Abstract
The heart failure illness trajectory is both complex and unpredictable, which makes providing palliative care services to patients with heart failure a challenge. As a result, although services are needed, few tend to be offered beyond basic medical management. The traditional model of palliative care is typically based on palliative care being considered a system of care delivery most appropriate for patients with a predictable illness/death trajectory, such a terminal cancer. This type of model, which is based on the ability to predict the course of a terminal disease, does not fit the heart failure trajectory. In this paper, we propose a new model of palliative care that conceptualizes palliative care as a philosophy of care that encompasses the unpredictable nature of heart failure.
Keywords: Palliative Care, Heart Failure, Illness Trajectories, Models
Introduction
Over the past 10 years the rates of death from heart disease have declined, yet it remains the leading cause of death in adults in the United States.(1) As treatment options improve for heart diseases, such as coronary heart disease and myocardial infarctions, individuals are living longer but many are developing subsequent heart problems, particularly heart failure. Consequently the incidence of heart failure is on the rise with over 5 million people in the United States living with the disease and ½ million new cases being added each year(1) Even with ever improving treatment options, in persons under age 65, 70-80% will die within 8 years of their heart failure diagnosis.(1) In addition, in those individuals who develop heart failure after an MI, 22% of males and 46% of females will be disabled from heart failure within six years.(1) Thus, although there are new medical and surgical treatment modalities for heart failure, patients still have irreversibly damaged hearts(2) and the decreased ability to perform up to their pre-heart failure level of functioning.
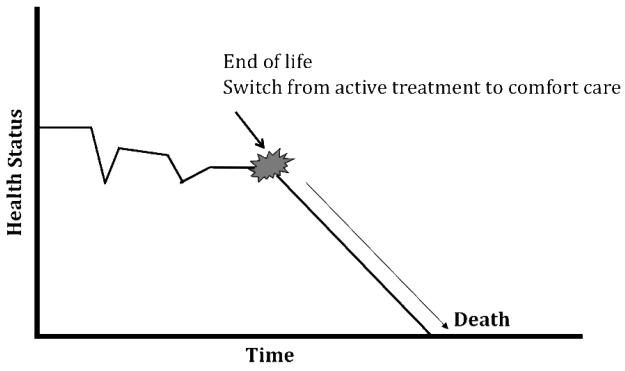
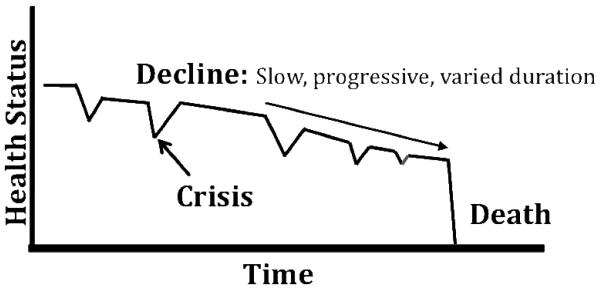
The course or illness trajectory of heart failure is complex. Although heart failure is typically characterized by acute crises or exacerbations followed by periods of stability lasting for months or even years, (see Model 1, adapted from Field and Cassel(3)) sudden death is also a possibility. In fact the risk of sudden death is 6 to 9 times that of the general population.(1) What makes the trajectory even more complex is the difficulty in predicting who is at-risk for sudden death and the lack of prognostic indicators to identify the terminal phase of the disease.(4, 5)
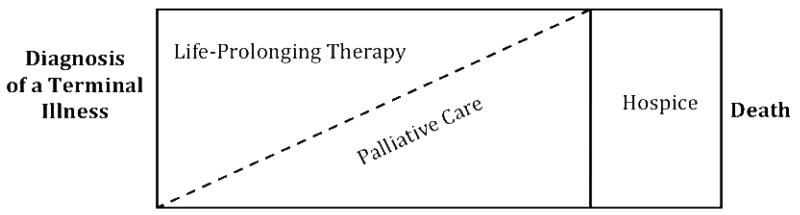
Compare the unpredictable trajectory of heart failure to the terminal trajectory of cancer. As depicted in Model 2,(3, 6) once cancer reaches the terminal phase, the slope of the trajectory shifts from a relatively stable course to one of rapid decline. At the same time, there is a marked change in the treatment plan from one of active treatment to comfort care or end-of-life care. With such a predictable change in course, patient and family needs can be anticipated and appropriate services provided. Since the heart failure trajectory is so unpredictable, the provision of services beyond medical management has been difficult and has been found to be severely lacking.(3, 7-9)
Palliative care interventions have been recommended as a means to meet the needs of patients throughout the heart failure trajectory.(10-12) These services are most salient for a person with heart failure, that is, someone who may not be ‘labeled’ as dying, but who needs comprehensive services concurrent with life-prolonging care throughout the illness/death trajectory.(13) However, <10% of patients with heart failure receive any palliative care services(7) and as of 2007, <12% of hospice admissions were patients with heart failure.(14) The purpose of this paper is to clarify the conceptualization of palliative care as both a philosophy and a system of care delivery. The accepted traditional model of palliative care is presented, and a new model of palliative care that would be appropriate for an individual living with and dying from heart failure is proposed.
