Abstract
Using data from the Study of Midlife in the United States (MIDUS), this article examines: (1) the effect of having children with developmental or mental health problems on parents’mental and physical health, (2) the extent to which this effect varies by parental age and gender, and (3) the effects of disability-related factors on the well-being of parents of children with disabilities. Compared to parents of non-disabled children, parents of disabled children experienced significantly higher levels of negative affect, marginally poorer psychological well-being, and significantly more somatic symptoms, controlling for sociodemographic variables. Mothers did not differ from fathers in their well-being. Older parents were significantly less likely to experience the negative effect of having a disabled child than younger parents, suggesting an age-related attenuation of the stress of non-normative parenting.
Having a child with developmental or mental health problems poses significant stress for parents who have the responsibility of providing daily help to their children, often even after their children become adults (Greenberg, Seltzer, and Greenley 1993; Kling, Seltzer, and Ryff 1997). Nevertheless, there is a great deal of heterogeneity in parental adaptation to children’s disability (Seltzer et al. 2001), although relatively little is known about the factors that affect which parents have poor physical and mental health and which evidence a pattern of resiliency.
We address this gap by examining three research questions. First, using a nationally representative probability sample of parents of children with developmental or mental health problems and parents of children without such problems, we examine the effects of having a disabled child on parents’ physical and mental health. Second, we investigate the extent to which the effects of children’s disability on parents’ well-being are moderated by parental age and gender. Finally, using only the sample of parents of disabled children, we explore the predictors of well-being among parents of disabled children. Examining these questions will help us better understand the variability across the life course of the impact of parenting a disabled child.
THEORY AND EVIDENCE
Stress of Parenting a Disabled Child
Parents of children with developmental or mental health problems face multiple challenges in child care. They take on additional financial burdens caused by the disability because insurance often fails to cover the full cost of services and treatment (Clark and Drake 1994). Among the objective burdens of care, parents find most stressful the challenge of managing their child’s problematic behavior (Baker and Heller 1996; Lecavalier, Leone, and Wiltz 2006). There are also emotional burdens associated with the stigma of disabilities, grief over the recognition that the child never will achieve normative adult milestones, and worry about the future care of the son or daughter after the parent’s death (Seltzer et al. 2001). As a consequence of these long-term chronic strains associated with parenting a disabled child, parents of disabled children experience more physical symptoms and higher levels of depression than parents of non-disabled children (Seltzer et al. 2004; Singer 2006), although parents of children with developmental disabilities appear to have more normative patterns of physical and mental health than parents of children with mental health problems (Seltzer et al. 2001).
Age Differences in the Effect of Having Children with Disabilities
There is a growing body of research on the consequences of parenting a disabled child, but most of this research has focused on parents at specific life stages. Few studies have sampled parents at different points in the life course to examine whether the effects of parenting a disabled child vary at different stages of life. Given the extended life expectancy of both children with disabilities and their parents (Seltzer and Krauss 1994), it is increasingly important to examine the impact of parenting a disabled child across the life course. Thus, we focus on parental age as one of the important factors that may influence adjustment to non-normative parenting stress.
Two conceptual models guided our investigation of age differences in the stress of parenting a disabled child. The adaptation model (Lazarus and Folkman 1984) suggests that the more time an individual has experience with a source of stress, the greater the adaptation to this challenge. Over time, parents adjust to the stress of their child’s disability as they develop skills to better respond to their family circumstances.
Alternatively, the cumulative stress model posits that the wear and tear of caregiving stress accumulates over time and that individuals who have been exposed to chronic stressors for a longer period of time are more vulnerable than those with a shorter period of exposure (Hoyert and Seltzer 1992; Townsend et al. 1989). Thus, according to this model, the stress of parenting a child with disability would be magnified in older age.
Although the adaptation and cumulative stress models have been examined in a variety of caregiving contexts, such as caring for impaired elders (Townsend et al. 1989) or Alzheimer’s patients (George 1983), to date no study that we know of has examined the age differences in the impact of non-normative parenting in light of these two conceptual models. The research on the relationship between the caregiver’s age and caregiver distress has been inconclusive. Age was related to lower levels of distress in several studies (Hoyert and Seltzer 1992; Magana et al. 2007; Parks and Pilisuk 1991; Reinhard and Horwitz 1995; Russo et al. 1995), but age was unrelated to caregiver burden in others (Draper et al. 1992; Dura, Stukenberg, and Kiecolt-Glaser 1991; Neundorfer 1991; Noh and Avison 1988; Schulz and Williamson 1991; Semple 1992). Older parents experience lower levels of distress in response to the child’s behavior problems than younger parents, yet they also experience increased levels of emotional and cognitive strain (Cook et al. 1994).
In contrast, research on the general population of non-caregivers reports a largely consistent positive association between age and affective well-being. For example, studies have suggested that older adults show greater positive well-being (Carstensen and Charles 1998) and less negative affect (Mroczek and Kolarz 1998). In addition, older adults evaluate many aspects of psychological well-being more positively than younger adults (Ryff and Keyes 1995). Lawton, Kleban, and Dean (1993) found lower levels of depression and anxiety among older adults than among younger adults, although other studies have found a curvilinear relationship between age and depression whereby levels of depressive symptoms are lowest at the midlife and highest among younger and older adults (Drentea 2005; Mirowsky and Ross 1992).
In sum, although the findings regarding the age differences in caregiving stress are inconclusive, a substantial body of literature suggests age-related attenuation in psychological distress in the general population. Our objective is to examine whether the stress of parenting a disabled child also declines with age, so that the gap between these parents and parents with non-disabled children in levels of well-being is reduced in older age. This decline would suggest a pattern of adaptation among parents of disabled children.
Gender Differences in the Effect of Having Children with Disabilities
Gender is a second factor that may be associated with variability in the effect of having a disabled child. A large body of research has suggested that women bear a greater caregiving burden than men. Women not only spend more time caring for other family members, but they tend to also experience greater depression, poorer well-being, and worse physical health outcomes than men in caregiving roles, although these differences are often small in magnitude (for meta-analyses of studies on gender differences in caregiving burden, see Miller and Cafasso [1992] and Pinquart and Sörensen [2006]). Studies have attributed these gender differences to life-long socialization patterns. In the traditional division of family labor, women were expected to take care of family members and household matters, while men were expected to engage in economic activities outside of the home (Barusch and Spaid 1989). Today, the boundaries between men’s and women’s roles are becoming less distinct, yet caregiving and parenting are still more the responsibility of women than men (Ross and Van Willigen 1996).
Despite much interest in gender differences in the consequences of caregiving, few studies have examined whether mothers and fathers are differentially affected by the experience of parenting a disabled child. Some research suggests that mothers of children with mental retardation provide greater hours of support and perceive greater burden than fathers (Heller, Hsieh, and Rowitz 1997; Pruchno and Patrick 1999), yet other studies report that mothers and fathers experience similar levels of subjective burden and depressive symptoms (Essex and Seltzer 1999). Seltzer et al. (2001) found that mothers of children with developmental disabilities experience a greater decrease in their hours of employment and job stability than fathers when compared to parents with a non-disabled child, but they found no gender differences in psychological or physical well-being. As for parents of children with mental health problems, Seltzer et al. (2001) found that mothers exhibit greater depressive symptoms and fathers experience greater alcohol symptoms than the comparison group, whereas Greenberg (2002) found few gender differences in parents’ level of stigma and frequency of disruptions related to the mental health problems of their children.
