Abstract
Objectives. We investigated whether mothers from ethnic minority groups have better pregnancy outcomes when they live in counties with higher densities of people from the same ethnic group—despite such areas tending to be more socioeconomically deprived.
Methods. In a population-based US study, we used multilevel logistic regression analysis to test whether same-ethnic density was associated with maternal smoking in pregnancy, low birthweight, preterm delivery, and infant mortality among 581 151 Black and 763 201 Hispanic mothers and their infants, with adjustment for maternal and area-level characteristics.
Results. Higher levels of same-ethnic density were associated with reduced odds of infant mortality among Hispanic mothers, and reduced odds of smoking during pregnancy for US-born Hispanic and Black mothers. For Black mothers, moderate levels of same-ethnic density were associated with increased risk of low birthweight and preterm delivery; high levels of same ethnic density had no additional effect.
Conclusions. Our results suggest that for Hispanic mothers, in contrast to Black mothers, the advantages of shared culture, social networks, and social capital protect maternal and infant health.
Numerous studies have shown that living in a socioeconomically deprived neighborhood exerts a contextual effect on the health of individual residents beyond their own socioeconomic status.1,2 This is likely to have a differential impact on some ethnic minority groups, such as African Americans and Hispanics. (Throughout this paper we have defined “ethnicity” as a global indicator of a person's heritage including both racial and ethnic origins.) Whereas the majority of poor White people live in nondeprived areas, poor African Americans are concentrated in areas of high poverty.3 Thus, it might be paradoxical to suggest that members of ethnic minority groups might be healthier when they live in areas with a high concentration of people of the same ethnicity.4,5 However, there is some evidence that living in communities that contain proportionally more people from the same ethnic group is protective for some health outcomes, once material deprivation is accounted for. The evidence for the protective effects of same-ethnic density is strongest for mental health,4,5 with the evidence for maternal and infant health outcomes more mixed.
The majority of studies that have investigated the impact of same-ethnic density on maternal and infant health have focused on African Americans or Black families (in this article, we use whichever term was used in the studies we describe). Two older ecological studies6,7 found that increasing levels of same-ethnic density for New York City African Americans were associated with increased fetal and neonatal mortality but not postneonatal mortality. Another study found no association between ethnic density measured in US cities and postneonatal mortality.8 More recent studies have tended to use multilevel analyses that controlled for individual-level measures of socioeconomic status, and focused on measures of morbidity, such as low birthweight (LBW), with less consistent results.9–14
One study of Chicago neighborhoods found that an increasing proportion of African American residents was associated with a reduced risk of LBW.13 Two other studies found that an increasing proportion of Black residents was associated with increased risk of LBW.11,14 However, other studies have found no significant associations between same-ethnic density and LBW.9,10,12
Five studies have investigated the impact of ethnic density on preterm delivery rates among African Americans.9,10,12,15,16 Studies of neighborhoods in Minnesota9 and North Carolina15 found same-ethnic density to be associated with increased risk of preterm delivery after adjustment for individual but not area measures of socioeconomic circumstances. Three other studies found no association between same-ethnic density and preterm delivery in models that included individual-level maternal education and area-level measures of socioeconomic circumstances.10,12,16
We are aware of only 1 study that has investigated the impact of same-ethnic density on maternal smoking during pregnancy, which found that it was associated with reduced risk of maternal smoking after adjustment for both individual and area measures of socioeconomic conditions.17
We found only 2 studies that have investigated the impact of ethnic density on Hispanic maternal and infant health. The first, conducted in the states of Arizona, California, New Mexico, and Texas, found lower rates of infant mortality for US-born Mexican-origin mothers living in counties with high concentrations of mothers of the same ethnicity.18 However, this effect was not found for mothers born outside the United States. The second study found no associations between same-ethnic density, as measured in Chicago census tracts, and LBW, preterm delivery, and maternal smoking after adjustment for economic disadvantage, maternal education, and violent crime.12
Further support for the protective effects of Hispanic density comes from the “Hispanic paradox.”19 Compared with the White majority population, Hispanic mothers tend to have better or equal pregnancy outcomes and better health-related behaviors despite generally having more disadvantaged socioeconomic circumstances.20–24 It has been proposed that this “paradox” can be explained by dietary factors, social support and cohesion, and cultural differences in relation to the importance of motherhood.23,24 However, long-term US residents who move away from ethnic enclaves25 are more likely to adopt Western health behaviors and values26 and may lose any protective effects of Hispanic culture. Thus, the protective effects of Hispanic culture are more likely to be maintained in communities of higher Hispanic density.