Palliative Care
Palliative care has been defined as both a philosophy of care and a system of care delivery. As a philosophy of care, any and all healthcare providers who come into contact with the patient or family can provide supportive care interventions aimed at managing symptoms and other issues throughout the patient's illness trajectory. According to the National Consensus Project for the Quality Palliative Care (NCP), “Palliative care expands the traditional disease-model medical treatments to include the goals of enhancing quality of life for patient and family, optimizing function, helping with decision-making and providing opportunities for personal growth. As such, it can be delivered concurrently with life-prolonging care or as the main focus of care.”(15)
Contrast the above definition with the one espoused by the World Health Organization that specifies that a team or service provide palliative care, “Palliative care improves the quality of life of patients and families who face life-threatening illness, by providing pain and symptom relief, spiritual and psychosocial support from diagnosis to the end of life and bereavement… uses a team to approach [italics added] to address the needs of patients and their families.”(16) This type of approach or system of care delivery is usually provided by an interdisciplinary team, including medicine, nursing, social work, nutrition, chaplaincy and others to treat the complex needs of a person with a life-limiting illness.(15) When conceptualized as a particular medical service (team) or system of care delivery, most often requiring a referral or consultation, palliative care tends to be entangled solely with end-of-life care or hospice care.(17, 18) In addition, this conceptualization has caused many professionals to consider palliative care interventions to be in the realm of specialists.(19, 20)
As a philosophy of care for patients with heart failure, palliative care, when disentangled from end-of-life or hospice care, is a viable approach for integrating symptom management, the discussion of the life-limiting nature of the illness, advance planning, and psychosocial interventions together with optimal medical management much earlier in the course of the disease.(7) Heart failure experts agree that palliative care, as supportive interventions for both patients and families, should be integrated throughout the various stages of heart failure. Yet, research is needed to determine which patients will benefit most from different interventions; which interventions will improve quality of life; how to improve coordination of care among sites (e.g., inpatient and outpatient services, palliative care, hospice); and the best ways to communicate courses of treatment and prognosis to patients and families.(21)
Although there appears to be agreement that patients with heart failure would benefit from palliative care interventions, lack of knowledge among healthcare providers appears to be a barrier to the provision of these services.(11, 22-25) This lack of knowledge is twofold: primary care providers and cardiologists are often unsure of how to integrate palliative care services into their practice(24, 25) and palliative care specialists often lack the specialty knowledge required for heart failure management.(22, 24) In addition, some physicians interpret the introduction of palliative care as a path to death that should be only implemented for those patients who are actively dying.(11, 26, 27)
Models of Palliative Care
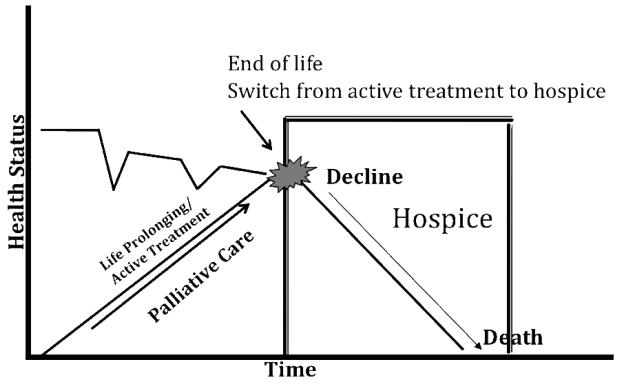
The model depicting the relationship between palliative care and life-prolonging therapies was originally developed in relationship to the somewhat predictable trajectory of cancer and other terminal illnesses. In a typical terminal cancer trajectory (see Figure 2), the patient has a steady decline, with a fairly short terminal phase. The shift from active treatment to comfort care is a sharp demarcation and death is usually the expected outcome of this progressive deterioration. The acknowledgement of the shift from curative care to comfort care allows appropriate end-of-life services to be provided for both patients and families. The generic model for palliative care as proposed by NCP(15) (see Figure 3) is appropriate for this type of predictable trajectory. This model balances a blend of life-prolonging therapy (active treatment) with palliative care through the majority of the trajectory. When life-prolonging treatment is a viable option, minimal palliative care interventions are introduced. Once life-prolonging therapy becomes less of an alternative, palliative care becomes the primary method of medical management and support for both patients and families. Finally, when the terminal phase of the illness is evident and life-prolonging treatments are no longer a feasible consideration, the patient converts to hospice care at the end of life.(15) This type of model would be most applicable for a patient with a disease trajectory that is rather well delineated and predictable. The application of this model for a terminal cancer trajectory is depicted in Figure 4. For this illness/death trajectory, as palliative care escalates, life-prolonging treatment begins to decrease until the predicted end-of-life phase begins. At this point, active curative treatment is stopped and hospice care becomes the focus of care until the patient dies.
