Abstract
Planning programs for the prevention and treatment of cardiovascular disease (CVD) is a challenge to every community that wants to make the best use of its limited resources. Selecting programs that provide the greatest impact is difficult because of the complex set of causal pathways and delays that link risk factors to CVD. We describe a system dynamics simulation model developed for a county health department that incorporates and tracks the effects of those risk factors over time on both first-time and recurrent events. We also describe how the model was used to evaluate the potential impacts of various intervention strategies for reducing the county's CVD burden and present the results of those policy tests.
More than 27 million Americans have experienced an ischemic heart event, stroke, or hospitalization for heart failure or peripheral arterial disease. These cardiovascular events are the leading cause of death in the United States and are responsible for over 700 000 deaths each year. The American Heart Association estimates the annual cost of cardiovascular disease (CVD) to be $155 billion in direct health care costs and another $92 billion in indirect costs reflecting lost productivity.1 Reducing the risk for CVD is a complex undertaking involving partnership among health providers, public and voluntary agencies, and the general public. Much of the responsibility for organizing local programs and systems of care for CVD falls on county health departments and other local agencies. We describe the application of system dynamics simulation modeling to support planning programs for CVD in El Paso County, Colorado. We used the system dynamics model to project trajectories for future incidence and prevalence of CVD under different plausible scenarios for population risk and different strategies for reducing the county's CVD burden.
The work presented here was done in support of and was funded by the Cancer, Cardiovascular, and Pulmonary Disease (CCPD) Project of the El Paso County Department of Public Health and Environment. The CCPD project is a collaborative effort to reduce the burden of chronic illness through comprehensive prevention, early detection, and treatment services.
System dynamics is an analytic approach for representing complex human systems and understanding how their components interact over time to create problems that resist easy solution. A system dynamics simulation model, which often consists of hundreds or thousands of equations, is developed uniquely to represent a dynamically changing problem situation as it is described by policymakers, subject matter experts, and available data. The participatory and iterative process of system dynamics model development are described elsewhere.2
Mathematically, a system dynamics model is an interconnected system of differential equations that are simulated on a computer because they are too large and complex to have closed-form analytic solutions. In health applications, the state or stock variables in these equations typically include population subgroups moving among various categories of health or disease, but they may also include resources such as staff and their skill sets. One specifies the initial values for the stocks, plus algebraic equations describing how the various flows into and out of the stocks are determined, and numerical estimates for the coefficients in these equations. The computer does the rest, calculating through the entire set of equations and updating the stock variables through small increments of time, until the final simulation time is reached, often decades into the future. With modern simulation software packages, such as Vensim (Ventana Systems, Harvard, MA), which we used in the present study, it is possible to simulate even a large system dynamics model in no more than a few seconds.
System dynamics simulation models help policymakers understand the impact of different interventions to find those that have the greatest leverage in the short term and in the longer term. To test an intervention, one simply makes appropriate changes to the corresponding input assumptions to the model and performs another simulation.
System dynamics has been applied to various chronic disease issues since the 1970s.3,4 The work described here builds most directly on a line of work that began in 2002 in Whatcom County, Washington, to help that community understand the potential impact of chronic disease programs focused on diabetes and heart failure and the financial impact of those programs on various providers and insurers.5 That work was carried further by the US Centers for Disease Control and Prevention (CDC) in the areas of diabetes and obesity, and more recently, cardiovascular disease.6–10
A SIMULATION MODEL OF CARDIOVASCULAR DISEASE FOR EL PASO COUNTY
The CVD modeling for El Paso County builds directly on a recent CDC-sponsored effort to model the causal factors leading up to first-time CVD events. The CDC model reproduces national-level risk factor prevalence data from the National Health and Nutrition Examination Survey (NHANES) covering 1988 through 2004, and first-event frequency and mortality data from the American Heart Association for 2003, and has been shown to have policy findings that are insensitive to parametric uncertainties.10 The model disaggregates the population into 6 subgroups based on gender and age group (18–29 years, 30–64 years, and 65 years and older). These subgroups have differing risk and mortality profiles, and the model shows how overall population rates of risk and mortality change inevitably over time as the population ages.
