Introduction
Impact of Hearing Loss on Speech Perception, Production, and Language of Children with Early-Onset Hearing Loss
Decreased auditory sensitivity manifested early in life can adversely affect the development of language, oral communication, cognition, and educational progress. Intervention, provided in a timely manner has been shown to mitigate some of the deleterious effects of early hearing loss (Yoshinaga-Itano, Sedey, Coutler, & Mehl, 1998; Kennedy et al., 2006; Moeller, 2000). Development of mature spoken communication depends on the capacity of the auditory channel to receive and transmit information to the central nervous system early during development. Inasmuch as spoken communication is learned primarily through the auditory modality, early-onset hearing loss will result in reduced ability to perceive and produce intelligible speech. Communication outcomes will be influenced by a number of factors including age at onset of hearing loss, age at and adequacy of intervention, degree of hearing loss, audiometric configuration, intervention program, and family and environmental influences.
The typically developing human cochlea is essentially mature at term birth, while auditory neural development, axonal, dendritic and synaptic maturation and myelination continue in the brainstem into very early childhood and in the cerebral cortex well into late childhood (Moore & Linthicum, 2007). Early development of the auditory system is dependent upon stimulation from a rich acoustic environment of relevant sound. As Moore & Linthicum point out “Perinatal infants, equipped with a mature inner ear and brainstem pathway but a relatively immature cortex, are active listeners and are particularly prone to listen to human speech sounds ” (pg 469).
Auditory system development, and particularly development of speech perception, is guided by access to relevant acoustic and linguistic information early in life (Kuhl, 2000). All theories of early development of speech perception rely on the infant’s capacity to perceive language (speech) in their environment from which they learn to extract relevant features with experience. At birth, hearing infants show a preference for listening to their own mother’s voice (DeCasper & Fifer, 1980), a skill that must be developed via in-utero exposure to the acoustic properties of that voice. By six months of age infants can distinguish speech sounds even when emitted by different talkers (Kuhl, 1979). Between six and nine months infants show distinct preference for listening to their native language (Jusczyk, Cutler, & Redanz, 1993) and the ability to distinguish phonemes that are not experienced in the child’s environment diminishes rapidly (Cheour-Luhtanen et al., 1995). Clearly, the auditory system of hearing infants is working to lay down the neural structure for processing of speech sounds very early in life and those abilities will diminish quickly when stimulation is absent. For a summary of evidence of the need for early stimulation see Sininger, Doyle, & Moore (1999).
This study seeks to evaluate the effects of auditory deprivation in early childhood on auditory-based communication skills including speech perception, speech production and spoken language skills. Recent studies have focused primarily on language outcome which is not necessarily an auditory skill. A critical period for language development has been suggested by studies of Yoshinaga-Itano et al. (1998) who found that infants with hearing loss who were identified prior to 6 months of age and who received early intervention soon after, developed language skills that were significantly superior to those children identified after 6 months of age. Two other studies have confirmed that language outcomes are enhanced by early intervention or access to early intervention. Moeller (2001) evaluated age of intervention as the predictor of language and Kennedy et al., (2006) compared language development in children born in periods of time with and without access to newborn hearing screening. Both of these studies evaluated language outcomes in school-aged children with a wide range of degree of hearing loss and both found that early access to intervention led to enhanced language skills in these children.
A few earlier studies have looked at more generalized outcome measures. White and White (1987) studied the relationships among age at intervention, hearing status of the family (deaf vs. hearing parents) and language outcomes on a group of young children with severe to profound deafness. Some of the children, primarily those born to deaf parents, were identified rather early considering that the study was performed prior to any type of routine hearing screening for infants. This study found a “consistently positive effect” of early intervention on language development in these children. Davis, Elfenbein, Schum, & Bentler (1986) studied children 5 to 18 years of age who exhibited mild to moderate hearing loss. They found that degree of loss had some relationship to speech perception as measured by the NU CHIPS but not to other outcome measures. They also concluded that age at intervention or fitting with amplification was not correlated with outcome in these children who were first fit with amplification between 3 and 9 years of age.
Levitt (1987) conducted a study of the interrelationships among measures performed on children with hearing loss. In one analysis, he used a multivariate regression approach to evaluate the effects of a variety of factors on two measures of communication: syntactic comprehension and speech intelligibility rating. He found that having deaf parents or being post-lingually deafened, and educational factors including mainstreaming or early special education were factors that explained much of the variance for syntactic comprehension. Factors explaining speech intelligibility were similar and included post-lingual deafness, mainstreaming, good high-frequency hearing and early special education.
Studies conducted in the 1980’s rarely include children who today would be considered to be identified “early”. If it is critical that intervention begin before 6 months of age as suggested by Yoshinaga-Itano and colleagues, it will be important to include children who are identified and receive intervention before that age in a study of the factors that should predict communication outcomes. However, some of the studies published after 2000 have not found that age at identification or intervention is associated with improved language outcomes. Wake, Poulakis, Hughes, Carey-Sargeant, & Richards (2005) evaluated language and related skills in a group of 7–8 year old children with hearing loss. In that study, degree of hearing loss was predictive of outcomes but overall, age at diagnosis was not. Nicholas & Geers (2006) measured spoken language skills in 3.5 year old children with cochlear implants. They found that hearing level as well as duration of implant use was predictive of outcome but age at fitting of amplification was not. Fitzpatrick, Durieux-Smith, Eriks-Brophy, Olds, & Gaines (2007) also did not confirm a predictive relationship between age at identification or intervention and language outcome in children with hearing loss. Again, hearing level was found to be an important predictor of language as was self-help skill, but no relationship could be established between language outcome (at 3–5 years of age) and age at intervention for children with hearing loss. Some of these studies have also looked at speech production ability but, again, not found a relationship between this outcome and early intervention (Kennedy et al., 2006; Wake, Poulakis, Hughes, Carey-Sargeant, & Rickards, 2005; Fitzpatrick, Durieux-Smith, Eriks-Brophy, Olds, & Gaines, 2007).
Blamey et al., (2001) studied the relationships among factors including speech perception, language, speech production and hearing loss with age (development of skills over time) in two groups of orally educated children, one using cochlear implants and the other using conventional ear-level amplification. This study did not specifically assess the relationship between age of intervention and outcome but the results did establish that speech perception ability was strongly related to language and speech production capacity. In addition, speech perception was significantly negatively correlated to degree of hearing loss, but no similar relationship was found between degree of loss with speech production or language.
Even studies conducted after 2000 may have suffered from having only small groups of children who were identified very early. In addition, most of the early-identified children were born to deaf parents or suffered greater degrees of deafness than later-identified children. Newborn hearing screening programs now identify infants with hearing loss of all degrees at early ages without such bias and studies performed today, in areas of where early identification and intervention is happening, may be expected to show considerably different findings relative to early intervention due to the lack of subject bias.
The primary purpose of the current study was to determine the effects of age at auditory intervention (fitting of amplification) and degree of hearing loss on auditory-based outcomes including speech perception, speech production and spoken language. The hypothesis is that earlier fitting of amplification will enhance auditory skills over time but that skills will decrease with degree of hearing loss. Effects of other relevant factors such as intensity of educational intervention, parental sensitivity, home language and cochlear implant use are expected to contribute to the overall outcomes and will also be assessed.
This study was designed to investigate the relationships among factors believed to influence auditory-based outcomes and the actual measured outcomes in children with hearing loss. This was a prospective study that sought to answer questions by selecting and following children with a variety of degrees of hearing loss and a range of ages at intervention, who could provide evidence. The study was longitudinal; each subject was studied over a period of his/her life that was appropriate for answering the study questions. Finally, this was an observational study. No intervention was planned as part of the study. Rather, predictive factors and outcomes were observed and documented.
MATERIALS & METHODS
Experimental Sites/Recruitment Process
This study was conducted at three individual sites. The coordinating site was the division of Head & Neck Surgery, David Geffen School of Medicine at the University of California, Los Angeles and the Audiology and Speech Clinic of the UCLA Medical Center. Additional enrollment sites were the Children’s Auditory Research and Evaluation (CARE) Center of the House Ear Institute (HEI) and Providence Speech and Hearing Center (PSHC), Orange, California. The UCLA IRB governed oversight for enrollment and procedures at UCLA and Providence and the St. Vincent’s Medical Center IRB governed HEI. Some of the data collected for the study was extracted from Audiology clinical records in these facilities. Other direct measures including parent surveys, developmental scales, parent-child interaction measures and outcome measures were obtained in the laboratories at UCLA and HEI over the duration of the study.
Participants
Inclusion criteria for participants in the study were bilateral, congenital, sensorineural hearing loss sufficient to warrant fitting of amplification and parents or guardians who were willing to consent and cooperate with the study requirements. The study design concentrated on hearing loss and excluded participants with other conditions that could possibly influence perceptual or linguistic outcomes.
The following exclusion criteria were also applied to selection of participants.
Neonatal Factors: The effects of low birthweight and/or prematurity on overall development, health and cognitive status are often not realized for months or years. To avoid unforeseen consequences, participants with birthweight less than 1200 grams or gestational age of less than 30 weeks were excluded.
Cognitive Function: Participants of 9–14 months of age were initially evaluated for cognitive function using the Bayley Scales of Infant Development, Second Edition (Bayley, 1993). After three years of age, the Leiter International Performance Scale-Revised, Brief IQ was administered (Roid & Miller, 1997). Participants with a Mental Development Index (MDI) on the Bayley or an IQ score on the Leiter of less than 80 were excluded from the study.
Other Disabling Conditions: Any report or confirmed diagnosis of autism or autism spectrum disorder, or significant visual or motor impairment eliminated a child from consideration as a subject.
Auditory Neuropathy: Any indication of the condition of auditory neuropathy spectrum disorder such as present otoacoustic emission in combination with hearing loss greater than 40 dB and/or a cochlear microphonic component recorded in combination with no obvious auditory brainstem response excluded a child from participation. Children with auditory neuropathy are known to have speech perception that is poorer than seen in children with comparable degrees of sensory hearing loss and the auditory abilities of these children are often unpredictable and variable over time.
Late Onset Loss: Any clear indication of onset of hearing loss after 1 month of age, or medical condition associated with acquired hearing loss, for example meningitis, would eliminate a participant. Although it was not always certain, every attempt was made to find children with congenital hearing loss.
Participants were enrolled between 2002 and 2005. The outcome measures evaluating speech production, perception and language were appropriate for children at the age of three years and older. Each child participated in two or more formal assessments, conducted approximately 6 months apart.
Initially, sixty-four families consented to participate in the study. For a variety of reasons, twenty families did not or could not complete the study. Eleven families withdrew for personal reasons such as moving from the area, changing of audiology service provider or just an inability to commit time to the project. Four participants were withdrawn due to a late diagnosis of autism and four for diagnosis or other disabling conditions such as visual disorder or developmental delay. These conditions were not apparent until some time after initial subject enrollment and participants were eliminated from the study as the conditions became obvious. In one case the diagnosis of hearing loss was incorrect due to a transient conductive hearing loss. All participants are described in detail in the Appendix. Those in the final group included in the outcome study are indicated in the last column. The distribution of sex shows slightly more male participants than female with 33 males of 64 initial participants and 24 males of 44 in the final group. Participants were born between 1996 and 2004 with the largest group (20) born in 2002.
APPENDIX.
