Abstract
This pilot study examined the efficacy of a spiritually based educational intervention for increasing informed decision making for prostate cancer screening among African-American men. The intervention appeared to be effective for some study outcomes, such as knowledge and self-efficacy for screening informed decision making.
Keywords: Prostate cancer screening, informed decision making, African-American men, church-based, health communication, spiritually based communication interventions
Introduction
Health communication interventions have been modestly effective for increasing informed decision making for prostate cancer screening among African-American men; however, knowledge and informed decision making is still questionable even with screening. Church-based programs may be more effective if they are spiritually based in nature.
Objective
The aims of the present study were to implement and provide an initial evaluation of a spiritually based prostate cancer screening informed decision making intervention for African-American men who attend church, and determine its efficacy for increasing informed decision making.
Design and Method
Churches were randomized to receive either the spiritually based or the non-spiritual intervention. Trained community health advisors, who were African-American male church members, led an educational session and distributed educational print materials. Participants completed baseline and immediate follow-up surveys to assess the intervention impact on study outcomes.
Results
The spiritually based intervention appeared to be more effective in areas such as knowledge, and men read more of their materials in the spiritually based group than in the non-spiritual group.
Conclusions
Further examination of the efficacy of the spiritually based approach to health communication is warranted.
Level of Evidence – !!
In the United States, prostate cancer is the leader in male cancer incidence and is second in cancer mortality (American Cancer Society [ACS], 2008). The disease takes a particularly high toll among African-American men who are 60% more likely to develop prostate cancer and twice as likely to die from the disease as are European-American men (Stanford et al., 1999). The National Institute on Aging's (2000) strategic plan on health disparities recognized that African-American men suffer from prostate cancer more than other men, and called for culturally appropriate strategies and interventions aimed at decreasing this disparity.
Consistent with the idea that informed decision making is more than just knowledge (Bowen et al., 2006), informed decision making is conceptualized as being composed of a variety of factors, including knowledge of the disease, knowledge of the relationship between screening and mortality, knowledge of the controversy regarding screening, beliefs regarding screening for the disease, self-efficacy for screening, and preparation for and stage of decision making regarding screening. Appropriate interventions in this context include offering screening and encouraging the man to make an informed decision about screening that is right for him based on his risk profile and values.
Educational interventions are one approach to increasing informed decision making for prostate cancer screening. Sometimes called decision aids, such educational programs should address cultural beliefs if they are to be maximally effective (Chan et al., 2003). They should also be developed using community-based methods in which the priority population is involved in every stage from intervention planning to implementation and evaluation (Woods, Montgomery, & Herring, 2004). A community approach is suggested to be more appropriate than a provider or health system-based approach for reaching African-American men with prostate cancer information (Weinrich, Boyd, Bradford, Mossa, & Weinrich, 1998).
The church is often used as an access point to reach African Americans with health information. Several church-based efforts have been effective for increasing prostate cancer knowledge and/or screening among African-American men (Boehm et al., 1995; Tingen, Weinrich, Heydt, Boyd, & Weinrich, 1998; Weinrich Holdford et al., 1998; Wilkinson, List, Sinner, Dai, & Chodak, 2003).
Problem Statement
These church-based interventions often resulted in statistically significant gains in knowledge; however, knowledge among African-American men remained relatively low, as was participation in screening. Further, informed decision making is often narrowly defined as being an increase in knowledge. Although many of these programs were delivered in church settings, none of them report having used a spiritually based approach (Winett et al., 1999). Using the church solely as a venue for the delivery of a secular (non-spiritual) health message may under-utilize the potential of churches for health promotion in this population.
Purpose
Spiritually based cancer communication interventions can be developed by using relevant spiritual themes to frame the cancer educational message, thus increasing personal relevance by putting health in a spiritual context. Use of a spiritually based approach may increase the cultural appropriateness of the intervention (Harris, Thoresen, McCullough, & Larson, 1999; Winett et al., 1999) and optimize use of the church as a social network for health promotion.
The aims of the present study were to implement and provide an initial evaluation of a spiritually based prostate cancer screening informed decision making intervention for African-American men who attend church to determine its efficacy for increasing informed decision making. In this context, one aspect of African-American culture was addressed through the spiritually based nature of the intervention.
Definition of Terms
In this context, the term spiritually based is used as opposed to religiously based. The terms religion and spirituality have been recognized as distinct yet overlapping constructs (Musick, Traphagan, Koenig, & Larson, 2000). Thoresen (1998) defined religion as “an organized system of beliefs, practices, rituals, and symbols…” (p. 415). Spirituality is a broader construct, involving a search for meaning and purpose that can, but does not have to, involve religion. Spirituality involves the territory that overlaps between the two constructs. In the formative research for the intervention development, when referring to what the research team would typically think of as religious constructs, the community used the term spiritual as opposed to religious. The current approach does involve religious concepts (such as scripture), as well as the broader concepts (such as balance of healthy body, mind, and spirit) of a more spiritual nature.
