Abstract
BACKGROUND
Minority women are more likely than white women to choose tubal sterilization as a contraceptive method. Disparities in rates of unintended pregnancy may help explain observed racial/ethnic differences in sterilization, but this association has not been investigated.
OBJECTIVE
To examine the associations among race/ethnicity, unintended pregnancy, and tubal sterilization.
DESIGN AND PARTICIPANTS
Cross-sectional analysis of data from a nationally representative sample of women aged 15–44 years [65.7% white, 14.8% Hispanic, and 13.9% African American (AA)] who participated in the 2002 National Survey of Family Growth.
MAIN MEASURES
Race/ethnicity, history of unintended pregnancy, and tubal sterilization. A logistic regression model was used to estimate the effect of race/ethnicity on unintended pregnancy while adjusting for socio-demographic variables. A series of logistic regression models was then used to examine the role of unintended pregnancy as a confounder for the relationship between race/ethnicity and sterilization.
KEY RESULTS
Overall, 40% of white, 48% of Hispanic, and 59% of AA women reported a history of unintended pregnancy. After adjusting for socio-demographic variables, AA women were more likely (OR: 2.0; 95% CI: 1.6–2.4) and Hispanic women as likely (OR: 1.0; 95% CI: 0.80–1.2) as white women to report unintended pregnancy. Sterilization was reported by 29% of women who had ever had an unintended pregnancy compared to 7% of women who reported never having an unintended pregnancy. In unadjusted analysis, AA and Hispanic women had significantly higher odds of undergoing sterilization (OR: 1.5; 95% CI: 1.3–1.9 and OR: 1.4; 95% CI: 1.2–1.7, respectively). After adjusting for unintended pregnancy, this relationship was attenuated and no longer significant (OR: 1.2; 95% CI: 0.95–1.4 for AA women and OR: 1.3; 95% CI: 1.0–1.6 for Hispanic women).
CONCLUSION
Minority women, who more frequently experience unintended pregnancy, may choose tubal sterilization in response to prior experiences with an unintended pregnancy.
KEY WORDS: unintended pregnancy, minority women, tubal sterilization
INTRODUCTION
Minority women in the United States are far more likely to rely on tubal sterilization as a method of contraception than white women.1–8 The reasons for this observed racial/ethnic difference in sterilization rates, which persists across socio-economic levels, is unclear. Several studies indicate that patient preference, rather than provider or health system factors, play a significant role in sterilization decision making.1,9 To provide high quality, patient-centered care, it is important that we understand what factors shape contraceptive preferences and ensure that these preferences are not based on unequal access to medical information or culturally based health myths.10
In our recent qualitative study exploring reasons for undergoing sterilization among African American (AA) and white women, race-related differences in unintended pregnancy emerged as a possible explanatory factor for why AA women are more likely than white women to prefer and choose tubal sterilization over other contraceptive methods.9 AA women were more likely to report that their decision to get sterilized was influenced by having had one or more unplanned pregnancies.9 Although prior literature has documented racial/ethnic disparities in unintended pregnancy rates,11 the relationship between unintended pregnancy and subsequent tubal sterilization has not been rigorously investigated. To address this knowledge gap, we used the National Survey of Family Growth (NSFG) to investigate the relationships among race/ethnicity, unintended pregnancy, and tubal sterilization.
MATERIALS AND METHODS
Data Source
This study is an analysis of cross-sectional data collected for Cycle 6 (2002) of the NSFG, a publicly available dataset (www.cdc.gov/nchs/nsfg.htm). The NSFG is conducted periodically by the National Center for Health Statistics (NCHS), Centers for Disease Control and Prevention, to provide national estimates of factors affecting pregnancy and birth outcomes including sexual activity, contraceptive use, marital status, infertility, and use of medical services for family planning.
The NSFG uses a stratified, multi-stage sample design to represent women and men aged 15–44 years in the civilian, non-institutionalized household population of the US. A complete description of the sampling methods for Cycle 6 of the NSFG is discussed elsewhere.12 Briefly, 121 Primary Sampling Units (PSUs) were selected from the 50 states and the District of Columbia. PSUs were located in nearly every state and included all of the largest metropolitan areas in the US. Within each of the PSUs, groups of adjacent blocks were selected at random. Addresses within these blocks were then selected randomly and visited in person. A short “screener” interview was conducted to see if anyone aged 15–44 years lived there. If so, one person was chosen at random for the interview and offered a chance to participate. Interviews were conducted in person by a trained female interviewer in the selected person’s home and were performed between March 2002 and March 2003. The overall response rate was approximately 80%. The 2002 NSFG sample included 12,571 men and women. Women, teenagers 15–19 years of age, and AA and Hispanic persons were oversampled. Because the NSFG selects sub-groups at different rates, sampling weights are applied to respondent data to adjust for different sampling rates, response rates, and coverage rates so that accurate, unbiased national estimates can be made.12 This study was approved by the University of Pittsburgh Institutional Review Board.
Study Population
The 2002 NSFG sample included 7,643 women and 4,928 men. Although the 2002 NSFG data included men, this analysis used only data obtained from women. We excluded women who reported that their race was “other” (n = 385) as this group was too heterogeneous (included Asians, Pacific Islanders, Alaskan natives, and American Indians) to draw meaningful conclusions.