The CDC model includes several proximal risk factors that have been shown to have a direct effect on the incidence of first-time events, namely, high blood pressure, high cholesterol, diabetes, smoking, secondhand smoke, and small particulate air pollution. Secondary factors associated with these primary risk factors were also included. For example, obesity, physical activity, and quality of diet act indirectly through their effects on high blood pressure, high cholesterol, and diabetes. Psychosocial stress acts indirectly through high blood pressure and obesity. Receiving quality primary care affects the likelihood of diagnosing and controlling high blood pressure, high cholesterol, and diabetes as well as guiding patients to quit smoking, lose weight, and manage their stress. Smoking cessation also reduces the likelihood that others will be exposed to secondhand smoke, another risk factor.
Social determinants such as economic or educational disadvantage are already reflected in the average prevalence of the various risk factors mentioned in the previous paragraph. Population subgroups with lower socioeconomic status typically have a higher prevalence of certain risks, including smoking, obesity, and poor diet. However, we have not modeled separate socioeconomic status subgroups in El Paso County, because the data needed to support this finer breakdown (simultaneously by gender, age group, and socioeconomic status) in many cases do not presently exist.
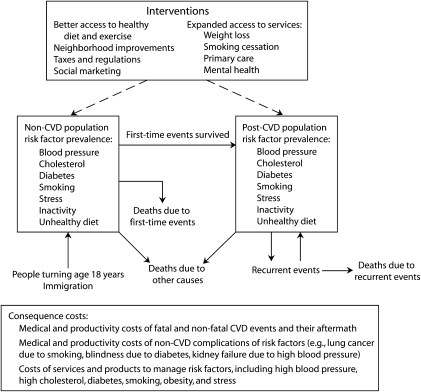
We recalibrated the CDC model for El Paso County on the basis of the local population and local conditions and also expanded upon the CDC model by including the “post-CVD” population, that is, the population of people who had already had an event and survived. An overview of the resulting model is presented in Figure 1. The post-CVD population, although only a small percentage of the population (we estimate 8% of adults in El Paso County in 2003), accounted for a substantial portion of the total CVD burden in the form of ongoing morbidity and care, as well as recurrent events. The El Paso County model consisted of about 900 input elements and 2400 output elements, all of them simulated every quarter-year starting in 2003 and ending in 2040. The model's output elements included 80 population stocks, which kept track of changes in the prevalence of obesity, smoking, high blood pressure, high cholesterol, and diabetes, and distinguishing between those stocks for the non-CVD and post-CVD populations. The overall population was increased by inflows of people turning 18 and by net immigration, and was decreased by deaths.
FIGURE 1.
Overview of the cardiovascular disease (CVD) model.
We used the El Paso County model to project what the prevalence and burden of CVD would be if conditions remained as they are currently, then to assess the potential impact of different programmatic interventions. The model also projected the capacity required for various programs to have their desired impacts. The model allowed for a variety of potential interventions, described further below. Several of these interventions increased the accessibility of relevant services (such as preventive medical care) and resources (such as recreational facilities), especially for those who cannot afford them, or promoted the utilization of these services and resources through social marketing. Other interventions were regulatory in nature, such as tobacco taxes or bans on smoking in public places.
The model calculated first-time cardiovascular events on the basis of the risk factor prevalence of the non-CVD population (those who had not previously experienced a cardiovascular event). The likelihood of a recurrent event for the post-CVD population was substantially higher than the likelihood of a first event for the non-CVD population. Because of the vulnerability of the post-CVD population to recurrent events, the model offered the possibility of targeting that population for certain interventions, including access to risk-management services and improvement in the quality of post-event medical care provided.