Hypothesis
Informed decision making was operationalized by means of knowledge of prostate cancer, knowledge of the relationship of screening to mortality, knowledge of the controversy regarding prostate cancer screening, prostate cancer screening beliefs, self-efficacy for screening, self-efficacy for decision making, perception of barriers to screening, preparation for decision making, and stage of decision making. Data were also collected on participant ratings of the acceptability/appropriateness of the intervention received. It was hypothesized that the spiritually based group would report higher pre/post-change scores on the measures of informed decision making and higher post-test scores on the acceptability/appropriateness of the intervention than the non-spiritual group.
Theoretical Framework
The intervention incorporated social cognitive theory (Bandura, 1986) through the use of peer role models and aimed to increase self-efficacy for screening. The Health Belief Model (Rosenstock, Strecher, & Becker, 1988) was incorporated by attempting to identify barriers to informed decision making and screening, and to increase knowledge and perceived benefits of screening. This is further discussed elsewhere (Holt et al., In Press).
Literature Review
Several community and/or church-based interventions have demonstrated success in reaching African-American men with prostate cancer education. In one church-based program delivered by prostate cancer survivors who served as lay health educators (Boehm et al., 1995), 102 African-American men completed the Prostate Cancer Screening Knowledge Inventory and the Prostate Cancer Screening Self-Efficacy Scale. From baseline to follow up, measures for knowledge and self-efficacy for screening improved significantly.
A church-based prostate cancer educational intervention was offered by Weinrich, Holdford et al. (1998) and attended by over 500 African-American men. Attendees received a voucher for a free prostate cancer examination that they could take to their doctor of choice. Attendance at the program was significantly predicted by having a member of the congregation previously diagnosed with prostate cancer.
Tingen and colleagues (1998) used a peer educator approach and recruited a sample of 1,522 men (72% African American) from churches and other community venues, including barber-shops, industries, housing projects, and car dealerships, to participate in an educational program on prostate cancer screening. The program had a significant impact on participation in screening.
More recently, Wilkinson and coauthors (2003) recruited 900 African-American men from multiple venues to participate in a one-hour educational seminar aimed at increasing awareness about prostate cancer. Effectiveness of the intervention was verified by the comparison of pre- and post-program scores on a multiple-choice instrument assessing knowledge. Mean scores improved from 26% correct at baseline to 73% correct at follow up. Further, 63% of the participants indicated they intended to obtain screening after the program.
The use of spiritually based communication interventions to encourage breast and cervical cancer early detection was supported by Matthews, Berrios, Darnell, and Calhoun (2006), who conducted focus groups for a church-based REACH 2010 project. Results showed that the participants thought using scripture to frame a health message was important, and they voiced a strong sense of the relationship between religion, spirituality, and health.
Methods
Research Design
The study used a pre-post randomized controlled trial in which churches were randomized to receive either the spiritually based or the comparison non-spiritual intervention condition. Baseline and immediate follow-up surveys assessed study outcomes.
Setting and Recruitment
Two area Baptist churches were recruited by convenience and through community contacts. These churches were in an urban area and were selected based on being comparable in size and structure. The churches were then randomized to the spiritually based or non-spiritual intervention.
African-American men ages 45 and older who had not had prostate cancer were recruited through word of mouth, flyers, and announcements in the church bulletins and on church television monitors. The study protocol was approved by the Institutional Review Board at the University of Alabama at Birmingham. Participants provided written informed consent, were told they could withdraw at any time without penalty, and could refuse to answer any survey question for any reason. Study participants received a gift card of $25.00 at the end of the session.
Intervention Description
The intervention built on previous work with African-American women wherein a spiritually based approach was used to encourage mammography screening (Holt, Kyles, Wiehagen, & Casey, 2003). Many of the processes of intervention development and pilot testing that were successful in the previous study were applied to the present study. The present intervention covered content areas, including anatomy and physiology, incidence, development, symptoms and treatment of prostate cancer, assessment of one's personal risk factors for prostate cancer (age, race, and family history), screening risks and benefits, and the importance of initial and repeat screening.
Because the focus of the intervention was informed decision making, potential risks of screening were also addressed, and each man was encouraged to weigh his own risk profile and make a decision regarding screening with which he was comfortable, given his risk profile. For example, a man with a strong family history of prostate cancer might give more serious consideration to screening than a man with a normal risk profile who may decide that for himself the risks of screening (such as false positive, unnecessary biopsy) are not worth the potential benefit.
The intervention consisted of an educational session led by a trained community health advisor (CHA) from each church. The pastor in each church identified a man to serve as the CHA. The study coordinator met with the potential CHA, introduced the project, verified his interest, and set up a time for his training session.
CHAs were trained according to their availabilities, each receiving a half-day training on a weekday. CHAs trained separately in the spiritually based and non-spiritual conditions, and each CHA received training on only their assigned condition. They received training in the role of a CHA, the aims of the project, cancer, prostate cancer, informed decision making for screening, ethics in research, and how to deliver the material to the experimental group in a spiritually based manner (see Figure 1 for outline of training curriculum). Before being certified, the CHAs conducted and passed a practice educational session where they were rated by members of the project team and passed a knowledge examination on the material at a score of 80% or higher.
Figure 1. Community Health Advisor Training Curriculum.
