS. Reactive oxygen species produced by NAD(P)H oxidase inhibit apoptosis in pancreatic cancer cells. J Biol Chem. 2004;279:34643–34654.8. doi: 10.1074/jbc.M400078200. [DOI] [PubMed] [Google Scholar]
- 29.Vizan P, Alcarraz-Vizan G, Diaz-Moralli S, Solovjeva ON, Frederiks WM, Cascante M. Modulation of pentose phosphate pathway during cell cycle progression in human colon adenocarcinoma cell line HT29. Int J Cancer. 2009;124:2789–2796. doi: 10.1002/ijc.24262. [DOI] [PubMed] [Google Scholar]
- 30.Inokuma T, Haraguchi M, Fujita F, Tajima Y, Kanematsu T. Oxidative stress and tumor progression in colorectal cancer. Hepatogastroenterology. 2009;56:343–347. [PubMed] [Google Scholar]
- 31.Huang F, Nie C, Yang Y, Yue W, Ren Y, Shang Y, et al. Selenite induces redox-dependent Bax activation and apoptosis in colorectal cancer cells. Free Radic Biol Med. 2009;46:1186–1196. doi: 10.1016/j.freeradbiomed.2009.01.026. [DOI] [PubMed] [Google Scholar]
- 32.Rosen EM, Fan S, Isaacs C. BRCA1 in hormonal carcinogenesis: basic and clinical research. Endocr Relat Cancer. 2005;12:533–548. doi: 10.1677/erc.1.00972. [DOI] [PubMed] [Google Scholar]
- 33.Rosen EM, Fan S, Pestell RG, Goldberg ID. BRCA1 gene in breast cancer. J Cell Physiol. 2003;196:19–41. doi: 10.1002/jcp.10257. [DOI] [PubMed] [Google Scholar]
- 34.Bae I, Fan S, Meng Q, Rih JK, Kim HJ, Kang HJ, et al. BRCA1 induces antioxidant gene expression and resistance to oxidative stress. Cancer Res. 2004;64:7893–7909. doi: 10.1158/0008-5472.CAN-04-1119. [DOI] [PubMed] [Google Scholar]
- 35.Cao L, Xu X, Cao LL, Wang RH, Coumoul X, Kim SS, et al. Absence of full-length Brca1 sensitizes mice to oxidative stress and carcinogen-induced tumorigenesis in the esophagus and forestomach. Carcinogenesis. 2007;28:1401–1407. doi: 10.1093/carcin/bgm060. [DOI] [PubMed] [Google Scholar]
- 36.Xu X, Qiao W, Linke SP, Cao L, Li WM, Furth PA, et al. Genetic interactions between tumor suppressors Brca1 and p53 in apoptosis, cell cycle and tumorigenesis. Nat Genet. 2001;28:266–271. doi: 10.1038/90108. [DOI] [PubMed] [Google Scholar]
- 37.Saha T, Rih JK, Rosen EM. BRCA1 downregulates cellular levels of reactive oxygen species. FEBS Lett. 2009;583:1535–1543. doi: 10.1016/j.febslet.2009.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kang HJ, Kim HJ, Kim SK, Barouki R, Cho CH, Khanna KK, et al. BRCA1 modulates xenobiotic stress-inducible gene expression by interacting with ARNT in human breast cancer cells. J Biol Chem. 2006;281:14654–14662. doi: 10.1074/jbc.M601613200. [DOI] [PubMed] [Google Scholar]
- 39.Jeon BH, Irani K. APE1/Ref-1: Versatility in Progress. Antioxid Redox Signal. 2008;20:20. doi: 10.1089/ars.2008.2223. [DOI] [PubMed] [Google Scholar]
- 40.Seo Y, Kinsella TJ. Essential Role of DNA Base Excision Repair on Survival in an Acidic Tumor Microenvironment. Cancer Res. 2009;1:1. doi: 10.1158/0008-5472.CAN-09-0624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shao C, Folkard M, Held KD, Prise KM. Estrogen enhanced cell-cell signalling in breast cancer cells exposed to targeted irradiation. BMC Cancer. 2008;8:184. doi: 10.1186/1471-2407-8-184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nagai MA, Ros N, Bessa SA, Mourao Neto M, Miracca EC, Brentani MM. Differentially expressed genes and estrogen receptor status in breast cancer. Int J Oncol. 2003;23:1425–1430. [PubMed] [Google Scholar]
- 43.Wang Z, Wijewickrama GT, Peng KW, Dietz BM, Yuan L, van Breemen RB, et al. Estrogen Receptor {alpha} Enhances the Rate of Oxidative DNA Damage by Targeting an Equine Estrogen Catechol Metabolite to the Nucleus. J Biol Chem. 2009;284:8633–8642. doi: 10.1074/jbc.M807860200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Weitsman GE, Weebadda W, Ung K, Murphy LC. Reactive oxygen species induce phosphorylation of serine 118 and 167 on estrogen receptor alpha. Breast Cancer Res Treat. 2008;21:21. doi: 10.1007/s10549-008-0221-0. [DOI] [PubMed] [Google Scholar]
