Abstract
Changes in health, functional abilities, and behavior problems among 150 adults with Down syndrome and 240 adults with mental retardation due to other causes were examined with seven assessments over a 9-year period. Adults were primarily younger than 40, the age at which declines begin to be evident in individuals with Down syndrome. Adults with Down syndrome were advantaged in their functional abilities and lack of behavior problems, comparable in health, and exhibited comparable rates of change on these measures as adults with mental retardation due to other causes. Placement out of the parental home and parental death were predictors of change in health, functional abilities, and behavior problems.
The past 50 years have been a time of remarkable change for individuals with Down syndrome, as medical breakthroughs and improvements in services have extended their life expectancy dramatically (Bittles & Glasson, 2004; Eyman & Borthwick-Duffy, 1994; Glasson et al., 2002). Significant research attention has been focused on the health and longevity of adults with Down syndrome in the modern era of antibiotics, easier access to health care and life-saving surgeries, and community rather than institutional residence (Bittles & Glasson, 2004; Day, Strauss, Shavelle, & Reynolds, 2005; Eyman, Call, & White, 1991; Glasson et al., 2002; Yang, Rasmussen, & Friedman, 2002; Zigman, Jenkins, Tycko, Schupf, & Silverman, 2005). There has been a particularly intense level of interest among the research community, families, and service providers in the age-related decline in adaptive behavior and cognitive abilities among older adults with Down syndrome. Such a decline is believed to be associated variously with dementia of the Alzheimer’s type, normal aging, and the underlying severity of mental retardation (Devenny, Hill, Patxot, Silverman, & Wisniewski, 1992; Devenny et al., 1996; Silverman, Zigman, Kim, Krinsky-McHale, & Wisniewski, 1998; Zigman, Schupf, Haveman, & Silverman, 1997).
Early researchers sounded the alarm regarding the risk of individuals with Down syndrome developing the behavioral or functional symptoms of Alzheimer’s disease Lott, 1982. However, recent investigators have concluded that the risk is considerably smaller than initially believed and not elevated until age 40 or 50. The prevalence of dementia among adults with Down syndrome has been estimated to be approximately 20% after age 40 (Janicki & Dalton, 2000) and 45% after age 55 (Silverman et al., 1998). However, even after age 60, only just over half of individuals with Down syndrome (56%) have a diagnosis of dementia (Janicki & Dalton, 2000).
The lower risk of dementia prior to age 40 is reinforced by most studies of the cognitive and functional abilities of adults with Down syndrome reporting either stability throughout adulthood or stability until around age 40 and declines thereafter, as described below. There is an emerging consensus that adults with Down syndrome younger than age 40 are not at risk of functional decline even though they may manifest the neuropathology of Alzheimer’s disease (Friedman & Brown, 2001). This conclusion is further reinforced by the work of Zigman, Silverman, Devenny, and their colleagues, who have reported both cross-sectional and longitudinal analyses of the risk of functional and cognitive decline in individuals with Down syndrome. Several cross-sectional studies reported that prior to age 50, adults with Down syndrome have significantly better skills than do their counterparts with mental retardation due to other causes, but after age 50 they lose their comparative advantage both functionally and cognitively (Zigman, Schupf, Lubin, & Silverman, 1987), experience functional declines at an earlier age (Zigman, Schupf, Urv, Zigman, & Silverman, 2002) and have a higher risk of Alzheimer’s disease (Zigman, Schupf, Sersen, & Silverman, 1995). In longitudinal studies, these researchers have reported that cognitive ability generally remains stable over 6 years. However, where declines are evident, the declines are more pronounced among older adults over age 50 and among adults with Down syndrome as compared to their counterparts with mental retardation due to other causes (Devenny et al., 1992; Devenny et al., 1996).
In other longitudinal studies, researchers reported similar patterns. In a study of 83 adults with Down syndrome, Collacott and Cooper (1997) found a pattern of stability of functional skills before age 40 and significant decline there-after. Carr (2000, 2003) has also found a pattern of stability of functional skills among adults with Down syndrome who were studied longitudinally at ages 21, 30, and 35. Rasmussen and Sobsey (1994) reported a significant decline in self-help skills and communication among institutionalized adults with Down syndrome over the age of 40. In contrast, Burt and colleagues (Burt et al., 1995) found no age-related decline on neuropsychological measures in a sample of 34 community-dwelling adults with Down syndrome aged 22 to 56 over a 3-year period. Further, Burt and colleagues found no longitudinal evidence for precocious aging in adaptive skills of adults with Down syndrome when comparing them with adults who had mental retardation due to other causes (Burt et al., 2005).
In another line of research, Prasher and colleagues (Prasher, Chung, & Haque, 1998) differentiated the trajectories of individuals with Down syndrome who are healthy and those who have health difficulties. In a 3-year longitudinal study of 128 adults with Down syndrome, they found that those who did not have dementia nor potentially confounding medical problems at the outset showed a pattern of stability over the study period. However, when the total group was analyzed together (including those who were healthy, those with medical problems, and those with dementia), there was a pattern of decline in functional abilities. This study clarifies that there are multiple trajectories that characterize individuals with Down syndrome in adulthood and suggests the need for more finely differentiated analyses during the later years of the life course. In an earlier cross-sectional study, Prasher and Chung (1996) reported a pattern of age-related differences in adaptive functioning, with higher scores in cohorts age 40 or younger than in cohorts age 50 or older.
Thus, although there is agreement that adults with Down syndrome are at increased risk of dementia as compared with both the general population and adults with mental retardation due to other causes, the risk does not manifest until after age 40 or 50. Indeed, on an absolute level, adults with Down syndrome appear to function better than their counterparts with mental retardation due to other causes until they reach the age of increased risk. Taken as a whole, this body of literature has made important contributions to understanding the life course trajectory of adults with Down syndrome, most of whom did not live to midlife in prior decades. The age of 40 appears to be a turning point for these individuals, with an elevated risk of health, functional, and cognitive problems thereafter.
The literature, however, suffers from several methodological limitations. In many longitudinal studies, functional and cognitive changes are the focus, to the exclusion of examination of changes in health and maladaptive behaviors, both of which are critical to quality of life in midlife. Additionally, the source of data regarding stability and change is often not constant across the points of data collection. A high level of residential relocation and staff turnover in residential facilities leads to change in respondent that could introduce problems with accuracy and reliability. It is, therefore, not evident whether and how measurement error contributes to or obscures the patterns reported in the literature. The duration of most longitudinal studies tends to be relatively short, with few points of measurement. Most longitudinal studies have just two points of data collection or span less than 5 years, possibly underestimating slowly developing trends. Finally, some studies have been limited by small samples, unrepresentative (institutionalized) samples, or lack of control groups, making interpretation of findings difficult.
The present analysis is unique because we focused on a large sample of adults with Down syndrome, all of whom lived in the parental home when the study began in 1988. The mother remained the primary respondent throughout the study period. The sample also included a large sample of adults with mental retardation due to other causes, facilitating comparisons in trajectories of change and stability. The study design involved eight assessments of each individual over a 12-year period, with each point of data collection scheduled 18 months after the previous one.
An additional feature of the present study is that our aim was to describe the health, functional abilities, and behavior problems of individuals with Down syndrome in the early and middle years of adulthood. As noted above, much more attention has been focused in past research on the period of life after age 40, when the risk of functional decline, health changes, and dementia threatens the well-being of individuals with Down syndrome. Comparatively less is known about patterns of change (including the possibility of gains) manifested by adults with Down syndrome during the long stretch of adulthood prior to age 40. Our goal in the present analysis was to examine changes in the health, functional abilities, and behavior problems of individuals with Down syndrome prior to the risk period of decline, in order to describe the normative patterns of adult development in this population. In the present analysis, 84% of the adults with Down syndrome were younger than 40 years of age, with a mean age of 32 at the start of the study period.
