INTRODUCTION
Suicide is a major public health problem throughout the world, taking approximately one million lives every year worldwide (WHO 2009, Mann 2003) .An intriguing and highly-replicated finding of this tragedy is its seasonal spring peak (Lester et al 1990, Maes et al 1993, Chew et al 1995, Hakko et al 1998, Lester et al 2001, Petridou et al 2002) with a temporal mirror image in the Southern Hemisphere (Cantor et al 2000, Rock et al 2003). At the same time, a peak in spring has also been reported for exacerbation of its most prominent risk factor, mood disorder , as manifested in hospital admissions, mood disorder severity, electroconvulsive therapy (ECT) use , and worsening of depression scores (Zung and Green 1974, Eastwood and Stiasny 1978, Frangos et al 1980, Fossey and Shapiro, 1992, Morken et al 2002, Maes et al 1993, Goodwin and Jamison 2007) . The association between spring peaks in suicide and spring peaks in exacerbation of mood disorder is conducive to a hypothesis that the spring peak in suicide is driven by a seasonal decompensation of mood disorder in spring. If so, one would expect a greater suicide peak in spring among individuals with a history of hospitalization for mood disorders. To our knowledge, only one previous study on a limited sample of 115 suicides has explored the pattern of seasonality of suicide in victims with versus without history of hospitalization for mood disorders, finding a spring/summer peak only in individuals with hospitalization for mood disorders (Kim et al 2004). . In this study using the data covering the entire national population in Denmark over a 32-year period, we plan to estimate seasonality of suicide in those with versus those without history of hospitalization for mood disorders. As we theorize that an environmental factor is responsible for precipitation or exacerbation of depressive episodes in spring which trigger suicide in vulnerable individuals, we expected to find an increased relative risk of suicide in spring among those with history of hospitalization for mood disorders compared to those without such a history. Previous research on seasonality of suicide has found gender differences, specifically a higher seasonality of suicide in males than in females (Micciolo et al 1989, Preti 1997) and the existence of a secondary peak in the fall in females (Hakko et al 1998, Micciolo et al 1989, Meares et al 1981, Lester and Frank 1988) . In addition, there are significant interactions between gender and deliberate self harm methods (Hawton et al 2008) and between seasons and deliberate self harm (with a greater seasonality in parasuicides in females: Barker et al 1994). Due to interactions between gender and seasonality of suicide and suicidality, we also aimed to analyze the interaction between genders, prior history of mood disorders, and the amplitude of the spring peak of suicide.
METHOD
Data sources
Data for the present study were retrieved from four Danish national longitudinal registers. The first was the Cause of Death Register which has recorded causes and dates of all deaths in Denmark since 1970. The second register was the Danish Psychiatric Central Register. This register covers all psychiatric inpatient facilities in Denmark and cumulatively records all admission and discharge information, such as dates and main and auxiliary diagnoses. Diagnoses of illnesses and causes of death in these two medical registries were coded according to the 8th edition of the International Classification of Diseases (ICD-8) until the end of 1993 and, thereafter, according to the 10th edition (ICD-10). The third register was the Integrated Database for Labour Market Research (IDA database) which contains yearly socioeconomic information such as employment, income, marital status, place of residence, etc., for all national residents in Denmark since 1980. Personal data is completed for individuals residing in Denmark on the 31st of December of the calendar year. The last register was the Danish Civil Registration System (CRS) which contains a personal identifier, designated as the CPR-number, for all individuals residing in Denmark. The CPR-number is used in all nationwide registers and can be logically checked for errors. It was therefore the key for the retrieval and merging of individual data from the different register databases in this study.
Subjects, variables, and statistical methods
Our primary study cases were composed of all definite suicides (codes E950–959 in ICD-8 and X60–84 in ICD-10) recorded in the Cause of Death Register from the years 1970 through 2001. From this register and the CPR number, we obtained the date of death and the method of suicide for all suicide victims. We categorized the date of suicide according to the 12 months of the year, and also into the time windows of the approximated four seasons, defined as winter (January–March), spring (April–June), summer (July–September), and fall (October–December). Method of suicide was also grouped into two categories delineated as nonviolent and violent methods.
We then obtained information about personal history of hospitalization for mood disorders from the Danish Psychiatric Central Register. We defined a positive history for a subject if the person had been admitted for hospital treatment because of a mood disorder since 1969 (when the first computerized data became available) until the time of suicide. Major mood disorder codes included manic-depressive illness (for ICD-8: 296.1, 296.2, 296.3, 298.1 and for ICD-10: F30, F31) and unipolar depression (for ICD-8: 300.4, 300.5, 296.0, 298.0 and for ICD-10: F32, F33).
For cases that occurred during 1981 to 1997, the only time during which complete data was available, we were able to obtain socioeconomic data from the IDA database for the year preceding the year in which the suicide took place. The examined variables included marital status (single or cohabitating versus married), annual gross income (by quartile according to the annual 5-year age-specific distribution in the general population), and place of residence (the capital, suburb of the capital, provincial city with more than 100,000 inhabitants, or provincial town with more than 10,000 inhabitants versus rural areas). We chose these variables for data adjustment because they are highly associated with suicide in Denmark (Qin et al 2003).