| Sex | Fit Age | Age CI | Right Degree | Left Degree | Hispanic/Latino | Race | SES | Final |
|---|---|---|---|---|---|---|---|---|
| M | 45.36 | Mild | Mild | No | White | 16 | X | |
| M | 32.86 | Mild | Mild | No | Black | 12 | ||
| M | 22.53 | Mild | Mild | No | Asian | 18 | X | |
| F | 8.09 | Mild | Mild | No | Asian | 16 | X | |
| M | 7.43 | Mild | Mild | Yes | Other | 16 | X | |
| F | 5.07 | Mild | Mild | No | White | 18 | X | |
| F | 24.97 | Mild | Mild | No | White | 18 | X | |
| M | 42.63 | Mild | Mild | No | White | 18 | X | |
| F | 4.77 | Mild | Mild | No | White | 16 | X | |
| M | 52.01 | Moderate | Mild | No | White | 18 | X | |
| M | 5.76 | Moderate | Mild | No | White | 14 | X | |
| F | 2.96 | Moderate | Mild | No | Asian | 16 | X | |
| M | 0.92 | Moderate | Moderate | No | White | 20 | X | |
| M | 2.04 | Moderate | Moderate | No | White | 20 | X | |
| M | 10.56 | Moderate | Moderate | Yes | White | 12 | ||
| M | 20.43 | Moderate | Moderate | Yes | Black | 16 | ||
| M | 5.66 | Moderate | Moderate | Yes | White | 12 | X | |
| M | 5.59 | Moderate | Moderate | No | white | 14 | X | |
| M | 72.83 | Moderate | Moderate | Yes | white | 9 | ||
| M | 2.34 | Moderate | Moderate | No | White | 13 | X | |
| M | 43.32 | Moderate | Moderate | Yes | Black | 12 | ||
| F | 33.85 | Moderate | Moderate | No | Black | |||
| M | 5.07 | Moderate | Moderate | No | White | 16 | X | |
| F | 60.56 | Moderate | Moderate | No | White | 17 | X | |
| M | 2.73 | Moderate | Moderate | No | White | 16 | X | |
| M | 5.56 | Moderate | Moderate | No | White | 12 | X | |
| F | 12.63 | Moderate | Moderate | Yes | White | 5 | X | |
| F | 33.19 | Moderate | Moderate | Yes | White | 14 | X | |
| M | 2.07 | Moderate | Moderate | No | White | 15.5 | X | |
| M | 4.41 | Severe | Mild | Yes | White | |||
| F | 3.36 | Severe | Moderate | No | White | 16 | X | |
| F | 10.46 | 18.68 | Severe | Moderate | No | White | 16 | X |
| F | 2.17 | Severe | Moderate | No | White | 19 | X | |
| F | 4.64 | Severe | Severe | No | White | 20 | X | |
| F | 14.44 | 21.88 | Severe | Severe | Yes | White | 14 | X |
| M | 38.89 | 50.89 | Severe | Severe | Yes | Other | 14 | |
| F | 10.36 | Severe | Severe | No | White | 18 | X | |
| F | 5.56 | Severe | Severe | No | Asian | 16 | ||
| F | 10.33 | Severe | Severe | No | Black | |||
| F | 5.59 | Severe | Severe | No | White | 18 | X | |
| M | 1.12 | Profound | Moderate | No | White | 18 | X | |
| F | 4.28 | Profound | Moderate | No | Asian | |||
| M | 21.32 | Profound | Moderate | No | White | |||
| M | 26.97 | 73.09 | Profound | Severe | Yes | White | 16 | X |
| M | 19.87 | 32.86 | Profound | Profound | Yes | White | 12 | X |
| F | 10.95 | 27.3 | Profound | Profound | Yes | White | 10 | |
| F | 14.34 | 32.96 | Profound | Profound | Yes | Other | 6 | X |
| F | 1.88 | Profound | Profound | No | White | 14 | ||
| M | 4.51 | 30.56 | Profound | Profound | Yes | White | 13 | X |
| F | 10.3 | Profound | Profound | Yes | Other | 12 | ||
| F | 1.55 | 34.01 | Profound | Profound | No | White | 16 | X |
| M | 1.61 | 12.76 | Profound | Profound | No | White | 18 | X |
| F | 29.14 | 63.68 | Profound | Profound | Yes | Other | 12 | X |
| F | 14.7 | 36.88 | Profound | Profound | No | Black | 12 | |
| M | 43.62 | 76.48 | Profound | Profound | Yes | Not Reported | 16 | X |
| M | 17.86 | 24.31 | Profound | Profound | Yes | White | 16 | X |
| M | 3.49 | 43.39 | Profound | Profound | No | White | 16 | X |
| F | 4.93 | 23.65 | Profound | Profound | Yes | Not Reported | 17 | X |
| F | 23.22 | 26.45 | Profound | Profound | No | Asian | 20 | X |
| M | 10.56 | 18.85 | Profound | Profound | No | White | 12 | X |
| F | 6.32 | Unknown | Unknown | Yes | White | |||
| M | 27.01 | Unknown | Unknown | No | White | |||
| F | 7.73 | Unknown | Unknown | No | White | |||
| F | 14.05 | Unknown | Unknown | Yes | White | 13 |
Summary of Participants in order of degree of hearing loss. Age Fit is the age in months at which the participant was first fitted with amplification. For those children who received cochlear implants, the age in months of the first implant is shown in column three. The average hearing level for 500, 1000 and 2000 is used to compute the degree of hearing loss with mild being 25–39 dB, moderate 40–69 dB, severe 70–89 dB and profound 90+ dB Hearing Level. SES (socio-economic status) is represented by the years of mother’s formal education. The final column indicates whether the participant’s data was used in the final analysis.
The families in the final group described the ethnicity of the participants as Hispanic/Latino in 13 cases and as non-Hispanic in 31. Race was described as Caucasian (White) in thirty-five cases, Asian in four, “Other” in three, and race was not declared for two children.
Clinical Management
Audiology Procedures and Amplification Fitting
This study was based on the premise that the children serving as participants were properly fit with amplification and carefully monitored by their clinical audiologists over time. Audiologists at the sites followed best-practices in fitting and verification of amplification (American Academy of Audiology, 2003). Children were fitted with appropriate analog or digital, bilateral, behind-the-ear amplification. Hearing aids were coupled to custom soft-shell earmolds, and were generally fitted with damped (filtered) ear hooks. Volume-control wheels or switches were either covered or de-activated through the fitting software.
Each clinic performed real-ear measures to aid in programming hearing aids to match the targets for gain and output to those prescribed by the Desired Sensation Level (DSL) method, specifically the DSL [i/o] version 4.1 hearing aid fitting software system (Seewald et al., 1997). The child’s real-ear to coupler difference (RECD) values were measured using the Audioscan Verifit RM500 real-ear system for each ear with custom earmolds when possible. When children would not cooperate for real ear measures, default RECD values, based on age normative data, were substituted. Further verification that hearing aids had achieved target output values was conducted with the hearing aids coupled to a standard HA-1 coupler in a test box/sound chamber. Hearing aids, ear hooks or earmolds were adjusted to achieve outputs as close as possible to targets.
Real ear adjusted measures of hearing aid output can be used to investigate the adequacy of the fitting of amplification and to compare fits across participants. Specifically, evaluation of the level of an amplified speech or speech-like signal over time relative to hearing thresholds can be used to calculate the speech intelligibility index or SII. The SII, ranging from 0 to 100 is an index of the audibility of the amplified speech signal or the proportion of the long term aided speech spectrum that is above threshold. SII has been shown to be predictive of aided speech intelligibility in school-aged children (Davidson & Skinner, 2006). The aided SII was automatically calculated by the Audioscan per ANSI S3.5 – 1997 for each aided measure.
Cochlear Implants
Sixteen of the final 44 participants received cochlear implants during the study, ten in the right ear only, two in the left ear and four were bilaterally fit. The median age of the first implant for this group was 28.5 months with a range of 12.78 to 76.48 months.
Participant-Related Measures: Predictor Variables
1) Age at Fitting of Amplification. The first primary outcome predictor was the age at which personal amplification was first fitted to the subject. This variable was chosen to represent the earliest age at which a consistent representation of the child’s acoustic surroundings, including speech, could be audible. The first day on which the family was given hearing aids and custom earmolds to use at home was considered the “date of first fit” and the “age at fit” was computed as the child’s age on this date.
2) Degree of Hearing Loss. The second primary factor evaluated in predicting outcomes for children with hearing loss was the severity or degree of loss. This study sought to evaluate auditory development in children with all degrees of hearing loss. Audiometric data were extracted from clinical records. Initial enrollment of subjects was often based on audiograms predicted by electrophysiologic measures such as Auditory Brainstem Response or Auditory Steady State Responses to frequency specific stimuli. The final audiometric data were based on standard clinical audiograms.
Other Participant-Related (Predictor) Variables Included in Regression Analysis
-
3) The effectiveness of parent-child interaction was evaluated using the Nursing Child Assessment Satellite Training (NCAST) Parent-Child Interaction Teaching Scale (Sumner & Spietz, 1994). This test provides a rating of caregiver-child interaction based on a set of observable behaviors that describe the communication dyad and interaction during a teaching situation. The teaching scales are appropriate for infants and toddlers from birth to thirty-six months of age. The kit includes a list of 30 skills or activities that are listed in developmental order. For example the first skill is holding onto a rattle, and later skills are squeaking a toy, scribbling on paper, turning the pages of a book and the most advanced skill is tying a shoelace. The parent chooses the first activity that the child does not yet know and attempts to teach the skill to the child. Appropriate props are available for the teaching situation.
The caregiver was allowed to set up the teaching situation and conduct the interaction, which generally lasted from 1 to 6 minutes in time. The caregiver was given minimal instructions, told to teach the activity and signal when finished regardless of the outcome. The session was videotaped for later analysis by a Registered Nurse who was specifically trained to score the test.
The interaction score was based on 73 observations that were grouped into the following categories: sensitivity to cues, response to distress, social-emotional growth fostering, cognitive growth fostering, clarity of cues, and responsiveness to caregiver. The last two categories relate to the child and the others to the caregiver.
4) The language of the home was documented by parent report. Parents were asked to indicate the primary and secondary languages spoken in the home. For analysis, the home language situation was classified as mono-lingual or multi-lingual depending on whether one or more than one language was used on a regular basis.
5) The nature and intensity of each subject’s intervention program was documented using a series of “Education Inventories” that were administered at six month intervals. The child’s interventionist, teacher or therapist filled out the inventories which were obtained for each distinct program in which the child was enrolled. Many participants were receiving therapy in a number of settings. The inventory documented the background and certification of the interventionist, the type of program (home-based, center-based, pre-school or classroom) as well as the total number of students in the program. The inventory documented the mode of communication used and the percentage of time devoted to manual, oral or combined communication. The number of hours per month that the child actually attended the program was documented and the family compliance with program goals was rated on a four-point scale.
For the purpose of data analysis, it was necessary to characterize the important characteristics of intervention in a single value. This value is termed “Annual Oral Training Scale” (AOTS). This process required that the nature and intensity of the intervention be incorporated over time, often from several programs. For each program, the total number of hours of intervention was calculated. For example, if a program was 10 hours a week for 24 weeks, the total was 240 hours. The hours were weighted by mode of communication, which was reported on the inventory. The weightings were derived from an adaptation of the scale developed by Geers (2002). This study used a communication mode scale from 1 to 4 while Geers’ scale is from 1–6. In the current scale, a rating of 1 indicated that communication was mostly sign (oral < sign), a rating of 2 indicated communication was balanced between oral and manual (oral = sign), a rating of 3 signifies that communication had a speech emphasis (oral > sign) and a rating of 4 indicates that communication was 100% oral (no signing). In the example above, if a speech emphasis with some signs was used, the program 240 hours would be scaled by 3 for a value of 720. In this way, oral education is weighted higher than manual. If a manual communication mode was primary in this case, the program would have been rated as 240. This emphasis was not meant to judge the value of communication mode, rather to be in line with the goals of the project to study “auditory” development which would be most enhanced with spoken or auditory input.
Finally the scores were annualized. Because children were enrolled for different periods of time, we computed an average year for all children. If the duration of evaluation was six months the value was doubled, if it were two years it was halved. In this way, we could compare the intensity of oral education across participants regardless of the duration of their enrollment in the study.
Other Subject Variables Not Included in Regression Analysis
Only those variables that might be expected to contribute to the development of the measured outcomes were used in the final data analysis. However, for a variety of reasons, some candidate variables were not used as predictors of performance. These are described below.
Subject selection criteria stipulated that cognitive functioning was to be within the normal range. As described under subject selection, the Bayley Scales of Infant Development were administered to the infants and the Leiter-R International Performance Scale Brief I.Q. was administered to the toddlers. The Leiter-R is a nonverbal measure of intelligence often employed to evaluate participants with hearing or speech impairment or autism. Scores on the Bayley Developmental Indices ranged from 74 to 118 with a median of 94, mean of 96.21 and a standard deviation of 11.69. The scores on the Leiter international ranged from 80 to 143 with a median of 119, mean of 114.11 and a standard deviation of 15.95. The data indicate that the participants in this study demonstrated cognitive development that was within normal limits on a non-verbal instrument. Consequently, no further use was made of intelligence quotients in analysis of outcome data and results of this study can only be generalized to populations with typical cognitive development.
It is noteworthy that although the Leiter scores are normally distributed, the mean is significantly above 100 (t= 5.017, p<0.0001). The Leiter test indicated consistently higher performance than the Bayley. In fourteen participants on whom both tests were administered, the mean difference is 24.57 points with a standard deviation of 13.55 which is significant at P < 0.0001 (t= 6.7842). Reasons for discrepancies are unclear but regardless of the apparent differences in the two measures, each indicated that performance of participants was in the normal range.
The socioeconomic status (SES) of the participants in this study was determined by parent report of the mother’s years of formal education (Yoshinaga-Itano et al., 1998). The mean SES of participants in the study was 15.63 years, median 16 years with a standard deviation of 3.19 years. Because of the small range of values represented for SES in this group, this factor was not suitable for use as a predictor variable. As with cognitive ability, the conclusions that can be drawn from the study of these participants will be limited to participants from reasonably high socioeconomic status and the effects of this variable on outcome cannot be evaluated.
Another factor used in some studies as a predictor of outcomes is the age at which intervention is initiated. This factor was evaluated and is discussed in some detail in a companion study (Sininger et al., 2009). Referral and enrollment in early intervention for children with hearing loss follows strict guidelines in California and is closely tied to the age at diagnosis and the age at fitting. Because the age at intervention is highly correlated to the age at fitting, only the age at fitting is used in the final regression analyses.
Family cooperation or involvement has been found to be a primary factor in prediction of outcome (Moeller, 2000). Educators of the children in this study were asked to evaluate the “level of compliance of the family with the program goals.” The possible ratings and their assigned values were Excellent (1), Good (2), Fair (3) and Poor (4). Subjects in the study had a mean compliance score of 1.28 with a standard deviation of 0.43 indicating consistently good to excellent compliance. Given the rigors and duration of study participation, it is reasonable to conclude that the families in our study were highly compliant. In fact, the compliance scores for the families who did not complete the study were found to be lower with a 2.06 mean score and standard deviation of 1.15. Because of the limited range of scores for the final participants, family compliance was not used as a predictive variable.