We hypothesized that maternal smoking during pregnancy, infant mortality, LBW, and preterm birth would be lower for non-Hispanic Black and Hispanic White (hereafter referred to as “Hispanic mothers”) mothers living in counties with a higher percentage of people of the same ethnicity, relative to their counterparts living in counties with a low percentage of people of the same ethnicity.
METHODS
We used data from the 2000 US Linked Birth and Infant Death Data Set,27 which was linked, via special license access, to the US Census 2000 summary file 328 by county of residence of the mother at the time of the infant's birth. The US Linked Birth and Infant Death Data Set cohort was created by the US National Center for Health Statistics (NCHS) by collating data from birth certificates for all live infants born in 2000 and the death certificates of those who died before their first birthday. The cohort is estimated to contain 98.6% of all non-White births.29 This study focuses on US resident non-Hispanic Black (n = 581 151) and Hispanic (n = 763 201) mothers of singleton births, living in 2215 and 2664 counties, respectively. The counties covered in the 2000 census vary in size from isolated communities such as Kalawao County, Hawaii, to Los Angeles County, California. The median population size of counties in which cohort members lived was 455 466 and the interquartile range was 118 085 to 1 223 499.
Maternal race/ethnicity was used as defined on the infant's birth certificate. Mothers described whether they were of Hispanic ethnicity and what race they considered themselves to belong to. We analyzed mothers who described themselves as non-Hispanic Black and Hispanic White, hereafter termed Black and Hispanic, respectively.
The same-ethnic density for each county of mother's residence was derived from summary file 3 of the US Census.28 Research has shown that the effects of ethnic density may not be linear14,30 and counties were categorized as having 0%–0.99%, 1%–4.99%, 5%–14.99%, 15%–49.99%, and ≥ 50% of Black residents for Black mothers, and having 0%–0.99%, 1%–4.99%, 5%–14.99%, 15%–49.99%, and ≥ 50% of Hispanic residents for Hispanic mothers. These categories were chosen as they enable the identification of small changes in ethnic density at low densities, yet they still facilitate the investigation of effects of higher ethnic density.
Three outcome measures were taken from birth certificate data: LBW (< 2500 g), preterm delivery (< 37 weeks gestation), and smoking during pregnancy (smoking 1 or more cigarettes per day during pregnancy). Smoking during pregnancy was not recorded in the State of California. Death certificates were used to ascertain whether the infant had died by his or her first birthday; failure to match birth and death certificates occurred in only 1.3% of records.27
Potential individual-level confounding variables of relationships between ethnic density and pregnancy outcomes included parity, maternal age, marital status, and socioeconomic status (as indicated by maternal education). Maternal nativity (whether the mother was born in the United States) was considered as both a confounding variable and a potential moderating variable for Hispanic mothers. County-level socioeconomic status was measured as median household income.
We conducted separate analyses for Black and Hispanic mothers and their infants. We used means and percentages to describe sample characteristics. These data have a multilevel structure with infant, maternal, and household characteristics at level 1 and counties at level 2. We used multilevel mixed-effects logistic regression, with the xtmelogit command in Stata version 10 (StataCorp LP, College Station, TX), to estimate the contextual effects of ethnic density in a random intercept model, with adjustment for individual-level sociodemographic characteristics and county-level median income. To assess whether maternal nativity moderated the effects of Hispanic ethnic density on infant outcomes we tested whether a random slope for maternal nativity that included a cross-level interaction between maternal nativity and county-level Hispanic density fit the data significantly better than a random intercept model. The significance test used was a likelihood ratio test with likelihood approximated by adaptive quadrature.
RESULTS
Table 1 shows the characteristics of mothers and infants by ethnicity. Compared with Hispanic mothers, a higher proportion of Black mothers smoked during pregnancy, and had infants who had LBW, who were delivered preterm, or who died during their first year. Black mothers were more likely to be unmarried, aged younger than 20 years or older than 35 years, primiparous, or of high parity. Black mothers also had more years of education and were much more likely to have been born in the United States. Additionally, Black mothers were more likely to live in counties with a low median income and in counties with a higher proportion of the population with the same ethnicity.
TABLE 1.