We constructed contingency tables for the study variables and computed the rate ratio of suicide across months and seasons using procedures available in SAS version 8.
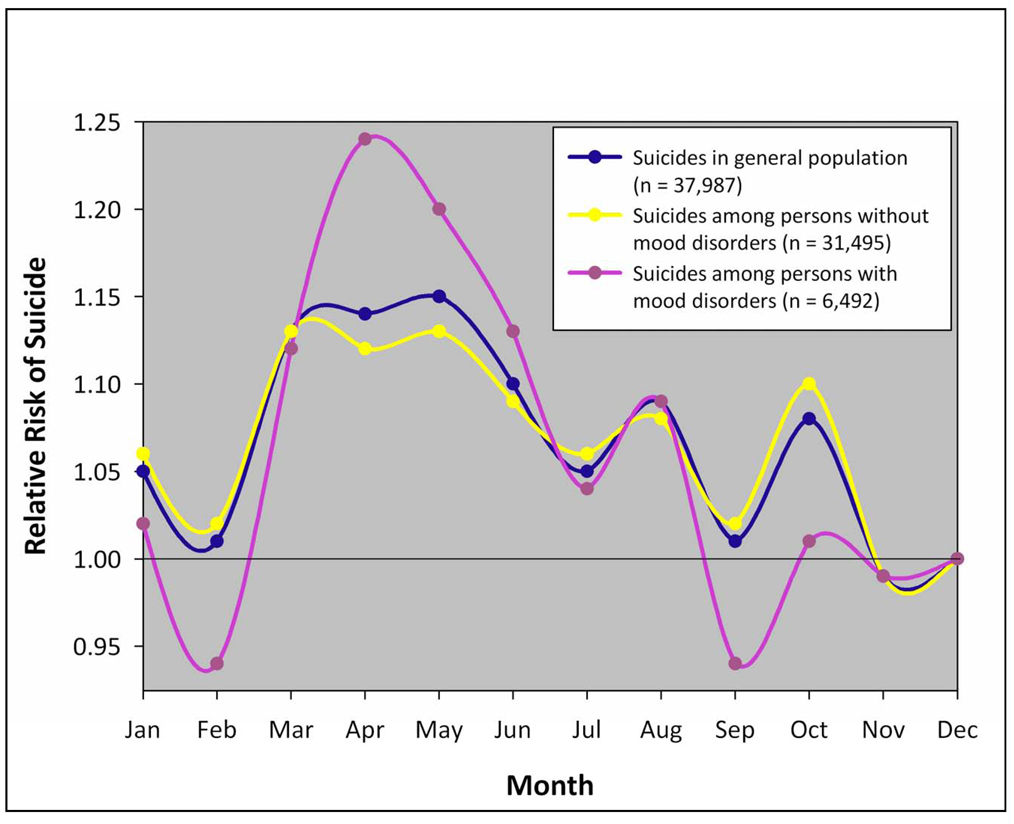
We first calculated rate ratio of suicide in each month based upon all 37,987 suicides over the 32-year period, according to history of hospitalization for mood disorders and by using the rate in December as the reference (see Figure 1 and Table 1). The rate ratio and 95% confidence intervals were obtained with Poisson regression analysis, where the logarithm of the expected number of suicides in each month was regressed on the logarithm of actual days in each period assuming the national population over a calendar year remained constant. Using a similar statistical technique, we then estimated the rate ratio of suicide, separately for men and women, for the approximated seasons of spring, summer, and fall and compared each with the reference season of winter (see Table 1).
Figure 1.
Relative Risk of Suicide by Month and Mood Disorder Status
Table 1.
| Season | Suicide caseswith mood disordersa |
Suicide cases without mood disorders |
Suicide cases with mood disordersa |
Suicide cases without mood disorders |
||
|---|---|---|---|---|---|---|
| Number cases |
Number cases |
Rate ratio |
95% CI | Rate ratio |
95% CI | |
| Men | 2938 | 21532 | ||||
| Jan – Mar | 700 | 5400 | 1.01 | 0.91, 1.12 | 1.05 | 1.01, 1.09* |
| Apr – Jun | 825 | 5533 | 1.18 | 1.07, 1.31* | 1.07 | 1.03, 1.11* |
| Jul – Sep | 707 | 5355 | 1.00 | 0.90, 1.11 | 1.02 | 0.98, 1.06 |
| Oct – Dec | 706 | 5244 | 1 | 1 | ||
| Women | 3554 | 9963 | ||||
| Jan – Mar | 856 | 2419 | 1.05 | 0.95, 1.15 | 1.02 | 0.97, 1.08 |
| Apr – Jun | 994 | 2653 | 1.20 | 1.10, 1.32* | 1.11 | 1.05, 1.18* |
| Jul – Sep | 869 | 2482 | 1.04 | 0.95, 1.14 | 1.03 | 0.97, 1.09 |
| Oct – Dec | 835 | 2409 | 1 | 1 | ||
P < 0.01.
Case classified as a history of hospital admission for mood disorders.
