Abstract
Objective:
This study examined the relationship of limb length inequality (LLI) with radiographic hip and knee osteoarthritis (OA) in a large, community-based sample.
Methods:
The total study group comprised 926 participants with radiographic knee OA, 796 with radiographic hip OA, and 210 (6.6%) with LLI ≥ 2 cm. The presence of radiographic OA was defined as Kellgren/Lawrence (K/L) grade ≥2. Multiple logistic regression models were used to examine the relationship of LLI with hip and knee OA, while controlling for age, gender, race, body mass index, and history of hip or knee problems (joint injury, fracture, surgery, or congenital anomalies).
Results:
In unadjusted analyses, participants with LLI were more likely than those without LLI to have radiographic knee OA (45.1% vs. 28.3%, p<0.001) and radiographic hip OA (35.2% vs. 28.7%, p=0.063). In multiple logistic regression models, knee OA was significantly associated with presence of LLI (adjusted Odds Ratio [aOR]=1.80, 95% Confidence Interval, [95% CI] 1.29-2.52), but there was no significant relationship between hip OA and LLI (aOR=1.20, 95% CI 0.86-1.67). Among participants with LLI, right hip OA was more common when the contralateral limb was longer than when the ipsilateral limb was longer (30.3% vs. 17.5%, p=0.070)
Conclusion:
LLI was associated with radiographic knee OA, controlling for other important variables. Future research should examine the relationship of LLI with hip or knee OA incidence, progression, and symptom severity, as well as the efficacy for LLI corrective treatments in OA.
Keywords: Osteoarthritis, leg length inequality
Introduction
Osteoarthritis (OA) is one of the most common chronic conditions in the United States and a leading cause of disability among older adults1-3. OA of the knee and hip affects up to 6% and 3% of the U.S. adult population, respectively4, and has a considerable impact on mobility, basic daily activities, employment, quality of life, and aspects of health (i.e., weight management and cardiovascular health)5-7. There is growing appreciation for the important role of local joint characteristics and biomechanical factors in the development of OA. Recent studies have shown that some mechanical factors, including joint instability and malalignment, contribute to the progressive degeneration that characterizes radiographic OA8-11.
Previous reports also suggest that limb length inequality (LLI), a condition in which paired lower extremities are of unequal length, alters gait symmetry and joint mechanics during weight bearing, potentially contributing to the development of radiographic knee and hip OA12-14. Individuals with LLI often modify their movement patterns to functionally minimize the inequality, i.e., increasing knee flexion or hip adduction of the longer limb. These compensatory mechanisms may amplify forces across a smaller joint contact area, thus acting as a biomechanical precursor to lower extremity OA12. Individuals with congenital, developmental, and post-traumatic disorders may develop LLI in combination with other joint abnormalities that increase their risk for OA. Additionally, individuals with greater magnitude LLIs may be more limited in their ability to participate in physical activities and thus, more likely to exhibit obesity, another risk factor associated with radiographic OA15. However, previous literature examining the potential relationship of LLI to radiographic knee and hip OA is sparse and based primarily on small sample sizes and clinical observations12, 16-19.
The purpose of this study was to examine the relationship of LLI with radiographic knee and hip OA in a large, community-based sample. Specifically, we compared the presence and severity of radiographic knee or hip OA between individuals with and without LLI, and among individuals with LLI, we also examined whether the occurrence of radiographic knee or hip OA was more common in the longer or shorter limb.
Methods
Study participants
The Johnston County Osteoarthritis Project is an ongoing, community-based study of the occurrence of knee and hip OA in African American and Caucasian residents in a rural county in North Carolina. Details of this study have been reported previously20, 21. Briefly, this study involved civilian, non-institutionalized adults aged 45 years and older who resided in six townships in Johnston County. Participants were recruited by probability sampling, with over-sampling of African Americans. A total of 3,187 individuals were recruited between May 1991 and December 1997. All participants completed a baseline clinical evaluation21. Twenty-six individuals with history of total knee arthroplasty and 27 with total hip arthroplasty were excluded from OA analyses. Other individuals were excluded because of incomplete LLI and/or radiographic data. The final sample included 3161 with knee Kellgren/Lawrence (K/L) radiographic and LLI data and 2778 individuals with hip K/L radiographic and LLI data.