Descriptive Statistics of Black and Hispanic Mothers and Their Infants Born in 2000: US Linked Birth and Infant Death Data Set, 2000
| Black, No. (%) | Hispanic, No. (%) | |
| Mortality | ||
| Surviving | 574 078 (98.78) | 759 442 (99.51) |
| Died | 7073 (1.22) | 3759 (0.49) |
| Birthweight, g | ||
| ≥ 2500 | 515 056 (88.71) | 722 148 (94.67) |
| < 2500 | 65 556 (11.29) | 40 678 (5.33) |
| Gestational age | ||
| Term birth | 446 193 (84.42) | 624 512 (89.83) |
| Preterm birth | 82 321 (15.58) | 70 725 (10.17) |
| Smoking status | ||
| Nonsmoker | 494 008 (91.81) | 493 940 (97.12) |
| Smoker | 44 044 (8.19) | 14 627 (2.88) |
| Parity | ||
| 1 birth | 220 620 (38.09) | 285 348 (37.59) |
| 2 births | 171 655 (29.64) | 231 326 (30.47) |
| 3 births | 102 106 (17.63) | 141 863 (18.69) |
| 4 births | 46 553 (8.04) | 60 755 (8.00) |
| ≥ 5 births | 38 227 (6.60) | 39 885 (5.25) |
| Maternal age, y | ||
| < 15 | 3674 (0.63) | 2479 (0.32) |
| 15–19 | 113 132 (19.47) | 122 280 (16.02) |
| 20–24 | 190 038 (32.70) | 232 515 (30.47) |
| 25–29 | 131 655 (22.66) | 204 255 (26.77) |
| 30–34 | 87 092 (14.99) | 131 245 (17.20) |
| 35–39 | 45 144 (7.77) | 57 879 (7.58) |
| 40–54 | 10 333 (1.78) | 12 445 (1.63) |
| Maternal education, y | ||
| 0–8 | 13 743 (2.40) | 161 846 (21.67) |
| 9–11 | 131 901 (23.08) | 207 902 (27.84) |
| 12 | 227 898 (39.88) | 222 386 (29.78) |
| 13–15 | 131 674 (23.04) | 99 202 (13.28) |
| ≥ 16 | 66 261 (11.59) | 55 525 (7.43) |
| Marital status | ||
| Married | 180 461 (31.06) | 440 331 (57.72) |
| Unmarried | 400 523 (68.94) | 322 602 (42.28) |
| Maternal nativity | ||
| United States | 517 678 (89.52) | 289 767 (38.06) |
| Outside United States | 60 621 (10.48) | 471 653 (61.94) |
| Same-ethnic density | ||
| 0–0.99% | 2594 (0.45) | 12 407 (1.63) |
| 1–4.99% | 25 928 (4.46) | 118 567 (15.54) |
| 5–14.99% | 147 376 (25.36) | 365 678 (47.91) |
| 15–49.99% | 344 618 (59.30) | 221 268 (28.99) |
| ≥ 50% | 60 635 (10.43) | 45 281 (5.93) |
| Median income, $10 000s, mean (SD) | 4.09 (0.97) | 4.33 (1.03) |
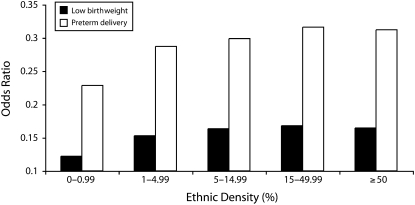
Table 2 shows the results of multilevel models that estimated associations between same-ethnic density and maternal and infant outcomes. All analyses were adjusted for parity, maternal age, marital status, maternal education, maternal nativity, and county-level median income. Among Black mothers, there was little evidence to support an association between ethnic density and infant mortality. However, ethnic density was significantly associated with each of the other outcomes. Black infants were at increased risk of LBW with increasing ethnic density. However, this was not a linear relationship (Figure 1 and Table 2). Black mothers who were categorized as living in counties with densities of 0%–0.99% Black residents had the lowest odds of LBW. A relatively small increase in Black density to 1%–4.99% led to the greatest increase in the odds ratio for LBW; the odds ratio (relative to the 1%–4.99% density) rose slightly for Black densities of 5%–14.99%; beyond this, increases in Black density had little additional impact.
TABLE 2.
