Abstract
Background
Patellar taping is widely used clinically to treat patients with patellofemoral pain syndrome (PFPS). Although patellar taping has been demonstrated to reduce patellofemoral pain in patients with PFPS, the kinematic source for this pain reduction has not been identified.
Objective
The purpose of this study was to quantify the changes in the 6-degrees-of-freedom patellofemoral kinematics due to taping in patients with PFPS.
Design
A within-subject design and a sample of convenience were used.
Participants
Fourteen volunteers (19 knees) who were diagnosed with patellofemoral pain that was present for a year or longer were included. Each knee had to meet at least 1 of the following inclusion criteria: Q-angle of ≥15 degrees, a positive apprehension test, patellar lateral hypermobility (≥10 mm), or a positive “J sign.”
Methods
Each knee underwent 2 randomly ordered testing conditions (untaped and taped). A full fast-phase contrast (PC) magnetic resonance image set was acquired for each condition while the participants volitionally extended and flexed their knee. Three-dimensional displacements and rotations were calculated through integration of the fast-PC velocity data. Statistical comparisons between baseline patellofemoral kinematics and the change in kinematics due to taping were performed using a 2-tailed paired Student t test. Correlations between baseline patellofemoral kinematics and the change in kinematics due to taping also were quantified.
Results
Patellar taping resulted in a significant patellofemoral inferior shift. The strongest correlation existed between the change in lateral-medial displacement with taping and baseline (r=−.60).
Conclusions
The inferior shift in patellar displacement with taping partially explains the previously documented decrease in pain due to increases in contact area. The lack of alteration in 5 of the 6 kinematic variables with taping may have been due to the fact that post-taping kinematic alterations are sensitive to the baseline kinematic values.
Patellofemoral pain syndrome (PFPS) is one of the most common causes of orthopedic-related physician visits each year, especially among women.1,2 Patellofemoral pain syndrome can be caused by direct trauma to the knee, or the cause can be insidious in nature. Altered lower-extremity biomechanics, such as poor hip rotation control,3 excessive foot pronation,4 femoral anteversion, tibial torsion, bone configuration, or tight muscles are thought to contribute to PFPS by initiating alterations in patellofemoral kinematics.5,6 Vastus medialis oblique muscle dysfunction also has been proposed as a contributor to altered patellofemoral kinematics.7–10 Interventions for PFPS include patellar taping, patellar bracing, selective strengthening of the vastus medalis muscle, iliotibial band stretching, ankle-foot orthotics, or a combination of these interventions.11–15
Patellar taping is widely practiced among clinicians to treat patients with PFPS. This intervention involves pushing the patella medially and securing it in this position with tape on the skin. Originally, the McConnell taping technique was developed to correct altered patellofemoral kinematics and permit participation in normal daily activity.16 Today, there exist several variations of McConnell taping techniques, where attempts are made to alter patellar tilt, glide, or rotation.17 Clinical application of these techniques is based on a physical examination of patellar position, orientation, and mobility.18,19 The underlying concept is that most patients with PFPS would benefit from medialization of the patella, which theoretically would off-load the compressive forces at the lateral patellofemoral joint.16,20
Although patellar taping has been demonstrated to reduce patellofemoral pain in patients with PFPS,21–26 the kinematic source of this pain reduction has not been identified. Likely, this failure to identify the kinematic source of the pain reduction is due to the fact that the complete 6 degrees of freedom patellofemoral kinematics (post-taping) during active extension has not been quantified in a group of patients with PFPS. Instead, patellofemoral axial alignment changes (patellar translation and tilt) due to taping in patients with PFPS have been quantified in a small number of studies.21,27–30 The majority of studies focused on static evaluation of knee posture without muscle activity. Isometric quadriceps muscle activity has been incorporated into a few of these studies.21,28 In these studies, no differences in lateral patellar translation or tilt were found with taping, with or without muscle contraction.
Thus, the purpose of this study was to quantify the changes in the 6-degrees-of-freedom patellofemoral kinematics due to McConnell taping in people with PFPS during dynamic knee flexion and extension using fast-phase contrast (PC) magnetic resonance imaging (MRI). In doing so, 2 null hypotheses were tested: (1) McConnell taping does not alter the patellofemoral kinematics in all 6 degrees of freedom, and (2) no correlations exist between the baseline patellofemoral kinematics (untaped condition) and the change in kinematics due to taping.