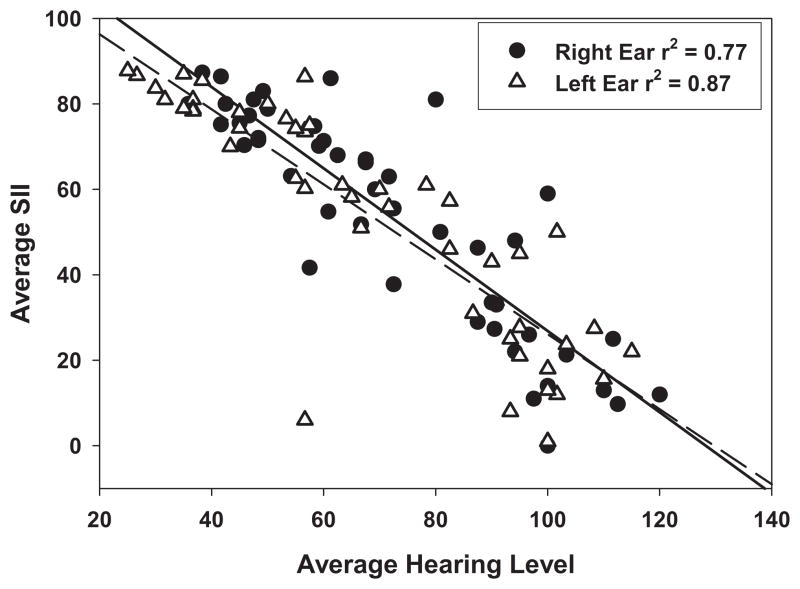
In the initial study design, the Speech Intelligibility Index (SII) was to be used as an indication of fitting adequacy and as a predictor variable for auditory performance. To determine the nature of the SII data gathered during the course of the study, a distribution of average SII values using either speech-shaped or DSL noise at 70 dB SPL was examined. The values ranged from 0 to 87.75. The SII values were normally distributed with means of 60.00 and 60.22 and standard deviations of 25.42 and 26.95 in the right and left ears respectively. Using SII as a predictor variable should have provided an individual predictor of the audibility of conversational level speech or the adequacy of the amplification fitting for each participant. However, preliminary investigation of candidate predictor variables included evaluating the interrelationships between variables to determine correlations in the predictors. This revealed a direct relationship between the degree of hearing loss and the average SII in individual ears across participants. Figure 1 shows that the SII and average hearing level are highly correlated. Consequently, the SII appears to add little or no additional information beyond the hearing levels and could be considered a proxy for the hearing information. For this reason, SII was not used as a “predictor variable” in the final multivariate regression modeling, although hearing level was used.
Figure 1.
The relationship between the average hearing level for 500, 1000 and 2000 Hz and the average Speech Intelligibility Index (SII) in each ear of individual participants. Regression lines are solid for the right ear and dashed for the left.
Outcome Measures
Children were evaluated on a series of outcome measures focused on speech perception, speech production and spoken language when they reached three years of age and then at intervals as close to six months as possible. Speech perception was measured using the Pediatric Speech Intelligibility Test (Jerger, Lewis, Hawkins, & Jerger, 1980) and the On-line Imitative Test of Speech Pattern Contrast Perception (Boothroyd, Eisenberg, & Martinez, 2005). Speech production was assessed using the Arizona Articulation Proficiency Scale-3 (Janet Barker Fudala, Ph.D. Western Psychological Services) and spoken language was evaluated using the Reynell Developmental Language Scales Receptive (Edwards et al., 1997). All outcome measures were administered with the children using their personal amplification. Although no specific validation of aided performance was used before testing, most children were evaluated on the day of an audiology visit. Testing was not conducted if amplification was missing or not working properly.
Speech perception tests were performed in a sound treated chamber. Audio information was delivered through an audiometer to a speaker or speakers in the test booth with presentation levels calibrated to 70 dB SPLA at the level of the child’s ear. Testing involved two research personnel, one delivering stimuli from outside and one in the booth to work with the child. Licensed speech-language pathologists administered both the Arizona-3 and the RDLS tests in a quiet, but not sound treated, area.
1) Pediatric Speech Intelligibility (PSI)
The PSI is a closed set test of word and sentence identification developed for children from 3 to 7 years of age. The child is asked to identify one of five color drawings after hearing a sentence or word. For example “A bear is brushing his teeth” would be used for sentence identification or “Show me frog” for word identification. The recorded message is presented in a free field from 0° azimuth at 70 dB SPLA.
A significant aspect of the PSI test is the assessment of the child’s ability to process linguistic stimuli in a competing message environment. The competing message is comprised of simple sentences presented from behind the child (180 ° azimuth). The addition of a competing message and the ability to vary the message-to-competition ratio (MCR) adds a significant level of complexity to the task and therefore to the ability of the PSI to provide insight into the child’s capacity for processing of speech stimuli in realistic environments.
The PSI materials were recorded digitally using a male talker for an earlier study (Eisenberg & Dirks, 1995). The same talker was used for both the target and competing stimuli. Preliminary data indicate that the original stimulus set and the re-recorded stimulus set used in this study produce comparable results for children with normal hearing and children with hearing loss, except that children with hearing loss were shown to be less accurate on the newer set of stimuli primarily at −10 dB MCR (Visser-Dumont, Martinez, Johnson, & Eisenberg, 2007). The picture sets were the originals developed by Susan Jerger and her colleagues. The child was first familiarized with the picture sets and instructed to indicate, by pointing, which of five pictures was named. Materials included four sets of pictures for words and two sets for sentences. Each test includes 10 items with each picture used twice. The test was performed in quiet and with MCRs of +10, 0 and −10 dB.
2) On-line Imitative Test of Speech Pattern Contrast Perception (OLIMSPAC)
This test is part of the Battery of Auditory Speech Perception Tests for Infants and Toddlers (BATIT) that originated in the Speech Pattern Contrast Test developed by Boothroyd (1984). It was designed to measure the child’s ability to hear and reproduce distinctions in phonemes based on a number of features or contrasts including vowel height and place and consonant features including voicing, manner and front or rear place. The OLIMSPAC is based on the principle that imitation is a natural skill for children and that children will be able to imitate features that they can perceive. The OLIMSPAC was developed for children of 3 years of age or older.
Test administration involves a presentation of a Vowel-Consonant-Vowel (VCV) nonsense syllable such as “ooboo” or “aataa” in either an audio-visual mode (video of a woman producing the utterance) or as an auditory signal alone (a drawing of a speaker is shown on the monitor). Tokens are routed through an audiometer to a loud speaker and video signals are routed directly to a computer monitor in the test booth. The child, seated in the booth facing the monitor, repeats the utterance into a microphone. The microphone signal is then routed to the tester outside the booth who, being masked to the original token presented, chooses the utterance that best approximates the VCV from a field of eight choices. Foils are selected to test for a number of contrasts. This method allows for assessment of multiple features simultaneously. For example, if the target stimulus is “oochoo” and the child’s utterance is judged as “ootoo” he would be given credit for vowel height and consonant manner but not for rear consonant place. The test score is based on percent correct with consideration for chance. Percent correct scores are produced for each of six categories (vowel height, vowel place, consonant voicing, consonant continuance, consonant place frontal, consonant place rear) as well as a composite score for both audio-visual and audio only modes of presentation. Each contrast is tested eight times per condition. Combinations of the vowels aa, oo and ee and consonants/d/ /t/ /b/ /p/ /sh/ and /ch/ were used as tokens.
3) Arizona Articulation Proficiency Scale-3
This test assesses production of all major speech sounds in the English language, including initial and final consonants and blends, vowels, and diphthongs. The child names an object depicted on picture cards. The test is administered by a speech-language pathologist who scores the child’s response according to simple quantitative rules. The test is normed on children from 1.5 to 18 years of age and scores are given in several formats including intelligibility descriptions, severity designations, percentile rankings and standardized scores (Z-scores, standard scores, and normal curve equivalents).
4) The Reynell Developmental Language Scales, Third Edition (RDLS)
The RDLS is a test of receptive and expressive language that is appropriate for ages from 15 months to 7 years of age. The two scales of the RDLS have been widely used both with normally hearing and children with hearing loss. The Comprehension Scale is organized into the following 10 sections: single words, relating two named objects, agents and actions, clausal constituents, attributes, noun phrases, locative relations, verbs and thematic role assignment, vocabulary and complex grammar. The Expressive Scale is organized into six sections: simple words, verbs/phrases, inflections (plurals, third person, past tense), clausal elements, auxiliaries (negatives, questions, tags), and complex structures (imitation, correction of errors, utterance completion). The RDLS uses toys, pictures and finger puppets, involving object manipulation and description based on questions that vary in length and grammatical complexity to elicit responses. Raw scores are converted to age equivalents and percentiles.
Test Intervals
The measures of outcome were taken on each child as close as possible to three years of age and then at approximately six months intervals. The number of assessments performed varied according to when the child was enrolled relative to the starting and ending of the study and how soon after enrollment the child passed the three-year age mark. Children enrolled as infants near the end of the enrollment period may have been eligible for only one or two assessments, whereas those enrolled near the age of three, early in the study, may have contributed 5 or 6 assessments. This is an unavoidable consequence of a prospective longitudinal study in which subjects are enrolled over time.
Data Management
All data were coded and entered into an Access database. Data were entered into two identical databases and compared at regular intervals to check for data entry errors. Data on individual tests were analyzed for distribution across participants and for time series in individual participants. For each of the final participants, data representing predictor variables and outcomes were extracted.
Modeling
Standard Least Squares Multiple Regression modeling was performed using JMP® Version 7.0 software from SAS. Models of the individual outcomes including the two speech perception test results, the speech production and receptive and expressive language results, all continuous variables, were fashioned using a linear combination of the predictor variables plus an error factor. The least squares modeling seeks to minimize the sum of the squared errors. Multiple linear regression analysis is a useful tool to cast light on the complex relationships between communication outcomes such as those described above in children with hearing loss and the subject or “predictor” factors. This modeling holds all other factors constant while evaluating the ability of individual ones to explain the variance in the outcome data. The procedure allowed simultaneous evaluation of the magnitude of effect or “leverage” of each factor in the prediction of an outcome and assigned a p-value to each. The significance of each factor is determined by comparing sum of the squared residual error with and without the contribution of the factor in question. If the error is reduced by the addition of a factor, then the factor is making a significant contribution to the model. Based on the weights of each factor in the model the influence of each was described. An F-ratio and corresponding p-value for the overall model were computed. The model itself was further evaluated by computing the R2 of modeled outcomes to actual outcomes.
All six predictors including age at fitting of amplification, average hearing level in the better ear, cochlear implant status, oral training, parent interaction and home language status were used in an initial analysis to determine the strongest factors. Cochlear implant and bilingual home were modeled as bivariate (yes-no) factors and all others as continuous variables. A second-stage modeling used only factors that had revealed p-values of <0.3 in the original model. The only exception to this was that all final models included age at fit and hearing level, as these were the primary factors to be evaluated.
RESULTS
PARTICIPANT-RELATED PREDICTORS
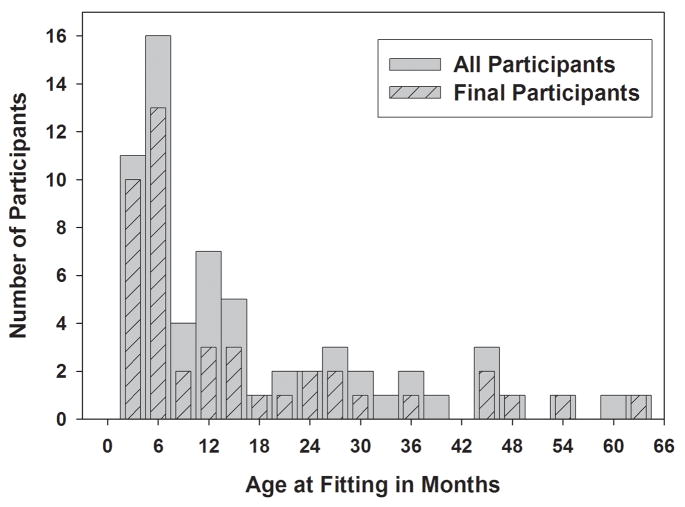
Age at Fitting
The distribution of the age at fitting of amplification for All Participants and Final Participants is shown in Figure 2. Comparison of the two distributions shows that the elimination of some participants did not change the shape of the original distribution. It is important to note that participants with early age of fitting of amplification are well represented. Twenty-three of the final subjects were fit before 6 months of age and 21 were fit after six months of age. Overall there was a good sampling of each with values ranging from less than one month to 72 months. Fifty percent of final participants were fit before 5.7 months of age.
Figure 2.
Distribution of the age at fitting of amplification for all participants (N=64, solid bars) and for the final participants (N=44, hatched bars) as described in the text. The emerging clear bars demonstrate that participants from the whole range of fitting categories were eliminated.