The model attempted to quantify all the costs related to the diseases and risk factors seen in Figure 1. These total consequence costs included both medical costs and productivity costs of disability and premature death, which were calculated for CVD events as well as for non-CVD complications of the risk factors. Smoking and diabetes, in particular, have costly non-CVD consequences (e.g., lung cancer and chronic obstructive pulmonary disease from smoking; kidney failure, blindness, and amputations from diabetes) that may be affected by interventions considered by the model. The model also captured the costs of the services and products used to manage the risk factors, that is, the costs of preventive medical care, smoking cessation, weight loss, and stress management.
Data Sources for the El Paso County Model
As seen in Table 1, we used several data sources to quantify the model and initialize it to represent El Paso County in 2003. Data specific to El Paso County were available on the population and its growth, the prevalence of key risk factors, and CVD hospitalization and mortality. For other matters, including event rates, unit costs, and intervention effect sizes, we relied on national-level data sources and studies, with adjustment in some cases to reflect known differences in El Paso County. Extension of the model to include recurrent events was based on national data from the American Heart Association and other sources. Adjustments of risk factor prevalence to El Paso County were based on the Behavioral Risk Factor Surveillance System (BRFSS) and various local sources. The El Paso County model reproduced data on CVD hospitalizations and deaths from the State Health Department and Colorado Hospital Association for the period of 2004 through 2006 (K. Bol, Colorado Department of Public Health and Environment, Health and Statistics Section, personal communication, January 31, 2008).
TABLE 1.
Data Sources for System Dynamics Simulation Modeling: El Paso County, Colorado
| Data Element | Source |
| El Paso County population estimates | State of Colorado population projections for El Paso County (2003) |
| El Paso County risk factor prevalence for high blood pressure, high cholesterol, obesity, and smoking | BRFSS data from the Colorado Department of Health and Environment, Health Statistics Section (2004–2006)a (also verified by using Colorado Steps to a Healthier US community data) |
| El Paso County diabetes prevalence | Prior unpublished El Paso County diabetes analysis (2006) |
| Estimates of program impacts for risk factor reduction | Expert judgment from CDC CVD study (2007)10 |
| Effects of risk factor prevalence on first-time CVD event rates | Framingham Heart Study data and Framingham risk calculators adapted from CDC CVD study10,11 |
| Recurrent CVD event rates and post-CVD prevalence | Derived from American Heart Association data (2006)b and adjusted to reflect lower event rates in El Paso County |
| Effects of risk factor prevalence on recurrent CVD events | Published medical literature12–16 |
| Hospital and nursing home utilization for CVD | National Center for Health Statistics National Hospital Discharge Survey (2005)17 and National Nursing Home Survey (1999)18 |
| CVD health care and disability costs | American Heart Association (2007)1 |
| El Paso County CVD hospitalization and mortality | Colorado Department of Health and Environment, Health Statistics Section, and Colorado Hospital Association (2004–2006)c |
Note. BRFSS = Behavioral Risk Factor Surveillance System; CDC = Centers for Disease Control and Prevention; CVD = cardiovascular disease.
Source: R. Tolliver, Colorado Department of Public Health and Environment, Health Statistics Section, personal communication, March 13, 2008.
Source: American Heart Association, heart disease and stroke statistics, 2006. Special run on database performed by Research Triangle Institute.
Source: K. Bol, Colorado Department of Public Health and Environment, Health Statistics Section, personal communication, January 31, 2008.
A Status Quo Simulation
After quantifying the model, we produced a “status quo” simulation that assumed continuation of existing programs at their current levels, with no new programmatic interventions. The status quo simulation also assumed no national or local trends driving changes in risk factors or in the management of these risk factors. It also assumed no inflation in unit costs, so that any simulated cost increases were due only to growth in the frequency of adverse events and in service volumes. This growth in events and volumes is largely the result of growth and aging of the population. But aging and turnover of the population also lead to a gradual decrease in smoking prevalence and gradual increases in prevalences of obesity, high blood pressure, and diabetes. These changes in risk factor prevalence have some modifying effect on the growth in events and volumes.