Effects of Ethnic Density on Birth Outcomes and Smoking During Pregnancy for Hispanic and Black Mothers, Adjusted for Parity, Maternal Age, Marital Status, Maternal Education, Maternal Nativity, and County-Level Median Income: US Linked Birth and Infant Death Data Set, 2000
| Black |
Hispanic |
|||
| OR (95% CI) | P | OR (95% CI) | P | |
| Mortality | ||||
| 0–0.99% (Ref) | 1.00 | 1.00 | ||
| 1–4.99% | 1.03 (0.67, 1.57) | .901 | 0.87 (0.68, 1.11) | .267 |
| 5–14.99% | 1.14 (0.76, 1.72) | .518 | 0.78 (0.61, 1.00) | .050 |
| 15–49.99% | 1.18 (0.79, 1.78) | .419 | 0.71 (0.55, 0.92) | .010 |
| ≥ 50% | 1.18 (0.77, 1.79) | .448 | 0.57 (0.42, 0.78) | <.001 |
| Low birthweight | ||||
| 0–0.99% (Ref) | 1.00 | 1.00 | ||
| 1–4.99% | 1.25 (1.08, 1.46) | .004 | 0.93 (0.85, 1.01) | .077 |
| 5–14.99% | 1.34 (1.16, 1.55) | <.001 | 0.91 (0.83, 0.99) | .036 |
| 15–49.99% | 1.38 (1.19, 1.59) | <.001 | 1.00 (0.91, 1.10) | .948 |
| ≥ 50% | 1.35 (1.16, 1.57) | <.001 | 0.96 (0.84, 1.10) | .590 |
| Preterm birth | ||||
| 0–0.99% (Ref) | 1.00 | 1.00 | ||
| 1–4.99% | 1.26 (1.09, 1.44) | .001 | 0.98 (0.92, 1.05) | .628 |
| 5–14.99% | 1.31 (1.15, 1.49) | <.001 | 1.01 (0.95, 1.09) | .690 |
| 15–49.99% | 1.38 (1.21, 1.58) | <.001 | 1.07 (1.00, 1.16) | .066 |
| ≥ 50% | 1.37 (1.19, 1.57) | <.001 | 1.08 (0.97, 1.20) | .162 |
| Smoking during pregnancy | ||||
| 0–0.99% (Ref) | 1.00 | 1.00 | ||
| 1–4.99% | 0.65 (0.54, 0.78) | <.001 | 0.60 (0.53, 0.68) | <.001 |
| 5–14.99% | 0.35 (0.29, 0.41) | <.001 | 0.39 (0.33, 0.46) | <.001 |
| 15–49.99% | 0.19 (0.16, 0.23) | <.001 | 0.35 (0.28, 0.42) | <.001 |
| ≥ 50% | 0.12 (0.10, 0.16) | <.001 | 0.11 (0.07, 0.17) | <.001 |
Notes. CI = confidence interval; OR = odds ratio.
FIGURE 1.
Odds of low birthweight and preterm delivery in Black mothers, by ethnic density: US Linked Birth and Infant Death Data Set, 2000.
The pattern for preterm delivery was similar to that of LBW (Figure 1 and Table 2). Again, the lowest odds of preterm delivery were for Black mothers living at Black densities of 0%–0.99%. Relative to the 0%–0.99% category, the greatest increase in odds of preterm delivery was for Black mothers living at Black densities of 1%–4.99%; there were additional small increases in odds ratios (relative to Black densities of 0%–0.99%) for preterm delivery for Black mothers living at Black densities of 5%–14.99% and 15%–49.99%. However, the odds ratio for mothers living at densities of 50% or more was very similar to that of the odds ratio for mothers living at densities of 15%–49.99%, suggesting that densities of greater than 50% have no additional impact compared with densities of 15%–49.99%.
The impact of Black ethnic density on smoking during pregnancy was very different from its impact on infant outcomes. There was a large reduction in the risk of smoking with a rise of ethnic density from the 0%–0.99% category to the 1%–4.99% category, with the risk of smoking continuing to fall with increasing density.
In contrast to the adverse effects of same-ethnic density for mortality, LBW, and preterm delivery among Black mothers, the effects of same-ethnic density for Hispanics were either protective or nonsignificant. For infant mortality, each increase in Hispanic density led to a decrease in risk. There was little evidence that ethnic density had any impact on LBW with the exception of a slight reduction in risk for the 5%–14.99% category. For preterm delivery there was a weak trend of increased risk at higher densities but this was not significant.
