Abstract
Objective
Clinical, radiographic, and outcomes assessments, focusing on complications, were performed in patients who underwent pedicle subtraction osteotomy (PSO) to assess correction effectiveness, fusion stability, procedural safety, neurological outcomes, complication rates, and overall patient outcomes.
Methods
We analyzed data obtained from 13 consecutive PSO-treated patients presenting with fixed sagittal imbalances from 1999 to 2006. A single spine surgeon performed all operations. The median follow-up period was 73 months (range 41-114 months). Events during perioperative course and complications were closely monitored and carefully reviewed. Radiographs were obtained and measurements were done before surgery, immediately after surgery, and at the most recent follow-up examinations. Clinical outcomes were assessed using the Oswestry Disability Index and subjective satisfaction evaluation.
Results
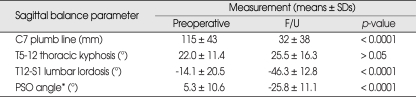
Following surgery, lumbar lordosis increased from -14.1° ± 20.5° to -46.3° ± 12.8° (p < 0.0001), and the C7 plumb line improved from 115 ± 43 mm to 32 ± 38 mm (p < 0.0001). There were 16 surgery-related complications in 8 patients; 3 intraoperative, 3 perioperative, and 10 late-onset postoperative. The prevalence of proximal junctional kyphosis (PJK) was 23% (3 of 13 patients). However, clinical outcomes were not adversely affected by PJK. Intraoperative blood loss averaged 2,984 mL. The C7 plumb line values and postoperative complications were closely correlated with clinical results.
Conclusion
Intraoperative or postoperative complications are relatively common following PSO. Most late-onset complications in PSO patients were related to PJK and instrumentation failure. Correcting the C7 plumb line value with minimal operative complications seemed to lead to better clinical results.
Keywords: Sagittal imbalance, Pedicle subtraction osteotomy, Clinical outcome, Proximal junctional kyphosis, Complication
INTRODUCTION
Disruption of normal sagittal alignment resulting in global sagittal imbalance can cause significant pain and impair ambulation directly and indirectly through compensatory mechanisms. When global sagittal imbalance arises because a long spinal segment is fixed or fused in a hyperkyphotic and/or hypolordotic position, the patient is said to have fixed sagittal imbalance. The causes of sagittal deformity are myriad, but most commonly include posttraumatic kyphosis, iatrogenic flat back syndrome, postlaminectomy kyphosis, degenerative lumbar kyphosis, and ankylosing spondylitis2,5,7). For many years, the Smith-Petersen15) osteotomy, with or without release of the anterior aspect of the spine, was the procedure of choice to shorten the posterior column and thereby reduce fixed kyphosis. A surgeon can usually achieve 5-10° of sagittal correction with each Smith-Petersen osteotomy; additional correction is limited by anatomical constraints of the anterior column.
More recently, pedicle subtraction osteotomy (PSO) has emerged as an effective alternative. This is a single-stage posterior procedure that affects all three columns of the spine. A PSO can usually produce 30-40° of lordosis at each level at which osteotomy is performed and, when complete, results in bone-on-bone contact throughout all three columns of the spine9,10,13). Unfortunately, the procedure is technically much more demanding than the Smith-Petersen osteotomy, so PSO is not commonly performed despite the fact that PSO can better restore lumbar lordosis and improve sagittal balance. Only a few studies have reported outcomes and complications associated with the procedure1,3,8,16). The purpose of the present study was to review long-term outcomes and complications seen in our 13 consecutive patients who underwent thoracic or lumbar PSO.
MATERIALS AND METHODS
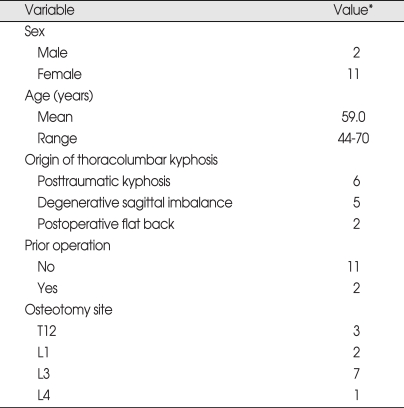
Thirteen consecutive adult patients on whom the senior spine surgeon (S.C.R.) performed PSO for fixed sagittal imbalance between December 1999 and January 2006 were enrolled. All patients complained of deformities and back pain before surgery. They were resistant to conservative treatment including physical therapy, medication, back muscle exercises, and wearing a brace for 3 months or more. The median follow-up period was 73 months (range 41-114 months). Six cases of posttraumatic kyphosis, five patients with degenerative sagittal imbalance, and two postoperative flat back syndrome patients were included in the study (Table 1). The patients included were 11 women and 2 men; the median age was 59 years (range 44-70 years).