Method
Participants
Fourteen volunteers diagnosed with PFPS gave informed consent prior to participating in this study. Participants were recruited from local orthopedic clinics and ongoing National Institutes of Health studies. This recruitment was primarily Web-based (http://clinicalresearch.nih.gov), conducted through the Clinical Center Patient Recruitment and Public Liaison Office. Participants were excluded if they had any contraindications to having an MRI scan. Both knees were evaluated in the initial screening examination. To be included in the study, each knee had to be clinically diagnosed with PFPS, with symptoms present for a year or longer. An in-house physiatrist, using both a physical examination and the patient's history, excluded any knee that had: (1) previous surgery (including arthroscopy); (2) ligament, meniscus, iliotibial band, or cartilage damage; (3) other lower-leg pathology or injury; or (4) traumatic onset of PFPS.
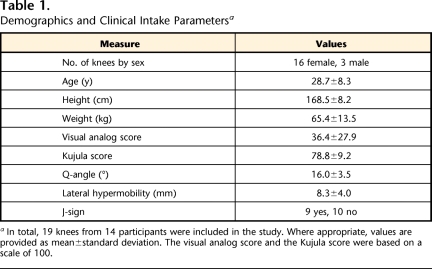
In addition, a physical therapist (T.J.B.) examined each knee for evidence of altered patellofemoral kinematics: (1) Q-angle of ≥15 degrees,18,31,32 (2) a positive apprehension test, (3) patellar lateral hypermobility of ≥10 mm,18 or (4) a positive J-sign.18,32,33 Any knee that did not exhibit 1 or more of these 4 signs was excluded. These measures were used solely as inclusion and exclusion criteria and were not included in the kinematic data analysis arm of the study. Both the Q-angle and lateral hypermobility were measured with the participants in a supine position with the knee in full extension and muscles relaxed. In this position, patellar lateral hypermobility was defined as the ability of the examiner to move the patella laterally by 10 mm or more. To confirm or deny the presence of a J-sign, participants were seated at the end of the table and the examiner evaluated patellar motion as the participants raised their leg into full extension. The pain in each knee was evaluated using a visual analog scale (VAS) pain score and a Kujula score.30 In total, 19 knees from 14 participants were included in this study (Tab. 1).
Table 1.
Demographics and Clinical Intake Parametersa
In total, 19 knees from 14 participants were included in the study. Where appropriate, values are provided as mean±standard deviation. The visual analog score and the Kujula score were based on a scale of 100.
Procedure
Each knee underwent 2 testing conditions in the MRI (untaped and taped), which were randomly ordered. For each condition, participants were placed supine in a 1.5-Tesla magnetic resonance imager (CV-9.1M4 or LX-9.1M4).*,32 After acquiring a set of static alignment scans, the participants were allowed to practice the extension-flexion exercise until they could repeatedly extend and flex their knee to and from maximum attainable flexion and full extension at 35 cycles per minute to the beat of an auditory metronome. Participants were instructed to generate knee extension without hip movement, and a loose strap was placed over the thighs as a reminder, but minor femoral motion was allowed to enable a natural movement. Next, a full fast-PC MRI image set (x,y,z velocity and anatomic images over 24 time frames) was acquired while the participants volitionally extended and flexed their knee to the beat of the auditory metronome, as practiced. In addition, fastcard images (anatomic only) were acquired in 3 axial planes during the cyclic movement. An in-house musculoskeletal radiologist reviewed all magnetic resonance images to rule out ligament, meniscus, iliotibial band, or cartilage damage.
During tape application, participants were positioned supine with their quadriceps muscle relaxed. They were taped by a physical therapist (T.J.B.) with more than 15 years of experience in orthopedics and sports medicine. Initially, Hypafix† was applied to the skin covering the knee. Next, a medial glide of the patella was obtained by manually pushing the patella medially to its end range of motion. Rigid strapping tape then was used to maintain the medial glide of the patella by pulling the skin and patella medially. Participants were required to walk for 5 minutes at a self-selected, comfortable pace after taping and prior to the MRI experiment.27,29
Three-dimensional rigid-body rotations and displacements of the femur, tibia, and patella were quantified through integration of the fast-PC velocity data. It is important to note that although the fast-PC acquisition was based on a single imaging plane, the 3-dimensional velocity data allowed the orientation and displacement of all bones to be accurately tracked 3-dimensionally throughout the movement.34 Kinematics were defined based on an anatomical coordinate system. Unlike earlier cine MRI experiments,35,36 this identification was completed for a single time frame only, and the fast-PC data were used to track the bones’ kinematics through all time frames. Thus, the need to visually identify anatomical landmarks at multiple time points35,36 was eliminated, which minimized errors due to inconsistency in image plane location and orientation37,38 and provided excellent accuracy (<0.5 mm39) and precision (<1.16°40). The kinematics of the patella relative to the femur were defined using 6 variables: 3 displacements—lateral-medial (LM), inferior-superior (IS), and posterior-anterior (PA)—and 3 rotations—lateral-medial tilt (LM tilt), extension-flexion (EF), valgus-varus rotation (VV). A significant increase in the superior position of the patellar origin relative to the femoral origin was defined as patella alta. From the patellar-tibial kinematic data, patellar tendon length was calculated as in a previous study.41 All data were presented for the extension portion of the movement only. Due to individual variations in range of motion within the magnetic resonance scanner, not all participants were represented at the extreme ranges of knee flexion and extension. Thus, the average data presented were limited to the central range of motion, where 3 or more participants were represented by the average.