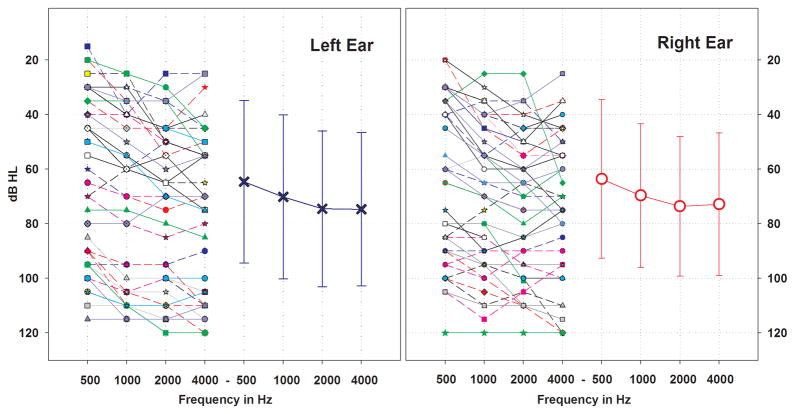
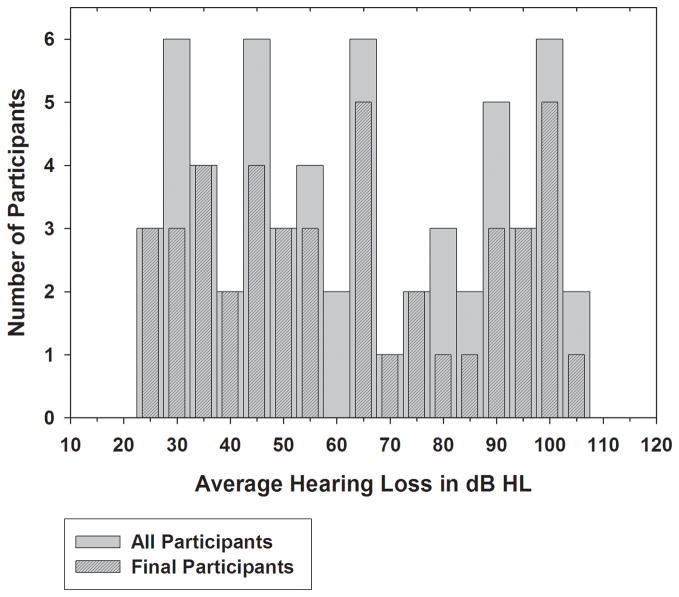
Degree of Hearing Loss
Figure 3 shows the individual audiograms for each participant as well as the mean audiograms for each ear. The distributions of average thresholds in the better ear for the initial sixty-four and final forty-four participants are shown in Figure 4. The degree of hearing loss was evenly distributed. The substantial representation of children with mild and moderate hearing loss is an important feature of this study. In addition, the distribution of degree of loss for those eliminated can be gleaned from the areas of solid bars that are visible. Participants eliminated from the study were evenly distributed with regard to degree of loss.
Figure 3.
Individual participant audiograms and average audiometric thresholds for octave frequencies from 500 to 4000 Hz in each ear. Error bars show one standard deviation. Symbols for both ears of each participant are matched.
Figure 4.
Distribution of pure tone average hearing loss in the better hearing ear based on thresholds for 500, 1000 and 2000 Hz for all participants (N=64, light bars) and final participants (N=44 dark bars). Range of hearing loss for both groups is 25 to 108.33 dB HL. The areas of light bars that are revealed represent those participants that were eliminated.
The configuration of the audiograms for final participants in this study was essentially flat. The slope of the hearing loss was computed as the difference between the threshold at 4000 Hz and that at 500 Hz (three octaves). The median slope for each ear was 10 dB and the mean/standard deviation was 10.48/12.21 dB for the right and 11.02/11.49 dB for the left. This computes to less than 4 dB/octave. Slopes ranged from 5 to +13.33 dB/octave. Two participants had audiograms with a per-octave slope of 10 dB or more.
The average hearing loss was computed using 500, 1000 and 2000 Hz. The importance of auditory sensitivity for 4000 Hz is well recognized (Stelmachowicz, Pittmann, Hoover, Lewis, & Moeller, 2004). However, as shown in Figure 3, the degree of loss for 2000 Hz and 4000 Hz was essentially identical. Degree of loss computed with 4000 rather than 2000 Hz resulted in an average, per subject difference of less than 1 dB with a standard deviation of less than 4 dB. Moeller et al (2007) also used 500, 1000 and 2000 Hz to compute average hearing loss in a similar group of subjects, i.e. children with early onset hearing loss, generally flat in configuration.
Hearing losses were also primarily symmetrical. The median difference in average hearing loss between ears was 5 dB, the seventy-fifth percentile was 11.87 dB and only three participants showed an asymmetry in hearing level greater than 30 dB. All subsequent analyses using degree of hearing loss utilized the average loss in dB in the better hearing ear.
Hearing Loss by Age at Fit
Table 1 gives the breakdown of degree of hearing loss by age at fitting categories for the final participants. The Chi Square likelihood ratio for this data is 6.402 (6 degrees of freedom, p=0.370) indicating no interaction between age at fit and degree of loss.
Table 1.
Breakdown of final subjects by age at fitting of amplification and degree of hearing loss.
| Age at Fit Category | |||||
|---|---|---|---|---|---|
| Hearing Category | 0–6 Months | 6–12 Months | 12–24 Months | [mt]24 Months | Total |
| Mild (25–45 dB) | 7 | 2 | 1 | 4 | 14 |
| Moderate (46–75 dB) | 10 | 2 | 1 | 2 | 15 |
| Sev-Profound (76+ dB) | 6 | 1 | 5 | 3 | 15 |
| Total | 23 | 5 | 7 | 9 | 44 |
Parent Child Interaction
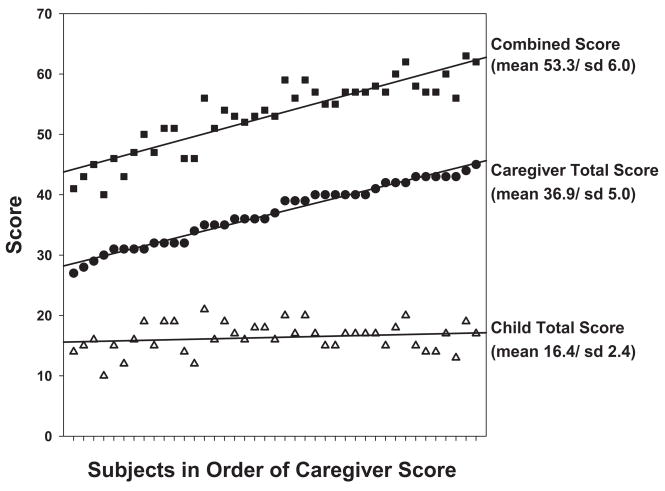
Data were available on the NCAST for 41 of the 44 final participants. Three of the participants were too old for the administration of the test at enrollment. The summary data are plotted on Figure 5 for each subject in order of the score of the caregiver. The mean and standard deviation of each sub-score on the right, demonstrate that the larger variance is found across the caregivers while the child scores are tightly grouped. The standard deviation of the combined score is dominated by the caregiver score and primarily reflects the differences in scores across the parents. For this reason, the caregiver score was used in the final analyses as the score best suited to predicting the variance in outcomes.
Figure 5.
NCAST scores (parent-child interaction) are plotted for all participants in the order of the score of the caregiver. The combined scores is the addition of the child and caregiver scores. The mean and standard deviations of the three scores are shown on the right.
Language in the Home
In the final group of 44 participants, English was the primary language in 40 cases and Spanish in four. Fourteen families were bilingual with second languages of Spanish in five, ASL in three, English in two and Chinese, Tagalog, Urdu and Farsi in one of each. In the final analysis the home language situation, monolingual vs. bilingual was used in the model to predict outcomes. None of the parents or guardians of the children in the study were deaf or hard of hearing.
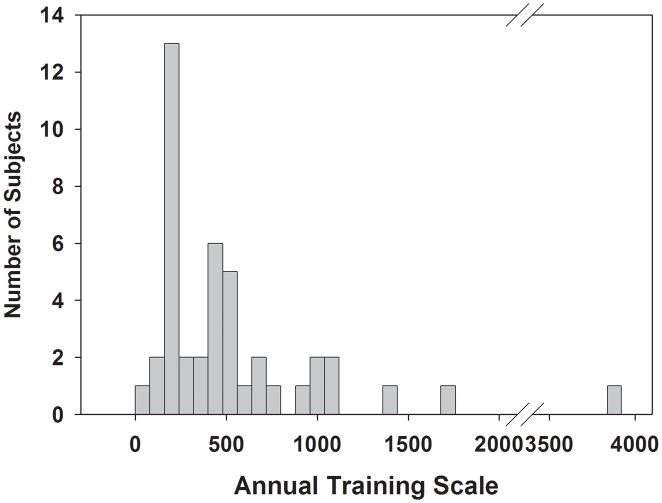
Education
The distribution of annual oral training scale values is found on Figure 6. The scores show a large variation ranged from 31.7 to 3840. The mean score is 555.90, the median is 417.4 and the standard deviation is 630.06.
Figure 6.
Distribution of Annual Oral Training Scale (see text) for final participants.
RAW OUTCOME MEASURE RESULTS
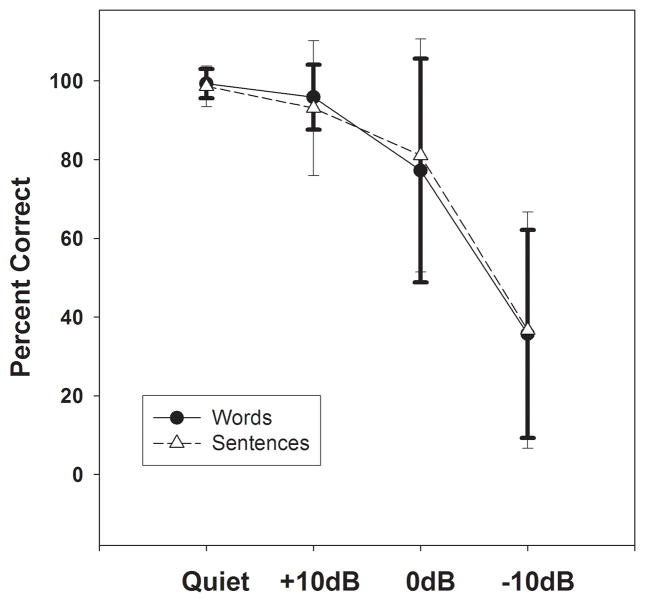
PSI
Figure 7 shows the average results from the participants’ final test for both the words and sentence subtests in quiet and the three MCRs. Both the quiet and +10 dB MCR conditions show very good performance for all subjects which reflects the ease of the test in those conditions but also indicates that the language level of the items was appropriate for the subjects of the study. The mean and standard deviations of the responses for both sentences and words show two important features of these test results. First, the mean scores for the 0 and −10 dB MCRs were well below 100%, thus avoiding ceiling effects. Second the standard deviations of these scores were quite high demonstrating that these PSI measures are able to differentiate between good and poor performers among the subjects. For these reasons, the average of the predicted age at 100% for the 0 and −10 dB MCR conditions for both sentences and words was chosen as the outcome measure for the PSI test.
Figure 7.
Group mean final scores for the four message-to-competition ratios (MCRs) on the Pediatric Speech Intelligibility Test. Results for words are shown with closed circles and sentences are shown with open triangles. Error bars indicate 1 standard deviation.
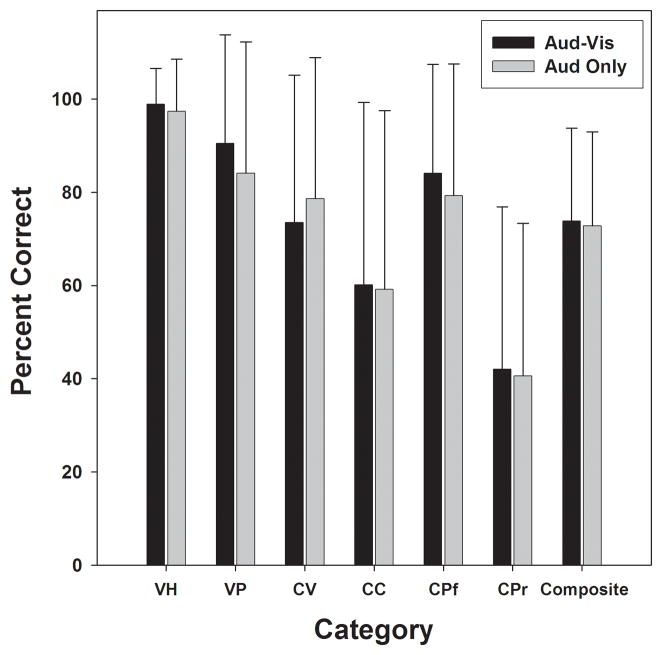
OLIMSPAC
Mean results of participants’ final tests on the OLIMSPAC, broken down by subtests and composite score, are shown on Figure 8. Overall, the subjects performed quite well in identifying vowels but had more difficulty with consonant perception, particularly with consonant continuance and with perception of consonant place in the rear of the mouth. The composite score was chosen for use in the final analysis because it gives a representation of the test results overall but does not suffer from ceiling effects. The audio-only mode composite score was chosen because of the study focus on auditory skills.
Figure 8.
Group mean final test results on the OLIMSPAC. Subtests include vowel height (VH), vowel place (VP), consonant voicing (CV), consonant continuance (CC), consonant place frontal (CPf), consonant place rear (CPr) as well as a composite score for both audio-visual and audio-only modes of presentation.