One reason for these inconsistent findings may be that the samples utilized in these studies vary in their characteristics. Although Heller et al. (1997) and Essex and Seltzer (1999) both used volunteer samples of parents of children with mental retardation, the former had a wide age range, whereas the latter used only mothers age 55 or older. Seltzer et al. (2001) used a probability sample, but this sample was based on one cohort of a single generation, all of whom graduated from high school. The current study extends previous literature by examining gender differences in the impact of having children with disabilities using a probability sample of different age cohorts.
Disability-Related Factors Affecting the Well-Being of Parents of Children with Developmental Disorders and Mental Health Problems
In addition to contrasting parents of children with disabilities and parents of non-disabled children, we investigate factors that may account for the variability in well-being within the group of parents of children with disabilities, including parental age at the onset of the child’s disability, duration of the child’s disability, whether the child lives with the parent, and the presence of multiple children with disabilities in the family.
As noted above, based on previous literature, we hypothesized that there would be age-related attenuation in the effect of having a disabled child. However, there may be two reasons why there would be such age-related differences. One possible reason is the level of maturity of parents when the child begins to have problems. Although focusing on adolescent parents, Sommer et al. (1993) suggest that parents who are older at the time of the birth of their child are more cognitively ready to parent than younger parents. By extension, it is possible that parents who are older at the onset of their child’s disability may be more mature and thus better able to deal with potential problems that may arise from parenting a disabled child. Older parents may also have more parenting experiences, including experiences parenting other non-disabled children, which may lead older parents to be less affected by the child’s disability than younger parents. A second possible reason for age-related attenuation of the effect of having a disabled child is the parent’s adaptation to stress over time. As the parent of a disabled child spends more time coping with the child’s disability, the parent may show greater adaptation to this role and thus show lower levels of distress and greater well-being.
In order to examine both the effects of maturity and the effect of adjustment over time, we decompose the effect of parental age into two variables: (1) parental age at the onset of disability and (2) duration of child’s disability. The former variable can illustrate how maturity plays a role in adjustment to non-normative parenting stress, whereas the latter can highlight the adaptation effects among parents of disabled children. These two effects (i.e., maturity and adaptation) are complementary rather than competing in explaining the predicted age-related attenuation in the stress of parenting a disabled child.
Next, we examine the effects of two other disability-related factors on the well-being of parents: (1) whether the child with the disability lives with the parent and (2) the presence of multiple children with disabilities in the family. The co-residence status of the child is included because parents of co-residing children spend more time providing care (Heller et al. 1997), which may in turn affect parental mental and physical health (Miltiades and Pruchno 2001). The presence of multiple children with disabilities can also make the parents more vulnerable to stress by increasing the amount of care they must provide (Orsmond, Lin, and Seltzer forthcoming).
Influences of Other Contextual Factors
In addition to parental age, gender, and disability-related factors, our multivariate analyses control for sociodemographic variables that may confound the effects of having a disabled child, including parental education, income, employment, and marital status. Lower socioeconomic status or single parenthood may be correlated with both the status of having a child with disability and poorer well-being (Seltzer et al. 2004). We also control for the number of children and the number of co-resident children, as these variables can affect the levels of caregiving burden among parents of disabled children (Greenberg et al. 2004).
RESEARCH HYPOTHESES
In sum, we examine the following six hypotheses based on the previous literature. The first three hypotheses address the differences between parents of children with disabilities and parents of non-disabled children. The next three hypotheses address within-group variability among parents of children with disabilities.
Parents of Children with Disabilities versus Parents of Non-Disabled Children
-
H1
Parents of children with developmental or mental health problems will have higher levels of negative affect, lower levels of psychological well-being, and a greater number of somatic symptoms than parents of non-disabled children.
-
H2
There will be age differences in the impact of parenting a disabled child. Specifically, we hypothesize that the negative impact of having a disabled child will be lower among older adults than among younger adults. That is, younger parents of disabled children will differ more from their age peers in the comparison group than older parents will differ from their same-age peers, and thus the well-being gap will narrow with older age.
-
H3
Mothers will be more negatively affected than fathers by having a disabled child.
Within-Group Variability
-
H4
Based on the maturity model, we hypothesize that parents who were older at the onset of their child’s disability will experience less distress and have better well-being than those who were younger at the onset of disability.
-
H5
Based on the adaptation model, we hypothesize that the longer the duration of disability the lower the level of distress and the higher the level of well-being.
-
H6
We hypothesize that parents who live with their child with the disability and parents who have multiple children with disabilities in the family will experience greater distress and lower levels of well-being.
METHODS
Data
Data for this analysis were drawn from the MIDUS study (Study on Midlife in the United States; Brim et al. 2004), a nationally representative probability sample of English-speaking, non-institutionalized adults ages 25 to 74 when they were first studied in 1995–1996. MIDUS is comprised of three samples: (1) a national sample selected by random digit dialing (which we refer to as the main respondents), (2) siblings of these respondents, and (3) twins whose co-twin was in the national sample. The first round of data collection took place between 1995 and 1996 (MIDUS I), which consisted of computer-assisted telephone interviews and mail-back questionnaires (n = 7,108). The response rate for MIDUS I data was 87 percent for the mail questionnaire and 70 percent for the phone interview. Followup data were collected from 2004 to 2005 (MIDUS II). The overall response rate for complete MIDUS II data (phone and mail survey) adjusting for mortality was 60.8 percent (n = 4,032).
We analyze MIDUS II data instead of MIDUS I for this article for two reasons. First, MIDUS II includes a set of screening questions to identify respondents who had a child with a developmental or a mental health problem. Such questions were not asked at MIDUS I. At MIDUS II, all parents were asked if any of their children had a developmental or a mental health problem. If a parent responded in the affirmative, he or she was asked which child had the condition, when the symptoms first appeared, and to identify the specific diagnosis. The second reason we used MIDUS II data for the present analysis is that for 26.7 percent of the sample of parents of children with either a developmental or a mental health problem identified at MIDUS II, the child’s symptoms did not begin to manifest until after the MIDUS I data collection. Thus, using MIDUS II yields a larger sample size for this analysis than MIDUS I.
Because we focus on only MIDUS II data, we cannot examine the extent to which having a disabled child affects longitudinal changes in parental well-being over time (i.e., between MIDUS I and II). However, given that our objective is to examine age differences in the effect of having a disabled child rather than age differences in the change in well-being over a ten-year period, cross-sectional data are appropriate for the current study.
We created two analytic samples. First, we included 296 respondents who had a disabled child. Of these, 163 respondents had a child with a developmental problem, including conditions such as attention deficit hyperactivity disorder, learning disabilities, cerebral palsy, Down syndrome, and other types of mental retardation. The other 133 respondents had a child with a mental health problem, including anxiety disorders, bipolar disorder, depression, and schizophrenia. Table 1 shows the frequency of different types of children’s disabilities and the mean age of onset for each disability condition.