Limb Length Measurement
With the participant supine, a tape measure was used to determine right and left lower extremity lengths (in centimeters (cm)) between two defined bony landmarks: the anterior superior iliac spine (ASIS) and the medial malleolus. Hoyle et al. 22 reported an inter-tester reliability of r=0.98 and an intra-tester reliability from r=0.89-0.95 with this measurement technique. According to a study by Friberg et al 23, the mean difference in LLI was 8.6 mm (1.1 mm intratester mean error) compared to radiographs. To account for potential measurement error in this clinical measurement, LLI was defined conservatively as a 2.0 cm or greater difference in length between limbs.
Radiographic Assessment
All participants completed bilateral anteroposterior radiography of the knee in weight bearing. Women over 50 years of age and all men completed supine anteroposterior pelvic radiography. Radiographs were rated by a single radiologist using the K/L radiographic atlas for overall knee and hip radiographic grades. As previously described, interrater and intrarater reliability for the radiologist were high (weighted kappa for interrater reliability 0.859; kappa for intrarater reliability 0.886)21. Radiographs without the features of OA were defined as K/L grade of 0 (normal findings). A minute radiographic osteophyte of doubtful pathologic significance was assigned a K/L grade of 1 (questionable). Radiographs showing an osteophyte without joint space narrowing were assigned a K/L grade of 2 (mild). A moderate decrease of the joint space was assigned a K/L grade of 3 (moderate). K/L grade 4 (severe) was defined as severe joint space narrowing with subchondral bone sclerosis24. The presence of radiographic OA was defined as a K/L grade ≥2. Radiographic severity was defined as mild for a K/L grade of 2 and moderate-to-severe for K/L grades 3 and 4.
Demographic and Clinical Characteristics
We examined the following participant characteristics as covariates in our analyses because they have been associated with radiographic knee and hip OA: gender; self-reported race (African American or Caucasian); age; history of knee joint problems among those with knee OA (i.e., knee injury [“Have you ever injured your right/left knee?”], knee fracture [“Has a doctor ever told you that you had broken or fractured your right/left knee?”], and knee surgery [“Have you ever had surgery on your right/left knee?”]); history of hip joint problems among those with hip OA (i.e., congenital hip problem [“Has a doctor ever told you that you had a problem with your right/left hip from birth or childhood?”], hip injury [“Have you ever injured your right/left hip?”], hip fracture [“Has a doctor ever told you that you had broken or fractured your right/left hip?”], and hip surgery [“Have you ever had surgery on your right/left hip?”]); and body mass index (BMI: calculated as weight in kilograms/height in meters squared). Height without shoes was measured in cm and weight was measured in kilograms (kg) using a balance beam scale.
Statistical analysis
Chi square, Fisher's exact, and t-tests were used to compare gender, race, age, BMI, history of knee or hip joint problems, and knee and hip OA between groups with and without LLI. Separate multiple logistic regression models were used to examine the relationship of knee and hip OA to LLI, while controlling for age, gender, race, BMI, and history of knee or hip problems, respectively (i.e., injury, fracture, surgery, or congential hip problem). Additionally, Chi-square tests were used to examine the presence of LLI with the following binary variables: unilateral knee OA, bilateral knee OA, right knee OA, left knee OA, unilateral hip OA, bilateral hip OA, right hip OA, and left hip OA. Unilateral OA was defined as having OA of only one knee joint or one hip joint. Bilateral OA was defined as having OA of both knees or both hips. Chi-square tests were used to examine the relationship of LLI with radiographic severity. Among participants with LLI, we used Chi-square tests to compare the presence of OA in the right longer vs. left longer limb. All statistical computations were performed using SAS Version 8 software (SAS Institute, Cary, NC). Statistical significance was evaluated at the p<0.05 level.