The kinematic data were reduced to the magnitudes of each of the 6 kinematic variables when the knee was at 10 degrees of knee extension (defined as the “value” of that variable). The untaped condition was considered baseline. A 10-degree knee flexion angle was used because not all participants were able to achieve full knee extension (0° flexion angle). In addition, patellar taping should have the greatest effect when the patella is in terminal extension and is most free from the constraints of the femoral groove.5,35,42
Data Analysis
Statistical differences between the taped and untaped conditions were investigated using a paired 2-tailed Student t test. Correlations between the baseline patellofemoral kinematics and the change in kinematics due to taping were quantified. Minimal correlations between pain scores (VAS and Kujula) and patellofemoral kinematics have been documented (only the slope of patellofemoral varus relative to knee extension correlated with VAS pain score) in patients with PFPS.5 Because the current population was a subset of this earlier study, these correlations were not performed in the current study. Statistical significance was set at P≤.05, (SPSS, version 14.0).‡ An a priori sample size calculation determined that adequate power (α=.05, β≥.80) could be achieved with the inclusion of 15 knees, assuming that taping would result in a 2-mm medial patellar shift30 and that the standard deviation associated with this change would be 2.5 mm.34
Results
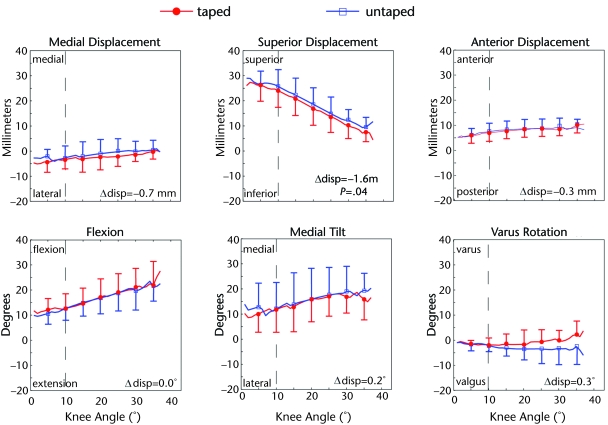
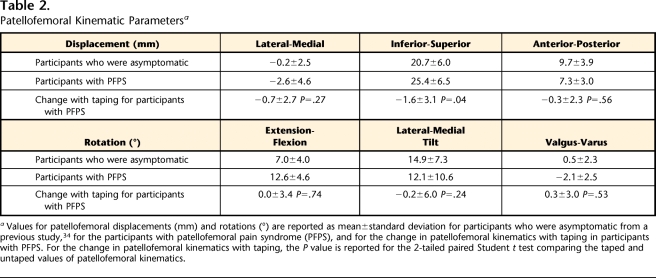
The null hypothesis that McConnell taping does not alter the patellofemoral kinematics was rejected for a single variable only: IS displacement (Fig. 1, −1.6 mm, P=.04). The only significant effect of patellar taping was an inferior (downward) shift in the patella. This inferior shift resulted in an insignificant decrease in the patellar tendon length at 10 degrees of knee extension (Δlength =−0.46, P=.79). However, there were significant differences in kinematics between the participants with PFPS included in the current study and a previous sample of individuals who were asymptomatic.34 On average, the participants with patellofemoral pain were 2.1 mm (P=.04), 4.2 mm (P=.03), and 2.3 mm (P=.05) more laterally, superiorly, and anteriorly displaced than the control population. In addition, these participants were 5.3 (P<.001) and 2.5 (P<.001) degrees more flexed and rotated into valgus than the control population (Tab. 2).
Figure 1.
Patellofemoral kinematics in the untaped and taped conditions: Each variable is plotted relative to knee extension, with full extension being equal to zero (participant movement is read from left to right). Data were interpolated to 1-degree knee angle increments, but symbols are provided at every 5 degrees for clarity. One standard deviation bars are provided. The dotted line represents a knee extension angle of 8 degrees. The top row contains displacements (medial, superior, and anterior are the positive directions, respectively), and the bottom row contains the rotations (flexion, medial tilt, and varus rotation are the positive directions, respectively). Δdisp=changed in displacement.
Table 2.