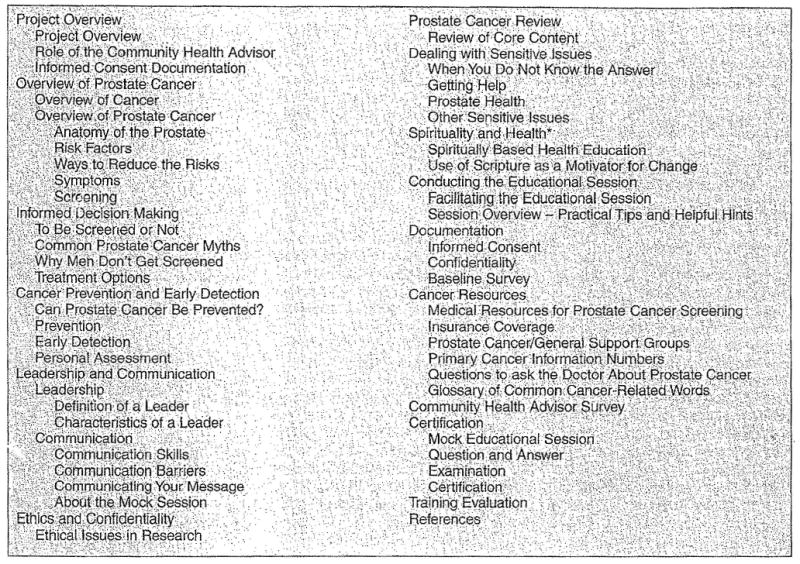
*Covered in spiritually based group only.
Each session was conducted in a “Sunday school” fashion in which the CHA taught the session material (the lesson) to the class at church, using printed materials as a guide as Sunday school teachers use their lesson or the Bible as a guide. Each man who attended received his own copy to follow along and keep.
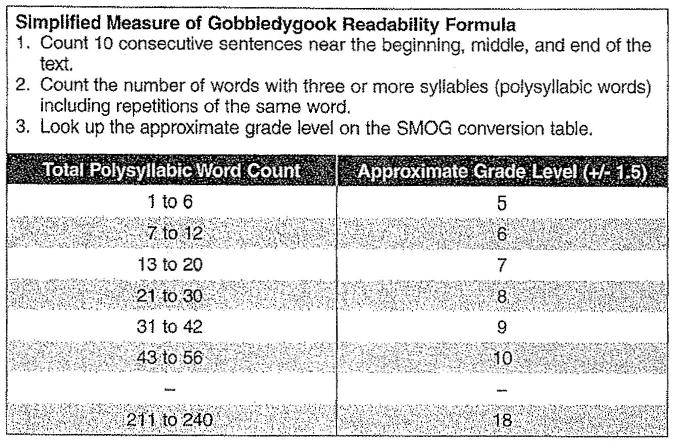
The materials consisted of a professionally designed and produced 16-page full-color booklet with information on the aforementioned topics. The booklet was developed and pilot tested for this project (Holt et al., In Press), The materials contained spiritual content along with wellness and prostate information. The print materials were tested for readability using the Simplified Measure of Gobbledygook (SMOG) formula and revised to the 6th grade level (see Figure 2). The non-spiritual intervention was identical in all ways as the spiritual except that the content did not include spiritual themes or scripture. The development and pilot testing of the print materials used as the basis for the intervention are described elsewhere (Holt et al., In Press).
Figure 2. Simplified Measure of Gobbledygook Readability Formula Developed by Harold C. McGraw, Office of Educational Research, Baltimore County School, Towson, MD.
Procedure
Educational sessions were held at a time of convenience for participants. All data were collected in a single session. Sessions began with a brief introduction to the project and written informed consent procedure in which study staff summarized the document and ensured that all questions were addressed. Study staff distributed the self-administered baseline survey. The CHAs then conducted their group educational session that generally lasted an hour. CHAs taught either a spiritually based or non-spiritual educational session, based on random assignment by church. Finally, study staff administered an immediate follow-up survey to assess study outcomes.
Instruments
The impact of the intervention was evaluated through use of pre-test and immediate follow-up post-test self-administered questionnaires assessing the study outcomes. Responses were summed to form a composite score for each scale.
Prostate cancer screening history
Screening history was assessed by first defining digital rectal examination (DRE) and prostate specific antigen (PSA) tests, and then asking participants if they had ever had the test, and if so, the length of time since the tests were performed (within the past 12 months; more than 12 months ago).
Knowledge
Three types of knowledge were assessed. A 9-item instrument was used to assess knowledge of prostate cancer and risk factors, based on a previously validated instrument used to assess breast cancer knowledge (Lukwago et al., 2003). To examine knowledge specifically about the screening controversy, another 4-item instrument was developed to assess aspects of the screening controversy. Finally, a single item assessed the men's awareness of whether prostate cancer screening would prevent prostate cancer mortality. This item was developed by the investigators.
For each of these instruments, correct responses were scored and summed. Possible scores for the Knowledge of Prostate Cancer Scale ranged from 0 to 9; possible scores for the Knowledge of the Screening Controversy Scale from 0 to 4. The single item Addressing Knowledge of the Relationship of Screening and Mortality was scored as either incorrect or correct for a possible score of 0 or 1. Higher scores indicated higher levels of knowledge.