- 45.Fernandez SV, Russo IH, Russo J. Estradiol and its metabolites 4-hydroxyestradiol and 2-hydroxyestradiol induce mutations in human breast epithelial cells. Int J Cancer. 2006;118:1862–1868. doi: 10.1002/ijc.21590. [DOI] [PubMed] [Google Scholar]
- 46.Fan S, Meng Q, Gao B, Grossman J, Yadegari M, Goldberg ID, et al. Alcohol stimulates estrogen receptor signaling in human breast cancer cell lines. Cancer Res. 2000;60:5635–5639. [PubMed] [Google Scholar]
- 47.Razandi M, Pedram A, Rosen EM, Levin ER. BRCA1 inhibits membrane estrogen and growth factor receptor signaling to cell proliferation in breast cancer. Mol Cell Biol. 2004;24:5900–5913. doi: 10.1128/MCB.24.13.5900-5913.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cavalieri E, Chakravarti D, Guttenplan J, Hart E, Ingle J, Jankowiak R, et al. Catechol estrogen quinones as initiators of breast and other human cancers: implications for biomarkers of susceptibility and cancer prevention. Biochim Biophys Acta. 2006;1766:63–78. doi: 10.1016/j.bbcan.2006.03.001. [DOI] [PubMed] [Google Scholar]
- 49.Mitra PS, Basu NK, Owens IS. Src supports UDP-glucuronosyltransferase-2B7 detoxification of catechol estrogens associated with breast cancer. Biochem Biophys Res Commun. 2009;382:651–656. doi: 10.1016/j.bbrc.2009.03.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Dabrosin C, Hammar M, Ollinger K. Impact of oestradiol and progesterone on antioxidant activity in normal human breast epithelial cells in culture. Free Radic Res. 1998;28:241–249. doi: 10.3109/10715769809069276. [DOI] [PubMed] [Google Scholar]
- 51.Mobley JA, Brueggemeier RW. Estrogen receptormediated regulation of oxidative stress and DNA damage in breast cancer. Carcinogenesis. 2004;25:3–9. doi: 10.1093/carcin/bgg175. [DOI] [PubMed] [Google Scholar]
- 52.Rao A, Ziegler Y, McLeod I, Yates J, Nardulli A. Thioredoxin and thioredoxin reductase influence estrogen receptor {alpha} mediated gene expression in human breast cancer cells. J Mol Endocrinol. 2009;20:20. doi: 10.1677/JME-09-0053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Benz CC, Atsriku C, Yau C, Britton D, Schilling B, Gibson BW, et al. Novel pathways associated with quinone-induced stress in breast cancer cells. Drug Metab Rev. 2006;38:601–613. doi: 10.1080/03602530600959391. [DOI] [PubMed] [Google Scholar]
- 54.Yau C, Benz CC. Genes responsive to both oxidant stress and loss of estrogen receptor function identify a poor prognosis group of estrogen receptor positive primary breast cancers. Breast Cancer Res. 2008;10:17. doi: 10.1186/bcr2120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Katiyar P, Ma Y, Fan S, Pestell RG, Furth PA, Rosen EM. Regulation of progesterone receptor signaling by BRCA1 in mammary cancer. Nucl Recept Signal. 2006;4:28. doi: 10.1621/nrs.04006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Katiyar P, Ma Y, Riegel A, Fan S, Rosen EM. Mechanism of BRCA1-mediated inhibition of progesterone receptor transcriptional activity. Mol Endocrinol. 2009;23:1135–1146. doi: 10.1210/me.2008-0347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Diehn M, Cho RW, Lobo NA, Kalisky T, Dorie MJ, Kulp AN, et al. Association of reactive oxygen species levels and radioresistance in cancer stem cells. Nature. 2009;458:780–783. doi: 10.1038/nature07733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Jang YY, Sharkis SJ. A low level of reactive oxygen species selects for primitive hematopoietic stem cells that may reside in the low-oxygenic niche. Blood. 2007;110:3056–3063. doi: 10.1182/blood-2007-05-087759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Naka K, Muraguchi T, Hoshii T, Hirao A. Regulation of reactive oxygen species and genomic stability in hematopoietic stem cells. Antioxid Redox Signal. 2008;10:1883–1894. doi: 10.1089/ars.2008.2114. [DOI] [PubMed] [Google Scholar]
