Abstract
Objectives
Jail incarceration represents an opportunity to deliver HIV counseling and testing (C&T) services to persons at increased risk of infection. However, jails can be chaotic with rapid turnover of detainees. We conducted a pilot study to investigate the feasibility of comparing the effect of different approaches to HIV counseling and testing (C&T) in jail on subsequent HIV risk behaviors among persons testing HIV-negative.
Methods
Consecutive cohorts of newly incarcerated jail detainees were recruited with 132 subjects completing standard HIV C&T as per jail protocol and 132 subjects completing rapid testing with an individualized counseling session. Risk behavior was assessed and compared at baseline and six weeks following jail release.
Results
Among the 264 male participants, pre-incarceration substance use and sexual risk were common. The follow-up visit was completed by 59% of eligible participants. There were no differences in post-release HIV risk behavior between the two arms but there was an overall decrease in risk behavior following jail release for the cohort. In addition, all participants in the rapid arm received rapid HIV test results compared to participants receiving 28% of conventional test results.
Conclusions
Jail incarceration represents an important public health opportunity to deliver HIV C&T. This study demonstrated (1) feasibility in delivering rapid HIV testing combined with individualized counseling to jail detainees, (2) improved test result delivery rates, and (3) success with evaluating risk behaviors during the transition from jail to the community. Further research is needed to determine the optimal approach to HIV C&T in jail with the goal of increasing awareness of HIV serostatus and decreasing HIV risk behavior.
Keywords: HIV counseling and testing, HIV prevention, correctional facilities, jail
Introduction
Correctional facilities represent an important venue for the delivery of HIV C&T services by accessing persons at increased risk of HIV infection and persons who may be marginalized from C&T services in their communities [1–2]. Prior to incarceration, many persons engage in high-risk behaviors including risky sex and substance abuse highlighting the importance of offering HIV testing and prevention services in this setting [3–4]. Jails, which act as the portal of entry to correctional systems, offer an opportunity to deliver C&T services to the majority of persons passing through the correctional system. However, jail incarcerations can be brief creating a challenge for jail-based HIV C&T programs that utilize standard HIV tests which may take days or weeks for test results to be available [5]. With FDA approval of rapid HIV tests, new opportunities for correctional screening programs have emerged.
Jail-based rapid HIV testing can facilitate immediate delivery of results to persons passing through the jail facility. Furthermore, it may be possible to couple negative rapid test results with individualized risk reduction counseling to maximize the HIV prevention impact of the C&T experience for detainees who quickly return to the community. This approach may reduce HIV risk behaviors following release from jail to a greater extent than standard HIV C&T where real-time HIV test results are not available and therefore cannot be combined with counseling.
To investigate the impact of rapid versus standard HIV C&T on HIV risk behaviors following release from jail, we conducted a pilot study that compared rapid HIV testing coupled with a single HIV prevention counseling session to standard HIV C&T with respect to changes in HIV risk behaviors following release from jail. Given the logistical challenges of conducting a study with a jailed population that is transitioning to the community, the objectives of this pilot study included assessing our ability to: 1) conduct rapid HIV testing with a counseling intervention within 48 hours of incarceration; 2) retain study participants following release to the community; 3) conduct a follow-up behavioral assessment in the community; and 4) analyze changes in HIV risk behaviors within the study cohort.
Methods
Recruitment
Males incarcerated at the Rhode Island Department of Corrections (RIDOC) central jail facility were recruited within 48 hours of incarceration by a research assistant. Detainees were randomly selected for participation from jail census rosters using a random number list. Participation was voluntary and informed consent was obtained. During the 10 month recruitment period, participants who received standard HIV C&T only [standard arm (SA)] were enrolled first, followed by participants who received rapid HIV C&T [rapid arm (RA)]. To be eligible for study entry, participants must have provided consent for HIV testing upon jail entry and provided a blood specimen for standard HIV testing per RIDOC protocol. Persons who had enrolled previously in the study and were released and re-incarcerated were not eligible to enroll again. The protocol was approved by the Miriam Hospital institutional review board, the RIDOC Medical Research Advisory Group, and the Office for Human Research Protections of the Department of Health and Human Services.