The results of the status quo simulation over the period of 2003 through 2040 are displayed in Table 2. In the case of chronic diseases like CVD, several decades may be required to see the full ramifications of interventions as they play out in the context of population aging and turnover. Because the status quo simulation is based on assumptions that may or may not come to pass, the results are presented not as a forecast, but rather as a reference point of departure for comparing other simulations. In Table 2, CVD events and deaths are categorized as first time and recurrent. From 2003 to 2020, annual CVD events were projected to increase by 58% (from 4479 to 7079) and annual CVD deaths by 77% (from 767 to 1358). Recurrent events began at 20% of total CVD events but grew to 37% by 2020, as the post-CVD population grew as a fraction of adults from 8% to 15%. This growth in CVD events and post-CVD population is of concern because it implies costly demands on the local healthcare infrastructure.
TABLE 2.
Results of the Status Quo Projection for Cardiovascular Disease (CVD) Events and Death From 2003 to 2040: El Paso County, Colorado
| Year 2003 | Year 2020 | Year 2040 | |
| No. of CVD events | |||
| First time | 3 566 | 4 889 | 6 688 |
| Recurrent | 913 | 2 190 | 4 003 |
| Total | 4 479 | 7 079 | 10 691 |
| No. of CVD deaths | |||
| First Time | 550 | 835 | 1 231 |
| Recurrent | 217 | 523 | 960 |
| Total | 767 | 1 358 | 2 191 |
| Post-CVD population | 32 356 | 78 685 | 144 272 |
| Post-CVD population as percentage of population over 18 years of age, % | 8 | 15 | 19 |
| Consequence costs, millions $ | |||
| CVD medicala | 171 | 370 | 652 |
| CVD productivity | 450 | 843 | 1 333 |
| Non-CVD complications | 460 | 526 | 674 |
| Risk factor management | 84 | 136 | 212 |
| Total | 1 165 | 1 875 | 2 871 |
| Medical costs for CVD events, millions $ | |||
| First-time events | 42 | 57 | 78 |
| Recurrent events | 11 | 26 | 47 |
| Total | 53 | 83 | 125 |
| Annual medical maintenance costs for post-CVD population, millions $ | |||
| Physician | 27 | 66 | 121 |
| Nursing home | 54 | 132 | 243 |
| Home care | 15 | 36 | 67 |
| Medication | 22 | 53 | 96 |
| Total | 118 | 287 | 527 |
Medical costs are the sum of event costs and annual maintenance costs.
Total consequence costs rose from $1.16 billion in 2003 to $1.88 billion in 2020. Most of this increase came from growth in CVD-related medical costs, which rose from $170 million to $370 million, and CVD-related productivity costs, which rose from $450 million to $843 million. CVD medical costs include hospitalization, physicians’ fees, and other costs of first-time and recurrent events and their sequelae. CVD-related productivity costs include workdays lost by those who survive CVD events and years of life lost by those who die as a result of the events.
The largest subset of CVD-related medical costs (starting at 69% in 2003 and rising to 77% in 2020) was annual maintenance costs for the post-CVD population, including physician's fees (aside from basic risk factor management), cardiovascular medications, and the costs of nursing homes, home care, and durable equipment. Nursing home expenses made up the largest portion of these maintenance costs, at 46%. Maintenance costs alone were projected to rise from $118 million in 2003 to $287 million by 2020.
Before examining simulations of specific CVD interventions, it is useful to understand what a dramatic reduction in risk factors might possibly, in theory, achieve. It is possible in the model to calculate the extent to which first-time CVD events and deaths would be reduced if all modifiable proximal risk factors we have modeled—high blood pressure, high cholesterol, diabetes, smoking, and small particulate air pollution—were eliminated. This would implicitly leave as determinants of CVD only the effects of genetics and aging combined with other risk factors we have not modeled, including the borderline disorders of prehypertension, borderline cholesterol, and prediabetes. The model suggested that elimination of the modifiable risk factors we have modeled could reduce first-time CVD events by 50% and fatalities from first-time CVD events by 60% below the status quo.