Figure 2.
Terminal Cancer Trajectory*
*Adapted from Field & Cassel (1997) p. 29
Figure 3.
Traditional Model of Palliative Care*
Adapted from NCP (2004) p. 3
Figure 4.
Palliative Model: Terminal Cancer
In contrast, diseases such as heart failure, which are more unpredictable in nature do not fit the model. The National Consensus Project(15) recommends the initiation of palliative care interventions at the time of diagnosis of any serious life threatening illness in concert with active care, with the intensity of palliative care interventions based upon prognostic indicators. Thus as the person's health status deteriorates, palliative care interventions increase, while life-prolonging treatments slowly decrease. The problem with basing palliative care needs solely on prognosis for patients with non-malignant chronic illness, such as heart failure, is the risk of overlooking significant palliative care needs in these patients.(28, 29) These patients simply do not follow a predicted illness/death trajectory and there is a lack of clear prognostic indicators to identify the end of life.(5, 23, 30) In fact numerous studies have confirmed that physicians over estimate the mortality rate in their heart failure patients,(23, 31) while patients tend to over estimate their life expectancy.(32) Both scenarios make the traditional model of palliative care not only ineffective, but also impractical.
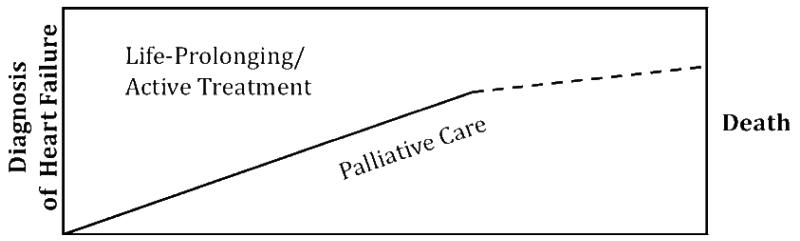
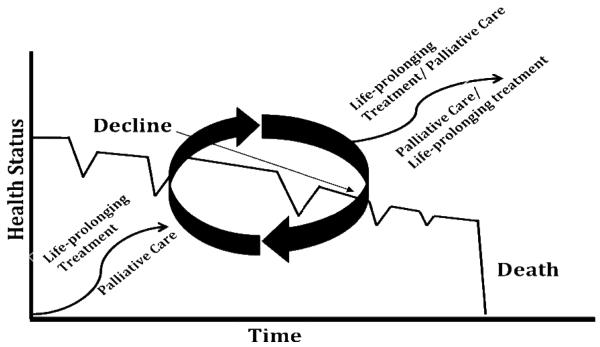
To address some of the issues with the generic model of palliative care, a new model of palliative care for heart failure was proposed by Hupcey and Penrod(33) (see figure 5). This model builds on the National Consensus Project's(15) original model; balancing life-prolonging therapies (active treatment) with palliative care throughout the illness trajectory. As the heart failure trajectory progresses, there is a gradual shift in dominance of palliative care as the patient's symptoms becomes increasingly refractory to medical management. The primary differences between the palliative care model presented by the National Consensus Project(15) and the palliative care model for heart failure is that active treatment continues throughout the trajectory and standard hospice services are not a part of the proposed model. The reason for this is three-fold: (a) death is often sudden in the heart failure population and otherwise not predictable, (b) heart failure patients usually seek life-prolonging (active therapy) treatment until their impending death, and (c) many life-prolonging therapies in heart failure are also palliative in nature.
