Abstract
Objectives. We compared findings on physical activity from national accelerometry data and Healthy People 2010 self-report data to identify differences in disparities by sociodemographic characteristics, gender, age, race/ethnicity, education level, and disability status.
Methods. Data were from the 2003 to 2004 National Health and Nutrition Examination Survey's accelerometry and the Healthy People 2010 Midcourse Review. We computed prevalence of inactivity and regular moderate- and vigorous-intensity movement according to Healthy People 2010 operational definitions.
Results. Mexican American adults were more active than non-Hispanic Blacks and Whites, and groups defined by race/ethnicity and educational attainment were more similar in physical activity in accelerometer than in self-report data. Disparities by gender and disability status were consistent with Healthy People 2010.
Conclusions. Disparities in physical activity differ from previous findings. Increased understanding of these disparities should be used to design better and more cost-effective physical activity interventions. Physical activity surveillance methods should be revised to make use of data collection methods that are more valid than self-report.
Healthy People 2010 objectives are used for many purposes, including addressing health disparities by informing policy and justifying community intervention programs. Physical activity plays a key role in the Healthy People 2010 overarching goals of increasing quality and years of healthy life and eliminating health disparities.1 Three Healthy People 2010 physical activity objectives designed for adults aim to reduce the prevalence of no leisure-time physical activity (22-1), increase regular physical activity (22-2), and increase vigorous-intensity physical activity (22-3).1 Progress toward meeting the Healthy People 2010 physical activity objectives2 is evaluated with self-report data from the National Health Interview Survey (NHIS)3 and at the state level from the Behavioral Risk Factor Surveillance System.4 The Healthy People 2010 Midcourse Review found sociodemographic disparities in physical activity, with racial/ethnic minorities less active than Whites and activity levels positively associated with more education.5
From 2003 to 2006 the National Health and Nutrition Examination Survey (NHANES) measured physical activity with accelerometers, small electronic devices that record bodily acceleration minute by minute, to provide an objective estimate of intensity and duration of locomotion.6 As the first nationally representative sample of accelerometry data in the United States,7 the NHANES data are significant for public health surveillance because they enable an alternative view of population physical activity levels not subject to the potential biases of self-report. The 2 methods can produce differing results on disparities and physical activity prevalence. The initial analyses of the NHANES accelerometer data found that Mexican Americans were more active than non-Hispanic Whites and that non-Hispanic Blacks were the least active racial/ethnic group.7–9 These findings were inconsistent with survey data.2,4 Thus, the inclusion of accelerometry to assess physical activity in surveillance settings has revealed previously unknown information, causing public health professionals to reevaluate some long-standing beliefs about disparities in physical activity.2,4,10–12
Little is known about disparities in physical activity captured by accelerometry data and applied to the Healthy People 2010 physical activity objectives for adults. We assessed sociodemographic disparities in physical activity identified in NHANES accelerometry data for indicators that were equivalent to the Healthy People 2010 objectives. We also aimed to determine whether disparities identified in accelerometer data differed from those in Healthy People 2010's NHIS self-report data. We compared the disparities in the 2003 to 2004 NHANES data with those in the Healthy People 2010 data for 2003.
METHODS
The NHANES is a household interview and examination survey of the health and nutrition status of the civilian, noninstitutionalized US population; its sample is selected with a complex, multistage probability design. In 2003 to 2004, NHANES data were collected for 10 122 persons of all ages.13 Low-income persons, adolescents aged 12 to 19 years, persons aged 60 years and older, Blacks, and Mexican Americans were oversampled.
Participants were initially interviewed at their residence about demographic and family characteristics. At the end of the initial interview, participants were invited to a Mobile Examination Center for a health examination and completion of an in-person survey about health conditions and behaviors. At the conclusion of the examination, ambulatory participants aged 6 years and older were asked to wear a uniaxial accelerometer (ActiGraph model 7164; ActiGraph, LLC, Pensacola, FL) for 7 consecutive days during waking hours to monitor their physical movement.14 Participants were asked to return the accelerometers in a prepaid envelope following the monitoring period. The response rates were 79.3% for the household interview and 85.7% for the accelerometer.