Study Outcome and Independent Variables
This study consisted of two separate analyses to examine: (1) the independent effect of race/ethnicity on unintended pregnancy and (2) the effect of unintended pregnancy on the relationship between race/ethnicity and tubal sterilization. For the first analysis, the primary outcome variable was self-reported history of an unintended pregnancy. Women who had ever been pregnant were asked to characterize each pregnancy as either “unwanted,” occurring at the “right time,” “overdue,” “too soon,” or that they “didn’t care” or “didn’t know.” Consistent with the conventional definition of unintended pregnancy,13 women reporting pregnancies that were either “unwanted” or occurred “too soon” were considered to have a history of unintended pregnancy. Because we were interested in understanding the relationship between unintended pregnancy and subsequent tubal sterilization decisions, we included only pregnancies that occurred prior to tubal sterilization in those women who had the procedure. Participants who had one or more pregnancies were asked to provide the month and year that each pregnancy began, and women who had a sterilization procedure were also asked to provide the month and year of their procedure. Using this retrospective sequence data, we were able to censor pregnancies that occurred after tubal sterilization. The primary predictor variable was self-reported race/ethnicity. We categorized race/ethnicity as non-Hispanic white, Hispanic, and non-Hispanic black. Age, insurance status, education level, income, parity, religion, and marital status were examined as potential confounders.
For the second analysis, the outcome variable was a history of tubal sterilization. Women were considered to have had a tubal sterilization if they answered yes to the question: “Have you ever had both of your tubes tied, cut, or removed? This procedure is often called a tubal ligation or tubal sterilization.” The primary predictor variables were race/ethnicity and history of unintended pregnancy. Age, insurance status, education level, income, parity, religion, and marital status were again examined as potential confounders.
Statistical Analysis
Sociodemographic characteristics of the study sample were compared by race/ethnicity using Rao-Scott chi-square tests for all categorical variables.
To investigate the relationship between race/ethnicity and unintended pregnancy, we first examined bivariate associations between all covariates and history of unintended pregnancy, and calculated unadjusted odds ratios for each pair. A multivariable logistic regression model was then used to determine the adjusted odds ratio of experiencing an unintended pregnancy while controlling for those variables that demonstrated a significant association with the outcome variable (p < 0.10) in bivariate analysis.
To investigate the relationships among race/ethnicity, unintended pregnancy, and tubal sterilization, we first examined bivariate associations between all socio-demographic covariates and tubal sterilization, and calculated unadjusted odds ratios for each pair. To better understand the specific role of unintended pregnancy as a confounder for the association between race/ethnicity and tubal sterilization, we examined the unadjusted odds ratio of undergoing tubal sterilization for each racial/ethnic category (Model 1), the change in the odds ratios after adjusting for unintended pregnancy (Model 2), and the fully adjusted odds ratios controlling for the remaining covariates that demonstrated a significant association with tubal sterilization (p < 0.10) in bivariate analysis (Model 3). We also assessed for an interaction between race/ethnicity and unintended pregnancy.
Because there is some debate over the meaning and measurement of unintended pregnancy,13,14 we conducted sensitivity analyses in which we repeated all of the above analyses using a history of unwanted (rather than unintended) pregnancy.
Analyses were conducted using SAS software, version 9.1, with appropriate adjustment for the NSFG’s complex sample design. As such, all percentages shown have been weighted to reflect national estimates, and ‘design-based’ estimates of sampling errors were calculated to account for the stratified and clustered sampling.
RESULTS
Sample Characteristics
After excluding women of “other” race, the sampling frame consisted of 7,258 women. The socio-demographic characteristics of the study sample are shown in Table 1. Briefly, Hispanic and AA women were less likely to have private insurance, were poorer, had lower educational attainment, and had more children compared to white women.
Table 1.
Socio-Demographic Characteristics of US Women 15–44 Years of Age, 2002 NSFG
| Variable | White (%) (n = 4,139) | Hispanic (%) (n = 1,589) | Black (%) (n = 1,530) |
|---|---|---|---|
| Total populationa | 65.7 | 14.8 | 13.9 |
| Insurance status | |||
| None | 12.2 | 29.9 | 16.4 |
| Private | 76.2 | 43.9 | 55.8 |
| Publicb | 11.6 | 26.2 | 27.8 |
| Age | |||
| 15–19 | 15.5 | 16.7 | 17.5 |
| 20–29 | 29.2 | 36.1 | 32.1 |
| 30–44 | 55.4 | 47.2 | 50.4 |
| Income | |||
| <100% of poverty levelc | 12.7 | 36.6 | 30.1 |
| 100%–299% | 37.4 | 44.1 | 42.0 |
| >300% | 49.9 | 19.3 | 27.9 |
| Education | |||
| <HS diploma | 16.2 | 42.1 | 24.5 |
| HS graduate (diploma or GED) | 27.5 | 28.4 | 32.6 |
| Some college but no degree | 22.4 | 15.3 | 22.5 |
| College degree or higher | 33.9 | 14.2 | 20.5 |
| Parity | |||
| 0 births | 44.2 | 32.4 | 36.8 |
| 1–2 births | 39.4 | 42.3 | 40.4 |
| 3 or more births | 16.5 | 25.4 | 22.9 |
| Marital status | |||
| Married | 50.5 | 45.4 | 25.8 |
| Divorced/widowed/separated | 12.1 | 12.4 | 13.6 |
| Never married | 37.4 | 42.1 | 60.6 |
| Religion | |||
| No religion | 15.7 | 11.1 | 9.6 |
| Catholic | 24.9 | 66.2 | 6.8 |
| Protestant | 53.6 | 21.2 | 79.5 |
| Other religions | 5.8 | 1.5 | 4.1 |
P values for all comparisons (using chi-square tests) were <0.001
HS, high school; GED, general equivalency diploma; NSFG, National Survey of Family Growth
Weighted to reflect the US female household population aged 15–44 years
aRacial/ethnic proportions shown do not add up to 100% because 5.6% of the population is of “other” race
bPublic insurance included Medicaid, Medicare, Medi-Gap, Indian health service, Children’s Health Insurance Program, state-sponsored, or other government program
cPoverty threshold based on 2001 level defined by the US Census Bureau, which takes into account total household income and number (i.e., $18,104 for a family of four)
The Relationship Between Race/Ethnicity and Unintended Pregnancy
Overall, 40% of white women, 48% of Hispanic women, and 59% of AA women reported a history of unintended pregnancy (p < 0.001; Table 2). In unadjusted analysis, Hispanic and AA women were more likely to report an unintended pregnancy compared to white women [odds ratio (OR): 1.4; 95% confidence interval (CI): 1.2–1.6 and OR: 2.2; 95% CI: 1.9–2.6, respectively]. After adjusting for socio-demographic characteristics, AA women remained significantly more likely than white women to have had an unintended pregnancy (OR: 2.0; 95% CI: 1.6 – 2.4; Table 3) while Hispanic women were as likely as white women to report an unintended pregnancy (OR: 1.0; 95% CI: 0.80 – 1.2).
