Abstract
Aims
The aims were to estimate the prevalence of mental distress in different socio-demographic groups; and to analyze use of health care services among persons reporting mental distress.
Methods
Face-to-face interviews with the Self-Reporting Questionnaires (SRQ-20) were conducted in a sample of 3,425 persons aged 18–60 years. A two-stage probability sampling design was applied to select study subjects. Persons with more than six positive responses to the SRQ-20 were identified as having mental distress. Prevalence was estimated for different socio-demographic groups, and odds ratios of having mental distress were obtained by multiple logistic regression analyses.
Main findings
The prevalence of mental distress was 5.4% (6.8% in women and 3.9% in men). Illiteracy and unstable employment status were significantly associated with mental distress among men. Nearly half of those with mental distress had no treatment. Among those who took some health care measures, use of private health services was the most common, followed by self-treatment. Only 5% of those with mental distress sought health care at facilities where mental health care services were available.
Conclusions
Although there was a low prevalence of mental distress, the low use of mental health services indicated that there was a treatment gap in mental health care. Since many people used private services, intervention programs should include private providers to strengthen their capacity to provide mental health care for the community.
Keywords: mental distress, mental disorders, health care, health services, treatment gap
The burden of mental health problems is increasing globally. According to the World Health Organization (WHO), mental health problems amount to nearly one-third of disability in the world (1, 2). The lifetime prevalence of mental or behavioral disorders in both developed and developing countries has been estimated as 25% (3–5). According to a WHO survey in 14 countries during the period 2001–2003, the prevalence of mental disorders was lowest in Nigeria (4.7%) and highest in USA (26.4%), while the prevalence of mental disorders in other countries varied between 9.1 and 16.9% (6).
Besides mental disorders, as defined according to diagnostic criteria, the wider concept of ‘mental distress’ comprises mental disorders as well as other mental problems that may not fall into standard diagnostic criteria. The term ‘mental distress’ has been used in several studies where it has not been possible to perform examinations to obtain a specific diagnosis of mental disorder (7–11). When it comes to needs for care and interventions in the community, occurrence of mental distress is a valid indicator of burden of mental health problems in the population. Mental distress is known to be associated with socioeconomic status. Although the association between mental distress and low socioeconomic status has not been replicated in all settings, several studies have found that poorer, less educated, and unemployed people are be at higher risk of mental distress (1, 9, 12–14). It has also been shown that mentally ill people in lower socioeconomic groups have less access to mental health care services than those in higher socioeconomic groups (1, 11, 15–17). According to an international interview survey by the WHO, 36–50% of persons with serious mental disorders in developed countries did not receive any treatment in the 12 months prior to interview, and the corresponding figure in developing countries was 76–85% (6). In order to meet an increasing burden of mental distress in developing countries, treatment and welfare systems have to develop and adapt to meet the needs of patients and the community.
Vietnam is now in a process of vigorous economic growth with major changes in social life, traditions, health policies, and use of health care services (18, 19). Increasing levels of mental health problems are reported in the media and in public debate, although there is little data at the community level addressing this. Most studies have focused on one specific disorder (e.g. schizophrenia and depression) and the study areas have been limited to one commune and thus had small sample sizes.
Nevertheless, the system of health care delivery is not suited to meet even modest levels of mental health problems. In Vietnam, health care services are available at the community level, and since 2004 community-based mental health care has been launched in 67% of communes nationwide. However, community mental health care is limited to case-management of schizophrenia and epilepsy (20). The health system has not been organized to detect, register, and care for other types of mental illness in the community. Thus, monitoring and follow up of mental health problems in the community is important, to assess needs for intervention and health services.
The aims of the study were to (1) estimate the prevalence of mental distress in different socioeconomic groups; (2) analyze the association between mental distress and socioeconomic status; and (3) find out the use of health care services among those reporting mental distress.
Methods
Setting
The study was conducted in Bavi, a rural district in the North of Vietnam. The district covers a land area of 410 km2, which includes highland, lowland, and mountainous areas. The population is about 240,000. Two thirds of the residents are farmers, the remaining one third are government staff, workers, small traders, etc. The main economic activities of this district are farming, forestry, and breeding. During the last few years, there has been a tendency for people to go to the city or other provinces to work as temporary workers during the slack period after harvest time. The illiteracy rate of people over 15 years is around 0.5% (0.4% among men and 0.6% among women). The major ethnic group is Kinh, which is the biggest group in Vietnam. The average household size is about five persons and there are often three generations living together in a household. The health care system in this district has been organized according to the general pattern in rural Vietnam. The public health care services consist of a district hospital with 150 inpatient beds, three polyclinics, and 32 communal health centres (CHCs). District hospital and polyclinics are mainly responsible for curative care, while CHCs are responsible for primary health care that includes essential curative care and preventive care. Apart from a drug outlet that is available in each CHC, there are few private pharmacies located in this district. There are 145 private providers; most of them are assistant doctors, traditional healers, and nurses. Services they provide mainly are selling essential medicine, treating common diseases, such as angina, mild pneumonia cases, diarrhea, etc.