To further examine the seasonal differences by history of mood disorder and to control for potentially confounding effects of personal socioeconomic factors and method of suicide, we used suicide victims with a history of hospitalization for mood disorders as cases and victims without such a history as comparison controls and then computed the relative risk ratio of suicide in relation to seasonality (see Table 2). Study subjects were restricted to the 21,169 suicides who, from 1981 to 1997, were residing in Denmark on the 31st of December before the year of death. We analyzed the data with conditional logistic regression with a stratum by calendar year, first using crude analysis and later adjusting for income, marriage, place of residence, and method of suicide. Based on the adjusted model and cases of both men and women, we tested sex differences of seasonal variance of suicide by history of hospitalization for mood disorders using the likelihood ratio test.
Table 2.
| Season | Casesa (suicide cases with mood disorders) |
Controlsa (suicide cases without mood disorders) |
Crude analysisb | Adjusted analysisc | ||
|---|---|---|---|---|---|---|
| Number suicides |
Number suicides |
Rate ratio | 95% CI | Rate ratio | 95% CI | |
| Men | 1710 | 11971 | ||||
| Jan – Mar | 395 | 3074 | 0.95 | 0.82, 1.11 | 1.01 | 0.87, 1.18 |
| Apr – Jun | 512 | 3083 | 1.23 | 1.07, 1.42 * | 1.25 | 1.08, 1.44 * |
| Jul – Sep | 418 | 2959 | 1.05 | 0.91, 1.22 | 1.05 | 0.91, 1.21 |
| Oct – Dec | 385 | 2855 | 1 | 1 | ||
| Women | 2239 | 5249 | ||||
| Jan – Mar | 561 | 1268 | 1.12 | 0.97, 1.29 | 1.18 | 1.02, 1.37** |
| Apr – Jun | 632 | 1364 | 1.17 | 1.02, 1.35** | 1.20 | 1.04, 1.38* |
| Jul – Sep | 533 | 1322 | 1.01 | 0.88, 1.17 | 1.02 | 0.88, 1.18 |
| Oct – Dec | 513 | 1295 | 1 | 1 | ||
P < 0.01
P < 0.05
Cases were suicide victims who had a history of hospital admission for mood disorders, while controls were suicide victims who did not had such a history;
Crude rate ratios were adjusted for calendar year;
Adjusted rate ratios were further adjusted for personal marital status, income, place of residence and method used for suicide.
Note: Test of sex differences of suicide seasonality, based on adjusted model: χ2=6.12, P = 0.106.
In addition, we also performed analyses examining seasonal differences by method of suicide; however, we did not observe statistically significant differences between violent suicides and nonviolent suicides.
RESULTS
Between 1970 and 2001, 24,470 males and 13,517 females committed suicide in Denmark. Among these, 17.1% of the suicides occurred in individuals previously hospitalized for mood disorders, with 2,938 males and 3,554 females accounting for the total.
A spring peak of suicide is apparent for both individuals with hospitalization for mood disorders and without hospitalization for mood disorders, but is more prominent in those with history of hospitalization for mood disorders (Figure 1). The distinction of the interpolated curves is most discernable during April and May. The spring peak, although small, was significant for both genders (see Table 1) in both the positive history of hospitalization for mood disorders group (males - relative risk [RR]: 1.18, 95% confidence interval [CI]: 1.07, 1.31; females - RR: 1.20, 95% CI: 1.10, 1.32) and also in the no history of hospitalization for mood disorders group (males - RR: 1.07, 95% CI: 1.03, 1.11; females - RR: 1.11, 95% CI: 1.05, 1.18). No significant gender difference was detected (χ 2 = 6.12, P = 0.11).
Meanwhile, we observed a marginal increase in spring for violent suicides (27% vs. 25 % expected) versus nonviolent suicides (25.5% versus 25% expected). However, the differences were not statistically significant (χ 2 = 9.84, P = 0.02).
A conditional logistic regression analysis on the somewhat smaller sample of the 1981 to 1997 interval, which allowed for adjustment of socioeconomic factors (see Table 2), showed that the presence of history of hospitalization for mood disorders is associated with a greater risk of suicide during spring in men (adjusted RR: 1.25, 95% CI: 1.08, 1.44) and women (adjusted RR: 1.20, 95% CI: 1.04, 1.38).