Table 2.
The Unadjusted Relationships Between Socio-Demographic Factors and Unintended Pregnancy and Tubal Sterilization among US Women 15–44 Years of Age, 2002 NSFG
| Variable | Unintended pregnancy | Tubal sterilization | ||
|---|---|---|---|---|
| % with unintended pregnancya | Unadjusted OR (95% CI) | % with tubal sterilizationa | Unadjusted OR (95% CI) | |
| Race/ethnicity | ||||
| White | 39.8 | ref | 15.0 | ref |
| Hispanic | 48.3 | 1.4 (1.2–1.6) | 20.1 | 1.4 (1.2–1.7) |
| Black | 59.1 | 2.2 (1.9–2.6) | 21.3 | 1.5 (1.3–1.9) |
| Insurance status | ||||
| None | 52.6 | 1.8 (1.5–2.1) | 22.1 | 1.7 (1.3–2.1) |
| Private | 38.0 | ref | 14.6 | ref |
| Publicb | 60.9 | 2.5 (2.2–3.0) | 20.5 | 1.5 (1.2–1.9) |
| Age | ||||
| 15–19 | 12.9 | 0.12 (0.096–0.15) | 0.091 | 0.002 (0.000–0.017) |
| 20–29 | 40.8 | 0.56 (0.49–0.64) | 6.3 | 0.17 (0.14–0.22) |
| 30–44 | 55.2 | ref | 27.7 | ref |
| Income | ||||
| <100% of poverty levelc | 51.9 | 1.8 (1.6–2.2) | 22.1 | 2.1 (1.7–2.6) |
| 100%– 299% | 47.6 | 1.5 (1.3–1.8) | 19.2 | 1.8 (1.4–2.2) |
| >300% | 37.0 | ref | 12.0 | ref |
| Education | ||||
| <HS diploma | 38.8 | ref | 17.0 | ref |
| HS graduate (diploma or GED) | 56.2 | 2.0 (1.7–2.4) | 23.2 | 1.5 (1.2–1.9) |
| Some college but no degree | 43.5 | 1.2 (1.0–1.5) | 16.1 | 0.94 (0.72–1.2) |
| College degree or higher | 36.3 | 0.90 (0.76–1.1) | 10.7 | 0.58 (0.45–0.76) |
| Parity | ||||
| 0 births | 13.3 | 0.10 (0.089–0.12) | 1.1 | 0.045 (0.029–0.068) |
| 1–2 births | 59.7 | ref | 19.4 | ref |
| 3 or more births | 77.8 | 2.4(1.9–3.0) | 45.4 | 3.4 (2.8–4.3) |
| Marital status | ||||
| Married | 49.9 | ref | 22.2 | ref |
| Divorced/widowed/separated | 70.9 | 2.4 (2.0–3.0) | 36.6 | 2.0 (1.6–2.5) |
| Never married | 29.4 | 0.42 (0.37–0.48) | 4.8 | 0.18 (0.14–0.22) |
| Religion | ||||
| No religion | 47.5 | 1.1 (0.92–1.3) | 15.0 | 0.73 (0.55–0.96) |
| Catholic | 41.3 | 0.86 (0.73–1.0) | 14.5 | 0.70 (0.57–0.87) |
| Protestant | 45.1 | ref | 19.4 | ref |
| Other religions | 38.3 | 0.76 (0.58–0.99) | 6.0 | 0.27 (0.16–0.45) |
| Prior unintended pregnancy | ||||
| Ever | - | - | 28.8 | 5.2 (4.4–6.3) |
| Never | - | - | 7.3 | ref |
OR, odds ratio; CI, confidence interval; HS, high school; GED, general equivalency diploma; NSFG, National Survey of Family Growth
Weighted to reflect the US female household population aged 15–44 years
aP values for all comparisons (using chi-square tests) were <0.001
bPublic insurance included Medicaid, Medicare, Medi-Gap, Indian health service, Children’s Health Insurance Program, state-sponsored, or other government program
cPoverty threshold based on 2001 level defined by the US Census Bureau, which takes into account total household income and number (i.e., $18,104 for a family of four)
Table 3.
