Abstract
Background
Previous studies have suggested that women with cardiovascular disease may receive less aggressive care than men. Using a large cardiology database from a tertiary referral center, we sought to determine if treatment differences still persist in the current era.
Methods
We analyzed data on 2462 patients who were referred for secondary prevention to the Preventive Cardiology Clinic at The Cleveland Clinic Foundation between 1997 and 2004. The primary objective was to evaluate use of effective secondary preventive therapies, by gender, as outlined in the ACC/AHA guidelines, such as antiplatelet therapy, beta-blockers, statins, and angiotensin-converting enzyme (ACE) inhibitors. Multivariate logistic regression analysis was performed to assess the independent effect of gender on all cause mortality.
Results
Women were older (62.2 ± 11.1 vs. 59.4 ± 11.0, p < 0.001) and more likely to be hypertensive (68.1% vs. 56.1%, p < 0.001) than men. Overall, women were more likely than men to have higher baseline C-reactive protein (CRP) (6.14 ± 13.4 vs. 4.9 ± 10.7, p < 0.001), low-density lipoprotein cholesterol (LDL-C) (135 ± 66 vs. 116 ± 46, p < 0.001), high-density lipoprotein cholesterol (HDL-C) (52 ± 17 vs. 41 ± 11, p < 0.001), and total cholesterol (238 ± 98 vs. 202 ± 65, p < 0.001). Women were less likely to be on antiplatelet therapy (76.6 % vs. 85.0%, p < 0.001) and statins or any lipid-lowering therapy (62.6% vs. 67.1%, p = 0.04) compared with men on presentation.
Conclusions
Even in the current era, women with established cardiovascular disease continue to receive less aggressive care than men. They are less likely to be on aspirin and statin therapy. More aggressive efforts should be made to treat both men and women with standard secondary preventive efforts.
INTRODUCTION
Despite advances in therapy, heart disease remains the leading cause of death among women and men in United States.1 In the last few years, there have been numerous studies that examined gender difference in presentation, diagnosis, and outcome in the setting of acute coronary syndromes.2–9 Most have focused on initial treatment strategies and procedures, such as cardiac catheterization and revascularization. However, there are few data on gender differences in guideline adherence in secondary prevention patients in the current era. Therefore, we sought to determine the effect of gender on adherence to recommended secondary preventive measures as stated in the 2006 American College of Cardiology and American Heart Association (ACC/AHA) Guidelines using a tertiary referral center database.10
MATERIALS AND METHODS
Study group
The study group consisted of women and men with a history of coronary artery disease (CAD), cerebrovascular disease (CVD), or documented peripheral vascular disease (PVD) who came to the Preventive Cardiology Clinic, a multidisciplinary clinic, at Cleveland Clinic between 1997 and 2004. All patients referred to the clinic who met secondary prevention criteria were included in these analyses. All patients included in our study met ACC/AHA class I guideline indications for blood pressure control, cholesterol control, antiplatelet, and lipid-lowering therapy11 and did not have contraindications to therapy. Patients were referred from cardiologists and general internists to treat risk factors for secondary prevention.
Data collection
Clinical and laboratory data were obtained at the time of the initial visit. We obtained data on traditional cardiovascular disease risk factors, including age, sex, body mass index (BMI), blood pressure, diabetes mellitus (DM), smoking, lipids, and family history of CAD as well as patient history through chart review and patient interview at baseline visit. CAD was defined as the presence of a documented acute coronary syndrome or stable angina or both or a positive coronary angiography (stenosis >50% in >1 vessel), history of percutaneous coronary intervention (PCI) or coronary artery bypass graft (CABG) surgery. CVD was defined as the presence of a documented transient ischemic attack (TIA) or stroke. The presence of PVD was documented by carotid duplex (>50% stenosis of an internal carotid artery), abnormal pulse volume recording, or duplex ultrasound showing >50% stenosis or history of vascular surgery or percutaneous peripheral arterial intervention. We also collected current medications at the time of the visit. Antiplatelet therapy was defined as taking aspirin, Plavix (Sanofi-Avantis, Bridgewater, NJ) or Aggrenox (Boehringer-Ingelheim, Ridgefield, CT). Lipid-lowering therapies were defined as using statins, fibrates, niacin, cholesterol absorption inhibitors, or bile acid sequestrants.
