Abstract
Background and Objectives
Evidence suggests the importance of skin biophysical properties in predicting diseases and in developing appropriate skin care. The results to date of studies on skin surface pH, stratum corneum (SC) hydration and sebum content in both genders and at various ages have been inconclusive, which was in part due to small sample size. Additionally, little is known about the skin physical properties of Asian, especially Chinese, subjects. In the present study, we assess the difference in skin surface pH, sebum content and SC hydration at various ages and in both genders in a large Chinese population without skin diseases.
Methods
713 subjects (328 males and 385 females) aged 0.5–94 years were enrolled in this study. The subjects were divided by age into 5 groups, i.e., 0–12, 13–35, 36–50, 51–70 and over 70 years old. A multifunctional skin physiology monitor was used to measure SC hydration, skin surface pH and sebum content on both the forehead and the forearms.
Results
In males, the highest sebum content was found on the forearm and the forehead in the age groups 36–50 (93.47 ± 10.01 μg/cm2) and 51–70 years (9.16 ± 1.95 μg/cm2), while in females, the highest sebum content was found on the forearm and the forehead in the age groups 13–35 (61.91 ± 6.12 μg/cm2) and 51–70 years (7.54 ± 2.55 μg/cm2). The forehead sebum content was higher in males aged 13–70 years than in age-matched females; the sebum content on the forehead in both males and females was higher than that on the forearm. Skin surface pH on the forehead of both males and females over the age of 70 years was higher than that in younger groups. SC hydration on the forehead in both males and females was lower above the age of 70, and the one in males aged 13–35 was higher than that in females (43.99 ± 1.88 vs. 36.38 ± 1.67 AU, p < 0.01). SC hydration on the forehead in both males and females did not significantly differ from that on the forearm.
Conclusions
In a large Chinese cohort, the skin surface pH, sebum content and SC hydration vary with age, gender and body site.
Key Words: Age differences, Stratum corneum hydration, Skin surface pH, Sebum
Introduction
Much attention has been paid to skin biophysical properties, such as skin surface pH, stratum corneum (SC) hydration, sebum content and epidermal permeability barrier function, because these parameters can indicate not only skin condition, but also the systemic status of the human organism. For example, decreased SC hydration and altered permeability barrier function are associated with some skin disorders, such as atopic dermatitis, psoriasis and ichthyosis [1,2,3,4,5]. Malnutrition (such as essential fatty acid deficiency) [6, 7] and psychological stress also alter epidermal permeability barrier function [8,9,10,11]. Moreover, a higher skin surface pH and lower SC hydration are found in hemodialysis patients and subjects who recovered from leprosy [12,13,14,15]. Furthermore, skin surface pH and the gradient differ from normal in both X-linked recessive and autosomal dominant ichthyoses [16]. Additionally, both skin temperature and sebum content decrease significantly on the forehead of menopausal women, and SC hydration declines in postmenopausal women [17]. On the other hand, systemic administration of estrogen improves SC hydration, and topical estrogens improve skin elasticity and skin firmness, suggesting that hormones regulate the physical properties of the skin [18,19,20]. Development of many pharmaceutical and skin care products has relied upon what is known about these parameters. Finally, measurement of skin capacitance is used to evaluate the efficacy of skin care products in SC hydration, and transepidermal water loss has been used as one of the indicators to assess the therapeutic efficacy and clinical status of some skin disorders [21,22,23,24,25,26].
Likewise, with regard to the effects of aging and gender on skin physiology and despite a number of available publications, the results are inconclusive. For example, Marrakchi and Maibach [27] demonstrated that sebum content on the forehead in the aged (aged 66–83 years) is higher than in a younger cohort (aged 24–34 years), while no differences in sebum content between young and old subjects have been observed in another study [28]. In contrast, the sebum content is significantly higher in younger than in older subjects [29, 30]. Although skin surface pH is reportedly higher in females than in males [31, 32], a lower surface pH has also been reported in females [33, 34]. Regarding SC hydration, the results are also contradictory, which is largely due to the limited number of subjects studied. Furthermore, few data are available comparing skin physiology in prepubertal children with other developmental stages. Finally, most published data on skin physiology are from the studies in Caucasians. Thus, little is known about skin physiology in Asians, especially Chinese, whose skin could differ from that of Caucasians in some respects. It has been shown that the skin of older Caucasian women is drier than that of Chinese women [35]. In the present study, we measured the sebum content, skin surface pH and SC hydration on both sebum-enriched and sebum-impoverished sites in males and females aged 0.5–94 years in a large normal Chinese population.
Subjects and Methods
Subjects
A total of 713 volunteers, 328 males and 385 females aged 0.5–94 years, were enrolled in this study (table 1). All subjects had no systemic or skin disorders which could influence skin surface pH, hydration and sebum content at the study sites. According to their developmental stage, the subjects were divided into 5 age groups, i.e., 0–12 years old (prepuberty group), 13–35 (young group), 36–50 (middle age), 51–70 (old group) and over 70 years (older). No skin care products were applied to the measured sites 24 h prior to the measurement being taken, and the measured sites were not washed with soaps or surfactants for at least 12 h prior to the study.