For this analysis, we addressed three research questions: First, would adults with Down syndrome differ from adults with mental retardation due to other causes with respect to initial levels of health, functional abilities, and behavior problems? We hypothesized that adults with Down syndrome would exhibit better functional abilities and fewer behavior problems. Although individuals with Down syndrome have increased rates of specific medical conditions (Roizen, 1996), we have no directional hypothesis regarding their overall health.
Second, do adults with Down syndrome differ from adults with mental retardation due to other causes with respect to their pattern of change or stability over time? We hypothesized that during this young adult and midlife age range, those with Down syndrome would show comparable patterns of change in health, functional abilities, and behavior problems as compared with their counterparts with mental retardation due to other causes.
Third, would absolute level and change in health, functional abilities, and behavior problems be predicted by other characteristics of the individual (including age, gender, level of mental retardation, and residential status) and of the family (including family relations and the occurrence of parental death). We hypothesized that risk factors for declines in health and functional abilities as well as worsening of behavior problems would include older age, more severe mental retardation, poorer family relations, and parental death. We included gender as a control variable. We had no directional hypothesis of the impact of residential placement on health, functional abilities, and behavior problems. Evidence has been reported indicating that changes in these variables lead to residential placement (Essex, Seltzer, & Krauss, 1997), and there is also evidence supporting the inverse relationship (i.e., that placement leads to changes in health, functional abilities, and behavior problems) (Borthwick-Duffy, Eyman, & White, 1987).
Methods
Sample
The analyses reported here are based on data from a longitudinal study of 461 adults with mental retardation and their aging parents (Krauss & Seltzer, 1999; Seltzer & Krauss, 1994). About half of the families lived in Massachusetts and the other half, in Wisconsin. Families were recruited if they met two criteria when the study began: the mother was between 55 and 85 years of age and the son or daughter lived at home with her. All families volunteered to participate.
The current analyses included data from seven of the eight waves of data collection, beginning at the second wave in the larger study spanning a 9-year period. We started at Time 2 because the measure of behavior problems was not administered at Time 1. Furthermore, the sample for the present analysis was restricted to adults who were co-residing with their mother at the second wave of data collection. For the purpose of this analysis, we considered the second wave of data collection in the larger study as the “initial” analytic time point. These decisions limited the sample to 390 adults with mental retardation. Of the 71 sample members not included in the current analysis, 40 mothers did not participate in the second wave but later continued with the study, 7 mothers dropped out of the study at the second wave and never re-joined, 18 adults were placed outside of the family home between the first and second waves, and 6 adults were deceased prior to the second wave of data collection.
The primary comparison in this analysis was between the adults with Down syndrome (n = 150) and the adults with mental retardation due to other causes (n = 240). The two groups were similar in level of mental retardation and likelihood of residential placement by the end of the study, but differed in gender, age distribution, and likelihood of experiencing parental death during the study (see Table 1). Regarding level of mental retardation, approximately three quarters of both groups had mild or moderate mental retardation. For placement status, approximately one third of both groups moved away from the parental home during the study period, whereas two thirds remained at home throughout the seven waves of data collection. A higher proportion of the adults with Down syndrome were male compared with the adults with mental retardation due to other causes (62.0% vs. 49.6%, respectively), χ2 (1, N = 390) = 5.74, p < .05, and were more likely to have parents who died during the course of the study (30.0% vs. 20.8%, respectively), χ2 (1, N = 390) = 4.21, p < .05. During the study period, 48 mothers and 54 fathers died; 6 adults experienced the death of both parents. The adults with Down syndrome were significantly younger than their counterparts (32.1 years vs. 36.1 years of age at initial time point, respectively), t(385) = 5.25, p < .001. Adults with Down syndrome ranged in age from 17 to 57 years (M = 32.11, SD = 7.25); and those with mental retardation due to other causes, from 19 to 68 years (M = 36.13, SD = 7.38). Although 84% of the adults with Down syndrome were below the age of 40 at the initial time point, this was true of only 68% of the adults with mental retardation due to other causes. Only 8 individuals were 50 years of age or older at the initial time point, one of whom had Down syndrome. Adults with Down syndrome were also more likely to have families with better family relations as measured by the Family Relations Index (Moos & Moos, 1986), as described below, t(388) = −3.10, p < .01, than were their counterparts.
Table 1.
Demographic Characteristics (in %) of the Sample (N = 390)
| Characteristic | DSa (n = 150) |
MRb
due to other causes (n = 240) |
|---|---|---|
| Level of MR | ||
| Mild/moderate | 75.3 | 75.8 |
| Severe/profound | 24.7 | 24.2 |
| Residential status | ||
| Placed during study period |
34.0 | 32.9 |
| Co-residing throughout study period |
66.0 | 67.1 |
| Gender | ||
| Female | 38.0 | 50.4 |
| Male | 62.0 | 49.6 |
| Parental death during study | ||
| Yes | 30.0 | 20.8 |
| No | 70.0 | 79.2 |
Down syndrome.
Mental retardation.
Data Collection
Mothers of individuals with mental retardation participated in in-person interviews at each point of data collection and completed self-administered questionnaires. As noted earlier, about one third of the adults moved to residential placements during the study. For all measures except one, mothers remained the primary respondent throughout the study, even after placement. The mother was able to remain a trusted source of data about her adult child even after placement because of the high level of contact between virtually all mothers in our study and their adult child who lived away from home (Seltzer, Krauss, Hong, & Orsmond, 2001). We found that during a 3-year period following placement, mothers had contact an average of several times a week with their son or daughter, either in person or by telephone. Mothers also had weekly contact with a service provider connected with the son or daughter’s new residence. Thus, they had access to current information about their son or daughter, even though they no longer shared a residence. The one exception was the measure of functional skills, including housework, personal care, meal-related activities, and mobility. For this measure, data were obtained from residential program care-providers.
In addition, in cases when the mother died, another family member (10 fathers, 34 siblings, and 1 other relative) or guardian (3 nonrelatives) became the new primary respondent.
Measures
The dependent variables for the present analysis were measures of the health, functional abilities, and behavior problems of the individual with mental retardation. All measures were included in the self-administered questionnaires completed by the mother. The independent variables include five demographic characteristics (whether or not the individual had Down syndrome, age, gender, level of mental retardation, and residential status) and two family characteristics (a measure of family relations and the occurrence of parental death).
Health was measured using a maternal rating of the current health status of her son or daughter (1 = poor, 2 = fair, 3 = good, 4 = excellent). Global ratings of health have been found to be accurate measures of health status (Idler & Benyamini, 1997). Our measure of functional abilities was a 30-item scale measuring functional skills in the areas of housework, personal care, meal-related activities, and mobility. This scale was based on a revised version of the Barthel Index (Mahoney & Barthel, 1965), which is used to measure personal and instrumental activities of daily living appropriate for aging individuals with mental retardation (Seltzer, Ivry, & Litchfield, 1987). Each item was rated on a 4-point scale of independence (1 = cannot perform the task at all, 2 = could do but doesn’t, 3 = can perform the task with help, 4 = performs the task independently) and averaged for each of the subscales. Internal consistency coefficients of the subscales at the initial time point were .76 for housekeeping, .94 for personal care, .84 for meal-related activities, and .83 for mobility. As noted earlier, the mother was the respondent for these items during the time when the son or daughter was living at home; thereafter, the careprovider was the respondent. Concurrent validity of maternal ratings with paternal ratings, r = .91, and caregiver ratings, r = .94, is excellent (Essex, 1998). However, because of this change in respondent, we included residential status as a time-varying covariate in all analyses.