All patients were clinically stable at the time of the visit. Patients were weighed on calibrated electronic scales, and height was measured on a stadiometer. Blood pressure measurements were obtained with sphygmomanometers and a mercury manometer using standard technique. The Cleveland Clinic Institutional Review Board approved the Preventive Cardiology database registry used in this study for collection and systematic analysis of patient data. Mortality data were obtained by a monthly query of the Social Security Administration death index database.
Laboratory tests
Venous blood samples were drawn after a 12-hour fasting period at the first visit. Patients had a baseline lipid panel, serum homocysteine, lipoprotein(a) (Lp(a)), ultrasensitive C-reactive protein (CRP), and a complete metabolic panel drawn. All samples were analyzed by the Cleveland Clinic Laboratory Medicine Department. Fasting low-density lipoprotein cholesterol (LDL-C) values were routinely calculated using the Friedwald equation or by direct determination if triglycerides were >250 mg/dL. Lipid assays were performed according to lipid research clinic methods. Total fasting serum homocysteine was measured using high-performance liquid chromatography (HPLC), and Lp(a) measurements were obtained using the method of Incstar (Incstar Co., Stillwater, MN) according to the package insert. Ultrasensitive CRP was measured using a high-sensitivity latex-enhanced assay (Dade Behring, Deerfield, IL).
Statistical analyses
Comparisons between women and men were performed using the nonparametric Mann-Whitney test. Categorical factors were compared using a chi-square test. Kaplan-Meier curves were used to show mortality risk over time, and Kaplan-Meier estimates and log-rank p values are presented. Multivariable Cox proportional hazards modeling was performed adjusting for age, history of DM, history of stroke, history of myocardial infarction (MI), BMI, diuretics, fibric acid, HDL-C, LDL-C, cholesterol, and homocysteine. Hazard ratios (HR) and 95% confidence intervals (95% CI) are reported. The statistical significance threshold was set at p ≤ 0.05. All analyses were performed using SAS version 8.2 (Cary, NC).
RESULTS
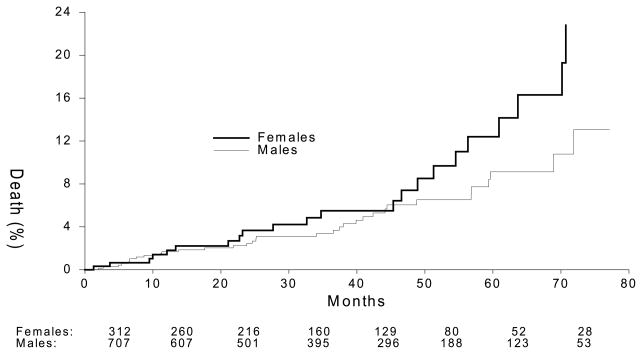
Between 1997 and 2004, 2462 patients were referred for secondary prevention. Of those, 25.9% (n = 637) were women. Most were referred to Preventive Cardiology for dyslipidemia (97.2% for women and 97.0% for men, p = 0.89), and the rest were obesity and medication recommendations. Mean duration of CVD was 9.7 years for women and 11.0 years for men (p < 0.001). Table 1 shows baseline demographic, medication, and laboratory values for the two groups. Women were older (62.2 ± 11.1 vs. 59.4 ± 11.0 years, p < .001), more likely to be African American (18.5% vs. 6.9%, p < 0.001), and more likely to have hypertension (68.1% vs. 56.1%, p < 0.001) than men. However, they had similar rates of DM, smoking, and PVD. Overall, women were more likely than men to have had CVD (32.0% vs. 17.9%, p < .001) but less likely than men to have CAD (84.8% vs. 94.1%, p < 0.001), MI (43.0% vs. 