Adjusted Odds of Experiencing an Unintended Pregnancy and of Undergoing Tubal Sterilization among US Women 15–44 Years of Age, 2002 NSFG
| Variables | Unintended pregnancy | Tubal sterilization | ||
|---|---|---|---|---|
| Adjusted OR (95% CI) | Model 1 OR (95% CI) | Model 2 OR (95% CI) | Model 3 OR (95% CI) | |
| Race/ethnicity | ||||
| White | ref | ref | ref | ref |
| Hispanic | 1.0 (0.80–1.2) | 1.4 (1.2–1.7) | 1.3 (1.0–1.6) | 1.2 (0.87–1.6) |
| Black | 2.0 (1.6–2.4) | 1.5 (1.3–1.9) | 1.2 (0.95–1.4) | 1.3 (1.0–1.6) |
| Prior unintended pregnancy | ||||
| Yes | ----- | ----- | 5.1 (4.1–6.2) | 1.8 (1.4–2.3) |
| No | ref | ref | ||
| Insurance status | ||||
| None | 1.4 (1.1–1.7) | ----- | ----- | 1.1 (0.85–1.5) |
| Private | ref | ref | ||
| Publica | 2.1 (1.7–2.6) | 1.2 (0.90–1.6) | ||
| Age | ||||
| 15–19 | 0.43 (0.31–0.59) | ----- | ----- | 0.013 (0.002–0.095) |
| 20–29 | 1.1 (0.91–1.3) | 0.25 (0.20–0.32) | ||
| 30–44 | ref | ref | ||
| Income | ||||
| <100% of poverty levelb | 0.72 (0.56–0.92) | ----- | ----- | 1.3 (0.9–1.8) |
| 100%– 299% | 0.89 (0.74–1.1) | 1.1 (0.9–1.5) | ||
| >300% | ref | ref | ||
| Education | ||||
| <HS diploma | ref | ----- | ----- | ref |
| HS graduate (diploma or GED) | 1.2 (0.92–1.5) | 0.77 (0.57–1.0) | ||
| Some college but no degree | 0.90 (0.69–1.2) | 0.58 (0.42–0.82) | ||
| College degree or higher | 0.69 (0.54–0.90) | 0.37 (0.26–0.52) | ||
| Parity | ||||
| 0 births | 0.10 (0.082–0.13) | ----- | ----- | 0.16(0.10–0.25) |
| 1–2 births | ref | ref | ||
| 3 or more births | 2.4 (1.9–3.1) | 2.3 (1.8–2.9) | ||
| Marital status | ||||
| Married | ref | ----- | ----- | ref |
| Divorced/widowed/separated | 2.4 (1.8–3.0) | 1.4 (1.2–1.9) | ||
| Never married | 1.6 (1.3–2.0) | 0.51 (0.37–0.70) | ||
| Religion | ||||
| No religion | 1.6 (1.3–2.0) | ----- | ----- | 0.88 (0.65–1.1) |
| Catholic | 0.88 (0.71–1.1) | 0.58 (0.41–0.81) | ||
| Protestant | ref | ref | ||
| Other religions | 1.3 (0.86–1.9) | 0.34 (0.19–0.63) | ||
Model 1: Unadjusted odds ratios; Model 2: Adjusted for history of unintended pregnancy; Model 3: Adjusted for all variables shown in table
OR, odds ratio; CI, confidence interval; HS, high school; GED, general equivalency diploma; NSFG, National Survey of Family Growth
Weighted to reflect the US female household population aged 15–44 years
aPublic insurance included Medicaid, Medicare, Medi-Gap, Indian health service, Children’s Health Insurance Program, state-sponsored, or other government program
bPoverty threshold based on 2001 level defined by the US Census Bureau, which takes into account total household income and number (i.e., $18,104 for a family of four)
The Relationships Among Race/Ethnicity, Unintended Pregnancy and Tubal Sterilization
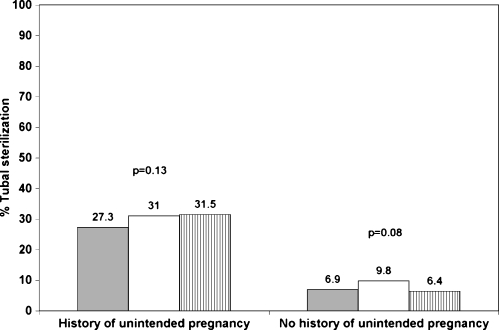
Tubal sterilization was less commonly reported by white women (15%) compared to Hispanic women (20%) or AA women (21%) (p < 0.001; Table 2). Tubal sterilization was reported by 29% of women who had ever had an unintended pregnancy compared to 7% of women who reported never having an unintended pregnancy [p < 0.0001; unadjusted odds ratio of 5.2 (95% CI: 4.4 – 6.3)]. In unadjusted analysis, Hispanic and AA women were more likely to report undergoing sterilization compared to white women (OR: 1.4; 95% CI: 1.2–1.7 and 1.5 95% CI: 1.3–1.9, respectively). When we adjusted for unintended pregnancy, the relationship between race/ethnicity and tubal sterilization was attenuated and no longer significant for Hispanic women (OR: 1.3; 95% CI: 1.0–1.6; Table 3) and for AA women (OR: 1.2; 95% CI: 0.95–1.4). Unintended pregnancy remained a significant predictor of tubal sterilization (OR: 5.1; 95% CI: 4.1–6.2). When we added the socio-demographic covariates (insurance status, age, income, education level, parity, marital status, and religion) to the model, the race/ethnicity point estimates changed only minimally (OR: 1.2; 95% CI: 0.87– 1.6 for Hispanic women and OR: 1.3; 95% CI: 1.0 – 1.6 for AA women). Although there was no significant interaction between race/ethnicity and unintended pregnancy (p = 0.23), we conducted a stratified analysis to better illustrate the effect of unintended pregnancy on tubal sterilization. In analyses stratified by history of unintended pregnancy, race/ethnicity had little effect on likelihood of having undergone tubal sterilization (Fig. 1).