Table 1.
Characteristics in 13 consecutive PSO-treated patients
*Values represent the number of patients, unless otherwise indicated. PSO : pedicle subtraction osteotomy
Clinical assessment and radiographic analysis
Clinical data were collected by retrospective chart review. Details on intraoperative blood loss, surgical complications, postoperative clinical courses, and medical complications, were of particular interest. Intraoperative neurophysiologic monitoring (somatosensory-and motor-evoked potentials; SEPs and MEPs, respectively) data were reviewed retrospectively. Oswestry Disability Index (ODI) scores obtained before and after surgery, in a prospective manner, were analyzed. Subjective satisfaction evaluation of final surgical results was classified by patients as one of the following : aggravated, no change, or improved; for back pain, leg pain, and stooping symptoms. Each patient was questioned and his or her responses were recorded by a spinal surgeon not involved in the procedure. All complications were noted and assigned to one of three categories : intraoperative, perioperative (< 2 weeks after surgery), and late-onset postoperative (> 2 weeks after surgery).
Long-cassette (14 × 36 inch) anteroposterior and lateral standing plain radiographs obtained before surgery, immediately following surgery, and at the most recent follow-up examinations, were analyzed retrospectively. The instrumented levels and sites of osteotomy were recorded. Global balance was assessed using C7 sagittal plumb lines. The extent of thoracic kyphosis was measured from T5 to T12, and that of lumbar lordosis was measured from the upper endplate of T12 to the endplate of S1, whereas the PSO angle assessing local curvature was measured between the level above and the level below osteotomy. The proximal junctional angle is defined as the angle between the caudal endplate of the uppermost instrumented vertebrae (UIV) to the cephalad endplate of the two supra-adjacent vertebrae above the UIV. Proximal junctional kyphosis (PJK) is a proximal junctional angle more than 10° and at least 10° greater than the preoperative value. Collection and review of clinical data and radiographic assessments did not involve either of the two operating surgeons.
Operative procedure and postoperative course
Our decision policy of PSO level depended on the site of the most significant pathological entity. For instance, lumbar PSO was indicated for the treatment of iatrogenic lumbar flat back syndrome and degenerative global sagittal imbalance, whereas thoracic PSO was indicated for isolated thoracic kyphosis such as posttraumatic kyphosis. PSOs was performed on patients for whom posterior osteotomies alone would be inadequate, as at least 30° of corrective lordosis was required to correct their sagittal imbalances. Osteotomy was performed on the lumbar spine in most cases, typically at L3. The osteotomy size was based on preoperative standing radiograph measurements of sagittal imbalance, with the surgical goal being restoration of normal sagittal balance with the C7 plumb line falling at or within 4 cm of the posterior-superior corner of S1. A multi-segmental pedicle screw technique was used for posterior spinal instrumentation. All patients were positioned prone on a Jackson frame and were continuously monitored using SEPs and MEPs.
