Abstract
Summary
Data of 17 male patients with a final diagnosis of transient osteoporosis (TO) of the hip seen at the radiology department of a university hospital over a period of 7 years were retrospectively studied. Comparison of the proportion of doctors among TO cases with that among other hip joint pathologies revealed a significant difference.
Purpose
The objective of this study is to present clinical and radiological findings of hip TO and to assess the association of the condition with patients' occupation.
Materials and methods
Data of 17 male patients with a final diagnosis of transient osteoporosis of the hip seen at the radiology department of a university hospital over a period of 7 years were retrospectively studied.
Results
The diagnosis of transient hip osteoporosis was in accordance with the published literature for clinical, imaging findings, and laboratory results. Among the 17 cases of male transient hip osteoporosis, 65% were physicians and 12% were commercial pilots. Comparison of the proportion of doctors among TO cases with that among other hip joint pathologies revealed a significant difference. Abnormal low hormone levels of testosterone and 25-cholicalciferol (vitamin D) were detected in three and two patients, respectively.
Conclusion
The preponderance of physicians among patients with transient hip osteoporosis has not been previously reported. Etiological contribution of endocrine pathology and type of occupation to the causation of transient osteoporosis merits further research.
Keywords: Transient osteoporosis, Hip MRI, Occupation, Hormones
Introduction
Transient osteoporosis (TO) most commonly affects middle-aged men with a male to female ratio of 3:1 [1, 2] and is primarily characterized by bone marrow edema. The hallmark that separates transient osteoporosis from other conditions presenting with bone marrow edema pattern lies in the self-limited nature of TO and the regional osseous demineralization detected on plain radiographs. Magnetic resonance imaging (MRI) is used primarily for early diagnosis and for monitoring disease progression. Early differentiation from more aggressive conditions with long-term sequelae is essential to avoid unnecessary treatment [3].
TO has good prognosis with complete restoration of bone density. Recurrence is not usual but has been reported [4], and follow up of TO patients is recommended for 2 years [5]. Many authors believe that TO is an early reversible stage of osteonecrosis [6]; however, the etiology and pathophysiology remain unclear. Factors implicated to cause TO include genetic predisposition, Sudeck′s atrophy, obturator nerve compression, small vessel ischemia, bone medullary hypertension, fatty marrow conversion of proximal femoral metaphysis, and chemical or hormonal factors related to pregnancy [7, 8]. Further risk factors include steroid intake, alcoholism (more than 400 ml/week of ethanol), obesity, hemoglobinopathies, and pregnancy [9, 10]. Hypothyroidism may be implicated in the etiology of TO [4] as well as iatrogenic hyperthyroxinemia [11]. Minor trauma preceding hip pain which may have caused a period of transient ischemia could precipitate to TO [12].
We present here the clinical, radiological, and occupation background of males with TO. To our knowledge, this is the first report assessing the relationship between TO and occupation.
Materials and methods
During the 8-year period between March 2001 and December 2008, 17 male cases of unilateral TO were confirmed at the Radiology Department of Jordan University Hospital (a tertiary care center). The mean age of cases was 40 years (range 26–71 years). The left hip was involved in nine patients and the right hip in eight patients.
In addition to the routine hematological and biochemical laboratory investigations, basic hormonal workup had been performed on seven cases referred from the endocrine clinic.
All patients underwent MRI of the hip joints at time of presentation, with repeat of MRI in four cases that had recurrences. Standard T1-weighted axial and coronal images with and without intravenous gadolinium administration (Fig. 1a, b), T2 and T2-fat-suppressed weighted axial, and coronal and sagittal images were obtained (Fig. 2). Surface coil was used due to its high spatial resolution.
Fig. 1.
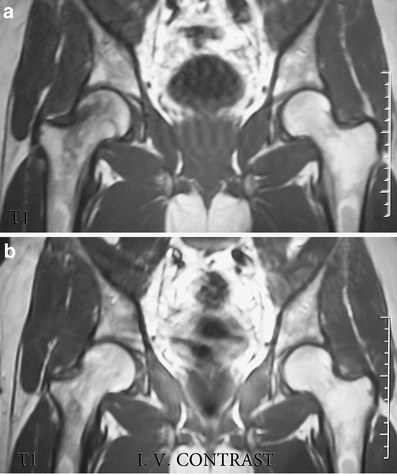
a, b Coronal MR images showing hypointense right femoral head and neck signal (a) which was normalized after intravenous gadolinium injection (b)
Fig. 2.