Arizona 3
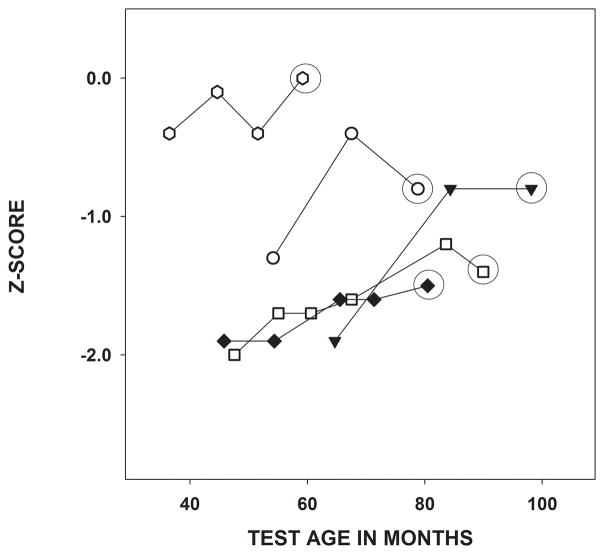
Results of the Arizona-test of speech production are expressed as a Z-scores based on the distribution of scores for age-matched, typically performing peers. The distribution is normalized to mean 0 and standard deviation of 1. Therefore, a score of −1 would indicate speech production performance was one standard deviation below normal. Each subject’s Z-scores were plotted by age at test. Examples of scores over time from 5 randomly selected subjects are found in Figure 9. A summary of group statistics on all outcome measures is provided in Table 2.
Figure 9.
Examples of Z-scores on the Arizona over time for four representative subjects. The final score (circled) was used to represent performance for that subject in the modeling.
Table 2.
Group descriptive statistics for all final outcome measures.
| Outcome Test | Measure | Mean | s.d. | Median | 90th % | 10th % |
|---|---|---|---|---|---|---|
| OLIMSPAC | Age in months at 100% Composite Score | 72.09 | 16.70 | 67.93 | 95.00 | 52.88 |
| PSI | Age at 100% Average Wds & Sent, 0 & −10 MCR | 72.58 | 24.73 | 66.62 | 106.93 | 41.34 |
| Arizona-3 | Age-Normalized Z score | −0.081 | −0.91 | −0.80 | 0.40 | −2.00 |
| Reynell Receptive | Language Age in months re typical peers | −12.59 | 16.38 | −9.00 | 5.60 | −41.20 |
| Reynell Expressive | Language Age in months re typical peers | −12.56 | 16.98 | −9.00 | 5.00 | −44.40 |
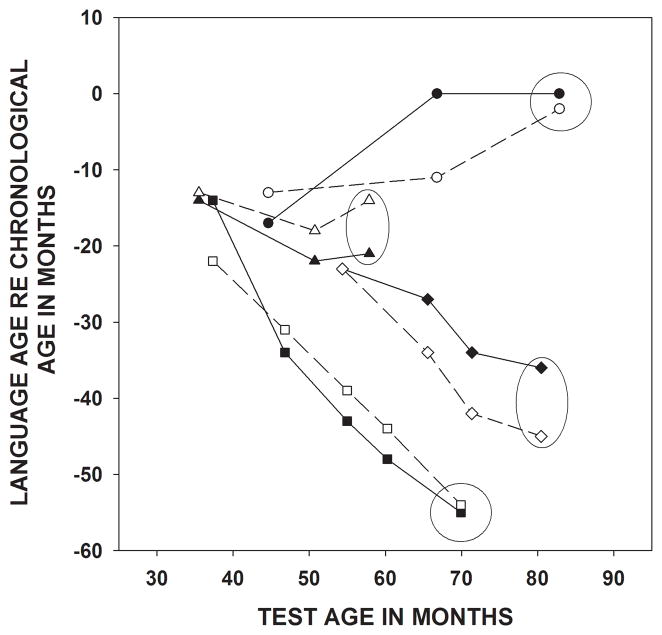
Reynell
For the RDLS the expressive or receptive language ability of each child was expressed in performance age in months relative to age-matched peers. A score of −3, for example, indicates that the child was performing three months below typically performing peers. Examples of expressive and receptive language ages relative to chronological age over time from four representative participants are shown on Figure 10 and the final score summary for the group is provided on Table 2.
Figure 10.
Examples of language age relative to chronological age on the RDLS over time from four typical participants. For each subject expressive language is indicated by the open symbols and receptive by filled symbols. The final scores (circled) were used to represent performance for that subject in the modeling.
Characterizing Outcomes
Both the RDLS and the Arizona-3 provide normative data based on age. Each child’s outcome for these tests can be characterized by where they fall on the distribution of scores for children their own age. The final test score obtained on each of these measures, circled on examples in Figures 9 and 10, were used to characterize each participants’ performance for the regression analysis.
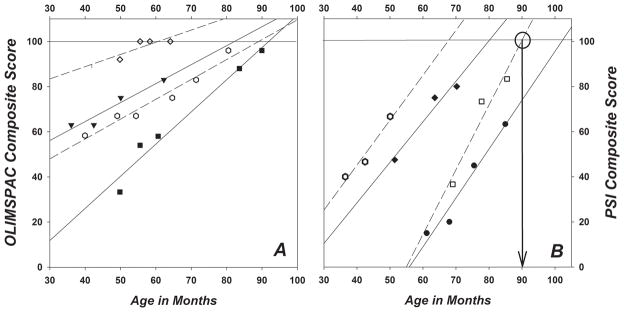
Characterizing performance over time for tests without age-based normative data is more complicated. One possibility was to look at the rate of growth of performance over time. Inspection of the growth data however revealed several flaws in this approach. The high performing child who approaches maximum performance at the time of initial testing demonstrates an obvious flaw with this approach. For this child, the growth of performance would be shallow because of ceiling effects. Another problem with using performance growth functions is an emphasis on slope of growth but not on overall performance level. For example, two children could show equal growth over time but at different points on the performance scale.
The measure used to describe overall performance must take into account testing of subjects at different ages and incorporate both the growth of performance over time as well as level of performance. The measure devised for this purpose was the age at which each subject would reach a specified degree of performance. This age was determined based on a regression line derived from actual performance over time. Regardless of the ages at which the child was tested, as long as performance was increasing over time, the age at which the criterion performance should be reached can be determined. This technique has several advantages. First, this measure has no ceiling effect. Second, this technique allows for characterization of performance over time when subjects were tested at a variety of different ages and intervals. Typical examples of the growth functions from a few subjects illustrating how age at 100% was calculated for both OLIMSPAC and PSI are found on Figure 11. The linearity of the age by score growth functions for both measures is demonstrated by the linear function fits (r2). From this random selection of subjects, for example, OLIMSPAC functions demonstrate r2 ranging from 0.64 to 0.96 with a mean of 0.87 and r2 for PSI functions range from 0.92 to 0.96 with a mean of 0.95.
Figure 11.
Examples of growth functions from individual subjects for OLIMPAC (A on left) and PSI (B on right) composite scores. Each symbol indicates a different subject and linear regression lines representing open symbols are dashed and closed symbol regression lines are solid. Like symbols for the two graphs do not indicate data from the same subjects. The linear nature of the growth of these functions is clear from the excellent fit to regression lines (see text). The computation of the final outcome for each subject is illustrated by the open squares subject on PSI. This subject would reach 100% at 90 months of age based on the regression and this value was used as the outcome for that subject.
For both the PSI and OLIMSPAC the linear regression equation for performance growth on each subject for this measure was computed and used to calculate the age at which 100% would be reached. If however, the subject reached 100% on any test session, the age at that test session was substituted for the predicted age. In no case did the predicted and actual differ by a substantial amount.
A summary of the results of the extracted outcome measures on all 44 subjects is found on Table 2. As might be expected, results of those tests with normative data revealed that children with hearing loss performed significantly below age-matched, hearing peers. Specifically, the Arizona test of speech production showed that, on average children with hearing loss were almost one standard deviation below normal performance and the RDLS test of language showed an average delay of just over one year. The measures of speech perception were without age-matched norms, but show some internal consistency, with both predicting 100% performance at just over 72 months of age. On all tests, however, the variability across subjects was quite high as might be expected.
Relationships among outcomes
The chosen auditory based outcomes cannot be expected to be independent of each other. Correlations among outcomes was investigated and can be found in correlation matrix form in Table 3. Speech feature perception as measured on the OLIMSPAC showed a mild relationship to both speech production and to receptive language but a strong relationship with expressive language. In addition, speech production as measured on the Arizona-3 showed very strong relationships with both expressive and receptive language. Finally, expressive and receptive language showed very high correlation, as might be expected.
Table 3.
Correlations (r2) among outcome variables.
| PSI | OLIMSPAC | ARIZONA | REY EXP | REY REC | |
|---|---|---|---|---|---|
| PSI | 1.00 | 0.034 | 0.017 | 0.025 | 0.003 |
| OLIMSPAC | 1.00 | 0.221* | 0.305** | 0.190* | |
| ARIZONA | 1.00 | 0.456*** | 0.637*** | ||
| REY EXP | 1.00 | 0.593*** | |||
| REY REC | 1.00 |
= <0.05
=<0.01
=<0.001
Multivariate Least Squares Regression Modeling: Results by Outcome
The results of each of the five outcome measures described above were modeled based on the participant related factors. Results of the modeling are summarized on Table 4. Predictors are listed in order of overall contribution to the model. Each modeled effect is also quantified.
Table 4.
Results of Multiple Linear Regression modeling of each outcome measure. Evaluation of the overall model includes the R2 between modeled and actual outcomes as well as the F-ratio and P-value from an analysis of variance. Modeling procedure is described in the text. The significance (p) of each factor in the model and the interpretation of the factor contribution based on the weighting of the factor in the model are provided.
| Overall Model | Individual Factors | |||||
|---|---|---|---|---|---|---|
| Outcome Measure | R2 | F-Ratio | P | Factor | p | Effect/Interpretation |
|
OLIMSPAC (Speech- Perception) Age to reach 100% |
0.56 | 5.00 | 0.0083 | 1) Age at Fit | <0.01 | Each mo delay in fitting relates to 0.77 mo increased age at outcome |
| 2) Parent Interaction | 0.08 | Each NCAST point relates to time to outcome reduced by 1.21 mo | ||||
| 3) Auditory Training | 0.22 | Each 100 hrs of training relates to time to outcome reduced 1.06 mo | ||||
| 4) Hearing Level | 0.43 | N/A | ||||
|
Pediatric Speech Intelligibility (Speech-Perception) Age to reach 100% |
0.50 | 5.67 | 0.0025 | 1) Age at Fit | <0.01 | Each mo delay in fitting relates to 0.75 mo increased age at outcome |
| 2) Cochlear Implant | 0.09 | Having a CI relates to increased time to outcome by 28.93 months | ||||
| 3) Multi-lingual Home | 0.18 | Multi-lingual home relates to 10.36 months earlier outcome | ||||
| 4) Hearing Level | 0.40 | N/A | ||||
|
Arizona III (Speech Production) Age Adjusted Z Score |
0.36 | 7.11 | 0.0007 | 1) Hearing Level | <0.01 | Each 10 dB of loss relates to reduced Z Score 0.29 points |
| 3) Age at Fit | 0.05 | Each mo delay in fitting relates to 0.02 points lower Z score | ||||
| 2) Cochlear Implant | 0.11 | Having a CI relates to improved Z score of .64 | ||||
|
Reynell Expressive (Language) Lang Age re peers |
0.27 | 4.66 | 0.0073 | 1) Hearing Level | <0.01 | Every 10 dB of loss relates to language age lag of 5.2 months |
| 2) Cochlear Implant | 0.04 | Having a CI relates to improved language age by 17.7 months | ||||
| 3) Age at Fit | 0.05 | Each mo delay in fit relates to 0.30 months lag in language age | ||||
|
Reynell Receptive (Language) Lang Age re peers |
0.47 | 10.76 | <.0001 | 1) Hearing Level | <0.01 | Every 10 dB of Hearing Loss relates to lang age lag of 5.9 mo |
| 2) Cochlear Implant | 0.09 | Having a CI relates to improved language age by 12 months | ||||
| 3) Age at Fit | 0.18 | Each mo delay in fit relates to 0.17 mo lag in language age | ||||
Speech Perception
The factor that was most important in predicting speech perception as measured by OLIMSPAC and PSI was the age at fitting of amplification. For both measures, every month of delay in fitting of amplification, related to an increase in the age at which they would reach the desired outcome by approximately ¾ of a month. Hearing level was fourth in the list of impact factors for both measures but in neither case was the hearing level highly correlated with outcome (P-values ≥ 0.4). For the OLIMSPAC, strong parent-child interaction was predictive of better outcome with each point on the NCAST relating to 1.2 months earlier achievement of outcome. Third in the list of predictive factors for the OLIMSPAC was intensity of oral education. This effect was weak, with every additional 100 hours of intervention related to one month earlier age at outcome.
Following age at fitting, the next most important predictor of PSI test outcome was whether the child was using a cochlear implant. This relationship however, was not in the expected direction; use of a cochlear implant was correlated with a 29-month delay in achieving maximum outcome on the PSI. Being from a multi-lingual home, however was correlated with a 10.36 month earlier outcome.
Speech Production
Speech, as measured by the Arizona-3, was best predicted by the degree of hearing loss. For every 10 dB of increase in the pure-tone average of the better hearing ear, the model predicted a drop of 1/3 Z-score (standard deviation). Age at fit was the next most important factor in prediction of performance with each month delay in age at fitting accounting for a drop of approximately 0.02 in Z-score. The third factor in the model was the use of a cochlear implant. In the case of speech production, a significant improvement in performance, .64 standard deviations in score, was predicted for children using a cochlear implant vs. those not implanted.