Study population
This study is part of a longitudinal demographic and epidemiological surveillance system that aims to provide basic health and health care data for epidemiological and health system research and serves as a background and sampling frame for specific studies. A more detailed description of this surveillance system can be found elsewhere (21, 22). We calculated a sample size to detect a level of 10% of the population 18–60 years old having mental distress, with a precision of ±5%, 95% confidence interval (CI) and a design effect equal to 2. The sample size was also calculated to make stratified analyses by socioeconomic subgroups possible.
Multi-stage cluster sampling design was applied. Each village formed a sampling unit. In the first stage, 69 original clusters were stratified according to geographical region, 31 clusters (14 from highland, nine from lowland, and eight from mountainous areas) were then randomly selected according to the population size in each region. In the second stage, in each selected cluster, we randomly selected 115 persons 18–60 years old from the identity number list of the population. However, some clusters in the mountainous area had less than 115 persons in study range ages, and 17 persons were absent during the data collection period. The sample finally comprised 3,425 persons. Socio-demographic characteristics of the study population are shown in Table 1
Table 1.
Socioeconomic characteristics of male and female study subjects
| Men (n=1,705) | Women(n=1,720) | |||
|---|---|---|---|---|
| Variables | N | (%) | N | (%) |
| Age | ||||
| 18–24 | 346 | 20.3 | 365 | 21.2 |
| 25–34 | 420 | 24.6 | 395 | 23.0 |
| 35–44 | 290 | 17.0 | 296 | 17.2 |
| 45–60 | 649 | 38.1 | 664 | 38.6 |
| Marital status | ||||
| Married | 1,308 | 76.1 | 1,247 | 72.5 |
| Previously married | 31 | 1.8 | 171 | 9.9 |
| Never married | 366 | 21.5 | 302 | 17.6 |
| Education | ||||
| Illiterate | 13 | 0.8 | 23 | 1.3 |
| Up to secondary school | 1,222 | 71.6 | 1,200 | 69.8 |
| From high school | 470 | 27.6 | 497 | 28.9 |
| Occupation | ||||
| Farmer | 998 | 58.5 | 1,045 | 60.8 |
| Government staff, student | 236 | 13.9 | 196 | 11.4 |
| Other | 471 | 27.6 | 479 | 27.9 |
| Economic status | ||||
| Poor | 217 | 12.7 | 219 | 12.7 |
| Average | 1,087 | 63.8 | 1,108 | 64.4 |
| Upper average | 401 | 23.5 | 393 | 22.9 |
| Employment status | ||||
| None | 841 | 49.3 | 1,408 | 81.9 |
| 1–3 months | 127 | 7.5 | 42 | 2.4 |
| 4–6 months | 193 | 11.3 | 44 | 2.6 |
| 7–12 months | 544 | 31.9 | 266 | 13.1 |
| Household size | ||||
| 1–2 | 57 | 3.3 | 68 | 3.9 |
| 3–5 | 936 | 54.9 | 954 | 55.5 |
| 6–9 | 663 | 38.9 | 650 | 37.8 |
| ≥10 | 49 | 2.9 | 48 | 2.8 |
| Location | ||||
| Highland | 788 | 46.2 | 800 | 46.5 |
| Mountain | 391 | 22.9 | 418 | 24.3 |
| Riverside | 526 | 30.9 | 502 | 29.2 |
Data collection
The data collection was carried out during two months from April to June, 2004.
To identify persons with mental distress, interviews were performed using the Vietnamese version of the Self-Reporting Questionnaire-20 (SRQ-20). Although another study on mental distress among female care givers in Vietnam had used the Vietnamese SRQ-20 at the cut-off level 7/8 (23), in our study we used the cut-off level 6/7 since the Vietnamese SRQ-20 has been adapted, validated and found to be acceptable to detect mental disorders in this area at this cut-off level (24). In this study, those who answered ‘yes’ to more than six questions of SRQ-20 were defined as having mental distress. The SRQ-20 was developed by WHO and is often used to detect mental disorders in primary health care or in community settings (25). Each time a person reported a symptom according to SRQ-20, he or she was asked if any type of health care service had been used and, if so, what type. Five types of health services were given as alternatives; communal health stations, private health care providers, traditional healers, district hospital/polyclinics, and provincial/central hospitals.
The household economic classification was provided by the local authority according to the guidelines from government and the District Peoples' Committee, which is mainly based on rice production and qualitative assessment. This classification included five categories: very poor, poor, average, upper-average, and rich. However, due to few observations in these subgroups, we regrouped ‘poor’ and ‘very poor’ into one group, as well as ‘rich’ and ‘upper-average’ to what we called the ‘upper-average’ group. Finally, three economic groups were poor, average, and upper-average.
Employment status
We divided study subjects into four groups based on the number of months people worked and got income from during the 12 months prior to the interview. Most of those who were classified in the group ‘none’ are farmers.
The interviewers and supervisors of the surveillance system carried out the data collection. They were permanent staff the of the surveillance site, having five years experience in doing household interviews and well connected with the community. The selected sample for this study included working areas of 25 interviewers and six field supervisors, and each interviewer conducted interviews in one or two clusters and each field supervisor, on average, supervised four interviewers.
Some background information, such as age, education level, household economic status, and ethnicity were taken from the database of the surveillance system, that contained updated information on all individuals and households in the community.