We categorized education levels as less than high school, high school graduate or general equivalency diploma, or at least some college. For race/ethnicity, the NHANES data were available for non-Hispanic Blacks, non-Hispanic Whites, and Mexican Americans13; Healthy People 2010 reported all Hispanics or Latinos and other minority groups.2 To make our indicator of disability similar to that used in the NHIS from different survey questions,3 we defined disability as having a physical, mental, or emotional limitation. In addition, we analyzed the data for age groups that are reported in Healthy People data tables (18–24, 25–44, 45–64, 65–74, and ≥ 75 years), but our source of Healthy People disparities did not include age.5
Healthy People 2010 disparities were derived from self-reported leisure-time physical activity data from the 2003 NHIS that were published in the Healthy People 2010 Midcourse Review.15 We compared disparities in physical activity by gender, race/ethnicity, education level, and disability status for objectives 22-1 (reducing prevalence of no leisure-time physical activity) and 22-2 (regular moderate or vigorous physical activity). To provide context for the accelerometer statistics, we obtained prevalence statistics from NHIS 20033 from DATA2010.2
Accelerometer Data Analysis
For objective monitoring of free-living physical activity, participants were instructed to wear the accelerometer on the right hip, attached by an elastic belt, during waking hours, with the exception of time spent bathing and engaging in other activities involving water.14 Accelerometers were programmed to record activity counts in 1-minute epochs. An NHANES contractor downloaded data from accelerometers returned by participants and checked them for calibration to verify that the units were still functioning within the manufacturer's specifications.
Of the 5620 adults in the survey, 3043 (54.1%) qualified for our analytic sample by providing at least 4 valid days of accelerometer data, including at least 1 weekend day (mean 6.1 ± 1.0 days; 14.2 ± 1.8 hours per day); 292 had sufficient accelerometer data but had no valid weekend days, and 2285 did not have sufficient accelerometer data or were excluded because their monitors were not in calibration upon return. Valid days were defined as having at least 10 hours of monitor wear. Wear time was determined by subtracting nonwear time from 24 hours. Nonwear time was defined as an interval of at least 60 consecutive minutes of 0 counts, with allowance for 1 to 2 minutes of observations of 1 to 100 counts per minute. Implausible data values that were consistent with monitor malfunction (e.g., 32 767 counts per minute) were replaced by imputed values that were the averages of the counts recorded in the minutes immediately preceding and following the implausible value(s).
Two physical activity indicators corresponded to the operational definitions for Healthy People 2010 objectives of reducing the prevalence of no leisure-time activity (22-1)16 and increasing regular physical activity, defined as the accumulation of 10-minute bouts of moderate-intensity movement totaling 30 minutes or more per day on 5 or more days per week or 20 minutes per day of vigorous-intensity movement on 3 or more days per week (22-2).17 Prevalence estimates for increased vigorous physical activity (objective 22-3) were not stable enough to report.
Moderate-intensity movement was defined as minutes with 760 to 5998 counts per minute as defined by Matthews et al.18 and vigorous-intensity movement was minutes with 5999 or more counts per minute,7 to correspond with Healthy People 2010 objective 22-2. We selected the count threshold for moderate-intensity movement defined by Matthews et al. to approximate activity described in the survey questions in the NHIS (i.e., light- to moderate-intensity leisure-time physical activity corresponds to 2.5–5.9 metabolic equivalents).17 The threshold for vigorous movement was selected because other NHANES studies identified it as equivalent to vigorous-intensity physical activity (i.e., 6 metabolic equivalents).7
To compare patterns of accelerometer-derived movement with Healthy People 2010 self-report data on objectives for physical activity, we derived 10-minute bouts from count data for all accelerometer-measured time during the week. To determine whether a participant engaged in moderate- or vigorous-intensity movement in a given minute, we compared activity counts to the respective lower thresholds for each intensity level. Bouts were defined as 10 or more minutes above the minimum threshold for moderate or vigorous intensity, with allowance for interruptions of 1 or 2 minutes below the threshold, which could occur while stopping for a street light while walking. All bouts were terminated with 3 minutes below the minimum threshold for moderate or vigorous activity. To estimate the daily duration of movement, we summed the minutes per day of light- to moderate- and vigorous-intensity movement that occurred in 10-minute bouts. Then, for each bout, we computed frequencies (days per week) of moderate- and vigorous-intensity movement by summing the numbers of valid days in which participants accumulated 30 minutes or more of light- to moderate-intensity activity and 20 minutes or more of vigorous-intensity movement.