Results
The total study group comprised 926 participants with radiographic knee OA (K/L ≥ 2) (61.4% female, 68.1% Caucasian), 796 participants with radiographic hip OA (K/L ≥ 2) (56.5% female, 69.5% Caucasian), and 210 (6.6%) with LLI ≥ 2 cm (Table 1). The left limb was longer in 65.7% of participants with LLI. Among participants with knee radiographs, the mean age was 62.6 years and the mean BMI was 29.0 kg/m2 (Table 1). Among participants with hip radiographs, the mean age was 64.2 years and the mean BMI was 28.9 kg/m2 (Table 1). There were no statistically significant differences in race or gender between groups with and without LLI. Participants with LLI were significantly older and had a higher mean BMI than participants without LLI. The proportion of patients with a history of knee problems or hip problems was significantly higher in participants with LLI compared to participants without LLI (Table 1).
Table 1.
Selected Characteristics of Sample, by LLI and Joint Site.
| Participants with Knee Radiographs | Participants with Hip Radiographs | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Total Sample (N=2989 ) |
With LLI* (N=195) |
Without LLI (N= 2794) |
p-value | Total Sample (N=2639 ) |
With LLI* (N=179) |
Without LLI (N= 2460) |
p-value | ||
| Female (%) | 61.4 | 61.0 | 61.5 | 0.906 | Female (%) | 56.5 | 57.0 | 56.5 | 0.892 |
| Caucasian (%) | 68.1 | 63.6 | 68.4 | 0.164 | Caucasian (%) | 69.5 | 67.0 | 69.6 | 0467 |
| Age (mean (SD)) years | 62.6(±11.1) | 64.2(± 11.0) | 62.3(±11.0) | 0.020 | Age (mean (SD)) years | 64.2(±10.4) | 66.2(±10.2) | 64.0(±10.4) | 0.006 |
| BMI (mean kg/m2(SD)) | 29.0(±6.0) | 30.0(±7.4) | 28.9(±5.9) | 0.013 | BMI (mean kg/m2(SD)) | 28.9 (±5.8) | 29.7(±6.9) | 28.8(±5.7) | 0.067 |
| History of Knee Problem (%) | 17.6 | 22.8 | 17.2 | 0.053 | History of Hip Problem (%) | 7.8 | 13.1 | 7.4 | 0.006 |
| Knee Injury (%) | 16.3 | 20.6 | 16.0 | 0.098 | Hip Injury (%)** | 5.7 | 9.7 | 5.4 | 0.017 |
| Knee Fracture (%) | 0.3 | 0.5 | 0.3 | 0.343 | Hip Fracture (%) | 0.1 | 0.6 | 0.1 | 0.177 |
| Knee Surgery (%) | 5.2 | 8.4 | 4.9 | 0.037 | Hip Surgery (%)** | 1.5 | 4.6 | 1.3 | <0.001 |
| Congenital Hip Problem(%)** | 1.8 | 2.8 | 1.7 | 0.291 | |||||
LLI = limb length inequality
Results of Fisher's exact test
Any radiographic knee or hip OA was present in 55.4% of participants with LLI and 45.2% of participants without LLI (p=0.006). Participants with LLI were significantly more likely than those without LLI to have radiographic knee and hip OA (Table 2). LLI was specifically associated with a greater likelihood of right knee OA, left knee OA, and right hip OA, but not left hip OA (Table 2). Both mild and moderate-to-severe radiographic knee OA were more common in individuals with LLI (Table 2). In adjusted models for covariates, those with LLI were 80% more likely than those without LLI to have radiographic knee OA (adjusted Odds Ratio [aOR]=1.80, 95% Confidence Interval, [95% CI] 1.29-2.52) and 20% more likely than those without LLI to have radiographic hip OA, with the latter association not statistically significant (aOR=1.20, 95% CI 0.86-1.67).
Table 2.