Table 1.
Characteristic of subjects
| Age group |
Total | |||||
|---|---|---|---|---|---|---|
| 0–12 | 13–35 | 36–50 | 51–70 | over 70 | ||
| Males | 128 | 85 | 60 | 31 | 24 | 328 |
| Females | 142 | 102 | 82 | 28 | 31 | 385 |
| Total | 270 | 187 | 142 | 59 | 55 | 713 |
Measurements
All measurements were performed by dermatologists. Surface sebum content, SC hydration and skin surface pH were measured on the forehead and the forearm (flexor site) with respective probes (Sebum Cassette, Corneometer CM825 and pH 905) attached to a Courage & Khazaka MPA5 system [36, 37]. All subjects rested for at least 30 min at 22–24°C, at a relative humidity of 45–55%, prior to measurement. This work was performed between February and May (spring time) at the Dalian Skin Disease Hospital, which is at a latitude of 38°43′ to 40°10′ north. The study protocol was approved by the Human Research Committee of Dalian Skin Disease Hospital, The People's Republic of China.
Statistics
Graph Pad Prism 4 software was used for all statistical analyses. Notably, repeated-measures ANOVA could not be performed in this study, since the measurements in each group were not from the same individual, and the groups differed both in size and subject age [38]. Instead, a one-way ANOVA analysis, with Tukey correction, was used to determine significant differences, when 3 or more groups were compared, while an unpaired t test with Welch's correction was used for comparisons between 2 groups. Data were expressed as means ± SEM.
Results
Sebum Content Varies with Age, Gender and Body Sites
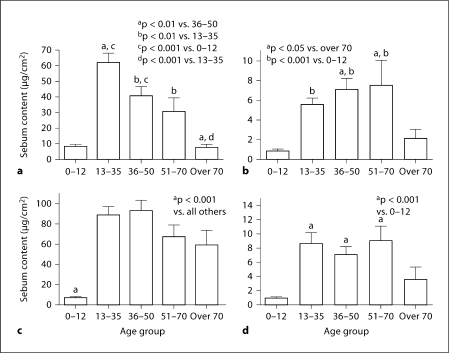
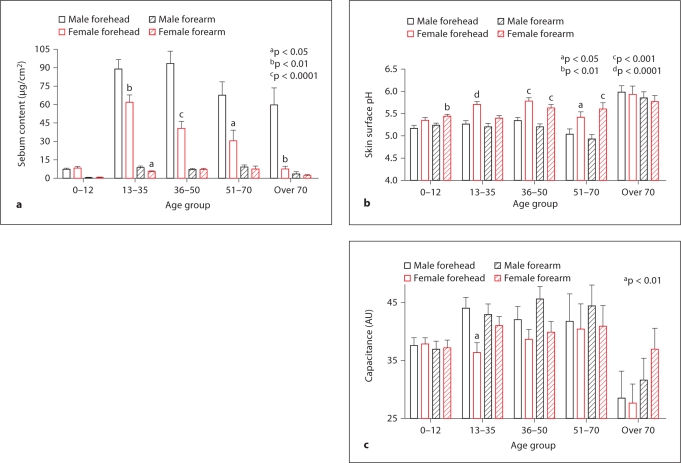
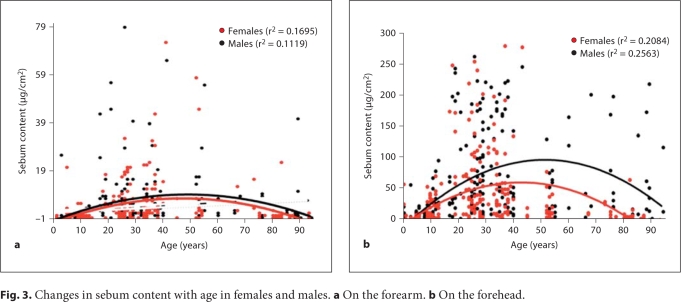
We first assessed the sebum content on a sebum-enriched site, the forehead, and a sebum-impoverished site, the forearm, in both males and females at various ages. In females aged 13–70 years, the sebum content on both the forehead and the forearm was significantly higher than that in females aged 0–12 years or over the age of 70 (fig. 1a, b). The sebum content on the forehead in males aged 0–12 years was significantly lower than that of males aged 13–70 years and over the age of 70 (fig. 1c); that on the forearm was significantly higher in males aged 13–70 than in those aged 0–12 (fig. 1d). There was no significant difference in sebum content on the forearm in males between the groups aged 0–12 and over 70 years. Overall, males tended to have a higher sebum content than females. The sebum content on the forehead of males aged over 13 years was significantly higher than that in females of comparable age (fig. 2a). Additionally, the sebum content on the forearm of males aged 13–35 years was also significantly higher than that in females of the same age (fig. 2a). Yet, changes in sebum content showed a comparable maximum with a peak at around the age of 40 years in females and 50 years in males (fig. 3a, b), and accordingly, the sebum content declined earlier in females than in males.
Fig. 1.