47.8%, p = 0.04), CABG (33.8% vs. 47.2%, p < 0.001), or PCI (49.5% vs. 62.9%, p < 0.001) (Table 1). Women were more likely than men to have higher baseline CRP (6.14 ± 13.4 vs. 4.9 ± 10.7, p < .001), LDL-C (135 ± 66 vs. 116 ± 46, p < 0.001), HDL-C (52 ± 17 vs. 41 ± 11, p < 0.001), total cholesterol (238 ± 98 vs. 202 ± 65, p < 0.001), and Lp(a) (50.3 ± 50.3 vs. 34.0 ± 34, p < 0.001) (Table 1). There was a trend toward increased long–term mortality in women compared with men (21.5% vs. 17.8%, p = 0.09) (Fig. 1). In multivariate analysis controlling for age, history of DM, history of stroke, history of MI, BMI, diuretics, fibric acid, HDL-C, LDL-C, cholesterol, and homocysteine, female gender was not associated with increased mortality (HR=1.51, 95% CI 0.61, 3.73, p = 0.37). Using the ACC/AHA Guidelines for secondary prevention goals, women were less likely than men to be at the LDL-C goal (28.4% vs. 38.1%, p < 0.001) (Table 2). Women were less likely than men to be on antiplatelet therapy (76.6 % vs. 85.0%, p < 0.001) or any lipid-lowering therapy (62.6% vs. 67.1%, p = 0.04) (Table 2); specifically, they were less likely to be on statin therapy (52.8% vs. 58.9%, p = 0.007). However, there was similar blood pressure control between women and men, <140/90 for nondiabetics and <130/80 for diabetics (91.1% vs. 93.1%, p = 0.13) (Table 2). There was no difference in beta-blocker or ACE inhibitor use at presentation.
Table 1.
Demographics
| Women (n = 637) | Men (n = 1825) | p value | |
|---|---|---|---|
| Age, years | 62.2 ± 11.1 | 59.4 ± 11.0 | <0.001 |
| Race | |||
| White | 79.8% | 89.0% | <0.001 |
| Black | 18.5% | 6.9% | |
| Others | 1.7% | 4.1% | |
| HTN,a mm Hg | 68.1% | 56.1% | <0.001 |
| DM | 25.4% | 22.4% | 0.11 |
| BMI (kg/m2) | 28.9 ± 6.20 | 29.1 ± 5.1 | 0.07 |
| Waist circumference (cm) | 94.1 ± 15.3 | 103.0 ± 12.5 | <0.001 |
| Smoking | 12.9% | 12.3% | 0.72 |
| Exercise | 0.001 | ||
| Less than once/week | 49.8% | 39.6% | |
| 1–2 times/week | 11.1% | 10.7% | |
| 3–5 times/week | 27.1% | 34.6% | |
| >5 times/week | 12.0% | 15.1% | |
| Family history CAD | 65.8% | 61.9% | 0.09 |
| CAD | 84.8% | 94.1% | <0.001 |
| CVD | 32.0% | 17.9% | <0.001 |
| PVD | 10.5% | 8.3% | 0.09 |
| History of MI | 43.0% | 47.8% | 0.04 |
| History of CABG | 33.8% | 47.2% | |
| History of PCI | 49.5% | 62.9% | |
| History of vascular surgery | 8.6% | 6.7% | 0.10 |
| Total cholesterol | 238 ± 980 | 202 ± 65 | <0.001 |
| LDL-C (mg/dL) | 135 ± 660 | 116 ± 46 | <0.001 |
| HDL-C (mg/dL) | 52 ± 17 | 41 ± 11 | <0.001 |
| Triglyceride (mg/dL) | 258 ± 348 | 228 ± 270 | 0.19 |
| CRP (mg/L) | 6.14 ± 13.4 | 4.9 ± 10.7 | <0.001 |
| Homocysteine (μmol/L) | 12.7 ± 5.20 | 13.9 ± 5.9 | <0.001 |
| Lp(a) (mg/dL) | 50.3 ± 50.3 | 34.0 ± 33.9 | <0.001 |
HTN, hypertension; DM, diabetes; BMI, body mass index; CAD, coronary artery disease; CVD, cerebrovascular disease; PVD, peripheral vascular disease; MI, myocardial infarction; CABG, coronary artery bypass graft surgery; PCI, percutaneous coronary intervention; LDL, low-density lipoprotein; HDL, high-density lipoprotein; CRP, c-reactive protein; Lp(a), lipoprotein (a).