DISCUSSION
Findings and possible explanations
The connection between the spring peak of suicide with seasonal decompensation of depression was first noticed and suggested more than 30 years ago (Zung and Green 1974). Yet, what drives this peak remains unknown. Considering the very high association between suicide and mood disorders, an obvious hypothesis is that decompensation of mood disorders occurs during or slightly preceding the peak of suicide in spring. As an initial step in the direction of associating the peak of suicide in spring with mood disorders, we now confirm that mood disorders are associated with a greater seasonality of suicide with peaks in spring. The Danish registers allowed the analysis of multiple years, covered the entire population of Denmark, provided the capability to link cause of death with psychiatric history, and substantially permitted an adjustment for socioeconomic factors which otherwise may have masked or spuriously created an erroneous temporal pattern. Previously, Kim et al. (2004) in a relatively small, all male sample (N = 115), reported that suicide victims with history of hospitalization for mood disorders showed a spring/summer seasonal pattern in contrast to suicide victims with personality disorders who did not show a seasonal distribution of suicide; those with psychotic disorders tended to commit suicide more often in fall/winter. Two other previous large scale analyses of seasonality of suicide in Denmark (Yip et al 2006) and Italy (Rochi et al 2007) related the suicide peak to mental illness in general, but did not specifically analyze data for the contribution of mood disorders. Valtonen et al (2006), reported amplitudes of the temporal fluctuations in suicide attempts in patients with mood disorders living in Helsinki, than in those with schizophrenia, although, while the troughs were in winter, the peaks were identified in the fall rather than in the spring. However, a study of more serious suicide attempts (requiring hospital treatment) in the entire population of Finland over 7 years period, reported troughs in December and peaks in April, consistent with the majority of reports on seasonality of completed suicide (Haukka et al 2008)
There are generally two theories about the driving forces involved in the seasonal peaks in suicide. The first theory is bioclimatic: seasonal variation in bright light, photoperiod, and other meteorological variables, such as environmental temperature, may induce adverse changes in neurotransmitter systems. Of potential relevance, the neurotransmitters implicated by the monoamine-deficiency theory of mood regulation/dysregulation (Tietjen and Kripke 1994) such as dopamine, norepinephrine, and serotonin are also neurotransmitters of thermoregulation. Seasonal changes in neurotransmitter systems have been previously reported. For instance, Maes et al. (1995) reported that plasma L-tryptophan, the precursor of serotonin, a neurotransmitter broadly implicated in depression and suicide has a trough in spring.
Despite limited evidence to the contrary (Silverstone et al 1995, Simkin et al 2003) the majority of research findings suggest the peak of suicide is greater in rural areas than in urban areas (Maes et al 1993, Chew and Mc. Cleary 1995, Meares et al 1981, Micciolo et al 1991, Flisher et al 1997) and in outdoor workers compared to indoor workers (Koskinen et al 2002), making it plausible that an outdoors-related environmental factor could contribute to suicide peaks in spring. If so, this factor could be physical, chemical, biological, socioeconomic, or some combination of these variables. Although many factors have been proposed to correlate with suicide peaks, no single factor has consistent support from the literature and/or withstands scrutiny.
For instance, the environmental factor most often suggested to trigger the suicide peak is light20. Photoperiod (day length from sunrise to sunset), changes in photoperiod, and light intensity have been proposed as possible driving forces for peaks of suicide and depression (Goodwin and Jamison 2007). However, upon careful scrutiny, the peak times of suicide occurrence (April and May) do not match the peak of photoperiod (centered on the summer solstice in late June) or the time when photoperiodic changes are at their greatest (centered on the spring equinox in March)27, 37–40 (Souetre et al 1990, Linkowski et al 1992, Tietjen and Kripke 1994, Terao et al 2002). The literature on the possible relationship between meteorological variables (including sunshine and temperature) and suicide is characterized by a large variability in the strength and direction of the reported associations (Deisenhammer 2003). For instance, a very recent work (Ruuhela et al 2009) concluded that winters with low global solar radiation are associated with an increase in the risk of suicide in Finland, while Papadopoulos et al (2005) suggest a positive association between solar radiation and suicide. It is possible that the latitude and bioclimatic differences between the two countries could explain the contradictory results. Alternative biological factors have been proposed as triggers of suicide in spring, such as the marked tree pollen peaks in spring (Postolache et al 2005) which could result in seasonally increased cytokine production in upper airways resulting in increased exacerbation of mood disturbance in spring (Guzman et al 2007). Consistent with these hypotheses, intranasal tree pollen administration in previously sensitized rodents results in increased cytokine expression in the brain and behavioral alterations consisting of increased anxiety and disturbed social interaction (Tonelli et al 2009) . Moreover, rodents sensitized and exposed to tree pollen and subjected to acute stress, manifest aggressive behaviors in the resident intruder test (Tonelli et al 2008a), being previously described that aggression is an important component of completed suicide (Mann 2003). Finally, victims of suicide have an increased level of gene expression of allergy related cytokines in the orbitofrontal cortex (Tonelli et al 2008b), a region of the brain manifesting histopathological abnormalities in suicide victims (Mann 2003).
Some studies have shown a pattern of seasonality of distinct methods of suicides. For instance, both Rasanen et al. (2002) and Ajdacic-Gross et al. (2003), using large sample sizes spread across long intervals, reported various methods of suicide have a distinct seasonality component supporting the claim that seasonality may result from seasonality of opportunity/availability of methods. If seasonality is distinct for each method, this would argue against a biological factor, which may be conducive to suicide in general and would point towards sociological considerations of opportunity, availability of means, and aborting factors. However, in our data, the spring peak was present for both violent and nonviolent means, although, consistent with the literature, it was marginally stronger for violent suicides.