The Ethical and Scientific Committee at Hanoi Medical University and the Ethical Committee of Gothenburg University approved the study. We got permission from the local authority for the demographic surveillance system and also for this specific study. The selected subjects were informed about this study and consented to participate.
Data analysis
The data analysis was performed with STATA version 8.0 for Windows. Prevalences of mental distress across socioeconomic groups were calculated separately for men and women. The distribution of SRQ-20 scores among men and women, as well as the prevalence of each specific symptom were also estimated. Logistic regression was applied to obtain multivariate odds ratios (OR) and 95% CIs for the associations between mental distress and socio-demographic factors. In these models we adjusted for age, marital status, education, occupation, economic status, employment status, location, number of household members, ethnicity, and religion. Those having mental distress OR were adjusted for clustering and stratified sampling. The proportion of persons having been in contact with health services among those with mental distress was calculated. Use of each type of health service was classified as ‘yes’ or ‘no.’ ‘Yes’ meant that the person had made at least one visit to a health service. We compared proportions of using each type of health care services between men and women who reported mental distress using a z-test.
Results
Prevalence of mental distress
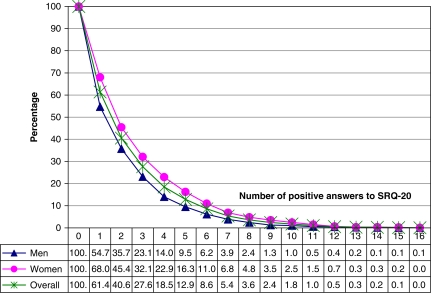
At the cut-off point of 6/7, we identified 184 cases of mental distress, yielding a prevalence of 5.4% for the total sample. The prevalences of mental distress were 6.8% in women and 3.9% in men. If lower cut-off points were used, the prevalence of mental distress would increase by 1.5 times at each lower threshold score (Fig. 1).
Fig. 1.
Distribution of men and women at different cut-off scores of SRQ-20.
Table 2 shows the occurrence of specific SRQ-20 symptoms among men and women. Women had significantly higher prevalence than men of several symptoms, such as headache, poor appetite, sleeping badly, easily frightened, having trouble thinking, feeling unhappy, crying more than usual, having thought of ending life, feeling tired all the time, being easily tired, etc. The most prevalent symptoms reported by men and women were headache (27.7 and 49.8%); sleeping badly (17.2 and 20.9%); feeling nervous/tense/worried (17.7 and 17%); feeling tired all the time (10.3 and 18.3%). The most uncommon symptoms in men were ‘crying more than usual’ (0.4%), ‘having thought of ending life’ (0.8%), while the less common symptoms in women were ‘difficult to make decision’ and ‘daily work suffering’ (2.3%).
Table 2.
Distribution of positive answers on each of SRQ-20 items
| Men (n=1,705) | Women (n=1,720) | ||||
|---|---|---|---|---|---|
| Questions | N | (%) | N | (%) | P-value (z) |
| Often headache | 472 | 27.7 | 857 | 49.8 | <0.000 (−1.3) |
| Poor appetite | 165 | 9.7 | 199 | 11.6 | 0.035 (−1.8) |
| Sleeping badly | 294 | 17.2 | 359 | 20.9 | 0.003 (−2.8) |
| Easily frightened | 34 | 2.0 | 107 | 6.2 | <0.001 (−6.2) |
| Hands shaking | 72 | 4.2 | 78 | 4.5 | 0.33 (−0.4) |
| Feeling nervous, tense, worried | 289 | 17.7 | 293 | 17.0 | 0.71 (0.5) |
| Poor digestion | 146 | 8.6 | 133 | 7.7 | 0.83 (0.9) |
| Having trouble thinking clearly | 121 | 7.1 | 189 | 11.0 | <0.0001 (−3.9) |
| Feeling unhappy | 64 | 3.8 | 152 | 8.8 | <0.0001 (−6.0) |
| Crying more than usual | 6 | 0.4 | 50 | 2.9 | <0.001 (−5.7) |
| Daily activities hardly found enjoyable | 84 | 4.9 | 104 | 6.1 | 0.06 (−1.54) |
| Difficult making decision | 39 | 2.3 | 39 | 2.3 | 0.5 (0) |
| Daily work suffering | 48 | 2.8 | 39 | 2.3 | 0.8 (0.9) |
| Unable to play a useful part | 77 | 4.5 | 75 | 4.4 | 0.6 (0.1) |
| Lost interest in things | 39 | 2.3 | 71 | 4.1 | 0.0014 (−2.9) |
| Feeling worthless | 33 | 1.9 | 53 | 3.1 | 0.012 (−2.2) |
| Having though of ending life | 14 | 0.8 | 57 | 3.3 | <0.001 (−5.15) |
| Feeling tired all the time | 209 | 12.3 | 377 | 21.9 | <0.001 (−7.5) |
| Uncomfortable feeling in stomach | 230 | 13.5 | 177 | 10.3 | 0.99 (2.9) |
| Being easily tired | 175 | 10.3 | 314 | 18.3 | <0.0001 (−6.7) |
Table 3 shows the prevalence and an adjusted OR of mental distress in different socio-demographic groups. In the logistic regression model for the total sample, women reported significantly more mental distress than men did (OR = 1.7; CI: 1.2–2.2). The prevalence increased by age in both men and women. However, mental distress was significantly associated with age only among women. Among men, the level of mental distress was particularly high among those who were previously married, illiterate, had unstable employment, and persons living in the highlands. Illiterate men were eight times more likely to suffer from mental distress compared to men who had high school or higher education (OR = 8.0; CI: 1.3–56.7). Men who were employed 1–3 months had highest risk of mental distress compared to men in other groups.