FIG. 1.
Kaplan-Meier curve of mortality between women and men. X axis shows months from baseline visit. There was a trend toward increased long-term mortality in women compared with men (21.5% vs. 17.8%, p = 0.09).
Table 2.
ACC/AHA Guideline Recommendation for Secondary Prevention
| Women | Men | p value | |
|---|---|---|---|
| BP goal (<140/90) (with DM <130/80) mm Hg | 91.2% | 93.1% | 0.13 |
| LDL-C <100 mg/dL | 28.4% | 38.1% | <0.001 |
| Antiplatelet therapy | 76.6% | 85.0% | <0.001 |
| ACE inhibitor | 38.6% | 37.0% | 0.47 |
| Beta-blockers | 55.3% | 57.3% | 0.38 |
| Any lipid-lowering agent | 62.6% | 67.1% | 0.04 |
DISCUSSION
CVD continues to be the leading cause of death for women in the United States.1 Although there has been a 50% decline in age-adjusted heart disease mortality, women continue to lag behind men.1 Much has been reported on gender differences in the diagnosis and treatment of acute coronary syndromes in women. Numerous studies have shown delays in healthcare-seeking behavior and diagnosis and underuse of both resources and procedures in women compared with their male counterparts in acute coronary syndromes.2–5,7–9,12–23 There are few data, however, on gender differences in secondary preventive measures in stable patients. The ACC/AHA committees recently updated their secondary prevention guidelines for patients with coronary and other atherosclerotic vascular disease.11,24 The guidelines recommend blood pressure control of <140/90 mm Hg for all patients or <130/80 mm Hg for patients with DM or chronic kidney disease, LDL <100 mg/dL, HgA1C <6.5%, the use of antiplatelet agents, ACE inhibitors in patients with ejection fraction (EF) <40%, and beta-blockers in all patients who have had MI, acute coronary syndromes (ACS), or left ventricular (LV) dysfunction. The guidelines also recommend smoking cessation, regular physical activity, and healthy weight management. These recommendations are not gender based.
In this large study assessing adherence to guideline recommendations, we found women were less likely than men to be on antiplatelet, statin, or lipid-lowering therapy even though statin intolerance rates were similar between the groups. As women are on lower rates of lipid-lowering therapy, it is understandable that they would have higher levels of LDL-C. Also, because both antiplatelet and statin therapy are known to lower CRP, it was not surprising that women were more likely than men to have higher CRP levels, given their medication regimen. There was a trend toward higher long-term, all-cause mortality in women compared with men. The association between higher use of evidence-based therapies and improved outcome is well described.25–28 Thus, the trend of increased mortality in women in our study is not unexpected. These data also suggest that there still is a major need for improved treatment with well-accepted, secondary preventive interventions in both women and men. LDL-C control and antiplatelet use appear to be the major areas in need of improvement.
In ST-elevation MI and in non-ST-elevation (NSTE) MI, there are well-described discrepancies in diagnosis and treatment between women and men. Recently, the Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes with Early Implementation of the ACC/AHA Guidelines (CRUSADE) investigators published their registry data on gender differences in patients with NSTE-ACS across the United States.2 They found that women were less likely than men to receive guideline-recommended therapy during hospitalization. Moreover, at discharge, women were less likely to receive aspirin, statins, and ACE inhibitors, which are guideline-recommended medical therapies, and in a large ST-elevation MI registry, women were less likely to receive accepted pharmacological intervention on admission and at discharge.4,7,16,18,23 In addition, there was delay in time-to-treatment, invasive diagnostic tests, and revascularization in women. Our study is similar to recently published data on stable angina patients in Europe, which reported that women with stable angina were less likely to be on evidence-based medical therapy or to be revascularized.5 Our study expands on the previously published data by assessing blood pressure and cholesterol control in this group.