Patellofemoral Kinematic Parametersa
Values for patellofemoral displacements (mm) and rotations (°) are reported as mean±standard deviation for participants who were asymptomatic from a previous study,34 for the participants with patellofemoral pain syndrome (PFPS), and for the change in patellofemoral kinematics with taping in participants with PFPS. For the change in patellofemoral kinematics with taping, the P value is reported for the 2-tailed paired Student t test comparing the taped and untaped values of patellofemoral kinematics.
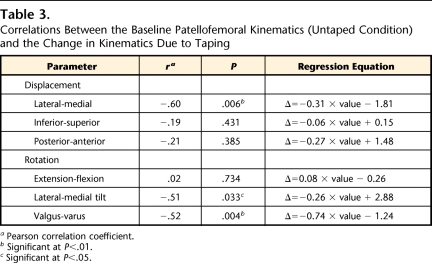
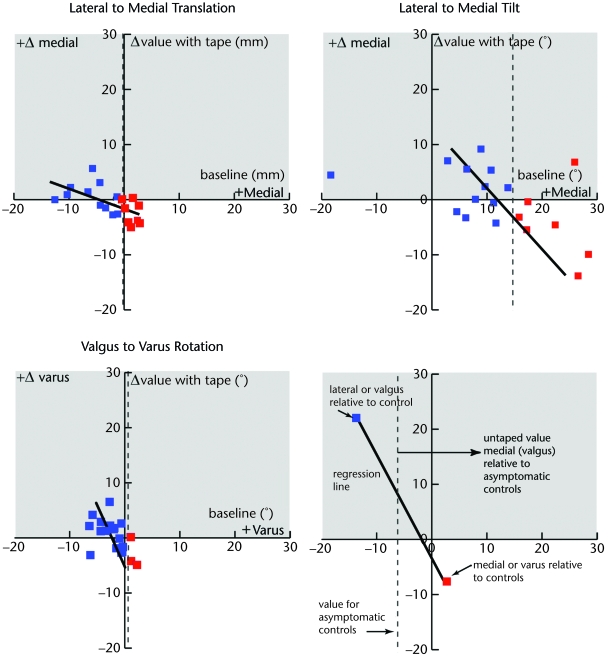
The second null hypothesis that no correlations exist between the baseline patellofemoral kinematics and the change in kinematics due to taping was rejected for 3 variables (Tab. 3 and Fig. 2). The strongest inverse correlation existed for LM displacement (r=−.67), and moderate inverse correlations existed for LM tilt and VV (r=−.52 for both). The correlations indicate that participants with larger absolute baseline kinematic values (further from the asymptomatic average34) would see the greatest absolute change with taping. Interestingly, not all of the participants with patellofemoral pain had baseline values of LM displacement, LM tilt, and VV that were lateral and valgus, relative to a previously defined asymptomatic average.34 Thus, participants who began with medial displacement, medial tilt, or varus rotation, relative to the asymptomatic population, demonstrated a lateral shift in displacement, lateral tilt, or valgus rotation, respectively, after taping was applied. The participant with the largest values of lateral tilt and displacement proved to be an outlier in that taping caused a much smaller change in these variables than the correlation would suggest. Data for this participant were not removed from the analyses, but when these data are removed, the correlation between baseline and change with taping increases (r=−.54, P=.02) for LM tilt and the correlations for LM displacement and VV rotation increase minimally.
Table 3.
Correlations Between the Baseline Patellofemoral Kinematics (Untaped Condition) and the Change in Kinematics Due to Taping
a Pearson correlation coefficient.
b Significant at P<.01.
c Significant at P<.05.
Figure 2.
Change in kinematics with taping (taped and untaped conditions) versus baseline. The 3 variables with significant correlations between the change with taping and the baseline value are shown (top row: lateral to medial displacement and lateral to medial tilt; bottom row: valgus to varus rotation and legend to symbols). The x-axis indicates the untaped value of each variable (positive values indicate medial displacement, medial tilt, and varus rotation). The y-axis indicates the change in each variable with taping (positive values indicate medial displacement, medial tilt, and varus rotation with taping, shown by gray shading). The regression lines are shown for each variable set using a thick black line. Based on previous work,34 the average value for an asymptomatic cohort (untaped, n=34) for each of the 3 variables is shown using a vertical dashed line (medial displacement=−0.11 mm, medial tilt=14.7, varus rotation=0.52°). All graphs represent kinematics at 10 degrees of knee extension. Participants who were laterally translated, laterally tilted, and in valgus rotation (relative to the asymptomatic population) are shown in blue. This distinction is independent for each graph. Thus, a single participant who demonstrated medial displacement and lateral tilt at baseline would be designated by 2 different colors in each of the respective graphs.
