Abstract
The purpose of this study was to investigate whether variations in disfluencies of young children who do (CWS) and do not stutter (CWNS) significantly change their talker group classification or diagnosis from stutterer to nonstutterer, and vice versa. Participants consisted of 17 3- to 5-year-old CWS and 9 3- to 5-year-old CWNS, with no statistically significant between-group difference in chronological age (CWS: M = 45.53 months, SD = 8.32; CWNS: M = 47.67 months, SD = 6.69). All participants had speech, language, and hearing development within normal limits, with the exception of stuttering for CWS. Both talker groups participated in a series of speaking samples that varied by: (a) conversational partner [parent and clinician], (b) location [home and clinic], and (c) context [conversation and narrative]. The primary dependent measures for this study were the number of stuttering-like disfluencies (SLD) per total number of spoken words [%SLD] and the ratio of SLD to total disfluencies (TD) [SLD/TD]. Results indicated that significant variability of stuttering did not exist as a result of conversational partner or location. Changes in context, however, did impact the CWS, who demonstrated higher SLD/TD in the conversation sample versus a narrative sample. Consistent with hypotheses, CWS and CWNS were accurately identified as stutterers and nonstutterers, respectively, regardless of changes to conversational partner, location or context for the overall participant sample. Present findings were taken to suggest that during assessment, variations in stuttering frequency resulting from changes in conversational partner, location or context do not significantly influence the diagnosis of stuttering, especially for children not on the talker group classification borderline between CWS and CWNS.
Introduction
Variability is considered to be one hallmark of childhood stuttering (e.g., Ingham & Riley, 1998; Johnson, 1961; Meyer, 1986; Sawyer & Yairi, 2006; Yaruss, 1997). In essence, a child who stutters (CWS) may demonstrate differences in frequency and/or severity of stuttering across various situations, over a given period of time (Guitar, 1998) or as the result of changes in speaking or articulatory rate (see Hall, Amir & Yairi, 1999, for a review of speaking rate in CWS). Although the exact reason(s) for the variability of childhood stuttering is still unknown, investigators have assessed several variables in attempts to determine those communicative contexts, events, etc. associated with such variability.
Specifically, researchers have investigated how stuttering varies or changes in relation to conversational partner (e.g., Martin, Kuhl, & Haroldson, 1972; Yaruss, 1997), conversational location (e.g., Onslow, Costa, & Rue, 1990; Silverman, 1971), as well as conversational context (e.g., Johnson, 1961; Yaruss, 1997). Central to all of these investigations is the notion that stuttering is most apparent when the child is conversing with a conversational partner, a situation that most closely emulates the child’s real-life speaking experiences (Ingham & Riley, 1998) and less apparent during a narrative or story-telling task (Yaruss, 1997). Thus, bi-directional communication, between a child who stutters and his or her conversational partner, typically a mother or father, in a naturalistic environment (i.e., home) is considered to be one key prerequisite for childhood stuttering to manifest itself (Martin et al., 1972). In contrast, CWS are less likely to exhibit more atypical disfluencies during a monologue-type task (i.e., a narrative or story telling task) (Yaruss, 1997) when compared to dialogue-type tasks (i.e.., conversational task).
Although less well studied than conversational discourse, stuttering variability within narrative tasks (i.e., story-retelling and story generation) has also been explored (e.g., Trautman, Healey, Brown, Brown & Jermano, 1999). Specifically, findings indicated that the percentage of stuttering was significantly higher during a story-retelling task in comparison to a story generation task. It is important to note that empirical studies of narrative abilities (e.g., Scott et al., 1995; Weiss & Zebrowski, 1994) and stuttering variability in (Trautman et al., 1999) in children who stutter have typically involved school-aged children with limited discussion regarding preschool-age children (e.g., Yaruss, 1997). Thus, if stuttering frequency of school-age children varies as the result of narrative task elicitation, one might expect to observe the same with preschool children who stutter. This assumption, however, awaits empirical verification.1
Interestingly, in most of the above studies there is minimal discussion of whether differences or variability of childhood stuttering actually have a significant impact in terms of the child being diagnosed or classified as a stutterer. For example, would a child conversing with the same conversational partner, in the child’s home versus a typical clinical setting, exhibit enough variability of stuttering to result in a different diagnosis of stuttering in the home versus clinic? In essence, would variability in stuttering frequency, from one situation or conversational partner to another be sufficient to lead a clinician or researcher to classify a child a stutterer one time but a normally fluent speaker another?
Realistically, not all clinicians have access to other communication partners (i.e., the parent), locations (i.e., home), or contexts (i.e., narrative). This fact would seem to suggest that obtaining multiple sampling of partners, location and context is the ideal or recommended protocol rather then the real protocol that most clinicians must perforce typically employ. It seems reasonable, therefore, to explore whether this relatively common practice – of using less than multiple samples of various communication partners, locations and contexts – significantly impacts a clinician’s ability to determine talker group classification.