Figure 1.
Percentage of women who report tubal sterilization by race/ethnicity and unintended pregnancy status. Grey bars = white women; white bars = Hispanic women; vertical stripes = African American women. Rao-Scott test for differences in tubal sterilization by race: p = 0.13 for women with history of unintended pregnancy and p = 0.08 for women without a history of unintended pregnancy. Estimates are weighted to reflect the US female household population aged 15–44 years.
Results from Sensitivity Analyses
Sensitivity analyses using “unwanted” pregnancy in place of “unintended” pregnancy produced very similar results. Overall, 14% of white women, 23% of Hispanic women, and 32% of AA women reported an unwanted pregnancy (p < 0.001). After adjustment for unwanted pregnancy, the relationship between race/ethnicity and tubal sterilization was again attenuated and no longer significant (OR: 1.2; 95% CI: 1.0–1.5 for Hispanic women and OR: 1.1; 95% CI: 0.92–1.4 for AA women) while unwanted pregnancy remained a significant predictor for tubal sterilization (OR: 4.3; 95% CI: 3.5–5.2).
DISCUSSION
In this nationally representative sample of women of reproductive age, we found that unintended pregnancy is a powerful predictor of subsequent tubal sterilization and may explain the observed racial/ethnic variation in tubal sterilization rates. Prior studies have established that AA and minority women are much more likely to choose sterilization as a method of contraception compared to white women, but it had remained unclear as to why this was the case. Our study indicates that unintended pregnancy may be the mediating variable.
By censoring pregnancies that occurred after tubal sterilization in this cross-sectional data, we were able to achieve a temporal sequence that lends itself to cause/effect reasoning. Therefore, our findings suggest that minority women, who experience higher rates of unintended pregnancy than white women, choose sterilization in response to their experiences with an unintended pregnancy. These results are consistent with those from a recent qualitative study in which AA women reported using sterilization to control perceived uncontrolled fertility.9 It is reasonable to speculate that women who have experienced an unplanned pregnancy may develop a heightened sense of susceptibility to pregnancy and/or poor contraceptive self-efficacy and perceive sterilization to be an effective way to gain control over their fertility. AA women, in particular, may turn to sterilization because they are familiar with it9 and also because they are less aware of other highly effective, reversible contraceptive options. In a survey study of women who had undergone tubal sterilization, AA women were less likely than white women to have heard of the IUD and to have overly (i.e., inaccurate) positive views of female sterilization and negative views of male sterilization.15 Although sterilization is an effective and often appropriate method of contraception, the tendency of minority women to choose sterilization as their contraceptive method of choice is concerning because the rate of post-sterilization regret is high, especially among minority women.3,16–20
Our results are also consistent with prior studies that report racial/ethnic disparities in unintended pregnancy across income levels.11 Our analysis took into account additional demographic and socio-economic variables that may confound the relationship between race/ethnicity and unintended pregnancy. While these socio-demographic variables are markers of, but do not necessarily predict, access to and use of contraceptive services, other studies have shown that minority women are just as likely to receive contraceptive services as white women.21,22 This is likely due to Title X programs that have been implemented to improve access to family planning services for vulnerable populations.23 There is also evidence that women who rely on publicly funded clinics, a population that is disproportionally made up of minorities, may actually receive more comprehensive services and be offered more contraceptive options than those who rely on private doctors.24,25 As access to comprehensive contraceptive services appears to be equal for minorities, we must consider other factors that might contribute toward racial disparities in unintended pregnancy. Attempting to understand disparities in unintended pregnancy requires consideration of a wide array of complex social and cultural issues, including sexuality, reproductive autonomy and power, gender relationships, attitudes towards pregnancy and contraception, and historical relationships with family planning programs. For example, there is some evidence suggesting that culturally based attitudes toward pregnancy and contraception may contribute toward ineffective contraceptive use and subsequent unplanned pregnancy. Another important consideration is that the level of mistrust toward the health-care system that has been noted in minority communities26 may be particularly heightened for reproductive issues because of the disturbing historical relationship between coercive family planning practices and minority populations.8,27–29 In fact, studies have shown that minority women often perceive race-based discrimination when receiving family planning services and also rate their family planning experiences less positively compared to white women.22,30 More research is needed to understand how contraceptive attitudes and patient-provider communication may vary by race/ethnicity, and how these factors as well as perceptions of family planning experiences impact contraceptive behavior across populations. While the relationship among race/ethnicity, conception, and contraceptive behavior is complex, research and advocacy efforts that shed light on the personal, historical, and cultural contexts in which unintended pregnancy and contraceptive decision making occur will help to promote reproductive health for all women.
