Abstract
Objectives. We aimed to describe socioeconomic disparities in the United States across multiple health indicators and socioeconomic groups.
Methods. Using recent national data on 5 child (infant mortality, health status, activity limitation, healthy eating, sedentary adolescents) and 6 adult (life expectancy, health status, activity limitation, heart disease, diabetes, obesity) health indicators, we examined indicator rates across multiple income or education categories, overall and within racial/ethnic groups.
Results. Those with the lowest income and who were least educated were consistently least healthy, but for most indicators, even groups with intermediate income and education levels were less healthy than the wealthiest and most educated. Gradient patterns were seen often among non-Hispanic Blacks and Whites but less consistently among Hispanics.
Conclusions. Health in the United States is often, though not invariably, patterned strongly along both socioeconomic and racial/ethnic lines, suggesting links between hierarchies of social advantage and health. Worse health among the most socially disadvantaged argues for policies prioritizing those groups, but pervasive gradient patterns also indicate a need to address a wider socioeconomic spectrum—which may help garner political support. Routine health reporting should examine socioeconomic and racial/ethnic disparity patterns, jointly and separately.
For years, public health statistics in several European countries have been routinely collected and reported for groups defined by social class, generally measured by ranking according to occupational hierarchies reflecting differences in social standing1–4; in the United Kingdom and France, for example, this has been the case for close to a century. At least 5 social classes have routinely been examined in the United Kingdom since 1913,5 and several European countries have used 6 or more social class groups in their routine health statistics.6,7 The presence of detailed socioeconomic information in routine health data in Europe has facilitated the monitoring of socioeconomic patterns in diverse health indicators, with the ability not only to compare the health of socioeconomically disadvantaged persons with that of all others but also to examine health differences among middle-class subgroups and, potentially, comparisons with the wealthy.
In contrast, routine public health statistics in the United States historically have been reported by racial or ethnic group,8 but health differences across groups defined by socioeconomic factors (typically, income or educational attainment) have been examined less frequently.2 When differences in income and education have been reported, the number of groups being compared has often been limited to two or at most three. A review of more than 20 National Center for Health Statistics (NCHS) publications9–32 on health status or health-related behaviors, released in 2009 and available on the NCHS Web site, revealed that although most examined differences in health by race or ethnicity, fewer than half examined differences by income or education, and most of those considered no more than 3 categories. For example, in the most recent edition of Health, United States,28 the US Department of Health and Human Services's annual health statistics report, 93 of its 151 tables report health differences by race or Hispanic origin, compared with 34 and 16 tables reporting differences by income (as a percentage of poverty) and education, respectively. With the exception of the Socioeconomic Status and Health Chartbook,33 part of the 1998 edition, Health, United States usually compares at most 3 income groups (the “poor,” with incomes below 100% of poverty; “near poor,” with incomes from 100% up to 200% of poverty; and all higher-income persons combined) and 3 education groups (persons who have not completed high school, high school graduates, and those with at least some postsecondary education). The Socioeconomic Status and Health Chartbook, the National Health Interview Survey (NHIS) Series 10 reports,34 and the Agency for Healthcare Research and Quality (AHRQ) National Healthcare Disparities Reports35 are notable exceptions of reports based on routine public health data in which differences are examined across 4 or 5 socioeconomic groups; however, the NHIS reports do not examine differences by race and socioeconomic factors considered jointly, the AHRQ reports focus primarily on health care, and the Socioeconomic Status and Health Chartbook is now more than a decade old.
The general lack of routinely reported information on social and economic differences in health in this country has public health implications. The ways that health disparities are patterned socially may help us understand their nature and how best to address them.36,37 Differences in health that suggest a socioeconomic threshold at or near the poverty line (e.g., a high rate of a particular illness among the poor, contrasted with more favorable and similar rates for all other income groups) would support targeted policies to address aspects of deprivation (e.g., substandard housing, hazardous work) uniquely experienced by the most disadvantaged. In contrast, differences in health that follow a gradient pattern (e.g., with worse outcomes not just among the poor but in “middle-class” subgroups as well, compared with higher-income groups) would suggest the need to consider policies that address factors such as relative deprivation or relative standing,38 degree of control over one's work,39 or levels of chronic stress associated with ongoing logistical challenges (e.g., child care or transportation needs) that may become progressively easier to address with additional economic and social resources,40,41 at least up to a threshold well above the poverty or near-poverty line. Furthermore, examining racial and socioeconomic patterns in health jointly can inform policies to address inequalities in both dimensions.
We aimed to describe patterns of socioeconomic differences in a wide array of important health indicators in the United States, among children and adults overall and within different racial or ethnic groups. A number of US studies have revealed gradient patterns in adult health indicators,42–45 but we are unaware of US studies or routine reports since Health, United States, 1998 that (1) have looked at socioeconomic patterns in health across a wide range of both child and adult health status and health-related behavior indicators, (2) have examined a sufficient number of income or education categories to be able to distinguish health differences among subgroups of the nonpoor (or those with at least a high school education), and (3) have jointly examined both socioeconomic and racial or ethnic differences in health.
METHODS
We examined patterns of socioeconomic disparities in 11 health indicators representing an array of health conditions and health-related behaviors that are of considerable public health importance for children and adults. The selected indicators for children were infant mortality, health status as reported by parents or guardians, activity limitation due to chronic disease, healthy eating behaviors, and sedentary behavior (among adolescents); adult health indicators were life expectancy at age 25, self-reported health status, activity limitation due to chronic disease, coronary heart disease, diabetes, and obesity. Data were obtained from 5 nationally representative data sources with well-documented strengths and limitations: the Period Linked Birth/Infant Death Data File, 2000–200246; the National Longitudinal Mortality Study (NLMS), 1988–1998 (through an agreement with the NLMS Steering Committee)47; the National Health Interview Survey (NHIS), 2001–200548; the National Health and Nutrition Examination Survey (NHANES), 1999–200449; and the Behavioral Risk Factor Surveillance System (BRFSS), 2005–2007.50 Table 1 gives a summary of the data sources and variable definitions. Changes in the data sources over time precluded comparison of the socioeconomic patterns across time periods.
TABLE 1.
Summary of Data Sources, Sample, Measures of Socioeconomic Status (SES), and Health-Related Indicators Used to Examine Income and Education Disparities in Child and Adult Health: United States, 1988–2007
| Data Source | Age Groups (Sample Size) | Racial/Ethnic Groups | Measures of SES | Health-Related Indicators |
| Period Linked Birth/Infant Death Data File, 2000–200246 | Maternal age ≥ 20 y (69 660 infant deaths among 10 742 652 live births) | Black (non-Hispanic), Hispanic, White (non-Hispanic) | Educational attainment (maternal)a | Infant mortality rate: number of infantdeaths before age 1 per 1000 live births |
| National Longitudinal Mortality Study (NLMS), 1988–199847 | Age ≥ 25 y (448 360 persons and 2 590 796 person-years) | Black (non-Hispanic), Hispanic, White (non-Hispanic) | Family income as a percentage of educational attainmentb | Life expectancy at age 25, in years |
| National Health Interview Survey (NHIS), 2001–200548 | Age ≤ 17 y (n = 127 394), Age ≥ 25 y (n = 286 536) | Black (non-Hispanic), Hispanic, White (non-Hispanic) | Family income as a percentage of FPL, educational attainment (for child indicators, head of household; for adult indicators, individual)c | Respondent-assessed health status: percentage with “poor,” “fair,” or “good” health vs “very good” or “excellent” health (children) |
| Activity limitation: percentage with any activity limitation due to chronic disease (children and adults); | ||||
| Coronary heart disease: percentage who had ever been told by a doctor or other health professional that he or she had coronary heart disease, angina, a heart attack, or any other kind of heart condition or heart disease (adults) | ||||
| National Health and Nutrition Examination Survey (NHANES), 1999–200449 | Age 2–19 y (n = 9066), Age 12–19 y (n = 7205), Age 20–64 y (n = 10 983), Age ≥ 20 y (n = 12 463) | Black (non-Hispanic), Mexican American, White (non-Hispanic) | Family income as a percentage of FPL, educational attainment (for child indicators, head of household; for adult indicators, individual)d | Healthy eating index (HEI) score (1999–2002 only): mean score for HEI, defined as the sum of equally weighted scores for 10 components (grains, vegetables, fruits, milk, meat, total fat, saturated fat, sodium, cholesterol, and variety), each ranging from 0 to 10, with higher scores indicating healthier eating (ages 2–19); |
| Sedentary behavior: percentage without moderate or vigorous leisure-time physical activity for at least 10 min in the past 30 d (ages 12–19); | ||||
| Diabetes: percentage with fasting blood glucose ≥ 126 mg/dL or self-report of doctor or health professional diagnosis (men and nonpregnant women, ages 20–64); | ||||
| Obesity: percentage with body mass index ≥ 30 kg/m2 (ages 20 and older) | ||||
| Behavioral Risk Factor Surveillance System (BRFSS), 2005–200750 | Age 25–74 y (n = 914 669) | Black (non-Hispanic), Hispanic, American Indian or Alaskan Native (non-Hispanic), Native Hawaiian or other Pacific Islander (non-Hispanic), Asian (non-Hispanic), White (non-Hispanic) | Educational attainmente | Self-assessed health status: percentage with “poor,” “fair,” or “good” health vs “very good” or “excellent” health |
Note. FPL = federal poverty line.
