Abstract
Acupuncture appears to be a clinically effective treatment for acute and chronic pain. A considerable amount of research has been conducted to evaluate the role that acupuncture plays in pain suppression; however, few studies have been conducted to evaluate the side effects of the acupuncture procedure. This case report describes a suspected postdural puncture headache following acupuncture for lower back pain. Considering the high opening pressure, cerebrospinal fluid leakage, and the patient's history of acupuncture in the lower back area, our diagnosis was iatrogenic postdural puncture headache. Full relief of the headache was achieved after administration of an epidural blood patch.
Keywords: Acupuncture, Iatrogenic complication, Postdural puncture headache
INTRODUCTION
Acupuncture seems to be a clinically effective treatment for acute and chronic pain, and a considerable amount of research is being conducted to evaluate its role in the suppression of pain, particularly lower back pain14,15). Acupuncture has a reputation among Koreans as being safe. However, some prospective studies on the frequency of adverse effects of acupuncture have recently been conducted11). Since 1965, there have been repeated reports of serious and even life-threatening incidents associated with acupuncture12). Additionally, several authors have compiled lists of complications caused by or associated with acupuncture. The most frequently reported complications are pneumothorax and lesions of the spinal cord1). Severe injuries of peripheral nerves and blood vessels due to acupuncture appear to be very rare1).
The depth of the insertion of the acupuncture needles varies from a few millimeters to several centimeters. The tip of the needle often lies in a muscle or overlies other structures, including nerves and pleura; therefore, acupuncturists need a working knowledge of anatomy to avoid causing direct trauma9).
In this case report, we describe a patient who developed a suspected postdural puncture headache following an acupuncture procedure on his lower back.
CASE REPORT
The patient was a 33-year-old man (height 170 cm and weight 62.5 kg) with no particular medical history other than lower back pain. The patient had received acupuncture at an Oriental medicine clinic for his lower back pain 3 days prior to admission to our facility. More than 10 acupuncture needles were inserted into acupuncture points around paramedian region from L3 level through L5 level. His aggravating headache developed 2 days before he visited our hospital.
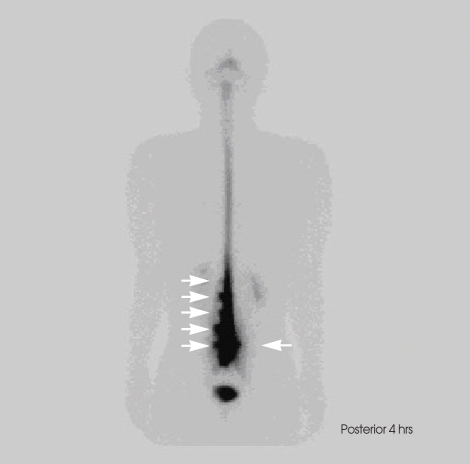
The patient complained of a bilateral, relentless squeezing and non-throbbing ache in the frontal area. The headache was relieved when recumbent and reappeared when upright. The patient also reported nausea but denied vomiting. The patient denied tinnitus, nystagmus or any other focal neurological symptoms. The patient had been taking acetaminophen over the past 2 days before his visit to our hospital with minimal relief of his headache. The patient had stable vital signs. In addition, the results of a neurological examination were unremarkable. Brain magnetic resonance imaging (MRI) revealed mild meningeal enhancement, but was otherwise normal. Because spontaneous intracranial hypotension was suspected, a cisternography was conducted to determine if there were any cerebrospinal fluid (CSF) leaks. It revealed multiple leaks at the L2-S1 level, with five foci of CSF leakage on the left side of the lumbar spine (from L1 to L5) and a small amount of CSF leakage on the right side at the L5 level (Fig. 1).
Fig. 1.
Cisternography confirming cerebrospinal fluid (CSF) leakage. Five foci of CSF leakage on the left side at the lumbar level (from L1 to L5) and a small amount of CSF leakage on the right side at the L5 level were observed.
Lumbar puncture was performed concomitantly to measure the opening pressure and for CSF analysis. The opening pressure, which is generally lower than normal for spontaneous intracranial hypotension, was 185 mmH2O (normal range : 70-180 mmH2O)7). The CSF analysis results were normal, which enabled us to rule out meningitis. Thus, although it was impossible to completely rule out the possibility of spontaneous intracranial hypotension8), considering the CSF leakage and his history of a recent acupuncture on the lower back area near the leakage site, it seemed rational to diagnose an iatrogenic postdural puncture headache. For the treatment, an epidural blood patch was conducted by injecting 10 mL of autologous blood into the L3-4 interspace6). The patient obtained dramatic, symptomatic relief within 15 minutes and was discharged on the same day in stable condition without any prescription medications. Also, there were no signs of symptom recurrence on 1st week and 4th week of follow up.
DISCUSSION
Acupuncture is a treatment modality commonly used in oriental medicine that generally involves directly inserting acupuncture needles ranging from 15 to 125 mm in length with a gauge of 26-32 F. into the back, buttocks and leg in symptomatic areas3,13). Recently, interest in oriental medicine has increased worldwide and acupuncture is now widely used in many countries, especially East Asia. Acupuncture is commonly used to manage lower back pain. Despite the benefits of this procedure, it can be associated with several complications such as acute infection, hemorrhage, disease transmission, and direct injury to internal organs, including neural tissue2,11).