Sebum content in females and males. Significant differences are shown in the figure. The number of subjects in each group is detailed in table 1. a On the forehead in females. b On the forearm in females. c On the forehead in males. d On the forearm in males.
Fig. 2.
Comparison of sebum content (a), pH (b) and SC hydration (c) between males and females. The number of subjects in each group is detailed in table 1.
Fig. 3.
Changes in sebum content with age in females and males. a On the forearm. b On the forehead.
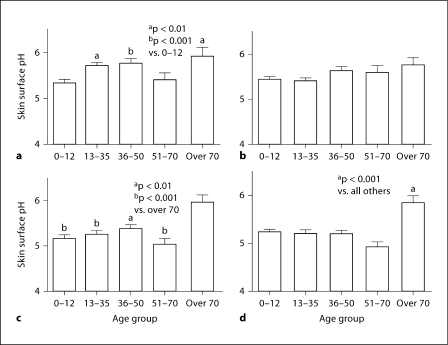
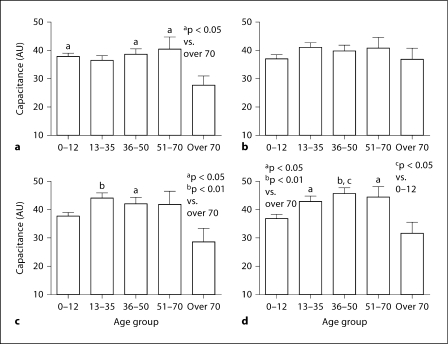
Skin Surface pH Varies with Age and Gender, but Not Body Site
Previous studies from our group have demonstrated that skin surface pH increases after the age of 50 [36]. In the present study, a higher skin surface pH also occurred in older age groups (fig. 4). In females, skin surface pH on the forehead was significantly lower at the age of 0–12 than that in older age groups (fig. 4a). Yet, skin surface pH on the forearms of females did not differ among the age groups (fig. 4b). In males, the highest skin surface pH on both the forehead and the forearm was found in the group aged over 70 (fig. 4c, d); there were no differences among males aged 0–12, 13–35, 36–50 and 51–70 years. Skin surface pH on the forehead of females aged 13–70 and the forearm of those aged 0–12, 36–50 and 51–70 was significantly higher than that in age-matched males (fig. 2b). The skin surface pH in females aged 13–35 was higher on the forehead than on the forearm (5.71 ± 0.066 vs. 5.40 ± 0.060, p < 0.001). In other age groups, there were no differences in skin surface pH between the forehead and forearm in either males or females. Overall, there was a positive linear correlation between skin surface pH and age (fig. 5a, b).
Fig. 4.
Skin surface pH in females and males. Significant differences are shown in the figure. The number of subjects in each group is detailed in table 1. a On the forehead in females. b On the forearm in females. c On the forehead in males. d On the forearm in males.
Fig. 5.
Changes in skin surface pH with age in females (a) and males (b) on the forearms and the forehead, respectively.
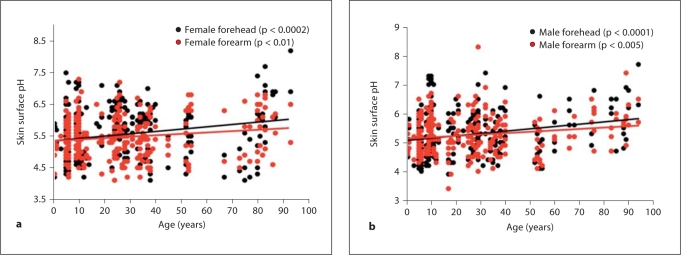
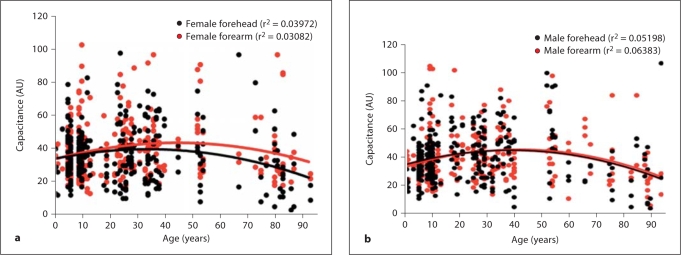
SC Hydration Significantly Varies with Age
As seen in figure 6a, SC hydration on the forehead in females aged over 70 years was significantly lower than that in females under the age of 70 except in the group aged 13–35. However, there was no significant difference in SC hydration on the forearm in females among all age groups (fig. 6b). In contrast to females, SC hydration on the forearm in males aged 13–70 was significantly higher than that in the age group over 70 (fig. 6d). And SC hydration on the forearm in males aged 0–12 was significantly lower than that of those aged 36–50 (fig. 6d). SC hydration on the forehead in males aged over 70 was also significantly lower than that in groups aged 13–35 and 36–50 years (fig. 6c). There were no differences in SC hydration between the forehead and the forearm in males. SC hydration on the forehead was higher in males aged 13–35 than that in females (fig. 2c). The changes in SC hydration over the lifetime also show typical curves, with the peak at around the age of 40–50 years in both females and males on both the forehead and the forearm (fig. 7a, b).