Baseline Assessment
On the day of enrollment, study participants completed a written baseline quantitative behavioral assessment on the day of enrollment that investigated risk behaviors during the 3 months prior to the current incarceration. The assessment was administered by the research assistant in a private setting within the medical clinic. Quantitative data included: demographics, education, employment, homelessness, health insurance, incarceration history, mental health history, substance abuse treatment, HIV testing history; alcohol use, drug use, and sexual activity (with main partner and non-main partners).
HIV C&T
Subjects in the SA completed standard HIV C&T per RIDOC protocol upon entry to jail. This consisted of routine opt-out HIV testing using a conventional enzyme immunoassay with western blot confirmation. Counseling is limited to interactions with nursing staff at the time of testing and through the HIV testing consent process. More intensive counseling is provided by HIV educators upon request and through educational sessions routinely held within the jail. HIV test results are typically available in 7–10 days. Negative HIV test results are delivered to detainees but not in a standardized or timely manner, yet, detainees can request their test result through the RIDOC medical clinic. Positive results are delivered to the detainee once available if the person is still incarcerated. If already released, the RIDOC notifies the RI Department of Health and an outreach worker contacts the person in the community. With conventional HIV testing, many detainees are released from the RIDOC prior to receiving test results.
Subjects enrolled into the RA were offered rapid HIV testing with the OraQuick® Advance HIV 1/2 rapid HIV test using an oral fluid specimen following completion of the baseline risk assessment. Since participants in the RA completed rapid testing within 48 hours of incarceration, results from conventional HIV testing completed upon intake were not yet available at the time of rapid HIV testing. During the processing of the rapid test, the participant received a single individualized risk reduction counseling session conducted by a research assistant and modeled after the Project RESPECT Brief Counseling Intervention [6]. Rapid HIV test results were delivered following completion of the counseling session. Confirmatory testing and immediate referral to the jail HIV clinical nurse was completed for any participant with a preliminary positive rapid HIV test. At the RIDOC, all persons with confirmed HIV infection receive comprehensive counseling, referral to specialized HIV care within the correctional facility, and linkage to community-based HIV care upon release.
Follow-up assessment
The length of incarceration was assessed for all study subjects by reviewing jail census rosters. Once released from jail, subjects were contacted by phone and/or letter and a follow-up behavioral assessment was scheduled six weeks after release. Participants were not eligible to complete the follow-up visit if: sentenced to prison, still awaiting trial > 6 months after enrollment, re-incarcerated at the time the follow-up assessment was to be conducted, transferred to another facility or deported, withdrew from the study, or found to be HIV-infected. At the follow-up assessment conducted in the community, participants completed a written quantitative behavioral assessment administered by a research assistant that investigated post-release risk behaviors and receipt of standard HIV test results. The extent of counseling received in jail was not quantified beyond what was provided by the research assistant to participants in the RA. Participants received $40 compensation for completing the follow-up risk assessment and compensation for transportation.
Data analysis
The baseline demographic characteristics and HIV risk behaviors of the study population were summarized using median and ranges for continuous and count data, and counts and proportions for categorical data. The risk behaviors were dichotomous or dichotomized as “presence” or “absence”. Characteristics of the SA and the RA were compared using Wilcoxon rank sum tests for continuous and count data and Fisher exact tests for categorical data. Heavy drinking was defined as five or more drinks in a day at least twice a month and drug use was considered to be any reported use of the named substance. Receipt of standard HIV test results was analyzed for participants in both arms and was compared by the Pearson Chi-square test.