Coronal T2 Fat saturation MRI showing hyperintense right femoral head and neck with minimal joint effusion and subchondral area involvement
For all patients, plain radiography for the particular painful joint was taken within the first 2 weeks of the symptoms at presentation (zero time), 4, 8, and 12 weeks. Computed tomography scan with coronal reconstruction, bone scan, and bone mineral densitometry were done for few patients.
MRI images were reviewed by two experienced radiologists with consensus diagnosis. The results were classified as follows: (a) bone marrow edema extends to less than 50% of the femoral head; (b) edema extends to more than 50% of the femoral head; (c) edema extends to the femoral neck; and (d) edema extends to the intertrochanteric region.
The amount of joint effusion was measured on T2-fat-suppressed coronal images and graded as 0 (none), 1 (minimal), 2 (surround femoral neck), and 3 (distention of capsule) [13].
The diagnosis of TO was based on the previously published criteria [14–16]: hip pain without any apparent history of infection and trauma, plain radiographic demineralization of the femoral head and or neck, decreased signal intensity of bone marrow in the femur on T1-weighted images and increased on T2-weighted images, and spontaneous resolution of both symptoms and radiographic demineralization.
Details of occupational history of all cases was recorded at the time of presentation and compared to the occupational history of 14 patients with bone marrow edema (BME) and five patients with avascular necrosis of hip (AVN) seen during the same period of study. BME syndrome was diagnosed in patients in whom osteopenia was never demonstrated radiographically [17]
Statistical analysis was done using Stata 9.2 for the Pearson chi-square test.
Results
The main clinical features of patients were acute progressive disabling hip pain that was also experienced at rest and nocturnally, limping antalgic gait, functional disability involving the affected extremity, and dull ache in the inguinal area, buttocks, or anterior aspect of the thigh. None of the patients reported antecedent trauma.
On examination, the hip region was slightly tender and the range of motion showed some reduction of abduction, flexion, and internal rotation. Occasionally, quadriceps muscle atrophy was noted.
Table 1 reports the occupation of all patients and their MRI hip findings. Among the 17 male patients, 10 were physicians, one was a dentist, and two were pilots. Among the group of 14 patients with BME, there were three physicians including a general surgeon (40 years), cardiologist (55 years), and an emergency resident (30 years). A 45-year-old internist was among the five patients with AVN of the hip. The proportion of doctors among patients with TO was significantly higher than the proportion of doctors among the combined cases of BME and AVN of the hip (p = 0.008).
Table 1.
Type of occupation and MRI hip findings among 17 male patients with TO
| Patient no. | Age | Occupation | Joint | Bone marrow Oedema/ | Subchondral Bone | Joint effusion | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| A | B | C | D | Spared | Involved | 0 | 1 | 2 | 3 | ||||
| 1 | 32 | Medicine resident | Rt hip | × | Yes | × | |||||||
| 2 | 50 | Commercial pilot | Lt hip | × | Yes | × | |||||||
| 3 | 52 | Commercial pilot | Rt hip | × | Yes | × | |||||||
| 4 | 40 | Farmer | Rt hip | × | Yes | × | |||||||
| 5 | 45 | Bank teller | Rt hip | × | Yes | × | |||||||
| 6 | 26 | Dentist | Lt hip | × | Yes | × | |||||||
| 7 | 38 | Gastroenterologist | Lt hip | × | Yes | × | |||||||
| 8 | 71 | Retired teacher | Rt hip | × | Yes | × | |||||||
| 9 | 50 | General practitioner | Lt hip | × | × | ||||||||
| 10 | 35 | Gastroenterologist | Rt hip | × | Yes | × | |||||||
| 11 | 55 | Anesthesiologist | Rt hip | × | Yes | × | |||||||
| 12 | Oncologist | Lt hip | × | Yes | × | ||||||||
| 13 | 47 | Internist | Lt hip | × | Yes | × | |||||||
| 14 | 48 | Driver | Lt hip | × | Yes | × | |||||||
| 15 | 44 | Maxillofacial surgeon | Rt hip | × | Yes | × | |||||||
| 16 | 47 | Radiologist | Lt hip | × | × | ||||||||
| 17 | 50 | Hepatobiliary surgeon | Lt hip | × | Yes | × | |||||||
All patients had normal plain radiographs at presentation and consistent osteopenia on follow-up at 4, 8, and 12 weeks except patient number 6 who had normal X-ray at fourth week but developed osteopenia on follow-up at eighth and 12th week.
