Abstract
Objectives. We sought to identify cross-sectional hepatitis B virus (HBV) and HCV prevalence among Asian Americans at a community health fair and to assess referral rates.
Methods. We determined HBV prevalence with hepatitis B surface antigen (HBsAg), antibodies to hepatitis B core antigen (anti-HBc), and antibodies to hepatitis B surface antigen (anti-HBs). We determined HCV prevalence with hepatitis C antibodies. Successful referral occurred when participants with HBV or HCV were contacted, medically evaluated, and given contact information of liver specialists for care.
Results. Of 202 people screened, 118 were Asian Americans (65 Chinese and 39 Vietnamese). Twelve had chronic HBV with positive HBsAg. However, chronic HBV prevalence increased from 10.2% to 13.6% by concomitant HBsAg, anti-HBc, and anti-HBs testing. Prevalence of HCV was 6% overall but 15.4% among Vietnamese. Overall, 83% of patients with chronic HBV and 100% of patients with occult HBV or HCV were successfully referred.
Conclusions. Concomitant HBsAg, anti-HBc, and anti-HBs testing permits diagnosis of chronic, occult HBV infections missed by testing with HBsAg alone. Persons identified with HBV or HCV at community health fairs can be successfully referred.
Hepatitis B virus (HBV) is a known cause of acute and chronic liver disease, and chronic infection is associated with hepatocellular carcinoma (HCC), regardless of the presence or absence of cirrhosis.1 Worldwide, 53% of HCC cases are attributed to chronic HBV infection.2 Approximately 75% of all people with chronic HBV infection live in Asia,2 where the high prevalence of HBV infection is attributable to vertical transmission from infected mother to newborn and horizontal transmission during early childhood.3
Asian immigrants to the United States and their families have an increased prevalence of HBV infection and chronic liver disease.4 However, Asian Americans are often underrepresented in population-based studies of HBV5 or combined with other groups to form an “other” category.6 Thus, cross-sectional prevalence studies at screening fairs have become a routine source of information about the prevalence of HBV infection among Asian Americans; such studies have indicated a prevalence of approximately 6% to 15%.5 This range shows unequivocally that Asian Americans have the highest rate of HBV infection in the United States.
HCV infection is also associated with acute and chronic liver disease, and in patients with cirrhosis, the incidence of HCC ranges from 3% to 5% per year. Cirrhosis caused by HCV infection appears to cause 25% of HCC cases worldwide.2 Many Asians are at risk for acquiring HCV infection through unsanitary medical practices during childhood or contaminated blood transfusions.3 The prevalence of HCV infection is approximately 2.5% among healthy adults in Asia7; however, rates of 5.6% in Thailand and 6.1% in Vietnam have been reported.3 Investigation of the prevalence of HCV in Asian Americans has been limited by small numbers of Asian American study participants in prior studies.3,8–11 To our knowledge, HCV screening has not been routinely included in Asian American community–based screening efforts.
Screening recommendations for HBV and HCV12–14 advocate early detection so that patients can start effective antiviral therapies and reduce the risk of HCC.12,13,15 Because chronic HBV and HCV infections are usually asymptomatic, active screening is important to early detection. Individuals with HBV and HCV should be referred to liver specialists for hepatitis treatment and screening for HCC. To detect HCC in patients with HBV or HCV, liver specialists may use α-fetoprotein and periodic ultrasonography or other imaging studies of the liver.14 Detection of HCC at a potentially treatable stage has been shown to improve survival.14,16,17 Little is known about the HCV screening rates among Asian Americans. Although Asian Americans have a high prevalence of HBV, only 38% to 66% of select Asian Americans surveyed reported that they had been screened for HBV.18–21 As universal HBV immunization is recommended for all children and for adults at risk for HBV, Asian Americans who test negative for HBV should be offered HBV immunization.4,22
Although cross-sectional hepatitis virus screening studies have provided useful information about hepatitis among Asian Americans, several key issues remain to be addressed. First, many screening fairs have relied on testing of only hepatitis B surface antigen (HBsAg), which misses those with occult HBV infection who have isolated antibodies to hepatitis B core antigen (anti-HBc) with subdetectable levels of HBsAg, those with convalescent markers of both antibodies to hepatitis B surface antigen (anti-HBs) and anti-HBc, and those with anti-HBs alone as a result of HBV vaccination. The prevalence of HBV infection can be ascertained accurately by using all 3 tests: HBsAg, anti-HBs, and anti-HBc. Second, screening fairs for Asian Americans have had testing for HBV infection but have neglected HCV infection. Third, although screening fairs have provided the results for hepatitis markers, it is unclear whether the communication of results has led to referral for subsequent health care.