Figure 5.
Proposed Model of Palliative Care: Heart Failure
Application of the proposed model of palliative care for heart failure
It is well known that the heart failure trajectory is markedly different from that of terminal cancer. Heart failure patients have multiple acute exacerbations (crises) and recuperations that occur across a longer, more chronic trajectory (see Figure 1) with a markedly different slope than terminal cancer. With each adverse event in heart failure (e.g., an exacerbation which results in a hospitalization), the patient re-compensates to a level perceptively “better” however, may not return back to the previous level of functioning. During the early phase of the heart failure trajectory, life-prolonging therapies are dominant in the comprehensive system of care (see Figure 5). Thus palliative care intervention may not be introduced as a system of care delivery, but should be integrated as a philosophy of care that undergirds the treatment of the patients and family. Ideally, palliative care interventions are introduced at the time of diagnosis. The patient is minimally supported with palliative care interventions as needed. Then, over time, as patients require sporadic intensive therapies such as diuresis, the intensity of palliative care interventions escalates, still in tandem with life-prolonging treatments (see Figure 6). Multiple exacerbations signal decompensation of cardiac function as the heart failure becomes increasingly life-threatening and functional status slowly declines. In this phase of the trajectory, palliative care interventions assume a more dominant position in the balance of care. However, in contrast to the NCP(15) model, life-prolonging therapies continue since the actual end-of-life phase is so unpredictable. More importantly, life prolonging and palliative therapies tend to overlap (as depicted by the circular phase interventions in the model). At this point active treatment is also palliative treatment. Discontinuing active medical treatment would result in greater pain and suffering for the patient and this treatment often continues until the patient's death.
Figure 1.
Typical Heart Failure Trajectory*
*Adapted from Field & Cassel (1997) p. 29
Figure 6.
Palliative Care: Heart Failure
The proposed model of palliative care for heart failure has implications for both patients and their families. Using this model as a means to conceptualize care delivery for patients with heart failure would diminish the emphasis on prognostication as a marker for offering palliative care interventions. Rather, palliative care interventions would be driven by assessed needs in a responsive dynamic flow of care. Those heart failure patients who live through a long protracted course and those patients who die a sudden death from heart failure would both have access to the benefits of palliative care. Thus for all patients there would be a potential for optimization of the quality of life from the time of diagnosis until death.
Conclusion
With the rise in prevalence of heart failure in the United States there is a compelling need to adopt a comprehensive model of palliative care for heart failure that is responsive to the ongoing challenges of living with an unpredictable chronic illness that is marked by a high death rate. The proposed model of palliative care for heart failure introduces the concepts of palliative care to patients and their families at the time of diagnosis and escalates in concert with exacerbations of illness or as triggered by patient needs. Underscoring the model is the conceptualization that palliative care is a philosophy of care and not solely a system of care delivery provided by an interdisciplinary team of experts. The overarching aim of the proposed model of palliative care as a philosophy of care for heart failure patients is to eliminate the disparities in the delivery of palliative care interventions to heart failure patients. Previously identified barriers to the introduction of palliative care interventions for heart failure patients could be overcome with an anticipatory palliative care model that is instituted at the time of diagnosis and includes careful coordination of services and clear, respectful communication with patients to promote quality of life despite the uncertainty of the trajectory.
Acknowledgments
This work was funded in part by:
NIH/National Institute of Nursing Research, 1 R15 NR009976-01 Hupcey, (PI) & Penrod, J. (Co-I) Comprehensive palliative care: Spousal caregivers of heart failure patients.
The American Heart Association, Pennsylvania/Delaware Affiliate, Grant-in-Aid program. Hupcey (PI), Penrod (Co-I) & Boehmer, J. (Co-I) Investigation of palliative care needs of elderly heart failure patients and their spousal caregivers.
Contributor Information
Judith E. Hupcey, School of Nursing, College of Medicine The Pennsylvania State University Hershey, PA, USA.
Janice Penrod, School of Nursing, College of Medicine The Pennsylvania State University University Park, PA, USA jlp198@psu.edu.