Bone marrow edema of stage D was the most commonly encountered stage followed by stages C then B. Only one patient, patient number 6, had stage A bone marrow edema. The subchondral bone was involved in the majority of patients, but none had subchondral fracture. Joint effusion in moderate amounts was noted in all patients. The time taken for complete resolution of the MRI changes averaged 7.5 months (range 4–11).
Recurrence in the same joint within 1 year of the initial attack was proved by typical MRI findings in four patients (nos. 2, 3, 10, 12) in the same joint.
Hormonal tests were done for seven patients and are summarized in Table 2. The low total testosterone (TT) levels together with normal leutinizing hormone (LH) and follicular stimulating hormone(FSH) levels suggesting the diagnosis of secondary hypogonadotrophic hypogonadism was seen in patients 1, 7, and 15. Patients 1 and 10 showed low 25-cholicalciferol levels.
Table 2.
Hormonal profile of seven male patients with TO
| Patient no. | Prolactin | Vit D | TT | LH | FSH | PTH | TSH | T3 | T4 |
|---|---|---|---|---|---|---|---|---|---|
| >13 mg/l | 47–144 nm/l | 2–10 ng/l | 2–15 IU/L | 2–12 IU/L | 13–54 pg/L | 0.4–5.5 ml IU/ml | 3.3–8.2 pmol/L | 9.4–25 pmol/L | |
| 1 | 8.9 | 24 | 1.18 | 2.15 | 2.16 | 39.7 | 0.92 | 3.9 | 10.2 |
| 7 | 7.9 | 122.1 | 1.17 | 7.1 | 3.9 | 39.6 | 1.77 | 3.9 | 11.8 |
| 9 | 7.2 | 129.1 | 5.1 | 5.3 | 6.2 | 26.5 | 0.37 | 6.8 | 14.2 |
| 10 | 13 | 16 | 4 | 4.8 | 5.7 | 52.1 | 1.96 | 5.2 | 13.8 |
| 15 | 4.8 | 103.5 | 0.75 | 4.8 | 6.4 | 29.3 | 1.89 | 7.6 | 16.7 |
| 16 | 3.9 | 87.3 | 4.6 | 2.1 | 2.5 | 38.9 | 1.63 | 8.1 | 24.2 |
| 17 | 3.8 | 93.7 | 6.7 | 2.3 | 2.5 | 47.4 | 2.1 | 4.1 | 12.5 |
Discussion
TO is an increasingly recognized cause of acute spontaneous unilateral hip pain that resolves spontaneously over a few months. Our patients with the final diagnosis of TO of the hip had clinical, physical, and imaging findings concordant with those published in the literature, where clinical symptoms had been present for an average of 4 months before the diagnosis was made [18], and the time taken for complete resolution of the MRI changes averaged 7.5 months [4].
Reports correlating the duration of symptoms with the presence of subchondral fracture and the extent of bone marrow edema gave conflicting results [19–21]. Our experience indicated that the patients' compliance to rest and avoidance of known risk factors during all phases of TO was the crucial factor in reducing the duration of symptoms with early complete recovery and better prognosis.
There are reports for recurrence of TO whether in the same or other joints [4]. In this study, recurrence was seen in four patients and could be attributed to continuous alcohol intake (patient no. 2), persistence of long-haul flights (patient no. 3), and noncompliance to protected weight bearing and immobilization (patient no. 10). All recurrences were in the same affected joint as encountered in other studies [1].
