Abstract
The Problem
Community health centers (CHCs) are part of the United States’ medical care safety net. Cost effectiveness is a critical element of value in today’s health policy environment. Not all cost-effectiveness studies employ formal peer-reviewed methodologies. A review of the literature on CHCs’ cost effectiveness is necessary to assess whether a higher level of evidence is needed to guide future policy.
Purpose
We sought to review the quality of the evidence on the economic value of CHCs and indicate whether a higher of level evidence would be useful for making policy.
Key Points
Evidence exists to support the general value of care in CHCs, but no evidence comes from formal economic evaluations of CHC care.
Conclusion
More formal cost-effectiveness evaluations would enhance the economic argument for CHCs but will remain difficult to conduct and may be unnecessary in light of other work on the value of care in CHCs.
Keywords: health facilities, health services research, uncompensated care, delivery of health services, health care quality access and evaluation
CHCs are and have been an important part of the United States’ health care safety net for more than 40 years.1 Indeed, society has invested in CHCs through government grants and private philanthropy; payments for services must be presumed to be worthwhile. Looking to the future, potential community health partners need to know whether empirical studies demonstrate the value of CHCs to society or the communities they serve. The answer depends in part on what is meant by value.
Throughout CHCs’ 40-year history, health policy making has often focused on whether value is being obtained from a treatment, intervention, or care system. Although the meaning of value encompasses more than economic outcomes, cost effectiveness is a critical element of value in today’s health policy environment. At a conceptual level, an intervention’s being cost effective indicates sufficient positive outcomes for the money being spent. However, cost effectiveness also refers to a set of formal methods that can be used to facilitate a structured, systematic comparison of treatments, interventions, and care systems.
Formal cost-effectiveness analyses use standard, state-of-the-art methods that facilitate comparisons not only among public health interventions within a study but also across studies. Although the U.S. government has never established standards for cost-effectiveness methods to guide policy, standards have been established by managed care pharmacy,2 and an expert panel made recommendations based on the state of the art in 1996.3
The panel’s recommendations can be used to judge the quality of data, assumptions, and methods used in cost-effectiveness studies related to CHCs. A review of the literature on CHCs’ cost effectiveness indicates whether more formal evidence is necessary to enhance the rationality of policy making process regarding the resource needs of CHCs.
CONCEPTUAL MODEL
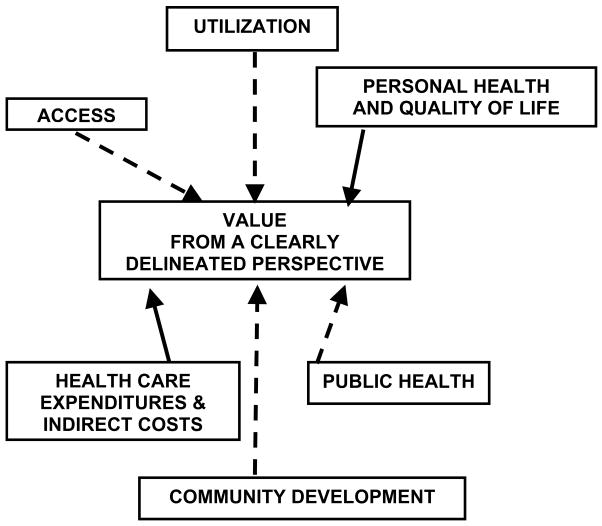
Figure 1 shows several effects of programs at CHCs. Each could be considered a component of the value proposition for interventions at CHCs. In business, value proposition has been defined as “the complete customer experience, including products, services, and any interaction with the company.”4 In health policy and intervention implementation, value proposition could be reinterpreted as meaning “the complete effects of a policy or intervention.” The value proposition, considered from whatever perspective an interest group or decision maker might take, can be incorporated into the process of allocating resources to CHCs.
Figure 1.
Components of the value proposition for community health center interventions being considered or implemented.