Statistical Analysis
We computed the prevalence and standard errors of the physical activity accelerometer data by gender, age group, race/ethnicity, education level, and disability status. We computed age-specific prevalence for movement minutes within each age group and age-adjusted prevalence for the remaining sociodemographic characteristics. Because we excluded 2577 adults with missing accelerometer data, we reweighted the data by age, gender, and race/ethnicity.
To assess sociodemographic disparities in physical activity in the NHANES accelerometry data, we performed 4 steps consistent with the Healthy People 2010 methodology19 for each physical activity indicator. First, we identified the best group as the group with the most favorable prevalence for each Healthy People 2010 physical activity objective. We also computed the percentage difference and z score between each estimate and the best group. To adjust for multiple comparisons of physical activity and sociodemographic characteristics, we set α levels at 0.05 per number of comparisons (Bonferroni adjustment). Finally, we identified statistically significant disparities in physical activity for each sociodemographic characteristic with significant z scores compared with the best group and identified the size of disparity by percentage differences.
To compare disparities identified in accelerometer data with those in self-report data, we graphically juxtaposed disparities determined from the 2003 to 2004 NHANES accelerometer data with those determined from the NHIS self-report data.15 We used SAS version 9.1 (SAS Institute Inc, Cary, NC) and SUDAAN version 9.0 (Research Triangle Institute, Research Triangle Park, NC) for the analysis of NHANES data and Excel 2003 (Microsoft Corp, Redmond, WA) to compute percentage differences and z statistics.
RESULTS
Our analytical sample had slightly more women (n = 1567; 51.5%) than men (n = 1476; 48.5%; Table 1). Thirteen percent (n = 392) were aged 18 to 24 years, and slightly more than half were in the 25 to 44 and 45 to 64 age groups. Blacks made up 19% of the sample; Mexican Americans, 23.1%; and Whites, 58.2%. Slightly less than half (46.9%) had at least some college education, and 28.4% had less than a high school education. A physical, mental, or emotional disability was reported for 30% of the sample.
TABLE 1.
Characteristics of the Analytical Sample (N = 3043): National Health and Nutrition Examination Survey, 2003-2004
| No. (%) | |
| Gender | |
| Men | 1476 (48.5) |
| Women | 1567 (51.5) |
| Age, y | |
| 18–24 | 392 (12.9) |
| 25–44 | 824 (27.1) |
| 45–64 | 888 (29.2) |
| 65–74 | 495 (16.3) |
| ≥ 75 | 444 (14.6) |
| Race/ethnicity | |
| White | 1657 (58.2) |
| Black | 534 (18.7) |
| Mexican American | 658 (23.1) |
| Education level | |
| < High school | 862 (28.4) |
| High school graduate | 750 (24.7) |
| At least some college | 1427 (46.9) |
| Disability status | |
| Persons with disabilities | 917 (30.1) |
| Persons without disabilities | 2126 (69.9) |
Table 2 shows the prevalence of adults aged 18 years and older who met Healthy People 2010 objectives 22-1 and 22-2 according to the NHANES accelerometer data, along with the percentage point differences between the most favorable and other groups. The prevalence of inactive adults (objective 22-1) was 9.3% in the NHANES data and 37% in the NHIS 2003 data. Women had nearly double the prevalence of inactivity of men (12.0% versus 6.4%), a significant difference derived from z scores computed from the prevalence estimates. Among the age groups with reportable prevalence estimates, the best group (most favorable prevalence) was 25 to 44 years, with 3.4% inactivity. The percentage increased with age to 46.6% among adults aged 75 years and older. Comparisons by race/ethnicity showed that Mexican Americans had the lowest estimate of inactivity (7.9%); however, estimates for Whites (9.3%) and Blacks (9.4%) were not significantly higher (P > .025). Inactivity was higher among those with less than a high school education (13.7%) than among those with at least some college, who composed the best group, with only 9.1% inactive.