Period Linked Birth/Infant Death Data File: income data were not available. Education was measured as years of school completed by mother, grouped to correspond with earned educational credentials, as follows: 0–11 y, 12 y, 13–15 y, 16 or more years.
NLMS: family income was calculated as a percent of FPL, adjusted for family size and grouped as ≤ 100%, 101%–200%, 201%–400%, and > 400% (missing values were imputed). Education was measured as highest grade completed, grouped to correspond with earned educational credentials, as follows: did not graduate from high school, high school graduate, some college, college graduate or more.
NHIS: family income was calculated as a percent of FPL, adjusted for family size and grouped as < 100%, 100%–199%, 200%–299%, 300%–399%, and ≥ 400% (missing values were replaced with imputed data available through NCHS). Education was measured as highest level or degree completed, as follows: did not graduate from high school, high school graduate, some college, college graduate or more.
NHANES: family income was calculated as a percent of FPL, adjusted for family size and grouped as < 100%, 100%–199%, 200%–299%, 300%–399%, and ≥ 400% (missing values were excluded). Education was measured as highest grade or level of school completed or degree received, as follows: did not graduate from high school, high school graduate, some college, college graduate or more.
BRFSS: income was not examined because the income data in the BRFSS does not permit adequate measurement of household income as a percentage of FPL. Education was measured as highest grade or year completed, as follows: did not graduate from high school, high school graduate, some college, college graduate or more.
We calculated levels, with 95% confidence intervals, of each indicator (rates of infant mortality, mean scores for healthy eating behaviors and mean years of life expectancy at age 25, and prevalence rates for other indicators) according to income or education, in the surveyed populations overall and within each racial or ethnic group for which sample sizes were sufficient. (Note that we use “Black” and “White” to refer to non-Hispanic Blacks and non-Hispanic Whites, respectively.) For indicators examined with NHIS, NHANES, and BRFSS data, weighted age-adjusted (to the 2000 standard population) prevalence rates were estimated to account for the complex sample designs. Differences in indicator levels were examined both by household income as a percentage of the federal poverty level (based on the survey year) and by years of educational attainment (as defined in Table 1) for all indicators except infant mortality (examined with data from the Period Linked Birth/Infant Death Data File, which lacked any income information) and self-reported health status among adults (examined with data from the BRFSS, in which income information is missing for 14% of respondents and otherwise grouped into categories that preclude accurate federal poverty level estimates at higher income levels); differences in these 2 indicators were examined only by highest level of educational attainment. Trend tests were performed with least squares linear regression (weighted by the inverse of the variance), which tested whether the slope, or socioeconomic gradient in health, differed from zero; given the relatively small sample sizes for some indicators, we used a P value of less than .10 to assess whether patterns in health levels by income and education were consistent with a gradient. Results are summarized in Table 2 and displayed graphically in Figure 1 and Figure 2 and in the supplemental figures (available in the online version of this article at http://www.ajph.org).
TABLE 2.
Income and Education Disparities in Child and Adult Health: United States, 1988–2007
| Family Income as Percentage of FPLa |
Educational Attainmentb |
||||||||||
| Health Indicator and Population Subgroup | < 100% FPL, % or %c (95% CI) | 100%–199% FPL, % or %c (95% CI) | 200%–299% FPL, % or %c (95% CI) | 300%–399% FPL, % or %c (95% CI) | ≥ 400% FPL, % or %c (95% CI) | Trend,d P | Not High School Graduate, % or %c (95% CI) | High School Graduate, % or %c (95% CI) | Some College, % or %c (95% CI) | College Graduate, % or %c (95% CI) | Trend,d P |
| US populatione | |||||||||||
| All | 12.5 | 18.0 | 17.1 | 13.9 | 38.5 | 16.0 | 30.0 | 27.0 | 27.0 | ||
| Black | 24.5 | 23.0 | 17.7 | 12.1 | 22.7 | 20.7 | 33.9 | 28.6 | 16.8 | ||
| Hispanic | 21.5 | 29.1 | 19.8 | 11.4 | 18.2 | 40.1 | 27.8 | 19.8 | 12.3 | ||
| White | 8.2 | 14.7 | 16.6 | 14.8 | 45.8 | 11.1 | 30.6 | 28.3 | 30.0 | ||
| Infant mortality (mothers aged ≥ 20 y) | |||||||||||
| All | 7.8 (7.7, 7.9) | 7.4 (7.3, 7.5) | 6.0 (5.9, 6.1) | 4.2 (4.1, 4.3) | .084 | ||||||
| Black | 15.1 (14.6, 15.6) | 13.4 (13.1, 13.7) | 12.1 (11.8, 12.5) | 10.5 (10.1, 10.9) | .028 | ||||||
| Hispanic | 5.2 (5.1, 5.4) | 5.2 (5.0, 5.4) | 4.9 (4.7, 5.1) | 4.0 (3.7, 4.3) | .228 | ||||||
| White | 9.2 (8.9, 9.5) | 6.4 (6.3, 6.5) | 4.8 (4.7, 4.9) | 3.8 (3.7, 3.9) | .012 | ||||||
| Health status not excellent or very good (age 0–17 y) | |||||||||||
| All | 30.9 (29.8, 32.0) | 22.7 (21.8, 23.6) | 15.4 (14.6, 16.2) | 11.8 (11.1, 12.6) | 8.2 (7.7, 8.6) | .009 | 32.1 (30.9, 33.3) | 23.6 (22.8, 24.4) | 16.5 (15.9, 17.1) | 8.1 (7.8, 8.5) | .013 |
| Black | 33.0 (30.8, 35.3) | 26.9 (24.8, 29.1) | 21.3 (19.2, 23.6) | 17.6 (14.9, 20.7) | 14.7 (12.7, 16.9) | .005 | 33.5 (30.5, 36.5) | 30.2 (28.1, 32.2) | 23.7 (22.2, 25.2) | 15.4 (13.6, 17.2) | .068 |