The measure of behavior problems was the Inventory for Client and Agency Planning—ICAP (Bruininks, Hill, Weatherman, & Woodcock, 1986), later known as the Scales of Independent Behavior–Revised—SIB-R (Bruininks, Woodcock, Weatherman, & Hill, 1996). This measure assesses the frequency and severity of eight types of behavior problems, thereby providing an overall measure of generalized behavior problems. There are three subscales: internalized maladaptive behavior (hurtful to self, unusual or repetitive habits, and withdrawn or inattentive behavior), asocial maladaptive behavior (socially offensive behavior and uncooperative behavior), and externalized maladaptive behavior (hurtful to others, destructive to property, and disruptive behavior). Individual problem behaviors are scored as present or absent. Index scores for the four subscales provide ratings of the seriousness of the problem behavior as normal (90 to 110), marginally serious (111 to 120), moderately serious (121 to 130), serious (131 to 140), or very serious (141 or above). Reliability and validity are excellent for the maladaptive behavior subscales (Bruininks et al., 1986). Mothers provided these data throughout the study period.
The demographic variables were age at the initial time point (measured in years), gender (0 = male, 1 = female), level of mental retardation (0 = severe or profound, 1 = mild or moderate), and place of residence (time-varying covariate: 0 = home, 1 = placed at each point of data collection). Level of mental retardation was based on maternal report and confirmed by agency records. All cases were classified as either having Down syndrome (1) or not (0), based on maternal report.
Family characteristics were family relations, as measured by the Family Relations Index of the Family Environment Scale (Moos & Moos, 1986), and death of a parent during the study (time-varying covariate: 0 = no death, 1 = one parent deceased, 2 = two parents deceased at each point of data collection). The Family Relations Index reflects maternal ratings of family cohesion, expressiveness, and conflict. Items measuring conflict were subtracted from items measuring cohesion and expressiveness. Higher scores reflect better family relations. The mean Family Relations Index score for the adults with mental retardation was 12.53 (SD = 2.96) and for those with mental retardation due to other causes, the mean was 11.40 (SD = 3.85).
Method of Data Analysis
The primary method of data analysis was hierarchical linear modeling–HLM (Bryk & Rau-denbush, 1987; Raudenbush & Bryk, 2001). This analysis makes it possible to use characteristics of the individual and family to predict change in individual characteristics over the study period. Two parameters are important in HLM: an intercept that describes the status of the sample members at the initial time point and a slope that describes their change (in health, functional abilities, and behavior problems) over time. Individual intercepts and slopes are outcome variables that are potentially explained by the characteristics of the individual and their family (Down syndrome, age, level of mental retardation, gender, and family relations). In addition, two characteristics of the individual and their family were time-varying covariates: residential placement during the study and death of a parent during the study. These covariates, which were allowed to differ across the seven time points, were used to predict the level of the outcome variable at the exact time that each estimate was made (e.g., the time of transition [residential placement, parental death] rather than at the initial estimate). Time-varying covariates provide three advantages: (a) prediction from each assessment point rather than assuming that prediction from the initial time point is sufficient; (b) allow growth trajectories to be estimated more reliably as they explain departures from linear growth trajectories; and (c) increase power with the consideration of more data points. Predictors of the intercept are called Level 1 predictors, and predictors of the slope are called Level 2 predictors. The model predicted random intercepts and random slopes, with the Levels 1 and 2 predictors all being centered on their grand mean. As developmental changes in health, functional abilities, and behavior problems are gradual and slow to emerge, both significant, p < .05, and trend, p < .10, findings are reported.
One advantage of HLM is that individual differences in trajectories of change can be modeled. A second advantage is that HLM does not require all individuals to have the same number of data points, as is the case in repeated measures ANOVA. Rather, individuals who have fewer data points due to dropping out (n = 40) or even the death of the person with mental retardation (n = 25) can be retained in the analysis up until the point when the data are no longer available, a particular advantage in this aging sample.
If the time-varying covariates of residential placement or parental death were significant predictors of differences in health, functional abilities, or behavior problems, we explored the direction of the effects. We described and graphed the pattern of change from the two time points before and the two time points after the occurrence of the transition for the subgroup of individuals affected.
Results
Initial Differences Between Adults With Down Syndrome and Adults With Mental Retardation Due to Other Causes
For our first research question, we asked, do adults with Down syndrome differ from adults with mental retardation due to other causes at the initial point of this analysis with respect to health, functional abilities, and behavior problems (see model for initial status section of Table 2,Table 3, and Table 4, respectively)? As shown in Table 2, having a diagnosis of Down syndrome was not a significant Level 1 predictor of initial status in health, t(371) = 0.65, p = .57. As shown in Table 3, consistent with our hypothesis, having a diagnosis of Down syndrome was a significant Level 1 predictor of better functional abilities on all measures, including housekeeping skills, t(371) = 2.37, p < .05, personal care, t(371) = 4.27, p < .001, meal-related activities, t(371) = 2.87, p < .01, and mobility, t(371) = 3.10, p < .01. Having a diagnosis of Down syndrome was also a significant Level 1 predictor of fewer behavior problems (see Table 4) as measured by the generalized maladaptive index, t(371) = −2.33, p < .05, and the asocial maladaptive index, t(371) = −2.50, p < .05. A trend was found for a diagnosis of Down syndrome to be predictive of fewer externalized maladaptive behaviors, t(371) = −1.86, p < .06. A diagnosis of Down syndrome was not significantly predictive of internalized maladaptive behaviors.
Table 2.
Hierarchical Linear Model Estimates for Health of Adults With Mental Retardation (MR)
| Model | Coefficient | Standard Error |
|---|---|---|
| Model for initial status | ||
| Intercept | 3.242** | .034 |
| Gender | 0.025 | .067 |
| Age | −0.013** | .005 |
| Level of MR | 0.153+ | .080 |
| DSa | 0.046 | .071 |
| Family relations | 0.033** | .009 |
| Model for change | ||
| Slope | −0.014* | .006 |
| Gender | −0.002 | .010 |
| Age | −0.001 | .001 |
| Level of MR | −0.016 | .012 |
| DS | −0.020+ | .011 |
| Family relations | −0.001 | .001 |
| Time varying covariates | ||
| Placement | −0.223** | .042 |
| Parental death | 0.099* | .044 |
Down syndrome.
p < .05.
p < .01.
p < .10.
Table 3.
Hierarchical Linear Model Estimates for Functional Abilities of Adults With Mental Retardation (MR)
| Housekeeping | Personal care | Meal-related activities |
Mobility | |||||
|---|---|---|---|---|---|---|---|---|
| Model | Coefficient | SEa | Coefficient | SE | Coefficient | SE | Coefficient | SE |
| Model for initial status | ||||||||
| Intercept | 2.547** | .036 | 3.612** | .030 | 3.046** | .031 | 3.401** | .032 |
| Gender | −0.007 | .073 | −0.105+ | .060 | 0.080 | .059 | −0.053 | .065 |
| Age | 0.003 | .005 | 0.004 | .004 | −0.001 | .004 | −0.003 | .004 |
| Level of MR | 0.772** | .087 | 0.717** | .071 | 0.683** | .071 | 0.316** | .077 |
| DSb | 0.183* | .077 | 0.271** | .063 | 0.181** | .063 | 0.212** | .069 |
| Family relations | 0.011 | .010 | 0.015+ | .008 | 0.012 | .008 | 0.013 | .009 |
| Model for change | ||||||||
| Slope | 0.024** | .005 | −0.007** | .003 | −0.000 | .004 | −0.022** | .004 |
| Gender | −0.009 | .009 | 0.007 | .005 | 0.008 | .007 | ||
| Age | −0.002** | .001 | −0.001** | .000 | −0.001 | .000 | ||
| Level of MR | −0.013 | .010 | −0.011+ | .006 | 0.006 | .008 | ||
| DS | −0.003 | .009 | −0.003 | .005 | −0.005 | .008 | ||
| Family relations | −0.000 | .001 | 0.001 | .001 | 0.002+ | .001 | ||
| Time varying covariates | ||||||||
| Placement | 0.264** | .037 | −0.042* | .021 | 0.177** | .030 | 0.014 | .030 |
| Parental death | 0.019 | .037 | 0.004 | .021 | −0.011 | .030 | 0.032 | .031 |
Standard error.