TABLE 2.
Comparison of Prevalence Data for Healthy People 2010 Objectives for Physical Activity From Accelerometry and Self-Report: National Health Interview Survey, 2003, and National Health and Nutrition Examination Survey, 2003–2004
| Objective 22-1a |
Objective 22-2b |
|||||
| Prevalence,c % (SE) | Difference From Best Group, % | Healthy People 2010, % | Prevalence,c % (SE) | Difference From Best Group, % | Healthy People 2010, % | |
| Overalld | 9.3 (0.6) | NA | 37 | 19.4 (1.0) | NA | 33 |
| Genderd | ||||||
| Men | 6.4 (0.6) | Best group | 35 | 26.8 (1.4) | Best group | 35 |
| Women | 12.0* (0.7) | 88.6 | 39 | 12.3* (1.0) | 54.0 | 31 |
| Age,e y | ||||||
| 18–24 | NA | NA | 29 | 18.7 (2.4) | 25.2 | 42 |
| 25–44 | 3.4 (0.7) | Best group | 34 | 25.0 (2.1) | Best group | 35 |
| 45–64 | 6.7*** (1.1) | 95.7 | 38 | 18.0* (1.3) | 28.0 | 31 |
| 65–74 | 20.6*** (1.8) | 497.7 | 45 | 12.9* (1.5) | 48.2 | 28 |
| ≥ 75 | 46.6*** (2.8) | 1254.0 | 57 | NA (NA) | NA | 18 |
| Race/ethnicityd | ||||||
| Non-Hispanic White | 9.3 (0.6) | 17.2 | 33 | 19.7* (1.1) | 26.1 | 36 |
| Non-Hispanic Black | 9.4 (1.2) | 17.7 | 48 | 15.3* (1.6) | 42.7 | 25 |
| Mexican Americanf | 7.9 (1.0) | Best group | 51 | 26.6 (1.0) | Best group | 25 |
| Education leveldg | ||||||
| < High school | 13.7** (2.0) | 51.3 | 63 | 21.4 (3.5) | 3.1 | 17 |
| High school graduate | 10.0 (1.1) | 9.9 | 45 | 22.1 (1.9) | Best group | 27 |
| ≥ Some college | 9.1 (0.8) | Best group | 28 | 18.2 (1.4) | 17.3 | 38 |
| Disability statusdf | ||||||
| Persons with disabilities | 13.4* (1.3) | 108.2 | 53 | 14.3* (2.4) | 31.6 | 21 |
| Persons without disabilities | 6.4 (0.6) | Best group | 34 | 20.9 (1.0) | Best group | 35 |
Note. NA = not available because SE divided by percentage was greater than 0.30.
Source. Healthy People 2010 database.2
This objective aims to reduce the prevalence of physical inactivity during leisure time. Measured as days that included 10-minute bouts of light–moderate or vigorous movement. Best group had the most favorable prevalence.
This objective aims to increase regular physical activity. Measured as days that included 10-minute bouts of moderate-intensity activity totaling at least 30 minutes on 5 or more days of the 7-day surveillance period or 20 minutes per day of vigorous activity on at least 3 days during the surveillance. Best group had the most favorable prevalence.
Significance determined by z score.
Age-adjusted to the following age groups: 18–24, 25–34, 35–44, 45–64, and 65 years and older.