Changes in HIV risk behaviors from baseline to study follow-up and the effect of RA compared to SA were assessed using a Markov-chain logistic transition model [7]. The transition model allowed us to examine two transition patterns from baseline to follow-up: 1) maintaining a protective behavior; and 2) correcting a risky behavior. The probabilities of having the two transition patterns in each arm were quantified by the odds, and the effectiveness of RA compared to SA was characterized by odds ratios (OR). The model was adjusted for probation/parole status, length of incarceration, and the time interval between jail release and completing the follow-up visit, by including them as regression covariates in the transition model. Due to sparse outcomes, the model was further adjusted for age (<30, 30−45, > 45), race, education, homelessness, employment status, recidivism (prior lifetime incarcerations < 6, ≥ 6), health insurance status, history of mental health disorder, ever participating in drug treatment, and ever having an HIV test prior to current incarceration, by including them as regression weights through propensity scores [8]. p-values < 0.05 were considered to be statistically significant. Analyses were performed using the statistical package R, version 2.6.1. (R Foundation for Statistical Computing, Vienna, Austria).
Results
Two-hundred and sixty four participants were enrolled from October 2006-July 2007 with 132 in each arm. Baseline characteristics (Table 1) were similar between the SA and the RA except SA participants were slightly older (median of 32 years vs. 29 years, p=0.03) and had a slightly higher proportion reporting ever participating in a drug treatment (62% vs. 49%, p=0.05), respectively. Lifetime recidivism with the correctional system was common with the median number of incarcerations being 7 and 6 for the SA and RA, respectively.
Table 1.
Baseline characteristics of the study population by arm: standard HIV testing or rapid HIV testing
| Standard arm (n=132) a |
Rapid arm (n=132) b |
p value c | ||||
|---|---|---|---|---|---|---|
| 1. Demographics | ||||||
| Age: median (range) | 32 (18–58) | 29 (19–65) | .03 | |||
| Race | Caucasian | 70 | 53% | 66 | 50% | .38 |
| African American | 32 | 24% | 25 | 19% | ||
| Hispanic | 17 | 13% | 20 | 15% | ||
| Other | 13 | 10% | 21 | 16% | ||
| Education | did not finish high school | 68 | 52% | 67 | 51% | .99 |
| Homeless | Ever | 69 | 52% | 59 | 45% | .27 |
| prior 3 months | 35 | 27% | 36 | 27% b | .89 | |
| Lifetime incarcerations: median (range) | 7 (1–200) | 6 (1–70) | .77 | |||
| Working | prior 3 months | 101 | 77% | 89 | 67% | .13 |
| 2. Insurance, mental health & drug treatment | ||||||
|
Health insurance |
prior 3 months | 43 | 33% | 40 | 31% b | .17 |
| Mental health | ever diagnosed with mental health disorder | 43 | 33% | 47 | 36% | .70 |
| ever taken medication for mental health disorder | 56 | 42% | 48 | 36% | .38 | |
|
Drug Treatment |
ever participated in drug or alcohol treatment program | 82 | 62% | 65 | 49% | .05 |
| drug or alcohol treatment program within prior 3 months | 23 | 17% | 23 | 18% b | .99 | |
| 3. HIV testing history | ||||||
| Number of times tested for HIV: median (range) | 5 (1–60) | 5 (1–50) | .92 | |||
|
Receipt of past HIV test results |
Never | 47 | 36% a | 76 | 58% | <.01 |
Missing data on the Standard Arm: ‘Have received test results?’ [Data not available (NA) = 1]
Missing data on the Rapid arm: ‘Homeless within the priors three months?’ (NA = 1); ‘Health insurance within the prior three months?’ (NA = 4); ‘Participate drug or alcohol treatment program within the prior three months?’ (NA = 2)
Wilcoxon rank sum tests are used to compare age, the numbers of lifetime incarcerations, and the numbers of HIV tests. The Fisher exact tests are used to compare the rest
There were no significant differences between the SA and RA participants in self-reported HIV risk during the three months prior to incarceration (Table 2). Recent substance use and sexual activity without condoms was common. In each arm, approximately 40% reported recent cocaine use and 10% heroin use. Approximately 20% of the cohort reported ever injecting drugs with 8% reporting recent injection. Recent sexual activity was reported by 233 participants overall (88%). Of those, 80% reported not using a condom at their last sexual encounter and 26% reported having at least 3 sexual partners within the past 3 months. Condom use with main partners was infrequent. One-hundred and eleven participants reported having recent non-main sexual partner/s and of those having vaginal sex, 36% reported never using a condom; of those having anal sex, 56% reported never using condoms.