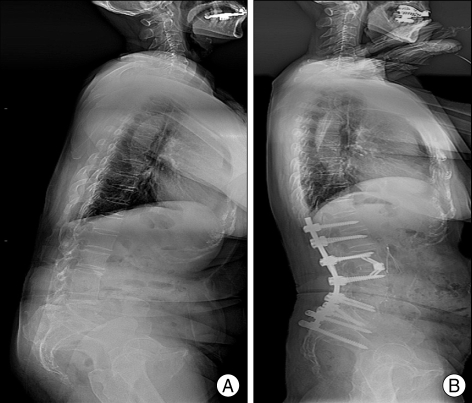
Although various descriptions of PSO exist, the first step in the technique used in the current study consisted of removing all posterior elements at the level of planned correction, including the spinous process, the lamina, and the superior and inferior facets adjacent to the pedicle. In addition, the cephalad and caudal laminae were undercut to avoid iatrogenic canal stenosis during osteotomy closure. Next, pedicles were taken down to the level of the posterior vertebral body. The vertebral body was then decancellated through each pedicle. In most instances, a temporary rod was placed across the osteotomy site to prevent subluxation or premature osteotomy closure. A wedge-shaped portion of the lateral vertebral body walls was removed through the pedicle. A reverse-angled curette or Woodson elevator was used to thin and fracture the posterior cortex of the vertebral body underlying the spinal canal into the wedge-shaped defect. A posterior compression force was applied to the spine facilitating spinal hyperextension across the osteotomy site hinging on the anterior margin of the vertebral body. Typically, this maneuver was performed by changing the bolsters on the Jackson frame to allow extension across the osteotomy, with further compression and correction obtained using compression techniques across the posterior instrumentation. With every step of correction/compression, careful attention was paid to ensure the central canal and exiting nerve roots were not compressed. After ensuring that exiting nerve roots were free, the final spinal contour was maintained with segmental rod fixation for which cantilever forces were employed. After completing the fixation procedure, autografts and allografts were placed over the laminae, facet joints, and transverse processes. Anterior-column support is known to decrease the pseudarthrosis rate associated with long-segment posterior fusions. In all cases where fusions extended to the sacrum, anterior column support was provided at L5-S1 by a transforaminal lumbar interbody fusion or an anterior lumbar interbody fusion (Fig. 1). In patients with severe osteopenia/osteoporosis or in those with histories of pseudarthrosis, a demineralized bone matrix was placed to supplement fusion.
Fig. 1.
A representative example of pedicle subtraction osteotomy (PSO) for fixed sagittal imbalance patients. A : Lateral long-cassette standing radiograph of a 60-year-old woman who presented with severe lower back pain and a stooping gait revealed global degenerative sagittal imbalance. B : The patient underwent L4 PSO with anterior column support, and the plain film obtained at her most recent follow-up examination shows dramatic improvement in lumbar kyphosis.
A 3- to 6-month course of thoracolumbosacral orthosis or lumbosacral orthosis with a thoracic extension pad was typically prescribed for any patient in whom the PSO was supported only by segmental posterior instrumentation. In any patient whose construct was supplemented by an anterior column interbody fusion, either no orthosis was suggested, or a supportive lumbosacral corset was worn for 1 to 3 months.
Statistical analysis
For statistical analysis, SPSS software (version 12.0; 2003; SPSS, Inc., Chicago, IL, USA) was used. The Mann-Whitney U test was employed for analysis of differences in noncategorical variables between intraoperative factors and neurological complications. For comparison between two groups with assumed unequal variance (that is, thoracic and lumbar PSO patients) the heteroscedastic t-test was used. Intra- and inter-observer measurement reliabilities were estimated using kappa statistics. A p-value less than 0.05 was considered statistically significant.
RESULTS
Surgical outcomes
PSOs were performed at the following levels : T12 in three patients, L1 in two patients, L3 in seven patients, and L4 in one patient (Table 1). The numbers of fused vertebrae ranged from 4 to 10 (average 5.8). The mean operation time was 6 hours 25 minutes (range 4 hours 35 minutes to 9 hours 10 minutes), and the mean operative blood loss was 2,984 mL (range 1,000-5,500 mL). In most patients, blood transfusions were usually needed perioperatively.
Radiological outcomes and measurement reliabilities
The mean correction angle at the PSO site was 31.5 ± 9.6°. The mean correction angle after PSOs performed at lumbar vertebrae (34.4 ± 10.1°) was significantly greater than the average correction angle after PSOs performed at thoracic vertebrae (25.8 ± 8.2°) (p = 0.022). Thoracic kyphosis increased from 22.0 ± 11.4° preoperatively to 25.5 ± 16.3° postoperatively (p = 0.076). Lumbar lordosis increased significantly from -14.1 ± 20.5° preoperatively to -46.3 ± 12.8° postoperatively (p < 0.0001) (Table 2). The C7 plumb line value decreased significantly from 115 ± 43 mm to 32 ± 38 mm (p < 0.0001). The prevalence of PJK was 23% (3 of 13 patients).
Table 2.