Medical literature review did not show any studies relating the occurrence of TO with the patients′ occupation. In this study, 11 of the 17 male patients were doctors, and two were commercial pilots. Medical doctors were of different specialties, but they all reported long periods of standing during their work. It could be argued that this preponderance of physicians is related to the fact that doctor patients seek medical advice quicker and so are investigated more rapidly than other patients. We, thus, endeavored to compare the ratios of doctor patients among the cases of TO with those among cases of BME and AVN of the hip diagnosed in the same department and during the same period of study. The comparison showed a statistically significant preponderance of doctors among the TO cases than among patients of both BME and AVN of the hip taken collectively.
Two of the cases were commercial pilots. It could be postulated that possible risk factors for TO include the long immobilization in long-haul flights, cosmic rays exposure [22], and variable different atmospheric pressure gradients which may result in barotraumas.
Hormonal factors have been implicated as possible causes for TO in females [7, 8] but have never been implicated in male patients, although hypogonadism is a recognized cause for generalized osteoporosis [23]. We noticed that some of our patients, particularly those who were referred from the endocrine clinic, had low testosterone and low vitamin D levels, a finding that encourages future research on the correlation of hormonal abnormalities with TO in males.
The limitations of this study include its retrospective nature that did not allow complete assessment of the hormonal profile for all patients and of performing repeat MRI for all cases. Moreover, the number of cases is small. The strength of the study comes from the fact that to our knowledge, occupation has not been previously investigated as a risk factor for TO.
Conclusion
Our patients exhibited the typical findings of TO regarding the clinical presentation, physical examination, and radiological findings particularly plain radiography and MRI features. The two interesting findings in this study include the presence of low TT levels during the acute presentation in two cases and the overwhelming high proportion of medical doctors among the patients. Further research is recommended to answer the question of whether occupation—physicians in particular—is a risk factor for developing TO of the hip.
Acknowledgments
Conflicts of interest
None.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- 1.Lakhanpal S, Ginsburg W, Luthra S, Hunder G. Transient regional osteoporosis: a study of 56 cases and review of the literature. Ann Intern Med. 1987;106:444–450. doi: 10.7326/0003-4819-106-3-444. [DOI] [PubMed] [Google Scholar]
- 2.Schapira D. Transient osteoporosis of the hip. Semin Arthritis Rheum. 1992;2:98–105. doi: 10.1016/0049-0172(92)90003-V. [DOI] [PubMed] [Google Scholar]
- 3.Korompilias AV, Karantanas AH, Lykissas MG, Beris AE. Transient osteoporosis. J Am Acad Orthop Surg. 2008;16(8):480–489. doi: 10.5435/00124635-200808000-00007. [DOI] [PubMed] [Google Scholar]
- 4.Balakrishnan A, Schemitsch E, Pearce D, Mckee M. Distinguishing transient osteoporosis of the hip from avascular necrosis. Can J Surg. 2003;46:187–192. [PMC free article] [PubMed] [Google Scholar]
- 5.Wilson AJ, Murphy WA, Hardy DC, Totty WG. Transient osteoporosis: transient bone marrow edema? Radiology. 1988;167:757–760. doi: 10.1148/radiology.167.3.3363136. [DOI] [PubMed] [Google Scholar]
- 6.Solomon L. Bone-marrow edema syndrome. J Bone and Joint Surg. 1993;75-B(2):175–176. doi: 10.1302/0301-620X.75B2.8444931. [DOI] [PubMed] [Google Scholar]