However, the association of same-ethnic density with smoking in pregnancy for Hispanics was comparable to the pattern seen for Black mothers. As ethnic density increased, the relative odds of smoking fell, and the risk of smoking continued to fall with increasing Hispanic density.
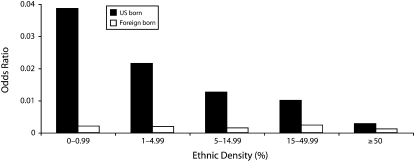
Among Hispanic mothers, we tested for cross-level interactions between county-level Hispanic density and individual-level maternal nativity in the prediction of smoking during pregnancy and infant mortality. There was little evidence of an interaction in relation to infant mortality. A random slope model for maternal nativity did not significantly improve model fit (P = .682). However, there was evidence that the effects of maternal nativity on smoking varied across counties. Inclusion of a random slope for maternal nativity significantly improved (P < .001) model fit. The effects of ethnic density on smoking during pregnancy by maternal nativity is presented in Figure 2. Hispanic mothers born in the United States and living at Hispanic densities of 0% to 0.99% had the highest odds of smoking during pregnancy and the odds fell with increasing ethnic density. In contrast, Hispanic mothers born outside the United States were generally much less likely to smoke but received much lower additional benefit from increasing ethnic density.
FIGURE 2.
Odds of smoking during pregnancy in Hispanic mothers, by ethnic density and maternal nativity: US Linked Birth and Infant Death Data Set, 2000.
DISCUSSION
Among Black mothers, we found little evidence of an association between same-ethnic density and infant mortality. This association is consistent with the 1 previous US study that looked at ethnic density in cities,8 but is inconsistent with the findings of older, ecological studies.6,7 The discrepancy could be attributable to improvements in statistical methodology, or social and technological changes that have altered infant mortality rates, or it could be because the high-density areas in New York City that were studied in the 1950s included Harlem, which had high mortality rates for children aged younger than 4 years.31
Among Black mothers, higher ethnic density was associated with increased odds of both preterm delivery and LBW. For preterm delivery, this is consistent with some studies9,15,16 although others have found no such association after adjustment for individual and area-level characteristics.10,12,16 The evidence on ethnic density and LBW is more mixed.
One study in Chicago found that the risk of LBW was lower for infants born to African American mothers who were living in community areas with greater same-ethnic density compared with African American mothers living in areas with lower same-ethnic densities,13 partly supported by another Chicago-based study12 that found a nonsignificant trend toward higher birthweights for residents of census tracts with higher proportions of Black residents. Ellen,11 in contrast, found that same-ethnic density within large metropolitan areas was associated with increased risk of LBW after adjustment for area-level characteristics. Two other studies found no association between ethnic density and LBW among Black mothers.9,10 Both geographic scale and level of density may be important factors in determining whether ethnic density exerts any effect on maternal and infant health for Black mothers and, if so, in what direction.
Our findings in relation to both preterm delivery and LBW suggest that there is a plateau effect for ethnic density for African American mothers, with small initial increases in ethnic density having a relatively large negative impact on infant health outcomes; once that threshold is passed, increases in ethnic density have relatively little impact. Other studies of infant and maternal health have not investigated ethnic density in a manner that could examine a plateau effect. However, Reidpath30 found a similar phenomenon for adult mortality. When Reidpath measured ethnic density at state level, the mortality rate for Black people increased up to a density of 10%, after which the mortality rate leveled out. This may be an artifact of the scale at which we were able to measure ethnic density. Counties are relatively large areas and, when one considers local influences on racial and economic segregation, ethnic density is unlikely to be homogeneous across a county. Many counties with an average-low or medium ethnic density may have pockets of high ethnic density in which the majority of Black mothers within the county live.
Maternal Smoking
The results for maternal smoking are very different than those for LBW and preterm delivery. First, higher ethnic densities appear to protect against maternal smoking, and, second, this protection continues to increase with increasing densities. The protective effect of ethnic density on smoking during pregnancy is consistent with the study by Bell et al.10 Our study is unable to test mechanisms; however, we note that the only outcome for which Black ethnic density is protective is perhaps most directly determined by social norms.