Fig. 6.
SC hydration in females and males. Significant differences are shown in the figure. The number of subjects in each group is detailed in table 1. a On the forehead in females. b On the forearm in females. c On the forehead in males. d On the forearm in males.
Fig. 7.
Changes in SC hydration with age in females (a) and males (b) on the forearms and the forehead, respectively.
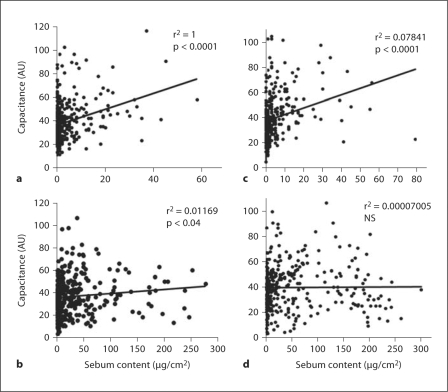
Previous studies have demonstrated that sebum is a major source for glycerol, which, in turn, regulates SC hydration [37, 39]. We therefore next assessed the correlation of SC hydration with sebum content. As seen in figure 8, there is a significantly positive correlation between sebum content and SC hydration on the forearms and the forehead of females (fig. 8a, b). In contrast, there is no significant correlation between SC hydration and sebum content on the forehead of males (fig. 8d).
Fig. 8.
Correlations of sebum content with SC hydration. Significances are shown in the figure. The number of subjects in each group is detailed in table 1. a For the forearms of females. b For the forehead of females. c For the forearms of males. d For the forehead of males.
Discussion
While previous studies were designed to compare skin physiology in young and old skin, here we compare multiple parameters over the whole spectrum of ages in both males and females. In agreement with previous findings [27, 36, 40], our results show that skin surface pH increases in the aged compared to the young group although no difference in skin surface pH on the forearms between old and young subjects was reported by others [28]. In contrast to the previous findings in 10 subjects studied in the USA [27], our results did not show any significant difference in skin surface pH in either males or females between the forehead and the forearm in all age groups. This result is in agreement with others [41]. Although the study on Caucasians aged 26–59 years showed that females have a lower skin surface pH on the forearm and axilla [33, 34], studies here demonstrated that skin surface pH on both the forehead of females aged 13–70 and the forearm of females aged 36–70 was higher than that of males. The difference may be due to sample size and/or the subjects’ ethnicities. The elevated skin surface pH in an aged group is attributable to the decrease in epidermal expression of Na/H+ exchange 1, which is one of the key factors regulating skin surface pH [36, 42].
It has been reported that the sebum content on the forehead in an older group is either not different from young subjects or higher than in a young group (study conducted in San Francisco, Calif., USA) [27, 28]. However, our results demonstrated that the sebum content on both the forehead and the forearm in females aged 13–70 years is significantly higher than in those under 13 and over the age of 70. And the sebum content on both the forehead and the forearm in males aged 0–12 is also significantly lower than that in other age groups. These differences may be due to sample size and/or ethnicity studied. Additionally, the sebum content on the forehead in males aged over 12 is higher than in females, which is consistent with the findings of others [29,30,31]. Interestingly, the sebum content curve on the forehead occurs earlier in females than in males over the lifetime. It is well known that sexual hormones influence sebum production [43,44,45]. Prior studies demonstrated that sebum production rates correlate positively with testosterone levels in both sexes, and with dehydroepiandrosterone in males and etiocholanolone in females [46,47,48]. Maximum dehydroepiandrosterone sulfate levels occur at about 24 years of age in women and at about 30 years of age in men, and the levels in females and males decline at 50 and 60 years of age, respectively. In contrast, dehydroepiandrosterone levels reach a maximum at about 20 years of age in both women and men [49]. These results are consistent with our findings which demonstrate that the peak sebum content occurs in the 13- to 35-year age group, and the content declines earlier in females than in males. Thus, the variation of sebum content with age is most likely due to the change in sex hormone levels, especially in women whose sebum content on the forehead begins to decline at about the age of 50, when menopause occurs. Thus, the gender differences in sebum content should be considered in the formulation of skin care products.
In contrast to the previous finding that SC hydration on the forearm in the old (mean age 73.6) is higher than that in the young group (mean age 29.8) [27], our results demonstrated that SC hydration on the forearm in males over the age of 70 is significantly lower than that in the group aged 13–70 years. In addition, a significant low SC hydration on the forehead in both males and females over the age of 70 was also observed in the present study. Cua et al. [50] reported no difference in SC hydration on either the forehead or the volar forearm between the old and the young. Again, the different results between ours and others may be due to either sample size or the subjects’ ethnicities. It has been described that the dryness of skin in aged Caucasians and African-Americans is higher than that in the Chinese [35]. A previous study showed no difference in SC hydration between males and females at around 40 years of age [51]. However, our present study demonstrates gender differences in SC hydration in the group aged 13–35 years, which is consistent with our prior finding [52]. There are several factors contributing to the reduced SC hydration in the older group. Natural moisturizers in SC are key factors regulating SC hydration. It has been shown that there is a reduction in epidermal lipids in aged mice [53]. In addition, sebum levels are decreased in aged humans [51]. Moreover, SC lactate is also decreased in the older human in addition to the reduction in sebum content discussed above [54]. Thus, the reductions of these natural moisturizers in the SC could account for the lower SC hydration in the old. SC hydration plays important roles in cutaneous functions such as regulating epidermal proliferation, differentiation or inflammation [55,56,57]. Finally, so far this is the first documentation of the change curves of both sebum content and SC hydration over the lifetime. Not only similarity of these two curves, but also the correlation between sebum content and SC hydration further suggest the importance of sebum in SC hydration, as shown in earlier studies [37, 39]. Nevertheless, the present study indicates that SC hydration declines at the age of 50, suggesting that moisturizers are required at this age.