Race was another contributing factor in our study, as women in our population were more likely to be African Americans. Studies have shown differing medical therapies in patients with CAD based on race and socioeconomic status.29,30 African American patients were less likely to receive guideline-recommended medications than Caucasian patients.31,32 It is unclear if this is a result of compliance, socioeconomic, cultural, or physician bias issues.31,32 Even though there has been much discussion, these gender disparities in treatment continue. Clearly, quality improvement on the part of healthcare providers and continued investigation in gender research are necessary.
Limitations
There are several limitations to our study. There is potential for selection and referral bias in patients enrolling in a tertiary preventive cardiology clinic. Most of our patients were referred by cardiologists and general internists for risk factor modification. Also, although we collected information about race, we did not collect detailed information on lifestyle, education level, employment, income, or marital status. These factors may have contributed to differences in secondary prevention therapies and compliance.
CONCLUSIONS
Even in the current era, women continue to receive less aggressive care than men. Regardless of gender, these data show that there is underuse of ACC/AHA Guideline-prescribed intervention in this population and that in men as well as in women, more effort needs to be made to treat patients with accepted secondary preventive interventions. Future education interventions should be targeted to both physicians and patients to improve adherence to national secondary prevention guidelines, especially among women, who are at higher risk.
Footnotes
DISCLOSURE STATEMENT
No competing financial interests exist.
References
- 1.Thom T, Haase N, Rosamond W, et al. Heart disease and stroke statistics—2006 update: A report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2006;113:e85. doi: 10.1161/CIRCULATIONAHA.105.171600. [DOI] [PubMed] [Google Scholar]
- 2.Blomkalns AL, Chen AY, Hochman JS, et al. Gender disparities in the diagnosis and treatment of non-ST-segment elevation acute coronary syndromes: Large-scale observations from the CRUSADE (Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes With Early Implementation of the American College of Cardiology/American Heart Association Guidelines) National Quality Improvement Initiative. J Am Coll Cardiol. 2005;45:832. doi: 10.1016/j.jacc.2004.11.055. [DOI] [PubMed] [Google Scholar]
- 3.Canto JG, Allison JJ, Kiefe CI, et al. Relation of race and sex to the use of reperfusion therapy in Medicare beneficiaries with acute myocardial infarction. N Engl J Med. 2000;342:1094. doi: 10.1056/NEJM200004133421505. [DOI] [PubMed] [Google Scholar]
- 4.Chandra NC, Ziegelstein RC, Rogers WJ, et al. Observations of the treatment of women in the United States with myocardial infarction: A report from the National Registry of Myocardial Infarction-I. Arch Intern Med. 1998;158:981. doi: 10.1001/archinte.158.9.981. [DOI] [PubMed] [Google Scholar]
- 5.Daly C, Clemens F, Lopez Sendon JL, et al. Gender differences in the management and clinical outcome of stable angina. Circulation. 2006;113:490. doi: 10.1161/CIRCULATIONAHA.105.561647. [DOI] [PubMed] [Google Scholar]
- 6.Danchin N. Acute coronary syndromes: Should women receive less antithrombotic medication than men? Heart. 2004;90:363. doi: 10.1136/hrt.2002.003483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gan SC, Beaver SK, Houck PM, MacLehose RF, Lawson HW, Chan L. Treatment of acute myocardial infarction and 30-day mortality among women and men. N Engl J Med. 2000;343:8. doi: 10.1056/NEJM200007063430102. [DOI] [PubMed] [Google Scholar]