Age-specific prevalence estimates.
Definitions of ethnicity and disability status differed between the surveys. The National Health and Nutrition Examination Survey sampled Mexican Americans. Healthy People 2010 used data from the National Health Interview Survey, which sampled all Hispanics/Latinos.
Age-adjusted for persons aged 25 years and older.
*P < .05; **P < .025; ***P < .017.
For Healthy People 2010 objective 22-2, 19.4% of adults met the criteria for regular physical activity. Persons aged 25 to 44 years were the best group, with the highest prevalence of moderate and vigorous movement (25.0%). This prevalence did not differ significantly for persons aged 18 to 24 years (18.7%) but was higher than among persons aged 45 to 64 years (18.0%) and 65 to 74 years (12.9%).
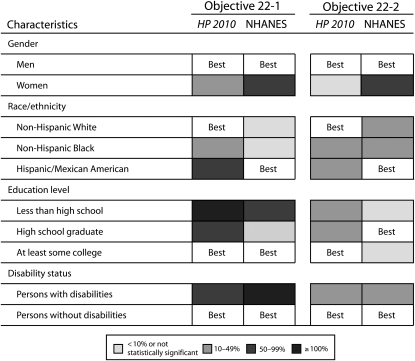
Figure 1 shows physical activity disparities by gender, race/ethnicity, education level, and disability status in the Healthy People 2010 Midcourse Review15 according to self-report data and NHANES accelerometer data. For 2 sociodemographic characteristics we found similar disparity patterns in the different data sets. For both objectives, men were identified as the best group in both the Healthy People 2010 and the NHANES data. However, the size of the disparities differed: we found a larger disparity for women in the accelerometer data than in the self-report data. For disability status, we observed no difference in best groups, and disparities were larger in the accelerometry than in the self-report data for inactivity; disparities were the same for regular physical activity.
FIGURE 1.
Comparison of physical activity disparities for Healthy People 2010 (HP 2010) objectives 22-1 and 22-2, by self-report and accelerometer: National Health and Nutrition Examination Survey (NHANES), 2003–2004.
Note. Shaded cells reflect the degree of disparity in physical activity within each sociodemographic characteristic; darker shades reflect greater disparities than those who had more favorable prevalence of physical activity; best indicates most favorable prevalence. Disparity from the best group prevalence was defined as the percentage difference between the best group prevalence and each of the other group prevalences for a characteristic. Definitions of ethnicity and disability status differed between Healthy People 2010 and NHANES. Source. Healthy People 2010 self-reported physical activity from the National Health Interview Survey 2003.15 Accelerometry data from NHANES 2003–2004.6
Disparities differed between self-report and accelerometer data for race/ethnicity and education. For race/ethnicity we found differences in best group for both objectives. Non-Hispanic Whites were previously identified as the best group in the self-report data, but we found that Mexican Americans were the best group in our analysis of the accelerometer data. For objective 22-1, Healthy People 2010 data showed Hispanics with a disparity of 50% to 99% compared with non-Hispanic Whites. The accelerometer data yielded smaller disparities for non-Hispanic Blacks and non-Hispanic Whites.
Examining objective 22-2 by education level, we found that the best group comprised participants with a high school education rather than those with more education. Because disparities computed with smaller prevalence estimates are more sensitive to small differences in estimates, the differences in the sizes of the disparities are related in part to the prevalence estimates for each data source. For reference, the overall prevalence in 2003 for objective 22-1 was 37% and for 22-2, 33%.2 However, the sizes of the disparities for 22-1 by race/ethnicity and for both objectives by education level were smaller in the NHANES data than in the Healthy People 2010 data, indicating less real variability across groups in accelerometer than in self-report data.
DISCUSSION
We used definitions of physical inactivity and regular physical activity that approximated those used by Healthy People 2010 for tracking physical activity objectives for adults and identified disparities that differed from those published in the Healthy People 2010 Midcourse Review.15 This challenges traditional thinking in the field2,4,10–12 and shows that physical activity levels may not differ by race/ethnicity and education level as much as expected.