For Hispanic mothers, Hispanic density is generally more beneficial (or in some cases less adverse) than ethnic density was for Black mothers. The associations between Hispanic density and LBW and preterm delivery are very modest, but we found much stronger evidence that Hispanic density is associated with factors that are protective against both infant mortality and smoking during pregnancy. The results for infant mortality are partially consistent with the results of Jenny et al.18 Although our study found no evidence that the impact of same-ethnic density on infant mortality varied by mothers' nativity, Jenny et al. found that ethnic density protected against infant mortality only for US-born mothers, and that the risk of infant mortality for Mexico-born mothers was similar at low and high ethnic densities.
The lack of evidence of associations between Hispanic density and LBW or preterm delivery suggests that the protective effects of Hispanic density for infant mortality are not attributable to processes that affect time of delivery or infant growth. It is unclear what these processes are. Cultural mechanisms would be more strongly supported if we had found that the effects of Hispanic density on infant mortality had been modified by maternal nativity. However, maternal nativity only modified the effects of Hispanic density on smoking during pregnancy.
Smoking during pregnancy among Hispanic mothers falls with increasing Hispanic density, but only among US-born mothers. This suggests that for non–US-born Hispanic mothers (who have very low rates of smoking in pregnancy), Hispanic ethnicity may be sufficient to protect against smoking, wherever they live, whereas for US-born Hispanic mothers, living in areas where social and cultural norms are more strongly arraigned against smoking in pregnancy matters.
Our study suggests that same-ethnic density, when measured at county level, represents different circumstances and processes depending on race/ethnicity and outcome. For Hispanic infant mortality and Black and Hispanic smoking during pregnancy, which are outcomes for which Hispanic and African American mothers have an advantage over White mothers in general,21,32 same-ethnic density represents protective processes. These processes become stronger in proportion to increasing ethnic density and may be attributed to living in Hispanic and African American communities, and there is evidence that smoking during pregnancy is heavily influenced by local norms.33,34 However, the shape of the relationship between same-ethnic density and LBW and preterm delivery for Black mothers would suggest that very different processes are involved that may be caused by residential segregation leading to poorer provision of antenatal care and other services.
Residential segregation has been defined as “the degree to which two or more groups live separately from one another, in different parts of the urban environment.”35(p282) In segregated areas, the politically and economically weaker groups generally have poorer access to service and markets, and as a consequence, segregation is strongly associated with concentrated levels of deprivation and lack of education and employment opportunities.3 For residential segregation to occur, the minority population has to be large enough for separate services and markets to develop. However, once a minority population is large enough that services are provided separately, an upper limit to the adverse effects of segregation may be reached. Thus, at the individual level, adverse same-ethnic density effects that are caused by segregation are unlikely to increase beyond the threshold required to establish segregated communities.
The lack of an adverse threshold effect of ethnic density for Hispanics may be attributable to how Hispanic neighborhoods are viewed. Once socioeconomic factors are controlled for, Hispanic density has little impact on residential preferences of White Americans, but Black density does36; thus, segregation on ethnic (as opposed to racial) grounds is likely to be less strong. In addition, Hispanics are more likely than their Black counterparts to prefer living in same-ethnic communities37; this may be either a cause or a consequence of Hispanic communities being a healthy environment. Additionally, the causes of deprivation in Hispanic and Black communities are different.38 High-density Hispanic communities tend to include a large proportion of new economic migrants who will not have had the opportunity to build up capital, and are likely to represent areas built on hope and aspiration. In contrast, Black communities are the product of a long history of racism and the embodiment of disadvantage.39
Strengths, Limitations, and Conclusions
One strength of this study is that it includes all US births to Black and Hispanic mothers, giving the power to examine effects on infant mortality, and to test interactions between nativity and ethnic density for Hispanic mothers. However, data available from vital records and the census are limited in scope, and we were unable to control for a full range of individual-level and county-level factors that might confound or mediate the effect of ethnic density on maternal and infant health. We were also unable to examine ethnic density at a lower geographic scale than counties. Whereas some smaller counties may feel and operate like a genuine community or neighborhood for residents, larger counties include numerous different communities. However, ethnic density has been shown to be associated with mortality for larger geographic units such as states30 and counties.40,41 and counties are genuine political and administrative units at which interventions can be targeted.
For Hispanic mothers, Hispanic ethnic density was associated with reduced risk of infant mortality and, for US-born Hispanic mothers, smoking during pregnancy. There was little evidence that Hispanic density was associated with either LBW or preterm delivery.