- 8.Ghali WA, Faris PD, Galbraith PD, et al. Sex differences in access to coronary revascularization after cardiac catheterization: Importance of detailed clinical data. Ann Intern Med. 2002;136:723. doi: 10.7326/0003-4819-136-10-200205210-00007. [DOI] [PubMed] [Google Scholar]
- 9.Guru V, Fremes SE, Austin PC, Blackstone EH, Tu JV. Gender differences in outcomes after hospital discharge from coronary artery bypass grafting. Circulation. 2006;113:507. doi: 10.1161/CIRCULATIONAHA.105.576652. [DOI] [PubMed] [Google Scholar]
- 10.Smith SC, Jr, Feldman TE, Hirshfeld JW, Jr, et al. ACC/AHA/SCAI 2005 guideline update for percutaneous coronary intervention: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/SCAI Writing Committee to Update 2001 Guidelines for Percutaneous Coronary Intervention) Circulation. 2006;113:e166. doi: 10.1161/CIRCULATIONAHA.106.173220. [DOI] [PubMed] [Google Scholar]
- 11.Smith SC, Jr, Allen J, Blair SN, et al. AHA/ACC guidelines for secondary prevention for patients with coronary and other atherosclerotic vascular disease: 2006 update: Endorsed by the National Heart, Lung, and Blood Institute. Circulation. 2006;113:2363. doi: 10.1161/CIRCULATIONAHA.106.174516. [DOI] [PubMed] [Google Scholar]
- 12.Diercks DB, Peacock WF, Hiestand BC, et al. Frequency and consequences of recording an electrocardiogram >10 minutes after arrival in an emergency room in non-ST-segment elevation acute coronary syndromes (from the CRUSADE Initiative) Am J Cardiol. 2006;97:437. doi: 10.1016/j.amjcard.2005.09.073. [DOI] [PubMed] [Google Scholar]
- 13.Goldberg RJ, O’Donnell C, Yarzebski J, Bigelow C, Savageau J, Gore JM. Sex differences in symptom presentation associated with acute myocardial infarction: A population-based perspective. Am Heart J. 1998;136:189. doi: 10.1053/hj.1998.v136.88874. [DOI] [PubMed] [Google Scholar]
- 14.Hochman JS, Tamis JE, Thompson TD, et al. Sex, clinical presentation, and outcome in patients with acute coronary syndromes. Global Use of Strategies to Open Occluded Coronary Arteries in Acute Coronary Syndromes IIb Investigators. N Engl J Med. 1999;341:226. doi: 10.1056/NEJM199907223410402. [DOI] [PubMed] [Google Scholar]
- 15.Jacobs AK. Women, ischemic heart disease, revascularization, and the gender gap: What are we missing? J Am Coll Cardiol. 2006;47(Suppl 3):S63. doi: 10.1016/j.jacc.2004.12.085. [DOI] [PubMed] [Google Scholar]
- 16.Kudenchuk PJ, Maynard C, Martin JS, Wirkus M, Weaver WD. Comparison of presentation, treatment, and outcome of acute myocardial infarction in men versus women (the Myocardial Infarction Triage and Intervention Registry) Am J Cardiol. 1996;78:9. doi: 10.1016/s0002-9149(96)00218-4. [DOI] [PubMed] [Google Scholar]
- 17.Lansky AJ, Pietras C, Costa RA, et al. Gender differences in outcomes after primary angioplasty versus primary stenting with and without abciximab for acute myocardial infarction: Results of the Controlled Abciximab and Device Investigation to Lower Late Angioplasty Complications (CADILLAC) trial. Circulation. 2005;111:1611. doi: 10.1161/01.CIR.0000160362.55803.40. [DOI] [PubMed] [Google Scholar]
- 18.Marrugat J, Sala J, Masia R, et al. Mortality differences between men and women following first myocardial infarction. RESCATE Investigators. Recursos Empleados en el Sindrome Coronario Agudo y Tiempo de Espera. JAMA. 1998;280:1405. doi: 10.1001/jama.280.16.1405. [DOI] [PubMed] [Google Scholar]