The effects of CHCs in the value proposition include, but are not limited to, economic components. The most basic noneconomic component of value is CHCs’ ability to enhance access. Access alone provides little indication of how CHCs affect the health of the community, and effects that are closer to community health and expenditures on health care play a larger role in the policy making process. Therefore, it is important to note that access to care can facilitate utilization of care, and utilization can affect individuals’ personal health and health-related quality of life. Improvements in individuals’ health contribute to the public’s health. Improvements in personal and public health facilitate community development. All other components of the value proposition can affect expenditures. Analysts can assess components of the value proposition from a variety of perspectives indicating whose costs and benefits matter. Perspectives include societal (everyone’s costs and benefits), the CHCs’ alone, public payers’ more generally, or the local community’s.
All components of value are relevant to a general value proposition and thinking of something as “cost effective.” All should be considered in decisions about policy and implementation. However, trying to review the literature on all components of value would be a nearly impossible task. Formal cost-effectiveness analyses focus almost exclusively on health and health-related quality of life and expenditures. These analyses provide a structured way to address two components of value. These components are connected to “value from a clearly delineated perspective” by solid lines in Figure 1 and are the focus of the review.
A study’s ability to add to the body of knowledge about the cost-effectiveness of CHCs is determined in part by the degree to which it conforms to methodological standards. Although formal criteria for judging such studies have been developed, the criteria were not designed for CHCs. Answers to several questions would facilitate formal cost-effectiveness analyses of, policy making for, and implementation of programs in CHCs.
Is the care provided at CHCs at least as effective as care outside CHCs? Without further defining effectiveness, this could span multiple components of the value proposition conceptual model.
Is the measure of effectiveness a process measure (like access or utilization), a clinical measure of health, or something that can be translated directly into health-related quality of life and a budget impact?
Were effectiveness and costs measured over the short term or the long term? Can short-term outcomes be linked to long-term changes in health, quality of life, disability, and costs?
Were the results presented from the payer’s perspective, the patient’s perspective, or the societal perspective? Can the results inform one of these perspectives?
METHODS
The published literature describing the components of the value proposition most directly related to the formal cost-effectiveness analyses of CHCs was reviewed by searching PubMed using the terms “cost effectiveness OR cost benefit” and “community health center OR federally qualified health center OR CHC OR FQHC.” Given the rapid rate of change in health care costs, articles published more than 5 years ago are unlikely to provide useful information about the formally assessed cost effectiveness of care provided at CHCs at present. Of these, only articles written in English focusing on health centers in the United States and performing empirical analyses were examined further. Reviews were examined to obtain published references that may have been missed in the PubMed search.
For each study, the review notes whether the study actually was a formal cost-effectiveness analysis. If not, the review notes the components of the value proposition that were addressed. Finally, the review notes what other measures or modeling (e.g., relating better primary care to better health outcomes) would be necessary to use the results as inputs in a formal cost-effectiveness analysis.
RESULTS
Using the search criteria in the Methods section, 179 articles were found dating back to 1973. Only 52 were published in the last 5 years. Of these 52, 4 were not written in English and 15 were on international topics. Of the 33 remaining, 10 were either nonempirical or only case studies or pilot work. None were formal cost-effectiveness analyses.
Several of the 179 articles were reviews. These were examined to identify articles that focused at least partially on the conceptual model of the value proposition for CHCs shown in Figure 1. The published work by Proser as well as a National Association of Community Health Centers white paper served as the basis for identifying articles in the past five years that dealt with economic outcomes (primarily the cost of care) in CHC settings.5,6 The reviews support a favorable value proposition for CHCs; the components of proposition have not been evaluated in a formal cost-effectiveness analysis.
Table 1 provides a summary of the articles included in the review, listing the author and year, the component of the value proposition that is discussed, and a summary of the data and modeling that would need to be added to use the results in a formal cost-effectiveness analysis.
Table 1.