- 7.Kim SY, Koo KH, Suh KT, Kim YS, Cho YJ, Min BW, Ha YC, Choi JA. Fatty marrow conversion of the proximal femoral metaphysis in transient bone marrow edema syndrome. Arch Orthop Trauma Surg. 2005;125:390–395. doi: 10.1007/s00402-005-0824-4. [DOI] [PubMed] [Google Scholar]
- 8.Koo KH, Ahn IO, Song HR, Kim SY, Jones JP., Jr Increased perfusion of the femoral head in transient bone marrow edema syndrome. Clin Orthop Relat Res. 2002;402:171–175. doi: 10.1097/00003086-200209000-00015. [DOI] [PubMed] [Google Scholar]
- 9.Diwanji SR, Cho YJ, Xin ZF, Yoon TR. Conservative treatment for transient osteoporosis of the hip in middle-aged women. Singapore Med J. 2008;49(1):17–21. [PubMed] [Google Scholar]
- 10.Daniel RS, Farrar EK, Norton HR, Nussbaum AI (2009) Bilateral transient osteoporosis of the talus in pregnancy. Osteoporos Int, in press [DOI] [PubMed]
- 11.Jennings PE, Malley BP O, Griffin KE, Northover B, Rosenthal FD. Relevance of increased serum thyroxine concentrations associated with normal serum triiodothyronine values in hypothyroid patients receiving thyroxine: a case for “tissue thyrotoxicosis”. BMJ. 1984;289:1645–1647. doi: 10.1136/bmj.289.6459.1645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Duncan CR, Evans RA, Somers NM. Bone death in transient regional osteoporosis. Bone. 1992;13:161–165. doi: 10.1016/8756-3282(92)90006-I. [DOI] [PubMed] [Google Scholar]
- 13.Mitchell DG, Rao V, Dalinka M, Spritzer CE, Gefter WB, Axel L, Steinberg M, Kressel HY. MRI of joint fluid in the normal and ischemic hip. AJR Am J Roentgenol. 1986;146:1215–1218. doi: 10.2214/ajr.146.6.1215. [DOI] [PubMed] [Google Scholar]
- 14.Shifrin LZ, Reis ND, Zinman H, Besser MI. Idiopathic transient osteoporosis of the hip. J Bone Joint Surg Br. 1987;69:769–773. doi: 10.1302/0301-620X.69B5.3680339. [DOI] [PubMed] [Google Scholar]
- 15.Pantazopoulous T, Exarchou E, Hartofilakidis-Garofalidis G. Idiopathic transient osteoporosis of the hip. J Bone Joint Surg Am. 1973;55:315–321. [PubMed] [Google Scholar]
- 16.Guerra JJ, Alabama B, Steinberg ME, Current concepts review Distinguishing transient osteoporosis from avascular necrosis of the hip. J Bone Joint Surg Am. 1995;77:616–624. doi: 10.2106/00004623-199504000-00017. [DOI] [PubMed] [Google Scholar]
- 17.Hays C, Conway W, Daniel W. MR imaging of bone marrow edema pattern: transient osteoporosis, transient bone marrow edema syndrome or osteonecrosis. Radiographics. 1993;13:1001–1011. doi: 10.1148/radiographics.13.5.8210586. [DOI] [PubMed] [Google Scholar]
- 18.Hofmann S, Engel A, Neuhold A, Leder K, Kramer J, Plenk H. Bone marrow edema syndrome and transient osteoporosis of the hip: an MRI-controlled study of treatment by core decompression. J Bone Joint Surg Br. 1993;75-B:210–216. doi: 10.1302/0301-620X.75B2.8444939. [DOI] [PubMed] [Google Scholar]
- 19.Ergun T, Lakadamyali H. The relation between MRI findings and duration of symptoms in transient osteoporosis of the hip. Acta Orthop Traumatol Turc. 2008;42(1):10–15. doi: 10.3944/AOTT.2008.010. [DOI] [PubMed] [Google Scholar]
- 20.Malizos KN, Zibis AH, Dailiana Z, Hantes M, Karachalios T, Karantanas AH. MR imaging findings in transient osteoporosis of the hip. Eur J Radiol. 2004;50:238–244. doi: 10.1016/j.ejrad.2004.01.020. [DOI] [PubMed] [Google Scholar]
- 21.Miyanishi K, Kaminomachi S, Hara T, Maeda H, Watanabe H, Shimizu A, Torisu T. A subchondral fracture in transient osteoporosis of the hip. Skeletal Radiol. 2007;36:677–680. doi: 10.1007/s00256-006-0248-4. [DOI] [PubMed] [Google Scholar]
- 22.Lim MK. Cosmic rays: are air crew at risk? Occup Environ Med. 2002;59:428–432. doi: 10.1136/oem.59.7.428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kronengerg H, Melmed S, Polonsky K, Larsen P. Williams textbook of endocrinology. Amsterdam: Elsevier; 2008. pp. 1036–1046. [Google Scholar]