Our analysis of accelerometer data identified Mexican Americans as the most active racial/ethnic group, a finding that, although contrary to the traditional beliefs about racial/ethnic disparities, makes sense in light of the Hispanic paradox (the puzzling findings of many studies that Hispanics enjoy better health outcomes than other US adults with the same low socioeconomic status20). Mexican Americans could be more active than Hispanics overall, but this is unlikely because Hispanic immigrants have similar occupational opportunities in the United States, and they generally involve physically active manual labor. Accelerometers can detect occupational time, which is difficult to assess through self-report and is therefore not measured in the surveys reported by Healthy People 2010.3,4 Thus, inclusion of data reflecting occupational physical activity in the NHANES accelerometer data could explain the surprising differences in racial/ethnic disparities for physical activity not seen with leisure-time physical activity surveys.
We also found disparities in accelerometer data by educational attainment that differed from survey data. Although the least educated had the highest levels of inactivity, a finding similar to survey data,2,10,11 we found smaller differences in regular physical activity across educational levels. This could be explained by the interrelationship of race/ethnicity and educational attainment with physical activity.
The disparities we identified follow the patterns reported by other studies that analyzed the NHANES accelerometer data.7–9 However, our prevalence estimates differed from these reports in that we estimated that 9% of US adults were inactive and 19% were regularly active. Troiano et al. found that 3% of US adults met the criteria for recommended levels of physical activity in 2003 to 2004.7 We derived bouts of moderate and vigorous physical activity separately, according to the operational definition of Healthy People 2010 objective 22-217; Troiano et al. identified activity bouts of combined moderate and vigorous activity.7
A second, more important factor in these differing results is that prevalence is highly dependent on the thresholds for discriminating between inactivity and light-to-moderate physical activity. For consistency with the NHIS definition of moderate activity,17 which includes activities of light-to-moderate intensity, we needed to capture similar light- to moderate-intensity movement and therefore set an accelerometer threshold of 760 counts per minute. This cutpoint is consistent with Matthews et al.'s definition of 760 counts per minute as lifestyle moderate activity.18 Troiano et al. defined moderate activity as 2020 or more counts per minute.7 If we had used a higher counts-per-minute threshold, the prevalence of inactivity would have been higher and regular physical activity would have approached the 3% figure reported by Troiano et al. Yet despite the variation in counts-per-minute cutpoints, all analyses of these data showed that overall, Americans are less active than was suggested by self-report data from the Behavioral Risk Factor Surveillance System2,4,11,12 and NHIS.2
A third caveat for interpreting NHANES data lies in the ambiguous meaning of accelerometer counts per minute.21 For example, an accelerometer can record a minute with a value of 1000 counts per minute, but it cannot reveal the fitness level of the person wearing the device. A person with a high fitness level could walk during that minute at a lower relative intensity than required for health benefits while still producing the high counts. By contrast, a less fit person could rake leaves, expending considerable effort, to produce the same accelerometer results. At the low end of the ability range, frail older adults might never move with an acceleration reaching 1000 counts per minute.
Interpretation of accelerometer counts also varies by type of activity performed. For example, bicycling vigorously requires leg movement that is not captured by accelerometers worn on the waist, so the cyclist might not reach 1000 counts per minute. However, only small percentages of US adults participate in activities that do not register accelerometer counts (e.g., swimming and bicycling) on any given day.22 Accelerometers are not considered to be a gold standard for measuring physical activity but are effective in capturing locomotion minute by minute for better assessment of the duration and intensity of movement without the issues of memory, cognition, and social effects that are inherent in self-report data.