- 60.Ogasawara MA, Zhang H. Redox Regulation and its Emerging Roles in Stem Cells and Stem-Like Cancer Cells. Antioxid Redox Signal. 2008;11:11. doi: 10.1089/ars.2008.2308. [DOI] [PubMed] [Google Scholar]
- 61.Blum R, Gupta R, Burger PE, Ontiveros CS, Salm SN, Xiong X, et al. Molecular signatures of prostate stem cells reveal novel signaling pathways and provide insights into prostate cancer. PLoS One. 2009;4:5722. doi: 10.1371/journal.pone.0005722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Boman BM, Huang E. Human colon cancer stem cells: a new paradigm in gastrointestinal oncology. J Clin Oncol. 2008;26:2828–2838. doi: 10.1200/JCO.2008.17.6941. [DOI] [PubMed] [Google Scholar]
- 63.Hill R, Wu H. PTEN, stem cells and cancer stem cells. J Biol Chem. 2009;284:11755–11759. doi: 10.1074/jbc.R800071200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Morel AP, Lievre M, Thomas C, Hinkal G, Ansieau S, Puisieux A. Generation of breast cancer stem cells through epithelial-mesenchymal transition. PLoS One. 2008;3:2888. doi: 10.1371/journal.pone.0002888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Tang Y, Kitisin K, Jogunoori W, Li C, Deng CX, Mueller SC, et al. Progenitor/stem cells give rise to liver cancer due to aberrant TGFbeta and IL-6 signaling. Proc Natl Acad Sci USA. 2008;105:2445–2450. doi: 10.1073/pnas.0705395105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Tothova Z, Gilliland DG. FoxO transcription factors and stem cell homeostasis: insights from the hematopoietic system. Cell Stem Cell. 2007;1:140–152. doi: 10.1016/j.stem.2007.07.017. [DOI] [PubMed] [Google Scholar]
- 67.Ito K, Bernardi R, Pandolfi PP. A novel signaling network as a critical rheostat for the biology and maintenance of the normal stem cell and the cancerinitiating cell. Curr Opin Genet Dev. 2009;19:51–59. doi: 10.1016/j.gde.2009.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Tothova Z, Gilliland DG. A radical bailout strategy for cancer stem cells. Cell Stem Cell. 2009;4:196–197. doi: 10.1016/j.stem.2009.02.008. [DOI] [PubMed] [Google Scholar]
- 69.Arner ES, Holmgren A. The thioredoxin system in cancer. Semin Cancer Biol. 2006;16:420–426. doi: 10.1016/j.semcancer.2006.10.009. [DOI] [PubMed] [Google Scholar]
- 70.Noike T, Miwa S, Soeda J, Kobayashi A, Miyagawa S. Increased expression of thioredoxin-1, vascular endothelial growth factor, and redox factor-1 is associated with poor prognosis in patients with liver metastasis from colorectal cancer. Hum Pathol. 2008;39:201–208. doi: 10.1016/j.humpath.2007.04.024. [DOI] [PubMed] [Google Scholar]
- 71.Michelet L, Zaffagnini M, Massot V, Keryer E, Vanacker H, Miginiac-Maslow M, et al. Thioredoxins, glutaredoxins and glutathionylation: new crosstalks to explore. Photosynth Res. 2006;89:225–245. doi: 10.1007/s11120-006-9096-2. [DOI] [PubMed] [Google Scholar]
- 72.Tsai CM, Levitzki A, Wu LH, Chang KT, Cheng CC, Gazit A, et al. Enhancement of chemosensitivity by tyrphostin AG825 in high-p185(neu) expressing non-small cell lung cancer cells. Cancer Res. 1996;56:1068–1074. [PubMed] [Google Scholar]
- 73.Nagane M, Levitzki A, Gazit A, Cavenee WK, Huang HJ. Drug resistance of human glioblastoma cells conferred by a tumor-specific mutant epidermal growth factor receptor through modulation of Bcl-XL and caspase-3-like proteases. Proc Natl Acad Sci USA. 1998;95:5724–5729. doi: 10.1073/pnas.95.10.5724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Pegram MD, Lopez A, Konecny G, Slamon DJ. Trastuzumab and chemotherapeutics: drug interactions and synergies. Semin Oncol. 2000;27:21–25. [PubMed] [Google Scholar]