Summary of preoperative and follow-up radiographic measurements
*PSO angle represent the local Cobb angle measured from one level above to one level below the PSO site. SDs : standard deviations, F/U : follow-up, PSO : pedicle subtraction osteotomy
All measurements were performed at least three times by two surgeons to ensure accuracy and reliability. The margins of inter-observer and intra-observer error were plus-or-minus 1.8 ± 0.7° and 1.3 ± 0.5°, respectively. Intra-observer agreement between the two readers was "excellent", with kappa values ranging from 0.908 to 0.954. Inter-observer agreement was expected to be relatively lower than intra-observer agreement; however, this was also "excellent", with kappa values ranging from 0.825 to 0.843.
Clinical outcomes
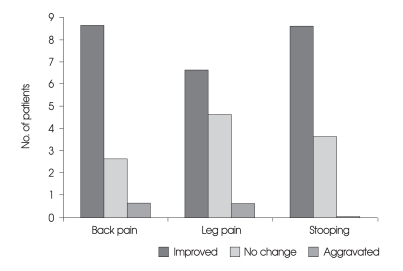
Ten of the 13 patients (76.9%) completed ODI questionnaires before and after surgery. The average preoperative ODI score was 55.4 ± 13.6, and the mean postoperative ODI score 30.2 ± 16.5. Improvement after surgery was statistically significant (p < 0.001). Subjective evaluation of back pain showed that nine patients perceived improvement, three no change, and one an aggravation (Fig. 2). Outcome of leg pain demonstrated that seven patients perceived improvement, five no change, and one an aggravation. The patients who experienced suboptimal outcome of leg pain had arthralgic pain rather than neuralgic. Subjective assessment of stooping symptoms showed that no patient perceived a result as aggravated even if the patient experienced PJK or rod fracture. Statistical analysis revealed that ODI score reduction was significantly related to the postoperative C7 plumb line value (p = 0.003), but not to lumbar lordosis, thoracic kyphosis, or PJK.
Fig. 2.
Subjective satisfaction evaluation of final surgical results showing acceptable clinical outcomes.
Operative complications
No patient died or became permanently paraplegic as a result of surgery. Surgery was associated with 16 complications in 8 patients (61%) (Table 3); there were 3 intraoperative complications, 3 perioperative complications, and 10 late-onset postoperative complications. Complication rates were significantly higher in patients who rated clinical outcomes as aggravated or unchanged than in patients who rated outcomes as improved (p = 0.012).
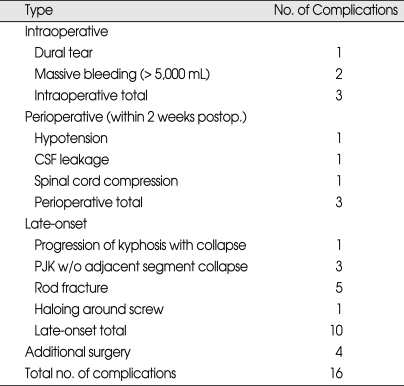
Table 3.
Summary of 16 PSO complications in 13 patients
PSO : pedicle subtraction osteotomy, CSF : cerebrospinal fluid, PJK : proximal junctional kyphosis, w/o : without
Intraoperative complications
One patient experienced a dural tear, which was successfully treated by primary suture closure with 6-0 monofilament nylon without additional surgical repair or wound infection. Massive bleeding (> 5,000 mL) occurred in two patients (15%) without any accidental damage to major blood vessels. It happened during the decancellation of vertebral body. At preoperative laboratory analysis, these patients had shown normal bleeding times. The operation times for these patients were more than 7 hours. Blood loss was significantly related to the numbers of levels fused (p = 0.015). Blood loss did not differ significantly by kyphosis etiology (traumatic or degenerative, p = 0.372).
Perioperative complications
Three perioperative complications (within 2 weeks postoperatively) were seen. Transient paraplegia resulting from spinal cord compression caused by a bone fragment occurred in one patient, requiring urgent additional surgery to remove the fragment of bone; intraoperative neuromonitoring of SEPs and MEPs had not detected the problem. The bone fragment was a retropulsion from the posterior wall of vertebral body. After the second operation, muscle power gradually recovered to normal at final follow-up. This patient also experienced cerebrospinal fluid (CSF) leakage, which was successfully treated using lumbar drainage with no wound problem. In one patient with intraoperative massive bleeding, postoperative hypotension (systolic blood pressure < 80 mmHg) was noted. After therapy in intensive care unit, blood pressure gradually recovered to normotensive levels during follow-up.