Spoken Language
As with speech production, hearing loss was the most important factor in the model predicting spoken language, both expressive and receptive as measured by the RDLS. The effect of hearing loss was very similar on both receptive and expressive language measures, receptive language showing that each 10 dB of additional hearing loss accounted for 5.9 months decrease in performance and expressive language showing each additional 10 dB accounted for 5.2 months of performance lag. The next factor in prediction of both language measures was cochlear implant use. Children with cochlear implants were predicted to show 12 months improvement in receptive language and almost 18 months improvement in expressive language compared to non-users. Age at fitting was predictive of both language measures with each month of lag in fitting attributing to a language lag of 0.17 months in receptive and 0.30 months in expressive language.
Results by Predictors
Age at fitting of amplification was an important factor in predicting every outcome measured and in each outcome, earlier fitting predicted improved performance. For the two measures of speech perception, the age at fit was by far the strongest predictor of performance. This gives clear indication that earlier fitting of amplification is associated with improved outcomes on all measures of auditory communication skills particularly for development of speech perception ability.
Figure 12 contains a leverage plot which represents the graphic display of an effect’s significance (Sall, 1990). The modeled effect of age at fitting of amplification on each of the outcomes is shown with solid line in the figure representing the modeled effect, the dashed enclosed area around the model representing the 95 confidence region and the dashed, horizontal line indicating the group mean value of the outcome parameter. The distance of each data point from the model line represents the residual error and the distance of each point from the mean (horizontal) represents the residual error without the effect of the model. The P-value represents the significance of the improvement in the overall error (fit) imparted by the model for that factor.
Figure 12.
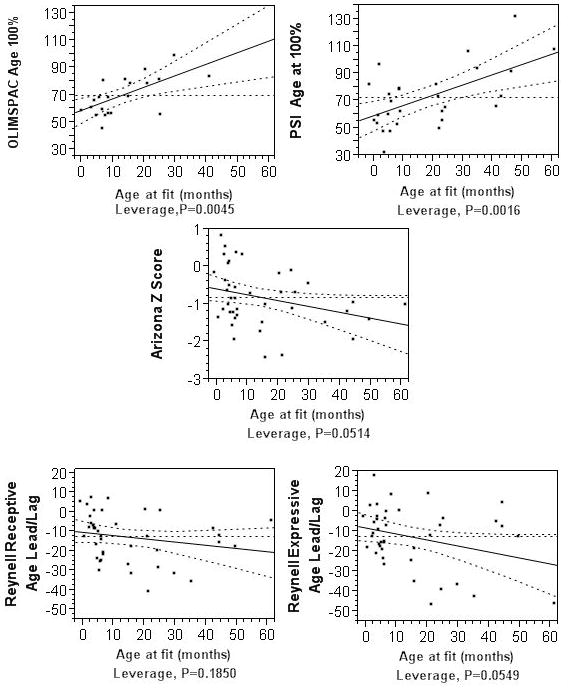
Leverage plots (Sall, 1990) of modeled linear relationships between each outcome and age at fitting of amplification. The solid lines indicate the modeled relationship, the dashed lines indicate the area within a .05 significance region and the horizontal dashed line is the group mean of the outcome measure.
One must note that there is a change in direction of the regressions for speech perception as compared to the production and language measures. For the speech perception measures, higher scores (age at maximum performance) is an indicator of poorer performance while higher scores on language and speech production indicated better performance.
An estimate of the effect of early fitting is quantified by the modeling procedure. This is actually the slope of the model line in the plots in Figure 12. For every month that hearing aid fitting is delayed the model predicts that outcomes on the OLIMSPAC and PSI are delayed by .75 and .77 months respectively and language age delays by 0.30 and 0.17 months for expressive and receptive skills. Each month of delay in fitting is predicted to reduce the Arizona-3 Z score by .02.
Hearing level as measured by the average audiometric thresholds in the better hearing ear was the top predictor of performance on speech production and on receptive and expressive language but did not play a significant role in predicting speech perception outcomes (P-values ≥ 0.4). The modeled linear predictions for speech production and language outcomes by level of hearing loss (leverage plots) are shown in Figure 13.
Figure 13.
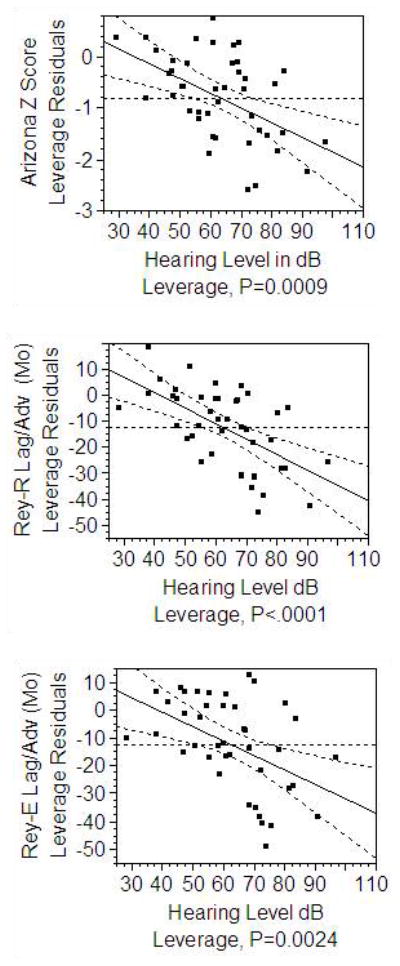
Leverage plots (Sall, 1990) for degree of hearing loss on language and speech production measures. Leverage of hearing loss for speech perception measures was not significant and is not shown. See Figure 12 legend.
Speech outcomes are reduced by 1/3 of a standard deviation for each 10 dB of additional hearing loss. Every additional 10 dB of average hearing loss is associated with delays of 5.9 months of receptive language and 5.2 months of expressive language.
Cochlear Implant use was a strong predictor of outcome on the Pediatric Speech Intelligibility test and for speech production and both receptive and expressive language. For both speech production and expressive and receptive language the CI was indicative of significantly improved outcomes. Having a CI was associated with an increase in speech production by 0.64 standard deviations, and with 12 months improvement in receptive and almost 18 months improvement in expressive language. In contrast, in the case of speech perception, the CI was not a significant factor in predicting the outcome on the OLIMSPAC and, use of a cochlear implant is associated with a delay to maximum outcome on the PSI.
The other predictive factors made relatively minor contributions to prediction of outcome as compared the first three. A multi-lingual home was predictive of improved outcome on speech perception as measured by the PSI but was not a factor in predicting performance on the other measure of speech perception, the OLIMSPAC. Both high parental interaction scores and increased hours of auditory training had small positive interactions with the OLIMSPAC measure of speech perception.
Discussion
The strength of this study lies in the fact that participants represent a full range of age at identification and intervention that can be expected to reasonably exist (between 1 month and 5 years of age) and a full range of degree of hearing loss from mild to profound. Our participants also represent a wide range of ethnic groups, races and use a variety of languages.
Age at fitting of amplification
The modeling of auditory-based communication outcomes clearly shows that, of the factors evaluated in this study, the age of access to auditory stimulation with hearing aids was the overall dominant factor in determining auditory based outcomes in children with congenital hearing loss. This study chose to look at age at amplification, but this factor is very closely related to age at identification and age at early intervention, at least for our group (Sininger et al., 2009) and these results can therefore be compared to other studies using those metrics. Age at amplification was the factor that explains the largest percentage of variance for both measures of speech perception and is also a significant predictor of language and speech production. Children with the earliest access to the speech signal through amplification, overall, will have the best outcomes on auditory-based communication measures. This is not surprising given the importance of access to auditory stimulation at very early ages for the development of stimulus-driven, complex neural networks in the auditory system.
Kennedy et. al., (2006) found that later age at identification and access to screening predicted delayed language ability but found no such relationship to speech production. Kennedy et. al., used a parent check-list rather than administering a formal test as used in this study. Certainly, a trained speech language pathologist may be able to detect speech errors that are not obvious to parents and the Arizona 3 could be expected to have greater sensitivity than a parent checklist. In addition, subjects in the Kennedy study were evaluated at an older age with a mean of 7.9 years while evaluations were started at age 3 years in the current study.
Strong influence of early intervention on language outcomes in children with hearing loss has been found in some previous studies (Yoshinaga-Itano et al., 1998; Moeller, 2000; Kennedy et al., 2006) but not in all. Wake, Poulakis, Hughes, Carey-Sargeant, & Rickards (2005) evaluated receptive and expressive language, speech production and reading in a group of 7–8 year old children with hearing loss. All children had been fitted with hearing aids by 4.5 years of age and demonstrated a wide range of hearing loss. Using an analysis approach similar to that used here, with age at diagnosis, severity of hearing loss and a block of covariates, Wake et al. found no predictive relationship between age at diagnosis and outcomes with the possible exception of the Peabody Picture Vocabulary Test. However, they found that degree of hearing loss was highly predictive of outcome.
A significant difference in the Wake et al. study and the current investigation comes in the range of ages of “diagnosis” (Wake et al) or “fitting of amplification” (current study). According to Wake and colleagues, age at diagnosis was highly correlated with age at fitting and the score means were within 2 months. The same close relationship between age at identification and age at intervention was found with the subjects of this study (Sininger et al., 2009) and therefore these two measures should be more or less equivalent. However, the median age of diagnosis in the Wake et al. study was 18.5 months (or fitting of amplification was 19.5 months.) The median age at fitting of amplification for the current study was 5.7 months. The very earliest ages of identification and hearing aid fitting were not well-represented in the Wake et al. study. An overall delay in fitting of amplification in the group studied by Wake et al. could have caused those children to miss the opportunity to take advantage of very early intervention and diminished the overall effect. Yoshinaga-Itano et al (1998) noted that the positive effects of early identification were found in the group identified before 6 months of age. Only 11 of 89 children in the Wake et al. study were diagnosed before 6 months of age and, to further complicate the comparison, the participants in the Wake et al. study who were identified under six months tended to be in the severe to profound hearing loss range with only one with mild loss. In contrast, half of their subjects in the current study were fitted before 5.7 months of age and there was no correlation between age at fitting and degree of hearing loss (r2 = .005, p = 0.64).
Nicholas and Geers (2008) also found no predictive value in age at amplification on spoken language skills in a group of 76 cochlear implant users at 3.5 years of age. For this group hearing level and duration of implant use were the primary predictors of outcome. The average age at identification for the children evaluated by Nicholas and Geers was 12 months of age. Therefore this study may have found the same bias as Wake et al. by not evaluating the effect of very early identification/intervention, although this is not clear. The differences in degree of hearing loss in the subject pool of the current study and the Nicholas and Geers study may help to reconcile the differences in the effect of age at initial intervention on outcome. The mean pure tone average hearing loss in Nicholas and Geers was 107 dB and ranged from 77 to 120 dB. The current study subjects ranged from mild to profound in degree of loss (mean of 64 dB and range of 25–108 dB).
Finally, Fitzpatrick, Durieux-Smith, Eriks-Brophy, Olds, & Gaines (2007) were also unable to demonstrate any effect of age at identification on language and speech outcomes in a study of young children with hearing impairment that utilized a design very similar to the current study. The only clear difference in this study and Fitzpatrick et al. is the distribution of the degree of hearing loss. Sixty-six percent of the subjects in the Fitzpatrick et al. study had severe or profound hearing loss whereas only 36% of subjects the current study had hearing loss >70 dB. The differences in findings across studies point out the importance of including all degrees of hearing loss in comprehensive studies of children with hearing loss. Concentrating exclusively on those children with severe to profound loss or those with cochlear implants can lead to conclusions that may not generalize to children with lesser degrees of loss.
Having a broad distribution of age at intervention is also important to be able to determine the effects. The current study benefited from timing relative to the inception of newborn hearing screening in California by allowing for many early and late identified children to be studied in the same cohort. In addition, because these infants were primarily identified through screening, no relationship between degree of loss and age at identification was found (Sininger et al., 2009) as is often seen in children identified though means other than universal screening.
Hearing Loss
Next in the list of factors influencing outcome in this study was hearing level in the better ear (degree of hearing loss), which dominated the model of performance for both speech production and spoken language measures but was not found to be an important factor in the modeling of speech perception. Several other studies have demonstrated the clear relationship between degree of hearing loss and language outcome with performance falling with degree of loss (Wake, Hughes, Poulakis, Collins, & Rickards, 2004; Nicholas & Geers, 2006; Fitzpatrick et al., 2007). Levitt (1987) also found a strong relationship between degree of hearing loss and speech intelligibility and a weak relationship of loss to syntactic comprehension.
In contrast, Blamey et al., (2001) found that speech perception was significantly negatively correlated to degree of hearing loss, but, unlike the current study and the others mentioned, did not find a relationship between degree of loss and speech production or language. Many of the children in the Blamey et al. study were cochlear implant users and overall, the degree of hearing loss was narrowly distributed in this study but this alone does not explain the discrepancy because other studies of participants with similar degrees of hearing loss (Nicholas & Geers, 2006) did find a relationships between degree of loss and language outcome.
One might assume that if amplification was providing adequate compensation for all degrees of hearing loss, the overall unaided hearing levels of the subjects would have only minor influence on outcome. However, as shown on Figure 1, the SII which predicts aided audibility of speech does not indicate an equal degree of aided audibility across all degrees of hearing loss. Rather the graph indicates that audibility falls with degree of loss regardless of amplification use. Based on the linear regression equation for the left and right ear combined, the SII score is predicted to be 117.93 − (0.91 × Hearing Level). Therefore an SII of 50 (approximately 50% of speech audibility) occurs for aided children with an average hearing level of 74.64 dB. In other words, children in our cohort with average hearing loss greater than 75 dB were missing more than half of speech in their environments regardless of the use of amplification.