Unintended pregnancy is a substantial problem in the US with serious consequences for women, their children, and society.14,31–34 This study provides evidence for yet another potential consequence of unintended pregnancy—it may lead women to take drastic (i.e., permanent) measures to control their fertility. Accordingly, clinicians who provide contraceptive counseling should explore the factors that shape women’s contraceptive preferences. Women who seek sterilization in response to one or more unintended pregnancies should be counseled about other highly effective, reversible methods and also informed about predictors of post-sterilization regret, including young age and non-white race.16–20 Eliciting women’s values and needs and understanding their psychosocial context are consistent with patient-centered care and will improve satisfaction with contraceptive decisions.35–37 Likewise, clinicians who are seeing women who have recently experienced unintended pregnancy should recognize that patient-centered counseling can build self-efficacy and empower women to change future health behaviors that put them at risk for unintended pregnancy.35–37 Such counseling should emphasize behaviors, assessment of abilities, and future intentions and then motivate women to develop a contraceptive plan that meets her short- and long-term reproductive goals.38,39 In addition, women who were using a contraceptive method that required adherence at the time of their unintended pregnancy (i.e., barrier or hormonal methods) may benefit from information and personalized discussion about methods that do not require adherence [i.e., intrauterine devices (IUDs) or implants].
There are important limitations to consider in interpreting the results of this analysis. First, there is considerable debate about the appropriateness of survey categories in capturing the nuances of pregnancy intention and whether interpretation of these categories varies across cultural and socio-economic groups.13,14 We have adhered to the conventional definition of unintended pregnancy and used the NSFG database, which is the primary source of data on unintended pregnancy in the US. While it is certainly possible that women mis-classify their pregnancy intentions, especially in retrospect, our sensitivity analyses examining the effect of unwanted pregnancy, a less ambiguous construct, were very similar to those for unintended pregnancy. Second, information on demographic and socio-economic factors that may have been related to unintended pregnancy or tubal sterilization was obtained at the time of interview rather than at the time of the outcome of interest. However, our primary variables of interest, race/ethnicity and history of unintended pregnancy, should remain stable over time. Third, we have no information about how health-care providers or the communication between providers and patients may have shaped decisions about sterilization. While studies have suggested that provider recommendations for a variety of medical or surgical procedures vary by patient race/ethnicity, it is unclear to what degree these variations are based on clinical rather than non-clinical factors, including racial stereotypes.26,40–43 In our prior qualitative study, AA and white women who underwent sterilization reported that their provider did not, in fact, influence their decision making about sterilization.9
In summary, in this nationally representative sample of women of reproductive age, we found that higher rates of unintended and unwanted pregnancies may help explain why minority women are more likely to undergo tubal sterilization compared to white women. Future research is needed to understand the causes of high rates of unintended pregnancy among minority women. Understanding and addressing disparities in unintended pregnancy may simultaneously offer an opportunity to eliminate currently observed racial disparities in rates of tubal sterilization.
Acknowledgements
This manuscript was made possible by Dr. Borrero’s grant (05 KL2 RR024154-04) from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research. The content of this publication is solely the responsibility of the authors and does not necessarily represent the official view of NCRR or NIH.
Conflict of Interest None disclosed.
References
- 1.Borrero S, Schwarz EB, Reeves MF, Bost JE, Creinin MD, Ibrahim SA. Race, insurance status, and tubal sterilization. Obstet Gynecol. 2007;109:94–100. doi: 10.1097/01.AOG.0000249604.78234.d3. [DOI] [PubMed] [Google Scholar]
- 2.Bumpass LL, Thomson E, Godecker AL. Women, men, and contraceptive sterilization. Fertil Steril. 2000;73:937–946. doi: 10.1016/S0015-0282(00)00484-2. [DOI] [PubMed] [Google Scholar]
- 3.Chandra A. Surgical sterilization in the United States: prevalence and characteristics, 1965–95. Hyattsville, Maryland: National Center for Health Statistics; 1998. [PubMed] [Google Scholar]
- 4.Godecker AL, Thomson E, Bumpass LL. Union status, marital history and female contraceptive sterilization in the United States. Fam Plann Perspect. 2001;33(9):35–41. doi: 10.2307/2673740. [DOI] [PubMed] [Google Scholar]
- 5.MacKay AP, Kieke BA, Jr, Koonin LM, Beattie K. Tubal sterilization in the United States, 1994–1996. Fam Plann Perspect. 2001;33:161–165. doi: 10.2307/2673719. [DOI] [PubMed] [Google Scholar]
- 6.Mosher WDMG, Chandra A, Abma JC, Wilson SJ. Use of contraception and use of family planning services in the Unites States: 1982–2002. Hyattsville, Maryland: National Center for Health Statistics; 2004. [Google Scholar]
- 7.Piccinino LJ, Mosher WD. Trends in contraceptive use in the United States: 1982–1995. Fam Plann Perspect. 1998;30(46):4–10. doi: 10.2307/2991517. [DOI] [PubMed] [Google Scholar]
- 8.Shapiro TM, Fisher W, Diana A. Family planning and female sterilization in the United States. Soc Sci Med. 1983;17:1847–1855. doi: 10.1016/0277-9536(83)90161-2. [DOI] [PubMed] [Google Scholar]
- 9.Borrero S, Nikolajski C, Rodriguez KL, Creinin MD, Arnold RM, Ibrahim SA. “Everything I Know I Learned from My Mother...or Not”: Perspectives of African-American and White Women on Decisions About Tubal Sterilization. J Gen Intern Med. 2008. [DOI] [PMC free article] [PubMed]
- 10.Kilbourne AM, Switzer G, Hyman K, Crowley-Matoka M, Fine MJ. Advancing health disparities research within the health care system: a conceptual framework. Am J Public Health. 2006;96:2113–2121. doi: 10.2105/AJPH.2005.077628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Finer LB, Henshaw SK. Disparities in rates of unintended pregnancy in the United States, 1994 and 2001. Perspect Sex Reprod Health. 2006;38:90–96. doi: 10.1363/3809006. [DOI] [PubMed] [Google Scholar]
- 12.Lepkowski JM, Mosher WD, Davis KE, Grove RM, van Hoewyk J, Willem J. National survey of family growth, cycle 6: Sample design, weighting, imputation, and variance estimation. National center for health statistics. Vital Health Stat. 2006;2(142). [PubMed]
- 13.Santelli J, Rochat R, Hatfield-Timajchy K, et al. The measurement and meaning of unintended pregnancy. Perspect Sex Reprod Health. 2003;35:94–101. doi: 10.1363/3509403. [DOI] [PubMed] [Google Scholar]
- 14.Brown S, Eisenberg L. The best intentions: unintended pregnancy and the well-being of children and families. Washington, DC: National Academy Press; 1995. [PubMed] [Google Scholar]
- 15.Borrero S, Lin Y, Dehlendorf C, et al. Differences in knowledge may contribute to racial variation in tubal sterilization rates [Abstract P25]. Contraception 2009;80.