Late-onset complications
A total of ten late-onset postoperative complications (more than 2 weeks postoperatively) occurred. Late-onset kyphosis progression occurred in four patients (30%). One patient suffered collapse of the lower junctional vertebrae and three experienced PJK without collapse outside of the fusion segments. Two patients had degenerative conditions, and two had suffered traumatic injuries; none of these four patients needed additional surgery for kyphosis correction. Among these four cases, three were asymptomatic (10° < PJK < 20°) and the only symptomatic patient (PJK > 20°) was readily compliant with medication and external orthosis. In our series, clinical outcomes were not adversely affected by PJK. Patients with late progression of kyphosis (mean age 61.7 ± 6.2 years) were older than those without progression (mean age 57.7 ± 12.5 years) (p = 0.068). There was no significant correlation between late-onset progression of kyphosis and assessed parameters including preoperative C7 plumb line, lumbar lordosis, thoracic kyphosis, and PSO angle.
Six instrumentation failures occurred in four patients. Five rod breakages occurred outside of the osteotomy sites and were caused by pseudarthrosis of the posterolateral fusions. In one patient, halos around the S1 screws were seen at the caudal end (Fig. 3). Loose screws were replaced, the posterior construct was extended to include iliac screws, and interbody grafts were inserted to support anterior columns, as required.
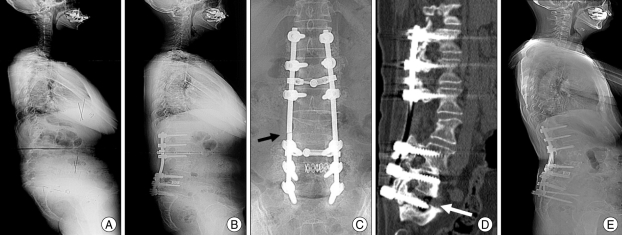
Fig. 3.
Preoperative (A) and postoperative (B-E) radiographs of a 62-year-old woman. The patient presented with intolerable lower back pain and stooping symptoms. B : Pedicle subtraction osteotomy at L3, transforaminal interbody fusion at L4-5, and a posterior fusion from T12 to S1, were performed. C and D : Three years postoperatively, rod fracture (black arrow) and haloing (white arrow) around the S1 screws occurred. E : Loose screws were replaced, the posterior construct was extended to include iliac screws, and interbody grafts were inserted to support the anterior column.
DISCUSSION
In the present study of 13 consecutive patients with fixed sagittal imbalance treated by PSO over a 7-year period (with a minimum follow-up time of 41 months), the incidence of intraoperative and postoperative neurological deficits was 7.6% (1 of 13 patients). There were no reports of permanent deficits (0 of 13 patients). We observed surgery-related complications in 8 of 13 patients (61%). Despite these complications, overall improvements in ODI scores and subjective satisfactory assessments were noted after surgery, including in patients with surgery-related complications. Several studies have reported complications of the PSO technique. Bridwell, et al.3) found that, in a series of 33 consecutive patients, 5 patients experienced transient neurologic deficits, giving an overall incidence of 15.2%. No patients had permanent deficits in the cited series, and, despite the complications, the authors reported significant improvements in overall ODI and pain scores, in which is consistent with the results of the present study. Of 83 patients treated, Ahn et al.1) found intraoperative complications in 25 and postoperative complications in 38.
Surgical and medical complications in earlier reports have included hypotension resulting from intraoperative massive bleeding, CSF leakage, neurological injury, wound-related problems, and nosocomial infections4,16). In our series, massive bleeding occurred in two patients with preoperative normal laboratory findings. An option to reduce the large blood loss known to be associated with all PSOs is vertebral body embolization, but this strategy awaits further clinical validation. In the present study, one patient experienced transient paraplegia because a bone fragment caused spinal cord compression that was not detected by intraoperative neuromonitoring. In a previous analysis of 45 patients with ankylosing spondylitis, Kim et al.11) found transient postoperative radiculopathy in four patients and spinal cord compression caused by a bone fragment at T12 in one patient. Although it is unclear what mechanisms were responsible for development of neurologic deficits in most previous reports, the problems were thought to arise from a com-bination of subluxation, residual dorsal impingement, dural buckling, and spinal cord ischemia1,4,16). To reduce the risk of intraoperative or postoperative neurologic deficits, some authors recommend central canal enlargement, careful osteotomy closure to prevent subluxation across the osteotomy site, limited osteotomy at the level of the spinal cord or conus medullaris, a wake-up test after osteotomy closure, and examination of all motor groups following surgery1,3,4,16).