In summary, the present study shows that sebum content, skin surface pH and SC hydration vary with age, gender and body sites in a Chinese population. These changes, especially sebum content, are correlated with age. Whether these results in the Chinese population are comparable to those in other ethnicities is not known yet. Nevertheless, these results suggest that special care should be given to the skin in older individuals, particularly the Chinese.
Acknowledgements
This work was supported by grants from the National Institutes of Health (AR 19098) and the Medical Research Service, Department of Veterans Affairs Medical Center, San Francisco, Calif., USA.
References
- 1.Firooz A, Gorouhi F, Davari P, Atarod M, Hekmat S, Rashighi-Firoozabadi M, Solhpour A. Comparison of hydration, sebum and pH values in clinically normal skin of patients with atopic dermatitis and healthy controls. Clin Exp Dermatol. 2007;32:321–322. doi: 10.1111/j.1365-2230.2007.02364.x. [DOI] [PubMed] [Google Scholar]
- 2.Sator PG, Schmidt JB, Hönigsmann H. Comparison of epidermal hydration and skin surface lipids in healthy individuals and in patients with atopic dermatitis. J Am Acad Dermatol. 2003;48:352–358. doi: 10.1067/mjd.2003.105. [DOI] [PubMed] [Google Scholar]
- 3.Hon KL, Wong KY, Leung TF, Chow CM, Ng PC. Comparison of skin hydration evaluation sites and correlations among skin hydration, transepidermal water loss, SCORAD index, Nottingham Eczema Severity Score, and quality of life in patients with atopic dermatitis. Am J Clin Dermatol. 2008;9:45–50. doi: 10.2165/00128071-200809010-00005. [DOI] [PubMed] [Google Scholar]
- 4.Gupta J, Grube E, Ericksen MB, Stevenson MD, Lucky AW, Sheth AP, Assa'ad AH, Khurana Hershey GK. Intrinsically defective skin barrier function in children with atopic dermatitis correlates with disease severity. J Allergy Clin Immunol. 2008;121:725–730. doi: 10.1016/j.jaci.2007.12.1161. [DOI] [PubMed] [Google Scholar]
- 5.Tomita Y, Akiyama M, Shimizu H. Stratum corneum hydration and flexibility are useful parameters to indicate clinical severity of congenital ichthyosis. Exp Dermatol. 2005;14:619–624. doi: 10.1111/j.0906-6705.2005.00341.x. [DOI] [PubMed] [Google Scholar]
- 6.Grubauer G, Feingold KR, Elias PM. Relationship of epidermal lipogenesis to cutaneous barrier function. J Lipid Res. 1987;28:746–752. [PubMed] [Google Scholar]
- 7.Proksch E, Feingold KR, Elias PM. Epidermal HMG CoA reductase activity in essential fatty acid deficiency: barrier requirements rather than eicosanoid generation regulate cholesterol synthesis. J Invest Dermatol. 1992;99:216–220. doi: 10.1111/1523-1747.ep12650440. [DOI] [PubMed] [Google Scholar]
- 8.Denda M, Tsuchiya T, Elias PM, Feingold KR. Stress alters cutaneous permeability barrier homeostasis. Am J Physiol Regul Integr Comp Physiol. 2000;278:R367. doi: 10.1152/ajpregu.2000.278.2.R367. [DOI] [PubMed] [Google Scholar]
- 9.Garg A, Chren MM, Sands LP, Matsui MS, Marenus KD, Feingold KR, Elias PM. Psychological stress perturbs epidermal permeability barrier homeostasis: implications for the pathogenesis of stress-associated skin disorders. Arch Dermatol. 2001;137:53–59. doi: 10.1001/archderm.137.1.53. [DOI] [PubMed] [Google Scholar]
- 10.Altemus M, Rao B, Dhabhar FS, Ding W, Granstein RD. Stress-induced changes in skin barrier function in healthy women. J Invest Dermatol. 2001;117:309–317. doi: 10.1046/j.1523-1747.2001.01373.x. [DOI] [PubMed] [Google Scholar]
- 11.Denda M, Tsuchiya T, Hosoi J, Koyama J. Immobilization-induced and crowded environment-induced stress delay barrier recovery in murine skin. Br J Dermatol. 1998;138:780–785. doi: 10.1046/j.1365-2133.1998.02213.x. [DOI] [PubMed] [Google Scholar]
- 12.Kato A, Hamada M, Maruyama T, Maruyama Y, Hishida A. Pruritus and hydration state of stratum corneum in hemodialysis patients. Am J Nephrol. 2000;20:437–442. doi: 10.1159/000046196. [DOI] [PubMed] [Google Scholar]