| Hispanic | 35.0 (33.2, 36.8) | 27.4 (25.9, 28.9) | 21.4 (19.8, 23.2) | 17.2 (14.8, 19.9) | 12.3 (10.5, 14.3) | .003 | 33.8 (32.2, 35.3) | 26.7 (25.2, 28.2) | 22.4 (21.0, 23.8) | 13.6 (12.0, 15.2) | .027 |
| White | 26.3 (24.6, 28.2) | 18.7 (17.5, 19.9) | 12.2 (11.4, 13.2) | 9.9 (9.1, 10.8) | 7.0 (6.5, 7.5) | .016 | 27.7 (25.1, 30.3) | 20.2 (19.2, 21.3) | 12.9 (12.3, 13.6) | 6.4 (6.0, 6.7) | .012 |
| Activity limited due to chronic disease (age 0–17 y) | |||||||||||
| All | 9.3 (8.8, 9.8) | 8.1 (7.7, 8.6) | 6.9 (6.5, 7.4) | 6.3 (5.8, 6.8) | 5.1 (4.7, 5.4) | .001 | 7.7 (7.2, 8.2) | 7.8 (7.4, 8.2) | 7.8 (7.5, 8.1) | 5.3 (5.0, 5.6) | .271 |
| Black | 10.1 (9.1, 11.1) | 8.6 (7.6, 9.7) | 6.7 (5.5, 8.1) | 5.8 (4.7, 7.3) | 5.1 (4.1, 6.2) | .005 | 10.9 (9.6, 12.3) | 8.6 (7.7, 9.5) | 7.5 (6.8, 8.2) | 6.0 (5.0, 7.1) | .002 |
| Hispanic | 6.1 (5.5, 6.7) | 5.2 (4.7, 5.7) | 4.8 (4.1, 5.7) | 5.2 (4.3, 6.4) | 5.9 (4.9, 7.1) | .686 | 4.6 (4.1, 5.1) | 6.2 (5.6, 6.9) | 5.9 (5.4, 6.4) | 5.8 (4.9, 6.7) | .152 |
| White | 12.3 (11.3, 13.4) | 9.9 (9.1, 10.6) | 7.6 (7.1, 8.2) | 6.6 (6.0, 7.3) | 5.1 (4.7, 5.5) | .005 | 12.9 (11.6, 14.4) | 8.3 (7.8, 8.9) | 8.5 (8.1, 8.9) | 5.3 (5.0, 5.6) | .047 |
| Healthy Eating Index (age 2–19 y) | |||||||||||
| All | 63.7 (62.6, 64.7) | 63.6 (62.5, 64.7) | 64.0 (62.8, 65.2) | 65.8 (64.5, 67.2) | 67.0 (65.8, 68.1) | .017 | 62.7 (61.9, 63.4) | 63.4 (62.4, 64.5) | 65.0 (63.8, 66.1) | 67.8 (66.6, 69.1) | .093 |
| Black | 63.5 (62.7, 64.3) | 63.0 (61.7, 64.3) | 64.7 (63.4, 65.9) | 63.7 (61.7, 65.8) | 65.7 (64.3, 67.1) | .068 | 62.3 (61.4, 63.2) | 63.9 (63.2, 64.6) | 64.2 (63.5, 64.8) | 65.7 (63.5, 67.9) | .017 |
| Mexican American | 65.8 (64.6, 67.0) | 65.0 (63.8, 66.2) | 65.0 (63.5, 66.5) | 65.1 (63.0, 67.3) | 64.9 (62.4, 67.4) | .179 | 65.5 (64.6, 66.4) | 64.0 (63.0, 65.0) | 65.6 (63.7, 67.5) | 66.1 (63.1, 69.2) | .616 |
| White | 62.8 (60.6, 64.9) | 63.5 (62.1, 64.9) | 63.8 (62.3, 65.4) | 66.2 (64.5, 67.9) | 67.1 (65.9, 68.4) | .006 | 60.9 (59.6, 62.2) | 63.2 (61.8, 64.6) | 65.0 (63.4, 66.7) | 68.1 (66.7, 69.5) | .026 |
| Sedentary behavior (age 12–19 y) | |||||||||||
| All | 18.3 (14.9, 22.2) | 17.4 (14.9, 20.1) | 10.6 (7.4, 15.0) | 8.9 (6.4, 12.4) | 6.3 (4.6, 8.6) | .007 | 20.0 (16.8, 23.7) | 11.7 (9.0, 15.0) | 10.1 (8.0, 12.8) | 7.4 (5.3, 10.3) | .013 |
| Black | 20.0 (16.2, 24.5) | 23.6 (20.2, 27.5) | 17.7 (13.9, 22.4) | 17.1 (12.4, 23.2) | 14.5 (10.7, 19.4) | .103 | 23.8 (19.0, 29.2) | 20.0 (16.1, 24.6) | 14.2 (10.9, 18.3) | 14.2 (10.1, 19.6) | .086 |
| Mexican American | 19.7 (16.5, 23.4) | 17.8 (13.9, 22.6) | 14.3 (10.0, 20.0) | 13.1 (7.4, 21.9) | 10.4 (5.7, 18.2) | .002 | 19.7 (16.7, 23.1) | 21.0 (15.7, 27.6) | 13.3 (9.7, 18.1) | 10.7 (5.7, 19.0) | .162 |
| White | 17.1 (11.3, 25.1) | 15.6 (11.8, 20.3) | 8.5 (4.8, 14.4) | 7.6 (4.8, 11.8) | 5.4 (3.5, 8.3) | .017 | 18.0 (11.3, 27.5) | 8.7 (5.7, 13.0) | 9.2 (6.7, 12.4) | 6.7 (4.4, 9.9) | .113 |
| Life expectancy (at age 25) | |||||||||||
| All | 49.2 (48.8, 49.7) | 51.4 (51.1, 51.8) | 53.8 (53.6, 54.1) | 55.7 (55.5, 56.0) | .020 | 50.7 (50.3, 51.0) | 53.9 (53.6, 54.1) | 55.0 (54.7, 55.3) | 56.4 (56.1, 56.7) | .001 | |
| Black | 45.5 (44.5, 46.5) | 48.0 (46.9, 49.1) | 50.7 (49.9, 51.6) | 52.6 (51.5, 53.7) | .025 | 47.0 (46.0, 47.9) | 49.9 (49.0, 50.8) | 50.9 (49.4, 52.3) | 52.3 (50.7, 53.8) | .001 | |
| Hispanic | 53.6 (52.6, 54.6) | 53.9 (53.0, 54.8) | 56.7 (55.9, 57.5) | 56.5 (55.4, 57.7) | .140 | 54.5 (53.8, 55.1) | 56.4 (55.4, 57.4) | 55.5 (53.9, 57.1) | 57.4 (55.7, 59.0) | .066 | |
| White | 49.0 (48.4, 49.6) | 51.4 (51.0, 51.8) | 53.8 (53.6, 54.1) | 55.8 (55.6, 56.0) | .022 | 50.1 (49.7, 50.6) | 54.1 (53.8, 54.3) | 55.2 (54.9, 55.5) | 56.5 (56.2, 56.8) | .011 | |
| Health status not excellent or very good (age 25–74 y) | |||||||||||
| All | 77.4 (76.7, 78.1) | 54.6 (54.2, 55.0) | 44.9 (44.5, 45.3) | 30.0 (29.7, 30.3) | .002 | ||||||
| Black | 72.7 (70.7, 74.6) | 62.1 (61.0, 63.3) | 54.7 (53.5, 56.0) | 43.6 (42.2, 45.0) | .023 | ||||||
| Hispanic | 84.2 (83.1, 85.2) | 68.2 (66.8, 69.5) | 55.6 (54.0, 57.3) | 42.9 (41.3, 44.5) | .012 | ||||||
| American Indian/Alaskan Native | 70.6 (64.2, 77.0) | 60.9 (57.3, 64.4) | 57.5 (54.1, 60.9) | 41.7 (37.4, 46.0) | .070 | ||||||
| Native Hawaiian/Pacific Islander | 69.8 (59.7, 80.0) | 54.5 (46.0, 63.1) | 45.4 (38.2, 52.6) | 36.0 (28.8, 43.2) | .004 | ||||||
| Asian | 70.3 (60.8, 79.7) | 59.5 (54.6, 64.4) | 48.6 (44.0, 53.1) | 39.5 (37.5, 41.5) | .015 | ||||||
| White | 69.4 (68.4, 70.4) | 50.0 (49.5, 50.4) | 41.4 (41.0, 41.8) | 26.7 (26.4, 27.0) | .004 | ||||||
| Activity limited due to chronic disease (age ≥ 25 y) | |||||||||||
| All | 32.2 (31.3, 33.1) | 22.4 (21.9, 23.0) | 16.0 (15.6, 16.5) | 12.9 (12.4, 13.4) | 9.4 (9.1, 9.6) | .014 | 23.5 (22.9, 24.1) | 16.1 (15.8, 16.4) | 15.0 (14.7, 15.4) | 9.3 (9.0, 9.7) | .017 |
| Black | 36.2 (34.6, 37.9) | 23.9 (22.7, 25.1) | 16.1 (14.9, 17.4) | 13.3 (11.9, 14.9) | 9.5 (8.6, 10.5) | .020 | 29.7 (28.3, 31.2) | 19.4 (18.5, 20.4) | 17.2 (16.2, 18.2) | 11.1 (10.1, 12.2) | .004 |
| Hispanic | 22.8 (21.6, 24.0) | 15.0 (14.2, 15.9) | 12.1 (11.1, 13.0) | 10.1 (8.6, 11.8) | 8.1 (7.2, 9.1) | .030 | 15.5 (14.9, 16.1) | 13.2 (12.4, 14.1) | 12.5 (11.2, 13.8) | 10.1 (9.0, 11.4) | .010 |
| White | 36.4 (35.0, 37.7) | 25.2 (24.4, 26.0) | 17.2 (16.7, 17.7) | 13.5 (12.9, 14.1) | 9.6 (9.3, 9.9) | .015 | 28.3 (27.3, 29.3) | 16.3 (15.9, 16.7) | 15.2 (14.9, 15.6) | 9.4 (9.0, 9.8) | .025 |
| Coronary heart disease (age ≥ 25 y) | |||||||||||
| All | 16.8 (16.2, 17.5) | 14.2 (13.7, 14.8) | 12.5 (12.0, 12.9) | 12.3 (11.8, 12.9) | 11.5 (11.1, 11.8) | .041 | 14.6 (14.1, 15.0) | 12.4 (12.1, 12.7) | 13.5 (13.2, 13.9) | 11.1 (10.8, 11.5) | .179 |