Unadjusted associations between LLI and frequency of radiographic knee and hip OA.
| LLI (N=195) |
No LLI (N=2794) |
p-value | LLI (N=179) |
No LLI (N=2460) |
p-value | ||
|---|---|---|---|---|---|---|---|
| Any Knee OA (%) | 45.1 | 28.3 | <0.001 | Any Hip OA (%) | 35.2 | 28.7 | 0.063 |
| Unilateral Knee OA (%)* | 27.7 | 16.5 | <0.001 | Unilateral Hip OA (%)* | 22.2 | 19.1 | 0.366 |
| Bilateral Knee OA (%)** | 30.5 | 16.5 | <0.001 | Bilateral Hip OA (%)** | 20.6 | 14.2 | 0.035 |
| Any Right Knee OA (%) | 34.9 | 22.7 | <0.001 | Any Right Hip OA (%) | 26.3 | 19.6 | 0.033 |
| Mild (%) | 22.6 | 12.3 | 0.006 | Mild (%) | 22.9 | 17.6 | 0.062 |
| Moderate-Severe (%) | 16.3 | 6.4 | <0.001 | Moderate-Severe (%) | 3.4 | 2.0 | 0.077 |
| Any Left Knee OA (%) | 34.4 | 19.8 | <0.001 | Any Left Hip OA (%) | 25.7 | 20.8 | 0.122 |
| Mild (%) | 22.1 | 14.5 | <0.001 | Mild (%) | 21.2 | 19.5 | 0.438 |
| Moderate-Severe (%) | 12.3 | 5.3 | <0.001 | Moderate-Severe (%) | 4.5 | 1.3 | 0.003 |
Unilateral OA = OA of only one hip joint or one knee joint.
Bilateral OA = OA of both hips or both knees.
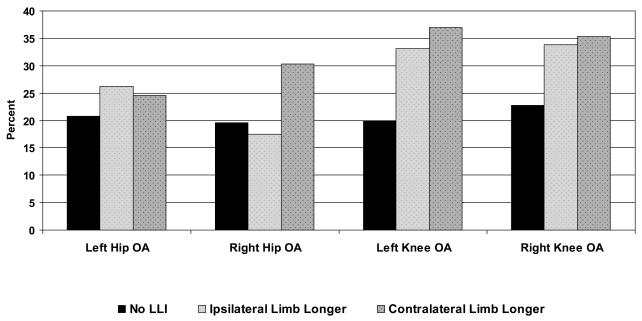
Among participants with LLI, right hip OA was more common when the contralateral limb was longer than when the ipsilateral limb was longer (30.3% vs. 17.5%, p=0.070) (Figure 1). There were no statistically significant differences in left hip, right knee, or left knee OA according to whether the ipsilateral or contralateral limb was longer.
Figure 1.
Proportion of sample with radiographic hip and knee OA, by laterality of joint site and LLI
Discussion
This is the first large, community-based study to examine the relationship of LLI with radiographic knee and hip OA. The prevalence and severity of knee OA was higher in participants with LLI than without LLI, even when adjusted for key risk factors. This is consistent with a review of medical records from a United Kingdom hospital, which revealed that 24 out of 37 patients (65%) with LLI of ≥ 2.5 cm had knee joint disease (arthritis or arthrosis) in the longer limb 16. LLI may lead to altered or amplified joint forces, resulting in accelerated degeneration of joint structures and increased OA severity. However, it is also possible that diminished joint spacing, degeneration of articular cartilage and subchondral bone, and possible joint disfigurement or malalignment may result in LLI. Additional studies are needed to investigate this potential relationship longitudinally.
In the present study, radiographic hip OA was more common in participants with LLI than without LLI, but this association was not statistically significant in adjusted models. Radiographic right hip OA tended to be more common when the contralateral limb was longer, but no remarkable differences were seen between the left hip, right knee, or left knee OA with the ipsilateral or contralateral limb. Previous studies present contradictory results of the association between hip OA and LLI 12, 17, 25-27. Some previous research in clinical samples has indicated that hip OA may be more common in the longer limb than the shorter limb 12, 17, 27. For example, in a study of 100 consecutive patients undergoing hip arthroplasty, Tallroth et al.27 reported that radiographic hip OA occurred more frequently in the longer limb (84%). In contrast, some other studies have suggested that the shorter limb may sustain greater forces through the hip compared to the longer limb25, 26.