- 13.Morton CA, Lafferty M, Hau C, Henderson I, Jones M, Lowe JG. Pruritus and skin hydration during dialysis. Nephrol Dial Transplant. 1996;11:2031–2036. doi: 10.1093/oxfordjournals.ndt.a027092. [DOI] [PubMed] [Google Scholar]
- 14.Yosipovitch G, Tur E, Morduchowicz G, Boner G. Skin surface pH, moisture, and pruritus in haemodialysis patients. Nephrol Dial Transplant. 1993;8:1129–1132. [PubMed] [Google Scholar]
- 15.Song SP, Lv CZ, Feingold KR, Hou QN, Li ZY, Guo CY, Elias PM, Man MQ. Abnormalities in stratum corneum function in patients recovered from leprosy. Skin Pharmacol Physiol. 2009;22:131–136. doi: 10.1159/000189802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ohman H, Vahlquist A. The pH gradient over the stratum corneum differs in X-linked recessive and autosomal dominant ichthyosis: a clue to the molecular origin of the ‘acid skin mantle’? J Invest Dermatol. 1998;111:674–677. doi: 10.1046/j.1523-1747.1998.00356.x. [DOI] [PubMed] [Google Scholar]
- 17.Ohta H, Makita K, Kawashima T, Kinoshita S, Takenouchi M, Nozawa S. Relationship between dermato-physiological changes and hormonal status in pre-, peri-, and postmenopausal women. Maturitas. 1998;30:55–62. doi: 10.1016/s0378-5122(98)00040-1. [DOI] [PubMed] [Google Scholar]
- 18.Guinot C, Malvy D, Ambroisine L, Latreille J, Mauger E, Guéhenneux S, Morizot F, Tschachler E. Effect of hormonal replacement therapy on skin biophysical properties of menopausal women. Skin Res Technol. 2005;11:201–204. doi: 10.1111/j.1600-0846.2005.00121.x. [DOI] [PubMed] [Google Scholar]
- 19.Sator PG, Schmidt JB, Sator MO, Huber JC, Hönigsmann H. The influence of hormone replacement therapy on skin ageing: a pilot study. Maturitas. 2001;39:43–55. doi: 10.1016/s0378-5122(00)00225-5. [DOI] [PubMed] [Google Scholar]
- 20.Sator PG, Sator MO, Schmidt JB, Nahavandi H, Radakovic S, Huber JC, Hönigsmann H. A prospective, randomized, double-blind, placebo-controlled study on the influence of a hormone replacement therapy on skin aging in postmenopausal women. Climacteric. 2007;10:320–334. doi: 10.1080/13697130701444073. [DOI] [PubMed] [Google Scholar]
- 21.McDaniel D, Neudecker B, Dinardo J, Lewis J, 2nd, Maibach H. Clinical efficacy assessment in photodamaged skin of 0.5 and 1.0% idebenone. J Cosmet Dermatol. 2005;4:167–173. doi: 10.1111/j.1473-2165.2005.00305.x. [DOI] [PubMed] [Google Scholar]
- 22.Tagami H. Scientific characterization of subclinical skin changes by noninvasive biophysical methods for development of more efficacious skin care products. Int J Cosmet Sci. 2007;29:409–410. [Google Scholar]
- 23.Aschoff R, Schwanebeck U, Bräutigam M, Meurer M. Skin physiological parameters confirm the therapeutic efficacy of pimecrolimus cream 1% in patients with mild-to-moderate atopic dermatitis. Exp Dermatol. 2009;18:24–29. doi: 10.1111/j.1600-0625.2008.00756.x. [DOI] [PubMed] [Google Scholar]
- 24.Kikuchi K, Tagami H, Agawa Y, Akazaki S, Ando M, Hayashi A, Hayashi T, Hirao T, Ishida T, Ito K, Kurimura I, Matsumoto K, Nozaki F, Ozawa T, Takahashi M. Noninvasive biophysical assessments of the efficacy of a moisturizing cosmetic cream base for patients with atopic dermatitis during different seasons. Br J Dermatol. 2008;158:969–978. doi: 10.1111/j.1365-2133.2008.08478.x. [DOI] [PubMed] [Google Scholar]
- 25.Brazzelli V, Barbagallo T, Prestinari F, Rona C, De Silvestri A, Trevisan V, Borroni G. Non-invasive evaluation of tacalcitol plus PUVA versus tacalcitol plus UVB-NB in the treatment of psoriasis: ‘right-left intra-individual pre/post comparison design’. Int J Immunopathol Pharmacol. 2005;18:755–760. doi: 10.1177/039463200501800419. [DOI] [PubMed] [Google Scholar]
- 26.Rim JH, Jo SJ, Park JY, Park BD, Youn JI. Electrical measurement of moisturizing effect on skin hydration and barrier function in psoriasis patients. Clin Exp Dermatol. 2005;30:409–413. doi: 10.1111/j.1365-2230.2005.01773.x. [DOI] [PubMed] [Google Scholar]