| Black | 16.9 (15.6, 18.4) | 12.8 (11.7, 13.9) | 10.1 (8.8, 11.7) | 8.2 (6.7, 10.1) | 8.9 (7.5, 10.6) | .049 | 14.5 (13.4, 15.7) | 10.6 (9.9, 11.4) | 11.7 (10.5, 13.0) | 9.8 (8.5, 11.3) | .141 |
| Hispanic | 12.7 (11.6, 13.8) | 10.2 (9.3, 11.1) | 8.1 (6.8, 9.7) | 8.0 (6.4, 10.0) | 7.3 (5.7, 9.3) | .032 | 9.6 (8.9, 10.3) | 9.5 (8.4, 10.7) | 11.1 (9.3, 13.2) | 8.9 (7.4, 10.5) | .951 |
| White | 18.4 (17.4, 19.4) | 15.5 (14.8, 16.3) | 13.2 (12.7, 13.8) | 13.1 (12.5, 13.7) | 11.8 (11.5, 12.2) | .031 | 16.9 (16.2, 17.6) | 12.9 (12.5, 13.3) | 14.0 (13.6, 14.4) | 11.4 (11.0, 11.8) | .136 |
| Diabetes (age 20–64 y) | |||||||||||
| All | 11.3 (8.6, 14.8) | 10.1 (7.4, 13.6) | 9.9 (6.7, 14.4) | 5.8 (3.8, 8.7) | 4.5 (3.2, 6.3) | .006 | 10.0 (8.1, 12.2) | 6.9 (5.0, 9.5) | 7.3 (5.5, 9.7) | 4.1 (2.9, 5.8) | .035 |
| Black | 17.0 (11.1, 25.1) | 10.9 (6.7, 17.4) | 12.3 (7.5, 19.5) | 9.5 (4.0, 21.0) | 7.7 (4.3, 13.3) | .045 | 15.8 (11.4, 21.5) | 9.8 (6.5, 14.3) | 10.6 (7.1, 15.5) | 7.3 (4.0, 12.9) | .057 |
| Mexican American | 15.3 (11.1, 20.8) | 7.7 (5.2, 11.3) | 9.8 (5.4, 16.9) | 8.8 (4.3, 17.0) | 9.5 (5.0, 17.2) | .586 | 11.1 (8.0, 15.3) | 6.7 (4.0, 11.0) | 12.9 (5.7, 26.7) | 8.1 (3.7, 16.6) | .401 |
| White | 8.8 (5.7, 13.3) | 10.4 (7.0, 15.3) | 9.2 (5.0, 16.4) | 5.0 (3.0, 8.2) | 4.2 (2.8, 6.1) | .031 | 6.9 (4.7, 10.0) | 6.7 (4.6, 9.7) | 6.7 (4.7, 9.3) | 3.8 (2.5, 5.7) | .192 |
| Obesity (age ≥ 20 y) | |||||||||||
| All | 35.6 (32.9, 38.3) | 34.6 (32.1, 37.3) | 35.4 (32.1, 38.7) | 31.2 (27.7, 35.0) | 26.7 (24.4, 29.2) | .018 | 34.7 (31.9, 37.7) | 33.6 (31.6, 35.6) | 32.5 (29.9, 35.2) | 24.9 (22.4, 27.6) | .182 |
| Black | 39.9 (34.8, 45.3) | 42.5 (38.2, 47.0) | 47.4 (41.3, 53.5) | 36.9 (30.9, 43.3) | 37.3 (32.8, 42.1) | .406 | 41.9 (39.0, 44.9) | 42.1 (37.3, 47.1) | 40.3 (36.7, 44.0) | 38.2 (32.9, 43.7) | .166 |
| Mexican American | 34.6 (30.1, 39.5) | 31.0 (26.6, 35.7) | 34.9 (30.2, 39.9) | 38.4 (33.1, 44.1) | 36.5 (31.1, 42.2) | .283 | 34.0 (30.7, 37.4) | 34.1 (28.5, 40.2) | 33.7 (28.1, 39.9) | 31.9 (24.6, 40.2) | .336 |
| White | 34.2 (30.7, 37.9) | 33.6 (30.0, 37.4) | 33.4 (29.3, 37.8) | 30.3 (26.2, 34.7) | 25.7 (23.2, 28.3) | .010 | 31.5 (27.1, 36.2) | 32.5 (30.2, 34.9) | 31.3 (28.4, 34.3) | 23.8 (21.1, 26.6) | .247 |
Note. FPL = federal poverty level.
Income categories for life expectancy were as follows: ≤ 100%, 101%–200%, 201%–400%, and > 400%.
Education categories for infant mortality were as follows: < 12 years, 12 years, 13–15 years, and ≥ 16 years.
Except for the following: infant mortality (per 1000 live births), Healthy Eating Index (average score), and life expectancy (years).
By the F test.
Racial/ethnic categories for US population percentages, family income as follows: all combined; Black, non-Hispanic; Hispanic, of any race; White, non-Hispanic. Data source: Current Population Survey, 2008 Annual Social and Economic Supplement.69 Racial/ethnic categories for US population percentages, educational attainment: all combined; Black or African American; Hispanic or Latino; White, non-Hispanic or Latino. Data source: 2005–2007 American Community Survey, 2005-2007.70
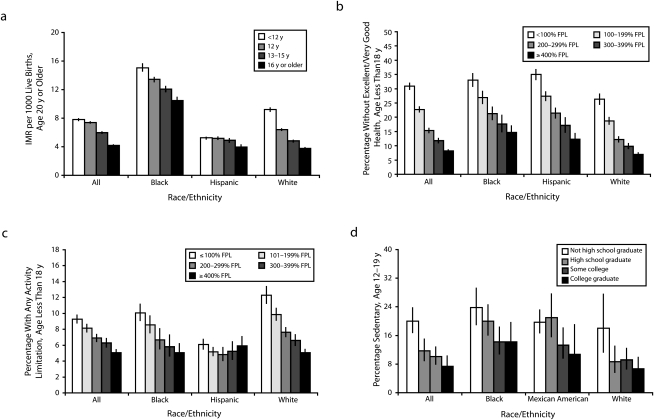
FIGURE 1.
Income and education disparities in child health by (a) infant mortality, (b) health status, (c) activity limitation, and (d) sedentary behavior: United States, 1999–2005.
Note. FPL = federal poverty level; IMR = infant mortality rate; Black = non-Hispanic Black; White = non-Hispanic White. All racial/ethnic groups are mutually exclusive. Source. Data for panel a is from the Period Linked Birth/Infant Death Data File, 2000-2002.46 Data for panels b and c are from the National Health Interview Survey, 2001-2005.48 Data for panel d is from the National Health and Nutrition Examination Survey, 1999-2004.49
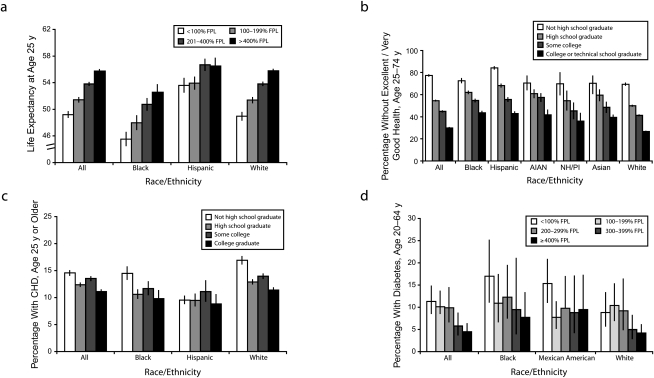
FIGURE 2.
Income and education disparities in adult health by (a) life expectancy, (b) health status, (c) heart disease, and (d) diabetes: United States, 1988–2007.
Note. FPL = federal poverty level; CHD = coronary heart disease; Asian = non-Hispanic Asian; AIAN = non-Hispanic American Indian or Alaskan Native; Black = non-Hispanic Black; NH/PI = non-Hispanic Native Hawaiian or Pacific Islander; White = non-Hispanic White. All racial/ethnic groups are mutually exclusive. Source. Data for panel a is from the National Longitudinal Mortality Study, 1988–1998.47 Data for panel b is from the Behavioral Risk Factor Surveillance System, 2005–2007.50 Data for panel c is from the National Health Interview Survey, 2001–2005.48 Data for panel d is from the National Health and Nutrition Examination Survey, 1999–2004.49
RESULTS
Results are presented first for the child health indicators and then for adult health. Table 2 included all results, which are illustrated in Figure 1 (child health) and Figure 2 (adult health).
Child Health
Table 2 includes all results by income and education for the 5 child health indicators. Figure 1 displays patterns in infant mortality by mother's educational attainment, in health status and activity limitation due to chronic disease by family income as a percentage of the federal poverty level, and in sedentary behavior among adolescents by head of household's educational attainment. The first online supplemental figure displays patterns in health status, activity limitation caused by chronic disease, and healthy eating behavior by head of household's educational attainment, and in healthy eating behavior and sedentary behavior among adolescents by family income as a percentage of the federal poverty level.