TABLE 1. Mean age of onset by conditions.
| Child’s age of onset |
Parental age at child’s onset |
|||||
|---|---|---|---|---|---|---|
| n | Mean | SD | n | Mean | SD | |
| Developmental Problems | ||||||
| Attention deficit hyperactivity disorder | 44 | 6.27 | 5.27 | 42 | 34.14 | 7.71 |
| Learning disabilities | 28 | 5.57 | 5.85 | 27 | 31.93 | 7.87 |
| Mental retardation | 17 | 2.82 | 4.25 | 17 | 30.24 | 5.54 |
| Cerebral palsy | 13 | .38 | 1.12 | 13 | 28.92 | 7.18 |
| Epilepsy | 11 | 12.00 | 8.99 | 11 | 39.42 | 11.44 |
| Down syndrome | 7 | .00 | .00 | 7 | 32.43 | 6.32 |
| Other developmental disorders | 38 | 4.03 | 5.75 | 37 | 31.36 | 7.38 |
| Mental Health Problems | ||||||
| Bipolar disorder | 45 | 18.09 | 7.82 | 44 | 44.44 | 8.38 |
| Depression | 34 | 17.18 | 8.30 | 34 | 43.38 | 10.65 |
| Schizophrenia | 16 | 22.31 | 6.36 | 16 | 50.11 | 6.00 |
| Anxiety disorder | 11 | 17.36 | 9.50 | 11 | 46.31 | 7.35 |
| Drug/alcohol problem | 9 | 18.11 | 5.18 | 7 | 41.71 | 8.28 |
| Other mental health problems | 9 | 14.89 | 4.08 | 9 | 43.11 | 6.58 |
Notes: Parental age at child’s onset could not be calculated for some cases because respondents did not provide information on child’s current age. Thus, sample sizes are not identical.
Through the screening questions in the telephone interview, we identified an additional 71 respondents who had a child with one of these disabilities. However, these respondents did not complete the mail survey containing many of the key variables for the present analysis, and thus they were not included in the analyses reported below. Furthermore, there were nine sibling or twin pairs of respondents, both of whom had a child with disability. To prevent dependency in the data, one sibling/twin respondent was selected, namely the one whose child had a more severe condition, and the other sibling/twin was removed from the sample. As compared with those who did not return the mail survey (n = 71), individuals with complete data (n = 296) were older (by four years), more likely to be female (by 12%), and had a slightly higher mean education level (by .63 years). In other respects (e.g., marital and employment status, proportion of non-Hispanic whites), the two groups were similar.
The second analytic sample was the comparison group, which was selected based on the following criteria: (1) the respondent had at least one living child, but no child with a disability or chronic health condition, (2) the respondent never provided care to a family member, and (3) the respondent did not have a sibling or a twin in the MIDUS sample who was included in the first analytic sample (to prevent dependence in the data). Of the MIDUS II respondents, 1,773 met these three criteria. Consistent with the procedures described above, we included only those 1,393 respondents in the comparison group who returned the mail survey as well as participated in the telephone interview. Compared to those who did not return the mail survey (n = 380), individuals with complete data (n = 1,393) were older (by five years), more likely to be female (by 11%), more likely to be non-Hispanic white (by 8%), and less likely to be employed (by 5%). In other respects (e.g., marital status and education), those with complete data were similar to those who were missing data in the mail survey.
Measures
Dependent variables
We included three dependent variables: negative affect, psychological well-being, and somatic symptoms. Negative affect (α = .85) is the sum of six items (Mroczek and Kolarz 1998). Respondents were asked, “During the past 30 days, how much of the time did you feel (1) so sad nothing could cheer you up, (2) nervous, (3) restless or fidgety, (4) hopeless, (5) that everything was an effort, and (6) worthless?” Response categories ranged from 1 to 5 (none of the time, a little of the time, some of the time, most of the time, and all of the time). Higher scores represent greater negative affect.
The measure of overall psychological well-being (α = .94) is the sum of 42 items measuring six domains of positive well-being (Ryff 1989): autonomy, environmental mastery, purpose in life, positive relations with others, personal growth, and self acceptance. Based on high-order factor analysis, Ryff and Keyes (1995) have shown that these domains form a second-order “well-being” factor. Participants indicated the extent to which they agreed or disagreed with each item on a scale, ranging from strongly disagree (coded 1) to strongly agree (7). Negative items were recoded so that higher scores indicated greater well-being.
The measures of negative affect and overall psychological well-being were calculated for a respondent when at least 50 percent of the items for that scale had valid responses. When this criterion was met, missing values were imputed with the mean of available items in calculating the total score.
The measure of somatic symptoms (α = .69) is a count of the number of somatic symptoms reported by the respondent from a list of seven symptoms: headaches, backaches, sweating a lot, stiffness in joints, trouble getting to sleep or staying asleep, leaking urine, and pains or aches in extremities. Respondents were asked how often they experienced these symptoms in the past 30 days. Response categories ranged from 1 to 6 (not at all, once a month, several times a month, once a week, several times a week, almost every day). Symptoms were counted toward the summary score if the frequency was several times a month or greater.
Conceptually, three outcome measures assess both positive (Ryff psychological well-being) and negative (negative affect) aspects of psychological well-being, as well as physical health (somatic symptoms). Empirically, the three measures are significantly correlated in the expected directions (p < .001): r = −.59 (negative affect and psychological well-being), .41 (negative affect and somatic symptoms), and −.33 (psychological well-being and somatic symptoms).
Independent variables
We included three main independent variables: parental age (in years), parental gender (1 = mother; 0 = father), and whether the parent had a disabled child. For the latter variable, we created two dichotomous variables: (1) parenting a child with a developmental problem, coded as 1 = respondent has a child with a developmental problem, 0 = otherwise; and (2) parenting a child with a mental health problem, similarly coded. Children who had both developmental and mental health problems (n = 33) were assigned to one group based on two decision rules. The first decision rule pertained to the chronic nature of the condition, and the child was assigned to either the developmental or mental health problems group based on which condition was the more chronic condition. For example, if the child had both bipolar disorder and attention deficit hyperactivity disorder, the respondent was assigned to the mental health problems group. The second rule pertained to the age of onset, and thus if a child had both a chronic developmental problem and a chronic mental health problem diagnosis, the respondent was assigned to the developmental problem group because developmental problems begin earlier in life than mental health problems. The categorization of children with dual diagnoses was conducted by two independent raters, with all disagreements resolved by consensus among the four authors.
Sociodemographic variables
We included as controls sociodemographic variables that may confound the effect of having a disabled child on parental well-being. The variables include employment status (1 = employed; 0 = not employed), marital status (1 = married; 0 = not married), race (1 = non-Hispanic white; 0 = others), education (in years), income, number of children, and the number of co-resident children.
Disability-related variables
For respondents who had a disabled child, we included four additional variables: (1) parental age at the onset of child’s disability (in years), (2) the duration of the child’s disability (in years), (3) whether the respondent has more than one child with a disability (1 = yes; 0 = no), and (4) whether the child with the disability co-resides with the parent (1 = yes; 0 = no). Duration was calculated by subtracting the age of onset of the disability from the child’s current age. Parent’s age at the onset of child’s disability was calculated by subtracting duration from parent’s current age.