Table 3.
Prevalence and adjusted odds ratios (OR) of mental distress in different socioeconomic groups of men and women
| Men | Women | Both | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Variables | (%) | OR | CI | (%) | OR | CI | (%) | OR | CI |
| Sex | |||||||||
| Male | NA | NA | 3.9 | Ref | |||||
| Female | NA | NA | 6.9 | 17. | 1.3–2.2 | ||||
| Age | |||||||||
| 18–24 | 0.6 | Ref | 1.9 | Ref | 1.1 | Ref | |||
| 25–34 | 1.9 | Ref | 0.4–5.6 | 4.8 | 3.5 | 1.1–10 | 3.3 | 2.8 | 1–7.8 |
| 35–44 | 5.2 | 2.9 | 0.7–11.8 | 6.1 | 4.5 | 1.7–12 | 5.6 | 4.4 | 1.6–12.3 |
| 45–60 | 6.3 | 4.7 | 1.4–15.9 | 11 | 7.6 | 2.9–19.5 | 8.8 | 7.4 | 3–18.2 |
| Marital status | |||||||||
| Never married | 0.3 | Ref | 3.3 | Ref | 1.7 | Ref | |||
| Previously marrieda | 12.9 | 24.1 | 4.4–131 | 15 | 1.5 | 0.6–3.8 | 14.4 | 2.4 | 1–5.9 |
| Married | 4.7 | 6.2 | 2.5–14.8 | 6.7 | 0.8 | 0.3–2.2 | 5.6 | 1.2 | 0.5–3.1 |
| Education | |||||||||
| From high school | 2.8 | Ref | 6.2 | Ref | 4.6 | Ref | |||
| To secondary school | 4.2 | 1.3 | 0.7–2.3 | 7.2 | 1.2 | 0.8–1.9 | 5.7 | 1.3 | 0.8–1.9 |
| Illiterate | 15.4 | 8.4 | 1.3–57 | 4.4 | 0.7 | 0.1–6.3 | 8.3 | 2.0 | 0.5–8.3 |
| Occupation | |||||||||
| Farmer | 4 | Ref | 7.7 | Ref | 5.7 | Ref | |||
| Government staff, student | 2.5 | 0.7 | 0.3–1.6 | 5.1 | 0.6 | 0.3–1.2 | 3.7 | 0.7 | 0.4–1.1 |
| Other | 4.3 | 1.1 | 0.6–1.9 | 5.8 | 0.7 | 0.4–1.1 | 5.1 | 0.8 | 0.5–1.2 |
| Economic status | |||||||||
| Upper average | 3.2 | Ref | 9.4 | Ref | 6.3 | Ref | |||
| Average | 4.3 | 1.3 | 0.7–2.2 | 5.3 | 0.5 | 0.3–1.2 | 3.7 | 0.7 | 0.5–1.1 |
| Poor | 2.8 | 0.9 | 0.3–2.6 | 10 | 0.9 | 0.5–1.8 | 6.4 | 0.9 | 0.5–1.6 |
| Employment statues | |||||||||
| 7–12 months | 1.7 | Ref | 7.5 | Ref | 3.4 | Ref | |||
| 4–6 months | 4.7 | 3.4 | 1.2–10 | 4.6 | 0.9 | 0.2–5.1 | 4.6 | 2.1 | 1–4.3 |
| 1–3 months | 9.5 | 7.1 | 2.5–19.7 | 7.1 | 1.2 | 0.3–6.8 | 8.9 | 3.5 | 1.5–8.3 |
| None | 4.3 | 2.7 | 1.1–6.9 | 6.8 | 1.1 | 0.6–2.2 | 5.9 | 1.7 | 1–2.8 |
| Location | |||||||||
| Highland | 4.8 | Ref | 8.6 | Ref | 6.7 | ||||
| Mountain | 2.3 | 0.4 | 0.2–0.9 | 3.8 | 0.4 | 0.2–0.7 | 3.1 | 0.4 | 0.1–1.1 |
| Riverside | 3.6 | 0.6 | 0.4–1.2 | 6.6 | 0.8 | 0.5–1.9 | 5.1 | 0.8 | 0.4–1.6 |
aPreviously married including separated, widowed, and divorced people.
Notes: Ref, reference group. The model for men: Pseudo R2 =0.13 (χ2=71.1, p<0.00001). Goodness-of-fit-test: p =0.7; Pearson χ2 =838.8. The model for women: Pseudo R2 =0.08 (χ2 =69.5, p<0.0001). Goodness-of-fit-test: p =0.4; Pearson χ2 =770.4.
In women, there was also a higher level of mental distress among those who were previously married, and those living in highlands. However, in the logistic regression only older age and living in highlands were significantly associated with high prevalence of mental distress. Regarding economic status, the odds of mental distress was significantly lower in ‘average’ group than in ‘upper-average’ group, while no significant difference between the ‘upper-average’ and the ‘poor’ groups was observed.