Down syndrome.
p < .05.
p < .01.
p < .10.
Table 4.
Hierarchical Linear Model Estimates of Behavior Problems Exhibited by Adults With Mental Retardation (MR)
| Generalized | Internalized | Asocial | Externalized | |||||
|---|---|---|---|---|---|---|---|---|
| Model | Coefficient | SEa | Coefficient | SE | Coefficient | SE | Coefficient | SE |
| Model for initial status |
||||||||
| Intercept | 105.397** | .290 | 104.991** | .369 | 103.373** | .367 | 100.557** | .258 |
| Gender | 1.396* | .569 | 2.236** | .725 | 0.832 | .609 | 0.901+ | .505 |
| Age | −0.085* | .039 | −0.116* | .049 | −0.037 | .042 | −0.069* | .034 |
| Level of MR | −1.861** | .676 | −1.212 | .862 | −2.283** | .727 | −1.671** | .601 |
| DSb | −1.413* | .606 | −1.250 | .772 | −1.623* | .649 | −1.000+ | .538 |
| Family relations | −0.274** | .079 | −0.278** | .101 | −0.265** | .085 | −0.160* | .070 |
| Model for change | ||||||||
| Slope | −0.254** | .059 | −0.155* | .074 | −0.076 | .084 | −0.315** | .058 |
| Gender | −0.038 | .107 | −0.062 | .133 | −0.029 | .105 | ||
| Age | 0.005 | .007 | 0.005 | .009 | 0.004 | .007 | ||
| Level of MR | −0.042 | .129 | 0.020 | .160 | −0.015 | .125 | ||
| DS | 0.039 | .115 | 0.094 | .143 | 0.029 | .112 | ||
| Family relations | 0.014 | .015 | 0.016 | .019 | −0.008 | .014 | ||
| Time varying covariates |
||||||||
| Placement | 1.068* | .416 | 0.068 | .518 | 1.458* | .572 | 1.063** | .396 |
| Parental death | 1.743** | .424 | 1.797** | .369 | 1.195* | .574 | 1.418** | .400 |
Standard error.
Down syndrome.
p < .05.
p < .01.
p < .10.
Thus, with respect to our first research question, adults with Down syndrome had better functional abilities and less severe asocial and externalized behaviors than did their counterparts with mental retardation due to other causes, but were similar to them on initial level of health and internalized maladaptive behaviors.
Differences Between Adults With Down Syndrome and Adults With Mental Retardation Due to Other Causes in Patterns of Change or Stability Over Time
Our second research question was, do adults with Down syndrome differ from adults with mental retardation due to other causes with respect to their pattern of change or stability over the study period in health, functional abilities, and behavior problems (see model for change section of Table 2,Table 3, and Table 4)? Across all of these analyses, having a diagnosis of Down syndrome was predictive of change only once. There was a trend for those with Down syndrome to decline more in health during the study period than those with mental retardation due to other causes, t(2394)=−1.80, p = .07. Thus, as predicted, with the exception of the trend toward declining health, adults with Down syndrome showed a similar pattern of change and stability over the seven waves of data collection as adults with mental retardation due to other causes. Furthermore, the 24 individuals in our sample with Down syndrome over the age of 40 were not significantly different at any time point on these outcome variables from the younger individuals with Down syndrome or from the younger or older individuals with mental retardation due to other causes.
Table 2,Table 3, and Table 4 also portray the degree of change over the seven waves of data collection for the sample as a whole. As shown in Table 2, the health of sample members declined significantly, as evidenced by the significant slope coefficient, t(2394) = −2.47, p < .05. On average, health declined from being rated in the good to excellent range to being rated as good. As shown in Table 3, two measures of functional abilities also declined: personal care, t(2202) = −2.62, p < .01, and mobility, t(2201) = −5.52, p < .001. However, improvement was observed with respect to housekeeping, t(2198) = 5.07, p < .001, and a pattern of stability was observed in meal-related activities, t(2201) = −0.24, p = .81. As shown in Table 4, the slope of behavior problems, as measured by the generalized, t(1987) = −4.27, p < .001, internalized, t(2000) = −2.10, p < .05, and externalized, t(2017) = −5.46, p < .001, maladaptive indices showed a pattern of decline over the seven waves of data, indicating less severe and less frequent behavior problems over time. However, the asocial maladaptive index showed a pattern of stability over the study period, t(2017) = −0.91, p = .36.
Predicting Initial Status and Patterns of Change or Stability Over Time
Our third research question was, what other characteristics of the individuals with mental retardation and the family predict initial status and changes over the study period in health, functional abilities, and behavior problems?
Health
The findings predicting the initial health status of adults with mental retardation are presented in Table 2 (see model for initial status). Younger adults, as compared to older adults, had better initial health, t(371) = −2.84, p < .01, as did adults whose families had better family relations, t(371) = 3.57, p < .001. A trend was evident for adults with mild or moderate mental retardation to also have better initial health as compared with adults who have severe or profound mental retardation, t(371) = 1.93, p = .054.
Regarding predictors of change in health over the seven waves of data collection, in addition to the trend regarding faster decline over the seven waves of data collection if the adult had a diagnosis of Down syndrome, t(2394) = −1.80, p = .07, being placed outside of the home during the study was also associated with poorer health, t(2394) = −5.29, p < .001, as compared with those who remained living at home throughout the study period. Unexpectedly, we found that experiencing parental death was associated with better health, t(2394) = 2.28, p < .05, in comparison to those whose parents remained alive. Due to the change in respondent associated with maternal death, this finding should be interpreted cautiously.
Functional abilities
The findings predicting the initial status of the four measures of functional abilities (housekeeping, personal care, meal-related activities, and mobility) are presented in Table 3 (see model for initial status). With regard to all measures of functional ability, adults with mild or moderate mental retardation, as compared with adults who had severe or profound mental retardation, had better initial functional abilities (housekeeping, t(371) = 8.92, p < .001; personal care, t(371) = 10.10, p < .001; meal-related activities, t(371) = 9.23, p < .001; and mobility, t(371) = 4.11, p < .001). We noted earlier that adults with Down syndrome compared with adults who had mental retardation due to other causes had better functional abilities at initial status with respect to housekeeping, personal care, meal-related activities, and mobility. There was a trend for higher initial levels of personal care skills when the adult had better family relations, t(371) = 1.76, p = .08, and when the adult child was male, t(371) = −1.76, p = .08.