Although the relative risk of suicide was elevated in spring and the differences between those with versus those without hospitalization for mood disorders were significant, the findings had relatively small magnitudes. It is important to mention that seasonality of suicide in Denmark is decreasing (Yip et al 2006), which is consistent with the trends seen in Sweden (Rihmer et al 1998), England and Wales (Yip et al 2000) and Hong Kong (Yip and Yang 2004). However, in other countries, such as (Hakko et al 1998, Rasanen et al 2002, Partonen et al 2004), and the United States (Bridges et al 2005) , the seasonal suicidal peaks do not show any abatement.
Strengths and limitations
Although exacerbation of mood disorders contributing to a seasonal peak of suicide in spring is a plausible explanation of the increased peak of suicide in spring among those with a history of hospitalization for mood disorders (Kim et al 2004), current limitations of this paper do not allow ruling out other explanations. Individuals with hospitalization for mood disorders could have a different distribution of socioeconomic risk factors, and the seasonal variation in unemployment, income, and marriage/divorce could theoretically contribute to the greater seasonality of suicide in individuals with a prior history of hospitalization for mood disorders. Even if we did adjust for many socioeconomic factors, we did not adjust for the seasonality in those factors.
Another important consideration is the undercoverage of mood disorders, as only cases of mood disorders which required medical attention and hospitalization were analyzed. Most individuals with mood disorders are never admitted to the hospital or visit an emergency room. Thus, the study is seriously limited by undercoverage of mood disorders. Even under the best circumstances, we know that not all cases are diagnosed and treated. Considering, however, that the majority of suicide victims have a history mood disorders (Mann 2002), it is likely that the impact of those with history of mood disorders on total suicidality is much stronger than suggested by the current results. It is possible however, that the seasonality in the patients without mood disorders is driven by individuals who have mood disorders but were never hospitalized for it, as it was previously postulated by Rihmer et al 1998.
Another limitation is that we did not have antidepressant prescription data available for analysis. In addition, it would have been useful to have information on comorbidity with axis II disorders for analysis. Kim et al. (2004) reported that those with pure mood disorders showed a peak of suicide in spring, while those with mood disorders comorbid with axis II conditions showed no seasonality of suicide attempts. The authors suggested that axis II conditions flattened the seasonal distribution of suicide. If those suicide victims without a history of mood disorders were to have greater axis II comorbidity, it might contribute to a lesser peak of suicide in spring. Similarly, other comorbid diagnoses may have been differentially distributed between groups and spuriously augment or diminish the effects.
Finally, it is difficult to generalize the socioeconomic environment in Denmark to other countries. Denmark is a small country, with small distances from countryside to cities, a comprehensive insurance system, relatively homogenous population and customs, and relatively narrow socioeconomic differences. Thus, our results bare replication. However, seasonality of suicide in Denmark is not different from other countries, and approaches to suicide prevention are similar to those in Western Europe and the United States. Furthermore, there is a distinct advantage to testing our hypothesis in a setting where socioeconomic differences, and especially their impact on the individuals’ access to mental health treatment, are not as prominent as elsewhere. Specifically, mental psychiatric treatment, inpatient or outpatient, is covered by the Danish National Health Service. Moreover, the Danish registers were critical to our findings, the first in a large total population sample, with the capability for detailed adjustments for demographic, diagnostic, social, and economic factors.
In summary, while peaks in depression and suicide during spring have been consistently reported, the cause of these seasonal peaks is still poorly understood. The key finding of this study suggests that the presence of a mood disorder increases the spring peak of suicide. If future research demonstrates that exacerbation of mood disorders directly contributes, then the next logical step is to postulate that any seasonal factors triggering mood disorder exacerbation in spring may contribute to the seasonality of suicide. Extrapolating from this, a flattening of the spring peak of suicide may well be achieved by successfully treating exacerbations of depression in spring and identifying and addressing the factors which trigger depression in spring.
Acknowledgements
The authors wish to thank Sarah Zimmerman for her overall contribution. Funding was received from a National Institutes of Health grant (R01MH074891 to T.P.) and from the Sygekassernes Helsefond and Ministry of Social Affair in Denmark (2007B074 and INSLEV 8651-0106 to P.Q).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Statement of author contributions: Research design (TTP, PQ, PBP, LH, CF, JJS,) funding (TTP, PQ, PBM), data analysis (PQ, CF), data interpretation (TTP, PQ,PBM, LHT, XJ, CF, JJS), critical input to the manuscript (TTP, PQ PBM, LHT,XJ,CF, JJS).