We performed comprehensive serological screening for HBV and HCV during a 1-day local health fair for Asian Americans in Houston, Texas, to determine the prevalence of these infections. We hypothesized that the use of the anti-HBc test would increase the identification of HBV in this population through the detection of occult HBV. Our results permitted us to define the cross-sectional prevalence of HBV and HCV infections and to evaluate the effectiveness of referrals for further health care among persons testing positive for HBV or HCV.
METHODS
On August 5, 2006, in Houston, Texas, a free HBV and HCV screening was offered at the Houston Alief Community Health Fair. The screening program was sponsored by (1) Advanced Liver Therapies, a clinical research unit at St Luke's Episcopal Hospital affiliated with Baylor College of Medicine; (2) Texas Liver Coalition, a nonprofit organization providing education and support to patients with liver disease and community hepatitis screening; (3) the Asian American Health Coalition's Helping Other People Through Encouragement (HOPE) Clinic, a community health clinic serving the medical needs of Houston Asian Americans; and (4) the University of Texas M. D. Anderson Cancer Center, a National Cancer Institute–designated comprehensive cancer center. Awareness of this event was promoted through Chinese- and Vietnamese-language announcements posted approximately 2 weeks beforehand in community centers and public areas and through advertisements on local Chinese and Vietnamese radio stations and newspapers.
All adults at the health fair who desired testing were screened; however, only Asian Americans were included in this analysis. Participants acknowledged their ethnicity and language preference on the demographic questionnaire. Prior to phlebotomy, participants signed an informed consent form available in English, Chinese, and Vietnamese. Participants also completed a demographic information sheet with their contact information. Each participant received printed educational materials about HBV and HCV in English, Chinese, or Vietnamese.
Serologic Evaluations
At the screening event, blood was drawn by Quest Laboratories phlebotomists and transported to Quest Laboratories according to the company's standard policies. Participants' blood was initially tested for HCV with an anti-HCV enzyme-linked immunosorbent assay (Ortho, Raritan, NJ). We considered all individuals with a positive anti-HCV test result, defined as signal to cut-off ratio greater than 1, to have possible HCV infection. These patients later underwent follow-up confirmatory testing for HCV RNA with a qualitative polymerase chain reaction (PCR; Roche Molecular Diagnostics, Pleasanton, CA) with lower limit of detection of 50 IU/mL.
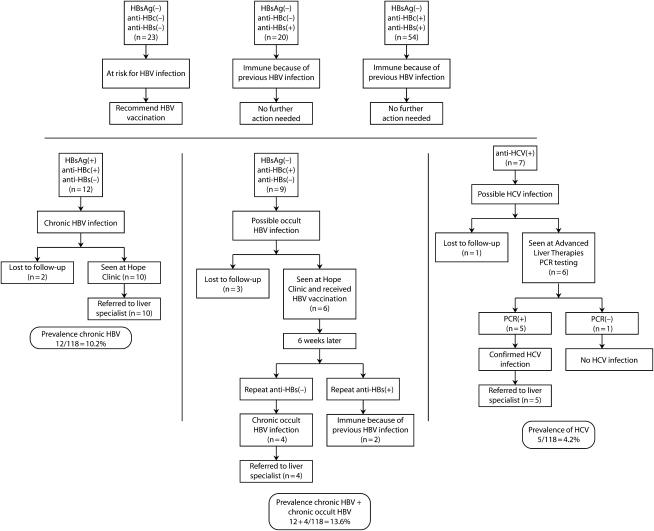
Participants' sera were tested for HBsAg, anti-HBc, and anti-HBs. The HBsAg and anti-HBc tests were qualitative, indicating the presence or absence of the markers. We considered all patients with positive HBsAg and anti-HBc tests to have chronic HBV infection. The anti-HBs test (Quest Laboratories, Houston, TX) was quantitative, and levels less than 5 mIU/mL were considered undetectable. Patients with an isolated positive anti-HBs test were immune because of previous HBV vaccination. We considered patients with positive anti-HBc and anti-HBs tests to be immune because of convalescence from previous HBV infection. Persons convalescent from a prior HBV infection may test positive only for anti-HBc because of a decline in anti-HBs to subdetectable levels; thus, all persons with an isolated positive anti-HBc received a single dose of HBV vaccine (Merck, Whitehouse Station, NJ) at the HOPE Clinic to stimulate an amnestic response for anti-HBs. Six weeks after immunization, anti-HBs was retested at the HOPE Clinic and subsequently analyzed at a different lab (LabCorp), where anti-HBs levels of less than 3 mIU/mL were considered negative. The appearance of detectable anti-HBs levels indicated convalescence from prior HBV infection, whereas continued negativity for anti-HBs was classified as indicating possible occult HBV infection. We considered patients who had negative hepatitis B tests to be at risk for HBV infection (Figure 1).