Discussion
This study was the first to quantify changes caused by McConnell taping in the complete 6-degrees-of-freedom patellofemoral kinematics during volitional knee extension in a sample of patients with PFPS. On average, the only consistent influence McConnell taping provided on patellar kinematics was to shift the patella inferiorly. The benefit of inferiorly shifting the patella within the femoral groove was an increase in the patellofemoral contact area. In a previous study, Ward and colleagues43 defined a 19.3% decrease in cartilage contact area in a group of participants with a 24% increase in the Insall ratio (superior displaced relative to a control population). In the current study, the patellae in the participants with PFPS were 24% (5.2 mm) more superiorly placed (dynamically) compared with those of the asymptomatic population.34 The inferior shift in displacement with taping (1.6 mm) represents 34.8% of the difference in IS displacement between the participants with PFPS and the asymptomatic controls (Tab. 2, 4.6 mm). Increased contact area decreases contact stress at the patellofemoral joint by spreading out the load over a wider area. Ultimately, this decrease in contact stress may account for some of the previously reported decrease in patellofemoral pain after taping.21–26
The correlation between the baseline patellofemoral kinematics and the change in kinematics due to taping supports earlier work that identified the existence of subgroups within the patellofemoral pain population.33 The expected medial change in patellar displacement or tilt occurred in participants with lateral baseline values of these variables. Conversely, participants with medial displacement or tilt at baseline demonstrated a lateral change in displacement or tilt with taping. The same relationship held true for VV rotation. Therefore, taping shifts the patella medially in patients with lateral baseline values of patellofemoral displacement (relative to an asymptomatic average), and it shifts the patella in the opposite direction in patients with medial baseline values of patellofemoral displacement. Similarly, taping is effective in medially tilting the patella in patients with PFPS and lateral baseline tilt, but it has the opposite effect for patients with medial baseline tilt. However, average differences in patellar kinematics after taping across all participants produced no significant change due to the contrary effect of patellar taping across participants. Thus, considering the participants in this study as a single population masked the true changes with taping seen on a person-by-person basis. Regardless, pain relief may have been further enhanced by the centralization of the patella in regard to patellar LM displacement, LM tilt, and VV rotation.
One interesting exception in this study was a single participant who had the largest lateral displacement at baseline (−14.5 mm), yet demonstrated minimal medialization with taping. This participant had the highest baseline values of superior displacement (39.0 mm, asymptomatic average [±SD]=21.7±6.3 mm). If the inferior shift in patellar placement is considered the primary effect of taping, then the lack of kinematic change for this specific participant may have been due to patella alta. In general, for most patients with PFPS with lateral baseline values of patellofemoral LM displacement, the inferior shift and taping may lead to further patellar engagement with the femoral sulcus. Thus, both the force of the taping and the bone constraint may have medialized the patella placement. This concept is supported by a previous study that demonstrated a strong correlation between patellofemoral superior and lateral displacement.5 Yet, for this participant, the small inferior shift may not have resulted in patellar engagement with the sulcus, and taping alone was insufficient to cause a large medialization force.
It is counterintuitive that a medial taping technique could cause lateralization of the patella in patients with PFPS. Yet, patients who begin with medial baseline values for LM displacement do not demonstrate patella alta.33 In the absence of patella alta, it is likely that the patella remained partially engaged with the femoral sulcus throughout extension, enabling the patella to remain medially placed. When the patella was inferiorly displaced with taping, the patella was further engaged with the sulcus. The bony constraints of the sulcus, due to either the shape of the groove or limb alignment, resulted in the patella shifting laterally relative to the femur, and taping could not overcome this bone force. The fact that any patient with PFPS had medial patellar placement relative to the femur may appear contrary to the fact that the clinical markers used as inclusion criteria should have confirmed the presence of excessive lateral tracking. This potential incongruity is explained by a recently published finding that the value of Q-angle is correlated with medial and not lateral patellofemoral displacement.33
The current results support and expand the findings of previous studies on the effectiveness of McConnell taping. Typically, previous taping studies focused on a static, 2-dimensional evaluation of patellar alignment with or without muscle contraction.21,27–30 On average, taping was shown to be ineffective in shifting and tilting the patella medially. Taping has been shown to be effective if it was evaluated prior to any exercise, but a short bout of exercise eliminated this effect.24,29 The current study design included a short bout of exercise prior to evaluating the taping condition, but our study differed from past studies in its 3-dimensional dynamic evaluation of a volitional task. Based on this experimental design, McConnell taping was shown to be effective in shifting the patella inferiorly after a short bout of exercise. We also demonstrated that taping tended to shift patellar LM displacement, LM tilt, and VV rotation back toward the asymptomatic average. Thus, it is likely that the ineffectiveness of taping found in previous studies was due to the fact that some patients were not laterally tilted or displaced prior to taping.