REFERENCES
- Ajdacic-Gross V, Wang J, Bopp M, Eich D, Rossler W, Gutzwiller F. Are seasonalities in suicide dependent on suicide methods? A reappraisal. Soc Sci Med. 2003;57:1173–1181. doi: 10.1016/s0277-9536(02)00493-8. [DOI] [PubMed] [Google Scholar]
- Barker A, Hawton K, Fagg J, Jennison C. Seasonal and weather factors in parasuicide. Br J Psychiatry. 1994;165:375–380. doi: 10.1192/bjp.165.3.375. [DOI] [PubMed] [Google Scholar]
- Bridges FS, Yip PS, Yang KC. Seasonal changes in suicide in the United States, 1971 to 2000. Percept Mot Skills. 2005;100:920–924. doi: 10.2466/pms.100.3c.920-924. [DOI] [PubMed] [Google Scholar]
- Cantor CH, Hickey PA, De Leo D. Seasonal variation in suicide in a predominantly Caucasian tropical/subtropical region of Australia. Psychopathology. 2000;33:303–306. doi: 10.1159/000029162. [DOI] [PubMed] [Google Scholar]
- Chew KS, McCleary R. The spring peak in suicides: a cross-national analysis. Soc Sci Med. 1995;40:223–230. doi: 10.1016/0277-9536(94)e0070-9. [DOI] [PubMed] [Google Scholar]
- Deisenhammer EA. Weather and suicide: the present state of knowledge on the association of meteorological factors with suicidal behaviour. Acta Psychiatr Scand. 2003;108:402–409. doi: 10.1046/j.0001-690x.2003.00209.x. [DOI] [PubMed] [Google Scholar]
- Eastwood MR, Peacocke J. Seasonal patterns of suicide, depression and electroconvulsive therapy. Br J Psychiatry. 1976;129:472–475. doi: 10.1192/bjp.129.5.472. [DOI] [PubMed] [Google Scholar]
- Eastwood MR, Stiasny S. Psychiatric disorder, hospital admission, and season. Arch Gen Psychiatry. 1978;35:769–771. doi: 10.1001/archpsyc.1978.01770300111012. [DOI] [PubMed] [Google Scholar]
- Flisher AJ, Parry CD, Bradshaw D, Juritz JM. Seasonal variation of suicide in South Africa. Psychiatry Res. 1997;66:13–22. doi: 10.1016/s0165-1781(96)02974-5. [DOI] [PubMed] [Google Scholar]
- Fossey E, Shapiro CM. Seasonality in psychiatry-a review. Can J Psychiatry. 1992;37:299–308. doi: 10.1177/070674379203700503. [DOI] [PubMed] [Google Scholar]
- Frangos E, Athanassenas G, Tsitourides S, Psilolignos P, Robos A, Katsanou N, et al. Seasonality of the episodes of recurrent affective psychoses. Possible prophylactic interventions. J Affect Disord. 1980;2:239–247. doi: 10.1016/0165-0327(80)90025-7. [DOI] [PubMed] [Google Scholar]
- Goodwin FK, Jamison KR. Sleep and biological rhythms. Manic-Depressive Illness: Bipolar Disorders and Recurrent Depression. 2007;19 541-574.14. [Google Scholar]
- Guzman A, Tonelli LH, Roberts D, Stiller J, Jackson MA, Soriano JJ, Yousufi S, Rohan KJ, Komarow H, Postolache TT. Mood worsening with high-pollen counts and seasonality: a preliminary report. J Affect Disord. 2007;101:269–274. doi: 10.1016/j.jad.2006.11.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hakko H, Rasanen P, Tiihonen J. Seasonal variation in suicide occurrence in Finland. Acta Psychiatr Scand. 1998;98:92–97. doi: 10.1111/j.1600-0447.1998.tb10048.x. [DOI] [PubMed] [Google Scholar]
- Haukka J, Suominen K, Partonen T, Lönnqvist J. Determinants and outcomes of serious attempted suicide: a nationwide study in Finland, 1996–2003. Am J Epidemiol. 2008;167:1155–1163. doi: 10.1093/aje/kwn017. [DOI] [PubMed] [Google Scholar]
- Hawton K, Bergen H, Casey D, Simkin S. General hospital presentations of non-fatal hanging over a 28-year period: case-control study. Br J Psychiatry. 2008;193:503–504. doi: 10.1192/bjp.bp.107.048561. [DOI] [PubMed] [Google Scholar]
- Kim CD, Lesage AD, Seguin M, Chawky N, Vanier C, Lipp O, Turecki G. Seasonal differences in psychopathology of male suicide completers. Compr Psychiatry. 2004;45:333–339. doi: 10.1016/j.comppsych.2004.06.007. [DOI] [PubMed] [Google Scholar]
- Koskinen O, Pukkila K, Hakko H, Tiihonen J, Vaisanen E, Sarkioja T, Pirrko R. Is occupation relevant in suicide? J Affect Disord. 2002;70:197–203. doi: 10.1016/s0165-0327(01)00307-x. [DOI] [PubMed] [Google Scholar]
- Lester D. Monthly variation in suicide is still strong in the USA. Br J Psychiatry. 2001;179:370. doi: 10.1192/bjp.179.4.370. [DOI] [PubMed] [Google Scholar]
- Lester D, Frank ML. The seasonal variation in suicide in urban and rural areas: comment on Micciolo, Zimmerman-Tansella, Williams and Tansella. J Affect Disord. 1990;19:171. doi: 10.1016/0165-0327(90)90087-o. [DOI] [PubMed] [Google Scholar]