Use of health services among people with mental distress
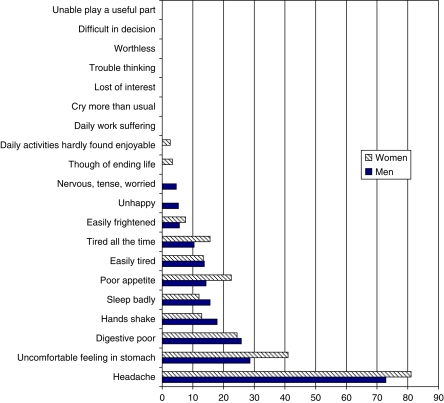
Fig. 2 presents the use of health services among those reporting mental distress. The proportion of persons visiting health services was calculated for each symptom. People with mental distress sought health care more often because of ‘somatic’ symptoms rather than ‘emotional and feeling’ symptoms. The proportion of persons who had used health services was highest among those who had headache (73 and 81%), uncomfortable feeling in the stomach (29 and 41%), poor digestion (25.8 and 24.4%), or hands shake (17.9 and 12.95%). Women tended to seek health care more frequently than men did, regardless of symptoms.
Fig. 2.
Percentage of men and women who reported having been in contact with health services among those with mental distress. Distrubtion by SRQ-20 items reported.
Table 4 shows the pattern of use of health services for men and women with mental distress. Women tended to use health services more than men did, although the difference was not statistically significant (61.7% vs. 51.5%). Among those who used health care services, the most common type of service used was private health care providers (35.6 and 42.4%). Very few people (5%) sought health care at district hospital and at provincial/central hospitals. The pattern of use of health services did not vary by socio-demographic groups. Women used significantly more CHC and provincial/national hospitals than did men.
Table 4.
Pattern of use of health services among men and women who reported mental distress
| Men (N=66) | Women (N=118) | Both (N=184) | ||||
|---|---|---|---|---|---|---|
| N | (%) | N | (%) | (%) | P* | |
| Self-treatment | 17 | 25.8 | 29 | 24.7 | 25.0 | 0.43 |
| Any source of health care services | 34 | 51.5 | 73 | 61.7 | 58.2 | 0.08 |
| Traditional healers | 4 | 6.1 | 11 | 9.3 | 8.2 | 0.22 |
| Community health station | 5 | 7.6 | 23 | 19.5 | 15.2 | 0.02 |
| Private health providers | 28 | 42.4 | 42 | 35.6 | 38.0 | 0.82 |
| District hospital | 3 | 4.6 | 1 | 0.9 | 2.2 | 0.94 |
| Provincial hospital/national hospital | 0 | 0 | 5 | 4.2 | 2.7 | 0.04 |
*P-value for the comparison of proportions of using each type of health care services between two sexes, use z-test.
Discussion
Prevalence of mental distress
The prevalence of mental distress found in this study seems low, since it has been reported that the median prevalence rate of mental distress in developing countries varies from 20 to 30% (14). A possible underreporting must be considered, but the instrument has been validated and the sensitivity was found to be 85%. This sensitivity does indicate a certain underreporting, but even taking this into account, the ‘true rate’ of mental distress would still be less than 10%. Our results are consistent with findings of 4–9% prevalence of depression in Hanoi and some other provinces of Vietnam (26, 27). Studies among Vietnamese refugees in the Western countries and Australia also found prevalence rates of mental distress around 5–7% (28, 29). Another study using SRQ at the cut-off of 7/8 among 400 female care givers of children under one-year old in a province in North Vietnam found a higher prevalence of mental distress of 20% (23). The two Vietnamese versions of SRQ used in the two studies are almost the same. The difference might be explained by the fact that mental distress is more prevalent among women taking care of children under one-year old or that the two studies were conducted in different settings. However, cross-cultural differences in rates of mental disorders are complex and is an important area for further comparative research.
In this population, somatic symptoms were more prevalent than ‘emotional’ symptoms. Several studies have found that somatic symptoms are the most common clinical expression of psychological distress (8, 30, 31). In our setting, the higher prevalence of somatic symptoms could probably be related to the prevailing cultural notion that a person was considered ill only when he or she had some physical ailment and it is easier for him or her to remember an abnormal event. In addition, a person with mental distress might dislike to report psychiatric symptoms because mental illness is stigmatized in the Vietnamese culture as in many other countries. Instead, somatic symptoms may be used to express psychological symptoms.
Like in many previous studies from different parts of the world, we found a higher rate of mental distress among women (7, 11, 12, 14, 32, 33). We found that the prevalence of mental distress increased significantly with increasing age in women (7, 9). Some previous studies have not found significant differences between age groups (11, 34). Some studies even reported less mental distress in the elderly (32, 33). Different classifications of age groups and different inclusion criteria to the studies might explain this discrepancy. Furthermore, mental distress is a general term comprising several specific conditions of mental health problems, while the distribution of each condition by age may not be identical.