FIGURE 1.
Interpretations of outcomes of serologic hepatitis testing: Alief Community Health Fair, Houston, TX, 2006.
Notes. anti-HBc = antibodies to hepatitis B core antigen; anti-HBs = antibodies to hepatitis B surface antigen; HBsAg = hepatitis B surface antigen; HBV = hepatitis B virus; PCR = polymerase chain reaction.
Interventions
Patients with chronic HBV or HCV were contacted by phone, and a follow-up appointment was scheduled at either the HOPE Clinic for HBV patients or Advanced Liver Therapies for HCV patients. There, the project physician (J. H.) and project staff informed participants of their test results and answered all questions. They recorded patient information in the medical record, including age, ethnicity, medical insurance status, history of hepatitis, treatment received for hepatitis, family history of hepatitis or cancer, and hepatitis vaccination. Patients with hepatitis were referred for further medical care by providing the contact information of local liver specialists who agreed to see these patients. Patients were also encouraged to apply for the county system health care, and the HOPE Clinic provided case management assistance. We did not confirm a patient's access to care because they were being referred to various private and public clinics.
All participants received a letter in English explaining their HBV and HCV status based on their test results. Chinese and Vietnamese participants also received a translated version of the letter in their native language prepared by official translators at M. D. Anderson Cancer Center. All other Asian American participants were contacted by phone in their native language to ensure that they understood the English letter. The content of the letters was individualized according to each patient's serologic test results, as outlined in Figure 1. Patients at risk for HBV were instructed to start and complete a 3-shot series for HBV vaccination. They received a list of community clinics where HBV vaccinations were available. Patients who had chronic or possible occult HBV infection were invited to the HOPE Clinic, and patients with possible HCV infection were invited to Advanced Liver Therapies.
At these 2 centers, we asked patients about their family history of hepatitis and liver cancer. Specifically, we asked whether family members such as spouse, children, parent, or any other relatives had ever been tested for hepatitis, if they had been told by a medical provider that they had hepatitis, or whether they had received a hepatitis vaccination in the past. Patients were also asked if any of their family members were told that they had liver cancer. Confidentiality was maintained by storing all patient information and printed materials in locked file cabinets at HOPE Clinic, Advanced Liver Therapies, and M. D. Anderson Cancer Center. All electronic data were maintained on a secure server at M. D. Anderson Cancer Center.
Chronic HBV infection.
At HOPE Clinic, participants with chronic HBV infection were referred to liver specialists in the community or in the Harris County Hospital District (HCHD) for follow-up and treatment. Our project team engaged several local liver specialists to see patients at discounted rates. For patients without an HCHD card, the case manager assisted patients in completing their paperwork to establish eligibility for HCHD services.
Possible occult HBV infection.
At HOPE Clinic, participants with possible occult HBV infection were informed that their test result could mean that they had had a previous HBV infection or that they might still have an occult infection. Participants received the HBV vaccine, and those with negative anti-HBs on repeat testing were referred for further care.
Possible HCV infection.
Individuals with possible HCV infection were evaluated by medical staff at Advanced Liver Therapies. There, they were informed that their screening test indicated past or current HCV infection, and they were offered a free confirmatory HCV RNA test. If HCV RNA was detected with PCR, further free testing was performed to determine the HCV genotype, and the individual was informed that he or she had chronic HCV infection and was referred to a hepatologist for further care.
Data Analysis
We used Microsoft Excel and Access to create a patient information database. We used SPLUS version 7.0 (Insightful Corporation, Seattle, WA) SAS version 9.1 (SAS Institute Inc, Cary, NC) to analyze the data. We used descriptive data analysis to explore the data, including disease type, frequency, or proportions. We used Fisher exact test to assess an association between 2 categorical variables. We considered P ≤ .05 statistically significant.