- 75.Fan S, Meng Q, Saha T, Sarkar FH, Rosen EM. Low concentrations of diindolylmethane, a metabolite of indole-3-carbinol, protect against oxidative stress in a BRCA1-dependent manner. Cancer Res. 2009;69:6083–6091. doi: 10.1158/0008-5472.CAN-08-3309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Fan S, Meng Q, Auborn K, Carter T, Rosen EM. BRCA1 and BRCA2 as molecular targets for phytochemicals indole-3-carbinol and genistein in breast and prostate cancer cells. Br J Cancer. 2006;94:407–426. doi: 10.1038/sj.bjc.6602935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Banerjee S, Li Y, Wang Z, Sarkar FH. Multi-targeted therapy of cancer by genistein. Cancer Lett. 2008;269:226–242. doi: 10.1016/j.canlet.2008.03.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Hatcher H, Planalp R, Cho J, Torti FM, Torti SV. Curcumin: from ancient medicine to current clinical trials. Cell Mol Life Sci. 2008;65:1631–1652. doi: 10.1007/s00018-008-7452-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Basu NK, Kole L, Basu M, Chakraborty K, Mitra PS, Owens IS. The major chemical-detoxifying system of UDP-glucuronosyltransferases requires regulated phosphorylation supported by protein kinase C. J Biol Chem. 2008;283:23048–23061. doi: 10.1074/jbc.M800032200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Basu NK, Kovarova M, Garza A, Kubota S, Saha T, Mitra PS, et al. Phosphorylation of a UDP-glucuronosyltransferase regulates substrate specificity. Proc Natl Acad Sci USA. 2005;102:6285–6290. doi: 10.1073/pnas.0407872102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Basu NK, Kole L, Basu M, McDonagh AF, Owens IS. Targeted inhibition of glucuronidation markedly improves drug efficacy in mice-a model. Biochem Biophys Res Commun. 2007;360:7–13. doi: 10.1016/j.bbrc.2007.05.224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Bhattacharjee S, Rana T, Sengupta A. Inhibition of lipid peroxidation and enhancement of GST activity by cardamom and cinnamon during chemically induced colon carcinogenesis in Swiss albino mice. Asian Pac J Cancer Prev. 2007;8:578–582. [PubMed] [Google Scholar]
- 83.Das I, Chakrabarty RN, Das S. Saffron can prevent chemically induced skin carcinogenesis in Swiss albino mice. Asian Pac J Cancer Prev. 2004;5:70–76. [PubMed] [Google Scholar]
- 84.Das I, Das S, Saha T. Saffron suppresses oxidative stress in DMBA-induced skin carcinoma: A histopathological study. Acta Histochem. 2009;26:26. doi: 10.1016/j.acthis.2009.02.003. [DOI] [PubMed] [Google Scholar]
- 85.Das I, Saha T. Effect of garlic on lipid peroxidation and antioxidation enzymes in DMBA-induced skin carcinoma. Nutrition. 2009;25:459–471. doi: 10.1016/j.nut.2008.10.014. [DOI] [PubMed] [Google Scholar]
- 86.Kaefer CM, Milner JA. The role of herbs and spices in cancer prevention. J Nutr Biochem. 2008;19:347–361. doi: 10.1016/j.jnutbio.2007.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Salim EI, Fukushima S. Chemopreventive potential of volatile oil from black cumin (Nigella sativa L.) seeds against rat colon carcinogenesis. Nutr Cancer. 2003;45:195–202. doi: 10.1207/S15327914NC4502_09. [DOI] [PubMed] [Google Scholar]
- 88.Giles GI. The redox regulation of thiol dependent signaling pathways in cancer. Curr Pharm Des. 2006;12:4427–4443. doi: 10.2174/138161206779010549. [DOI] [PubMed] [Google Scholar]
- 89.Tew KD. Redox in redux: Emergent roles for glutathione S-transferase P (GSTP) in regulation of cell signaling and S-glutathionylation. Biochem Pharmacol. 2007;73:1257–1269. doi: 10.1016/j.bcp.2006.09.027. [DOI] [PubMed] [Google Scholar]
- 90.Copple IM, Goldring CE, Kitteringham NR, Park BK. The Nrf2-Keap1 defence pathway: role in protection against drug-induced toxicity. Toxicology. 2008;246:24–33. doi: 10.1016/j.tox.2007.10.029. [DOI] [PubMed] [Google Scholar]
- 91.Itoh K. Protective mechanism against oxidative stress by Keap1/Nrf2 pathway. Seikagaku. 2006;78:79–92. [PubMed] [Google Scholar]
- 92.Zhang DD. Mechanistic studies of the Nrf2-Keap1 signaling pathway. Drug Metab Rev. 2006;38:769–789. doi: 10.1080/03602530600971974. [DOI] [PubMed] [Google Scholar]