One could argue that early fitting of amplification should not matter to children with profound hearing loss who eventually receive cochlear implants. This should have resulted in an interaction between effects of age at fit and effects of degree of loss but no such interaction was found. Age at implantation was not specifically used a variable in this study because it applied to only a subset of our subjects. Age at fitting and age at implantation were correlated revealing a clear relationship between early fitting of amplification and early implantation (r2 = 0.56 p = 0.0009). For children with implants the age at implantation in months, was 17.09 + 1.22*age at fitting of amplification. The effect of early amplification may have been carried over even to those children for whom the amplification was not adequate, because those early amplified were then early implanted. The positive effects of early implantation, which have been shown in many studies including Nicholas and Geers (2006), were reflected in the early amplification.
Cochlear Implantation
The modeling procedure holds all other factors constant when predicting the effect of any one factor. Therefore, one could conclude, holding the age at fitting or degree of hearing loss constant, the child using a cochlear implant can expect an improvement in speech production ability of 2/3 of a standard deviation and to be 12 months advanced in receptive and almost 18 months advanced in expressive language. An interesting finding in the database is that all children in the final participant group with 88 dB or more average hearing loss in the better hearing ear, received one or more cochlear implants. Some children with slightly better hearing also received implants but the children with 88 dB or greater were universally implanted in our sample. It seems that amplification was not providing adequate access to audibility of speech for children in our group with severe hearing losses. Although it appears that the implants were providing adequate compensation for audibility, a measure comparable to the SII for assessing the access to the speech signal with cochlear implants was not available, although most centers measured sound-field speech reception or awareness thresholds and found the implant provided significant improvement over the aided thresholds or awareness levels. It must be assumed that the cochlear implant can provide the necessary auditory input that is currently not provided by standard amplification when average hearing levels exceed some amount between about 75 and 88 dB.
The relationship between cochlear implantation and speech perception as measured by the PSI, seems counter-intuitive; use of a CI was related to a later age for reaching maximum PSI performance. One possible explanation of this result is that children struggling with speech perception will be those who are most likely to receive intervention by cochlear implant. A similar discussion is found related to auditory training in a later section. It is also possible that the age of implantation did not allow adequate time for progress in processing ability to be realized before the study was concluded. The median age of implantation for our subjects is just under 30 months and testing for speech perception is initiated at 36 months.
It is also possible that development of speech perception in the presence of speech competition is not adequately compensated by the use of a cochlear implant. Only the PSI test, and not the OLIMSPAC, showed a negative correlation between implantation and outcome and only the PSI evaluates speech perception in a competing talker background. This condition is known to be highly challenging for children with cochlear implants. Nelson, Jin, Carney and Nelson (2003) have shown that cochlear implant users may be at a significant disadvantage when attempting to understand a signal in the presence of a modulated masker (such as speech) and they and others have shown that cochlear implant users show little or no release from masking with modulated noise or real-speech maskers (Stickney, Zeng, Litovsky, & Assmann, 2004; Cullington & Zeng, 2008). The most congruous explanation for this single negative finding of cochlear implantation on speech perception in the presence of a competing talker is that the implant is not providing the expected release from modulated masking and consequently, the implant is impeding performance on speech perception in the presence of a competing talker.
Other predictive factors
The procedure used to assess the importance of predictive factors on auditory-based outcomes involved a multivariate regression analysis that creates a model of the outcomes based on the combined contributions of the factors analyzed. The strength of the model is assessed by comparing the modeled outcome to the actual outcomes, revealing a correlation coefficient or R2. This value indicates the percentage of variance accounted for by the model. The five outcome models have corresponding R2 values ranging from 0.27 to 0.56. While these models are reasonably strong, it is clear that they do not account for all of the variance in the prediction. Factor interactions were not found in the modeling and could not be responsible for the unaccounted variance.
Certainly test scores have inherent variability that will contribute to variance in outcome measures. This was especially problematic when one (final) score was used to characterize the outcome although all previous data was scrutinized to guard against severe outliers in the final scores. Using a linearly predicted outcome for the OLIMSPAC and PSI would reduce but not eliminate the natural variability in the measure used to measure outcome.
The most likely reason for unaccountable variance is that not every important factor was evaluated or used in the model. The original study design included a measure of the audibility provided by the amplification, such as SII, as an important factor for predicting outcome. Initial analysis found a close relationship between SII and degree of hearing loss. Using both SII and degree of loss would have provided redundant information in the model. Another factor that was initially considered for use in a model of performance was socio-economic status. However, our final group included a very narrow range of SES that could not have been predictive. The distribution of SES as measured by the years of formal education of the mother for this study, had a median of 16 years (college graduate) with the lower 10th percentile being a high school graduate and the 90th percentile being 7.5 years of college. Unfortunately, the nature and demands of this type of longitudinal study may influence the SES makeup of the participant families. That is, the time demands and financial strains of participation may inadvertently exclude some subjects of lesser means. This, in turn, limits the generalizability of this study.
Parent interaction, as measured by the NCAST, was influential in predicting only the outcome of the OLIMSPAC. This could be interpreted as indicating that parents who are effective teachers of their children can provide important insight into development of phoneme perception. It is not clear why the same would not be true of other communication outcomes, especially language and speech production. It is important to distinguish between parent-child interaction in a teaching situation, as was measured by the NCAST and general parent cooperation or follow-through. Moeller (2000) found family involvement, as measured on a 5 point rating scale completed by interventionists, was a very important factor in predicting language outcome. Education inventories used in this study included a similar 4-point scale to measure interventionist’s ratings of parent involvement. The parents of children in this study were consistently exceptional at follow-through. Consequently, with no real variance in our group on this measure, we were not able to assess the influence of parent involvement on outcome, merely the influence of parent interaction or teaching ability. However, teaching ability appears to show no significant influence on most of the outcomes measured.
Pressman, Pipp-Siegel, Yoshinaga-Itano, & Deas (1999) have found a clear relationship between maternal sensitivity and language outcome in children with hearing loss. The measure used in that study evaluated items such as sensitivity to cues, which were scored from a videotape of a mother-infant dyad. Except for the restrained “teaching” activity of the recorded dyad used in the NCAST measure, the descriptions of the tests are very similar as were the subject groups and ages used in the present study and in Pressman et al. The language measures of Pressman and colleagues were from parent report and included manual as well as spoken communications while the current study focused on spoken language. It is possible that different aspects of parental behaviors may influence spoken and manual communication. This points out the need for replication studies particularly in areas that involve complex relationships. Many factors, including specific features of individual tests or characteristics of the subpopulation studied, may influence findings in ways that are not always apparent.
Auditory Training
There is a large variation in the intensity of oral education provided to our participants. For example, the child with the highest AOTS was enrolled in an oral only program for 4 hours per day throughout the year. The child with the smallest AOTS of 31 had a mild hearing loss and was consistently receiving only to one hour per month of oral only intervention. Only a weak relationship is found between annual oral training and degree of hearing loss (r2 = 0.042). The educational inventories evaluated only targeted intervention for hearing loss, speech or language delay. For example, only hours of individual pull-out therapy would contribute to the AOTS score of a child in a mainstreamed classroom whereas all of hours of a self-contained classroom for children with hearing loss would be counted as intervention. Educational intervention, in general is quite complex and difficult to characterize.
The intervention factor, as characterized in this study, explained some of the variance for only one outcome, the OLIMSPAC. Given that the purpose of the study was to determine factors in development of auditory skills, it would seem that training would be a significant factor in all outcomes measured. However, the methods for allocation of services in the U.S. may help to understand why this factor was not found to predict outcomes. The National Early Intervention Longitudinal Study (NEILS) looked at early intervention in a variety of settings in the U.S. One section of that study investigated the relationship between the level of spending on early intervention services and outcomes of children receiving the services at 36 months of age (Levin, Perez, Lam, Chambers, & Hebbeler, 2004). The report found that the higher the expenditure for services, the worse the outcome! They explain that this is not a causal relationship, rather reflects the fact that the initial severity of the condition dictates the allocation of service. The same is true of children with hearing loss. Children who are poor performers will receive more services rather than the other way around. Poor outcomes lead to increased intervention and good outcomes will reduce it. The fact that no relationship was found between auditory intervention and measured outcomes in 4 of 5 findings and one positive relationship, points to a positive overall effect of intervention when one weighs in the “NEILS” effect. Clearly the relationship between educational intervention and outcome is quite complex and requires the attention of carefully controlled and very large-scale studies.
Multilingual Home
The impact of being in a multilingual home was seen in only one outcome, the Pediatric Speech Intelligibility test. In this case, being in a multilingual home was found to be a positive predictor and, according to the model, children in a multi-lingual environment would achieve maximum score 10 months earlier than those in a mono-lingual home. Very few other studies have looked specifically at the effect of this factor on outcomes in children with hearing loss. Three studies looked at development of spoken language and speech in multilingual children with hearing loss but in all cases the subjects were cochlear implant users (Waltzman, Robbins, Green, & Cohen, 2008; McConkey Robbins, Green, & Waltzman, 2004; Thomas, Hussam, & Zwolan, 2008). These studies found no adverse effects on language or speech development associated with the use of multiple languages in the home. In the current study of children with a full range of hearing loss, for most outcomes our finding is the same, no effect, either positive or negative, on outcomes. The fear that learning more than one language at a time may place too much linguistic and perceptual demand on children with hearing loss appears to be unfounded. In fact, our findings indicate that there may be advantages to speech perception, in this case in listening to speech with competition, for children who are exposed to more than one language. In the final study group, fourteen families were bilingual with second (spoken) languages including Spanish, English, Chinese, Tagalog, Urdu and Farsi. Three subjects were bilingual in English and ASL.
Table 5 summarizes and compares results of this study with others. In all cases the studies involved children with hearing loss as subjects and a variety of communication measures as outcomes. Some of the common predictive factors studied include variations on age at identification or intervention, hearing level, cochlear implant status, cognitive or self-help skills, and family involvement. The variety in the subject factors across studies is the most credible origin for the variability in the outcomes.
Table 5.
Results of communication outcome studies of children with hearing loss are summarized and some of the common predictive factors are listed. N/A indicates not applicable to this study. Numbers next to YES show the ranking of effect size in the study.
| Summary of Outcome Studies on Children with Hearing Loss | ||||||||
|---|---|---|---|---|---|---|---|---|
| Study | Population | Test Age | Outcomes | Positive Predictive Factors | ||||
| Age at ID or Fit | Hearing Level | Cochlear Implant | Self Help/Cognitive | Family Involvement | ||||
| Yoshinaga-Itano et al. 1998 | Mild to profound, with Addtl. Disabilities | 5 Years | Language | YES (< 6 months) | YES * | N/A | YES | N/A |
| Moeller 2000 | Mild to profound W/O Addtl. Disabilities | 1–3 Years | Language | YES-2 | NO | N/A | YES-3 | YES-1 |
| Wake et al 2005 | Mild to Profound W/O Addtl. Disabilities | 7–8 Years | Language, Speech Prod Reading | NO | YES | N/A | N/A | N/A |
| Kennedy et al. 2006 | Mod to profound with Addtl. Disabilities | 7.9 Years | Language | YES | N/A | N/A | N/A | N/A |
| Speech | NO | |||||||
| Nicholas & Geers 2006 | Severe-Prof CI Users W/O Addtl. Disabilities | 3.5 Years | Language | NO | YES | YES (duration) | N/A | N/A |
| Fitzpatrick et al. 2007 | Mild to Profound W/O Addtl. Disabilities | 24–60 Mo. | Language & Speech | NO | YES-1 | N/A | YES-2 | N/A |
| Present Study | Mild to Profound W/O Addtl. Disabilities | 36–60 Mo | Speech Perception | YES-1 | NO | YES-3 Neg Effect | N/A | YES-2** |
| Language, | YES-3 | YES-1 | YES-2 | NO** | ||||
| Speech Production | YES-2 | YES-1 | YES-3 | NO** | ||||
For children with late identification.
teaching skills rather than involvement
Limitations of Generalizability
Discussion of these results must include a caveat regarding the limitations of any conclusions to the specific group and factors studied. These results can be generalized to children with congenital or very early onset hearing loss, who are without other significant disabling conditions, from homes with well educated parents who are highly compliant with their child’s intervention. Subject selection for this study included only typically functioning children with hearing loss but no cognitive or other disabling conditions. A much larger group of participants would have been required to discern the relationships seen if a more diverse population was studied. To make meaningful statements regarding the analysis, we chose to study as few predictor variables as was reasonable. However it is clear that many children with auditory difficulties may have other disabling conditions and that intelligence, vision, motor skills etc. will have a significant impact on all learning including the development of communication skills. It will be difficult but very important to study more diverse populations with study designs that will allow for more variability in the outcomes in the future.
The longitudinal, prospective nature of this study ultimately resulted in a selection bias regarding participants. This bias is essentially unavoidable. The SES and the high parental cooperation data are good examples of how the study design can influence the subject pool. Some families who did not enroll stated that the added commitment of time was not possible due to demands of jobs and family. Economic pressures were obvious challenges to full participation. The mean SES of the families who dropped from the study was 12.6 while the average SES of those who completed the study was 15.63 indicating that those with higher SES were more likely to be able to complete the study.