Examining differences in indicator levels by income and education within the overall population, we found that—with the exception of activity limitation, for which no education gradient was apparent—the patterns were consistent with a socioeconomic gradient: whereas the most adverse levels of health were observed for the least-educated or lowest-income groups, improvements in health generally were seen at each higher level of socioeconomic advantage. Looking at income and education differences within racial or ethnic subgroups, we found similar stepwise patterns among both White and Black children in every indicator except sedentary behavior, for which the education gradient among Whites and income gradient among Blacks were less apparent. Among Hispanic or Mexican American children, gradient patterns were seen for health status by both income and education and for sedentary behavior by income only, but not for infant mortality, activity limitation, or healthy eating behaviors.
Adult Health
Table 2 also includes results by income and education for each of the 6 adult health indicators. Figure 2 displays patterns in self-reported health status and coronary heart disease by education and in life expectancy at age 25 and diabetes by income. The second online supplemental figure displays patterns in life expectancy, activity limitation due to a chronic disease, diabetes, and obesity by education and in activity limitation, heart disease, and obesity by income. In the overall population, gradients were observed as follows: gradients by both income and education for life expectancy at age 25, activity limitation, and diabetes; gradients by education for health status; gradients by income but not by education for coronary heart disease; and gradients by education but not by income for obesity. Gradients by income were apparent in every racial or ethnic subgroup for activity limitation and coronary heart disease; among Whites and Blacks but not Hispanics or Mexican Americans for life expectancy and diabetes; and among Whites but not Blacks or Mexican Americans for obesity. Gradients by education were apparent in every racial or ethnic group for life expectancy, health status, and activity limitation; among Blacks only for diabetes; and in none of the racial or ethnic subgroups for coronary heart disease or obesity.
DISCUSSION
Our findings revealed pervasive—albeit not invariable—patterns suggesting incremental income or education gradients for a range of important health indicators among both children and adults in the United States. For most of the indicators examined here, clear, stepwise patterns were generally seen among Whites and Blacks but less consistently among Hispanics or Mexican Americans. Although their slopes appeared to vary, most of the observed gradients were statistically significant on the basis of tests of linear trend. Overall, these findings confirm earlier evidence from the United States and other countries indicating that relative advantage often (though not always) shapes health not only above and below specified income or education thresholds but across a wide socioeconomic spectrum. Those at the bottom—the poor and least educated—generally experience the worst health, but even those with intermediate levels of income and education are less healthy than the wealthiest and most educated.
Some health indicators did not follow a clear socioeconomic gradient in any racial or ethnic group. Inconsistent patterns in socioeconomic disparities in obesity have been noted previously51–55 and may be relevant to the patterns observed here in healthy eating and diabetes, which are closely related to obesity. Different health outcomes can have distinct causal pathways, and different populations in different contexts can experience unique combinations of mediating and effect-modifying factors, making it unsurprising that patterns would vary across different indicators; furthermore, social disparities in some indicators are known to vary by age56 or life stage,57 gender,54,58 nativity,54 geographic location,59,60 socioeconomic measure,61,62 or historical period.63–65 Given this causal complexity and the wide array of both child and adult indicators examined here, the relative consistency of our findings for most indicators is particularly striking.
Examining Class and Race Jointly
Our main objective was to examine disparities in health by income and education in the United States, where routine public health data and discourse have typically focused on measuring and reporting health disparities by race and ethnicity. Our results illustrate the importance of examining both socioeconomic and racial/ethnic disparities, separately and jointly. Kawachi et al. noted that “Much of the history of thinking about inequality in the United States, including health inequality, has usually been framed in terms of race or class, but seldom both.”66(p347) The absence of adequate data on socioeconomic differences overall and within racial/ethnic groups can lead policymakers, researchers, and practitioners to make unfounded assumptions about the nature of both socioeconomic and racial disparities.61 Our findings demonstrated, for example, that for many of the child and adult health indicators examined, socioeconomic differences within Black and White racial/ethnic groups were at least as striking as socioeconomic differences overall. Consistent with previous literature,67 socioeconomic gradients in health were seen least frequently among Hispanics, perhaps reflecting the “Hispanic paradox” of good health despite relatively low incomes and educational attainment; the higher life expectancy among Hispanics may also, however, reflect data quality issues, including misclassification of Hispanic names and underreporting of Hispanic deaths.68 Although some evidence suggested that socioeconomic disparities for Hispanics may vary by nativity,54,71 we did not examine differences by nativity in this study.
Our findings also revealed other important differences in levels of health when both race/ethnicity and socioeconomic level were considered. The results for several indicators, including infant mortality and adult life expectancy, for example, revealed that Blacks have worse outcomes than do Whites at each level of income or education. Blacks may not experience the same health benefits from a given level of income or education as Whites; this could potentially be explained by adverse health effects of more concentrated disadvantage (e.g., far lower levels of wealth and greater likelihood of living in more disadvantaged neighborhoods at a given level of income) or a range of experiences related to racial bias that are not captured by routinely collected socioeconomic measures.61,72–74
Limitations
The approach we used revealed the magnitude of relative differences in health across socioeconomic and racial or ethnic groups, but disparities in the total burden of ill health across groups, reflecting differences in their underlying socioeconomic distributions, should be considered as well. As shown by data at the top of Table 2, Blacks and Hispanics have far higher rates of poverty, near-poverty, and low educational attainment than do Whites, for example, and are underrepresented at higher levels of income and education. Given these differences in income distributions, the shorter average life expectancy at age 25 for poor adults applies to more than 1 in 5 Black and Hispanic adults and fewer than 1 in 10 White adults. Conversely, the longer average life expectancy for the highest-income adults is experienced by nearly half of White adults, compared with only 1 in 5 Blacks and Hispanics.
Although we can only conjecture, our findings may understate the extent of socioeconomic inequalities in health. The highest income group we were able to examine—persons with incomes over 400% of federal poverty level, or approximately $88 200 for a family of 4 during 200975—comprises 38.5% of the US population. Findings from studies that have examined more socioeconomic groups44,76,77 suggest that we might have observed even greater disparities if our data sources had permitted us to use higher income cutoffs. On the other hand, some experts have noted that there may be a threshold in the health benefits of higher income, with a leveling off at a certain point in the income distribution78,79; even if this is the case, however, the threshold may occur at a considerably higher level than the upper limit we were able to observe here. In addition, clustering of adverse socioeconomic factors (including neighborhood socioeconomic characteristics, wealth, and other factors not measured here), which is particularly likely among Blacks and Hispanics,61,80,81 suggests that the true magnitude of socioeconomic differences—overall and particularly across racial or ethnic groups—may be considerably larger than that observed for income or education alone.61,80,82–85
Links Between Social Advantage and Health
The striking socioeconomic gradient patterns observed in a variety of health indicators suggest a dose–response relationship for many health indicators, with factors related to social and economic advantage reflected by income and educational attainment. Along with biological plausibility and other criteria, a dose–response relationship is a standard criterion for inferring causality.86 Results of these observational and unadjusted analyses certainly do not establish a causal role for income or educational attainment per se. However, the findings add to and support a large and growing body of evidence, including research identifying pathways and physiological mechanisms, that suggests likely causal roles in many health conditions for factors tightly linked with income and education.87–91 Although income or education deficits in and of themselves are unlikely to be the immediate proximate cause of poorer health, ample evidence from the United States and other countries supports the fundamental, powerful, and pervasive links between income and education and access to a range of opportunities and resources that shape health through myriad, often complex, pathways and physiological mechanisms.
Although reverse causation—with poor health leading to lower income—may in part explain the observed income gradients in health, it is a less likely explanation for the education gradients observed for most of the indicators we examined. Medical care is one of the resources for health linked with income (or with a good job, which often depends on education). Lack of health insurance can affect health by limiting both access to needed medical care and the ability to pay for other necessities, including food and housing, when serious illness strikes. Previous studies, however, tell us that although medical care may make an important contribution to socioeconomic inequalities in health,92,93 medical care alone is unlikely to be the primary explanation for worsening health with decreasing levels of income, and there is wide and growing consensus that, in general, the impact of medical care on health is likely to be limited relative to the impacts of social and physical environments.59,94–98
Policy Implications
These findings have important implications for efforts to reduce social disparities in health. Gradient patterns suggest the need for strategies that address factors affecting a large proportion of the population across a wide socioeconomic spectrum, rather than focusing exclusively on those at greatest disadvantage. There may, however, be tension between population-wide and targeted approaches, particularly when resources are scarce. Awareness of gradients should not be used to justify diverting resources from those who have both the greatest deficits in health and the most limited means of escaping the social disadvantage that produces health disadvantage. Wider awareness of the socioeconomic gradients in health among the public and policymakers, however, could lead to more effective policies by increasing understanding of how social disparities in health are created and perpetuated, and potentially by building greater middle-class “buy-in” for policies addressing the social determinants of health.