Analysis Plan
We first present means and standard deviations of all variables to describe the sample. We used analysis of variance (ANOVA) to detect significant differences in means between the comparison, developmental problems, and mental health problems groups. We used chisquare tests to detect significant differences in proportions (for the binary variables) between the three groups. Post-hoc t-tests were conducted when F ratios were significant. Specifically, in order to further examine differences between developmental and mental health problems groups and the control group, we conducted post-hoc tests using Dunnett t-tests. Dunnett’s test is more appropriate than other tests (e.g., Bonferroni’s) for this kind of comparison because we are interested in contrasting developmental and mental health problems groups to the comparison group, rather than comparing all three groups. Next, we used ordinary least squares (OLS) hierarchical regression to examine the effects of parenting a disabled child, parental age, and parental gender on well-being outcomes, controlling for potential confounding factors. In this analysis, we included the entire sample of 1,689 respondents (296 who had a disabled child and 1,393 in the comparison group). Finally, we focused on only the sample of 296 parents who had a disabled child, and using OLS regression models, we conducted within-disability group analyses to examine the effect of disability-specific variables as well as demographic variables on the well-being of these parents. Models are presented separately for the developmental problems group and the mental health problems group.
In preliminary analyses, we also examined the effects of the gender and age of the child with a disability, but these variables were never significantly related to our dependent variables, so we dropped them from our regression models.
RESULTS
Group Comparisons
Table 2 presents descriptive statistics comparing the means (or proportions) of dependent and independent variables for the comparison, developmental problems, and mental health problems samples. The three groups (see Table 2, panel a) differed significantly with respect to levels of negative affect, psychological well-being, and somatic symptoms. Post-hoc contrasts indicated that both parents of children with developmental problems and parents of children with mental health problems reported greater levels of negative affect and a greater number of somatic symptoms than the comparison group. Parents of children with developmental problems showed poorer psychological well-being than the comparison group, but parents of children with mental health problems were not significantly different from the comparison group with respect to psychological well-being.
TABLE 2. Descriptive Statistics.
| Comparison (N = 1,393) | DP (N = 162) | MHP (N = 133) | ||||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | |
| 2a. Three group comparison | ||||||
| Dependent variables | ||||||
| Negative affect | 8.83 | 3.29 | 10.20 | 4.32 | 10.03 | 4.08***a,b |
| Psychological well-being | 231.50 | 34.77 | 224.38 | 38.01 | 226.08 | 38.49*a |
| Somatic symptoms | 3.53 | 2.04 | 4.18 | 2.08 | 4.19 | 2.18***a,b |
| Independent variables | ||||||
| Parent’s age (in years) | 56.17 | 12.97 | 53.79 | 12.30 | 58.73 | 11.69**a |
| Parent’s gender (1 = mother; 0 = father) | .48 | .60 | .67***a,b | |||
| Sociodemographic variables | ||||||
| Race (1 = non-Hispanic White; 0 = others) | .89 | .88 | .92 | |||
| Education (in years) | 14.39 | 2.66 | 14.04 | 2.86 | 14.33 | 2.92 |
| Income | 83130.99 | 66368.19 | 76550.18 | 54661.52 | 75861.24 | 52406.16 |
| Employment status (1 = employed; 0 = not employed) | .53 | .50 | .47 | |||
| Marital status (1 = married; 0 = not married) | .77 | .78 | .67*b | |||
| Number of children | 2.74 | 1.42 | 3.59 | 2.24 | 3.24 | 1.78***a,b |
| Number of co-resident children | .78 | 1.06 | 1.30 | 1.47 | .59 | .90***a |
| 2b. DP vs. MHP comparison | ||||||
| Respondent has more than one child with disability (1 = yes; 0 = no) | .09 | .14 | ||||
| Respondent co-resides with the target child (1 = yes; 0 = no) | .53 | .29*** | ||||
| Parent’s age at the onset of child’s disability (in years) | 32.51 | 7.93 | 44.80 | 8.78*** | ||
| Target child’s years with disability (in years) | 21.29 | 14.25 | 13.93 | 9.79*** | ||
| Age of the target child | 25.79 | 13.10 | 32.02 | 12.34*** | ||
| Gender of the target child (1 = daughter; 0 = son) | .34 | .52** | ||||
p ≤ .05
p ≤ .01
p ≤ .001
Notes: DP refers to parents of a child with developmental problems; MHP refers to parents of a child with mental health problems. Standard deviations are omitted for dichotomous variables. ANOVA F-tests were used to assess significant differences between means across three groups. Chi-square statistics were used to assess significant differences between proportions. Post-hoc test results are noted next to F-test results.
a significant difference between the comparison and the DP group (at the .05 level).
indicates a significant difference between the comparison and the MHP group (at the .05 level).
The mean age of parents and the proportion of women also significantly differed across the three groups. Post-hoc analyses showed that, on average, parents of children with developmental problems were several years younger than the parents in the comparison group, whereas the average age was similar between parents of children with a mental health problem and the comparison group. The proportion of mothers was higher than fathers in both the developmental problems and mental health problems groups, whereas the proportion of mothers and fathers was nearly equal in the comparison group.
The three groups did not differ in race, level of education, income, or employment status. However, the groups differed significantly in the proportion who were currently married, the number of children, and the number of coresident children. Post-hoc comparisons showed that parents of children with mental health problems were significantly less likely to be married than parents in the comparison group, but parents of children with developmental problems did not significantly differ from parents in the comparison group in marital status. Both parents of children with developmental problems and parents of children with mental health problems had more children than parents in the comparison group. Parents of children with developmental problems had a significantly greater number of co-residing children than parents in the comparison group, but there was no significant difference in the number of co-resident children between parents of children with mental health problems and parents in the comparison group.
Table 2 (panel b) presents differences between parents of children with developmental problems and parents of children with mental health problems on disability-related variables. Although the two groups did not differ significantly with respect to the likelihood of having more than one child with a disability, a significantly greater number of parents of children with developmental problems co-resided with their son or daughter with the disability than did parents of children with mental health problems. Parents of children with mental health problems experienced the onset of the child’s disability at a later age than parents of children with developmental problems, consistent with the later onset of mental health problems versus developmental problems. For this reason, children with developmental problems had a significantly longer mean duration of disability than children with mental health problems. On average, children with developmental problems were younger at MIDUS II (26 versus 32 years of age) and more likely to be male than children with mental health problems.
Effects of Having a Child with a Developmental or Mental Health Problem: Age and Gender Differences
Next, we examined the effects of having a child with a developmental problem or a mental health problem on parents’ well-being relative to the comparison group, and investigated the extent to which these effects differ by age and gender. The results are shown in Table 3. We used hierarchical regression models to examine the main effects of having a child with a developmental or a mental health problem (model 1), the moderating effects of age (model 2), and the moderating effects of gender (model 3).