Reliability as internal consistency for the Knowledge of Prostate Cancer Scale was assessed by means of Cronbach's alpha and found to be acceptable in the present sample given the varied content domain (Cronbach's alpha = 0.66). Internal consistency for the Knowledge of the Screening Controversy Scale was low in the present sample but reflected the varied content domain (Cronbach's alpha = 0.43). In this way, these instruments function more as indices than as scales (Helms, Henze, Sass, & Mifsud, 2006).
Prostate cancer beliefs
An existing Prostate Cancer Beliefs Scale was used to assess prostate cancer beliefs (Cormier, Kwan, Reid, & Litwin, 2002). This 5-item instrument was scored by summing the agree/affirmative responses; possible scores range from 0 to 5, with higher scores indicating more positive beliefs associated with the benefits of prostate cancer screening. Internal consistency was acceptable in the present sample (Cronbach's alpha = 0.75).
Self-efficacy
Self-efficacy was assessed for three behaviors: screening for prostate cancer, informed decision making regarding screening by means of PSA, and informed decision making regarding screening by means of a DRE. Self-efficacy for screening was assessed using the four-item Prostate Cancer Screening Self-Efficacy Scale used in previous research with this population (Boehm et al., 1995). Participant responses were obtained on a 5-point Likert scale ranging from 1 to 5, with 1 indicating “not at all sure” and 5 indicating “very sure.” Responses were summed for a composite score operationalizing self-efficacy, with possible scores ranging from 4 to 20; higher scores indicated higher degrees of self-efficacy, The scale had strong internal reliability in the present sample (Cronbach's alpha = 0.81). The instrument was also shown to have discriminant validity in previous work (Boehm et al., 1995).
Self-efficacy for informed decision making about screening was assessed using a previous item used for PSA (Gattellari & Ward, 2003) and an additional item adapted to assess self-efficacy for informed decision making for DRE. These items are treated as two separate and single items, and they are further independent measures from self-efficacy for prostate cancer screening.
Perceived barriers to prostate cancer screening
Not having identified an existing instrument in the literature, the authors developed an 8-item instrument to assess common barriers to having a prostate cancer screening based on an instrument from the mammography screening literature (Lukwago et al., 2003). Participants were asked to indicate if they agreed (score of 1) or disagreed (score of 0) that the item was a barrier. This instrument was scored by summing the responses, with scores ranging from 0 to 8, with higher scores indicating that the participant perceived a larger number of barriers to screening. Internal consistency was modest (Cronbach's alpha = 0.50) but sufficient given the variety of concepts assessed (cost, time, embarrassment) and comparable to previous work (Lukwago et al., 2003).
Preparation for decision making
The Preparation for Decision Scale assessed participants' evaluation of the intervention's impact upon their preparation for making a screening decision (Graham & O'Conner, 2005). This instrument consisted of 10 items to which the participant could respond on a 1 to 5 Likert scale wherein 1 indicated “not at all” and 5 indicated “a great deal.” The responses were summed for a composite score; possible scores ranged from 10 to 50, with higher scores indicating a higher preparation for making a screening decision. Internal consistency was strong in the present sample (Cronbach's alpha = 0.99).
Acceptability/appropriateness
Immediately after the session, the men were asked if they believed the intervention was both acceptable and appropriate by assessing these variables in closed-ended fashion. They were also asked how much they liked the session. Participants were asked to write open-ended comments, such as what they learned from the session and if they found the session to be different from information typically received in a physician's office.
Results
Initial examination of the data was conducted to evaluate the sample distributions and identify potential entry errors. Participant mean age, education, and income were compared between the study groups by t-tests. Baseline screening rates for PSA and DRE were compared using the chi-square test.
Pre-test and post-test scores were calculated for the scales. The scores were approximately normally distributed, and group means for these measures were compared using t-tests. Items that were observed only at a single time point showed skewed distributions, and comparisons were conducted using Mann-Whitney U tests. For frequency-data, chi-square tests were conducted (except with low expected frequencies when Fisher's exact test was used).
Sample
A total of 49 men ages 45 to 90 (M = 56,08, SD = 9.46) participated. The median household income before taxes was in the $50,000 to $60,000 bracket, and ranged from less than $5,000 to more than $70,000. Six (12.2%) reported having a family history of prostate cancer. About half (51%) indicated that they had ever had a PSA test, and of those, 28.6% indicated that they had a PSA test in the past 12 months. More than half (69%) indicated that they had ever had a DRE, and of those, 38.8% indicated that they had a DRE within the past 12 months. Participant characteristics are summarized in Table 1.
Table 1. Demographic Characteristics of Participants (N = 49).
| Characteristic | n | % |
|---|---|---|
| Relationship Status | ||
| Single | 5 | 10.2 |
| Married | 38 | 77.5 |
| Living with partner | 1 | 2.0 |
| Separated/divorced | 2 | 4.1 |
| Widowed | 1 | 2.0 |
| No answer | 2 | 4.1 |
| Education | ||
| Less than high school | 3 | 6.0 |
| High school/GED | 15 | 30.6 |
| Some college or tech school | 16 | 32.6 |
| College graduate | 13 | 26.5 |
| No answer | 2 | 4.1 |
| Employment | ||
| Not employed | 2 | 4.1 |
| Receiving disability | 5 | 10.2 |
| Part-time or retired | 4 | 8.2 |
| Full-time | 28 | 57.1 |
| No answer | 10 | 20.4 |
| Health Insurance* | ||
| Medicaid | 6 | 12.2 |
| Medicare | 7 | 14.3 |
| Private | 34 | 69.5 |
| Other | 4 | 8.2 |
| No answer | 2 | 4.1 |
Exceeds 100% because participants marked all that apply.