It also is worth stressing that awareness of socioeconomic disparities in health, whether in the form of gradients or other patterns, should not justify inattention to racial or ethnic disparities. On several indicators, Blacks did worse than Whites at each income and education level—suggesting that these systematic racial or ethnic differences are unlikely to respond to purely socioeconomic strategies but rather require additional steps to address profoundly embedded structural factors, such as racial residential segregation, that disadvantage Blacks at all socioeconomic levels. Our findings reinforced the importance of examining both socioeconomic and racial or ethnic disparities, jointly whenever possible, as well as changes in patterns over time in relation to policies that may have an impact—positive or negative—on disparities.
Many people in this country have been brought up to take pride in seeing the United States as a classless society. Unfortunately, our findings not only confirmed the existence of profound racial or ethnic differences in health, which have been extensively documented previously,28,99,100 but also revealed pervasive social class differences in health in this country. The income and education gradients in health observed here suggest fundamental links between hierarchies of social and economic advantage and hierarchies of health. We know from extensive literature that health differences according to income and education reflect differences in material and psychosocial advantages and disadvantages that should be modifiable with social policies, including but not limited to policies affecting medical care.94
The health of the most socially advantaged group in a society indicates a level of health that should be possible for everyone101; these gradients thus reveal that the large majority of the US population—overall and across racial or ethnic groups—is not as healthy as it could be. From an ethical and human rights perspective, it is unacceptable for so many people to be less healthy than they could be, on the basis of their (or their parents') income or educational attainment—particularly because unhealthy individuals are less able to escape from poverty and social disadvantage.101 The steep socioeconomic gradients in most children's health indicators examined here are especially disturbing, given that health during childhood lays the foundation for health and economic well-being across the life course. These patterns also are troubling from a pragmatic perspective, given that a nation's health influences its economic productivity.102 Lack of attention to these patterns in routine health data reflects a long-standing tradition in the United States of making race “a highly visible feature of public policy while hiding or disguising anything that resembles class.”66(p347) Interpreted in light of a large body of previous research, our findings tell us that most members of our society fail to reach their full health potential, that the underlying reasons are likely to be closely linked with modifiable social conditions, and that both targeted and broader, population-wide social policies are needed to reduce socioeconomic and racial or ethnic disparities in health.
Acknowledgments
We acknowledge support from the Robert Wood Johnson Foundation (RWJF) for much of the analytic work for this study as part of the research effort informing the RWJF Commission to Build a Healthier America.
We thank Colleen Barclay for her assistance in multiple phases of the research; Norman J. Johnson, PhD, US Census Bureau, for his analyses of data from the National Longitudinal Mortality Study; Mah-Jabeen Soobader, PhD, for her analyses of data from the National Health Interview Survey; Tabashir Sadegh-Nobari, Jane An, Mercedes Dekker, Rebecca Grossman-Kahn, and Teri Moore for their assistance with the research; and Rebecca Wilson-Loots for her assistance with preparing the article.
Human Participant Protection
Approval for this study was obtained from the University of California, San Francisco, Human Subjects Protection Program.
References
- 1.Fox AJ. Longitudinal studies based on vital registration records. Rev Epidemiol Sante Publique. 1989;37(5–6):443–448 [PubMed] [Google Scholar]
- 2.Krieger N, Fee E. Measuring social inequalities in health in the United States: a historical review, 1900–1950. Int J Health Serv. 1996;26(3):391–418 [DOI] [PubMed] [Google Scholar]
- 3.Liberatos P, Link BG, Kelsey JL. The measurement of social class in epidemiology. Epidemiol Rev. 1988;10:87–121 [DOI] [PubMed] [Google Scholar]
- 4.Susser M, Watson W, Hopper K. Sociology in Medicine. 3rd ed. New York, NY: Oxford University Press; 1985 [Google Scholar]
- 5.Office for National Statistics, UK The National Statistics Socio-Economic Classification (NS-SEC). Available at: http://www.ons.gov.uk/about-statistics/classifications/current/ns-sec/index.html. Accessed July 17, 2009
- 6.Kunst AE, Mackenbach JP. International variation in the size of mortality differences associated with occupational status. Int J Epidemiol. 1994;23(4):742–750 [DOI] [PubMed] [Google Scholar]
- 7.Rose D, Pevalin DJ, Elias P, Martin J. Towards a European Socio-Economic Classification: Final Report to Eurostat of the Expert Group. London, England: Office for National Statistics and Institute for Social and Economic Research, University of Essex; 2001 [Google Scholar]
- 8.Krieger N, Chen JT, Ebel G. Can we monitor socioeconomic inequalities in health? A survey of US health departments' data collection and reporting practices. Public Health Rep. 1997;112(6):481–491 [PMC free article] [PubMed] [Google Scholar]
- 9.US Dept of Health and Human Services Healthy People 2010: midcourse review. Available at: http://www.healthypeople.gov/data/midcourse. Accessed July 22, 2009
- 10.America's Children: Key National Indicators of Well-Being, 2009. Washington, DC: Federal Interagency Forum on Child and Family Statistics; Available at: http://www.childstats.gov/pdf/ac2009/ac_09.pdf. Accessed July 27, 2009 [Google Scholar]
- 11.Pleis JR, Lucas JW. Summary health statistics for US adults: National Health Interview Survey, 2007. National Center for Health Statistics. Vital Health Stat 10. 2009;No. 240. Available at: http://www.cdc.gov/nchs/data/series/sr_10/sr10_240.pdf. Accessed July 27, 2009 [PubMed]
- 12.Bloom B, Cohen RA. Summary health statistics for US children: National Health Interview Survey, 2007. National Center for Health Statistics. Vital Health Stat 10. 2009;No. 239. Available at: http://www.cdc.gov/nchs/data/series/sr_10/sr10_239.pdf. Accessed July 27, 2009 [PubMed]
- 13.McDowell MA, Fryar CD, Ogden CL. Anthropometric reference data for children and adults: United States, 1988–1994. National Center for Health Statistics. Vital Health Stat 11. 2009;No. 249. Available at: http://www.cdc.gov/nchs/data/series/sr_11/sr11_249.pdf. Accessed July 27, 2009 [PubMed]
- 14.Jones AL, Dwyer LL, Bercovitz AR, Strahan GW. The National Nursing Home Survey: 2004 overview. National Center for Health Statistics. Vital Health Stat 13. 2009;No. 167. Available at: http://www.cdc.gov/nchs/data/series/sr_13/sr13_167.pdf. Accessed July 27, 2009 [PubMed]
- 15.Martin JA, Hamilton BE, Sutton PD, et al. Births: final data for 2006. Natl Vital Stat Rep. January 7, 2009;57(7). Available at: http://www.cdc.gov/nchs/data/nvsr/nvsr57/nvsr57_07.pdf. Accessed July 27, 2009 [PubMed]
- 16.MacDorman MF, Kirmeyer S. Fetal and perinatal mortality, United States, 2005. Natl Vital Stat Rep. January 28, 2009;57(8). Available at: http://www.cdc.gov/nchs/data/nvsr/nvsr57/nvsr57_08.pdf. Accessed July 27, 2009 [PubMed]
- 17.Hamilton BE, Martin JA, Ventura SJ. Births: preliminary data for 2007. Natl Vital Stat Rep. March 18, 2009;57(12). Available at: http://www.cdc.gov/nchs/data/nvsr/nvsr57/nvsr57_12.pdf. Accessed July 27, 2009 [PubMed]
- 18.Heron MP, Hoyert DL, Murphy SL, Xu JQ, Kochanek KD, Tejada-Vera B. Deaths: final data for 2006. Natl Vital Stat Rep. April 17, 2009;57(14). Available at: http://www.cdc.gov/nchs/data/nvsr/nvsr57/nvsr57_14.pdf. Accessed July 27, 2009 [PubMed]
- 19.Ervin RB. Prevalence of metabolic syndrome among adults 20 years of age and over, by sex, age, race and ethnicity, and body mass index: United States, 2003–2006. Natl Health Stat Rep. May 5, 2009;No. 13. Available at: http://www.cdc.gov/nchs/data/nhsr/nhsr013.pdf. Accessed July 27, 2009 [PubMed] [Google Scholar]