- 93.Lee JM, Johnson JA. An important role of Nrf2-ARE pathway in the cellular defense mechanism. J Biochem Mol Biol. 2004;37:139–143. doi: 10.5483/bmbrep.2004.37.2.139. [DOI] [PubMed] [Google Scholar]
- 94.Kobayashi M, Yamamoto M. Nrf2-Keap1 regulation of cellular defense mechanisms against electrophiles and reactive oxygen species. Adv Enzyme Regul. 2006;46:113–140. doi: 10.1016/j.advenzreg.2006.01.007. [DOI] [PubMed] [Google Scholar]
- 95.Ding Y, Choi KJ, Kim JH, Han X, Piao Y, Jeong JH, et al. Endogenous hydrogen peroxide regulates glutathione redox via nuclear factor erythroid 2-related factor 2 downstream of phosphatidylinositol 3-kinase during muscle differentiation. Am J Pathol. 2008;172:1529–1541. doi: 10.2353/ajpath.2008.070429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Hsieh CY, Hsiao HY, Wu WY, Liu CA, Tsai YC, Chao YJ, et al. Regulation of shear-induced nuclear translocation of the Nrf2 transcription factor in endothelial cells. J Biomed Sci. 2009;16:12. doi: 10.1186/1423-0127-16-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Surh YJ, Kundu JK, Na HK. Nrf2 as a master redox switch in turning on the cellular signaling involved in the induction of cytoprotective genes by some chemopreventive phytochemicals. Planta Med. 2008;74:1526–1539. doi: 10.1055/s-0028-1088302. [DOI] [PubMed] [Google Scholar]
- 98.Harvey CJ, Thimmulappa RK, Singh A, Blake DJ, Ling G, Wakabayashi N, et al. Nrf2-regulated glutathione recycling independent of biosynthesis is critical for cell survival during oxidative stress. Free Radic Biol Med. 2009;46:443–453. doi: 10.1016/j.freeradbiomed.2008.10.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Jin W, Wang H, Yan W, Xu L, Wang X, Zhao X, et al. Disruption of Nrf2 enhances upregulation of nuclear factor-kappaB activity, proinflammatory cytokines, and intercellular adhesion molecule-1 in the brain after traumatic brain injury. Mediators Inflamm. 2008;725174:25. doi: 10.1155/2008/725174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Kim SK, Yang JW, Kim MR, Roh SH, Kim HG, Lee KY, et al. Increased expression of Nrf2/AREdependent anti-oxidant proteins in tamoxifen-resistant breast cancer cells. Free Radic Biol Med. 2008;45:537–546. doi: 10.1016/j.freeradbiomed.2008.05.011. [DOI] [PubMed] [Google Scholar]
- 101.Czeczuga-Semeniuk E, Jarzabek K, Lemancewicz D, Wolczynski S. The vitamin A family can significantly decrease the expression of ERbeta of ERs positive breast cancer cells in the presence or absence of ER ligands and paclitaxel. Gynecol Endocrinol. 2009;26:1–7. doi: 10.1080/09513590802530924. [DOI] [PubMed] [Google Scholar]
- 102.Tan KP, Kosuge K, Yang M, Ito S. NRF2 as a determinant of cellular resistance in retinoic acid cytotoxicity. Free Radic Biol Med. 2008;45:1663–1673. doi: 10.1016/j.freeradbiomed.2008.09.010. [DOI] [PubMed] [Google Scholar]
- 103.Frohlich DA, McCabe MT, Arnold RS, Day ML. The role of Nrf2 in increased reactive oxygen species and DNA damage in prostate tumorigenesis. Oncogene. 2008;27:4353–4362. doi: 10.1038/onc.2008.79. [DOI] [PubMed] [Google Scholar]
- 104.Antunes F, Han D. Redox Regulation of NFkappaB: from basic to clinical research. Antioxid Redox Signal. 2009;13:13. doi: 10.1089/ars.2009.2659. [DOI] [PubMed] [Google Scholar]
- 105.Hagemann T, Biswas SK, Lawrence T, Sica A, Lewis CE. Regulation of macrophage function in tumors: the multifaceted role of NFkappaB. Blood. 2009;113:3139–3146. doi: 10.1182/blood-2008-12-172825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Kim YS, Young MR, Bobe G, Colburn NH, Milner JA. Bioactive food components, inflammatory targets and cancer prevention. Cancer Prev Res (Phila Pa) 2009;2:200–208. doi: 10.1158/1940-6207.CAPR-08-0141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Mauro C, Zazzeroni F, Papa S, Bubici C, Franzoso G. The NFkappaB transcription factor pathway as a therapeutic target in cancer: methods for detection of NFkappaB activity. Methods Mol Biol. 2009;512:169–207. doi: 10.1007/978-1-60327-530-9_10. [DOI] [PubMed] [Google Scholar]