Hypothesis Testing
Table 2 provides the means and the standard deviations of the pre- and post-measures of informed decision making for the non-spiritual and the spiritual groups. Table 3 summarizes the comparisons of pre-post differences and post-only outcomes between the study groups. Table 4 presents the comparisons of the categorical outcomes between the study groups. Study group differences were not significant for any of the study outcomes.
Table 2. Means and Standard Deviations for the Pre- and Post-Test Measures of informed Decision Making for Non-Spiritual and Spiritual Intervention Groups.
| Measure | Non-Spiritual | Spiritual | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre-Test | Post-Test | Pre-Test | Post-Test | |||||||||
| M | SD | n | M | SD | n | M | SD | n | M | SD | n | |
| Knowledge of prostate cancer | 6.50 | 2.22 | 16 | 8.85 | 0.38 | 13 | 6.41 | 2.01 | 29 | 8.39 | 1.07 | 28 |
| Knowledge of relationship of screening and mortality | 0.07 | 0.26 | 15 | 0.24 | 0.44 | 17 | 0.10 | 0.30 | 31 | 0.07 | 0.25 | 30 |
| Knowledge of screening controversy | 1.93 | 1.22 | 15 | 2.00 | 1.17 | 17 | 1.36 | 0.78 | 28 | 2.14 | 0.89 | 28 |
| Beliefs regarding screening | 3.54 | 1.17 | 13 | 4.24 | 1.44 | 17 | 4.03 | 1.24 | 29 | 4.48 | 0.83 | 29 |
| Self-efficacy for informed decision making for screening | 17.21 | 4.17 | 14 | 18.07 | 3.63 | 15 | 16.90 | 4.54 | 30 | 18.72 | 3.34 | 29 |
| Self-efficacy for informed decision making for PSA | 4.19 | 1.11 | 16 | 4.41 | 1.33 | 17 | 4.16 | 1.21 | 31 | 4.76 | 0.64 | 29 |
| Self-efficacy for informed decision making for DRE | 4.13 | 1.09 | 16 | 4.59 | 1.00 | 17 | 4.17 | 1.21 | 30 | 4.76 | 0.62 | 29 |
| Barriers to screening | 0.00 | 0.00 | 12 | 0.25 | 0.78 | 16 | 0.31 | 0.60 | 29 | 0.35 | 0.69 | 26 |
Table 3. Comparisons of Pre- and Post-Test Differences and Post-Test-Only Outcomes Between the Study Groups.
| Pre/Post-Test Change Scores | Non-Spiritual | Spiritual | t | df | |||||
|---|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | ||||||
| Knowledge of prostate cancer | 1.82* | 1.08 | 2.15* | 1.75 | -0.58 | 36 | |||
| Knowledge of relationship of screening and mortality | 0.14∼ | ||||||||
| Knowledge of screening controversy | 0.36 | 1.08 | 0.76* | 1.05 | -1.14 | 37 | |||
| Beliefs regarding screening | 0.83 | 1.75 | 0.50$ | 1.53 | 0.61 | 38 | |||
| Self-efficacy for screening | 2.00* | 2.97 | 1.29 | 4.13 | 0.56 | 39 | |||
| Self-efficacy informed decision making regarding PSA | 0.44 | 1.46 | 0.55* | 1.18 | -0.29 | 43 | |||
| Self-efficacy informed decision making regarding DRE | 0.50 | 1.37 | 0.59* | 1.12 | -0.23 | 43 | |||
| Barriers to screening | 0.33 | 0.89 | 0.04 | 0.61 | 1.18 | 35 | |||
| Post-Only Scores | MDN | n | 25th Percentile | 75th Percentile | p@ | ||||
| How much liked | 5 | 48 | 5 | 5 | 0.29 | ||||
| Acceptable | 7 | 44 | 7 | 7 | 0.69 | ||||
| Appropriate | 7 | 43 | 6 | 7 | 0.51 | ||||
| Preparation for decision making | 50 | 40 | 47.25 | 50 | 0.91 | ||||
Notes:
pre-post increase was significant at p < 0.05,
p < 0.10 ∼ knowledge item with different response scale analyzed separately with chi-square,
by Mann-Whitney U test.
Table 4. Comparisons of Categorical Outcomes Between Study Groups.
| Non-Spiritual (n = 18) | Spiritual (n = 31) | n | pˆ | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Stage of Decision Making | -1 0/11 | 0 9/11 | 1 2/11 | 2 0/11 | 4 0/11 | -1 2/17 | 0 12/17 | 1 1/17 | 2 1/17 | 4 1/17 | 28 | 0.70 |
| How Much Read | All 8/18 | Most 6/18 | Some 4/18 | None 0/18 | All 25/30 | Most 2/30 | Some 2/30 | None 1/30 | 48 | 0.0088 | ||
| Liked Compared to Other information from Doctor's Office | More 11/15 | Same 4/15 | Less# 0/15 | More 24/26 | Same 2/26 | Less# 0/27 | 41 | 0.11 | ||||
Notes:
by Fisher's exact test because low expected cell frequencies occurred;
0 respondents indicated they liked the materials less than other information; thus, this category was excluded from analysis. Values in the cells represent frequencies/N.