- 20.Fryar CD, Merino MC, Hirsch R, Porter KS. Smoking, alcohol use, and illicit drug use reported by adolescents aged 12–17 years: United States, 1999–2004. Natl Health Stat Rep. May 20, 2009;No. 15. Available at: http://www.cdc.gov/nchs/data/nhsr/nhsr015.pdf. Accessed July 27, 2009 [PubMed] [Google Scholar]
- 21.Schoenborn CA, Heyman KM. Health characteristics of adults aged 55 years and over: United States, 2004–2007. Natl Health Stat Rep. July 8, 2009;No. 16. Available at: http://www.cdc.gov/nchs/data/nhsr/nhsr016.pdf. Accessed July 27, 2009 [PubMed] [Google Scholar]
- 22.Holmes J, Powell-Griner E, Lethbridge-Cejku M, Heyman K. Aging differently: Physical limitations among adults aged 50 years and over: United States, 2001–2007. NCHS Data Brief. July 2009;No. 20. Available at: http://www.cdc.gov/nchs/data/databriefs/db20.pdf. Accessed July 27, 2009 [PubMed]
- 23.Goodwin P, McGill B, Chandra A. Who marries and when? Age at first marriage in the United States, 2002. NCHS Data Brief. June 2009;No. 19. Available at: http://www.cdc.gov/nchs/data/databriefs/db19.pdf. Accessed July 27, 2009 [PubMed]
- 24.Ventura SJ. Changing patterns of nonmarital childbearing in the United States. NCHS Data Brief. May 2009;No. 18. Available at: http://www.cdc.gov/nchs/data/databriefs/db18.pdf. Accessed July 27, 2009 [PubMed]
- 25.Wright JD, Hirsch R, Wang C-Y. One-third of US adults embraced most heart healthy behaviors in 1999–2002. NCHS Data Brief. May 2009;No. 17. Available at: http://www.cdc.gov/nchs/data/databriefs/db17.pdf. Accessed July 27, 2009 [PubMed]
- 26.MacDorman MF, Kirmeyer S. The challenge of fetal mortality. NCHS Data Brief. April 2009;No. 16. Available at: http://www.cdc.gov/nchs/data/databriefs/db16.pdf. Accessed July 27, 2009 [PubMed]
- 27.Park-Lee E, Caffrey C. Pressure ulcers among nursing home residents: United States, 2004. NCHS Data Brief. February 2009;No. 14. Available at: http://www.cdc.gov/nchs/data/databriefs/db14.pdf. Accessed July 27, 2009 [PubMed]
- 28.Health, United States, 2008, With Chartbook. Hyattsville, MD: National Center for Health Statistics; 2009. Available at: http://www.cdc.gov/nchs/data/hus/hus08.pdf. Accessed July 22, 2009 [Google Scholar]
- 29.Schiller JS, Euler GL. Vaccination coverage estimates from the National Health Interview Survey: United States, 2008. NCHS Health E-Stats. 2009. Available at: http://www.cdc.gov/nchs/data/hestat/vaccine_coverage.pdf. Accessed July 27, 2009
- 30.Fryar CD, Ogden CL. Prevalence of underweight among adults: United States, 2003–2006. NCHS Health E-Stats. 2009. Available at: http://www.cdc.gov/nchs/data/hestat/underweight_adults.pdf. Accessed July 27, 2009
- 31.Fryar CD, Ogden CL. Prevalence of underweight among children and adolescents: United States, 2003–2006. NCHS Health E-Stats. 2009. Available at: http://www.cdc.gov/nchs/data/hestat/underweight_children.pdf. Accessed July 27, 2009
- 32.Mathews TJ. Trends in spina bifida and anencephalus in the United States, 1991–2006. NCHS Health E-Stats. 2009. Available at: http://www.cdc.gov/nchs/data/hestat/spine_anen.pdf. Accessed July 27, 2009
- 33.Health, United States, 1998, With Socioeconomic Status and Health Chartbook. Hyattsville, MD: National Center for Health Statistics; 1998. Available at: http://www.cdc.gov/nchs/data/hus/hus98.pdf. Accessed July 27, 2009 [Google Scholar]
- 34.National Center for Health Statistics Vital and Health Statistics, Series 10: data from the National Health Interview Survey. Available at: http://www.cdc.gov/nchs/products/series.htm#sr10. Accessed July 23, 2009
- 35.Agency for Healthcare Research and Quality National Healthcare Disparities Reports, Appendix D: Data Tables. Available at: http://www.ahrq.gov/qual/measurix.htm. Accessed July 23, 2009
- 36.Adler N, Boyce T, Chesney MA, Folkman S, Syme SL. Socioeconomic inequalities in health. No easy solution. JAMA. 1993;269(24):3140–3145 [PubMed] [Google Scholar]
- 37.Macintyre S. Understanding the social patterning of health: the role of the social sciences. J Public Health Med. 1994;16(1):53–59 [DOI] [PubMed] [Google Scholar]
- 38.Wilkinson RG, Pickett KE. The problems of relative deprivation: why some societies do better than others. Soc Sci Med. 2007;65(9):1965–1978 [DOI] [PubMed] [Google Scholar]
- 39.Marmot MG, Bosma H, Hemingway H, Brunner E, Stansfeld S. Contribution of job control and other risk factors to social variations in coronary heart disease incidence. Lancet. 1997;350(9073):235–239 [DOI] [PubMed] [Google Scholar]
- 40.Braveman P, Marchi K, Egerter S, et al. Poverty, near-poverty, and hardship around the time of pregnancy. Matern Child Health J. 2008 Nov 27. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 41.Orpana HM, Lemyre L. Explaining the social gradient in health in Canada: using the National Population Health Survey to examine the role of stressors. Int J Behav Med. 2004;11(3):143–151 [DOI] [PubMed] [Google Scholar]
- 42.Kanjilal S, Gregg EW, Cheng YJ, et al. Socioeconomic status and trends in disparities in 4 major risk factors for cardiovascular disease among US adults, 1971–2002. Arch Intern Med. 2006;166(21):2348–2355 [DOI] [PubMed] [Google Scholar]
- 43.Kennedy BP, Kawachi I, Glass R, Prothrow-Stith D. Income distribution, socioeconomic status, and self rated health in the United States: multilevel analysis. BMJ. 1998;317(7163):917–921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Minkler M, Fuller-Thomson E, Guralnik JM. Gradient of disability across the socioeconomic spectrum in the United States. N Engl J Med. 2006;355(7):695–703 [DOI] [PubMed] [Google Scholar]
- 45.Thurston RC, Kubzansky LD, Kawachi I, Berkman LF. Is the association between socioeconomic position and coronary heart disease stronger in women than in men? Am J Epidemiol. 2005;162(1):57–65 [DOI] [PubMed] [Google Scholar]
- 46.National Center for Health Statistics Period Linked Birth/Infant Death Data File, 2000–2002. Available at: http://www.cdc.gov/nchs/linked.htm. Accessed April 20, 2009
- 47.US Census Bureau National Longitudinal Mortality Study, 1988–1998. Available at: http://www.census.gov/nlms/index.html. Accessed April 20, 2009
- 48.Centers for Disease Control and Prevention National Health Interview Survey. Available at: http://www.cdc.gov/nchs/nhis.htm. Accessed April 20, 2009
- 49.Centers for Disease Control and Prevention National Health and Nutrition Examination Survey, 1999–2004. Available at: http://www.cdc.gov/nchs/nhanes.htm. Accessed April 20, 2009
- 50.Centers for Disease Control and Prevention Behavior Risk Factor Surveillance System, 2005–2007. Available at: http://www.cdc.gov/brfss. Accessed April 20, 2009
- 51.Burke GL, Jacobs DR, Sprafka JM, Savage PJ, Sidney S, Wagenknecht LE. Obesity and overweight in young adults: the CARDIA study. Prev Med. 1990;19(4):476–488 [DOI] [PubMed] [Google Scholar]
- 52.Chang VW, Lauderdale DS. Income disparities in body mass index and obesity in the United States, 1971–2002. Arch Intern Med. 2005;165(18):2122–2128 [DOI] [PubMed] [Google Scholar]
- 53.Goodman E. The role of socioeconomic status gradients in explaining differences in US adolescents' health. Am J Public Health. 1999;89(10):1522–1528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sanchez-Vaznaugh EV, Kawachi I, Subramanian SV, Sanchez BN, Acevedo-Garcia D. Do socioeconomic gradients in body mass index vary by race/ethnicity, gender, and birthplace? Am J Epidemiol. 2009;169(9):1102–1112 [DOI] [PubMed] [Google Scholar]
- 55.Wang Y, Beydoun MA. The obesity epidemic in the United States—gender, age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and meta-regression analysis. Epidemiol Rev. 2007;29:6–28 [DOI] [PubMed] [Google Scholar]
- 56.Ford G, Ecob R, Hunt K, Macintyre S, West P. Patterns of class inequality in health through the lifespan: class gradients at 15, 35 and 55 years in the west of Scotland. Soc Sci Med. 1994;39(8):1037–1050 [DOI] [PubMed] [Google Scholar]
- 57.Frank JW, Cohen R, Yen I, Balfour J, Smith M. Socioeconomic gradients in health status over 29 years of follow-up after midlife: the Alameda County Study. Soc Sci Med. 2003;57(12):2305–2323 [DOI] [PubMed] [Google Scholar]
- 58.Stafford M, Cummins S, Macintyre S, Ellaway A, Marmot M. Gender differences in the associations between health and neighborhood environment. Soc Sci Med. 2005;60(8):1681–1692 [DOI] [PubMed] [Google Scholar]
- 59.Egerter S, Braveman P, Pamuk E, et al. America's Health Starts With Healthy Children: How Do States Compare? Princeton, NJ: Robert Wood Johnson Foundation; 2008 [Google Scholar]