- 108.Zhu F, Park E, Liu B, Xia X, Fischer SM, Hu Y. Critical role of IkappaB kinase alpha in embryonic skin development and skin carcinogenesis. Histol Histopathol. 2009;24:265–271. doi: 10.14670/HH-24.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Kiessling MK, Klemke CD, Kaminski MM, Galani IE, Krammer PH, Gulow K. Inhibition of constitutively activated nuclear factor-kappaB induces reactive oxygen species- and iron-dependent cell death in cutaneous T-cell lymphoma. Cancer Res. 2009;69:2365–2374. doi: 10.1158/0008-5472.CAN-08-3221. [DOI] [PubMed] [Google Scholar]
- 110.Park SA, Na HK, Kim EH, Cha YN, Surh YJ. 4-hydroxyestradiol induces anchorage-independent growth of human mammary epithelial cells via activation of IkappaB kinase: potential role of reactive oxygen species. Cancer Res. 2009;69:2416–2424. doi: 10.1158/0008-5472.CAN-08-2177. [DOI] [PubMed] [Google Scholar]
- 111.Ruiz-Ramos R, Lopez-Carrillo L, Rios-Perez AD, De Vizcaya-Ruiz A, Cebrian ME. Sodium arsenite induces ROS generation, DNA oxidative damage, HO-1 and c-Myc proteins, NFkappaB activation and cell proliferation in human breast cancer MCF-7 cells. Mutat Res. 2009;674:109–115. doi: 10.1016/j.mrgentox.2008.09.021. [DOI] [PubMed] [Google Scholar]
- 112.de Oliveira-Marques V, Cyrne L, Marinho HS, Antunes F. A quantitative study of NFkappaB activation by H2O2: relevance in inflammation and synergy with TNFalpha. J Immunol. 2007;178:3893–3902. doi: 10.4049/jimmunol.178.6.3893. [DOI] [PubMed] [Google Scholar]
- 113.Lupertz R, Chovolou Y, Kampkotter A, Watjen W, Kahl R. Catalase overexpression impairs TNFalpha induced NFkappaB activation and sensitizes MCF-7 cells against TNFalpha. J Cell Biochem. 2008;103:1497–1511. doi: 10.1002/jcb.21538. [DOI] [PubMed] [Google Scholar]
- 114.Cristofanon S, Morceau F, Scovassi AI, Dicato M, Ghibelli L, Diederich M. Oxidative, multistep activation of the noncanonical NFkappaB pathway via disulfide Bcl-3/p50 complex. Faseb J. 2009;23:45–57. doi: 10.1096/fj.07-104109. [DOI] [PubMed] [Google Scholar]
- 115.Jimenez-Lopez JM, Wu D, Cederbaum AI. Synergistic toxicity induced by prolonged glutathione depletion and inhibition of nuclear factor-kappaB signaling in liver cells. Toxicol In Vitro. 2008;22:106–115. doi: 10.1016/j.tiv.2007.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Sarkar FH, Li Y, Wang Z, Kong D. NFkappaB signaling pathway and its therapeutic implications in human diseases. Int Rev Immunol. 2008;27:293–319. doi: 10.1080/08830180802276179. [DOI] [PubMed] [Google Scholar]
- 117.Janssen-Heininger YM, Poynter ME, Aesif SW, Pantano C, Ather JL, Reynaert NL, et al. Nuclear factor kappaB, airway epithelium and asthma: avenues for redox control. Proc Am Thorac Soc. 2009;6:249–255. doi: 10.1513/pats.200806-054RM. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Epperly MW, Bernarding M, Gretton J, Jefferson M, Nie S, Greenberger JS. Overexpression of the transgene for manganese superoxide dismutase (MnSOD) in 32D cl 3 cells prevents apoptosis induction by TNFalpha, IL-3 withdrawal, and ionizing radiation. Exp Hematol. 2003;31:465–474. doi: 10.1016/s0301-472x(03)00041-9. [DOI] [PubMed] [Google Scholar]
- 119.Place RF, Haspeslagh D, Giardina C. Induced stabilization of IkappaBalpha can facilitate its re-synthesis and prevent sequential degradation. J Cell Physiol. 2003;195:470–478. doi: 10.1002/jcp.10262. [DOI] [PubMed] [Google Scholar]
- 120.Masamune A, Shimosegawa T. Signal transduction in pancreatic stellate cells. J Gastroenterol. 2009;44:249–260. doi: 10.1007/s00535-009-0013-2. [DOI] [PubMed] [Google Scholar]