Acknowledgments
This study was funded by the National Institute of Deafness and Other Communication Disorders R01 DC04433 Sininger. The authors wish to acknowledge the research and audiology staff who made this study possible, in particular, Dr. Laurie Eisenberg and Amy Martinez who coordinated the efforts at the House Ear Institute, Elizabeth Christensen who served as study coordinator at the UCLA site and Jasmine Hu, staff research assistant who helped in data collection and analysis. Dr. Barbara Cone gave valuable commentary on the manuscript. We greatly appreciate statistical consultation from Dr. Jeffrey Gornbein and associates from the UCLA Department of Biomathematics. Audiologists at all three sites were invaluable in enrolling participants and providing audiologic data and included Gina Gracia, Stanton Jones, Frances Miranda, Erin Mahnke, Danielle Dzubak, Katy Sullivan-Harm, Aprille Engalla, Kim Swaim, Talisa Blount, Jodi Wilske, and Carey Williams. Psychological/cognitive assessments were provided by Marie Poulson, PhD, Karin Best, PhD and Carren Sticka, PhD. Speech and language assessments were provided by Kathy Khalehpari, MA, Sophie Ambrose, MA, Kathy Lehnert, MS and Jennifer Regnery, MS. NCAST tests were scored by Pat Place, R.N. Many early interventionists in the Los Angeles area provided valuable feedback on educational performance of the children. Most importantly, we express our deepest gratitude to the families who participated in the studies and gave so much of themselves to help advance our knowledge regarding the development of communication in children with hearing loss.
Funding for this study was provided by the NIDCD R01 DC04433
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Reference List
- 1.American Academy of Audiology. Pediatric Amplification Protocol. 2003. [Google Scholar]
- 2.Bayley N. Bayley Scales of Infant Development (Version Behavior Rating Scales) [Computer software] San Antonio, TX: Psychological Corporation; 1993. [Google Scholar]
- 3.Blamey PJ, Sarant JZ, Paatsch LE, Barry JG, Bow CP, Wales RJ, et al. Relationships Among Speech Perception, Production, Language, Hearing Loss, and Age in Children With Impaired Hearing. J Speech Lang Hear Res. 2001;44:264–285. doi: 10.1044/1092-4388(2001/022). [DOI] [PubMed] [Google Scholar]
- 4.Boothroyd A. Auditory perception of speech pattern contrasts by subjects with sensorineural hearing loss. J Speech Hear Res. 1984;27:134–144. doi: 10.1044/jshr.2701.134. [DOI] [PubMed] [Google Scholar]
- 5.Boothroyd A, Eisenberg LS, Martinez AS. OLIMSPAC Version 3.1d. Los Angeles: House Ear Institute; 2005. [Google Scholar]
- 6.Cheour-Luhtanen M, Alho K, Kujala T, Reinikainen K, Renlund M, Aaltonen O, et al. Mismatch negativity indicates vowel discrimination in newborns. Hear Res. 1995;82:53–58. doi: 10.1016/0378-5955(94)00164-l. [DOI] [PubMed] [Google Scholar]
- 7.Cullington HE, Zeng FG. Speech recognition with varying numbers and types of competing talkers by normal-hearing, cochlear-implant, and implant simulation subjects. J Acoust Soc Am. 2008;123:450–461. doi: 10.1121/1.2805617. [DOI] [PubMed] [Google Scholar]
- 8.Davidson LS, Skinner MW. Audibility and Speech Perception of Children Using Wide Dynamic Range Compression Hearing Aids. Am J Audiol. 2006;15:141–153. doi: 10.1044/1059-0889(2006/018). [DOI] [PubMed] [Google Scholar]
- 9.Davis JM, Elfenbein J, Schum R, Bentler RA. Effects of Mild and Moderate Hearing Impairments on Language, Educational, and Psychosocial Behavior of Children. J Speech Hear Dis. 1986;51:53–62. doi: 10.1044/jshd.5101.53. [DOI] [PubMed] [Google Scholar]
- 10.DeCasper AJ, Fifer WP. Of Human Bonding: Newborns Prefer their Mothers’ Voices. Science. 1980;208:1174–1176. doi: 10.1126/science.7375928. [DOI] [PubMed] [Google Scholar]
- 11.Edwards S, Fletcher P, Garman M, Hughes A, Letts C, Sinda I. Reynell Developmental Language Scales [Computer software] Windsor, England: NFER-Nelson Publishing; 1997. [Google Scholar]
- 12.Eisenberg LS, Dirks DD. Reliability and sensitivity of paired comparisons and category rating in children. J Speech Hear Res. 1995;38:1157–1167. doi: 10.1044/jshr.3805.1157. [DOI] [PubMed] [Google Scholar]
- 13.Fitzpatrick E, Durieux-Smith A, Eriks-Brophy A, Olds J, Gaines R. The impact of newborn hearing screening on communication development. J Med Scr. 2007;14:123–131. doi: 10.1258/096914107782066248. [DOI] [PubMed] [Google Scholar]
- 14.Geers AE. Factors Affecting the Development of Speech, Language, and Literacy in Children with Early Cochlear Implantation. Lang Speech Hear Serv Sch. 2002;33:172–183. doi: 10.1044/0161-1461(2002/015). [DOI] [PubMed] [Google Scholar]
- 15.Jerger S, Lewis S, Hawkins J, Jerger J. Pediatric speech intelligibility test. I. Generation of test materials. Int J Ped Otorhinol. 1980;2:217–230. doi: 10.1016/0165-5876(80)90047-6. [DOI] [PubMed] [Google Scholar]
- 16.Jusczyk PW, Cutler A, Redanz NJ. Infants’ Preference for the Predominant Stress Patterns of English Words. Child Dev. 1993;64:675–687. [PubMed] [Google Scholar]
- 17.Kennedy CR, McCann DC, Campbell MJ, Law CM, Mullee M, Petrou S, et al. Language Ability after Early Detection of Permanent Childhood Hearing Impairment. N Eng J Med. 2006;354:2131–2141. doi: 10.1056/NEJMoa054915. [DOI] [PubMed] [Google Scholar]
- 18.Kuhl PK. A new view of language acquisition. Proc Natl Acad Sci. 2000;97:11850–11857. doi: 10.1073/pnas.97.22.11850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kuhl PK. Speech perception in early infancy: Perceptual constancy for spectrally dissimilar vowel categories. J Acoust Soc Am. 1979;66:1668–1679. doi: 10.1121/1.383639. [DOI] [PubMed] [Google Scholar]
- 20.Levin J, Perez M, Lam I, Chambers JG, Hebbeler KM. National Early Intervention Longitudinal Study:Expenditure Study. Menlo Park, CA: U.S. Office of Special Eduation and SRI International; 2004. (Rep. No. NEILS Data Report No. 4) [Google Scholar]
- 21.Levitt H. Interrelationships Among the Speech and Language Measures. In: Levitt H, McGarr N, Geffner D, editors. ASHA Monographs. Development of Language and Communication Skills in Hearing-Impaired Children. Vol. 26. 1987. pp. 123–138. [PubMed] [Google Scholar]
- 22.McConkey Robbins A, Green JE, Waltzman SB. Bilingual Oral Language Proficiency in Children With Cochlear Implants. Arch Otolaryngo-Head Neck Surg. 2004;130:644–647. doi: 10.1001/archotol.130.5.644. [DOI] [PubMed] [Google Scholar]
- 23.Moeller MP. Early Intervention and Language Development in Children Who Are Deaf and Hard of Hearing. Pediatrics. 2000;106:1–9. doi: 10.1542/peds.106.3.e43. [DOI] [PubMed] [Google Scholar]
- 24.Moeller MP. Intervention and Outcomes for Young Children who are Deaf and Hard of Hearing and Thier families. In: Kurtzer-White E, Luterman D, editors. Early Childhood Deafness. Baltimore: York Press, Inc; 2001. pp. 109–138. [Google Scholar]
- 25.Moeller MP, Hoover B, Putman C, Arbataitis K, Bohnenkamp G, Peterson B, et al. Vocalizations of Infants with Hearing Loss Compared with Infants with Normal Hearing:Part I-Phonetic Development. Ear Hear. 2007;28:605–627. doi: 10.1097/AUD.0b013e31812564ab. [DOI] [PubMed] [Google Scholar]
- 26.Moore JK, Linthicum FH. The human auditory system: A timeline of development. Int J Audiol. 2007;46:460–478. doi: 10.1080/14992020701383019. [DOI] [PubMed] [Google Scholar]
- 27.Nelson PB, Jin SH, Carney AE, Nelson DA. Understanding speech in modulated interference: cochlear implant users and normal-hearing listeners. J Acoust Soc Am. 2003;113:961–968. doi: 10.1121/1.1531983. [DOI] [PubMed] [Google Scholar]
- 28.Nicholas JG, Geers AE. Effects of Early Auditory Experiences on the Spoken Language of Deaf Children at 3 Years of Age. Ear Hear. 2006;27:286–298. doi: 10.1097/01.aud.0000215973.76912.c6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nicholas JG, Geers AE. Effects of Early Auditory Experiences on the Spoken Language of Deaf Children at 3 Years of Age. Ear Hear. 2008;27:286–298. doi: 10.1097/01.aud.0000215973.76912.c6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pressman L, Pipp-Siegel S, Yoshinaga-Itano C, Deas A. Maternal sensitivity predicts language gain in preschool children who are deaf and hard of hearing. J Deaf Stud Educ. 1999;4:294–304. doi: 10.1093/deafed/4.4.294. [DOI] [PubMed] [Google Scholar]
- 31.Roid GH, Miller LJ. Leiter International Performance Scale-Revised. Wood Dale, IL: Stoelting Company; 1997. [Google Scholar]
- 32.Seewald RC, Cornelisse LE, Ramji KV, Sinclair ST, Moodie KS, Jamieson DG. DSL v4.1 for Windows. A software implementation of the desired sensation level (DSL[i/o]) method of fitting linear gain and wide-dynamic-range compression hearing instruments. [Computer software] Hearing Health Care Research Unit, The University of Western Ontario; 1997. [Google Scholar]
- 33.Sininger YS, Doyle KJ, Moore JK. The case for early identification of hearing loss in children. Ped Clin North Amer. 1999;46(1):1–14. doi: 10.1016/s0031-3955(05)70077-8. [DOI] [PubMed] [Google Scholar]
- 34.Sininger YS, Martinez A, Eisenberg LS, Christensen E, Grimes A, Hu J. Newborn Hearing Screening Speeds Diagnosis and Access to Intervention by 20–24 Months. J Am Acad Audiol. 2009;20:49–57. doi: 10.3766/jaaa.20.1.5. [DOI] [PubMed] [Google Scholar]
- 35.Stelmachowicz PG, Pittmann A, Hoover BM, Lewis DC, Moeller MP. The importance of high-frequency audibility in the speech and language development of children with hearing loss. Arch Otolaryngol Head Neck Surg. 2004;130:556–562. doi: 10.1001/archotol.130.5.556. [DOI] [PubMed] [Google Scholar]
- 36.Stickney GS, Zeng FG, Litovsky R, Assmann P. Cochlear implant speech recognition with speech maskers. J Acoust Soc Am. 2004;116:1081–1091. doi: 10.1121/1.1772399. [DOI] [PubMed] [Google Scholar]
- 37.Sumner G, Spietz A. NCAST Caregiver/Parent-Child Interaction Teaching Manual. NCAST/Caregiver 1994 [Google Scholar]
- 38.Thomas E, Hussam EK, Zwolan TA. Children with cochlear implants who live in monolingual and bilingual homes. Otol Neurotol. 2008;29:230–234. doi: 10.1097/mao.0b013e31815f668b. [DOI] [PubMed] [Google Scholar]
- 39.Wake M, Hughes EK, Poulakis Z, Collins C, Rickards FW. Outcomes of Children with Mild-Profound Congenital Hearing Loss at 7 to 8 years: A population study. Ear Hear. 2004;25:1–8. doi: 10.1097/01.AUD.0000111262.12219.2F. [DOI] [PubMed] [Google Scholar]
- 40.Wake M, Poulakis Z, Hughes EK, Carey-Sargeant C, Rickards FW. Hearing impairment: a population study of age at diagnosis, severity, and language outcomes at 7–8 years. Archives of Disease in Childhood. 2005;90:238–244. doi: 10.1136/adc.2003.039354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Waltzman SB, Robbins AM, Green JE, Cohen NL. Second oral language capabilities in children with cochlear implants. Otol Neurotol. 2008;24:757–763. doi: 10.1097/00129492-200309000-00012. [DOI] [PubMed] [Google Scholar]
- 42.White SJ, White REC. The effects of hearing status of the family and age of intervention on receptive and expressive oral language skills in hearing-impaired infants. ASHA Monographs. In: Levitt H, McGarr N, Geffner D, editors. Development of Language and Communication Skills in Hearing-Impaired Children. Vol. 26. 1987. pp. 9–24. Ref Type: Serial (Book, Monograph) [PubMed] [Google Scholar]
- 43.Yoshinaga-Itano C, Sedey AL, Coutler DK, Mehl AL. Language of early-and later-identified children with hearing loss. Pediatrics. 1998;5:1161–1171. doi: 10.1542/peds.102.5.1161. [DOI] [PubMed] [Google Scholar]
Reference Notes
- 44.Visser-Dumont LJ, Martinez AS, Johnson KC, Eisenberg LS. Pediatric speech intelligibility test: Comparison of two recordings; Charlotte, NC. April 11–14.2007. [Google Scholar]