Kimberly Fenstermacher, School of Nursing The Pennsylvania State University Hershey, PA, USA kxf131@psu.edu.
References
- 1.American Heart Association Heart Disease and Stroke Statistics-2008 Update At-a-Glance. 2008 December 18; 2008. Available from: http://www.americanheart.org/downloadable/heart/1200078608862HS_Stats%202008.final.pdf.
- 2.Kirkpatrick JN, Kim AY. Ethical issues in heart failure: overview of an emerging need. Perspect Biol Med. 2006 Winter;49(1):1–9. doi: 10.1353/pbm.2006.0009. [DOI] [PubMed] [Google Scholar]
- 3.Field M, Cassel C. Approaching death Improving care at the end of life. Washington, D.C.: 1997. [PubMed] [Google Scholar]
- 4.Levenson JW, McCarthy EP, Lynn J, Davis RB, Phillips RS. The last six months of life for patients with congestive heart failure. J Am Geriatr Soc. 2000 May;48(5 Suppl):S101–9. doi: 10.1111/j.1532-5415.2000.tb03119.x. [DOI] [PubMed] [Google Scholar]
- 5.Zambroski CH. Managing beyond an uncertain illness trajectory: palliative care in advanced heart failure. Int J Palliat Nurs. 2006 Dec;12(12):566–73. doi: 10.12968/ijpn.2006.12.12.22543. [DOI] [PubMed] [Google Scholar]
- 6.Murray SA, Kendall M, Boyd K, Sheikh A. Illness trajectories and palliative care. BMJ. 2005;330:1007–11. doi: 10.1136/bmj.330.7498.1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pantilat SZ, Steimle AE. Palliative care for patients with heart failure. JAMA. 2004;291(20):2476–82. doi: 10.1001/jama.291.20.2476. [DOI] [PubMed] [Google Scholar]
- 8.Murray SA, Boyd K, Kendall M, Worth A, Benton TF, Clausen H. Dying of lung cancer or cardiac failure: Prospectie qualitative interview study of patients and their carers in the community. BMJ. 2002;325(26):1–5. doi: 10.1136/bmj.325.7370.929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Exley C, Field D, Jones L, Stokes T. Palliative care in the community for cancer and end-stage cardiorespiratory disease: the views of patients, lay-carers and health care professionals. Palliat Med. 2005 Jan;19(1):76–83. doi: 10.1191/0269216305pm973oa. [DOI] [PubMed] [Google Scholar]
- 10.Davidson P, Paull G, Rees D, Daly J, Cockburn J. Activities of home-based heart failure nurse specialists: a modified narrative analysis. Am J Crit Care. 2005 Sep;14(5):426–33. [PubMed] [Google Scholar]
- 11.Lewis C, Stephens B. Improving palliative care provision for patients with heart failure. Br J Nurs. 2005;14(10):563–7. doi: 10.12968/bjon.2005.14.10.18105. [DOI] [PubMed] [Google Scholar]
- 12.Lunder U, Sauter S, Furst C. Evidence-based palliative care: Beliefs and evidence for changing practice (Editorial) Palliat Med. 2004;18:265–6. doi: 10.1191/0269216304pm900ed. [DOI] [PubMed] [Google Scholar]
- 13.Zimmermann C, Rodin G. The denial of death thesis: Sociological critique and implications for palliative care. Palliat Med. 2004;18:121–8. doi: 10.1191/0269216304pm858oa. [DOI] [PubMed] [Google Scholar]
- 14.National Hospice and Palliative Care Organization NHPCO Facts and Figures: Hospice care in America 2008. Available from: http://www.nhpco.org/files/public/Statistics_Research/NHPCO_facts-and-figures_2008.pdf.
- 15.National Consensus Project for Quality Palliative Care Clinical Practice Guidelines for quality palliative care, executive summary. J Palliat Med. 2004 Oct;7(5):611–27. doi: 10.1089/jpm.2004.7.611. [DOI] [PubMed] [Google Scholar]
- 16.World Health Organization Palliative Care 2002. Available from: http://www.who.int/cancer/palliative/en/
- 17.Hupcey JE, Penrod J, Fogg J. Heart failure and palliative care: Implications in practice. doi: 10.1089/jpm.2009.0010. in review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.American Academy of Hospice and Palliative Care Medicine Statement on access to palliative care and hospice. 2008 December 18; 2008. Available from: >http://www.aahpm.org/positions/access.html.