Table 2.
Pre-incarceration HIV risk behavior of the study population by arm: standard HIV testing or rapid HIV testing
| Standard arm (n=132) |
Rapid arm (n=132) |
Total (N=264) |
p value g | ||||
|---|---|---|---|---|---|---|---|
| 1. Pre-incarceration alcohol use | |||||||
|
Alcohol use within prior 3 months |
heavy drinking a | 48 | 36% | 55 | 42% | 39% | .45 |
| 2. Pre-incarceration drug use | |||||||
|
Drug use within prior 3 months |
Cocaine | 52 | 40% b | 48 | 36% | 38%d | .61 |
| Heroin | 12 | 9% b | 15 | 11% | 10% d | .69 | |
| Methamphetamines | 2 | 2% b | 1 | 1% | 1% d | .62 | |
| Marijuana | 77 | 59% b | 84 | 64% | 61% d | .45 | |
| prescription meds | 38 | 29% b | 36 | 27% | 28% d | .79 | |
| other street drugs | 17 | 13% b | 12 | 9% | 11% d | .33 | |
| Injection drug use | Ever | 27 | 21% b | 22 | 17% | 19% d | .43 |
| prior 3 months | 10 | 8% b | 12 | 9% | 8% d | .82 | |
| 3. Pre-incarceration sexual history | |||||||
|
Sexual history within prior 3 months |
sex within prior 3 months | 114 | 88% b | 119 | 92% c | 90% d | .14 |
| >= 3 sexual partners | 29 | 25% e | 32 | 27% f | 26% | .88 | |
| exchange sex for drugs/money | 5 | 4% e | 8 | 7% f | 6% | .57 | |
| no condom use at last sexual encounter | 91 | 80% e | 95 | 90% f | 20% | .99 | |
|
With a main sexual partner (n=203) |
have vaginal sex within prior 3 months | 96/96 | 100% b | 106/106 | 100% | 100% d | 1.0 |
| never use condom | 80/96 | 83% | 90/106 | 85% | 84% | .47 | |
| have anal sex within prior 3 months | 23/97 | 24% | 18/106 | 17% | 20% | .29 | |
| never use condom | 19/23 | 83% | 16/18 | 89% | 85% | .68 | |
|
With a non-main sexual partner (n=111) |
have vaginal sex within prior 3 months | 52/55 | 95% b | 51/53 | 96% | 95% d | .99 |
| never use condom | 19/52 | 37% | 18/51 | 35% | 36% | .43 | |
| have anal sex within prior 3 months | 10/58 | 17% | 6/53 | 11% | 14% | .62 | |
| never use condom | 4/10 | 40% | 5/6 | 83% | 56% | .20 | |
Heavy drinking defined as ≥ 5 drinks in one day ≥ 2 times/month
Missing data on the Standard Arm: Drug use of cocaine, heroin, etc [Data not available (NA) = 1]; injection drug use (NA = 1); have sex within prior 3 months before incarceration (NA=2); have vaginal sex with a main partner (NA=1); have vaginal sex with a non-main partner (NA=3)
Missing data on the Rapid Arm: have sex within prior 3 months before incarceration (NA=2)
Missing data for Total Cohort: Drug use of cocaine, heroin, etc (NA=1); have sex within prior 3 months before incarceration (NA=4); have vaginal sex with a main partner (NA=1); have vaginal sex with a non-main partner (NA=3)
Among those having sex within prior 3 months before incarceration (n = 114)
Among those having sex within prior 3 months before incarceration (n = 119)
The p values are calculated using the Fisher exact tests
All participants in the RA received rapid HIV test results at the time of testing. Receipt of standard HIV test results was assessed at the follow-up visit. There was one newly diagnosed HIV-infected participant in the RA who was released from jail prior to learning of his confirmed diagnosis. He was contacted in the community by a Department of Health outreach worker, notified of his HIV serostatus, and was referred to treatment. One participant in the SA tested positive for HIV but was later identified as a known chronic infection.