- 60.Riva M, Curtis S, Gauvin L, Fagg J. Unravelling the extent of inequalities in health across urban and rural areas: evidence from a national sample in England. Soc Sci Med. 2009;68(4):654–663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Braveman P, Cubbin C, Egerter S, et al. Socioeconomic status in health research: one size does not fit all. JAMA. 2005;294(22):2879–2888 [DOI] [PubMed] [Google Scholar]
- 62.Winkleby MA, Jatulis DE, Frank E, Fortmann SP. Socioeconomic status and health: how education, income, and occupation contribute to risk factors for cardiovascular disease. Am J Public Health. 1992;82(6):816–820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Black D, Morris JN, Smith C, Townsend P. The Black Report. : Townsend P, Davidson N, Whitehead M, Inequalities in Health: The Black Report and the Health Divide. London, England: Penguin Books; 1992:29–213 [Google Scholar]
- 64.Krieger N, Rehkopf DH, Chen JT, Waterman PD, Marcelli E, Kennedy M. The fall and rise of US inequities in premature mortality: 1960–2002. PLoS Med. 2008;5(2):e46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Pappas G, Queen S, Hadden W, Fisher G. The increasing disparity in mortality between socioeconomic groups in the United States, 1960 and 1986. N Engl J Med. 1993;329(2):103–109 [DOI] [PubMed] [Google Scholar]
- 66.Kawachi I, Daniels N, Robinson DE. Health disparities by race and class: why both matter. Health Aff (Millwood). 2005;24(2):343–352 [DOI] [PubMed] [Google Scholar]
- 67.Morales LS, Lara M, Kington RS, Valdez RO, Escarce JJ. Socioeconomic, cultural, and behavioral factors affecting Hispanic health outcomes. J Health Care Poor Underserved. 2002;13(4):477–503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Patel KV, Eschbach K, Ray LA, Markides KS. Evaluation of mortality data for older Mexican Americans: implications for the Hispanic paradox. Am J Epidemiol. 2004;159:707–715 [DOI] [PubMed] [Google Scholar]
- 69.US Census Bureau Current Population Survey, Annual Social and Economic Supplement, 2008. Available at: http://www.census.gov/cps. Accessed April 20, 2009
- 70.US Census Bureau American Community Survey, 2005-2007. Available at: http://www.census.gov/acs/www/index.html. Accessed April 20, 2009
- 71.Guendelman S, Gould JB, Hudes M, Eskenazi B. Generational differences in perinatal health among the Mexican American population: findings from HHANES 1982–84. Am J Public Health. 1990;80(suppl):61–65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Farmer MM, Ferraro KF. Are racial disparities in health conditional on socioeconomic status? Soc Sci Med. 2005;60(1):191–204 [DOI] [PubMed] [Google Scholar]
- 73.Nuru-Jeter A, Dominquez TP, Hammond WP, et al. “It's the skin you're in”: African-American women talk about their experiences of racism. An exploratory study to develop measures of racism for birth outcome studies. Matern Child Health J. 2009;13(1):29–39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Williams D, Mohammed SA. Discrimination and racial disparities in health: evidence and needed research. J Behav Med. 2009;32(1):20–47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.US Dept of Health and Human Services HHS poverty guidelines. Available at: http://aspe.hhs.gov/poverty/figures-fed-reg.shtml. Accessed April 20, 2009
- 76.Demakakos P, Nazroo J, Breeze E, Marmot M. Socioeconomic status and health: the role of subjective social status. Soc Sci Med. 2008;67(2):330–340 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Martikainen P, Makela P, Koskinen S, Valkonen T. Income differences in mortality: a register-based follow-up study of three million men and women. Int J Epidemiol. 2001;30(6):1397–1405 [DOI] [PubMed] [Google Scholar]
- 78.Ecob R, Smith GD. Income and health: what is the nature of the relationship? Soc Sci Med. 1999;48(5):693–705 [DOI] [PubMed] [Google Scholar]
- 79.Mackenbach JP, Martikainen P, Looman CW, Dalstra JA, Kunst AE, Lahelma E. The shape of the relationship between income and self-assessed health: an international study. Int J Epidemiol. 2005;34(2):286–293 [DOI] [PubMed] [Google Scholar]
- 80.Williams D. Race, socioeconomic status, and health: the added effects of racism and discrimination. Ann N Y Acad Sci. 1999;896:173–188 [DOI] [PubMed] [Google Scholar]
- 81.Williams D, Collins C. US socioeconomic and racial differences in health: patterns and explanations. Annu Rev Sociol. 1995;21:349–386 [Google Scholar]
- 82.Do DP, Finch BK. The link between neighborhood poverty and health: context or composition? Am J Epidemiol. 2008;168(6):611–619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Macintyre S. The social patterning of exercise behaviours: the role of personal and local resources. Br J Sports Med. 2000;34(1):6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Morenoff JD. Neighborhood mechanisms and the spatial dynamics of birth weight. Am J Sociol. 2003;108(5):976–1017 [DOI] [PubMed] [Google Scholar]
- 85.Steptoe A, Feldman PJ. Neighborhood problems as sources of chronic stress: development of a measure of neighborhood problems, and associations with socioeconomic status and health. Ann Behav Med. 2001;23(3):177–185 [DOI] [PubMed] [Google Scholar]
- 86.Greenberg RS, Daniels SR, Flanders WD, Eley JW, Boring JR. Medical Epidemiology. 4th ed. New York, NY: McGraw-Hill Professional; 2004 [Google Scholar]
- 87.Berkman LF. Social epidemiology: social determinants of health in the United States: are we losing ground? Annu Rev Public Health. 2009;30:27–41 [DOI] [PubMed] [Google Scholar]
- 88.Chandola T, Britton A, Brunner E, et al. Work stress and coronary heart disease: what are the mechanisms? Eur Heart J. 2008;29(5):640–648 [DOI] [PubMed] [Google Scholar]
- 89.Cubbin C, Winkleby MA. Protective and harmful effects of neighborhood-level deprivation on individual-level health knowledge, behavior changes, and risk of coronary heart disease. Am J Epidemiol. 2005;162(6):559–568 [DOI] [PubMed] [Google Scholar]
- 90.Kramer MS, Goulet L, Lydon J, et al. Socio-economic disparities in preterm birth: causal pathways and mechanisms. Paediatr Perinat Epidemiol. 2001;15(suppl 2):104–123 [DOI] [PubMed] [Google Scholar]
- 91.Marmot MG, Shipley MJ, Hemingway H, Head J, Brunner EJ. Biological and behavioural explanations of social inequalities in coronary heart disease: the Whitehall II Study. Diabetologia. 2008;51(11):1980–1988 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.James PD, Wilkins R, Detsky AS, Tugwell P, Manuel DG. Avoidable mortality by neighbourhood income in Canada: 25 years after the establishment of universal health insurance. J Epidemiol Community Health. 2007;61(4):287–296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Mackenbach JP, Stronks K, Kunst AE. The contribution of medical care to inequalities in health: differences between socio-economic groups in decline of mortality from conditions amenable to medical intervention. Soc Sci Med. 1989;29(3):369–376 [DOI] [PubMed] [Google Scholar]
- 94.Final Report of the Commission on Social Determinants of Health. Geneva, Switzerland: World Health Organization; 2008 [Google Scholar]
- 95.Marmot M, Friel S, Bell R, Houweling TA, Taylor S. Closing the gap in a generation: health equity through action on the social determinants of health. Lancet. 2008;372(9650):1661–1669 [DOI] [PubMed] [Google Scholar]
- 96.McGinnis JM, Foege WH. Actual causes of death in the United States. JAMA. 1993;270(18):2207–2212 [PubMed] [Google Scholar]
- 97.Ross CE, Mirowsky J. Does medical insurance contribute to socioeconomic differentials in health? Milbank Q. 2000;78(2):291–321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Schroeder SA. We can do better—improving the health of the American people. N Engl J Med. 2007;357(12):1221–1228 [DOI] [PubMed] [Google Scholar]
- 99.Healthy People 2010. With Understanding and Improving Health and Objectives for Improving Health. 2 vol 2nd ed. Washington, DC: US Dept of Health and Human Services; November 2000 [Google Scholar]
- 100.National Center on Health Statistics Health, United States, 1998–2007 editions. Available at: http://www.cdc.gov/nchs/hus/previous.htm#editions. Accessed July 31, 2009 [PubMed]
- 101.Braveman P. Health disparities and health equity: concepts and measurement. Annu Rev Public Health. 2006;27:167–194 [DOI] [PubMed] [Google Scholar]
- 102.World Health Organization WHO Commission on Macroeconomics & Health, 2001. Available at: http://www.who.int/macrohealth. Accessed April 15, 2009