The strengths of this study include that it is community-based, consists of Caucasian and African-American males and females, includes information on both radiographic knee and hip OA for each study participant, and is the largest study to date to examine LLI and radiographic knee and hip OA. There are also several limitations to this study. In this sample, we did not assess knee and hip contracture measurements, which are factors that may decrease limb length measurement. Our study had a very low prevalence of advanced knee and hip OA (0.8% and 2.7% with K/L grade of 4, respectively). Therefore, it is unlikely that knee and hip flexion contractures were common in this sample. Although Gogia and Braatz28 reported that tape measurement of leg length (which was used in this study) is highly accurate between testers when compared to supine radiography, this method may be less reliable compared to standing radiographs29. Measurement error in this study may have reduced the likelihood of finding a significant relationship of LLI with knee and hip OA. Sources of measurement error with this technique include: 1) difficulty with accurately placing the tape measure on identical bilateral bony landmarks; 2) difference in lower extremity girth affecting measurements; 3) masking of functional LLIs (which are only seen in weight bearing) in the supine position; and 4) lack of consideration of the contributions of the foot and ankle to limb length. To account for these potential sources of error, we defined LLI conservatively and categorically as discrepancies ≥ 2 cm, rather than as a continuous variable. Woerman and Binder-MacLeod30 reported that the ASIS to medial malleolus measurement differed from standing radiographic measurements by a mean difference of 0.73 ± 1.01 cm. Thus, we believe that subjects with supine tape measurement differences between limbs ≥ 2 cm would demonstrate a LLI in standing radiographs. Furthermore, we believe our definition of ≥ 2 cm is conservative and would include only individuals with a clinically meaningful inequality.
Future research should examine the relationships of LLI and OA according to limb dominance, another factor that may contribute to gait asymmetry. Although the concept of limb dominance is controversial, several studies have shown that there are strength imbalances between the dominant and non-dominant limbs that have been associated with increased injury rates in athletes31, 32. We attempted to examine limb dominance and LLI in our sample, but we were unable to complete these analyses due to small cell sizes. Knowledge of the relationship of limb dominance with knee and hip OA may help further explain our results of the occurrence of radiographic knee or hip OA in the longer or shorter limb. There are also other biomechanical and anatomical factors (i.e., abnormalities in hip morphology and lower extremity alignment) that may be associated with LLI and OA that should be included in future studies.
In summary, in this community-based sample, LLI was associated with radiographic knee OA, controlling for several other related variables. The positive association between LLI and radiographic hip OA warrants consideration and further investigation. These results may have important clinical implications for patients seeking treatment for knee or hip OA. Evaluation of LLI should be incorporated into physical examinations for these patients. Treatment of LLI in patients with knee or hip OA, with heel or shoe lifts, may aid in reducing joint stresses, pain, and disability, but the literature supporting the effect of lifts is not conclusive 33-36. Further understanding of how LLI may contribute to the development of knee and hip OA is necessary to facilitate development of medical and self-care interventions to improve pain and function. Future research should examine the relationship of LLI to knee or hip OA incidence and progression over time, as well as the relationship of LLI and symptom severity (pain and function) in individuals with knee or hip OA.
Acknowledgements
Centers for Disease Control and Prevention / Association of Schools of Public Health cooperative agreements S1734 and S3486 (JMJ, JBR), the NIAMS Multipurpose Arthritis and Musculoskeletal Disease Center grant 5-P60-AR30701 (JMJ), the NIAMS Multidisciplinary Clinical Research Center grant 5 P60 AR49465-03 (JMJ), and NIH National Research Service Award Institutional Research Training Grant (T32) - Arthritis and Immunology AR07416 (YMG).