TABLE 3. Effect of Having a Child with Developmental or Mental Health Problems on Well-Being.
| Negative affect | Psychological Well-Being | Physical Symptoms | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 1 | Model 2 | Model 3 | Model 1 | Model 2 | Model 3 | |
| Independent variables | |||||||||
| Target child has a DP condition | .09*** | .08*** | .05 | −.04† | −.03 | −.01 | .08** | .08** | .08* |
| Target child has a MHP condition | .09*** | .10*** | .10** | −.04† | −.05* | −.03 | .06** | .08** | .07† |
| Parent’s age (standardized) | −.14*** | −.11** | −.14*** | .02 | −.01 | .02 | −.02 | .01 | −.02 |
| Parent’s gender (1 = mother; 0 = father) | .05* | .06* | .05† | .00 | .00 | .01 | .11*** | .12*** | .12*** |
| Interaction effects | |||||||||
| DP condition × parental age | −.05* | .06* | .00 | ||||||
| MHP condition × parental age | −.06* | .05* | −.09** | ||||||
| DP condition × parental gender | .05 | −.04 | .00 | ||||||
| MHP condition × parental gender | −.01 | −.01 | −.02 | ||||||
| Sociodemographic variables | |||||||||
| Race (1 = non-Hispanic white; 0 = others) | −.04† | −.05† | −.04† | −.01 | .00 | .00 | .00 | −.01 | .00 |
| Education (in years) | −.11*** | −.11*** | −.11*** | .18*** | .18*** | .18*** | −.13*** | −.13*** | −.13*** |
| Income | −.07** | −.07** | −.07** | .05† | .05† | .05† | −.07** | −.07** | −.07** |
| Employment status (1 = employed; 0 = not employed) | −.10*** | −.10*** | −.10*** | .06* | .05† | .05* | .02 | .02 | .02 |
| Marital status (1 = married; 0 = not married) | −.07** | −.07** | −.07** | .10*** | .10*** | .10*** | .03 | .03 | .03 |
| Number of children | −.01 | −.01 | −.01 | .07** | .07** | .07** | .06* | .06* | .06* |
| Number of co-resident children | .07* | .07* | .08* | −.14*** | −.14*** | −.14*** | −.09** | −.08** | −.09 |
| N | 1655 | 1655 | 1655 | 1679 | 1679 | 1679 | 1675 | 1675 | 1675 |
| Adjusted R2 | .08 | .08 | .08 | .07 | .07 | .07 | .06 | .07 | .06 |
Notes: DP refers to developmental problems; MHP refers to mental health problems. Standardized coefficients are presented.
p ≤ .10
p ≤ .05
p ≤ .01
p ≤ .001 (two-tailed)
Main effects of parenting a child with a developmental or a mental health problem
Model 1 shows that, controlling for sociodemographic characteristics, parents of a child with developmental problems and parents of a child with a mental health problem show significantly higher levels of negative affect, marginally poorer psychological well-being, and significantly more somatic symptoms than the comparison group (see the coefficients for “target child has a DP condition” and “target child has a MHP condition”). Thus, the uncontrolled group differences between parents of children with disabilities and the comparison group that were reported in Table 2 were fully confirmed in these regression analyses, even with potentially confounding sociodemographic characteristics controlled. These main effects of having a disabled child are supportive of our first hypothesis.
Age differences
Model 2 shows the interaction effect of age in predicting the effects of having a child with either developmental or mental health problems on parents’ well-being. We found significant age by condition interaction effects for negative affect and psychological well-being for parents of children with developmental problems. The significant interaction terms indicate that, although parents of children with developmental problems have more negative affect and poorer well-being than the comparison group, these effects attenuate with age. Younger parents of children with developmental problems are more divergent than older parents from the comparison group with respect to negative affect and psychological well-being. This pattern is consistent with our second hypothesis predicting a narrowing of the well-being gap with advancing age.
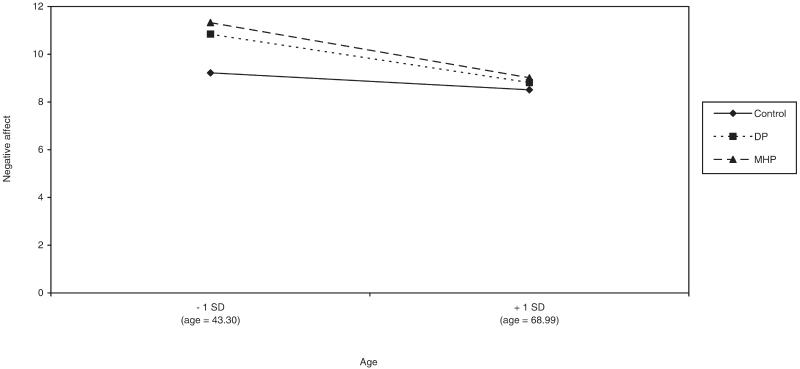
For parents of children with mental health problems, the moderating effects of age were significant for all three outcome variables. Although parents of children with mental health problems have more negative affect, poorer well-being, and more somatic symptoms than the comparison group, these effects attenuate significantly with age, similar to the findings for parents of children with developmental problems and consistent with our second hypothesis. Figure 1 shows the form of the interaction effects between conditions and age, predicting levels of negative affect. All significant interactions show the same pattern.
FIGURE 1. Age Differences in the Effects on Negative Affect of Having a Child with Developmental or Mental Health Problems.
Gender differences
Model 3 presents the data regarding whether the effects of developmental or mental health problems differ by gender. Counter to our third hypothesis, we did not find any significant gender differences in the effect of parenting a child with a developmental problem or a mental health problem. However, consistent with previous research (Mroczek and Kolarz 1998), gender had significant main effects on negative affect and somatic symptoms, suggesting that gender differences in physical and mental well-being exist for both parents of disabled children and the comparison group. Women showed higher negative affect and a greater number of somatic symptoms than men, but these patterns were no more pronounced for parents of disabled children than the comparison group.
Factors Predicting Well-Being among Parents of Disabled Children
Table 4 presents a within-group analysis of predictors of well-being among parents of children with developmental or mental health problems. We examined the effects of four disability-related variables (parent’s age at the onset of the child’s disability, duration of the child’s disability, number of children with disability, and co-residence status of the target child) as well as other sociodemographic variables, separately for parents of children with developmental problems and parents of children with mental health problems, in order to investigate disability-specific predictors of well-being for these parents.
TABLE 4. Predictors of Well-Being among Parents of Children with a Developmental or Mental Health Problem.
| Parents of Children with DP |
Parents of Children with MHP |
|||||
|---|---|---|---|---|---|---|
| Negative affect |
Psychological Well-Being |
Somatic Symptoms |
Negative Negative affect |
Psychological Well-Being |
Somatic Symptoms |
|
| Disability-related variable | ||||||
| Parent’s age at the onset of child’s disability (in years) | −.26** | .15† | −.03 | −.25** | .17† | −.30** |
| Target child’s duration of disability (in years) | −.39*** | .37*** | −.01 | −.30** | .21* | −.33** |
| Respondent has more than one child with disability (1 = yes; 0 = no) | .16* | −.11 | .16† | .19* | −.12 | .03 |
| Respondent co-resides with the target child (1 = yes; 0 = no) | .04 | −.07 | −.11 | .09 | −.11 | −.19† |
| Sociodemographic variables | ||||||
| Parent’s gender (1 = mother; 0 = father) | .05 | .01 | .07 | −.02 | .04 | .10 |
| Race (1 = non-Hispanic white; 0 = others) | −.14† | .14† | −.05 | .03 | .07 | .09 |
| Education (in years) | −.13 | .11 | −.14† | −.10 | .18† | −.07 |
| Income | −.08 | .17† | −.07 | .03 | −.11 | −.01 |
| Work status (1 = employed; 0 = not employed) | −.18* | .17* | .00 | −.34*** | .21* | −.11 |
| Marital status (1 = married; 0 = not married) | −.21* | .17† | −.06 | .00 | .12 | .18† |
| N | 152 | 154 | 152 | 118 | 120 | 119 |
| Adjusted R2 | .18 | .17 | .03 | .19 | .10 | .09 |
Notes: DP refers to developmental problems; MHP refers to mental health problems. Standardized coefficients are presented.
p ≤ .10
p ≤ .05
p ≤ .01
p ≤ .001
Parents of children with developmental problems
Regarding disability-related variables, both the parent’s age at the onset of child’s disability and the duration of disability were significantly related to the dependent variables. Consistent with the maturity hypothesis (H4), parents who were older when their child was diagnosed with a developmental problem reported lower levels of negative affect and marginally better psychological well-being than those who were younger at the age of their child’s diagnosis. Furthermore, consistent with the adaptation hypothesis (H5), those who had children with a longer duration of disability showed lower levels of negative affect and better psychological well-being than those with a shorter duration of disability, net of parental age at the onset of child’s disability. Consistent with our last hypothesis (H6), having more than one child with a disability was associated with significantly higher levels of negative affect and marginally greater somatic symptoms for parents of children with developmental problems. Counter to our hypothesis, co-residing with the child with developmental problems was not predictive of any outcome variable.