The follow-up visit was completed by 58 (44%) in the SA and 50 (38%) in the RA, (Pearson Chi-square p=0.31, Figure 1). Of those eligible to complete the follow-up (183/284), completion rates were 68% (58/85) and 51% (50/98) for the SA and RA, respectively (Pearson Chi-square p=0.02) with 75 being lost-to-follow-up. Eighty-one participants were not eligible to complete the follow-up assessment for the following reasons: sentenced to prison (57%); re-incarcerated (14%); awaiting trial for > 6 months (10%); transferred to another facility (9%); withdrew from the study (7%); found to be HIV-infected (2%); and deported (1%). Participants who completed the follow-up visit were compared to those that did not and were more likely to have ever been homeless (59% vs. 41%; p<0.01), homeless within prior 3 months (38% vs.19%; p<0.01), and had a greater number of lifetime incarcerations [7 (range 1–200) vs. 6 (range 1–100), p=0.02], respectively. There were no significant differences in baseline HIV risk behaviors between those that did and did not complete the follow-up visit. Twenty-eight percent (30/108) of those who completed the follow-up visit received results from their standard HIV test conducted within the RIDOC with no significant difference between the RA (31%) and SA (26%) groups (p=0.29).
Figure 1.
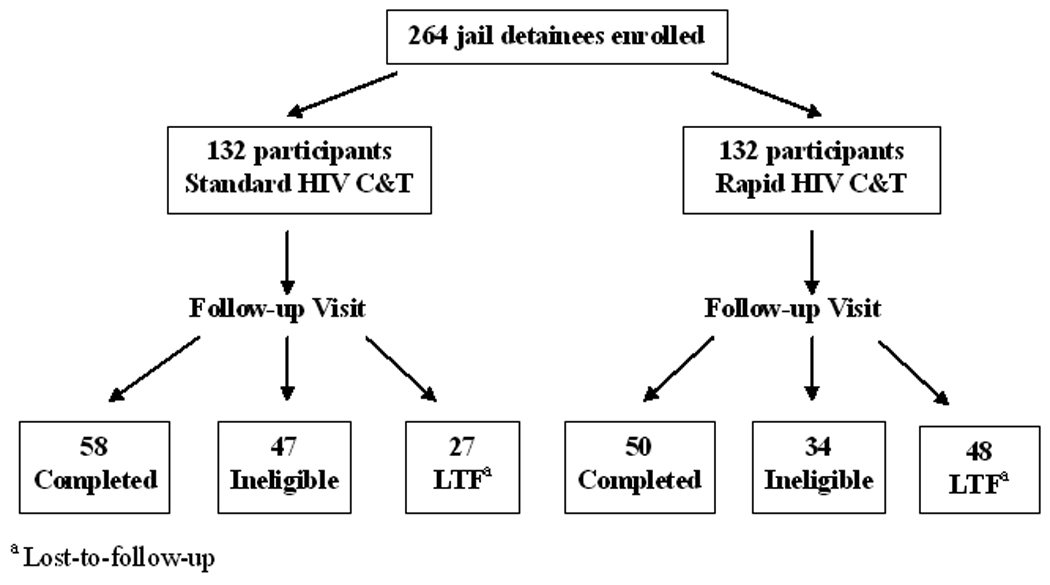
Participant disposition and follow-up
The transition model analysis (Table 3) was limited to the 108 participants who completed follow-up visits and included two sub-analyses using the Markov logistic transition model. Analysis 1 examined ‘maintaining a protective behavior’ for participants that reported absence of a particular risk behavior at baseline. Analysis 2 examined ‘correcting a risky behavior’ for participants that reported engaging in a particular risk behavior at baseline. Table 3 shows the total number of participants reporting either the absence or presence of a particular risk behavior at the follow-up visit in comparison to baseline reporting. For example, for cocaine use in Analysis 1, 32 participants in the standard arm who completed the follow-up visit reported no cocaine use at baseline. Two of these participants reported using cocaine since jail release and 30 still reported no cocaine use at the follow-up visit. For cocaine use in Analysis 2, 20 participants in the rapid group reported using cocaine at baseline. Of these, 9 reported no cocaine use at the follow-up visit and 11 reported continued use since jail release. The odds ratios comparing the RA to SA for each risk behavior are shown in columns OR0 (starting a risky behavior) and OR1 (correcting a risky behavior) with associated p-values. Compared to the standard HIV C&T arm, the rapid HIV C&T intervention would be more effective in preventing initiation of a risky behavior if OR0 was less than 1 (Analysis 1), and would be more effective in correcting a risky behavior if OR1 was greater than 1 (Analysis 2).