- 27.Marrakchi S, Maibach HI. Biophysical parameters of skin: map of human face, regional, and age-related differences. Contact Dermatitis. 2007;57:28–34. doi: 10.1111/j.1600-0536.2007.01138.x. [DOI] [PubMed] [Google Scholar]
- 28.Wilhelm KP, Cua AB, Maibach HI. Skin aging: effect on transepidermal water loss, stratum corneum hydration, skin surface pH, and casual sebum content. Arch Dermatol. 1991;127:1806–1809. doi: 10.1001/archderm.127.12.1806. [DOI] [PubMed] [Google Scholar]
- 29.Aisen E, Shafran A, Gilhar A. Sebum and water content in the skin of aged immobilized patients. Acta Derm Venereol. 1997;77:142–143. doi: 10.2340/0001555577142143. [DOI] [PubMed] [Google Scholar]
- 30.Wendling PA, Dell'Acqua G. Skin biophysical properties of a population living in Valais, Switzerland. Skin Res Technol. 2003;9:331–338. doi: 10.1034/j.1600-0846.2003.00040.x. [DOI] [PubMed] [Google Scholar]
- 31.Kim MK, Patel RA, Shinn AH, Choi SY, Byun HJ, Huh CH, Park KC, Youn SW. Evaluation of gender difference in skin type and pH. J Dermatol Sci. 2006;41:153–156. doi: 10.1016/j.jdermsci.2005.12.001. [DOI] [PubMed] [Google Scholar]
- 32.Jacobi U, Gautier J, Sterry W, Lademann J. Gender-related differences in the physiology of the stratum corneum. Dermatology. 2005;211:312–317. doi: 10.1159/000088499. [DOI] [PubMed] [Google Scholar]
- 33.Ehlers C, Ivens UI, M⊘ller ML, Senderovitz T, Serup J. Females have lower skin surface pH than men: a study on the surface of gender, forearm site variation, right/left difference and time of the day on the skin surface pH. Skin Res Technol. 2001;7:90–94. doi: 10.1034/j.1600-0846.2001.70206.x. [DOI] [PubMed] [Google Scholar]
- 34.Williams S, Davids M, Reuther T, Kraus D, Kerscher M. Gender difference of in vivo skin surface pH in the axilla and the effect of a standardized washing procedure with tap water. Skin Pharmacol Physiol. 2005;18:247–252. doi: 10.1159/000086671. [DOI] [PubMed] [Google Scholar]
- 35.Diridollou S, de Rigal J, Querleux B, Leroy F, Holloway Barbosa V. Comparative study of the hydration of the stratum corneum between four ethnic groups: influence of age. Int J Dermatol. 2007;46(suppl 1):11–14. doi: 10.1111/j.1365-4632.2007.03455.x. [DOI] [PubMed] [Google Scholar]
- 36.Choi EH, Man MQ, Xu P, Xin S, Liu Z, Crumrine DA, Jiang YJ, Fluhr JW, Feingold KR, Elias PM, Mauro TM. Stratum corneum acidification is impaired in moderately aged human and murine skin. J Invest Dermatol. 2007;127:2847–2856. doi: 10.1038/sj.jid.5700913. [DOI] [PubMed] [Google Scholar]
- 37.Choi EH, Man MQ, Wang F, Zhang X, Brown BE, Feingold KR, Elias PM. Is endogenous glycerol a determinant of stratum corneum hydration in humans? J Invest Dermatol. 2005;125:288–293. doi: 10.1111/j.0022-202X.2005.23799.x. [DOI] [PubMed] [Google Scholar]
- 38.Kuss O, Diepgen TL. Proper statistical analysis of transepidermal water loss (TEWL) measurements in bioengineering studies. Contact Dermatitis. 1998;39:64–67. doi: 10.1111/j.1600-0536.1998.tb05834.x. [DOI] [PubMed] [Google Scholar]
- 39.Fluhr JW, Man MQ, Brown BE, Wertz PW, Crumrine D, Sundberg JP, Feingold KR, Elias PM. Glycerol regulates stratum corneum hydration in sebaceous gland deficient (asebia) mice. J Invest Dermatol. 2003;120:728–737. doi: 10.1046/j.1523-1747.2003.12134.x. [DOI] [PubMed] [Google Scholar]
- 40.Zlotogorski A. Distribution of skin surface pH on the forehead and cheek of adults. Arch Dermatol Res. 1987;279:398–401. doi: 10.1007/BF00412626. [DOI] [PubMed] [Google Scholar]
- 41.Fluhr JW, Dickel H, Kuss O, Weyher I, Diepgen TL, Berardesca E. Impact of anatomical location on barrier recovery, surface pH and stratum corneum hydration after acute barrier disruption. Br J Dermatol. 2002;146:770–776. doi: 10.1046/j.1365-2133.2002.04695.x. [DOI] [PubMed] [Google Scholar]
- 42.Behne MJ, Meyer JW, Hanson KM, Barry NP, Murata S, Crumrine D, Clegg RW, Gratton E, Holleran WM, Elias PM, Mauro TM. NHE1 regulates the stratum corneum permeability barrier homeostasis: microenvironment acidification assessed with fluorescence lifetime imaging. J Biol Chem. 2002;277:47399–47406. doi: 10.1074/jbc.M204759200. [DOI] [PubMed] [Google Scholar]