Although the current study used dynamic movement, which is representative of how muscle action can influence patellar kinematics, there were limitations. The movements were isolated to the knee, neglecting the influence of proximal or distal joints on patellofemoral kinematics. The range of motion was limited, but did cover from just prior to and through terminal extension, where altered patellofemoral kinematic patterns are most evident. The experimental design did not include an axial compressive load applied to the leg; thus, it is not known how such loading could affect patellar kinematics and taping. Another potential limitation of this study was the fact that the exact force applied with taping was not quantified. Yet, in previous studies, participants often applied their own tape,21,44 and no previous study measured the force applied with taping.17,21,24,29,30,44,45 Lastly, pain was not measured after tape application. This measure was not included in the study design, as previous studies21–26 have clearly shown the effectiveness of taping for pain reduction. Thus, the current study was focused specifically on accurately quantifying how taping alters 3-dimensional patellofemoral kinematics by measuring them noninvasively and in vivo during volitional activity. The noninvasive nature of this experiment and its high accuracy, excellent precision, and ability to demonstrate 3-dimensional kinematic differences during volitional activities justify these limitations.
Conclusions and Clinical Relevance
This is the first study to evaluate 3-dimensional changes in patellar kinematics with McConnell taping during voluntary active motion. For the participants in this study, patellar taping shifted the patella inferiorly with respect to the femur, which may account for some of the previously reported pain relief with taping, due to an increase in contact area. McConnell taping medialized the patella in participants who demonstrated lateral displacement at baseline and lateralized the patella in participants who demonstrated medial patellar displacement at baseline. Thus, medialization of the patella with taping was dependent upon the patellofemoral kinematic alterations present in each participant. This finding reinforces the need to clinically identify the specific alterations in patellofemoral kinematics present in each patient so that specific interventions can be used and optimized to correct these altered kinematics and reduce pain. All patients with PFPS and altered patellofemoral kinematics are likely to benefit from an inferior shift of the patella, which should reduce patellofemoral contact stress.
Footnotes
Ms Derasari, Dr Alter, and Dr Sheehan provided concept/idea/project design, data analysis, and project management. Dr Brindle, Dr Alter, and Dr Sheehan provided writing. All authors provided data collection. Dr Sheehan provided fund procurement. Ms Derasari provided participants. Dr Brindle provided consultation (including review of manuscript before submission).
The authors thank Elizabeth K. Rasch, PT, PhD, for support on the statistical analysis and Steven Stanhope, PhD, for guidance throughout the project. They also thank Bonnie Damaska, Jamie Fraunhaffer, Jere McLucas, Dr Ken Fine, and the Diagnostic Radiology Department at the National Institutes of Health for their support and research time.
This study was approved by the National Institute of Child Health and Development.
This research was supported, in part, by the Howard Hughes Foundation and the Intramural Research Program of the National Institutes of Health (Clinical Center and National Institute of Child Health and Human Development). Any opinions, findings, and conclusions or recommendations expressed in this material are those of the authors and do not necessarily reflect the views of the National Institutes of Health or the US Public Health Service.
GE Medical Systems, 4855 W Electric Ave, Milwaukee, WI 53219-1628.
Smith & Nephew DonJoy, 2777 Loker Ave, Carlsbad, CA 92010.
SPSS Inc, 233 S Wacker Dr, Chicago, IL 60606.