Knowledge
Scores for the subscales for knowledge for both groups increased significantly from pre- to post-test except for the non-spiritual group, whose scores for knowledge of the screening controversy did not increase from pre- to post-assessment. The spiritual group's scores did increase significantly.
Beliefs
Prostate cancer beliefs did not increase from pre- to post-test in the non-spiritual group, and they increased only marginally in the spiritual group.
Self-efficacy
Scores on the screening self-efficacy scale increased significantly from pre- to post-test in the non-spiritual group only. Self-efficacy for informed decision making (for both PSA and DRE) increased significantly from pre- to post-test only in the spiritually based group.
Perceived barriers to screening
Perceived barriers were low in both groups at the pre-test measure and did not decrease significantly from pre- to post-test.
Stage of decision making
With regard to the stage of decision making, most (n = 13, 26.5%) reported at baseline that they had already made a screening decision and were unlikely to change their mind, and this was also the case after the session (n = 18, 36.7%). Most did not change their stage of decision making from pre- to post-test (see Table 4).
Acceptability
Both groups liked the intervention and found it to be acceptable and appropriate (non-spiritual, M = 4.89, SD = 0.32, spiritual, M = 4.97, SD = 0.18). Both groups felt that the intervention helped them prepare to make an informed decision about prostate cancer screening (non-spiritual, M = 47.15, SD = 7.03; spiritual, M = 46.15, SD = 10.03). Those in the spiritually based group reported reading significantly more of their print materials during the session, with 80.6% reporting that they had read the entire booklet compared to 44.4% in the non-spiritual group (p < 0.01).
Participant Reactions to the Intervention
In addition to the closed-ended survey items, participants were asked a number of open-ended questions regarding the program. When asked how the educational session was different from information they would usually find in a doctor's office, participants indicated: “had time to ask more questions,” “up close with people I know,” and “someone you know you can now talk to about it.” When asked what they learned from the session, participants indicated: “that I need to be checked even if there are no symptoms,” “Black men are at high risk,” and “talking about it helps.”
Discussion
In summary, both church-based educational programs on informed decision making for prostate cancer screening were very well received by participants. This is a testimony to the impact and importance of working closely with the community through all stages of intervention planning, development, and implementation. There was some suggestion in the trend of the data that the spiritually based intervention may have a differential impact in some areas; however, due to the small sample size, these effects need to be verified with greater statistical power.
Further, the hypothesis that the spiritually based content alone would improve efficacy of the informed decision making program is a difficult one to confirm because both interventions were of high quality, community-based, targeted, and theory-based. Thus, it may be expected that both interventions would have a significant impact upon study outcomes. The question of whether a spiritually based intervention has more impact than a non-spiritual intervention appears to merit further study.
Men who attended the spiritually based session reported reading significantly more of the printed educational materials than those who attended the non-spiritual session. This is consistent with the idea that the spiritually based approach would be more personally relevant for this population and would catch their attention to a greater degree than a non-spiritual program. Although this increased reading may have resulted in increases in pre-post knowledge relative to the non-spiritual group, it did not result in significant group differences in the measures of informed decision making, stage of decision making, or preparation for decision making. It is possible that a more in-depth intervention would be needed to assess impact on these outcomes or that these are outcomes that might be expected to appear in a longer-term follow up.
The program increased self-efficacy from baseline to follow up for screening among the non-spiritual group only. It influenced the ability of participants to make an informed choice about having a screening among the spiritual group only. This, along with suggestions of patterns of increased knowledge and changes in beliefs among the spiritual group, speaks to the potential of this approach to impact informed decision making in future, more extensive trials. The present findings are comparable to another project in which awareness about prostate cancer was increased through the use of African-American health educators (Wilkinson et al., 2003).
Limitations
The present findings should be considered preliminary and within the context of several limitations. The sample size was relatively small and resulted in modest statistical power for the examination of between-group differences. For this reason, an examination of trends across means and frequencies/percentages may be more informative than p-values in the present context. While it is possible that the pre-test/post-test differences observed could have been due to a testing effect only, a testing effect would not be expected to account for differential trends between groups.
The findings may not be generalizable to non-church settings, to other geographic areas of the country, or to men of other race/ethnicities. Similarly, while the strength of the targeted approach is that it allows for an intervention developed specifically for this particular population (Kreuter & Wray, 2003), it would have to be modified for use with other populations. For example, denominational variation in health behaviors and outcomes is an important consideration when developing church-based health interventions, and it needs to be assessed carefully and accurately (Matthews, 1999).
There are other aspects of African-American culture, such as racial pride and collectivism (Lukwago, Kreuter, Bucholtz, Holt, & Clark, 2001) that were not addressed in the present intervention. The focus of this project was on the spiritual/religious aspects, being that they are central to African-American culture (Lincoln & Mamiya, 1990) and associated with health behaviors and outcomes (Koenig, McCullough, & Larson, 2001).