We confirmed CSF leakage through cisternography, which led to the conclusion that the patient's headache was due to CSF leakage. Other diseases were ruled out through CSF analysis and MRI. The two suspicious diagnoses were spontaneous intracranial hypotension (SIH) and iatrogenic postdural puncture headache due to the acupuncture procedure. Although it is possible that dural puncture CSF leakage may occur in SIH, our final diagnosis was iatrogenic postdural puncture headache due to the acupuncture procedure. This diagnosis was made because the patient did not suffer from any symptoms other than lower back pain, his headache developed just 1 day after the acupuncture procedure on his back and there were no other reasons for the headache according to various studies4). Therefore, we reasoned that the CSF leakage was due to an iatrogenic dural puncture rather than SIH. Furthermore, although the opening pressure is generally normal (normal range : 70-180 mmH2O) in SIH patients, this patient's opening pressure was 185 mmH2O7). According to recent studies, CSF volume itself is thought to be the main cause for headaches in SIH patients and CSF hypovolemia seems to occur in patients with normal intracranial pressure5). Several authors have reported spinal cord injuries following acupuncture similar to those observed in the present case10).
Once CSF leakage occurs, CSF volume decreases irrelevant to opening pressure. In an attempt to relieve the symptom by preventing further loss of CSF and normalizing CSF volume, blood patch is performed. This rationale for performing blood patch is applied in all CSF leakage cases, apart from the variation of opening pressure since the opening pressure does not necessarily reflect the CSF volume.
We could not identify a previously reported case of postdural puncture headache caused by an acupuncture needle in the literature. Nevertheless, the findings presented here indicate that clinicians should consider rare complications such as inadvertent puncture of the dura in patients complaining of headache following acupuncture.
CONCLUSION
Here, we reported a case of a suspected postdural puncture headache following acupuncture for lower back pain in which dramatic, symptomatic relief was obtained after treatment with a blood patch.
References
- 1.Ernst E, White A. Life-threatening adverse reactions after acupuncture? A systematic review. Pain. 1997;71:123–126. doi: 10.1016/s0304-3959(97)03368-x. [DOI] [PubMed] [Google Scholar]
- 2.Hadden WA, Swanson AJ. Spinal infection caused by acupuncture mimicking a prolapsed intervertebral disc. A case report. J Bone Joint Surg Am. 1982;64:624–626. [PubMed] [Google Scholar]
- 3.Hwang JK, Kim J, Lee BJ, Park JJ, Kim JS, Bak YT. Pneumoretroperitoneum following acupuncture. J Altern Complement Med. 2008;14:1299–1301. doi: 10.1089/acm.2008.0261. [DOI] [PubMed] [Google Scholar]
- 4.Hyun SH, Lee KH, Lee SJ, Cho YS, Lee EJ, Choi JY, et al. Potential value of radionuclide cisternography in diagnosis and management planning of spontaneous intracranial hypotension. Clin Neurol Neurosurg. 2008;110:657–661. doi: 10.1016/j.clineuro.2008.03.014. [DOI] [PubMed] [Google Scholar]
- 5.Kelley G. CSF hypovolemia vs intracranial hypotension in "spontaneous intracranial hypotension syndrome". Neurology. 2004;62:1453. doi: 10.1212/wnl.62.8.1453. [DOI] [PubMed] [Google Scholar]
- 6.Miller RD. Miller's Anesthesia. ed 6. Philadelphia: Elsevier Inc; 2005. pp. 1668–1670. [Google Scholar]
- 7.Mokri B. Spontaneous low cerebrospinal pressure/volume headaches. Curr Neurol Neurosci Rep. 2004;4:117–124. doi: 10.1007/s11910-004-0025-5. [DOI] [PubMed] [Google Scholar]
- 8.Park ES, Kim E. Spontaneous intracranial hypotension : clinical presentation, imaging features and treatment. J Korean Neurosurg Soc. 2009;45:1–4. doi: 10.3340/jkns.2009.45.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Peuker ET, White A, Ernst E, Pera F, Filler TJ. Traumatic complications of acupuncture. Therapists need to know human anatomy. Arch Fam Med. 1999;8:553–558. doi: 10.1001/archfami.8.6.553. [DOI] [PubMed] [Google Scholar]
- 10.Sasaki H, Abe H, Iwasaki Y, Tsuru M, Itoh T. [Direct spinal cord and root injury caused by acupuncture-report of 2 cases] No Shinkei Geka. 1984;12:1219–1223. [PubMed] [Google Scholar]
- 11.White A. A cumulative review of the range and incidence of significant adverse events associated with acupuncture. Acupunct Med. 2004;22:122–133. doi: 10.1136/aim.22.3.122. [DOI] [PubMed] [Google Scholar]
- 12.White A, Hayhoe S, Hart A, Ernst E. Adverse events following acupuncture : prospective survey of 32 000 consultations with doctors and physiotherapists. BMJ. 2001;323:485–486. doi: 10.1136/bmj.323.7311.485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wolsko PM, Eisenberg DM, Davis RB, Kessler R, Phillips RS. Patterns and perceptions of care for treatment of back and neck pain : results of a national survey. Spine (Phila Pa 1976) 2003;28:292–297. doi: 10.1097/01.BRS.0000042225.88095.7C. discussion 298. [DOI] [PubMed] [Google Scholar]
- 14.Yuan J, Kerr D, Park J, Liu XH, McDonough S. Treatment regimens of acupuncture for low back pain-a systematic review. Complement Ther Med. 2008;16:295–304. doi: 10.1016/j.ctim.2008.04.006. [DOI] [PubMed] [Google Scholar]
- 15.Yuan J, Purepong N, Kerr DP, Park J, Bradbury I, McDonough S. Effectiveness of acupuncture for low back pain : a systematic review. Spine (Phila Pa 1976) 2008;33:E887–E900. doi: 10.1097/BRS.0b013e318186b276. [DOI] [PubMed] [Google Scholar]