References
- 1.Almeida SA, Trone DW, Leone DM, et al. Gender differences in musculoskeletal injury rates: a function of symptom reporting? Med Sci Sports Exerc 1999;31:1807–1812 [DOI] [PubMed] [Google Scholar]
- 2.Rauh MJ, Koepsell TD, Rivara FP, et al. Epidemiology of musculoskeletal injuries among high school cross-country runners. Am J Epidemiol 2006;163:151–159 [DOI] [PubMed] [Google Scholar]
- 3.Cibulka MT, Threlkeld-Watkins J. Patellofemoral pain and asymmetrical hip rotation. Phys Ther 2005;85:1201–1207 [PubMed] [Google Scholar]
- 4.Sutlive TG, Mitchell SD, Maxfield SN, et al. Identification of individuals with patellofemoral pain whose symptoms improved after a combined program of foot orthosis use and modified activity: a preliminary investigation. Phys Ther 2004;84:49–61 [PubMed] [Google Scholar]
- 5.Sheehan FT, Derasari A, Brindle TJ, Alter KE. Understanding patellofemoral pain with maltracking in the presence of joint laxity: complete 3D in vivo patellofemoral and tibiofemoral kinematics. J Orthop Res 2008;27:561–570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wilson NA, Press JM, Koh JL, et al. In vivo and noninvasive evaluation of abnormal patellar tracking during squatting in patellofemoral pain. J Bone Joint Surg Am 2008;91:558–566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Boucher JP, King MA, Lefebvre R, Pepin A. Quadriceps femoris muscle activity in patellofemoral pain syndrome. Am J Sports Med 1992;20:527–532 [DOI] [PubMed] [Google Scholar]
- 8.Cowan SM, Bennell KL, Hodges PW, et al. Delayed onset of electromyographic activity of vastus medialis obliquus relative to vastus lateralis in subjects with patellofemoral pain syndrome. Arch Phys Med Rehabil 2001;82:183–189 [DOI] [PubMed] [Google Scholar]
- 9.Karst GM, Willett GM. Onset timing of electromyographic activity in the vastus medialis oblique and vastus lateralis muscles in subjects with and without patellofemoral pain syndrome. Phys Ther 1995;75:813–823 [DOI] [PubMed] [Google Scholar]
- 10.Powers CM. Patellar kinematics, part I: the influence of vastus muscle activity in subjects with and without patellofemoral pain. Phys Ther 2000;80:956–964 [PubMed] [Google Scholar]
- 11.Adams WB. Treatment options in overuse injuries of the knee: patellofemoral syndrome, iliotibial band syndrome, and degenerative meniscal tears. Curr Sports Med Rep 2004;3:256–260 [DOI] [PubMed] [Google Scholar]
- 12.Crossley K, Bennell K, Green S, et al. Physical therapy for patellofemoral pain: a randomized, double-blinded, placebo-controlled trial. Am J Sports Med 2002;30:857–865 [DOI] [PubMed] [Google Scholar]
- 13.Gilleard W, McConnell J, Parsons D. The effect of patellar taping on the onset of vastus medialis obliquus and vastus lateralis muscle activity in persons with patellofemoral pain. Phys Ther 1998;78:25–32 [DOI] [PubMed] [Google Scholar]
- 14.Moller BN, Krebs B. Dynamic knee brace in the treatment of patellofemoral disorders. Arch Orthop Trauma Surg 1986;104:377–379 [DOI] [PubMed] [Google Scholar]
- 15.Sathe VM, Ireland ML, Ballantyne BT, et al. Acute effects of the Protonics system on patellofemoral alignment: an MRI study. Knee Surg Sports Traumatol Arthrosc 2002;10:44–48 [DOI] [PubMed] [Google Scholar]
- 16.McConnell J. The management of chondromalacia patellae: a long term solution. Aust J Physiother 1986;32:215–223 [DOI] [PubMed] [Google Scholar]
- 17.Crossley K, Cowan SM, Bennell KL, McConnell J. Patellar taping: is clinical success supported by scientific evidence? Man Ther 2000;5:142–150 [DOI] [PubMed] [Google Scholar]
- 18.Fredericson M, Yoon K. Physical examination and patellofemoral pain syndrome. Am J Phys Med Rehabil 2006;85:234–243 [DOI] [PubMed] [Google Scholar]
- 19.LaBella C. Patellofemoral pain syndrome: evaluation and treatment. Prim Care 2004;31:977–1003 [DOI] [PubMed] [Google Scholar]
- 20.Hergenroeder AC. Prevention of sports injuries. Pediatrics 1998;101:1057–1063 [DOI] [PubMed] [Google Scholar]
- 21.Bockrath K, Wooden C, Worrell T, et al. Effects of patella taping on patella position and perceived pain. Med Sci Sports Exerc 1993;25:989–992 [PubMed] [Google Scholar]
- 22.Christou EA. Patellar taping increases vastus medialis oblique activity in the presence of patellofemoral pain. J Electromyogr Kinesiol 2004;14:495–504 [DOI] [PubMed] [Google Scholar]
- 23.Salsich GB, Perman WH. Patellofemoral joint contact area is influenced by tibiofemoral rotation alignment in individuals who have patellofemoral pain. J Orthop Sports Phys Ther 2007;37:521–528 [DOI] [PubMed] [Google Scholar]