An association between mental distress and socio-demographic factors was only found among men. In previous studies, these associations have been found also among women (7, 9–12, 14, 33–36). In our study, the employment status of men was much better than that of women, but the economic status distributions of both sexes were quite identical. The lower employment status and the higher prevalence of mental distress among women may lead to a hypothesis that employment status was a predictor of mental distress in women. However, in the logistic regression the association was not statistically significant. One reason may be that in rural Vietnam a woman seems to have less social pressures than a man if she is unemployed or illiterate, since household finance is often considered as men's responsibility. In addition, unemployment and illiteracy is more likely to threaten a man's self confidence than a woman's. It should be noted that few observations in some subgroups, such as men in the ‘previously married’ group and men and women in the ‘illiterate’ group, give a low power to detect differences.
In contrast to several other studies, poor household finance was not significantly associated with mental distress in our study. One may argue that our classification of household finance is not sensitive enough. Khe et al. have shown, however, that other economic classification systems (based on income quintiles; wealth index based on assets; housing conditions; and household expenditures) were not better in assessing household economic status in this setting (36). On the one hand, it is possible that the economic gap between groups in this setting is not large enough to show the disparity in mental distress between economic groups. On the other hand, it might be true that low economic status is not a predictor of metal distress. For example, a study from Bangladesh found that mental illness was more common among persons from higher socioeconomic class (31). Also, a WHO survey found that countries with higher international socioeconomic standing, such as the USA, have the highest prevalence of mental disorders (6).
Use of health services among people with mental distress
We found that a large proportion of people with mental distress used private services, while few of them used CHCs and hospitals. This finding is consistent with previous studies on the use of health services among those who reported the presence of illness. In those studies, the main interest was about physical illnesses (22, 37, 38). The similarity in the pattern of use of health services between our study and the previous studies is understandable since persons with mental distress in our study sought health care because of the occurrence of ‘somatic’ symptoms rather than the occurrence of ‘emotional’ symptoms.
The extensive use of private health care facilities among persons with mental distress in this setting points at the need of taking the private sector into account when planning mental health services. Remarkably, only 5% of persons with mental distress sought health care at hospitals where mental health care is available. Although having mental distress does not necessarily express the need of specialized mental health care, this finding indicates a high possibility that a person with a mental disorder does not get appropriate care. Several studies across countries have pointed out the gap between the need for mental health care and the actual use of mental health care services (6, 39, 40). For instance, a study in California found that only 58% of women who reported mental health problems sought mental health services, and that 88% of these actually had used mental health services (17). A study in the USA reported that people with frequent mental disorders were 30% more likely to be without health care coverage (33).
Jorm discussed public knowledge and beliefs and meant that ‘mental health literacy’ is important since the recognition of mental disorders can influence to mental health care seeking (41). Furthermore, the stigmatization of people with mental illness may reduce the propensity to health care (42, 43). In our setting, there is also a possibility that people either did not recognize their problem as a mental health problem or did not know that they could be assessed and cared for if they sought help at mental health care services. Finally, there are some issues related to the current health system in this setting that limit the use of mental health care services among people with mental illness, such as the lack of a community-based mental health care in each commune, the inadequate capacity of private providers and staff at communal health stations regarding diagnosis and treatment of mental illness.
Limitations
Since this was a cross sectional study, we were unable to draw conclusions about the causal directions regarding socio-demographic factors and mental distress. Furthermore, using interviews with SRQ-20 and without applying further diagnostic instrument or psychiatric examination, we could not make diagnoses of specific mental disorders. However, SRQ-20 has been widely used in primary care and community settings (25) and has been validated in our setting (24). We did not study the public's knowledge of mental health and its association to the accessibility to mental health care of people with mental distress, but further studies should explore these to provide good evidence for the introduction of appropriate intervention programs.
Conclusion
Although we found a low prevalence of mental distress, the low use of mental health services among those who reported symptoms indicates a need to make mental health care services more accessible at community level. Also, the awareness in the community about mental health problems should be increased. Private providers should be included in intervention programs to strengthen capacity to provide primary mental health care at community level.
Conflict of interest and funding
The authors have not received any funding or benefits from industry to conduct this study.