Finally, some instruments used to assess study outcomes were limited in their internal consistency. The current figures may be viewed as appropriate since the instruments are relatively brief and would be expected given their varied content (Helms et al., 2006; Nunnally & Bernstein, 1994). However, the modest internal reliability of the study outcomes may also be viewed as a limitation of the current investigation in terms of uncertainty of where the intervention actually had its effects (such as knowledge and beliefs).
Implications
The present findings suggest that a spiritually based approach may be promising for use in promoting awareness of prostate cancer among church-attending African-American men.
Nursing Practice
With regard to practice in clinical settings, it may behoove nursing practitioners to be aware of the role of religious/spiritual beliefs among the populations they serve. Such beliefs may be particularly relevant for African-American populations. Religious/spiritual beliefs may play a role in health decision-making, behaviors, and coping with serious illness.
Future Research
Future studies should examine the long-term efficacy of the CHA-led spiritually based program on informed decision making for prostate cancer screening. A trial with more statistical power, a more intensive intervention, and longer-term follow up could provide more conclusive evidence of whether the spiritually based approach is effective for health promotion in this population.
Conclusions
In summary, the findings of this pilot project suggest that further study of spiritually based approaches to health education and promotion may be indicated for use with African-American populations in faith-based settings.
Acknowledgments
This study was supported by a grant from the University of Alabama at Birmingham Comprehensive Cancer Center through the American Cancer Society Institutional Research Grant Program (#ACS IRG-60-001-47, NCI-CA-13148-31) and was approved by the University of Alabama at Birmingham Institutional Review Board.
Contributor Information
Cheryl L. Holt, Department of Public and Community Health, School of Public Health, College Park, MD.
Theresa Ann Wynn, University of Alabama at Birmingham, School of Medicine-Division of Preventive Medicine, Birmingham, AL.
Mark S. Litaker, Department of Diagnostic Sciences, University of Alabama at Birmingham, Birmingham, AL.
Penny Southward, Media for Health, Inc., Birmingham, AL.
Sanford E. Jeames, University of Massachusetts, Donahue Institute, Donahue Institute, Hadley, MA.
Emily K. Schulz, A.T. Still University, Arizona School of Health Sciences, Mesa, AZ.
References
- American Cancer Society (ACS) Cancer facts and figures 2008. Atlanta, Georgia: Author; 2008. [Google Scholar]
- Bandura A. Social foundations of thought and action: A social cognitive theory. Englewood Cliffs, NJ: Prentice-Hall; 1986. [Google Scholar]
- Boehm S, Coleman-Burns P, Schlenk EA, Funnell MM, Parzuchowski J, Powell IJ. Prostate cancer in African American men: Increasing knowledge and self-efficacy. Journal of Community Health Nursing. 1995;12:161–169. doi: 10.1207/s15327655jchn1203_4. [DOI] [PubMed] [Google Scholar]
- Bowen DJ, Allen JD, Vu T, Johnson RE, Fryer-Edwards K, Hart A. Theoretical foundations for interventions designed to promote informed decision making for cancer screening. Annals of Behavioral Medicine. 2006;32:202–210. doi: 10.1207/s15324796abm3203_5. [DOI] [PubMed] [Google Scholar]
- Chan EC, Vernon SW, O'Donnell FT, Ahn C, Greisinger A, Aga DW. Informed consent for cancer screening with prostate-specific antigen: How well are men getting the message? American Journal of Public Health. 2003;93:779–785. doi: 10.2105/ajph.93.5.779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cormier L, Kwan L, Reid K, Litwin MS. Knowledge and beliefs among brothers and sons of men with prostate cancer. Urology. 2002;59:895–900. doi: 10.1016/s0090-4295(01)01657-0. [DOI] [PubMed] [Google Scholar]
- Gattellari M, Ward JE. Does evidence-based information about screening for prostate cancer enhance consumer decision-making? A randomized controlled trial. Journal of Medical Screening. 2003;10:27–39. doi: 10.1258/096914103321610789. [DOI] [PubMed] [Google Scholar]
- Graham ID, O'Conner AM. Preparation for decision making scale. 2005 doi: 10.1016/j.pec.2009.05.012. Retrieved June 11, 2009, from http://decisionaid.ohri.ca/eval.html#PrepDM. [DOI] [PubMed]
- Harris AHS, Thoresen CR, McCullough ME, Larson DB. Spiritually and religiously oriented health interventions. Journal of Health Psychology. 1999;4:413–433. doi: 10.1177/135910539900400309. [DOI] [PubMed] [Google Scholar]
- Helms JE, Henze KT, Sass TL, Mifsud VA. Treating Cronbach's alpha reliability coefficients as data in counseling research. The Counseling Psychologist. 2006;34:630–660. [Google Scholar]
- Holt CL, Kyles A, Wiehagen T, Casey C. Development of a spiritually based breast cancer educational booklet for African American. 2003. [DOI] [PubMed] [Google Scholar]