References
- 1.Centers for Disease Control and Prevention Public health and aging: Projected prevalence of self-reported arthritis or chronic joint symptoms among persons aged >65 years--United States, 2005-2030. Morb Mortal Wkly Rep. 2003;52:489–491. [PubMed] [Google Scholar]
- 2.Hughes SL, Dunlop D. The prevalence and impact of arthritis in older persons. Arthritis Care Res. 1995;8:257–264. doi: 10.1002/art.1790080409. [DOI] [PubMed] [Google Scholar]
- 3.Lawrence RC, Helmick CG, Arnett FC, Deyo RA, Felson DT, Giannini EH. Estimates of the prevalence of arthritis and selected musculoskeletal disorders in the United States. Arthritis Rheum. 1998;41:778–799. doi: 10.1002/1529-0131(199805)41:5<778::AID-ART4>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- 4.Felson DT, Lawrence RC, Dieppe PA, Hirsch R, Helmick CG, Jordan JM. Osteoarthritis: New insights. Part 1: The disease and its risk factors. Ann Intern Med. 2000;133(9):635–646. doi: 10.7326/0003-4819-133-8-200010170-00016. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention Health-related quality of life among adults with arthritis--Behavioral Risk Factor Surveillance System, 11 states, 1996-1998. Morb Mortal Wkly Rep. 2000;49:366–369. [PubMed] [Google Scholar]
- 6.deBock GH, Kaptein AA, Touw-Otten F, Mulder JD. Health-relate quality of life in patients with osteoarthritis in a family practice setting. Arthritis Care Res. 1995;8(2):88–93. doi: 10.1002/art.1790080206. [DOI] [PubMed] [Google Scholar]
- 7.Dominick KL, Ahern FM, Gold CH, Heller DA. Health-related quality of life among older adults with arthritis. Health Qual Life Outcomes. 2004;2(1):5. doi: 10.1186/1477-7525-2-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cerejo R, Dunlop DD, Cahue S, Channin D, Song J, Sharma L. The influence of alignment on risk of knee osteoarthritis progression according to baseline stage of disease. Arthritis Rheum. 2002;46(10):2632–2636. doi: 10.1002/art.10530. [DOI] [PubMed] [Google Scholar]
- 9.Sharma L. The role of proprioceptive deficits, ligamentous laxity, and malalignment in development and progression of knee osteoarthritis. J Rheumatol. 2004;31:87–92. [PubMed] [Google Scholar]
- 10.Sharma L, Lou C, Felson DT, et al. Laxity in healthy and osteoarthritis knees. Arthritis Rheum. 1999;42:861–870. doi: 10.1002/1529-0131(199905)42:5<861::AID-ANR4>3.0.CO;2-N. [DOI] [PubMed] [Google Scholar]
- 11.Sharma L, Song J, Felson DT, Cahue S, Shamiyeh E, Dunlop DD. The role of knee alignment in disease progression and functional decline in knee osteoarthritis. JAMA. 2001;286:188–195. doi: 10.1001/jama.286.2.188. [DOI] [PubMed] [Google Scholar]
- 12.Friberg O. Clinical symptoms and biomechanics of lumbar spine and hip joint in leg length inequality. Spine. 1982;8(6):643–651. doi: 10.1097/00007632-198309000-00010. [DOI] [PubMed] [Google Scholar]
- 13.McCaw ST, Bates BT. Biomechanical implications of mild leg length inequality. Br J Sports Med. 1991;25:10–12. doi: 10.1136/bjsm.25.1.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Morscher E. Etiology and pathophysiology of leg length discrepancies. Prog Orthop Surg. 1977;1:9–19. [Google Scholar]
- 15.Felson DT. Risk factors for osteoarthritis: understanding joint vulnerability. Clin Orthop Relat Res. 2004;427(Suppl):S16–21. doi: 10.1097/01.blo.0000144971.12731.a2. [DOI] [PubMed] [Google Scholar]
- 16.Dixon AST, Campbell-Smith S. Long leg arthropathy. Ann Rheum Dis. 1969;28(4):359–365. doi: 10.1136/ard.28.4.359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gofton JP, Trueman GE. Studies in osteoarthritis of the hip: Part II. Osteoarthritis of the hip and leg-length disparity. Can Med Assoc J. 1971;104(9):791–799. [PMC free article] [PubMed] [Google Scholar]