- Lester D, Frank ML. Sex differences in the seasonal distribution of suicides. Br J Psychiatry. 1988;153:115–117. doi: 10.1192/bjp.153.1.115. [DOI] [PubMed] [Google Scholar]
- Linkowski P, Martin F, De Maertelaer V. Effect of some climatic factors on violent and nonviolent suicides in Belgium. J Affect Disord. 1992;25:161–166. doi: 10.1016/0165-0327(92)90001-m. [DOI] [PubMed] [Google Scholar]
- Maes M, Cosyns P, Meltzer HY, De Meyer F, Peeters D. Seasonality in violent suicide but not in nonviolent suicide or homicide. Am J Psychiatry. 1993;150:1380–1385. doi: 10.1176/ajp.150.9.1380. [DOI] [PubMed] [Google Scholar]
- Maes M, Meltzer HY, Suy E, De Meyer F. Seasonality in severity of depression: relationships to suicide and homicide occurrence. Acta Psychiatr Scand. 1993;88:156–161. doi: 10.1111/j.1600-0447.1993.tb03431.x. [DOI] [PubMed] [Google Scholar]
- Maes M, Scharpe S, Verkerk R, D'Hondt P, Peeters D, Cosyns P, Thompson P, De Meyer F, Wauters A, Neels H. Seasonal variation in plasma L-tryptophan availability in healthy volunteers. Relationships to violent suicide occurrence. Arch Gen Psychiatry. 1995;52:937–946. doi: 10.1001/archpsyc.1995.03950230051008. [DOI] [PubMed] [Google Scholar]
- Mann JJ. Neurobiology of suicidal behaviour. Nat Rev Neurosci. 2003;4:819–828. doi: 10.1038/nrn1220. [DOI] [PubMed] [Google Scholar]
- Meares R, Mendelsohn FA, Milgrom-Friedman J. A sex difference in the seasonal variation of suicide rate: a single cycle for men, two cycles for women. Br J Psychiatry. 1981;138:321–325. doi: 10.1192/bjp.138.4.321. [DOI] [PubMed] [Google Scholar]
- Micciolo R, Williams P, Zimmermann-Tansella C, Tansella M. Geographical and urban/rural variation in the seasonality of suicide: some further evidence. J Affect Disord. 1991;21:39–43. doi: 10.1016/0165-0327(91)90017-m. [DOI] [PubMed] [Google Scholar]
- Micciolo R, Zimmermann-Tansella C, Williams P, Tansella M. Seasonal variation in suicide: is there a sex difference? Psychol Med. 1989;19:199–203. doi: 10.1017/s0033291700011156. [DOI] [PubMed] [Google Scholar]
- Morken G, Lilleeng S, Linaker OM. Seasonal variation in suicides and in admissions to hospital for mania and depression. J Affect Disord. 2002;69:39–45. doi: 10.1016/s0165-0327(00)00373-6. [DOI] [PubMed] [Google Scholar]
- Papadopoulos FC, Frangakis CE, Skalkidou A, Petridou E, Stevens RG, Trichopoulos D. Exploring lag and duration effect of sunshine in triggering suicide. J Affect Disord. 2005;88:287–297. doi: 10.1016/j.jad.2005.08.010. [DOI] [PubMed] [Google Scholar]
- Partonen T, Haukka J, Nevanlinna H, Lonnqvist J. Analysis of the seasonal pattern in suicide. J Affect Disord. 2004;81:133–139. doi: 10.1016/S0165-0327(03)00137-X. [DOI] [PubMed] [Google Scholar]
- Petridou E, Papadopoulos FC, Frangakis CE, Skalkidou A, Trichopoulos D. A role of sunshine in the triggering of suicide. Epidemiology. 2002;13:106–109. doi: 10.1097/00001648-200201000-00017. [DOI] [PubMed] [Google Scholar]
- Postolache TT, Stiller JW, Herrell R, Goldstein MA, Shreeram SS, Zebrak R, Thrower CM, Volkov J, No MJ, Volkov I, Rohan KJ, Redditt J, Parmar M, Mohyuddin F, Olsen C, Moca M, Tonelli LH, Merikangas K, Komarow HD. Tree pollen peaks are associated with increased suicide in women. Mol Psychiatry. 2005;10:232–235. doi: 10.1038/sj.mp.4001620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preti A. The influence of seasonal change on suicidal behaviour in Italy. J Affect Disord. 1997;44:123–130. doi: 10.1016/s0165-0327(97)00035-9. [DOI] [PubMed] [Google Scholar]
- Qin P, Agerbo E, Mortensen PB. Suicide risk in relation to socioeconomic, demographic, psychiatric, and familial factors: a national register-based study of all suicides in Denmark, 1981–1997. Am J Psychiatry. 2003;160:765–772. doi: 10.1176/appi.ajp.160.4.765. [DOI] [PubMed] [Google Scholar]
- Qin P, Nordentoft M. Suicide risk in relation to psychiatric hospitalization: evidence based on longitudinal registers. Arch Gen Psychiatry. 2005;62:427–432. doi: 10.1001/archpsyc.62.4.427. [DOI] [PubMed] [Google Scholar]