RESULTS
More than 1000 people attended the Houston Alief Health Fair, and 202 consented to be tested for markers of HBV and HCV. Those consenting included 118 Asian Americans, 52 Latinos, 15 African Americans, and 2 Whites. Fifteen individuals did not report their race/ethnicity. Of the Asian American participants, 71 (60%) were female. Sixty-five (55%) were Chinese American, 39 (33%) were Vietnamese American, 3 (3%) were Filipino, and 11 (9%) identified their ethnicity as “Asian.” The median age was 55 years (range = 21–83 years). Characteristics of the Asian Americans with chronic HBV infection and possible HBV or HCV infection are reported in Table 1.
TABLE 1.
Characteristics of 28 Asian American Participants, by HBV or HCV Infection Status: Alief Community Health Fair, Houston, TX, 2006
| Characteristics | Chronic HBV Infection (n = 12), No. (%) or Median (Range) | Convalescent or Occult HBV Infection (n = 9), No. (%) or Median (Range) | Possible HCV Infection (n = 7), No. (%) or Median (Range) |
| Gender | |||
| Men | 3 (25) | 2 (22) | 6 (86) |
| Women | 9 (75) | 7 (78) | 1 (14) |
| Age, y | 54 (36–71) | 57 (45–68) | 54 (41–74) |
| Ethnicity | |||
| Chinese | 7 (58) | 7 (78) | 0 |
| Vietnamese | 4 (33) | 1 (11) | 6 (86) |
| Other Asian | 1 (8) | 1 (11) | 1 (14) |
| Insurance | |||
| Medicare/Medicaid | 0 | 0 | 0 |
| Commercial | 0 | 2 (22) | 2 (29) |
| County hospital | 0 | 0 | 2 (29) |
| None | 12 (100) | 7 (78) | 3 (42) |
| Previous hepatitis infection | |||
| Yes | 1 (8) | 1 (8) | 3 (43) |
| No | 11 (92) | 8 (89) | 4 (57) |
| Previous hepatitis type | |||
| HBV | 1 (8) | 1 (11) | 0 |
| HCV | 0 | 0 | 3 (43) |
| None | 11 (92) | 8 (89) | 4 (57) |
| Previous treatmenta | |||
| Yes | 0 | 0 | 3 (43) |
| No | 12 (100) | 9 (100) | 4 (57) |
| Pharmacy coverageb | |||
| Yes | 0 | 0 | 2 (29) |
| No | 12 (100) | 8 (89) | 5 (71) |
| Do not know | 0 | 1 (11) | 0 |
| Gold card statusc | |||
| Card available | 0 | 1 (11) | 2 (29) |
| None | 12 (100) | 8 (89) | 5 (71) |
Note. HBV = hepatitis B virus.
All 3 patients who had previously received treatment were treated in the United States.
Insurance coverage for medications.
Gold card allows access to the Harris County, Texas, health care system.
HBV Infection
Twelve individuals (10.2%; 95% confidence interval [CI] = 5.9%, 16.9%) had chronic HBV infection (Table 2). Of these, 11 (92%; 95% CI = 65%, 99%) did not know that they had chronic HBV infection, and none of the family members of patients with chronic HBV infection had been screened for HBV infection. None of the adult family members had been immunized with HBV vaccine, and only 1 patient with chronic HBV infection reported having had his children vaccinated against HBV (Table 3).
TABLE 2.
HBV or HCV Infection Status of Asian American Participants: Alief Community Health Fair, Houston, TX, 2006
| All Participants (N = 118), No. (%) | Possible HCV Infection (n = 7), No. (%) | |
| Chronic HBV infection | 12 (10) | 0 |
| Possible convalescent or occult HBV infection | 9 (10) | 0 |
| Immune because of convalescence from previous HBV infection | 54 (43) | 4 (57) |
| At risk for HBV infection because of absence of immunity | 23 (19) | 2 (29) |
| Immune because of previous HBV vaccination | 20 (17) | 1 (14) |
Note. HBV = hepatitis B virus.
TABLE 3.