Summary of Evidence
| Authors | Year | Components Of Value Proposition Discussed | Steps Necessary to Translate into a Formal Cost-Effectiveness Analysis |
|---|---|---|---|
| Hadley and Cunningham7 | 2004 | Access (decreased unmet need) | Place dollar value on care at CHC |
| Utilization (less emergency care) | Place dollar value on reduced emergency care | ||
| Public health | Place dollar and health-related quality of life value on decreased unmet need | ||
| Project from short-term to long-term effects | |||
| Epstein8 | 2001 | Access (fewer avoidable hospitalizations) | Place dollar value on care at CHC |
| Health (fewer avoidable hospitalizations) | Place dollar value on avoided preventable hospitalization | ||
| Public health | Translate short-term effects on health-related quality of life into long-term effects on health-related quality of life and economic productivity | ||
| Falik et al.9 | 2001 | Access (fewer avoidable hospitalizations for Medicaid population) | Place dollar value on care at CHC |
| Health (fewer avoidable hospitalizations for Medicaid population) | Place dollar value on avoided preventable hospitalization | ||
| Public health | Translate short-term effects on health-related quality of life into long-term effects on health-related quality of life and economic productivity | ||
| Starfield and Shi10 | 2004 | Utilization (better primary care) | Place dollar value on care at CHCs |
| Place health-related quality of life value on better primary care | |||
| Translate short-term effects into long-term effects | |||
| Porterfield and Kingsinger11 | 2002 | Utilization (better process of care) | Place dollar value on care at CHCs |
| Place dollar value on care outside CHCs | |||
| Place health-related quality of life value on improved process of care | |||
| Translate short-term effects into long-term effects | |||
| Carlson et al.12 | 2001 | Access (uninsured at CHCs more likely to have a usual source of care) | Place dollar value on care at CHCs |
| Utilization (uninsured at CHCs have more regular contact with physicians) | Place health-related quality of life value on more regular contact with physician | ||
| Translate short-term effects into long-term effects | |||
| Ulmer et al.13 | 2000 | Utilization (better process of care) | Place dollar value on care at CHCs |
| Place dollar value on care outside CHCs | |||
| Place health-related quality of life value on improved process of care | |||
| Translate short-term effects into long-term effects | |||
| Klein et al.14 | 2001 | Utilization (better preventive care and counseling) | Place dollar value on care at CHCs prior to guideline implementation |
| Place dollar value on care at CHCs after guideline implementation | |||
| Place health-related quality of life on improved preventive care and counseling | |||
| Translate short-term effects into long-term effects | |||
| Hunt15 | 2005 | Community development (wages, entry level jobs, career ladders) | Place dollar value on the resources used to run CHCs |
| Place dollar value on the short-term and long-term impacts of community development associated with CHCs’ presence |
CHC, community health center
Hadley and Cunningham reported that uninsured patients’ proximity to federally qualified health centers (FQHC) was associated with lower levels of unmet need and decreased utilization of emergency care.7 This result holds whether the patient actually used the FQHC. This is not a formal cost-effectiveness analysis, but provides information on the access and utilization components of the value proposition and information relevant to public health. To be used as an input into a formal cost-effectiveness analysis, the results need to be translated into health and expenditure values of decreased unmet need and use of emergency care. Placing dollar values on the care provided at the CHC and the decreased use of emergency care would be relatively straightforward. A dollar and health value also need to be associated with reduced unmet need. Untreated depression provides a useful example of the effects of unmet need; it can lead to increased morbidity and lower functional status. The former imposes direct costs on the health care system because it is more costly to treat more severe depression. The latter imposes indirect costs on society; depression reduces worker productivity and lowers quality of life. Both affect health-related quality of life. Formal cost-effectiveness analyses value all these effects. To move from short-term to long-term effects of the findings, the effects of keeping adults and children healthier would need to be projected. Healthier adults are likely to be more economically productive. Healthier children are likely to have improved long-term educational attainment, higher economic productivity, and better health outcomes in adulthood.
Epstein8 reported that patients in areas served by a CHC had 5.8 fewer preventable hospitalizations per 1000 individuals over a 3-year period compared with similar patients in areas not served by a CHC. A reduction in preventable hospitalizations is an indication of greater access to primary care, preventive care, and outpatient care for chronic conditions. Communities with lower rates of preventable hospitalizations are presumed to have better systems of outpatient care. To use these results in a formal cost-effectiveness analysis, it would be necessary to assess the cost of CHC care, translate the avoided hospitalizations into reduced expenditures, and link the short-term improvements in health to long-term improvements in health-related quality of life.