Most late-onset complications were related to kyphosis progression and instrumentation failure. There was a higher incidence of complications in patients with compression fractures, caused mainly by osteoporosis, compared with patients with degenerative changes. Correcting kyphosis after a compression fracture is associated with a high risk of additional compression fractures in adjacent vertebrae. Some researchers have studied complications after PSO using the combined anterior-posterior approach and have emphasized the need for anterior reconstruction3). In our series, however, late-onset segment collapse did not occur within fusion levels but at the lowest vertebra of the fusion segment. Thus, anterior support within the fusion segment would not have prevented collapse in our patient. We found the PJK prevalence on 3-year follow-up to be 23% and clinical outcomes were not adversely affected by PJK. We suggest that angular kyphosis of the thoracic and thoracolumbar junction may not always provoke pain. Kim et al.12) reported that 62 (39%) of 161 adult spinal deformity patients with segmental posterior spinal instrumented fusions were diagnosed with PJK at an average of 7.8 years postoperative follow-up. As in our series, self-reported patient satisfaction was not adversely affected by PJK.
In one patient, halos around screws were seen at the caudal end. The inferior fixation points bear the greatest proportion of the cantilever forces generated by the posterior construct. The lumbar vertebrae are mobile and are considerably more weight-bearing than the thoracic vertebrae, which are additionally sustained by the rigid rib cage. Furthermore, the lumbosacral spine has a complex local anatomy, unique biomechanical forces, and poor bone quality in the sacrum14). These factors may contribute to increased rates of pseudarthrosis and rod fracture in this spinal region. We used titanium rods as replacements in all cases of rod breakages. Several investigators have noted that titanium rods have the advantages of magnetic resonance imaging compatibility and increased rigidity, but are prone to microfracture propagation and are notch-sensitive in bending6,16). Stainless steel rods are thus used in most patients, except for those with infections or tumors. With increasing experience, some groups, including ours, have found that supplementation of a posterior construct with anterior column support markedly decreased the pseudarthrosis rate after lumbar PSO. The cantilever forces that the posterior spinal construct must resist become more significant as PSOs become more caudal; this probably explains the increased incidence of loose or broken screws at the inferior aspects of spinal constructs after lumbar PSO.
One of the weaknesses of this study might be the somewhat heterogenous diagnostic categories. However, the surgeries, types of implants, and surgical goal were all relatively uniform. Therein, the goals and treatments were uniform in that the indication for surgical treatment was their spinal deformity as opposed to a purely degenerative or traumatic etiology.
CONCLUSION
Intraoperative or postoperative neurologic deficits are relatively common following PSO. Most late-onset complications in our patients were related to kyphosis progression and instrumentation failure. However, clinical outcomes were not adversely affected by PJK. Correcting the C7 plumb line value, with minimal operative complications, seemed to lead to better clinical results.
Acknowledgements
The authors give special thanks to Dr. Youngjung J. Kim, orthopaedic surgeon, Spine service, Columbia University, School of Medicine, New York, USA and Dr. Young-Bae Kim, orthopaedic surgeon, Bohun Medical Center, Seoul, Korea, for invaluable assistance and kind support.