Among sociodemographic variables, consistent with previous research (Campbell, Converse, and Rodgers 1976), race, education, and income had marginally significant effects on some well-being indicators. Being currently employed and married predicted significantly lower levels of negative affect and better psychological well-being for parents of children with developmental problems.
Parents of children with mental health problems
Similar to the results for the parents of children with developmental problems and consistent with our hypotheses, parents who were older at the onset of their child’s disability and parents who had children with longer duration of disability reported lower levels of negative affect, better psychological well-being, and fewer somatic symptoms. Parents of children with mental health problems who had more than one child with a disability showed greater levels of negative affect than those who had only one such child. Surprisingly, parents who co-reside with a child with mental health problems reported marginally lower levels of somatic symptoms.
For parents of children with mental health problems, those who are better educated report marginally higher psychological well-being. Parents who were employed reported significantly lower levels of negative affect and better psychological well-being, whereas parents who were married showed a marginally greater number of somatic symptoms. Other than these effects, sociodemographic factors were not predictive of the well-being of parents of children with mental health problems.
DISCUSSION
Using a probability sample of men and women across a 50-year age range, we investigated age and gender differences in the effect of having disabled children on parental well-being. Our analyses yielded four major findings.
First, consistent with our first hypothesis, findings from multivariate analyses showed that parents of children with developmental or mental health problems experienced significantly higher levels of negative affect, marginally poorer well-being, and more somatic symptoms than parents without children with disabilities. Thus, our findings based on a national probability sample of midlife to older adults strengthen the findings from previous research that having children with disabilities takes a toll on parents’ mental and physical health. However, it is worth noting that, although parents of children with disabilities differ significantly from the comparison group, this difference accounts for a relatively small proportion of the variance in the well-being outcomes. This finding highlights the fact that having a disabled child is only one factor among many that affect parental well-being.
Second, older parents of disabled children did not diverge as much from the comparison group as younger parents did in their levels of negative affect and psychological well-being, supporting our hypothesis that the impact of parenting a disabled child attenuates in old age (H2). Furthermore, our analyses revealed that parental age at the diagnosis of the child’s disability and the duration of the disability were both important predictors of well-being of parents of disabled children, supporting both the maturity and the adaptation hypotheses (H4 and H5).
Third, contrary to our third hypothesis, yet consistent with some previous studies (Essex and Seltzer 1999), the analysis showed that the effect of having a disabled child did not differ by gender, suggesting that having children with developmental or mental health problems is equally stressful for both mothers and fathers. Several reasons may explain the lack of significant interaction between gender and the effect of having a disabled child on parental well-being, despite evidence in prior literature that women report greater caregiving burden than men (Heller et al. 1997; Pruchno and Patrick 1999). It may be that, even though they perceive greater burden than fathers, mothers may reap greater emotional gratification and satisfaction from caregiving than men (Pruchno and Patrick 1999), which may reduce psychological distress and enhance well-being. Mothers may also have access to greater informal social support (Antonucci 1990), which may buffer the stress of being a caregiver. Future studies should explore possible underlying mechanisms that produce differences or similarities in psychological and physical outcomes of caregiving mothers and fathers.
Finally, our study showed that, among sociodemographic factors, parental work status was the most prominent predictor of well-being. Parents who were employed showed lower levels of negative affect and higher levels of psychological well-being, both for parents of children with developmental problems and for parents of children with mental health problems, suggesting that taking a break from caregiving tasks and engaging in other activities may protect parents from experiencing acute distress.
Among parents of children with developmental problems, non-Hispanic white parents experience marginally lower levels of negative affect and significantly higher levels of psychological well-being than parents of different races or ethnicities. This finding is consistent with some prior research, which indicated that Hispanic mothers of children with mental retardation were significantly more depressed than non-Hispanic white mothers (Magana, Seltzer, and Krauss 2004; Magana et al. 2002). However, it is inconsistent with other research, which found no significant differences in well-being between black and white mothers of children with mental retardation (Pruchno, Patrick, and Burant 1997). Given that our analytic sample consists predominantly (about 85%) of non-Hispanic white parents, with different racial-ethnic minorities accounting for only a small proportion of the sample, we will need further study using more diverse samples in order to examine the racial-ethnic differences in the effect of having children with disabilities.
Limitations
Our study has three limitations that deserve mention. First, the cross-sectional design of this study is an important limitation, as age effects may be confounded with cohort effects. That is, people in different age groups belong to different birth cohorts, and these cohort differences, rather than age differences, may be leading to the differences in the outcome measures. Furthermore, with cross-sectional data we cannot examine within-person changes over time. Thus, we should be cautious about interpreting age differences as aging effects.
Second, although our finding of a non-significant effect of the disabled child’s co-residence on parental well-being suggests that the burden of daily care is not the chief source of distress among parents, because MIDUS did not have direct measures of caregiving, we were not able to investigate precisely whether the differences between parents of children with disabilities and parents of non-disabled children are attributable to the actual provision of care or to the more general effects of having a child with disability. The well-being of parents of children with disabilities may be compromised by various sources, such as time burden associated with managing the condition, self-concept issues associated with self-blame, stress associated with child behavioral problems, anxiety about the future, and feelings of loss associated with prior aspirations for children. With more specific measures of caregiving (e.g., hours and intensity of care), child’s characteristics, and parents’ expectations of the disabled child, we may be able to better understand the mechanisms by which having a disabled child affects the well-being of parents.
Finally, MIDUS did not specifically assess the severity of the disability conditions, and thus we were not able to examine how the severity of the disability affects parents’ well-being. Furthermore, because some diagnostic categories were small in size, we were not able to examine separately the impact of different types of developmental and mental health problems. Future studies should use more refined measures to investigate differential effects of various disabilities and the extent to which severity of the disability affects parental stress.
In conclusion, this is the first study to use a nationally representative sample and a comparison group to systematically examine the variability in the effect of having children with developmental or mental health problems on parental well-being. We have benchmarked the absolute toll taken by long-term parental caregiving in multiple domains of well-being, and we have highlighted the positive effects of parental maturity and adaptation over time to the caregiving role. Although stress effects appear to attenuate with age, ultimately longitudinal studies are needed to confirm these patterns. Future studies should build upon this one by examining how other factors that are known to explain differences in caregiving burden in the general population—such as caregiver socioeconomic status, race, health characteristics, social support, and community resources (Dilworth-Anderson, Goodwin, and Williams 2004; Martin and Sörensen 2005)—influence the extent to which caring for disabled children affects parents’ physical and mental health.