Falik and colleagues9 found that Medicaid patients who received their care from CHCs were less likely to have avoidable admissions. The components of the value proposition with which these results are associated and the steps that would be necessary to use these results in formal cost-effectiveness analysis are similar to those for Epstein’s article. Starfield and Shi10 found that populations in communities with health centers obtain better primary care than populations in communities without health centers. To use these results in a formal cost-effectiveness analysis, the cost of the care at CHCs would need to be projected along with the health-related quality of life effects of better primary care. All results would need to be projected to the long-term.
Porterfield and Kinsinger11 examined the effect of CHC care on CHC patients. These authors abstracted medical records of diabetes patients in a sample of eight physicians’ offices and three CHCs. Their results indicated that diabetes patients at CHCs were more likely to have appropriate values for four of six process measures of quality of care. Process is most closely linked with utilization in the value proposition. To use the results in a formal cost-effectiveness analysis, the costs of care in CHCs and non-CHC offices need to be compared. Further, the improved process of care needs to be linked to improved health-related quality of life. Finally, short-term results need to be translated into long-term outcomes.
Carlson and co-workers12 found that uninsured users of CHCs were more likely to have a usual source of care and more likely to have regular contact with physicians. These reflect the access and utilization components of the value proposition. The results from this study can be used in a formal cost-effectiveness analysis if a cost is applied to the care at CHCs, the more regular contact with a physician is translated into health-related quality of life, and the short-term effects of improved access and utilization are translated into long-term effects for costs and health-related quality of life.
Ulmer and associated13 reported that, based on process measures of care for four common conditions, CHCs provided care of quality at least as high as care provided in other settings. This study’s results could be used as inputs into a formal cost-effectiveness analysis by collecting extra data and making projections similar to those made for Porterfield and Kinsinger.11
Klein and co-workers14 showed that the implementation of Guidelines for Adolescent Preventive Services improved the receipt of preventive services for adolescents and the discussions between adolescents and providers for a whole list of topics. These results inform the access and utilization components of the value proposition for CHCs. To use the results of this pre- and postimplementation study to inform a formal cost-effectiveness analysis, costs of care without and with the guidelines would need to be compared. Further, long-term projections must be made of the effects of preventive services and better communication on health-related quality of life and expenditures. The effects of some types of counseling can be projected in a straightforward way. For example, counseling on responsible sexual behavior can lead to greater use of condoms, which can lead to a decrease in incidence of sexually transmitted infections, which affects quality of life and expenditures.
Only one study provided insight on the community development component of the value proposition.15 CHCs were described as economic engines—providing not only wages, but providing entry-level jobs, mentoring, and career ladders for local community members. This type of result is most easily translated into a cost–benefit analysis (where both costs and benefits are measured in dollars) rather than a cost-effectiveness analysis relying on dollar outcomes and health. Projections of the cost of using resources to fund CHCs and the dollar value of the improved community development would be necessary to use the results in a formal cost–benefit analysis.
DISCUSSION
In summary, evidence exists to support the value proposition for CHCs, but no evidence comes from formal cost-effectiveness studies. This surprising result holds although CHCs have been part of the safety net in the U.S. health care system over a period of time when economic considerations have been important. The best established components of a value proposition are access and utilization. Favorable findings for public health (e.g., reduced avoidable hospitalizations) and community development also are reported in the literature. The literature is weaker on health, health-related quality of life, and long-term changes in expenditures. Also, none of the prior studies carefully evaluate the costs of provide care in CHCs versus alternative settings. To move from a value proposition that allows us to think of CHCs as being conceptually “cost-effective” to a formal analysis of the cost-effectiveness of CHCs, costs must be assessed and the linkages must be made between process and other utilization measures and health outcomes.