References
- 1.WHO. Geneva: World Health Organisation; 2001. The World Health Report 2001 – Mental Health: New Understanding, New Hope. [Google Scholar]
- 2.WHO. Geneva: World Health Organization; 2002. The World Health Report 2002: reducing risks, promoting healthy life; pp. 3–6. [DOI] [PubMed] [Google Scholar]
- 3.Almeida-Filho N, Mari Jde J, Coutinho E, Franca JF, Fernandes J, Andreoli SB, et al. Brazilian multicentric study of psychiatric morbidity. Methodological features and prevalence estimates. Br J Psychiatry. 1997;171:524–9. doi: 10.1192/bjp.171.6.524. [DOI] [PubMed] [Google Scholar]
- 4.Regier DA, Boyd JH, Burke JD, Jr., Rae DS, Myers JK, Kramer M, et al. One-month prevalence of mental disorders in the United States. Based on five epidemiologic catchment area sites. Arch Gen Psychiatry. 1988;45:977–86. doi: 10.1001/archpsyc.1988.01800350011002. [DOI] [PubMed] [Google Scholar]
- 5.Wells JE, Bushnell JA, Hornblow AR, Joyce PR, Oakley- Browne MA. Christchurch psychiatric epidemiology study, part I: methodology and lifetime prevalence for specific psychiatric disorders. Aust NZ J Psychiatry. 1989;23:315–26. doi: 10.3109/00048678909068289. [DOI] [PubMed] [Google Scholar]
- 6.Demyttenaere K, Bruffaerts R, Posada-Villa J, Gasquet I, Kovess V, Lepine JP, et al. Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization World Mental Health Surveys. JAMA. 2004;291:2581–90. doi: 10.1001/jama.291.21.2581. [DOI] [PubMed] [Google Scholar]
- 7.Alem A, Kebede D, Woldesemiat G, Jacobsson L, Kullgren G. The prevalence and socio-demographic correlates of mental distress in Butajira, Ethiopia. Acta Psychiat Scand Suppl. 1999;397:48–55. doi: 10.1111/j.1600-0447.1999.tb10694.x. [DOI] [PubMed] [Google Scholar]
- 8.De Waal MW, Arnold IA, Spinhoven P, Eekhof JA, van Hemert AM. The reporting of specific physical symptoms for mental distress in general practice. J Psychosom Res. 2005;59:89–95. doi: 10.1016/j.jpsychores.2005.02.011. [DOI] [PubMed] [Google Scholar]
- 9.Kebede D, Alem A, Rashid E. The prevalence and sociodemographic correlates of mental distress in Addis Ababa, Ethiopia. Acta Psychiatr Scand Suppl. 1999;397:5–10. doi: 10.1111/j.1600-0447.1999.tb10687.x. [DOI] [PubMed] [Google Scholar]
- 10.Husain N, Creed F, Tomenson B. Depression and social stress in Pakistan. Psychol Med. 2000;30:395–402. doi: 10.1017/s0033291700001707. [DOI] [PubMed] [Google Scholar]
- 11.Rohrer JE, Borders TF, Blanton J. Rural residence is not a risk factor for frequent mental distress: a behavioral risk factor surveillance survey. BMC Public Health. 2005;5:46. doi: 10.1186/471-2458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Women Watch. Women and mental health [database on the Internet] Women Watch. 2006. Available from: http://www.un.org/womenwatch/daw/csw/mental.htm [cited 1 March 2006]
- 13.Brown DW, Balluz LS, Ford ES, Giles WH, Strine TW, Moriarty DG, et al. Associations between short- and longterm unemployment and frequent mental distress among a national sample of men and women. J Occup Environ Med. 2003;45:1159–66. doi: 10.1097/01.jom.0000094994.09655.0f. [DOI] [PubMed] [Google Scholar]
- 14.Patel V, Kleinman A. Poverty and common mental disorders in developing countries. Bull World Health Organ. 2003;81:609–15. [PMC free article] [PubMed] [Google Scholar]
- 15.Borowsky SJ, Rubenstein LV, Meredith LS, Camp P, Jackson-Triche M, Wells KB. Who is at risk of nondetection of mental health problems in primary care? J Gen Intern Med. 2000;15:381–8. doi: 10.1046/j.1525-1497.2000.12088.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Saldivia S, Vicente B, Kohn R, Rioseco P, Torres S. Use of mental health services in Chile. Psychiatr Serv. 2004;55:71–6. doi: 10.1176/appi.ps.55.1.71. [DOI] [PubMed] [Google Scholar]
- 17.Kimerling R, Baumrind N. Access to specialty mental health services among women in California. Psychiatr Serv. 2005;56:729–34. doi: 10.1176/appi.ps.56.6.729. [DOI] [PubMed] [Google Scholar]
- 18.Khe ND, Toan NV, Xuan LT, Eriksson B, Hojer B, Diwan VK. Primary health concept revisited: where do people seek health care in a rural area of Vietnam? Health Policy. 2002;61:95–109. doi: 10.1016/s0168-8510(01)00198-1. [DOI] [PubMed] [Google Scholar]
- 19.World Bank. Hanoi: World Bank; 2001. Vietnam – growing healthy – a review of Viet Nam's health sector. (Report No.: 22210) [Google Scholar]
- 20.Nghi TV. National Workshop on Mental Health Care and Suicide Prevention (In Vietnamese) Hue: Ministry of Health of Vietnam; 2004. Developing mental health care strategies in Vietnam. [Google Scholar]
- 21.Chuc NT, Diwan V. FilaBavi, a demographic surveillance site, an epidemiological field laboratory in Vietnam. Scand J Public Health Suppl. 2003;62:3–7. doi: 10.1080/14034950310015031. [DOI] [PubMed] [Google Scholar]