References
- 1.Ahn UM, Ahn NU, Buchowski JM, Kebaish KM, Lee JH, Song ES, et al. Functional outcome and radiographic correction after spinal osteotomy. Spine (Phila Pa 1976) 2002;27:1303–1311. doi: 10.1097/00007632-200206150-00011. [DOI] [PubMed] [Google Scholar]
- 2.Booth KC, Bridwell KH, Lenke LG, Baldus CR, Blanke KM. Complications and predictive factors for the successful treatment of flatback deformity (fixed sagittal imbalance) Spine (Phila Pa 1976) 1999;24:1712–1720. doi: 10.1097/00007632-199908150-00013. [DOI] [PubMed] [Google Scholar]
- 3.Bridwell KH, Lewis SJ, Edwards C, Lenke LG, Iffrig TM, Berra A, et al. Complications and outcomes of pedicle subtraction osteotomies for fixed sagittal imbalance. Spine (Phila Pa 1976) 2003;28:2093–2101. doi: 10.1097/01.BRS.0000090891.60232.70. [DOI] [PubMed] [Google Scholar]
- 4.Buchowski JM, Bridwell KH, Lenke LG, Kuhns CA, Lehman RA, Jr, Kim YJ, et al. Neurologic complications of lumbar pedicle subtraction osteotomy : a 10-year assessment. Spine (Phila Pa 1976) 2007;32:2245–2252. doi: 10.1097/BRS.0b013e31814b2d52. [DOI] [PubMed] [Google Scholar]
- 5.Casey MP, Asher MA, Jacobs RR, Orrick JM. The effect of Harrington rod contouring on lumbar lordosis. Spine (Phila Pa 1976) 1987;12:750–753. doi: 10.1097/00007632-198710000-00007. [DOI] [PubMed] [Google Scholar]
- 6.Dick JC, Bourgeault CA. Notch sensitivity of titanium alloy, commercially pure titanium, and stainless steel spinal implants. Spine (Phila Pa 1976) 2001;26:1668–1672. doi: 10.1097/00007632-200108010-00008. [DOI] [PubMed] [Google Scholar]
- 7.Farcy JP, Schwab FJ. Management of flatback and related kyphotic decompensation syndromes. Spine (Phila Pa 1976) 1997;22:2452–2457. doi: 10.1097/00007632-199710150-00025. [DOI] [PubMed] [Google Scholar]
- 8.Ikenaga M, Shikata J, Takemoto M, Tanaka C. Clinical outcomes and complications after pedicle subtraction osteotomy for correction of thoracolumbar kyphosis. J Neurosurg Spine. 2007;6:330–336. doi: 10.3171/spi.2007.6.4.8. [DOI] [PubMed] [Google Scholar]
- 9.Jaffray D, Becker V, Eisenstein S. Closing wedge osteotomy with transpedicular fixation in ankylosing spondylitis. Clin Orthop Relat Res. 1992:122–126. [PubMed] [Google Scholar]
- 10.Jang JS, Jung BJ, Lee SH. Pedicle subtraction and extension wedge osteotomy for the correction of fixed kyphotic deformity of the lumbar spine : technical note. J Korean Neurosurg Soc. 2003;33:230–233. [Google Scholar]
- 11.Kim KT, Suk KS, Cho YJ, Hong GP, Park BJ. Clinical outcome results of pedicle subtraction osteotomy in ankylosing spondylitis with kyphotic deformity. Spine (Phila Pa 1976) 2002;27:612–618. doi: 10.1097/00007632-200203150-00010. [DOI] [PubMed] [Google Scholar]
- 12.Kim YJ, Bridwell KH, Lenke LG, Glattes CR, Rhim S, Cheh G. Proximal junctional kyphosis in adult spinal deformity after segmental posterior spinal instrumentation and fusion : minimum five-year follow-up. Spine. 2008;33:2179–2184. doi: 10.1097/BRS.0b013e31817c0428. [DOI] [PubMed] [Google Scholar]
- 13.Murrey DB, Brigham CD, Kiebzak GM, Finger F, Chewning SJ. Transpedicular decompression and pedicle subtraction osteotomy (eggshell procedure) : a retrospective review of 59 patients. Spine (Phila Pa 1976) 2002;27:2338–2345. doi: 10.1097/00007632-200211010-00006. [DOI] [PubMed] [Google Scholar]
- 14.Peretz AM, Hipp JA, Heggeness MH. The internal bony architecture of the sacrum. Spine (Phila Pa 1976) 1998;23:971–974. doi: 10.1097/00007632-199805010-00001. [DOI] [PubMed] [Google Scholar]
- 15.Smith-Petersen MN, Larson CB, Aufranc OE. Osteotomy of the spine for correction of flexion deformity in rheumatoid arthritis. Clin Orthop Relat Res. 1969;66:6–9. [PubMed] [Google Scholar]
- 16.Yang BP, Ondra SL, Chen LA, Jung HS, Koski TR, Salehi SA. Clinical and radiographic outcomes of thoracic and lumbar pedicle subtraction osteotomy for fixed sagittal imbalance. J Neurosurg Spine. 2006;5:9–17. doi: 10.3171/spi.2006.5.1.9. [DOI] [PubMed] [Google Scholar]