Returning to the questions posed at the end of the section outlining the conceptual model, the care at CHCs has been shown to be at least as effective as care provided elsewhere. This finding is largely in terms of short-term process measures that have not been translated into long-term health-related quality of life outcomes necessary for state-of-the-art formal cost-effectiveness analyses. Limited aspects of public health and community development have been investigated. Costs have not been reported in most studies. Substantial modeling would be required to link the short-term process changes to long-term health-related quality of life and expenditure changes to use in formal economic analyses. The perspective of an analysis generally only applies to cost-effectiveness analyses, so this was not analyzed.
Given the importance of economic evaluation in today’s policy environment, researchers, policy makers, advocates, and those given the job of implementing CHC programs are left with two questions: (1) Why has so little been done to assess the cost-effectiveness of CHCs formally? and (2) Is this type of research is necessary for CHC policy making and implementation?
The dearth of research may be explained in part by the difficulty of assessing organizations’ cost effectiveness. Although some cost-effectiveness research has been done on organizations such as long-term care organizations,16 most cost-effectiveness research has been done on specific treatments. As an example, in contrast to the limited literature on CHCs, a search of “chronic obstructive pulmonary disease” and “cost effectiveness” yields 66 articles from 2005 alone.
The standards that have been set for cost-effectiveness evaluations of medical interventions may not be appropriate for evaluating CHCs. Standards for economic evaluation studies were set sufficiently high so that several years after the recommendations were released, even some general cost-effectiveness studies failed to follow basic recommendations.17 There would be many challenges to meeting the standards when evaluating CHCs. Making long-term epidemiological projections to link to cost and quality of life is difficult for care provided by CHCs because the CHC represents a piece of a system of care for multiple diseases experienced by multiple population subgroups. Earlier, the prevalence of literature on CHC cost effectiveness was compared with clinical cost-effectiveness literature. For most clinical conditions, there are many interventions or pharmaceutical products that can be analyzed individually or in combination. Each alternative often is dealing with only a specific condition. More complexity is found in an analysis of testing blood products prior to transfusion in which analysts had to model the incidence of hepatitis B, hepatitis C, and HIV.18 Modeling the effects of CHCs or the care provided at them would be even more complex because of the need for a diverse set of disease models. Further, users of CHCs face many other environmental factors that can affect their lives so that standard epidemiological models may not be valid for this population. Long-term epidemiological models specific to this population may need to be developed. Further, cost data can be difficult to summarize at any level more specific than that reported in standard administrative databases. Because CHCs obtain funds from multiple sources, trying to track their costs using the funds received from a single source would be meaningless. Determining which perspective to use is also difficult as the CHC population may be its users or may be the entire local population.
To facilitate formal cost-effectiveness analyses that can add structure to policy debates, future analyses of care at CHCs should extend beyond process measures. A formal cost-effectiveness analyses could provide transparent information about the economic value of care at CHCs. If such analyses prove to be impossible to conduct, the degree to which all components of the value proposition are understood can be described for all concerned. Even this will facilitate rational decision making. Although having an understanding of all components of the value proposition is not equivalent to adding formal cost-effectiveness analysis to the policy and implementation process, any additional structure is useful.
In conclusion, more formal cost-effectiveness studies could enhance the discussion of policy options for improved access to primary care in underserved areas. Policy makers have several options to achieve this goal: (1) establishing and supporting a CHC; (2) subsidizing private providers through bonus payments, debt relief, or exchanging service for educational funding; or (3) expanding health insurance coverage. Cost-effectiveness analyses, although continuing to be difficult to perform and needing to be supplemented by noneconomic considerations, will help in understanding whether the first option is most valuable.
Footnotes
This paper was written with the support of the Health Resources and Services Administration (HRSA) of the Department of Health and Human Services (DHHS). The views expressed by the authors do not necessarily reflect the policies of HRSA or DHHS.