Biography
Jung-Hwa Ha conducted this research when she was a post-doctoral researcher at the Waisman Center, University of Wisconsin-Madison. She is now an assistant professor of social work at the University of Chicago. Her research examines the impact of life stress on older adults’ well-being and social relationships.
Jinkuk Hong is an associate researcher at the Waisman Center, University of Wisconsin-Madison. His research examines the effects of multiple roles and caregiving on the well-being of older adults.
Marsha M. Seltzer is a professor in the School of Social Work and the director of the Waisman Center at the University of Wisconsin-Madison. Her research examines the life course impacts of disability on the family.
Jan S. Greenberg is a professor in the School of Social Work at the University of Wisconsin-Madison. His research examines the challenges faced by families of persons with severe and persistent mental illness.
Footnotes
This research was supported by National Institute on Aging grant P01-AG020166 to conduct a longitudinal follow-up of the MIDUS (Midlife in the United States) investigation. The original study was supported by the John D. and Catherine T. MacArthur Foundation Research Network on Successful Midlife Development. Support was also provided by grant P30 HD03352 from the Waisman Center at the University of Wisconsin-Madison.
REFERENCES
- Antonucci Tony C. Social Supports and Social Relationships. In: Binstock RH, George LK, editors. Handbook of Aging and the Social Sciences. Academic Press; San Diego, CA: 1990. pp. 205–226. [Google Scholar]
- Baker Bruce L., Heller Tracy L. Preschool Children with Externalizing Behaviors: Experience of Fathers and Mothers. Journal of Abnormal Child Psychology. 1996;24:513–32. doi: 10.1007/BF01441572. [DOI] [PubMed] [Google Scholar]
- Barusch AS, Spaid WM. Gender Differences in Caregiving: Why Do Wives Report Greater Burden? The Gerontologist. 1989;29:667–76. doi: 10.1093/geront/29.5.667. [DOI] [PubMed] [Google Scholar]
- Brim Orville Gilbert, Ryff Carol D., Kessler Ronald C. How Healthy Are We? A National Study of Well-Being at Midlife. University of Chicago Press; Chicago, IL: 2004. [Google Scholar]
- Campbell A, Converse PE, Rodgers WL. The Quality of American Life. Russell Sage Foundation; New York: 1976. [Google Scholar]
- Carstensen Laura, Charles Susan T. Emotions in the Second Half of Life. Current Directions in Psychological Science. 1998;7:144–49. [Google Scholar]
- Clark Robin E., Drake Robert E. Expenditures of Time and Money by Families of People with Severe Mental Illness and Substance Use Disorders. Community Mental Health Journal. 1994;30:145–63. doi: 10.1007/BF02188626. [DOI] [PubMed] [Google Scholar]
- Cook Judith A., Lefley Harriet P., Pickett Susan A., Cohler Bertram J. Age and Family Burden among Parents of Offspring with Severe Mental Illness. American Journal of Orthopsychiatry. 1994;64:435–47. doi: 10.1037/h0079535. [DOI] [PubMed] [Google Scholar]
- Dilworth-Anderson Peggye, Goodwin Paula Y., Williams Sharon Wallace. Can Culture Help Explain the Physical Health Effects of Caregiving over Time among African American Caregivers? Journal of Gerontology: Social Sciences. 2004;59B:S138–S145. doi: 10.1093/geronb/59.3.s138. [DOI] [PubMed] [Google Scholar]
- Draper BM, Poulos CJ, Cole AD, Poulos RG, Ehrlich F. A Comparison of Caregivers for Elderly Stroke and Dementia Victims. Journal of the American Geriatrics Society. 1992;40:896–901. doi: 10.1111/j.1532-5415.1992.tb01986.x. [DOI] [PubMed] [Google Scholar]
- Drentea Patricia. Work Activity Characteristics across the Life Course. Advances in Life Course Research. 2005;9:303–29. [Google Scholar]
- Dura JR, Stukenberg KW, Kiecolt-Glaser JK. Spousal Caregivers of Persons with Alzheimer’s and Parkinson’s Disease Dementia: A Preliminary Comparison. The Gerontologist. 1991;30:332–36. doi: 10.1093/geront/30.3.332. [DOI] [PubMed] [Google Scholar]
- Essex Elizabeth Lehr, Seltzer Marsha M. Differences in Coping Effectiveness and Well-Being among Aging Mothers and Fathers of Adults with Mental Retardation. American Journal of Mental Retardation. 1999;104:545–63. doi: 10.1352/0895-8017(1999)104<0545:DICEAW>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- George L. Caregiver Well-Being: Correlates and Relationships with Participation in Community Self-Help Groups. Duke University Medical Center; Durham, NC: 1983. [Google Scholar]
- Greenberg Jan S. The Role of Fathers in the Lives of Their Sons and Daughters with Mental Illness. In: Kramer BJ, Thompson EH, editors. Men as Caregivers: Theory, Research, and Service Implications. Springer Publications; New York: 2002. pp. 269–93. [Google Scholar]
- Greenberg Jan S, Seltzer Marsha Mailick, Greenley James R. Aging Parents of Adults with Disabilities: The Gratifications and Frustrations of Later-Life Caregiving. The Gerontologist. 1993;33:542–50. doi: 10.1093/geront/33.4.542. [DOI] [PubMed] [Google Scholar]
- Greenberg Jan S., Seltzer Marsha M., Krauss Marty W., Chou Rita, Hong Jinkuk. The Effect of Quality of the Relationship between Mothers and Adult Children with Schizophrenia, Autism, or Down Syndrome on Maternal Well-Being: The Mediating Role of Optimism. American Journal of Orthopsychiatry. 2004;74:14–25. doi: 10.1037/0002-9432.74.1.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heller Tamar, Hsieh Kelly, Rowitz Louis. Maternal and Paternal Caregiving of Persons with Mental Retardation across the Lifespan. Family Relations. 1997;46:407–15. [Google Scholar]
- Hoyert Donna L., Seltzer Marsha M. Factors Related to the Well-Being and Life Activities of Family Caregivers. Family Relations. 1992;41:74–81. [Google Scholar]
- Kling Kristen C., Seltzer Marsha M., Ryff Carol D. Distinctive Late-Life Challenges: Implications for Coping and Well-Being. 1997;12:288–95. doi: 10.1037//0882-7974.12.2.288. [DOI] [PubMed] [Google Scholar]
- Lawton M. Powell, Kleban Morton H., Dean Jennifer. Affect and Age: Cross-Sectional Comparisons of Structure and Prevalence. Psychology and Aging. 1993;8:165–75. doi: 10.1037//0882-7974.8.2.165. [DOI] [PubMed] [Google Scholar]
- Lazarus R, Folkman S. Stress, Appraisal, and Coping. Free Press; New York: 1984. [Google Scholar]
- Lecavalier L, Leone S, Wiltz J. The Impact of Behaviour Problems on Caregiver Stress in Young People with Autism Spectrum Disorders. Journal of Intellectual Disability Research. 2006;50:172–83. doi: 10.1111/j.1365-2788.2005.00732.x. [DOI] [PubMed] [Google Scholar]