- 16.Borrero SB, Reeves MF, Schwarz EB, Bost JE, Creinin MD, Ibrahim SA. Race, insurance status, and desire for tubal sterilization reversal. Fertility and sterility. 2007. [DOI] [PMC free article] [PubMed]
- 17.Hillis SD, Marchbanks PA, Tylor LR, Peterson HB. Poststerilization regret: findings from the United States collaborative review of sterilization. Obstet Gynecol. 1999;93:889–895. doi: 10.1016/S0029-7844(98)00539-0. [DOI] [PubMed] [Google Scholar]
- 18.Jamieson DJ, Kaufman SC, Costello C, Hillis SD, Marchbanks PA, Peterson HB. A comparison of women’s regret after vasectomy versus tubal sterilization. Obstet Gynecol. 2002;99:1073–1079. doi: 10.1016/S0029-7844(02)01981-6. [DOI] [PubMed] [Google Scholar]
- 19.Moseman CP, Robinson RD, Bates GW, Jr, Propst AM. Identifying women who will request sterilization reversal in a military population. Contraception. 2006;73:512–515. doi: 10.1016/j.contraception.2005.11.005. [DOI] [PubMed] [Google Scholar]
- 20.Schmidt JE, Hillis SD, Marchbanks PA, Jeng G, Peterson HB. Requesting information about and obtaining reversal after tubal sterilization: findings from the US collaborative review of sterilization. Fertil Steril. 2000;74:892–898. doi: 10.1016/S0015-0282(00)01558-2. [DOI] [PubMed] [Google Scholar]
- 21.Borrero S, Schwarz EB, Creinin M, Ibrahim S. The impact of race and ethnicity on receipt of family planning services in the United States. J Women’s Health (2002) 2009;18:91–96. doi: 10.1089/jwh.2008.0976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Forrest JD, Frost JJ. The family planning attitudes and experiences of low-income women. Fam Plann Perspect. 1996;28(77):246–255. doi: 10.2307/2136053. [DOI] [PubMed] [Google Scholar]
- 23.Kaeser L. Title X and the US family planning effort. New York: Alan Guttmacher Institute; 1997. [Google Scholar]
- 24.Landry DJ, Wei J, Frost JJ. Public and private providers’ involvement in improving their patients’ contraceptive use. Contraception. 2008;78:42–51. doi: 10.1016/j.contraception.2008.03.009. [DOI] [PubMed] [Google Scholar]
- 25.Frost JJ. Public or private providers? US women’s use of reproductive health services. Fam Plann Perspect. 2001;33:4–12. doi: 10.2307/2673736. [DOI] [PubMed] [Google Scholar]
- 26.Smedley BD, Stith AY, Nelson AR, editors. Unequal treatment: confronting racial and ethnic disparities in health care. Washington, DC: National Academies Press; 2003. [PubMed] [Google Scholar]
- 27.Eliot J. Fertility control and coercion. Fam Plann Perspect. 1973;5(87):132. [PubMed] [Google Scholar]
- 28.Roberts D. The pill at 40-a new look at a familiar method. Black women and the pill. Fam Plann Perspect. 2000;32:92–93. doi: 10.2307/2648220. [DOI] [PubMed] [Google Scholar]
- 29.Stern AM. Sterilized in the name of public health: race, immigration, and reproductive control in modern California. Am J Public Health. 2005;95:1128–1138. doi: 10.2105/AJPH.2004.041608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Thorburn S, Bogart LM. African American women and family planning services: perceptions of discrimination. Women Health. 2005;42:23–39. doi: 10.1300/J013v42n01_02. [DOI] [PubMed] [Google Scholar]
- 31.Cheng D, Schwarz EB, Douglas E, Horon I. Unintended pregnancy and associated maternal preconception, prenatal and postpartum behaviors. Contraception. 2009;79:194–198. doi: 10.1016/j.contraception.2008.09.009. [DOI] [PubMed] [Google Scholar]
- 32.Gipson JD, Koenig MA, Hindin MJ. The effects of unintended pregnancy on infant, child, and parental health: a review of the literature. Stud Fam Plann. 2008;39:18–38. doi: 10.1111/j.1728-4465.2008.00148.x. [DOI] [PubMed] [Google Scholar]
- 33.Najman JM, Morrison J, Williams G, Andersen M, Keeping JD. The mental health of women 6 months after they give birth to an unwanted baby: a longitudinal study. Soc Sci Med. 1991;32:241–247. doi: 10.1016/0277-9536(91)90100-Q. [DOI] [PubMed] [Google Scholar]
- 34.Wulf D, Donovan P. Women and societies benefit when childbearing is planned. Issues Brief (Alan Guttmacher Inst) 2002;1–4. [PubMed]