References
- 1.Lewin ME, Altman S. America’s health care safety net: Intact but endangered. Washington, D.C.: Institute of Medicine, National Academy Press; 2000. [PubMed] [Google Scholar]
- 2.Tarn TYH, Smith MD. Pharmacoeconomic guidelines around the world. ISPOR CONNECTIONS. 2004;10(4):5–15. [Google Scholar]
- 3.Gold MR, Siegel JE, Russell LB, Weinstein MC, editors. Cost effectiveness in health and medicine. New York: Oxford University Press; 1996. [Google Scholar]
- 4.Selden L, MacMillan IC. Manage customer-centric innovation—systematically. Harv Bus Rev. 2006;84(4):108–16. 149. [PubMed] [Google Scholar]
- 5.Proser M. A nation’s health at risk II: A front row seat in a changing health care system. Washington, D.C.: National Association of Community Health Centers; 2004. [Google Scholar]
- 6.National Association of Community Health Centers. Studies of Health Center Cost Effectiveness. Available from: www.nachc.com/research/Files/HCCostEffectivenessStudies10.04.pdf.
- 7.Hadley J, Cunningham P. Availability of safety net providers and access to care of uninsured persons. Health Serv Res. 2004;39(5):1527–46. doi: 10.1111/j.1475-6773.2004.00302.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Epstein AJ. The role of public clinics in preventable hospitalizations among vulnerable populations. Health Serv Res. 2001;32(2):405–20. [PMC free article] [PubMed] [Google Scholar]
- 9.Falik M, Needleman J, Wells BL, Korb J. Ambulatory care sensitive hospitalizations and emergency visits: experiences of Medicaid patients using Federally Qualified Health Centers. Med Care. 2001;39(6):551–56. doi: 10.1097/00005650-200106000-00004. [DOI] [PubMed] [Google Scholar]
- 10.Starfield B, Shi L. The medical home, access to care, and insurance: A review of evidence. Pediatrics. 2004;113(5):1493–8. [PubMed] [Google Scholar]
- 11.Porterfield DS, Kinsinger L. Quality of care for uninsured patients with diabetes in a rural area. Diabetes Care. 2002;25(2):319–23. doi: 10.2337/diacare.25.2.319. [DOI] [PubMed] [Google Scholar]
- 12.Carlson BL, Eden J, O’Connor D, Regan J. Primary care of patients without health insurance by community health centers. J Ambul Care Manage. 2001;24(2):47–59. doi: 10.1097/00004479-200104000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Ulmer C, Lewis-Idema D, Von Worley A, Ridgers J, Berger LR, Darling EJ, et al. Assessing primary care content: four conditions common in community health center practice. J Ambul Care Manage. 2000;23(1):23–38. doi: 10.1097/00004479-200001000-00003. [DOI] [PubMed] [Google Scholar]
- 14.Klein JD, Allan MJ, Elster AB, Stevens D, Cox C, Hedberg VA, et al. Improving adolescent preventive care in community health centers. Pediatrics. 2001;107(2):318–27. doi: 10.1542/peds.107.2.318. [DOI] [PubMed] [Google Scholar]
- 15.Hunt JW. Community health centers’ impact on the political and economic environment: The Massachusetts example. J Ambul Care Manage. 2005;28(4):340–7. doi: 10.1097/00004479-200510000-00009. [DOI] [PubMed] [Google Scholar]
- 16.Grabowski DC. The cost-effectiveness of noninstitutional long-term care services: review and synthesis of the most recent evidence. Med Care Res Rev. 2006;63(1):3–28. doi: 10.1177/1077558705283120. [DOI] [PubMed] [Google Scholar]
- 17.Phillips KA, Chen JL. Impact of the U.S. panel on cost-effectiveness in health and medicine. Am J Prev Med. 2002;22(2):98–105. doi: 10.1016/s0749-3797(01)00409-3. [DOI] [PubMed] [Google Scholar]
- 18.Marshall DA, Kleinman SH, Wong JB, AuBuchon JP, Grima DT, Kulin NA, et al. Cost-effectiveness of nucleic acid test screening of volunteer blood donations for hepatitis B, hepatitis C and human immunodeficiency virus in the United States. Vox Sanguinis. 2004;86(1):28–40. doi: 10.1111/j.0042-9007.2004.00379.x. [DOI] [PubMed] [Google Scholar]