Table 3.
Transition model analysis of HIV risk behavior among those completing follow-up stratified by arm
| Analysis 1 | Analysis 2 | |||||||
|---|---|---|---|---|---|---|---|---|
| Starting a risky behavior | Correcting a risky behavior | |||||||
| a: # engaging in risky behavior at follow-up b: # reporting absence of behavior at follow-up a+b: total # reporting absence of behavior at baseline |
c: # reporting absence of behavior at follow-up d: # engaging in behavior at follow-up c+d: total # reporting engaging in behavior at baseline |
|||||||
| HIV-risk behaviors | Standard arm | Rapid arm | OR0 (p value) a | Standard arm | Rapid arm | OR1 (p value) a | ||
| Substance use: | a/b | a/b | c/d | c/d | ||||
| Cocaine use | 2/30 | 1/29 | 0.42, (.53) | 19/6 | 9/11 | 0.26, (.06) | ||
| Heroin use | 0/49 | 0/45 | - | 7/1 | 2/3 | 0.07, (.10) | ||
| Injection drug use | 0/51 | 0/46 | - | 6/0 | 2/2 | - | ||
| Heavy drinking | 5/30 | 3/25 | 0.5, (.41) | 10/13 | 10/11 | 1.1, (.85) | ||
| Sexual behaviors: | ||||||||
| No condom use during vaginal, anal sex with any partner |
0/1 | 1/1 | - | 2/33 | 6/25 | 4.3, (.08) | ||
| No condom at last sexual encounter |
3/2 | 3/2 | 1.02, (.99) | 5/27 | 4/25 | 1.0, (0.99) | ||
No statistically significant differences were found in the transition analysis. The rapid HIV C&T intervention was not found to reduce HIV risk behavior following release compared to standard HIV C&T. There was an overall decrease in substance use and sexual risk behavior after jail release in both arms with the following proportions of participants not resuming a risk behavior since jail release: 62% (28/45) cocaine use; 69% (9/13) heroin use; 80% (8/10) injection of any drug; 45% (20/44) heavy alcohol use; 12% (8/66) unprotected vaginal or anal sex with any partner; and, 15% (9/61) no condom use at last sexual encounter.
Discussion
This pilot study examined whether individualized HIV prevention counseling could be successfully coupled with rapid HIV testing in jail and whether persons who completed HIV C&T in jail could be followed into the community in order to investigate changes in HIV risk behaviors. Incarceration represents an opportune time to deliver HIV testing and prevention services to persons at increased risk of infection since accessing this population in the community can be difficult due to active substance abuse, mental illness, homelessness, and disparities in health care. Rapid HIV testing is increasingly being utilized in jails given the transient nature of this population and the need to expand HIV screening [9]. Given recent challenges in developing successful HIV prevention interventions, the need for effective primary prevention interventions for high-risk persons has become a priority [10].