For Black mothers, increased Black ethnic density was associated with increased protection against smoking during pregnancy. There was also evidence that modest increases in ethnic density from the 0% to 0.99% category to the 1% to 4.99% category were associated with increased risk of LBW and preterm delivery; however, further increases in ethnic density had little additional impact.
Acknowledgments
This study was funded by the UK Medical Research Council (grant R1032101). K. E. Pickett is supported by a UK National Institutes of Health Research Career Scientist Award.
The authors thank the US National Center for Health Statistics for provision of the restricted-use data set, and Kathleen Kiernan and Karl Atkin for ongoing discussions about ethnic density and health.
Human Participant Protection
No protocol approval was needed for this study
References
- 1.Pickett KE, Pearl M. Multilevel analyses of neighbourhood socioeconomic context and health outcomes: a critical review. J Epidemiol Community Health 2001;55(2):111–112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Riva M, Gauvin L, Barnett TA. Toward the next generation of research into small area effects on health: a synthesis of multilevel investigations published since July 1998. J Epidemiol Community Health 2007;61(10):853–861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Williams DR, Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Rep 2001;116(5):404–416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Halpern D. Minorities and mental health. Soc Sci Med 1993;36(5):597–607 [DOI] [PubMed] [Google Scholar]
- 5.Pickett KE, Wilkinson RG. People like us: ethnic group density effects on health. Ethn Health 2008;13(4):321–334 [DOI] [PubMed] [Google Scholar]
- 6.Yankauer A., Jr The relationship of fetal and infant mortality to residential segregation: an inquiry into social epidemiology. Am Sociol Rev 1950;15:644–648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yankauer A, Allaway NC. The relation of indices of fetal and infant loss to residential segregation: a follow-up report. Am Sociol Rev 1958;23:573–578 [Google Scholar]
- 8.LaVeist TA. The political empowerment and health status of African-Americans: mapping a new territory. Am J Sociol 1992;97:1080–1095 [Google Scholar]
- 9.Baker AN, Hellerstedt WL. Residential racial concentration and birth outcomes by nativity: do neighbors matter? J Natl Med Assoc 2006;98(2):172–180 [PMC free article] [PubMed] [Google Scholar]
- 10.Bell JF, Zimmerman FJ, Almgren GR, Mayer JD, Huebner CE. Birth outcomes among urban African-American women: a multilevel analysis of the role of racial residential segregation. Soc Sci Med 2006;63(12):3030–3045 [DOI] [PubMed] [Google Scholar]
- 11.Ellen IG. Is segregation bad for your health? The case of low birthweight. Brookings-Wharton Papers on Urban Affairs; 2000:203–238 [Google Scholar]
- 12.Masi CM, Hawkley LC, Piotrowski ZH, Pickett KE. Neighborhood economic disadvantage, violent crime, group density, and pregnancy outcomes in a diverse, urban population. Soc Sci Med 2007;65(12):2440–2457 [DOI] [PubMed] [Google Scholar]
- 13.Roberts EM. Neighborhood social environments and the distribution of low birthweight in Chicago. Am J Public Health 1997;87(4):597–603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Reichman NE, Teitler JO, Hamilton ER. Effects of neighborhood racial composition on birthweight. Health Place 2009;15:784–791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mason SM, Messer LC, Laraia BA, Mendola P. Segregation and preterm birth: the effects of neighborhood racial composition in North Carolina. Health Place 2009;15(3):1–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pickett KE, Ahern JE, Selvin S, Abrams B. Neighborhood socioeconomic status, maternal race and preterm delivery a case-control study. Ann Epidemiol 2002;12(6):410–418 [DOI] [PubMed] [Google Scholar]
- 17.Bell JF, Zimmerman FJ, Mayer JD, Almgren GR, Huebner CE. Associations between residential segregation and smoking during pregnancy among urban African-American women. J Urban Health 2007;84(3):372–388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jenny AM, Schoendorf KC, Parker JD. The association between community context and mortality among Mexican-American infants. Ethn Dis 2001;11(4):722–731 [PubMed] [Google Scholar]