Table 3 also presents findings regarding changes in functional abilities, as measured by housekeeping, personal care, and mobility, over the seven waves of data collection (see model for change). Because meal-related activities remained stable, predictors of change were not analyzed. Skills in housekeeping improved during the study. The rate of improvement of housekeeping skills for adults was faster for younger individuals, t(2198) = −2.85, p < .01. In contrast, skills in personal care and mobility declined during the study period. The rate of decline in personal care was faster for older individuals, t(2202) = −4.46, p < .001, and, surprisingly, a trend was evident for a faster rate of decline for those with mild or moderate mental retardation, t(2202) = −1.94, p = .052. In interpreting this finding, it is important to note that although individuals with severe or profound mental retardation consistently required help in personal care throughout the study period, those with mild or moderate mental retardation showed minor declines in personal care and remained within the range of continued independence. A trend was also evident for decline in mobility, which was faster for adults with poorer family relations, t(2201) = 1.68, p = .09.
Finally, regarding the time-varying covariates, parental death did not predict differences in any measure of functional abilities. However, being placed outside of the home during the study was associated with significant gains in housekeeping, t(2198) = 7.15, p < .001, and meal-related activities, t(2206) = 5.87, p < .001, and declines in personal care, t(2202) = −2.01, p < .04. Placement outside of the home was not associated with mobility, t(2201) = 0.46, p = .65.
Behavior problems
The findings predicting the initial status of behavior problems, as measured by the generalized, internalized, asocial, and externalized maladaptive indices of the ICAP/SIBR, are presented in Table 4 (see model for initial status). Fewer behavior problems were exhibited initially if the adult with mental retardation was male (generalized, t(371) = 2.46, p < .05; internalized, t(371) = 3.08, p < .01), older (generalized, t(371) = −2.20, p < .05; internalized, t(371) = −2.36, p < .05; externalized, t(371) = −2.01, p < .05), had less severe mental retardation (generalized, t(371) = −2.75, p < .01; asocial, t(371) = −3.14, p < .01; externalized, t(371) = −2.78, p < .01), had better family relations (generalized, t(371) = −3.47, p < .001; internalized, t(371) = −2.76, p < .01; asocial, t(371) = −3.12, p < .01; externalized, t(371) = −2.28, p < .05), and, as previously noted, had a diagnosis of Down syndrome (for the generalized and asocial maladaptive indices). On a trend level, fewer externalized behavior problems were exhibited initially if the adult with mental retardation was male, t(371) = 1.78, p = .08, and had Down syndrome.
Table 4 presents the findings predicting changes in generalized, internalized, and externalized maladaptive indices over the seven waves of data collection (see model for change). Because the asocial maladaptive index remained stable, predictors of change in this variable were not analyzed. No characteristics of the adult with mental retardation or family relations were significant predictors of the decline in these behavior problems.
However, being placed outside of the home during the study period was associated with elevations in some measures of behavior problems (generalized, t(1987) = 2.57, p < .05; asocial, t(2017) = 2.55, p < .05; externalized, t(2017) = 2.69, p < .01), and experiencing parental death during the study was associated with elevations in all measures of behavior problems (generalized, t(1987) = 4.11, p < .001; internalized, t(2000) = 3.40, p < .001; asocial, t(2017) = 2.08, p < .05; externalized, t(2017) = 3.55, p < .001).
Changes preceding and following residential placement and parental death
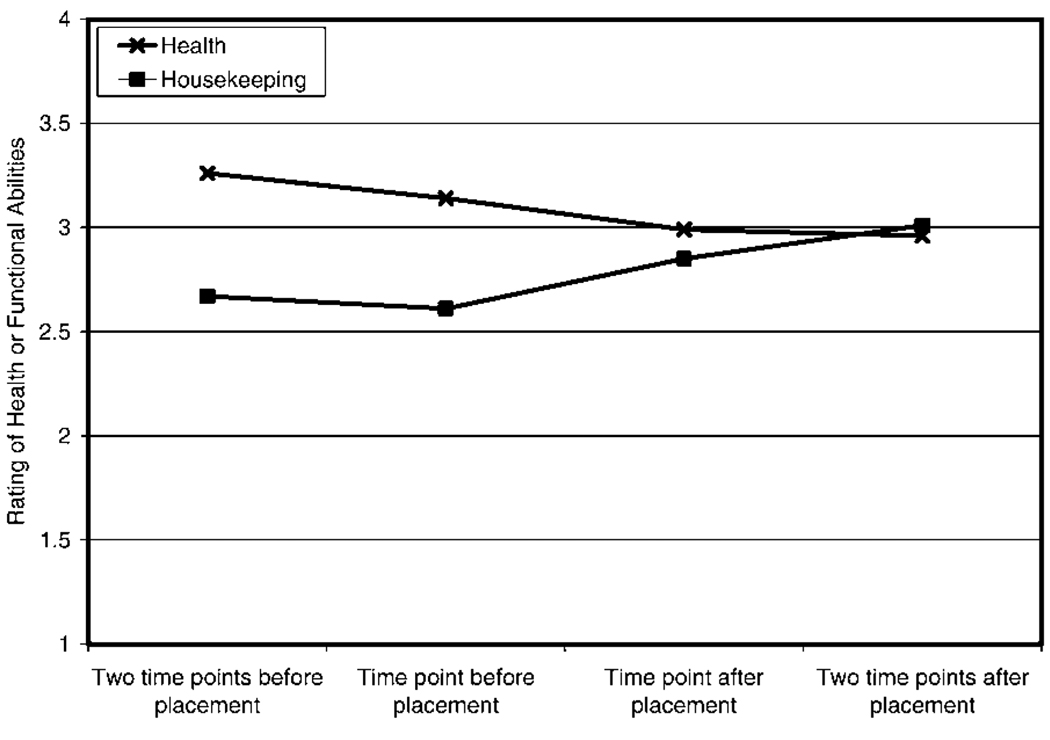
To determine whether the changes in health, functional abilities, and behavior problems preceded or followed residential placement and parental death, we examined the subgroup of individuals experiencing these major life transitions. We examined only those variables for which there were significant effects in the HLM analysis for these time-varying covariates. To explore these changes, we calculated the mean scores of health, functional abilities, and behavior problems at the two points of data collection before and the two points of data collection after these transitions for those cases for whom such data were available. Regarding placement, Figure 1 illustrates that a pattern of gradual decline in health was evident at the two points of data collection before the adult moved from the parental home and just after the adult moved into their residential placement, with a leveling off after that. This observation suggests that declines in health preceded placement temporally. A pattern of improvement was evident in housekeeping from the time point prior to the residential placement to the time point after (see Figure 1). This observation suggests that residential placement could be contributing to improved housekeeping abilities. We were unable to observe any directional effect for meal-related activities and personal care.
Figure 1.
Pattern of change in health and housekeeping before and after placement spanning a time period of 4.5 years (n = 148).