Family History of Liver Disease Among 28 Asian American Participants, by HBV or HCV Infection Status: Alief Community Health Fair, Houston, TX, 2006
| Characteristic | Chronic HBV Infection (n = 12), No. (%) | Convalescent or Occult HBV Infection (n = 9), No. (%) | Possible HCV Infection (n = 7), No. (%) |
| Family been checked for hepatitisa | |||
| Yes | 0 | 1 (11) | 2 (29) |
| No | 12 (100) | 8 (89) | 5 (71) |
| Do not know | 0 | 0 (0) | 0 |
| Family history of hepatitis | |||
| Yes | 0 | 2 (22) | 4 (57) |
| No | 12 (100) | 7 (78) | 2 (29) |
| Do not know | 0 | 0 | 1 (14) |
| Family member with hepatitis | |||
| Spouse | 0 | 1 (11) | 1 (14) |
| Parent | 0 | 0 | 1 (14) |
| Child | 0 | 0 | 0 |
| Other relatives | 0 | 1 (11) | 1 (14) |
| None | 12 | 7 (78) | 4 (57) |
| Family received vaccine | |||
| Yes | 0 | 0 | 0 |
| No | 11 (92) | 9 (100) | 7 (100) |
| Do not know | 1 (8) | 0 (0) | 0 |
| Children received vaccine | |||
| Yes | 1 (8) | 0 | 1 (14) |
| No | 11 (92) | 8 (89) | 5 (72) |
| Do not know | 0 | 1 (11) | 1 (14) |
| Family member with HCC | |||
| Yes | 0 | 0 | 0 |
| No | 12 (100) | 9 (100) | 7 (100) |
Note. HBV = hepatitis B virus; HCC = hepatocellular carcinoma.
Family includes spouse, parent, child, or other relatives.
Nine patients (7.6%; 95% CI = 4.1%, 13.9%) had possible occult HBV infection (Table 2). Three were lost to follow-up, but 6 participants were given 1 dose of HBV vaccine to stimulate an amnestic immunological anti-HBs response. Six weeks later, 4 participants (66.7%) had undetectable anti-HBs levels. Addition of these 4 patients with chronic, occult HBV infection to the 12 patients initially diagnosed with chronic HBV infection increased the prevalence of chronic HBV infection from 10.2% to 13.6%. None of the persons screened had evidence of a serological response to HBV vaccination (a positive anti-HBs with negative HBsAg and anti-HBc).
HCV Infection
Seven patients (6%; 95% CI = 2.9%, 11.7%) were positive for anti-HCV antibodies (Table 2). Six of these persons were Vietnamese Americans (Table 1). The prevalence of HCV among the 39 Vietnamese American participants was 15.4% (6 participants), whereas the prevalence of HCV among the rest of the 79 Asian participants was 1.3% (1 participant); this difference was statistically significant (P = .005). One patient with HCV was lost to follow-up. Notably, 3 of the persons with a positive anti-HCV test were aware that they were infected with HCV and had previously received HCV treatment (Table 1). Using PCR, we found HCV RNA in 5 of the 6 participants (83%) with positive anti-HCV antibodies. None of the participants was coinfected with HBV and HCV.
Referral
None of the 12 persons with chronic HBV infection had insurance (Table 1). However, 10 persons (83%) were referred for further care: 3 were referred to the HCHD hepatology clinic through the assistance of HOPE Clinic, 6 were referred to liver specialists and sought care on their own, and 1 elected to see his primary care physician (Figure 1). Two persons were lost to follow-up.
Two (22%) of the 9 persons with possible occult HBV infection had insurance. Of the 6 persons who received further care for an isolated anti-HBc test, 4 persons were suspected to have chronic occult HBV infection. All 4 were successfully referred for further care: 3 were referred to private liver specialists, and 1 was referred to the county hepatology clinic (Figure 1).
Four of the 7 persons with a positive anti-HCV test result had insurance, and all 5 persons with HCV RNA confirmed with PCR were referred for further care (Figure 1).
DISCUSSION
The cross-sectional prevalence of chronic HBV infection in our screening fair population was 10.2% based on the HBsAg test alone but increased to 13.6% when comprehensive testing with HBsAg, anti-HBc, and anti-HBs was used in combination with a single dose of HBV vaccine to differentiate persons convalescent from prior HBV infection from those with chronic, occult HBV. The prevalence of HCV infection was 6% overall but substantially higher (15%) in the Vietnamese American population. Favorably, more than 80% of persons with chronic HBV infection and HCV infection were referred to liver specialists for further evaluation and treatment of liver disease.