- 24.Lesher JD, Sutlive TG, Miller GA, et al. Development of a clinical prediction rule for classifying patients with patellofemoral pain syndrome who respond to patellar taping. J Orthop Sports Phys Ther 2006;36:854–866 [DOI] [PubMed] [Google Scholar]
- 25.Warden SJ, Hinman RS, Watson MA, Jr, et al. Patellar taping and bracing for the treatment of chronic knee pain: a systematic review and meta-analysis. Arthritis Rheum 2008;59:73–83 [DOI] [PubMed] [Google Scholar]
- 26.Whittingham M, Palmer S, Macmillan F. Effects of taping on pain and function in patellofemoral pain syndrome: a randomized controlled trial. J Orthop Sports Phys Ther 2004;34:504–510 [DOI] [PubMed] [Google Scholar]
- 27.Larsen B, Andreasen E, Urfer A, et al. Patellar taping: a radiographic examination of the medial glide technique. Am J Sports Med 1995;23:465–471 [DOI] [PubMed] [Google Scholar]
- 28.Gigante A, Pasquinelli FM, Paladini P, et al. The effects of patellar taping on patellofemoral incongruence. A computed tomography study. Am J Sports Med 2001;29:88–92 [DOI] [PubMed] [Google Scholar]
- 29.Pfeiffer RP, DeBeliso M, Shea KG, et al. Kinematic MRI assessment of McConnell taping before and after exercise. Am J Sports Med 2004;32:621–628 [DOI] [PubMed] [Google Scholar]
- 30.Worrell T, Ingersoll CD, Bockrath-Pugliese K, Minis P. Effect of patellar taping and bracing on patellar position as determined by MRI in patients with patellofemoral pain. J Athl Train 1998;33:16–20 [PMC free article] [PubMed] [Google Scholar]
- 31.Bourne MH, Hazel WA, Jr, Scott SG, Sim FH. Anterior knee pain. Mayo Clin Proc 1988;63:482–491 [DOI] [PubMed] [Google Scholar]
- 32.Post WR. Clinical evaluation of patients with patellofemoral disorders. Arthroscopy 1999;15:841–851 [DOI] [PubMed] [Google Scholar]
- 33.Sheehan FT, Derasari A, Fine KM, et al. Q-angle and J-sign: indicative of maltracking subgroups in patellofemoral pain. Clin Orthop Relat Res 2009May9 [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Seisler A, Sheehan FT. Normative three-dimensional patellofemoral and tibiofemoral kinematics: a dynamic, in vivo study. IEEE Trans Biomed Eng 2007;54:1333–1341 [DOI] [PubMed] [Google Scholar]
- 35.Brossmann J, Muhle C, Schroder C, et al. Patellar tracking patterns during active and passive knee extension: evaluation with motion-triggered cine MR imaging. Radiology 1993;187:205–212 [DOI] [PubMed] [Google Scholar]
- 36.Draper CE, Besier TF, Santos JM, et al. Using real-time MRI to quantify altered joint kinematics in subjects with patellofemoral pain and to evaluate the effects of a patellar brace or sleeve on joint motion. J Orthop Res 2009;27:571–577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Shibanuma N, Sheehan FT, Lipsky PE, Stanhope SJ. Sensitivity of femoral orientation estimates to condylar surface and MR image plane location. J Magn Reson Imaging 2004;20:300–305 [DOI] [PubMed] [Google Scholar]
- 38.Shibanuma N, Sheehan FT, Stanhope SJ. Limb positioning is critical for defining patellofemoral alignment and femoral shape. Clin Orthop Relat Res 2005;(434):198–206 [DOI] [PubMed] [Google Scholar]
- 39.Sheehan FT, Zajac FE, Drace JE. Using cine phase contrast magnetic resonance imaging to non-invasively study in vivo knee dynamics. J Biomech 1998;31:21–26 [DOI] [PubMed] [Google Scholar]
- 40.Rebmann AJ, Sheehan FT. Precise 3D skeletal kinematics using fast phase contrast magnetic resonance imaging. J Magn Reson Imaging 2003;17:206–213 [DOI] [PubMed] [Google Scholar]
- 41.Sheehan FT, Drace JE. Human patellar tendon strain (a non-invasive, in vivo study). Clin Orthop Relat Res 2000;370:201–207 [PubMed] [Google Scholar]
- 42.Powers CM. Patellar kinematics, part II: the influence of the depth of the trochlear groove in subjects with and without patellofemoral pain. Phys Ther 2000;80:965–978 [PubMed] [Google Scholar]
- 43.Ward SR, Terk MR, Powers CM. Patella alta: association with patellofemoral alignment and changes in contact area during weight-bearing. J Bone Joint Surg Am 2007;89:1749–1755 [DOI] [PubMed] [Google Scholar]
- 44.Kowall MG, Kolk G, Nuber GW, et al. Patellar taping in the treatment of patellofemoral pain. A prospective randomized study. Am J Sports Med 1996;24:61–66 [DOI] [PubMed] [Google Scholar]
- 45.Bennell K, Duncan M, Cowan S. Effect of patellar taping on vasti onset timing, knee kinematics, and kinetics in asymptomatic individuals with a delayed onset of vastus medialis oblique. J Orthop Res 2006;24:1854–1860 [DOI] [PubMed] [Google Scholar]