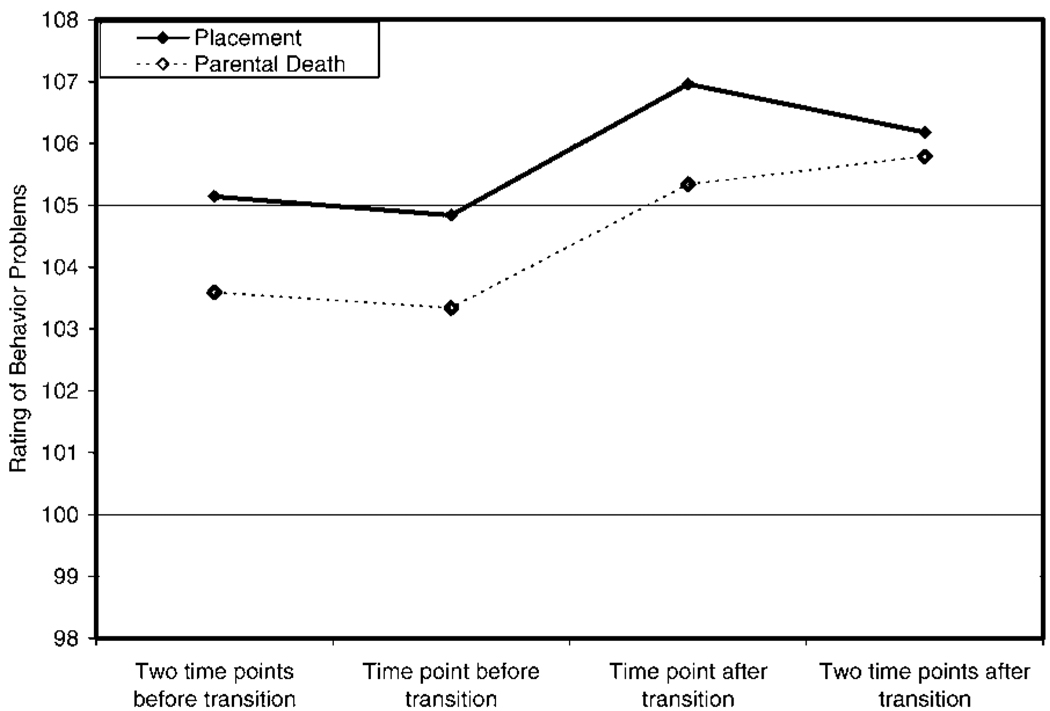
Figure 2 illustrates the ratings of behavior problems at the two points of data collection before and the two points of data collection after the transitions. The pattern observed for all measures of behavior problems was similar, and, therefore, we graphed the generalized maladaptive index only (see Figure 2). Behavior problems appeared to be stable prior to the transition (placement or parental death), worsened just after the transition, and then tended to remain stable or changed slightly. These observations suggest that residential placement and parental death could have contributed to the worsening of behavior problems over time.
Figure 2.
Pattern of change in generalized maladaptive behaviors before and after placement (n = 148) or parental death (n = 102) spanning a time period of 4.5 years.
Discussion
We examined the normative pattern of change in functional abilities of adults with and without Down syndrome prior to the age when declines are common in individuals with Down syndrome. Our analyses suggest a central and important conclusion. That is, prior to age 40, adults with Down syndrome are advantaged with respect to their functional skills and behavioral problems in comparison with others who have mental retardation and comparable with other adults who have mental retardation with respect to their health. This result supports past findings of a Down syndrome advantage in functional abilities (Zigman et al., 1987; Zigman et al., 2002) and extends this advantage to the domains of behavior problems. This is a particularly important finding in light of the solid empirical evidence that as adults with Down syndrome enter mid-life and their elder years, the probability of disadvantaged functioning increases markedly.
Second, we found that adults with Down syndrome had patterns of change over 9 years comparable with adults whose mental retardation was due to other causes with regard to functional abilities and behavior problems. However, there was a trend for health to be declining faster for adults with Down syndrome. Nevertheless, 83% of the adults in our sample, both with and without Down syndrome, remained in good or excellent health by the end of the study when their mean age was 44. Thus, although adults with Down syndrome are at slightly higher risk of declining health than are their counterparts, even prior to the age of 40, the absolute magnitude of this risk is quite small and increases very slowly. So, although adults with Down syndrome generally have a history of medical problems (Roizen, 1996), there is no significant need for concern regarding their age-related health changes in middle adulthood as compared with adults who have mental retardation due to other causes.
Regarding functional abilities, whereas other researchers have found a pattern of stability in functional abilities in younger adults with Down syndrome (Collacott & Cooper, 1997), we found evidence for a pattern of age-related change. For both adults with and those without Down syndrome, functional abilities relating to personal care and mobility evidenced decline, whereas housekeeping skills continued to improve, and only abilities relating to meal-related activities remained stable over the 9 years. Further, in considering behavior problems, we found evidence of improvements (i.e., declines in severity) in overall behavior problems, particularly in internalized and externalized behavior problems for both adults with and without Down syndrome. Thus, prior to the time of elevated risk for dementia, adults with Down syndrome show a strikingly favorable profile of functional skills and behavior problems–better initially on an absolute level in functional abilities and behavior problems than do their counterparts and changing at a rate similar to them on both of these dimensions. Although the current findings are different from those of earlier researchers who found stability, they may also be more sensitive to individual differences because we used a longer time period with more frequent measurement points. As such, our findings provide a very positive outlook for adults with Down syndrome in early to middle adulthood, confirming that their risk for functional and behavioral decline during these life stages is no greater than that found in adults with mental retardation due to other causes.
For our third research question, which was concerned with predictors of absolute levels and change in health, functional abilities, and behavior problems, we found that the most prominent predictors of initial status and change were age, level of mental retardation, gender, family relations, and, as previously discussed, having a diagnosis of Down syndrome. With regard to age, older sample members (who in this study were in their 40s and 50s) had fewer behavior problems and poorer initial health, regardless of whether they had Down syndrome, but age did not predict changes in behavior problems or health. Age did not predict initial levels of functional abilities, but it did predict changes in functional abilities for both adults with and without Down syndrome. This is consistent with past findings among adults with Down syndrome that age was a risk factor for functional decline after age 40 (Friedman & Brown, 2001; Prasher & Chung, 1996; Prasher et al., 1998). Further, because the cross-sectional findings (initial status) are not consistent with the longitudinal findings (change), the need to focus on longitudinal analyses to eliminate the impact of cohort effects in examining changes associated with advancing age is confirmed.
With regard to level of mental retardation, sample members with more severe mental retardation had poorer initial health, poorer initial functional abilities, and worse initial behavior problems. Although severity of mental retardation did not predict changes in health or behavior problems over the study period, it did predict changes in functional abilities. Personal care skills decline more among adults with less severe mental retardation, whereas the skills of adults with more severe mental retardation decline less. This finding both supports (Prasher & Chung, 1996) and contradicts (Burt et al., 1995; Prasher et al., 1998) previous research on the prediction of changes in functional abilities from level of mental retardation or intellectual ability. Because of the contradictory past literature and the current finding being at the trend level, the impact of level of mental retardation on changes in functional ability should be interpreted cautiously.
With regard to gender, females had poorer initial personal care skills and worse behavior problems. However, gender did not predict changes in health, functional abilities, or behavior problems over the study period, consistent with past findings (Burt et al., 1995; Prasher & Chung, 1996; Prasher et al., 1998). Future researchers should continue to control for gender differences in outcome variables. However, there appears to be no need for concern regarding gender and its impact on the trajectory of change over time.
Considering the family environment, having poorer initial family relations was associated with having worse health, poorer personal care skills, and worse behavior problems. Further, mobility declined more among adults with poorer family relations, whereas the skills of adults with better family relations declined less. Having better family relations may lead to more social connections and, thus, a greater focus on maintaining independence in mobility and transportation. However, because this finding was at the trend level, it should be interpreted cautiously and warrants replication. Nevertheless, our finding that the family environment impacts adults with mental retardation is consistent with the literature. There is ample evidence that developmental change is affected by a variety of environmental factors, such as other aspects of the family environment, the social worlds and opportunities available to individuals, and the appropriateness of supportive services. For example, in a Canadian study Temple, Jozsvai, Konstantareas, and Hewitt (2001) found that more years of education predicted lower rates of Alzheimer’s disease among adults with Down syndrome. Hauser-Cram and colleagues (1999), who also used HLM techniques, reported that among children with Down syndrome, growth in communication, daily living skills, and socialization skills were predicted by family cohesion and quality of the mother–child relationship. At the initial time point of this study, all adults were co-residing with their mothers. However, during the study period, about a third of the sample moved from the parental home. It appears that in our sample, health declines in adults with and without Down syndrome preceded and perhaps contributed to their residential placement, consistent with prior analyses of these data (Essex et al., 1997). However, changes in functional abilities and behavior problems followed and may have been influenced by residential placement. A complex pattern was evident with respect to functional abilities, with both gains and losses following placement. These changes may reflect personal care being given greater emphasis in the parental home than in residential care settings, and housekeeping and meal-related skills being given greater emphasis in residential care settings than at home. However, because the rater of functional abilities changed from the mother to a residential caregiver at the time of residential placement, and because other investigators have not found an impact of residential placement on changes in adaptive and maladaptive behaviors (Prasher et al., 1998; Urv, Zigman, & Silverman, 2003), this observation should be interpreted cautiously.