- 22.Giang KB, Allebeck P. Self-reported illness and use of health services in a rural district of Vietnam: findings from an epidemiological field laboratory. Scand J Public Health Suppl. 2003;62:52–8. doi: 10.1080/14034950310015112. [DOI] [PubMed] [Google Scholar]
- 23.Lives Y. Young lives preliminary country report: Vietnam. Hanoi: Young Lives; 2003. pp. 25–26. [Google Scholar]
- 24.Giang KB, Allebeck P, Kullgren G, Tuan NV. The Vietnamese version of the Self Reporting Questionnaire 20 (SRQ-20) in detecting mental disorders in rural Vietnam: a validation study. Int J Soc Psychiat. 2006;52:175–84. doi: 10.1177/0020764006061251. [DOI] [PubMed] [Google Scholar]
- 25.WHO. A user's guide to the Self Reporting Questionnaire (SRQ) Geneva, Switzerland: World Health Organisation; 1994. [Google Scholar]
- 26.Nghi TV, Siem NV, Thiem NV, Buoi LT, editors. A clinical epidemiological study on depression in some communities. National conference: taking care of psychiatric patients and suicide prevention. Hue, Vietnam: Hanoi Medical University; 2004. Apr, pp. 1–5. [Google Scholar]
- 27.Binh TH, editor. Study on depression in a commune in Hanoi (in Vietnamese). National conference: taking care of psychiatric patient and suicide prevention. Hue: Hanoi Medical University and World Health Organisation; 2004. Apr, pp. 30–37. [Google Scholar]
- 28.Buchwald D, Manson S, Brennenman D, Dinges N, Keane E, Beals J. Screening for depression among newly arrived Vietnamese refugees in primary care settings. West J Med. 1995;163:341–5. [PMC free article] [PubMed] [Google Scholar]
- 29.Zachary S, Derrick S, Tuong P, Bauman A. Long-term effect of psychological trauma on the mental health of Vietnamese refugees resettled in Australia: a population-based study. Lancet. 2002;360:1058–61. doi: 10.1016/S0140-6736(02)11142-1. [DOI] [PubMed] [Google Scholar]
- 30.Parker G, Gladstone G, Chee KT. Depression in the planet's largest ethnic group: the Chinese. Am J Psychiat. 2001;158:857–64. doi: 10.1176/appi.ajp.158.6.857. [DOI] [PubMed] [Google Scholar]
- 31.Islam MM, Ali M, Ferroni P, Underwood P, Alam MF. Prevalence of psychiatric disorders in an urban community in Bangladesh. Gen Hosp Psychiat. 2003;25:353–7. doi: 10.1016/s0163-8343(03)00067-7. [DOI] [PubMed] [Google Scholar]
- 32.Chow JC, Jaffee K, Snowden L. Racial/ethnic disparities in the use of mental health services in poverty areas. Am J Public Health. 2003;93:792–7. doi: 10.2105/ajph.93.5.792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Strine TW, Balluz L, Chapman DP, Moriarty DG, Owens M, Mokdad AH. Risk behaviors and healthcare coverage among adults by frequent mental distress status, 2001. Am J Prev Med. 2004;26:213–6. doi: 10.1016/j.amepre.2003.11.002. [DOI] [PubMed] [Google Scholar]
- 34.Araya R, Rojas G, Fritsch R, Acuna J, Lewis G. Common mental disorders in Santiago, Chile: prevalence and sociodemographic correlates. Br J Psychiat. 2001;178:228–33. doi: 10.1192/bjp.178.3.228. [DOI] [PubMed] [Google Scholar]
- 35.Maziak W, Asfar T, Mzayek F, Fouad FM, Kilzieh N. Sociodemographic correlates of psychiatric morbidity among lowincome women in Aleppo, Syria. Soc Sci Med. 2002;54:1419–27. doi: 10.1016/s0277-9536(01)00123-x. [DOI] [PubMed] [Google Scholar]
- 36.Khe ND, Eriksson B, Phuong do N, Hojer B, Diwan VK. Faces of poverty: sensitivity and specificity of economic classifications in rural Vietnam. Scand J Public Health Suppl. 2003;62:70–5. doi: 10.1080/14034950310015149. [DOI] [PubMed] [Google Scholar]
- 37.Dzung TV, Hung VV, Thu NT. Study on provision and use of health care services in 28 rural communes in 2000–2001. Hanoi: Policy Unit, Department of Health Planning and Vietnam–Sweden Cooperation Program; 2002. [Google Scholar]
- 38.Ministry of Health. Office GS . Hanoi: Hanoi Medical Publishing House; 2003. National Health Survey, 2001–02. [Google Scholar]
- 39.Kohn R, Saxena S, Levav I, Saraceno B. The treatment gap in mental health care. Bull World Health Organ. 2004;82:858–66. [PMC free article] [PubMed] [Google Scholar]
- 40.Bijl RV, de Graaf R, Hiripi E, Kessler RC, Kohn R, Offord DR, et al. The prevalence of treated and untreated mental disorders in five countries. Health Aff (Millwood) 2003;22:122–33. doi: 10.1377/hlthaff.22.3.122. [DOI] [PubMed] [Google Scholar]
- 41.Jorm AF. Mental health literacy. Public knowledge and beliefs about mental disorders. Br J Psychiat. 2000;177:396–401. doi: 10.1192/bjp.177.5.396. [DOI] [PubMed] [Google Scholar]
- 42.Raguram R, Weiss MG, Channabasavanna SM, Devins GM. Stigma, depression, and somatization in South India. Am J Psychiat. 1996;153:1043–9. doi: 10.1176/ajp.153.8.1043. [DOI] [PubMed] [Google Scholar]
- 43.Liggins J, Hatcher S. Stigma toward the mentally ill in the general hospital: a qualitative study. Gen Hosp Psychiat. 2005;27:359–64. doi: 10.1016/j.genhosppsych.2005.05.006. [DOI] [PubMed] [Google Scholar]