Examining the Effects of Alternative Interventions
Interventions assessed with the model fall into 2 broad clusters: lifestyle and environment, and medical and mental health care. Although these interventions can be tested individually, the simulations reported below used them together in the following clusters.
For lifestyle and environment, the interventions included were as follows:
promote and improve access to physical activity (2 interventions),
promote and improve access to healthy diet (2 interventions),
restrict or tax junk food sales (1 intervention),
promote and improve access to weight-loss services (2 interventions),
campaign against smoking (1 intervention),
increase taxes and restrictions on tobacco sales (1 intervention),
promote and improve access to smoking cessation services and products (2 interventions),
ban smoking in workplaces and other public places (1 intervention),
pass local ordinances to reduce small particulate air pollution (1 intervention), and
provide social supports, income supports, job/training programs, or neighborhood safety programs to reduce sources of stress in socioeconomically disadvantaged areas (1 intervention).
For medical and mental health care, the interventions included were as follows:
promote and improve access to medical care (2 interventions),
improve the quality of medical care by promoting adherence to established guidelines (1 intervention), and
promote and improve access to mental health services to mitigate stress (2 interventions).
We assumed that the lifestyle and environment interventions were applicable to the entire adult population, being available to or affecting individuals whether they have already experienced a CVD event. In contrast, each of the medical and mental health care interventions may be made available to the entire adult population, or, if desired, may be targeted only to the post-CVD population. Medical interventions for the non-CVD population would emphasize improved diagnosis and control of high blood pressure, high cholesterol, and diabetes by primary care providers. Medical interventions for the post-CVD population similarly would address these chronic disorders, but would also include the use of other procedures and medications that have been shown to reduce the likelihood of recurrent CVD events.
In evaluating these interventions, we assumed that increased access would make services available to 100% of the population (i.e., no financial barriers) and social marketing and tobacco and junk food taxes would achieve the maximum impacts demonstrated or seriously proposed elsewhere in the United States. Furthermore, we assumed that small-particle air pollution and chronic stress both could be reduced by 50%, exposures to secondhand smoke in public places could be reduced to zero, and adherence to guidelines in primary care would increase from 54% to 75%.
We tested a variety of interventions singly and in combination. These included 3 combination strategies listed below. We assumed that every component intervention of a strategy and its effects were phased in over time starting in 2008 and would be fully implemented by 2012.
The strategies were as follows:
Community-wide lifestyle and environment: All 14 lifestyle and environment interventions described above were implemented, but none in medical and mental health care;
Community-wide lifestyle and environment plus post-CVD care: In addition to the 14 lifestyle and environment interventions, the 5 medical and mental health care interventions were implemented, but only for the post-CVD population;
Community-wide lifestyle and environment plus care for all: In addition to the 14 lifestyle and environment interventions, the 5 medical and mental health care interventions were implemented for the entire adult population, not only for the post-CVD population.
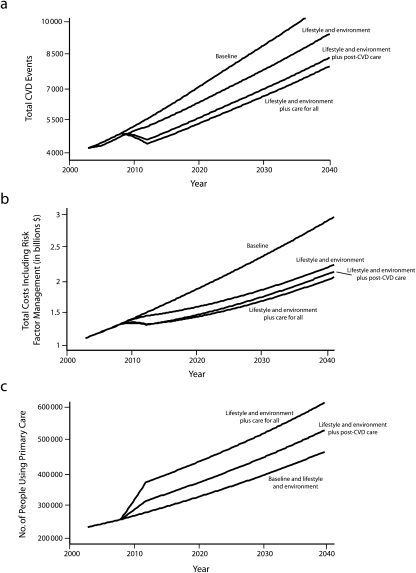
The results of these combination strategies are presented in Figure 2 and Table 3. Of the 3 strategies, community wide lifestyle and environment plus care for all had the greatest ability to reduce CVD events and deaths as well as total consequence costs. It was at least twice as effective at reducing CVD events and deaths as the community-wide lifestyle and environment strategy, and to a lesser degree was also more effective than the community-wide lifestyle and environment plus post-CVD care strategy. However, the community-wide lifestyle and environment plus care for all strategy also implied a large increase in the need for primary care capacity, 30% relative to the status quo. In this context, a strategy that depends so heavily on the expansion of primary care may not be realistic.