- 121.Palozza P, Serini S, Torsello A, Di Nicuolo F, Piccioni E, Ubaldi V, et al. Beta-carotene regulates NFkappaB DNA-binding activity by a redox mechanism in human leukemia and colon adenocarcinoma cells. J Nutr. 2003;133:381–388. doi: 10.1093/jn/133.2.381. [DOI] [PubMed] [Google Scholar]
- 122.Sriram N, Kalayarasan S, Ashokkumar P, Sureshkumar A, Sudhandiran G. Diallyl sulfide induces apoptosis in Colo 320 DM human colon cancer cells: involvement of caspase-3, NFkappaB and ERK-2. Mol Cell Biochem. 2008;311:157–165. doi: 10.1007/s11010-008-9706-8. [DOI] [PubMed] [Google Scholar]
- 123.Junttila MR, Li SP, Westermarck J. Phosphatase-mediated crosstalk between MAPK signaling pathways in the regulation of cell survival. Faseb J. 2008;22:954–965. doi: 10.1096/fj.06-7859rev. [DOI] [PubMed] [Google Scholar]
- 124.Mebratu Y, Tesfaigzi Y. How ERK 1/2 activation controls cell proliferation and cell death: Is subcellular localization the answer? Cell Cycle. 2009;8:1168–1175. doi: 10.4161/cc.8.8.8147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.McCubrey JA, Steelman LS, Abrams SL, Bertrand FE, Ludwig DE, Basecke J, et al. Targeting survival cascades induced by activation of Ras/Raf/MEK/ERK, PI3K/PTEN/Akt/mTOR and Jak/STAT pathways for effective leukemia therapy. Leukemia. 2008;22:708–722. doi: 10.1038/leu.2008.27. [DOI] [PubMed] [Google Scholar]
- 126.Russo AE, Torrisi E, Bevelacqua Y, Perrotta R, Libra M, McCubrey JA, et al. Melanoma: molecular pathogenesis and emerging target therapies (Review) Int J Oncol. 2009;34:1481–1489. doi: 10.3892/ijo_00000277. [DOI] [PubMed] [Google Scholar]
- 127.Eguchi M, Monden K, Miwa N. Role of MAPK phosphorylation in cytoprotection by pro-vitamin C against oxidative stress-induced injuries in cultured cardiomyoblasts and perfused rat heart. J Cell Biochem. 2003;90:219–226. doi: 10.1002/jcb.10643. [DOI] [PubMed] [Google Scholar]
- 128.Schraml E, Fuchs R, Kotzbeck P, Grillari J, Schauenstein K. Acute adrenergic stress inhibits proliferation of murine hematopoietic progenitor cells via p38/MAPK signaling. Stem Cells Dev. 2009;18:215–227. doi: 10.1089/scd.2008.0072. [DOI] [PubMed] [Google Scholar]
- 129.Liu B, Yu HM, Huang J, Hsu W. Co-opted JNK/SAPK signaling in Wnt/beta-catenin-induced tumorigenesis. Neoplasia. 2008;10:1004–1013. doi: 10.1593/neo.08548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Nguyen HT, Hsieh MH, Gaborro A, Tinloy B, Phillips C, Adam RM. JNK/SAPK and p38 SAPK-2 mediate mechanical stretch-induced apoptosis via caspase-3 and -9 in NRK-52E renal epithelial cells. Nephron Exp Nephrol. 2006;102:22. doi: 10.1159/000088401. [DOI] [PubMed] [Google Scholar]
- 131.Matsuzawa A, Ichijo H. Redox control of cell fate by MAP kinase: physiological roles of ASK1-MAP kinase pathway in stress signaling. Biochim Biophys Acta. 2008;1780:1325–1336. doi: 10.1016/j.bbagen.2007.12.011. [DOI] [PubMed] [Google Scholar]
- 132.Nadeau PJ, Charette SJ, Toledano MB, Landry J. Disulfide Bond-mediated multimerization of Ask1 and its reduction by thioredoxin-1 regulate H(2) O(2)-induced c-Jun NH(2)-terminal kinase activation and apoptosis. Mol Biol Cell. 2007;18:3903–3913. doi: 10.1091/mbc.E07-05-0491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Torres M. Mitogen-activated protein kinase pathways in redox signaling. Front Biosci. 2003;8:369–3691. doi: 10.2741/999. [DOI] [PubMed] [Google Scholar]
- 134.Nguyen A, Chang AC, Reddel RR. Stanniocalcin-1 acts in a negative feedback loop in the prosurvival ERK1/2 signaling pathway during oxidative stress. Oncogene. 2009;28:1982–1992. doi: 10.1038/onc.2009.65. [DOI] [PubMed] [Google Scholar]
- 135.Kang GY, Lee ER, Kim JH, Jung JW, Lim J, Kim SK, et al. Downregulation of PLK-1 expression in kaempferol-induced apoptosis of MCF-7 cells. Eur J Pharmacol. 2009;611:17–21. doi: 10.1016/j.ejphar.2009.03.068. [DOI] [PubMed] [Google Scholar]