We also examined the impact of parental death on adults with mental retardation. At the initial time point of this study, all mothers and 70% of fathers were alive. However, 48 mothers and 54 fathers died during the study period. In our sample, parental death was not associated with change in functional abilities, but it was associated with change in behavior problems. In examining the pattern of change before and after parental death, we found that behavior problems worsen after parental death and stay elevated for a period greater than 2 years. This supports past findings suggesting that adults with mental retardation experience atypical and prolonged grief following the death of a friend or family member (Dodd, Dowling, & Hollins, 2005; McHale & Carey, 2002). Further, this finding suggests that individuals with mental retardation may benefit from longer grief counseling, continued monitoring of grief symptoms, and continued assessments of their mental health for several years after a parent dies (Dowling, Hubert, White, & Hollins, 2006). Although the current findings are consistent with the literature, they should still be interpreted with care due to the change in respondent that occurred following maternal death. Nevertheless, together with the findings that family relations impact health, functional abilities, and behavior problems, these results confirm the long-term effects of the family and the family environment on the functioning of individuals with mental retardation.
Overall, then, our study brings very good news about the well-being of adults with Down syndrome in early and middle adulthood. The limitations of this analysis are that it was based on a volunteer, largely Caucasian sample. In addition, our observations to determine whether changes in health, functional abilities, and behavior problems preceded or were influenced by residential placement and parental death need to be considered as exploratory. Moreover, findings in this study regarding the impact of the family environment on the individual could be bidirectional, where declines evidenced by the adult with mental retardation could negatively impact the family. Also, the age of the sample members needs to be considered when interpreting the advantage in functional abilities and behavior problems and the disadvantage in health exhibited by individuals with Down syndrome. On average, these individuals were 4 years younger than those with mental retardation due to other causes. Although age was adjusted in the HLM models, it may still be a contributing factor to the advantage exhibited by the individuals with Down syndrome in this sample. Finally, although we extended past research by examining patterns of change in health, functional abilities, and behavior problems, we are limited in that we did not also examine patterns of change in cognitive ability in early to middle adulthood.
Despite these limitations, this study makes several contributions to the understanding of the normative aging of adults with and without Down syndrome. We extend past research contributions by introducing constancy in the source of most data, focusing on a longer period of time in the early and middle years of adulthood and including a comparison group of adults with mental retardation due to other causes. Further, the research in this area is extended through examination of both individual and family characteristics as factors to explain differences in developmental trajectories. The next analytic challenge is to continue to examine possible causal relationships among the outcome variables (Urv et al., 2003). The better we understand normative aging of adults with and without Down syndrome, the more able we will be to understand functional declines that may be evidenced later in life.
Acknowledgments
This manuscript was prepared with support from the National Institute on Aging (R01 AG08768) and the National Institute on Child Health and Human Development (P30 HD03352, T32 HD07489). We acknowledge Jan Greenberg for his helpful comments on this project and Doris Kistler for her assistance on an earlier version of this manuscript, which was presented at the 2001 Gatlinburg Conference on Research and Theory in Intellectual and Developmental Disabilities.
Contributor Information
Anna J. Esbensen, Waisman Center, University of Wisconsin-Madison
Marsha Mailick Seltzer, Waisman Center, University of Wisconsin-Madison.
Marty Wyngaarden Krauss, Brandeis University.
References
- Bittles AH, Glasson EJ. Clinical, social, and ethical implications of changing life expectancy in Down syndrome. Developmental Medicine and Child Neurology. 2004;46:282–286. doi: 10.1017/s0012162204000441. [DOI] [PubMed] [Google Scholar]
- Borthwick-Duffy SA, Eyman RK, White JF. Client characteristics and residential placement patterns. American Journal of Mental Deficiency. 1987;92:24–30. [PubMed] [Google Scholar]
- Bruininks RH, Hill BK, Weatherman RF, Woodcock RW. Inventory for Client and Agency Planning (ICAP) Allen, TX: DLM Teaching Resources; 1986. [Google Scholar]
- Bruininks RH, Woodcock RW, Weatherman RE, Hill BK. Scales of Independent Behavior–Revised comprehensive manual. Itasca, IL: Riverside; 1996. [Google Scholar]
- Bryk AS, Raudenbush SW. Applications of hierarchical linear models to assessing change. psychological Bulletin. 1987;101:147–158. [Google Scholar]
- Burt DB, Loveland KA, Chen YW, Chuang A, Lewis KR, Cherry L. Aging in adults with Down syndrome: Report from longitudinal study. American Journal on Mental Retardation. 1995;100:262–270. [PubMed] [Google Scholar]
- Burt DB, Primeaux-Hart S, Loveland KA, Cleveland LA, Lewis KR, Lesser J, Pearson PL. Aging in adults with intellectual disabilities. American Journal on Mental Retardation. 2005;110:268–284. doi: 10.1352/0895-8017(2005)110[268:AIAWID]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Carr J. Intellectual and daily living skills of 30-year-olds with Down’s syndrome: Continuation of a longitudinal study. Journal of Applied Research in Intellectual Disabilities. 2000;13:1–16. [Google Scholar]
- Carr J. Patterns of ageing in 30–35-year-olds with Down’s syndrome. Journal of Applied Research in Intellectual Disabilities. 2003;16:29–40. [Google Scholar]
- Collacott RA, Cooper S. A five-year follow-up study of adaptive behaviour in adults with Down syndrome. Journal of Intellectual and Developmental Disability. 1997;22:187–197. [Google Scholar]
- Day SM, Strauss DJ, Shavelle RM, Reynolds RJ. Mortality and causes of death in persons with Down syndrome in California. Developmental Medicine and Child Neurology. 2005;47:171–176. doi: 10.1017/s0012162205000319. [DOI] [PubMed] [Google Scholar]
- Devenny DA, Hill AL, Patxot O, Silverman W, Wisniewski KE. Ageing in higher functioning adults with Down’s syndrome: An interim report in a longitudinal study. Journal of Intellectual Disability Research. 1992;36:241–250. doi: 10.1111/j.1365-2788.1992.tb00511.x. [DOI] [PubMed] [Google Scholar]
- Devenny DA, Silverman W, Hill AL, Jenkins E, Sersen EA, Wisniewski KE. Normal ageing in adults with Down’s syndrome: A longitudinal study. Journal of Intellectual Disability Research. 1996;40:208–221. [PubMed] [Google Scholar]