- 19.Franzini L, Ribble JC, Keddie AM. Understanding the Hispanic paradox. Ethn Dis 2001;11(3):496–518 [PubMed] [Google Scholar]
- 20.Acevedo-Garcia D, Soobader MJ, Berkman LF. The differential effect of foreign-born status on low birth weight by race/ethnicity and education. Pediatrics 2005;115(1):e20–e30 [DOI] [PubMed] [Google Scholar]
- 21.Hummer RA, Powers DA, Pullum SG, Gossman GL, Frisbie WP. Paradox found (again): infant mortality among the Mexican-origin population in the United States. Demography 2007;44(3):441–457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lara M, Gamboa C, Kahramanian MI, Morales LS, Hayes Bautista DE. Acculturation and Latino health in the United States: a review of the literature and its sociopolitical context. Annu Rev Public Health 2005;26:367–397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McGlade MS, Saha S, Dahlstrom ME. The Latina paradox: an opportunity for restructuring prenatal care delivery. Am J Public Health 2004;94(12):2062–2065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Page RL. Positive pregnancy outcomes in Mexican immigrants: what can we learn? J Obstet Gynecol Neonatal Nurs 2004;33(6):783–790 [DOI] [PubMed] [Google Scholar]
- 25.Perreira KM. Migration and health behaviour during pregnancy: immigrant women adopt poorer health behaviour after migration. BMJ 2008;336(7652):1027–1028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bethel JW, Schenker MB. Acculturation and smoking patterns among Hispanics: a review. Am J Prev Med 2005;29(2):143–148 [DOI] [PubMed] [Google Scholar]
- 27.National Center for Health Statistics Birth cohort linked birth/infant death data for 2000 with all counties identified data and documentation. NCHS CD-ROM Series 20, No. 18a, issued January 2004. Washingon, DC: US Department of Health and Human Services; 2000 [Google Scholar]
- 28.Census 2000 Summary File 3, Census of Population and Housing, National File Washington, DC: US Bureau of the Census; 2003 [Google Scholar]
- 29.Vital Statistics of the United States, 2000 Natality, Technical Appendix Vol I Hyattsville, MD: National Center for Health Statistics; 2002 [Google Scholar]
- 30.Reidpath DD. “Love thy neighbour”–it's good for your health: a study of racial homogeneity, mortality and social cohesion in the United States. Soc Sci Med 2003;57(2):253–261 [DOI] [PubMed] [Google Scholar]
- 31.McCord C, Freeman HP. Excess mortality in Harlem. N Engl J Med 1990;322(3):173–177 [DOI] [PubMed] [Google Scholar]
- 32.Barbeau EM, Krieger N, Soobader MJ. Working class matters: socioeconomic disadvantage, race/ethnicity, gender, and smoking in NHIS 2000. Am J Public Health 2004;94(2):269–278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pickett KE, Wakschlag LS, Rathouz PJ, Leventhal BL, Abrams B. The working-class context of pregnancy smoking. Health Place 2002;8(3):167–175 [DOI] [PubMed] [Google Scholar]
- 34.Sellström E, Arnoldsson G, Bremberg S, Hjern A. The neighbourhood they live in: does it matter to women's smoking habits during pregnancy? Health Place 2008;14(2):155–166 [DOI] [PubMed] [Google Scholar]
- 35.Massey DS, Denton NA. The dimensions of residential segregation. Soc Forces 1988;67:281–315 [Google Scholar]
- 36.Emerson MO, Chai KJ, Yancey G. Does race matter in residential segregation? Exploring the preferences of White Americans. Am Sociol Rev 2001;66(6):922–935 [Google Scholar]
- 37.Clark WA. Residential preferences and residential choices in a multiethnic context. Demography 1992;29(3):451–466 [PubMed] [Google Scholar]
- 38.Wahl AMG, Breckenridge RS, Gunkel SE. Latinos, residential segregation and spatial assimilation in micropolitan areas: exploring the American dilemma on a new frontier. Soc Sci Res 2007;36:995–1020 [Google Scholar]
- 39.Krieger N. Discrimination and health. : Berkman L, Kawachi I, Social Epidemiology. Oxford, England: Oxford University Press Inc; 2000:36–75 [Google Scholar]
- 40.Cooper GS, Yuan Z, Rimm AA. Racial disparity in the incidence and case-fatality of colorectal cancer: analysis of 329 United States counties. Cancer Epidemiol Biomarkers Prev 1997;6(4):283–285 [PubMed] [Google Scholar]
- 41.Blanchard TC, Cossman JS, Levin ML. Multiple meanings of minority concentration: incorporating contextual explanations into the analysis of individual-level US black mortality outcomes. Popul Res Policy Rev 2004;23(3):309–326 [Google Scholar]