- 19.Maynard C, Litwin PE, Martin JS, Weaver WD. Gender differences in the treatment and outcome of acute myocardial infarction. Results from the Myocardial Infarction Triage and Intervention Registry. Arch Intern Med. 1992;152:972. [PubMed] [Google Scholar]
- 20.Rathore SS, Wang Y, Radford MJ, Ordin DL, Krumholz HM. Sex differences in cardiac catheterization after acute myocardial infarction: The role of procedure appropriateness. Ann Intern Med. 2002;137:487. doi: 10.7326/0003-4819-137-6-200209170-00008. [DOI] [PubMed] [Google Scholar]
- 21.Schulman KA, Berlin JA, Harless W, et al. The effect of race and sex on physicians’ recommendations for cardiac catheterization. N Engl J Med. 1999;340:618. doi: 10.1056/NEJM199902253400806. [DOI] [PubMed] [Google Scholar]
- 22.Vaccarino V. Angina and cardiac care: Are there gender differences, and if so, why? Circulation. 2006;113:467. doi: 10.1161/CIRCULATIONAHA.105.602284. [DOI] [PubMed] [Google Scholar]
- 23.Vaccarino V, Parsons L, Every NR, Barron HV, Krumholz HM. Sex-based differences in early mortality after myocardial infarction. National Registry of Myocardial Infarction 2 Participants. N Engl J Med. 1999;341:217. doi: 10.1056/NEJM199907223410401. [DOI] [PubMed] [Google Scholar]
- 24.Lonn E, Yusuf S, Dzavik V, et al. Effects of ramipril and vitamin E on atherosclerosis: The study to evaluate carotid ultrasound changes in patients treated with ramipril and vitamin E (SECURE) Circulation. 2001;103:919. doi: 10.1161/01.cir.103.7.919. [DOI] [PubMed] [Google Scholar]
- 25.Eagle KA, Montoye CK, Riba AL, et al. Guideline-based standardized care is associated with substantially lower mortality in medicare patients with acute myocardial infarction: The American College of Cardiology’s Guidelines Applied in Practice (GAP) Projects in Michigan. J Am Coll Cardiol. 2005;46:1242. doi: 10.1016/j.jacc.2004.12.083. [DOI] [PubMed] [Google Scholar]
- 26.Higashi T, Shekelle PG, Adams JL, et al. Quality of care is associated with survival in vulnerable older patients. Ann Intern Med. 2005;143:274. doi: 10.7326/0003-4819-143-4-200508160-00008. [DOI] [PubMed] [Google Scholar]
- 27.Chen J, Radford MJ, Wang Y, Marciniak TA, Krumholz HM. Do “America’s Best Hospitals” perform better for acute myocardial infarction? N Engl J Med. 1999;340:286. doi: 10.1056/NEJM199901283400407. [DOI] [PubMed] [Google Scholar]
- 28.Peterson ED, Roe MT, Mulgund J, et al. Association between hospital process performance and outcomes among patients with acute coronary syndromes. JAMA. 2006;295:1912. doi: 10.1001/jama.295.16.1912. [DOI] [PubMed] [Google Scholar]
- 29.Kahn LS, Fox CH, Olawaiye A, Servoss TJ, McLean-Plunkett E. Facilitating quality improvement in physician management of comorbid chronic disease in an urban minority practice. J Natl Med Assoc. 2007;99:377. [PMC free article] [PubMed] [Google Scholar]
- 30.Williams ML, Morris MT, 2nd, Ahmad U, Yousseff M, Li W, Ertel N. Racial differences in compliance with NCEP-II recommendations for secondary prevention at a Veterans Affairs medical center. Ethnic Dis. 2002;12:S1. [PubMed] [Google Scholar]
- 31.Bach PB, Pham HH, Schrag D, Tate RC, Hargraves JL. Primary care physicians who treat blacks and whites. N Engl J Med. 2004;351:575. doi: 10.1056/NEJMsa040609. [DOI] [PubMed] [Google Scholar]
- 32.Lillie-Blanton M, Maddox TM, Rushing O, Mensah GA. Disparities in cardiac care: Rising to the challenge of Healthy People 2010. J Am Coll Cardiol. 2004;44:503. doi: 10.1016/j.jacc.2004.04.043. [DOI] [PubMed] [Google Scholar]