FIGURE 2.
Impacts from 2003–2040 of the interventions on cardiovascular disease (CVD) (a) events, (b) costs, and (c) primary care: El Paso County, Colorado.
TABLE 3.
Percentage Changes From Status Quo Values to 2020 Based on Simulations With Cardiovascular Disease (CVD) Interventions: El Paso County, Colorado
| CVD Events |
CVD Costs |
People Receiving Primary Care |
|||||||
| CVD Intervention | First Time | Recurrent | Total | Complications and maintenance | Risk factor management | Total | Non-CVD | Post-CVD | Total |
| Lifestyle and environment, % change | −10 | −8 | −9 | −15 | −2 | −14 | 1 | −5 | 0 |
| Lifestyle and environment + post-CVD care, % change | −9 | −40 | −19 | −23 | 4 | −20 | 9 | 32 | 12 |
| Lifestyle and environment + care for all, % change | −13 | −41 | −22 | −28 | 47 | −22 | 30 | 29 | 30 |
Note. Post-CVD care includes medical and mental health care for those who have experienced a CVD incident. Care for all includes medical and mental health care for the total population, regardless of CVD status.
The community-wide lifestyle and environment plus post CVD care strategy reduced CVD events by 85% to 86% as much as the reduction achieved by the community-wide lifestyle and environment plus care for all strategy. Similarly, it reduced CVD deaths by 73% to 79% as much as the community-wide lifestyle and environment plus care for all strategy. It required a smaller expansion of primary care capacity relative to the status quo, 12% to 13% rather than 30%, which may be a more achievable goal in El Paso County.
Focusing on the post-CVD population yielded substantial benefit for a smaller increment in resources. The community-wide lifestyle and environment plus care for all strategy produced a 41% reduction in recurrent events by 2020 but only a 13% reduction in first-time events. Yet, of the increase in primary care demand noted above, about 60% was for the non-CVD population and only 40% for the post-CVD population. Consequently, the extra medical effort for the non-CVD population was not as effective, in terms of primary care resource requirements, as it was for the post-CVD population. Note also that the lifestyle and environmental programs within the community-wide lifestyle and environment plus care for all strategy accounted for 77% to 79% of the reduction in first-time CVD events and 57% to 62% of the reduction in deaths from first-time events. This means that the lifestyle and environmental programs accounted for more of the total benefit for the non-CVD population than do the medical and mental health care interventions. Thus, with the community-wide lifestyle and environment plus post CVD care strategy, one can get substantial improvements for the non-CVD population with lifestyle and environmental programs alone and, for a relatively modest increase in primary care capacity, substantial improvements for the post-CVD population as well.
IMPLICATIONS OF RESULTS
System dynamics modeling is a proven methodology for assessing the potential impact of interventions to reduce the burden of chronic illness. We have presented a system dynamics modeling effort that applied this approach to planning CVD interventions for El Paso County. Simulations with the model have revealed strategies that can have an impact on CVD while operating within realistic resource constraints. The results of these simulations are not meant to be forecasts—given uncertainties about the trajectory of population risks—but can nonetheless provide robust conclusions about how strategies compare with one another. These conclusions also reflect assumptions about the efficacy of various interventions that may not hold true when programs are actually implemented.