- Dodd P, Dowling S, Hollins S. A review of the emotional, psychiatric and behavioral responses to bereavement in people with intellectual disabilities. Journal of Intellectual Disability Research. 2005;49:537–543. doi: 10.1111/j.1365-2788.2005.00702.x. [DOI] [PubMed] [Google Scholar]
- Dowling S, Hubert J, White S, Hollins S. Bereaved adults with intellectual disabilities: A combined randomized controlled trial and qualitative study of two community-based interventions. Journal of Intellectual Disability Research. 2006;50:277–287. doi: 10.1111/j.1365-2788.2005.00759.x. [DOI] [PubMed] [Google Scholar]
- Essex EL. Parental caregivers of adults with mental retardation: The experience of older mothers and fathers. Dissertation Abstracts International. 1998;59(08):3208. (UMI No. 9837038) [Google Scholar]
- Essex EL, Seltzer MM, Krauss MW. Residential transitions of adults with mental retardation: predictors of waiting list use and placement. American Journal on Mental Retardation. 1997;101:613–629. [PubMed] [Google Scholar]
- Eyman RK, Borthwick-Duffy SA. Trends in mortality rates and predictors of mortality. In: Seltzer MM, Krauss MW, Janicki MP, editors. Life course perspectives in adulthood and old age. Washington, DC:: American Association on Mental Retardation; 1994. pp. 93–105. [Google Scholar]
- Eyman RK, Call RL, White JF. Life expectancy of persons with Down syndrome. American Journal on Mental Retardation. 1991;95:603–612. [PubMed] [Google Scholar]
- Friedman O, Brown I. Assessing dementia of the Alzheimer type in people with Down syndrome. Journal of Developmental Disabilities. 2001;8:75–92. [Google Scholar]
- Glasson EJ, Sullivan SG, Hussain R, Petterson BA, Montgomery PD, Bittles AH. The changing survival profiles of people with Down’s syndrome: Implications for genetic counselling. Clinical Genetics. 2002;62:390–393. doi: 10.1034/j.1399-0004.2002.620506.x. [DOI] [PubMed] [Google Scholar]
- Hauser-Cram P, Warfield ME, Shonkoff JP, Krauss MW, Upshur CC, Sayer A. Family influences on adaptive development in young children with Down syndrome. Child Development. 1999;70:979–989. doi: 10.1111/1467-8624.00071. [DOI] [PubMed] [Google Scholar]
- Idler EL, Benyamini Y. Self-rated health and mortality: A review of twenty-seven community studies. Journal of Health and Social Behavior. 1997;38:21–37. [PubMed] [Google Scholar]
- Janicki MP, Dalton AJ. Prevalence of dementia and impact on intellectual disability services. Mental Retardation. 2000;38:276–288. doi: 10.1352/0047-6765(2000)038<0276:PODAIO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Krauss MW, Seltzer MM. An unanticipated life: The impact of lifelong care-giving. In: Bersani H, editor. Responding to the challenge: International trends and current issues in developmental disabilities. Brookline, MA: Brookline Books; 1999. pp. 173–187. [Google Scholar]
- MacHale R, Carey S. An investigation of the effects of bereavement on mental health and challenging behaviour in adults with learning disability. British Journal of Learning Disabilities. 2002;30:113–117. [Google Scholar]
- Mahoney FE, Barthel DW. Functional evaluation: The Barthel Index. Mary-land State Medical Journal. 1965;14:61–65. [PubMed] [Google Scholar]
- Moos RH, Moos BS. Family Environment Scale: Manual. Second Edition. Palo Alto, CA: Consulting Psychologists Press; 1986. [Google Scholar]
- Prasher VP, Chung MC. Causes of age-related decline in adaptive behavior in adults with Down syndrome: Differential diagnoses of dementia. American Journal on Mental Retardation. 1996;101:175–183. [PubMed] [Google Scholar]
- Prasher VP, Chung MC, Haque MS. Longitudinal changes in adaptive behavior in adults with Down syndrome: Interim findings from a longitudinal study. American Journal on Mental Retardation. 1998;103:40–46. doi: 10.1352/0895-8017(1998)103<0040:LCIABI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Raudenbush SW, Bryk AS. Hierarchical linear models: Applications and data analysis methods. 2nd ed. Thousand Oaks, CA: Sage; 2001. [Google Scholar]
- Rasmussen DE, Sobsey D. Age, adaptive behavior, and Alzheimer disease in Down syndrome: Cross-sectional and longitudinal analyses. American Journal on Mental Retardation. 1994;99:151–165. [PubMed] [Google Scholar]
- Roizen NJ. Down syndrome and associated medical disorders. Mental Retardation and Developmental Disability Research Reviews. 1996;2:85–89. [Google Scholar]
- Seltzer MM, Krauss MW. Aging parents with co-resident adult children: The impact of lifelong caregiving. In: Seltzer MM, Krauss MW, Janicki MP, editors. Life course perspectives on adulthood and old age. Washington, DC: American Association on Mental Retardation; 1994. pp. 3–18. [Google Scholar]
- Seltzer MM, Ivry J, Litchfield LC. Family members as case managers: partnership between the formal and informal support networks. The Gerontologist. 1987;27:722–728. doi: 10.1093/geront/27.6.722. [DOI] [PubMed] [Google Scholar]
- Seltzer MM, Krauss MW, Hong J, Orsmond GI. Continuity or discontinuity of family involvement following residential transitions of adults who have mental retardation. Mental Retardation. 2001;39:181–194. doi: 10.1352/0047-6765(2001)039<0181:CODOFI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Silverman W, Zigman WB, Kim H, Krinsky-McHale S, Wisniewski HM. Aging and dementia among adults with mental retardation and Down syndrome. Topics in Geriatric Rehabilitation. 1998;13:49–64. [Google Scholar]
- Temple V, Jozsvai E, Konstantareas MM, Hewitt TA. Alzheimer dementia in Down’s syndrome: The relevance of cognitive ability. Journal of Intellectual Disability Research. 2001;45:47–55. doi: 10.1046/j.1365-2788.2001.00299.x. [DOI] [PubMed] [Google Scholar]
- Urv TK, Zigman WB, Silverman W. Maladaptive behaviors related to adaptive decline in aging adults with mental retardation. American Journal on Mental Retardation. 2003;108:327–339. doi: 10.1352/0895-8017(2003)108<327:MBRTAD>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Yang Q, Rasmussen SA, Friedman JM. Mortality associated with Down’s syndrome in the USA from 1983 to 1997: A population-based study. The Lancet. 2002;359:1019–1025. doi: 10.1016/s0140-6736(02)08092-3. [DOI] [PubMed] [Google Scholar]
- Zigman WB, Jenkins EC, Tycko B, Schupf N, Silverman W. Mortality is associated with apolipoprotein E γ4 in nondemented adults with Down syndrome. Neuroscience Letters. 2005;390:93–97. doi: 10.1016/j.neulet.2005.08.002. [DOI] [PubMed] [Google Scholar]
- Zigman WB, Schupf N, Haveman M, Silverman W. The epidemiology of Alzheimer disease in intellectual disability: Results and recommendations from an international conference. Journal of Intellectual Disability Research. 1997;41:76–80. doi: 10.1111/j.1365-2788.1997.tb00679.x. [DOI] [PubMed] [Google Scholar]
- Zigman WB, Schupf N, Lubin RA, Silverman WP. Premature regression of adults with Down syndrome. American Journal of Mental Deficiency. 1987;92:161–168. [PubMed] [Google Scholar]
- Zigman WB, Schupf N, Sersen E, Silverman W. Prevalence of dementia in adults with and without Down syndrome. American Journal on Mental Retardation. 1995;100:403–412. [PubMed] [Google Scholar]
- Zigman WB, Schupf N, Urv T, Zigman A, Silverman W. Incidence and temporal patterns of adaptive behavior change in adults with mental retardation. American Journal on Mental Retardation. 2002;107:161–174. doi: 10.1352/0895-8017(2002)107<0161:IATPOA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]