The prevalence of chronic HBV infection on the basis of HBsAg testing alone in our study, 10.2% (95% CI = 5.9%, 16.9%), was within the range of 6% to 15% previously reported in a review of Asian Americans tested at screening fairs,5 8.9% reported in a study of Asian Americans in California,23 and 14.8% reported in a study of screening fairs and community clinics in New York City.24
We found that an extraordinary 92% (95% CI = 65%, 99%) of the persons diagnosed with chronic HBV infection on the basis of HBsAg testing alone did not know that they were infected. This level of unawareness was much higher than the 45% (95% CI = 39.2%, 50.7%) reported by Lin et al.,23 although their study included individuals who may have been exposed to extensive HBV educational outreach efforts in the Asian American community of San Francisco. Such exposure may have attracted participation by patients who knew they had chronic HBV.
The prevalence of HCV infection in the United States is not well established in ethnic and racial subgroups because of the methodologies used in National Health and Nutrition Examination Surveys. However, our HCV infection prevalence of 6% was within the range reported in some Asian countries of 2.5% to 6.1%.3,7 Studies describing the HCV burden among Asian Americans are limited. One study in California by Celona et al.25 reported the rate of HCV infection in Asian Americans to be 8%, but this reflects the number of infected Asian Americans in a cohort of patients of various ethnicities known to have HCV infection rather than actual prevalence of HCV among Asian Americans.
Our study shows that concomitant use of HBsAg, anti-HBc, and anti-HBs testing as the initial screening tests in high-risk groups, as opposed to HBsAg testing alone, increases the accuracy of the diagnosis of persons with chronic, occult HBV or who were convalescent from prior HBV infection. A study by Hann et al.26 employed HBsAg in the initial screening and anti-HBc test in later clinic follow-up, but it is unclear what role anti-HBc testing played in the diagnosis of chronic HBV infection.
The high prevalence of HCV infection among Vietnamese participants was anticipated because of the high prevalence of HCV infection in Vietnam. Indeed, 1 study of Asian Americans with HCV infection referred to a tertiary hepatology clinic in California reported Vietnamese Americans to have one of the highest rates of HCV infection: 27.7%.27 However, previous screening fair studies have not focused on HCV among Asian Americans, despite evidence that the prevalence of HCV infection is higher than the 1.8% in the general American population. Community outreach efforts, including information about HCV screening and the role of HCV in liver cancer, should be developed for Vietnamese Americans.
Our study differs from previous cross-sectional studies of HBV infection prevalence because we provided referrals for further care and monitored compliance with our referral recommendations. Although the previously mentioned New York City study24 reported that 91.4% of patients with HBV infection were referred for further care, it is notable that the researchers provided free follow-up medical evaluation and treatment as an inducement. In Houston, as in many US cities, there is no system for free medical care for patients diagnosed with HBV. However, through the efforts of a coalition of community and academic organizations committed to connecting patients with care, we were able to refer more than 80% of patients with chronic HBV infection for medical care, even when there were no established programs in place that provided free care. Because many Asian Americans do not have health insurance or financial resources to purchase health care,5,24 it is imperative to preplan for the care of persons who are diagnosed with HBV infection during free screening events. In addition, it should be recognized that cultural norms often require Asian Americans to place their individual health needs below the needs of the family.5 Without provision of affordable and culturally sensitive access to care, screening for HBV infection may have little impact on the health of Asian Americans found to be infected.
Limitations
Our study suffers from several limitations associated with screening events. Because screening fair participants may have a higher level of health awareness than those who do not attend such fairs, estimates of the prevalence of HBV or HCV in the community may be elevated by selection bias. However, as more than 90% of participants with HBV infection were unaware of their condition, this limitation appears to have had a minimal impact. On the other hand, the fact that 43% of those with possible HCV infection were aware of their illness and had previously been treated indicates that our study prevalence estimate was biased. Because we did not ask all screening participants about their knowledge of previous hepatitis infection, prevalence estimates have limited accuracy. We recommend that all screening events ensure that this question is asked of all participants prior to screening.
We were unable to explore whether participants with HBV or HCV actually adhered to recommendations to seek care from a liver specialist because participants were referred to multiple providers and we did not have access to medical information from all providers. In addition, we did not collect information on income or educational level of our participants. Because the majority of our study participants were Chinese or Vietnamese, our findings may not be generalizable to other Asian American groups. The specific Asian ethnicities of 11 participants were not known because they described themselves only as “Asian.” We do not have the country of birth of the study participants, and this may limit the generalizability of our findings to specific groups of Asian Americans (foreign-born versus born in the United States). We encourage future screening event planners to ask this information of their participants so that risks specific to these different groups can be more fully studied.