- Holt CL, Wynn TA, Southward P, Litaker MS, Jeames S, Schulz E. Development of a spiritually based educational intervention to increase informed decision making for prostate cancer screening among church-attending African American men. Journal of Health Communication. doi: 10.1080/10810730903120534. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koenig HG, McCullough ME, Larson DB. Handbook of religion and health. New York: Oxford University Press; 2001. [Google Scholar]
- Kreuter MW, Wray RJ. Tailored and targeted health communication: Strategies for enhancing information relevance. American Journal of Health Behavior. 2003;27:S227–232. doi: 10.5993/ajhb.27.1.s3.6. [DOI] [PubMed] [Google Scholar]
- Lincoln CE, Mamiya LH. The Black church in the African American experience. Durham, NC: Duke University Press; 1990. [Google Scholar]
- Lukwago SL, Kreuter MW, Bucholtz DC, Holt CL, Clark EM. Development and validation of brief scales to measure collectivism, religiosity, racial pride, and time orientation in urban African American women. Family and Community Health. 2001;24:63–71. doi: 10.1097/00003727-200110000-00008. [DOI] [PubMed] [Google Scholar]
- Lukwago SL, Kreuter MW, Holt CL, Steger-May K, Bucholtz DC, Skinner CS. Sociocultural correlates of breast cancer knowledge and screening in urban African American women. American Journal of Public Health. 2003;93:1271–1274. doi: 10.2105/ajph.93.8.1271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthews AK, Berrios N, Darnell JS, Calhoun E. A qualitative evaluation of a faith-based breast and cervical cancer screening intervention for African American women. Health Education and Behavior. 2006;33:643–663. doi: 10.1177/1090198106288498. [DOI] [PubMed] [Google Scholar]
- Matthews DA. Religious commitment and health status. Do people of different religious denominations have different average life expectancies? Archives of Family Medicine. 1999;8:476. doi: 10.1001/archfami.8.6.476-a. [DOI] [PubMed] [Google Scholar]
- Melnyk BM, Fineout-Overholt E. Evidence-based practice in nursing & healthcare: A guide to best practice. Philadelphia: Lippincott, Williams & Wilkins; 2005. [Google Scholar]
- Musick MA, Traphagan JW, Koenig HG, Larson DB. Spirituality in physical health and aging. Journal of Adult Development. 2000;7:73–86. [Google Scholar]
- National Institute on Aging. Strategic plan. 2000 Retrieved June 11, 2009, from http://www.nia.nih.gov/AboutNIA/StrategicPlan/
- Nunnally JC, Bernstein IH. Psychometric theory. 3rd. New York: McGraw-Hill; 1994. [Google Scholar]
- Rosenstock IM, Strecher VJ, Becker MH. Social learning theory and the health belief model. Health Education and Behavior. 1988;15:175–183. doi: 10.1177/109019818801500203. [DOI] [PubMed] [Google Scholar]
- Stanford JL, Stephenson RA, Coyle LM, Cerhan J, Correa R, Eley JW, et al. Prostate cancer trends 1973-1995, SEER Program, National Cancer Institute. Bethesda, MD: National Cancer Institute; 1999. [Google Scholar]
- Thoresen CE. Spirituality, health, and science: The coming revival? In: Roth RS, Kurpius SR, editors. The emerging role of counseling psychology in health care. New York: W.W Norton; 1998. pp. 409–431. [Google Scholar]
- Tingen MS, Weinrich SP, Heydt DD, Boyd MD, Weinrich MC. Perceived benefits: A predictor of participation in prostate cancer screening. Cancer Nursing. 1998;21:349–357. doi: 10.1097/00002820-199810000-00006. [DOI] [PubMed] [Google Scholar]
- Weinrich SP, Boyd MD, Bradford D, Mossa MS, Weinrich M. Recruitment of African Americans into prostate cancer screening. Cancer Practice. 1998;6:23–30. doi: 10.1046/j.1523-5394.1998.1998006023.x. [DOI] [PubMed] [Google Scholar]
- Weinrich S, Holdford M, Boyd M, Creanga D, Cover K, Johnson A, et al. Prostate cancer education in African American churches. Public Health Nursing. 1998;15:188–195. doi: 10.1111/j.1525-1446.1998.tb00338.x. [DOI] [PubMed] [Google Scholar]
- Wilkinson S, List M, Sinner M, Dai L, Chodak G. Educating African-American men about prostate cancer: Impact on awareness and knowledge. Urology. 2003;61:308–313. doi: 10.1016/s0090-4295(02)02144-1. [DOI] [PubMed] [Google Scholar]
- Winett RA, Anderson ES, Whiteley JA, Wojcik JR, Rovniak LS, Graves KD, et al. Church-based health behavior programs: Using social cognitive theory to formulate interventions for at-risk populations. Applied and Preventive Psychology. 1999;8:129–142. [Google Scholar]
- Woods VD, Montgomery SB, Herring RP. Recruiting Black/African American men for research on prostate cancer prevention. Cancer. 2004;100:1017–1025. doi: 10.1002/cncr.20029. [DOI] [PubMed] [Google Scholar]
Additional Readings
- Centers for Disease Control and Prevention (CDC) Behavioral risk factor surveillance system survey questionnaire. Atlanta, Georgia: Author; 2006. [Google Scholar]
- Witmer A, Seifer SD, Finocchio L, Leslie J, O'Neil EH. Community health workers: Integral members of the health care work force. American Journal of Public Health. 1995;85:1055–1058. doi: 10.2105/ajph.85.8_pt_1.1055. [DOI] [PMC free article] [PubMed] [Google Scholar]