This study confirms that jail detainees engage in HIV risk behaviors prior to incarceration. Sexual risk was frequent among study participants. Close to 40% of study participants were active cocaine users or heavy drinkers, both of which have been associated with HIV infection [11–12]. Interestingly, the rate of IDU was relatively low and may be reflective of an overall decline in IDU in Rhode Island as a whole. New HIV diagnoses related to IDU in Rhode Island have steadily declined since the early 1990’s [13]. These findings support the implementation of HIV prevention interventions in jail focusing on increasing condom use and decreasing HIV risk related to substance use.
We were successful in conducting rapid HIV testing in combination with an individualized counseling session for recently incarcerated detainees. All participants who completed rapid HIV testing received rapid HIV test results whereas less than 30% of participants who completed the follow-up visit received results from their standard HIV test. This finding supports the use of rapid HIV testing in jails where brief incarcerations are common for many detainees. Real-time delivery of rapid HIV test results will enable detainees to learn their HIV status and may help to efficiently link HIV-infected persons to HIV care. While we were able to provide individualized counseling during the processing of the rapid HIV test, this approach may present challenges to jail facilities. Individualized counseling requires time and a private setting, both of which may be limited given jails often operate at or above census capacity. Further studies are needed to examine the integration of individualized counseling services into HIV testing programs.
Forty-one percent of the entire cohort and in 59% of those eligible completed the follow-up assessment. There were challenges with evaluating risk behaviors among persons exiting jails. Thirty-one percent of the subjects were ineligible for the follow-up visit most commonly due to incarceration greater than 6 months. To limit the overall length of the study, individuals who were incarcerated greater than 6 months were excluded from the follow-up assessment. Our follow-up visit completion rate was similar to other studies where participants have been followed from the incarcerated setting to the community [14], although higher retention rates have been observed with more intensive multi-session interventions that utilized more elaborate methods for tracking subjects in the community [15]. In future studies, follow-up rates could be maximized by recruiting participants who would be expected to be released within a brief period of time, such as those with misdemeanor charges. This study did not take into account criminal charge in the recruitment process. Our follow-up completion rate of 59% of those eligible with only one interaction in jail prior to the single follow-up assessment in the community suggests that further studies utilizing jail-based interventions are possible.
There were limitations related to the study design that may have introduced bias including non-randomization and reliance on participant’s self-report of risk behaviors. In addition to potential recall bias, participants may have been reluctant to reveal true risk behaviors in the jail setting thus underestimating actual HIV risk. Given this was a pilot study; we only conducted a one-time follow-up visit six weeks following jail release. To better assess HIV risk behaviors in the community, assessments should be conducted greater than 6 weeks after release and other predictors of risk behavior, such as court-ordered drug testing or substance abuse treatment, and probationary status, should be investigated. Finally, this study did not demonstrate greater effectiveness of the RA compared to the SA with respect to post-release HIV risk behaviors; however, as a pilot study, it was not adequately powered to do so. Therefore, conclusions about the efficacy of rapid testing combined with individualized counseling on post-release HIV risk behaviors cannot be made from the results of this study.
Jail incarceration provides a public health opportunity to deliver rapid HIV testing in combination with HIV prevention services to persons at increased risk of infection and to those who may be marginalized from HIV services in their communities. Ideally, a brief, yet effective counseling intervention could be coupled with rapid testing thus facilitating efficient diagnosis as well as risk reduction among those receiving it. The study was successful in combining an individualized risk reduction counseling session with rapid HIV testing that was completed within 48 hours of jail incarceration. In addition, this study demonstrated feasibility with investigating HIV risk behaviors following release from jail. Future studies with larger cohorts and optimized follow-up rates will be needed to determine the efficacy of jail-based HIV testing and prevention interventions designed to increase knowledge of HIV serostatus and decrease HIV risk behavior among those most in need.