Our findings have implications for public health practice because they improve our understanding of disparities in physical activity and low physical activity levels in the United States. Programs such as the Steps to a HealthierUS initiative23 and REACH US24 intervene at the community level to reduce disparities in chronic disease and related factors. Although we found evidence suggesting that Hispanics have less extra risk than previously thought for physical activity–related health conditions, we do not suggest that funding should be shifted away from Hispanic communities. Rather, these findings can help in the design of multicomponent community programs intended to reduce disparities in chronic disease and related factors, such as the Steps to a HealthierUS initiative and REACH US, that more effectively target components of groups that will benefit the most and thereby facilitate more cost-effective allocation of funds within programs.
Our study also revealed some of the limitations of self-report data in physical activity surveillance. Because surveillance data informs the planning of multicomponent, multisectoral interventions and is used for research, public health stakeholders' interests in surveillance data are many and varied. The NHANES data only serve the needs of researchers, so multiple data sources at the individual and community levels are required for other purposes. Our findings and those of others who analyzed accelerometer data from the 2003 to 2004 NHANES suggest that physical activity surveillance that relies on self-report alone to assess individual behavior may not be accurate enough to meet the needs of stakeholders.7–9 We recommend that future surveillance employ both accelerometry and self-report surveys linked to data sources from related sectors of society. Thus, surveillance could provide contextual information about physical activity behaviors while ensuring that the complementary data sources have acceptable accuracy and precision for researchers and practitioners.
The analytic sample of the NHANES data yielded usable prevalence estimates for 2 of 3 Healthy People 2010 objectives of interest (22-1 and 22-2) and for all sociodemographic characteristics. The prevalence of vigorous activity in the sample was too low to evaluate objective 22-3. Prevalence of 2 age groups was also too low to include in the analyses. However, our data captured the most important indicators for public health (i.e., inactivity and regular moderate- to vigorous-intensity activity). Although our definitions of race/ethnicity and disability status differed from those used by Healthy People 2010 because the surveys varied, we believe that the analyses of these groups provide valuable insights into potential disparities in physical activity.
In response to the release of the NHANES accelerometer data, we investigated differences in identifying disparities between 2 methods of physical activity surveillance: accelerometry and self-report. We used indicators from the NHANES data that were similar to Healthy People 2010 self-report data and found that Mexican American adults were more active than non-Hispanic Blacks and Whites and that groups defined by race/ethnicity and educational attainment were more similar than previously thought. Our findings are consistent with other studies of accelerometer data, with the Hispanic paradox, and with previously identified issues regarding self-report data on physical activity in surveillance systems. Our study has implications for public health practice because it increases our understanding of physical activity disparities, which may lead to better and more cost-effective interventions. We hope that findings such as ours will encourage reevaluation of physical activity surveillance methods that depend on self-report data.
Human Participant Protection
No protocol approval was required for this study because secondary data were used. Data collection protocols for the NHANES were approved by the institutional review board at the Centers for Disease Control and Prevention.
References
- 1.Healthy People 2010: With Understanding and Improving Health and Objectives for Improving Health. 2nd ed. 2 vols Washington, DC: US Dept of Health and Human Services; 2000 [Google Scholar]
- 2.Centers for Disease Control and Prevention DATA2010: the Healthy People 2010 database. Available at: http://wonder.cdc.gov/data2010. Accessed August 2, 2009
- 3.Centers for Disease Control and Prevention, National Center for Health Statistics National Health Interview Survey questionnaires, datasets, and related documentation. Updated June 17, 2009. Available at: http://www.cdc.gov/nchs/nhis/nhis_questionnaires.htm. Accessed August 2, 2009 [Google Scholar]