The simulations suggest a few broad conclusions. Lifestyle and environment strategies alone can have a significant impact on reducing first-time CVD events and deaths as well as total consequence costs. Medical interventions can also help substantially in reducing the CVD burden for both the non-CVD and post-CVD populations, but most impressively for the latter. Limiting the medical interventions to the post-CVD population does not sacrifice much in terms of benefits but requires much less of an expansion in medical capacity than what would be the case otherwise.
Our analysis identified that some of the component interventions are more effective and cost-saving than others, which gives some indication of how a community should focus its efforts when public health resources are limited. For example, although an expansion of mental health services could be a valuable tool for broader reasons, the model suggests that it may not be a cost-effective way of reducing psychosocial stress contributing to the county's CVD burden. To explore this idea further, we could remove components of the community-wide lifestyle and environment plus care for all strategy in a stepwise fashion and observe which combination of interventions offered the greatest payoff in return for the additional requirements of public health effort and clinical and other community resources.
The third graph in Figure 2 also reflects the value of this model for CVD planning at the county level by providing specific targets for planning capacity expansion. Having specific targets for primary care availability or smoking cessation programs, for example, allows the county's public health and health care provider community to plan a set of service expansions that, taken together, meet the overall need. Without specific targets, planning is less directed and outcomes may be unmeasurable.
For El Paso County, even the less resource-intensive strategy, community-wide lifestyle and environment plus post-CVD care, would require almost a 20% increase in overall primary care capacity over the period 2008 through 2012 and 12% more capacity than for the status quo in 2020. Community stakeholders will need to discuss how this increase can be achieved. How much can come from attracting additional physicians? How much can come from having nurse practitioners and physician assistants take on expanded roles? There is an additional question of how services will be financed for those without insurance or the ability to pay. Ensuring that primary care is effective in reducing the prevalence of CVD risk factors will also require education in the provider community and adoption of practice guidelines that stress attention to CVD risks for the general population and risks of recurrent events for those in the post-CVD group.
Significant increases in capacity of other services such as smoking cessation will also be needed. The simulation results suggest that an 80% increase in smoking cessation capacity would be required over the 4-year period. There would be a decrease in utilization of this capacity after the initial peak as people actually quit smoking, but some capacity would continue to be required to deal with new smokers and people who relapse. Similar increases would be required for weight-loss services. Stakeholders will need to decide where that capacity will come from and, for those without the ability to pay out-of-pocket or through insurance, how those services will be financed.
Many county and local health departments are well-placed to serve as convenors of comprehensive efforts to reduce the burden of CVD and other chronic diseases. System dynamics models can inform and guide these efforts by projecting the potential impacts of interventions and helping communities focus scarce resources on the interventions likely to be the most effective.
Acknowledgments
The work was funded by the Cancer, Cardiovascular Disease, and Pulmonary Disease Competitive Grants Program of the Colorado Department of Public Health and Environment (grant 06-00833).
The authors thank the following individuals, all of whom were employed by the El Paso County Department of Health and Environment, for their contributions to the work presented in this article: Kathy Rice, MS, Community Health Planner; Mary Talbott, MEd, Development Director; Karen Williamson, BS, Lead System Project Manager; Kandi Buckland, RN, MPA, Acting Public Health Director; Bernadette Albanese, MD, MPH, Medical Director; Rosemary Bakes-Martin, MS, MPH, Public Health Administrator (deceased July 2008).
Human Participant Protection
No institutional review board approval was required because only aggregate data were used in the course of this work.