Acknowledgments
Sources of support:
This research was supported by the Lifespan/Tufts/Brown Center for AIDS Research (grant P30AI42853). In addition, C. Beckwith received support from the National Institute on Drug Abuse (grant K23DA021095 and grant 5T32DA013911) and L. Bazerman and T. Flanigan received support from the Tufts Nutrition Collaborative, A Center for Drug Abuse and AIDS Research (grant P30DA013868).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Spaulding A, Stephenson B, Macalino G, et al. Human Immunodeficiency Virus in correctional facilities: a review. Clin Infect Dis. 2002;35:305–312. doi: 10.1086/341418. [DOI] [PubMed] [Google Scholar]
- 2.Conklin TJ, Lincoln T, Flanigan TP. A public health model to connect correctional health care with communities. Am J of Pub Health. 1998;88:1249–1250. [PubMed] [Google Scholar]
- 3.Mumola CJ. Substance abuse and treatment of state and federal prisoners, 1997: Bureau of Justice Statistics Bulletin. Washington, DC: Office of Justice Programs, US Department of Justice; 1999. NCJ 172871. [Google Scholar]
- 4.Stephenson BL, Wohl DA, McKaig R, et al. Sexual behaviours of HIV-seropositive men and women following release from prison. Int J STD AIDS. 2006;17:103–108. doi: 10.1258/095646206775455775. [DOI] [PubMed] [Google Scholar]
- 5.Cohen TH, Reaves BA. Felony defendants in large urban counties, 2002: Bureau of Justice Statistics Bulletin. Washington, DC: Office of Justice Programs, US Department of Justice; 2006. NCJ 210818. [Google Scholar]
- 6.Kamb ML, Fishbein M, Douglas JM, Jr, et al. Efficacy of risk-reduction counseling to prevent human immunodeficiency virus and sexually transmitted diseases: a randomized controlled trial. Project RESPECT Study Group. JAMA. 1998;280:1161–1167. doi: 10.1001/jama.280.13.1161. [DOI] [PubMed] [Google Scholar]
- 7.Diggle PJ, Heagerty P, Liang KY, Zeger SL. Analysis of Longitudinal Data. Second edition. Oxford, England: Oxford University Press; 2005. [Google Scholar]
- 8.Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70:41–55. [Google Scholar]
- 9.Macgowan R, Margolis A, Richarson-Moore A, et al. Voluntary rapid human immunodeficiency virus (HIV) testing in jails. Sex Transm Dis. 2009;36(2 Suppl):S9–S13. doi: 10.1097/OLQ.0b013e318148b6b1. [DOI] [PubMed] [Google Scholar]
- 10.Coates TJ, Richter L, Caceres C. Behavioural strategies to reduce HIV transmission: How to make them work better. Lancet. 2008;372:669–684. doi: 10.1016/S0140-6736(08)60886-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Edlin BR, Irwin KL, Faruque S, et al. Intersection epidemics – crack cocaine use and HIV infection among inner city young adults. Multicenter Crack Cocaine and HIV Infection Study Team. N Engl J Med. 1994;331:1422–1427. doi: 10.1056/NEJM199411243312106. [DOI] [PubMed] [Google Scholar]
- 12.Shillington AM, Cottler LB, Compton WM, 3rd, Spitznagel EL. Is there a relationship between “heavy drinking” and HIV high risk sexual behaviors among general population subjects? Int J Addict. 1995;30:1453–1478. doi: 10.3109/10826089509055842. [DOI] [PubMed] [Google Scholar]
- 13.Beckwith CG, Moreira CC, Aboshady HM, et al. A success story: HIV prevention for injection drug users in Rhode Island. Subst Abuse Treat Prev Policy. 2006;1:34. doi: 10.1186/1747-597X-1-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Grinstead O, Zack B, Faigeles B. Reducing postrelease risk behavior among HIV seropositive prison inmates: the health promotion program. AIDS Educ Prev. 2001;13:109–119. doi: 10.1521/aeap.13.2.109.19737. [DOI] [PubMed] [Google Scholar]
- 15.Wolitski RJ. Relative efficacy of a multisession sexual risk-reduction intervention for young men released from prisons in 4 states. Am J Public Health. 2006;96:1854–1861. doi: 10.2105/AJPH.2004.056044. [DOI] [PMC free article] [PubMed] [Google Scholar]