- 19.Hibbert D, Hanratty B, May C, Mair F, Litva A, Capewell S. Negotiating palliative care expertise in the medical world. Social Science Medicine. 2003;57:277–88. doi: 10.1016/s0277-9536(02)00346-5. [DOI] [PubMed] [Google Scholar]
- 20.Selman L, Harding R, Beynon T, Hodson F, Coady E, Hazeldine C, et al. Improving end-of-life care for patiens with chronic heart failure: “Let's hope it'll get better, when I know in my heart of hearts it won't”. Heart. 2007;93:963–7. doi: 10.1136/hrt.2006.106518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Goodlin SJ, Hauptman PJ, Arnold R,KG, Hershberger RE, Kutner J, et al. Consensus statement: Palliative and supportive care in advanced heart failure. Journal of Cardiac Failure. 2004;10(3):200–9. doi: 10.1016/j.cardfail.2003.09.006. [DOI] [PubMed] [Google Scholar]
- 22.Gibbs LME, Khatri AK, Gibbs JSR. Survey of specialist palliative care and heart failure: September 2004. Palliative Medicine. 2006;20:603–9. doi: 10.1177/0269216306071063. [DOI] [PubMed] [Google Scholar]
- 23.Hanratty B, Hibbert D, Mair F, May C, Ward C, Capewell S, et al. Doctors' perceptions of palliative care for heart failure: Focus group study. BMJ. 2002;325:581–585. doi: 10.1136/bmj.325.7364.581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hanratty B, Hibbert D, Mair F, May C, Ward C, Corcoran G, et al. Doctor's understand of palliative care. Palliat Med. 2006;20:493–7. doi: 10.1191/0269216306pm1162oa. [DOI] [PubMed] [Google Scholar]
- 25.McIlfatrick S. Assessing palliative care needs: Views of patients, informal carers and healthcare professionals. J Ad Nsg. 2006;57(1):77–86. doi: 10.1111/j.1365-2648.2006.04062.x. [DOI] [PubMed] [Google Scholar]
- 26.Fitzsimons D, Mullan D, Wilson J, Chew E, Conway B, Corcoran B, et al. The palliative care needs of patients with heart failure from the perspective of the patient, carer, and clinical team. Eur J Cardiovasc Nurs. 2006;5:S35. [Google Scholar]
- 27.Fitzsimons D, Mullan D, Wilson JS, Conway B, Corcoran B, Dempster M, et al. The challenge of patients' unmet palliative care needs in the final stages of chronic illness. Palliat Med. 2007 Jun;21(4):313–22. doi: 10.1177/0269216307077711. [DOI] [PubMed] [Google Scholar]
- 28.Coventry PA, Grande GE, Richards DA, Todd CJ. Prediction of appropriate timing of palliative care for older adults with non-malignant life-threatening disease: a systematic review. Age Ageing. 2005 May;34(3):218–27. doi: 10.1093/ageing/afi054. [DOI] [PubMed] [Google Scholar]
- 29.Wotton K, Borbasi S, Redden M. When all else has failed Nurses' perception of factors influencing palliative care for patients with end-stage heart failure. Journal of Cardiovascular Nursing. 2005;20(1):18–25. doi: 10.1097/00005082-200501000-00006. [DOI] [PubMed] [Google Scholar]
- 30.Gott M, Barnes S, Parker C, Payne S, Seamark D, Gariballa S, et al. Dying trajectories in heart failure. Palliative Medicine. 2007;21:95–9. doi: 10.1177/0269216307076348. [DOI] [PubMed] [Google Scholar]
- 31.Muntwyler J, Abetel G, Gruner C, Follath F. One-year mortality among unselected outpatients with heart failure. Eur Heart J. 2002 Dec;23(23):1861–6. doi: 10.1053/euhj.2002.3282. [DOI] [PubMed] [Google Scholar]
- 32.Allen LA, Yager JE, Funk MJ, Levy WC, Tulsky JA, Bowers MT, et al. Discordance between patient-predicted and model-predicted life expectancy among ambulatory patients with heart failure. JAMA. 2008 Jun 4;299(21):2533–42. doi: 10.1001/jama.299.21.2533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hupcey JE, Penrod J. Living through the trajectory of heart failure: Palliative care needs of male patients and their spousal caregivers. Eastern Nurses Research Society; Providence, RI2007 [Google Scholar]