- Magana SM, Ramirez Garcia JI, Hernandez M, Cortez R. Psychological Burden among Latino Family Caregivers of Adults with Schizophrenia: The Roles of Burden and Stigma in the Stress-Process Model. Psychiatric Services. 2007;58:378–84. doi: 10.1176/appi.ps.58.3.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magana Sandra, Seltzer Marsha M., Krauss Marthy W. Cultural Context of Caregiving: Differences in Depression between Puerto Rican and Non-Latina White Mothers of Adults with Mental Retardation. Mental Retardation. 2004;42:1–11. doi: 10.1352/0047-6765(2004)42<1:CCOCDI>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Magana Sandra, Seltzer Marsha M., Krauss Marthy W., Rubert Mark P., Szapocznik Jose. Well-Being and Family Role Strains among Cuban American and Puerto Rican Mothers of Adults with Mental Retardation. Journal of Human Behavior in the Social Environment. 2002;5:31–55. [Google Scholar]
- Martin Pinquart, Sörensen Silvia. Ethnic Differences in Stressors, Resources, and Psychological Outcomes of Family Caregiving: A Meta-Analysis. The Gerontologist. 2005;45:90–106. doi: 10.1093/geront/45.1.90. [DOI] [PubMed] [Google Scholar]
- Miller Baila, Cafasso Lynda. Gender Differences in Caregiving: Fact or Artifact. The Gerontologist. 1992;32:498–507. doi: 10.1093/geront/32.4.498. [DOI] [PubMed] [Google Scholar]
- Miltiades Helen B., Pruchno Rachel. Mothers of Adults with Developmental Disability: Change over Time. American Journal on Mental Retardation. 2001;106:548–61. doi: 10.1352/0895-8017(2001)106<0548:MOAWDD>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Mirowsky John, Ross Catherine E. Age and Depression. Journal of Health and Social Behavior. 1992;33:187–205. [PubMed] [Google Scholar]
- Mroczek Daniel K., Kolarz Christian M. The Effect of Age on Positive and Negative Affect: A Developmental Perspective on Happiness. Journal of Personality and Social Psychology. 1998;75:1333–49. doi: 10.1037//0022-3514.75.5.1333. [DOI] [PubMed] [Google Scholar]
- Neundorfer M. Coping and Health Outcomes in Spouse Caregivers of Persons with Dementia. Nursing Research. 1991;40:260–65. [PubMed] [Google Scholar]
- Noh S, Avison WR. Spouses of Discharged Psychiatric Patients: Factors Associated with Their Experience of Burden. Journal of Marriage and the Family. 1988;50:377–89. [Google Scholar]
- Orsmond Gael I., Lin Ling-Yi, Seltzer Marsha M. Mothers of Adolescents and Adults with Autism: Parenting Multiple Children with Disabilities. Journal of Intellectual and Developmental Disabilities. 2007;45:257–270. doi: 10.1352/1934-9556(2007)45[257:MOAAAW]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Parks SH, Pilisuk M. Caregiving Burden: Gender and the Psychological Costs of Caregiving. American Journal of Orthopsychiatry. 1991;61:501–09. doi: 10.1037/h0079290. [DOI] [PubMed] [Google Scholar]
- Pinquart Martin, Sörensen Silvia. Gender Differences in Caregiver Experiences: An Updated Meta-Analysis. Journal of Gerontology: Psychological Sciences. 2006;61B:P33–P45. doi: 10.1093/geronb/61.1.p33. [DOI] [PubMed] [Google Scholar]
- Pruchno Rachel, Patrick Julie H. Mothers and Fathers of Adults with Chronic Disabilities: Caregiving Appraisals and Well-Being. Research on Aging. 1999;21:682–713. [Google Scholar]
- Pruchno Rachel, Patrick Julie Hicks, Burant Christopher J. African American and White Mothers of Adults with Chronic Disabilities: Caregiving Burden and Satisfaction. Family Relations. 1997;46:335–46. [Google Scholar]
- Reinhard SC, Horwitz AV. Caregiver Burden: Differentiating the Content and Consequences of Family Caregiving. Journal of Marriage and Family. 1995;57:741–50. [Google Scholar]
- Ross Catherine E., Van Willigen Marieke. Gender, Parenthood, and Anger. Journal of Marriage and the Family. 1996;58:572–84. [Google Scholar]
- Russo J, Vitaliano Peter P, Brewer DD, Katon W, Becker J. Psychiatric Disorders in Spouse Caregivers of Care Recipients with Alzheimer’s Disease and Match Controls: A Diathesis-Stress Model of Psychopathology. Journal of Abnormal Psychology. 1995;104:197–204. doi: 10.1037//0021-843x.104.1.197. [DOI] [PubMed] [Google Scholar]
- Ryff Carol D., Keyes Corey Lee M. The Structure of Psychological Well-Being Revisited. Journal of Personality and Social Psychology. 1995;69:719–27. doi: 10.1037//0022-3514.69.4.719. [DOI] [PubMed] [Google Scholar]
- Schulz R, Williamson GM. A 2-Year Longitudinal Study of Depression among Alzheimer’s Caregivers. Psychology and Aging. 1991;6:569–78. doi: 10.1037//0882-7974.6.4.569. [DOI] [PubMed] [Google Scholar]
- Seltzer Marsha M., Greenberg Jan S., Floyd Frank J., Hong Jinkuk. Accommodative Coping and Well-Being of Midlife Parents of Children with Mental Health Problems or Developmental Disabilities. American Journal of Orthopsychiatry. 2004;74:187–95. doi: 10.1037/0002-9432.74.2.187. [DOI] [PubMed] [Google Scholar]
- Seltzer Marsha M., Greenberg Jan S., Floyd Frank J., Pettee Yvette, Hong Jinkuk. Life Course Impacts of Parenting a Child with a Disability. American Journal of Mental Retardation. 2001;106:265–86. doi: 10.1352/0895-8017(2001)106<0265:LCIOPA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Seltzer Marsha M., Krauss Marthy W. Aging Parents with Coresident Adult Children: The Impact of Lifelong Caregiving. In: Seltzer MM, Krauss MW, Janicki MP, editors. Life Course Perspectives on Adulthood and Old Age. American Association on Mental Retardation; Washington, DC: 1994. pp. 3–18. [Google Scholar]
- Semple SJ. Conflict in Alzheimer’s Families: Its Dimensions and Consequences. The Gerontologist. 1992;32:648–55. doi: 10.1093/geront/32.5.648. [DOI] [PubMed] [Google Scholar]
- Singer George H. S. Meta-Analysis of Comparative Studies of Depression in Mothers of Children with and without Developmental Disabilities. American Journal on Mental Retardation. 2006;111:155–69. doi: 10.1352/0895-8017(2006)111[155:MOCSOD]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Sommer Kristen, Whitman Thomas L., Borkowski John G., Schellenbach Cynthia, Maxwell Scott, Keogh Deborah. Cognitive Readiness and Adolescent Parenting. Developmental Psychology. 1993;29:389–98. [Google Scholar]
- Townsend Aloen, Noelker Linda, Deimling Gary, Bass David. Longitudinal Impact of Interhousehold Caregiving on Adult Children’s Mental Health. Psychology and Aging. 1989;4:393–401. doi: 10.1037//0882-7974.4.4.393. [DOI] [PubMed] [Google Scholar]