- Rasanen P, Hakko H, Jokelainen J, Tiihonen J. Seasonal variation in specific methods of suicide: a national register study of 20,234 Finnish people. J Affect Disord. 2002;71:51–59. doi: 10.1016/s0165-0327(01)00411-6. [DOI] [PubMed] [Google Scholar]
- Rihmer Z, Rutz W, Pihlgren H, Pestality P. Decreasing tendency of seasonality in suicide may indicate lowering rate of depressive suicides in the population. Psychiatry Res. 1998;81:233–240. doi: 10.1016/s0165-1781(98)00106-1. [DOI] [PubMed] [Google Scholar]
- Rocchi MB, Sisti D, Miotto P, Preti A. Seasonality of suicide: relationship with the reason for suicide. Neuropsychobiology. 2007;56:86–92. doi: 10.1159/000111538. [DOI] [PubMed] [Google Scholar]
- Rock D, Greenberg DM, Hallmayer JF. Increasing seasonality of suicide in Australia 1970–1999. Psychiatry Res. 2003;120:43–51. doi: 10.1016/s0165-1781(03)00165-3. [DOI] [PubMed] [Google Scholar]
- Ruuhela R, Hiltunen L, Venäläinen A, Pirinen P, Partonen T. Climate impact on suicide rates in Finland from 1971 to 2003. Int J Biometeorol. 2009;2009:53167–53175. doi: 10.1007/s00484-008-0200-5. [DOI] [PubMed] [Google Scholar]
- Silverstone T, Romans S, Hunt N, McPherson H. Is there a seasonal pattern of relapse in bipolar affective disorders? A dual northern and southern hemisphere cohort study. Br J Psychiatry. 1995;167:58–60. doi: 10.1192/bjp.167.1.58. [DOI] [PubMed] [Google Scholar]
- Simkin S, Hawton K, Yip PS, Yam CH. Seasonality in suicide: a study of farming suicides in England and Wales. Crisis. 2003;24:93–97. doi: 10.1027//0227-5910.24.3.93. [DOI] [PubMed] [Google Scholar]
- Souetre E, Wehr TA, Douillet P, Darcourt G. Influence of environmental factors on suicidal behavior. Psychiatry Res. 1990;32:253–263. doi: 10.1016/0165-1781(90)90030-9. [DOI] [PubMed] [Google Scholar]
- Terao T, Soeda S, Yoshimura R, Nakamura J, Iwata N. Effect of latitude on suicide rates in Japan. Lancet. 2002;360:1892. doi: 10.1016/S0140-6736(02)11761-2. [DOI] [PubMed] [Google Scholar]
- Tietjen GH, Kripke DF. Suicides in California (1968–1977): absence of seasonality in Los Angeles and Sacramento counties. Psychiatry Res. 1994;53:161–172. doi: 10.1016/0165-1781(94)90107-4. [DOI] [PubMed] [Google Scholar]
- Yip PS, Chao A, Chiu CW. Seasonal variation in suicides: diminished or vanished. Experience from England and Wales, 1982–1996. Br J Psychiatry. 2000;177:366–369. doi: 10.1192/bjp.177.4.366. [DOI] [PubMed] [Google Scholar]
- Yip PS, Yang KC. A comparison of seasonal variation between suicide deaths and attempts in Hong Kong SAR. J Affect Disord. 2004;81:251–257. doi: 10.1016/j.jad.2003.09.001. [DOI] [PubMed] [Google Scholar]
- Yip PS, Yang KC, Qin P. Seasonality of suicides with and without psychiatric illness in Denmark. J Affect Disord. 2006;96:117–121. doi: 10.1016/j.jad.2006.05.012. [DOI] [PubMed] [Google Scholar]
- Tonelli LH, Hoshina A, Katz M, Postolache TT. Acute stress promotes aggressive like behavior in rats made allergic to tree pollen. Int J Child Health Hum Dev. 2008a;1:305–312. [PMC free article] [PubMed] [Google Scholar]
- Tonelli LH, Stiller J, Rujescu D, Giegling I, Schneider B, Maurer K, Schnabel A, Möller H-J, Postolache TT. Elevated cytokine expression in the orbitofrontal cortex of victims of suicide. Acta Psychiatr Scand. 2008b;117:198–206. doi: 10.1111/j.1600-0447.2007.01128.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tonelli LH, Katz M, Kovacsics CE, Gould TD, Joppy B, Hoshino A, Hoffman G, Komarow H, Postolache TT. Allergic rhinitis induces anxiety-like behavior and altered social interaction in rodents. Brain Behav Immun. 2009 doi: 10.1016/j.bbi.2009.02.017. Webpublished ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valtonen H, Suominen K, Partonen T, Ostamo A, Lönnqvist J. Time patterns of attempted suicide. J Affect Disord. 2006;90:201–207. doi: 10.1016/j.jad.2005.12.004. 2006. [DOI] [PubMed] [Google Scholar]
- World Health Organization (WHO) WHO; [Accessed February, 2009];Suicide prevention (SUPRE) http://www.who.int/mental_health/prevention/suicide/suicideprevent/en/.
- Zung WW, Green RLJ. Seasonal variation of suicide and depression. Arch GenPsychiatry. 1974;30:89–91. doi: 10.1001/archpsyc.1974.01760070067010. [DOI] [PubMed] [Google Scholar]