- 18.Rothenberg RJ. Rheumatic disease aspects of leg length inequality. Semin Arthritis Rheum. 1988;17:196–205. doi: 10.1016/0049-0172(88)90020-0. [DOI] [PubMed] [Google Scholar]
- 19.Stanitski DF. Limb length inequality: assessment and treatment options. J Am Acad Orthop Surg. 1999;7:143–153. doi: 10.5435/00124635-199905000-00001. [DOI] [PubMed] [Google Scholar]
- 20.Jordan JM, Helmick CG, Renner JB, et al. Prevalence of knee symptoms and radiographic and symptomatic knee osteoarthritis in Africans and Caucasians: The Johnston County Osteoarthritis Project. J Rheumatol. 2007 in press. [PubMed] [Google Scholar]
- 21.Jordan JM, Linder GF, Renner JB, Fryer JG. The impact of arthritis in rural populations. Arthritis Care Res. 1995;8:242–250. doi: 10.1002/art.1790080407. [DOI] [PubMed] [Google Scholar]
- 22.Hoyle DA, Latour M, Bohannon RW. Intraexaminer, interexaminer, and interdevice comparability of leg length measurements obtained with measuring tape and metrecom. J Orthop Sports Phys Ther. 1991;14(6):263–268. doi: 10.2519/jospt.1991.14.6.263. [DOI] [PubMed] [Google Scholar]
- 23.Friberg O, Nurminen M, Kouhonen K, Soininen E, Manttari T. Accuracy and precision of clinical estimation of leg length inequality and lumbar scoliosis: comparison of clinical and radiological measurements. Int Disability Stud. 1988;10:49–53. doi: 10.3109/09638288809164098. [DOI] [PubMed] [Google Scholar]
- 24.Kellgren JH, Lawrence JS. The epidemiology of chronic rheumatism, atlas of standard radiographs. Blackwell Scientific; Oxford: 1963. [Google Scholar]
- 25.Brand RA, Yack HJ. Effects of leg length discrepancies on the forces at the hip joint. Clin Orthop. 1996;333:172–180. [PubMed] [Google Scholar]
- 26.Schuit D, Adrian M, Pidoce P. Effect of heel lifts on ground reaction force patterns in subjects with structural leg-length discrepancies. Phys Ther. 1989;69:663–670. doi: 10.1093/ptj/69.8.663. [DOI] [PubMed] [Google Scholar]
- 27.Tallroth K, Ylikoski M, Lamminen H, Ruohonen K. Preoperative leg-length inequality and hip osteoarthritis: a radiographic study of 100 consecutive arthroplasty patients. Skeletal Radiol. 2005;34(3):136–9. doi: 10.1007/s00256-004-0831-5. [DOI] [PubMed] [Google Scholar]
- 28.Gogia PP, Braatz JH. Validity and reliability of leg length measurements. J Orthop Sports Phys Ther. 1986;8:185–188. doi: 10.2519/jospt.1986.8.4.185. [DOI] [PubMed] [Google Scholar]
- 29.Brady RJ, Dean JB, Skinner TM, Gross MT. Limb length inequality: clinical implications for assessment and intervention. J Orthop Sports Phys Ther. 2003;33:221–234. doi: 10.2519/jospt.2003.33.5.221. [DOI] [PubMed] [Google Scholar]
- 30.Woerman AL, Binder-MacLeod SA. Leg length discrepancy assessment: accuracy and precision in five clinical methods of evaluation. J Orthop Sports Phys Ther. 1984;5:230–239. doi: 10.2519/jospt.1984.5.5.230. [DOI] [PubMed] [Google Scholar]
- 31.Burkett LN. Causative factors in hamstring strains. Med Sci Sports. 1970;2:39–42. [PubMed] [Google Scholar]
- 32.Knapik JJ, Bauman CL, Jones BH, Harris JM, Vaughan L. Preseason strength and flexibility imbalances associated with athletic injuries in female collegiate athletes. Am J Sports Med. 1991;19(7681) doi: 10.1177/036354659101900113. [DOI] [PubMed] [Google Scholar]
- 33.Gofton JP. Persistent low back pain and leg length disparity. J Rheumatol. 1985;12(4):747–750. [PubMed] [Google Scholar]
- 34.Menelaus MB. Management of limb inequality. Churchill Livingstone; New York: 1991. [Google Scholar]
- 35.Patriquin DA. Lift therapy: a study of results. J Am Osteopath Assoc. 1964;63:840–844. [PubMed] [Google Scholar]
- 36.Pratt WA. The lumbopelvic torsion syndrome. J Am Osteopath Assoc. 1952;51:335–341. [PubMed] [Google Scholar]