- 43.Nouveau S, Bastien P, Baldo F, de Lacharrière O. Effects of topical DHEA on aging skin: a pilot study. Maturitas. 2008;59:174–181. doi: 10.1016/j.maturitas.2007.12.004. [DOI] [PubMed] [Google Scholar]
- 44.Fritsch M, Orfanos CE, Zouboulis CC. Sebocytes are the key regulators of androgen homeostasis in human skin. J Invest Dermatol. 2001;116:793–800. doi: 10.1046/j.1523-1747.2001.01312.x. [DOI] [PubMed] [Google Scholar]
- 45.Giltay EJ, Gooren LJ. Effects of sex steroid deprivation/administration on hair growth and skin sebum production in transsexual males and females. J Clin Endocrinol Metab. 2000;85:2913–2921. doi: 10.1210/jcem.85.8.6710. [DOI] [PubMed] [Google Scholar]
- 46.O'Connell K, Westhoff C. Pharmacology of hormonal contraceptives and acne. Cutis. 2008;81(1 suppl):8–12. [PubMed] [Google Scholar]
- 47.Stewart ME, Downing DT, Cook JS, Hansen JR, Strauss JS. Sebaceous gland activity and serum dehydroepiandrosterone sulfate levels in boys and girls. Arch Dermatol. 1992;128:1345–1348. [PubMed] [Google Scholar]
- 48.Yamamoto A, Ito M. Sebaceous gland activity and urinary androgen levels in children. J Dermatol Sci. 1992;4:98–104. doi: 10.1016/0923-1811(92)90066-k. [DOI] [PubMed] [Google Scholar]
- 49.Sulcová J, Hill M, Hampl R, Stárka L. Age and sex related differences in serum levels of unconjugated dehydroepiandrosterone and its sulphate in normal subjects. J Endocrinol. 1997;154:57–62. doi: 10.1677/joe.0.1540057. [DOI] [PubMed] [Google Scholar]
- 50.Cua AB, Wilhelm KP, Maibach HI. Frictional properties of human skin: relation to age, sex and anatomical region, stratum corneum hydration and transepidermal water loss. Br J Dermatol. 1990;123:473–479. doi: 10.1111/j.1365-2133.1990.tb01452.x. [DOI] [PubMed] [Google Scholar]
- 51.Fluhr JW, Pelosi A, Lazzerini S, Dikstein S, Berardesca E. Differences in corneocyte surface area in pre- and post-menopausal women: assessment with the noninvasive videomicroscopic imaging of corneocytes method (VIC) under basal conditions. Skin Pharmacol Appl Skin Physiol. 2001;14(suppl):10–16. doi: 10.1159/000056384. [DOI] [PubMed] [Google Scholar]
- 52.Xin SJ, Liu ZL, Shi YJ, Feingold KR, Elias PM, Man MQ. Study on the sebum content and stratum corneum hydration in the normal Chinese population (in Chinese) J Clin Dermatol. 2007;36:131–133. [Google Scholar]
- 53.Ghadially R, Brown BE, Sequeira-Martin SM, Feingold KR, Elias PM. The aged epidermal permeability barrier: structural, functional, and lipid biochemical abnormalities in humans and a senescent murine model. J Clin Invest. 1995;95:2281–2290. doi: 10.1172/JCI117919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Egawa M, Tagami H. Comparison of the depth profiles of water and water-binding substances in the stratum corneum determined in vivo by Raman spectroscopy between the cheek and volar forearm skin: effects of age, seasonal changes and artificial forced hydration. Br J Dermatol. 2008;158:251–260. doi: 10.1111/j.1365-2133.2007.08311.x. [DOI] [PubMed] [Google Scholar]
- 55.Kikuchi K, Kobayashi H, Hirao T, Ito A, Takahashi H, Tagami H. Improvement of mild inflammatory changes of the facial skin induced by winter environment with daily applications of a moisturizing cream: a half-side test of biophysical skin parameters, cytokine expression pattern and the formation of cornified envelope. Dermatology. 2003;207:269–275. doi: 10.1159/000073089. [DOI] [PubMed] [Google Scholar]
- 56.Hagemann I, Proksch E. Topical treatment by urea reduces epidermal hyperproliferation and induces differentiation in psoriasis. Acta Derm Venereol. 1996;76:353–356. doi: 10.2340/0001555576353356. [DOI] [PubMed] [Google Scholar]
- 57.Engelke M, Jensen JM, Ekanayake-Mudiyanselage S, Proksch E. Effects of xerosis and ageing on epidermal proliferation and differentiation. Br J Dermatol. 1997;137:219–225. doi: 10.1046/j.1365-2133.1997.18091892.x. [DOI] [PubMed] [Google Scholar]