- 35.Abdel-Tawab N, Roter D. The relevance of client-centered communication to family planning settings in developing countries: lessons from the Egyptian experience. Soc Sci Med. 2002;54:1357–1368. doi: 10.1016/S0277-9536(01)00101-0. [DOI] [PubMed] [Google Scholar]
- 36.Houle C, Harwood E, Watkins A, Baum KD. What women want from their physicians: a qualitative analysis. Journal of women’s health (2002) 2007;16:543–550. doi: 10.1089/jwh.2006.M079. [DOI] [PubMed] [Google Scholar]
- 37.Weisman CS, Maccannon DS, Henderson JT, Shortridge E, Orso CL. Contraceptive counseling in managed care: preventing unintended pregnancy in adults. Womens Health Issues. 2002;12:79–95. doi: 10.1016/S1049-3867(01)00147-5. [DOI] [PubMed] [Google Scholar]
- 38.Oakley D. Rethinking patient counseling techniques for changing contraceptive use behavior. Am J Obstet Gynecol. 1994;170:1585–1590. doi: 10.1016/s0002-9378(94)05024-6. [DOI] [PubMed] [Google Scholar]
- 39.Singh R, Frost J, Jordan B, Wells E. Beyond a prescription: strategies for improving contraceptive care. Contraception. 2009;79:1–4. doi: 10.1016/j.contraception.2008.09.015. [DOI] [PubMed] [Google Scholar]
- 40.Ryn M, Burgess D, Malat J, Griffin J. Physicians’ perceptions of patients’ social and behavioral characteristics and race disparities in treatment recommendations for men with coronary artery disease. Am J Public Health. 2006;96:351–357. doi: 10.2105/AJPH.2004.041806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ryn M, Burke J. The effect of patient race and socio-economic status on physicians’ perceptions of patients. Soc Sci Med. 2000;50:813–828. doi: 10.1016/S0277-9536(99)00338-X. [DOI] [PubMed] [Google Scholar]
- 42.Ryn M, Fu SS. Paved with good intentions: do public health and human service providers contribute to racial/ethnic disparities in health? Am J Public Health. 2003;93:248–255. doi: 10.2105/AJPH.93.2.248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ryn M. Research on the provider contribution to race/ethnicity disparities in medical care. Med Care. 2002;40:I140–I151. doi: 10.1097/00005650-200201001-00015. [DOI] [PubMed] [Google Scholar]
- 44.Afable-Munsuz A, Speizer I, Magnus JH, Kendall C. A positive orientation toward early motherhood is associated with unintended pregnancy among New Orleans youth. Matern Child Health J. 2006;10:265–276. doi: 10.1007/s10995-005-0049-8. [DOI] [PubMed] [Google Scholar]
- 45.Gilliam ML, Davis SD, Neustadt AB, Levey EJ. Contraceptive attitudes among inner-city African American female adolescents: Barriers to effective hormonal contraceptive use. J Pediatr Adolesc Gynecol. 2009;22:97–104. doi: 10.1016/j.jpag.2008.05.008. [DOI] [PubMed] [Google Scholar]
- 46.Guendelman S, Denny C, Mauldon J, Chetkovich C. Perceptions of hormonal contraceptive safety and side effects among low-income Latina and non-Latina women. Matern Child Health J. 2000;4:233–239. doi: 10.1023/A:1026643621387. [DOI] [PubMed] [Google Scholar]
- 47.Kendall C, Afable-Munsuz A, Speizer I, Avery A, Schmidt N, Santelli J. Understanding pregnancy in a population of inner-city women in New Orleans-results of qualitative research. Soc Sci Med. 2005;60:297–311. doi: 10.1016/j.socscimed.2004.05.007. [DOI] [PubMed] [Google Scholar]
- 48.Sangi-Haghpeykar H, Ali N, Posner S, Poindexter AN. Disparities in contraceptive knowledge, attitude and use between Hispanic and non-Hispanic whites. Contraception. 2006;74:125–132. doi: 10.1016/j.contraception.2006.02.010. [DOI] [PubMed] [Google Scholar]
- 49.Thorburn S, Bogart LM. Conspiracy beliefs about birth control: barriers to pregnancy prevention among African Americans of reproductive age. Health Educ Behav. 2005;32:474–487. doi: 10.1177/1090198105276220. [DOI] [PubMed] [Google Scholar]
- 50.Unger JB, Molina GB. Acculturation and attitudes about contraceptive use among Latina women. Health Care Women Int. 2000;21:235–249. doi: 10.1080/073993300245285. [DOI] [PubMed] [Google Scholar]