Our study, like others in the literature, reflects the serious limitations of cross-sectional data collection. To improve information, we recommend the creation of a national population-based surveillance registry for HBV and HCV infections. To achieve this goal, policymakers should institute a systematic approach to screening and providing access to care for those found to have HBV or HCV infections.
Conclusions
Populations at increased risk of HBV or HCV should be routinely screened. Not only is antiviral medication effective in reducing the risk of HCC, but active surveillance of patients with HBV and HCV also may lead to early detection of HCC, ultimately improving survival. Although current recommendations for HBV infection screening advocate HBsAg testing alone,14 our data indicate that concomitant testing for HBsAg, anti-HBc, and anti-HBs more accurately identifies persons in high-prevalence populations who have HBV infection or convalescent immunity. The use of these tests, in conjunction with the amplification of HBV DNA by PCR in the subsequent evaluation of possible HBV infection, will help identify true occult HBV infection.28 Future studies of larger populations are needed to determine if this strategy is cost-effective as a result of cost savings downstream. In addition, future studies are needed to track the outcomes of screening, including compliance with referral and treatment recommendations and vaccinations, to define and minimize barriers resulting in noncompliance.
Acknowledgments
Funding for laboratory tests came from St Luke's Episcopal Health Charities.
Stephanie Deming provided editorial assistance. Jing Peng assisted with data collection.
Human Participant Protection
The institutional review board at M. D. Anderson Cancer Center approved retrospective review of the screening fair data and follow-up patient information and waived the requirement for informed consent.
References
- 1.Report on Carcinogens. 11th ed US Department of Health and Human Services, Public Health Service, National Toxicology Program. 2004. Available at: http://ntp.niehs.nih.gov/ntp/roc/eleventh/profiles/s092thpb.pdf. Accessed October 7, 2008
- 2.Perz JF, Armstrong GL, Farrington LA, Hutin YJ, Bell BP. The contributions of hepatitis B virus and hepatitis C virus infections to cirrhosis and primary liver cancer worldwide. J Hepatol. 2006;45(4):529–538 [DOI] [PubMed] [Google Scholar]
- 3.Nguyen MH, Keeffe EB. Chronic hepatitis B and hepatitis C in Asian Americans. Rev Gastroenterol Disord. 2003;3(3):125–134 [PubMed] [Google Scholar]
- 4.Mast EE, Margolis HS, Fiore AE, et al. A comprehensive immunization strategy to eliminate transmission of hepatitis B virus infection in the United States: recommendations of the Advisory Committee on Immunization Practices (ACIP) part 1: immunization of infants, children, and adolescents. MMWR Recomm Rep. 2005;54(RR–16):1–31 [PubMed] [Google Scholar]
- 5.Hu KQ. Hepatitis B virus (HBV) infection in Asian and Pacific Islander Americans (APIAs): how can we do better for this special population? Am J Gastroenterol. 2008;103(7):1824–1833 [DOI] [PubMed] [Google Scholar]
- 6.McQuillan GM, Coleman PJ, Kruszon-Moran D, Moyer LA, Lambert SB, Margolis HS. Prevalence of hepatitis B virus infection in the United States: the National Health and Nutrition Examination Surveys, 1976 through 1994. Am J Public Health. 1999;89(1):14–18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kao JH, Chen DS. Transmission of hepatitis C virus in Asia: past and present perspectives. J Gastroenterol Hepatol. 2000;15(suppl):E91–E96 [DOI] [PubMed] [Google Scholar]
- 8.Nguyen MH, Whittemore AS, Garcia RT, et al. Role of ethnicity in risk for hepatocellular carcinoma in patients with chronic hepatitis C and cirrhosis. Clin Gastroenterol Hepatol. 2004;2(9):820–824 [DOI] [PubMed] [Google Scholar]