References
- 1.American Heart Association. Heart Disease and Stroke Statistics. 2007 Update-at-a-Glance Dallas, TX: American Heart Association; 2007:2, 37 [Google Scholar]
- 2.Sterman JD. Business Dynamics: Systems Thinking and Modeling for a Complex World Boston, MA: Irwin/McGraw-Hill; 2000 [Google Scholar]
- 3.Luginbuhl W, Forsyth B, Hirsch G, Goodman M. Prevention and rehabilitation as a means of cost-containment: the example of myocardial infarction. J Public Health Policy 1981;2(2):103–115 [PubMed] [Google Scholar]
- 4.Homer JB, Hirsch GB. System dynamics modeling for public health: background and opportunities. Am J Public Health 2006;96(3):452–458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Homer J, Hirsch G, Minniti M, Pierson M. Models for collaboration: how system dynamics helped a community organize cost-effective care for chronic illness. Syst Dynamics Rev 2004;20(3):199–222 [Google Scholar]
- 6.Jones AP, Homer JB, Murphy DL, Essien JDK, Milstein B, Seville DA. Understanding diabetes population dynamics through simulation modeling and experimentation. Am J Public Health 2006;96(3):488–494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Milstein B, Jones A, Homer J, Murphy D, Essien J, Seville D. Charting plausible futures for diabetes prevalence: a role for system dynamics simulation modeling. Prev Chronic Dis 2007;4(3):A52. [PMC free article] [PubMed] [Google Scholar]
- 8.Homer J, Milstein B, Dietz W, Buchner D, Majestic D. Obesity population dynamics: exploring historical growth and plausible futures in the US. Paper presented at: 24th International Conference of the System Dynamics Society; July 26, 2006; Nijmegen, The Netherlands [Google Scholar]
- 9.Homer J, Milstein B, Wile K, Pratibhu P, Farris R, Orenstein D. Modeling the local dynamics of cardiovascular health: risk factors, context, and capacity. Prev Chronic Dis 2008;5(2):A63. [PMC free article] [PubMed] [Google Scholar]
- 10.Homer J, Milstein B, Wile K, Trogdon J, Huang P, Orenstein D. Simulating and evaluating local interventions to improve cardiovascular health. Prev Chronic Dis 2010:7(1). [PMC free article] [PubMed] [Google Scholar]
- 11.Anderson KM, Odell PM, Wilson PW, Kannel WB. Cardiovascular disease risk profiles. Am Heart J 1991;121(1 pt 2):293–298 [DOI] [PubMed] [Google Scholar]
- 12.Rashid P, Leonardi-Bee J, Bath P. Blood pressure reduction and secondary prevention of stroke and other vascular events: a systematic review. Stroke 2003;34(11):2741–2748 [DOI] [PubMed] [Google Scholar]
- 13.Critchley JA, Capewell S. Mortality risk reduction associated with smoking cessation in patients with coronary heart disease: a systematic review. JAMA 2003;290(1):86–97 [DOI] [PubMed] [Google Scholar]
- 14.LaRosa JC, He J, Vupputuri S. Effect of statins on risk of coronary disease: a meta-analysis of randomized controlled trials. JAMA 1999;282(24):2340–2346 [DOI] [PubMed] [Google Scholar]
- 15.Stettler C, Alleman S, Juni P, Cull CA, Holman RR, Egger M, Krahenbuhl S, Diem P. Glycemic control and macrovascular disease in types 1 and 2 diabetes mellitus: meta-analysis of randomized trials. Am Heart J 2006;152(1):27–38 [DOI] [PubMed] [Google Scholar]
- 16.Hackam DG, Spence DJ. Combining multiple approaches for the secondary prevention of vascular events after stroke: a quantitative modeling study. Stroke 2007;38(6):1881–1885 [DOI] [PubMed] [Google Scholar]
- 17.DeFrances CJ, Hall MJ. 2005National Hospital Discharge Survey. Advance data from vital and health statistics; no 385 Hyattsville, MD: National Center for Health Statistics; 2007:Table 4 [Google Scholar]
- 18.Jones AL, Dwyer LL, Bercovitz AR, Strahan GW. The National Nursing Home Survey: 2004 Overview. Table 28. National Center for Health Statistics. Vital Health Stat 2009;13(167). [PubMed] [Google Scholar]