- 136.Kim BW, Lee ER, Min HM, Jeong HS, Ahn JY, Kim JH, et al. Sustained ERK activation is involved in the kaempferol-induced apoptosis of breast cancer cells and is more evident under 3-D culture condition. Cancer Biol Ther. 2008;7:1080–1089. doi: 10.4161/cbt.7.7.6164. [DOI] [PubMed] [Google Scholar]
- 137.Shim HY, Park JH, Paik HD, Nah SY, Kim DS, Han YS. Acacetin-induced apoptosis of human breast cancer MCF-7 cells involves caspase cascade, mitochondria-mediated death signaling and SAPK/JNK1/2-c-Jun activation. Mol Cells. 2007;24:95–104. [PubMed] [Google Scholar]
- 138.Kuo PL, Chen CY, Tzeng TF, Lin CC, Hsu YL. Involvement of reactive oxygen species/c-Jun NH(2)-terminal kinase pathway in kotomolide A induces apoptosis in human breast cancer cells. Toxicol Appl Pharmacol. 2008;229:215–226. doi: 10.1016/j.taap.2008.01.034. [DOI] [PubMed] [Google Scholar]
- 139.Donadelli M, Dalla Pozza E, Costanzo C, Scupoli MT, Piacentini P, Scarpa A, et al. Increased stability of P21(WAF1/CIP1) mRNA is required for ROS/ ERK-dependent pancreatic adenocarcinoma cell growth inhibition by pyrrolidine dithiocarbamate. Biochim Biophys Acta. 2006;1763:917–926. doi: 10.1016/j.bbamcr.2006.05.015. [DOI] [PubMed] [Google Scholar]
- 140.Hsu WH, Hsieh YS, Kuo HC, Teng CY, Huang HI, Wang CJ, et al. Berberine induces apoptosis in SW620 human colonic carcinoma cells through generation of reactive oxygen species and activation of JNK/p38 MAPK and FasL. Arch Toxicol. 2007;81:719–728. doi: 10.1007/s00204-006-0169-y. [DOI] [PubMed] [Google Scholar]
- 141.Liu Y, Borchert GL, Surazynski A, Hu CA, Phang JM. Proline oxidase activates both intrinsic and extrinsic pathways for apoptosis: the role of ROS/superoxides, NFAT and MEK/ERK signaling. Oncogene. 2006;25:5640–5647. doi: 10.1038/sj.onc.1209564. [DOI] [PubMed] [Google Scholar]
- 142.Joo SS, Yoo YM. Melatonin induces apoptotic death in LNCaP cells via p38 and JNK pathways: therapeutic implications for prostate cancer. J Pineal Res. 2009;47:8–14. doi: 10.1111/j.1600-079X.2009.00682.x. [DOI] [PubMed] [Google Scholar]
- 143.Kinkade CW, Castillo-Martin M, Puzio-Kuter A, Yan J, Foster TH, Gao H, et al. Targeting AKT/ mTOR and ERK MAPK signaling inhibits hormonerefractory prostate cancer in a preclinical mouse model. J Clin Invest. 2008;118:3051–3064. doi: 10.1172/JCI34764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Sanchez AM, Malagarie-Cazenave S, Olea N, Vara D, Chiloeches A, Diaz-Laviada I. Apoptosis induced by capsaicin in prostate PC-3 cells involves ceramide accumulation, neutral sphingomyelinase and JNK activation. Apoptosis. 2007;12:2013–2024. doi: 10.1007/s10495-007-0119-z. [DOI] [PubMed] [Google Scholar]
- 145.Valentini A, Conforti F, Crispini A, De Martino A, Condello R, Stellitano C, et al. Synthesis, oxidant properties and antitumoral effects of a heteroleptic palladium(II) complex of curcumin on human prostate cancer cells. J Med Chem. 2009;52:484–491. doi: 10.1021/jm801276a. [DOI] [PubMed] [Google Scholar]
- 146.Alexandre J, Batteux F, Nicco C, Chereau C, Laurent A, Guillevin L, et al. Accumulation of hydrogen peroxide is an early and crucial step for paclitaxelinduced cancer cell death both in vitro and in vivo. Int J Cancer. 2006;119:41–48. doi: 10.1002/ijc.21685. [DOI] [PubMed] [Google Scholar]
- 147.Llobet D, Eritja N, Encinas M, Sorolla A, Yeramian A, Schoenenberger JA, et al. Antioxidants block proteasome inhibitor function in endometrial carcinoma cells. Anticancer Drugs. 2008;19:115–124. doi: 10.1097/CAD.0b013e3282f24031. [DOI] [PubMed] [Google Scholar]
- 148.Guzman ML, Li X, Corbett CA, Rossi RM, Bushnell T, Liesveld JL, et al. Rapid and selective death of leukemia stem and progenitor cells induced by the compound 4-benzyl, 2-methyl, 1,2,4-thiadiazolidine, 3,5 dione (TDZD-8) Blood. 2007;110:4436–4444. doi: 10.1182/blood-2007-05-088815. [DOI] [PMC free article] [PubMed] [Google Scholar]