- 9.Nguyen MH, Garcia RT, Simpson PW, Wright TL, Keeffe EB. Racial differences in effectiveness of alpha-fetoprotein for diagnosis of hepatocellular carcinoma in hepatitis C virus cirrhosis. Hepatology. 2002;36(2):410–417 [DOI] [PubMed] [Google Scholar]
- 10.Freeman AJ, Dore GJ, Law MG, et al. Estimating progression to cirrhosis in chronic hepatitis C virus infection. Hepatology. 2001;34(4 pt 1):809–816 [DOI] [PubMed] [Google Scholar]
- 11.Reddy KR, Hoofnagle JH, Tong MJ, et al. Racial differences in responses to therapy with interferon in chronic hepatitis C. Consensus Interferon Study Group. Hepatology. 1999;30(3):787–793 [DOI] [PubMed] [Google Scholar]
- 12.Lok AS, McMahon BJ. Chronic hepatitis B. Hepatology. 2007;45(2):507–539 [DOI] [PubMed] [Google Scholar]
- 13.Strader DB, Wright T, Thomas DL, Seeff LB. Diagnosis, management, and treatment of hepatitis C. Hepatology. 2004;39(4):1147–1171 [DOI] [PubMed] [Google Scholar]
- 14.Weinbaum CM, Williams I, Mast EE, et al. Recommendations for identification and public health management of persons with chronic hepatitis B virus infection. MMWR Recomm Rep. 2008;57(RR-8):1–20 [PubMed] [Google Scholar]
- 15.Di Bisceglie AM. Hepatitis B and hepatocellular carcinoma. Hepatology. 2009;49(5):S56–S60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bruix J, Sherman M. Management of hepatocellular carcinoma. Hepatology. 2005;42(5):1208–1236 [DOI] [PubMed] [Google Scholar]
- 17.Chin PL, Chu DZ, Clarke KG, Odom-Maryon T, Yen Y, Wagman LD. Ethnic differences in the behavior of hepatocellular carcinoma. Cancer. 1999;85(9):1931–1936 [PubMed] [Google Scholar]
- 18.Taylor VM, Choe JH, Yasui Y, Li L, Burke N, Jackson JC. Hepatitis B awareness, testing, and knowledge among Vietnamese American men and women. J Community Health. 2005;30(6):477–490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hwang JP, Huang CH, Yi JK. Knowledge about hepatitis B and predictors of hepatitis B vaccination among Vietnamese American college students. J Am Coll Health. 2008;56(4):377–382 [DOI] [PubMed] [Google Scholar]
- 20.Taylor VM, Yasui Y, Burke N, et al. Hepatitis B testing among Vietnamese American men. Cancer Detect Prev. 2004;28(3):170–177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bastani R, Glenn BA, Maxwell AE, Jo AM. Hepatitis B testing for liver cancer control among Korean Americans. Ethn Dis. 2007;17(2):365–373 [PubMed] [Google Scholar]
- 22.Mast EE, Weinbaum CM, Fiore AE, et al. A comprehensive immunization strategy to eliminate transmission of hepatitis B virus infection in the United States: recommendations of the Advisory Committee on Immunization Practices (ACIP) part II: immunization of adults. MMWR Recomm Rep. 2006;55(RR–16):1–33 [PubMed] [Google Scholar]
- 23.Lin SY, Chang ET, So SK. Why we should routinely screen Asian American adults for hepatitis B: a cross-sectional study of Asians in California. Hepatology. 2007;46(4):1034–1040 [DOI] [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention Screening for chronic hepatitis B among Asian/Pacific Islander populations–New York City, 2005. MMWR Morb Mortal Wkly Rep. 2006;55(18):505–509 [PubMed] [Google Scholar]
- 25.Celona AF, Yu MC, Prakash M, Kuo T, Bonacini M. Hepatitis C in a Los Angeles public hepatitis clinic: demographic and biochemical differences associated with race-ethnicity. Clin Gastroenterol Hepatol. 2004;2(6):459–462 [DOI] [PubMed] [Google Scholar]
- 26.Hann HW, Hann RS, Maddrey WC. Hepatitis B virus infection in 6130 unvaccinated Korean-Americans surveyed between 1988 and 1990. Am J Gastroenterol. 2007;102(4):767–772 [DOI] [PubMed] [Google Scholar]
- 27.Cheng JT, Hsien C, Sun HE, Tong MJ. The emerging importance of chronic hepatitis C infection in Asian Americans. Am J Gastroenterol. 2006;101(12):2737–2743 [DOI] [PubMed] [Google Scholar]
- 28.Cacciola I, Pollicino T, Squadrito G, Cerenzia G, Orlando ME, Raimondo G. Occult hepatitis B virus infection in patients with chronic hepatitis C liver disease. N Engl J Med. 1999;341(1):22–26 [DOI] [PubMed] [Google Scholar]