- 4.Centers for Disease Control and Prevention Behavioral Risk Factor Surveillance System prevalence and trends data. Updated October 8, 2008. Available at: http://apps.nccd.cdc.gov/BRFSS. Accessed August 2, 2009 [Google Scholar]
- 5.Healthy People 2010 Midcourse Review. Washington, DC: US Dept of Health and Human Services; 2007 [Google Scholar]
- 6.Centers for Disease Control and Prevention, National Center for Health Statistics National Health and Nutrition Examination Survey. Available at: http://www.cdc.gov/nchs/nhanes.htm. Accessed August 2, 2009 [PubMed]
- 7.Troiano RP, Berrigan D, Dodd KW, Mâsse LC, Tilert T, McDowell M. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–188 [DOI] [PubMed] [Google Scholar]
- 8.Matthews CE, Chen KY, Freedson PS, et al. Amount of time spent in sedentary behaviors in the United States, 2003–2004. Am J Epidemiol. 2008;167(7):875–881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hawkins MS, Storti KL, Richardson CR, et al. Objectively measured physical activity of USA adults by sex, age, and racial/ethnic groups: a cross-sectional study. Int J Behav Nutr Phys Act. 2009;6:31 Available at: http://www.ijbnpa.org/content/6/1/31. Accessed August 2, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Physical Activity and Health: A Report of the Surgeon General. Atlanta, GA: Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion; 1996 [Google Scholar]
- 11.Centers for Disease Control and Prevention Trends in leisure-time physical inactivity by age, sex, and race/ethnicity—United States, 1994–2004. MMWR Morb Mortal Wkly Rep. 2005;54(39):991–994 [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention Prevalence of self-reported physically active adults—United States, 2007. MMWR Morb Mortal Wkly Rep. 2008;57(48):1297–1300 [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention, National Center for Health Statistics National Health and Nutrition Examination Survey 2003–2004. Available at: http://www.cdc.gov/nchs/nhanes/nhanes2003-2004/nhanes03_04.htm. Accessed August 2, 2009
- 14.Centers for Disease Control and Prevention, National Center for Health Statistics Mobile Exam Center component descriptions. Available at: http://www.cdc.gov/nchs/data/nhanes/meccomp.pdf. Accessed August 2, 2009
- 15.Healthy People 2010 Midcourse Review: Physical Activity and Fitness. Washington, DC: US Dept of Health and Human Services; 2007 [Google Scholar]
- 16.Centers for Disease Control and Prevention Healthy People 2010 operational definition: 22-1: reduce the proportion of adults who engage in no leisure-time physical activity. Available at: ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Datasets/DATA2010/Focusarea22/O2201.pdf. Accessed August 2, 2009
- 17.Centers for Disease Control and Prevention Healthy People 2010 operational definition: 22-2: increase the proportion of adults who engage in moderate physical activity for at least 30 minutes per day 5 or more days per week or vigorous physical activity for at least 20 minutes per day 3 or more days per week. Available at: ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Datasets/DATA2010/Focusarea22/O2202.pdf. Accessed August 2, 2009
- 18.Matthews CE. Calibration of accelerometer output for adults. Med Sci Sports Exerc. 2005;37(11 suppl):S512–S522 [DOI] [PubMed] [Google Scholar]
- 19.Keppel KG, Pearcy JN, Klein RJ. Measuring Progress in Healthy People 2010. Hyattsville, MD: National Center for Health Statistics; 2004. Statistical Notes, No. 25 [PubMed] [Google Scholar]
- 20.Abraído-Lanza AF, Chao MT, Flórez KR. Do healthy behaviors decline with greater acculturation? Implications for the Latino mortality paradox. Soc Sci Med. 2005;61(6):1243–1255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ham SA, Reis JP, Strath SJ, Dubose KD, Ainsworth BE. Discrepancies between methods of identifying objectively determined physical activity. Med Sci Sports Exerc. 2007;39(1):52–58 [DOI] [PubMed] [Google Scholar]
- 22.Ham SA, Kruger J, Tudor-Locke C. Participation by US adults in sports, exercise, and recreational physical activities. J Phys Act Health. 2009;6(1):6–14 [DOI] [PubMed] [Google Scholar]
- 23.US Dept of Health and Human Services Steps to a HealthierUS initiative. Available at: http://www.healthierus.gov/STEPS. Accessed August 2, 2009
- 24.Centers for Disease Control and Prevention Racial and ethnic approaches to community health (REACH U.S.). Available at: http://www.cdc.gov/reach. Accessed August 2, 2009