We hasten to note, however, that none of the above suggests that variability in stuttering frequency does not occur with changes in partners, situations or context. Instead, what it does suggest is that such variability may not make a significant difference when determining whether a child should be classified or diagnosed as someone who stutters. Indeed, we are suggesting that the importance of stuttering variability should be considered in reference to how it may or may not impact a variety of diagnostic, treatment or research decisions like talker group classification. These are, of course, all empirical issues in wait of objective examination.
It is apparent, upon reflection, that the number of permutations of different conversations, conversational partners and conversational situations is beyond the scope of any one empirical study. Nevertheless, some reasonable beginning can and should be initiated in attempts to determine whether variation, at both group as well as individual levels, is sufficient to impact diagnostic decisions. It would seem that if such variability was of sufficient magnitude, most preschool-age CWS would frequently be diagnosed as a person who stutters in one situation but not in another. Although not an unreasonable conjecture, such possibilities do not appear to be supported, one way or the other, based on clinical experience as well as empirical data.
Again, the present writers are not questioning whether variability exists among CWS. Variability in stuttering frequency is apparent to anyone who treats and studies childhood stuttering. Indeed, variability in stuttering is one of the main reasons prudent clinicians attempt to characterize the degree (as well as possible sources) of variability of stuttering for the child they are treating (Ingham & Riley, 1998). This window of variability serves as a referent or benchmark against which to assess whether the child’s therapeutic intervention is more or less effective. Those are sound practices that we do not question. What we do question, however, is whether variability of stuttering frequency is sufficient to “cross” diagnostic boundaries for most children who stutter.
We speculate that for children who stutter as a group – averaging across those who are mild, moderate and severe in nature - variations in stuttering make little differences diagnostically. We further speculate that this is particularly true for those who are moderate to severe. Conversely, we believe this is less the case for children whose stuttering is very mild and closer to the boundary between being a child who does or does not stutter (CWNS). For these children whose stuttering is relatively mild, we speculate that some may appear not to stutter in one situation but stutter in another. If the above speculation is supported after manipulation of some of the more typical aspects of bi-directional communication (e.g., changes in conversational partner, location and conversational context), we will need more systematic empirical assessment of the oft-suggested notion that CWS should be examined in various situations, with various partners, etc.
Diagnostically and empirically, the frequency of stuttering-like (SLD) and non-stuttering-like disfluencies (nSLD) is commonly used to help determine the presence or absence of stuttering (e.g., Cordes & Ingham, 1994; Pellowski & Conture, 2002; Yairi & Ambrose, 2005; Yaruss, 1998). Typically, presence or frequency of stuttering is based on two fundamental measurements: (1) number of total disfluencies (SLD + nSLD) per total number of spoken words [%TD] and (2) number of SLDs per total number of spoken words [%SLD] (Yaruss, 1998). Empirical evidence suggests that for CWS, the %TD and %SLD are typically greater than 10% and 3%, respectively (see Conture, 2001; Cordes & Ingham, 1994; Sawyer & Yairi, 2006).
The ratio of SLD to TD (%SLD/TD) is another diagnostic index that has been used empirically to reliably distinguish between CWS and CWNS. On average, the %SLD/TD for CWS has been found to be approximately 65% or greater whereas the %SLD/TD for CWNS has been reported at 40% or lower (Ambrose & Yairi, 1999; Pellowski & Conture, 2002; Yairi, 1997). However, the question that remains unanswered is whether known variability in childhood stuttering significantly affects the diagnostic categories driven by the %SLD/TD.
Thus, the purpose of the present study was to determine whether variations in disfluencies of young CWS and young CWNS significantly influence their diagnosis from stutterer to nonstutterer, and vice versa. Specifically, we wanted to assess whether changes in diagnostic categories would occur as a result of changes in conversational partner (parent – clinician), location (home – clinic setting) and context (conversation – narrative).
If, for most children, the diagnostic category (CWS or CWNS) does change in association with changes in conversational partner, location and context, this would imply that basing the diagnosis of stuttering on a limited number and type of samples is contraindicated, even if the clinician has limited access to obtaining additional samples (i.e., in the home or with the parent). If, however, the diagnostic category does not change substantially, this would imply that clinicians should be able to diagnosis stuttering (or nonstuttering) in preschool-age children with some level of confidence for most children based on a limited number and type of speech samples. This latter implication would seem to provide support for those clinicians who have limited to no access to other conversational partners (i.e., the parent), other locations (i.e., home), or contexts (i.e., narrative).
Given the above, we developed two hypotheses. First, we hypothesized, for both preschool CWS and CWNS, that their respective diagnostic categories would not significantly change as a result of changes in conversational partner, context or location. Secondly, it was hypothesized that changes in these variables (i.e., conversational partner, context, and location), would have their greatest impact on children on or around the borderline for each talker group classification (CWS or CWNS).
Method
Participants
Participants consisted of 17 preschool CWS and 9 preschool CWNS, all of whom were native speakers of American English. All children participated in a series of studies through the Vanderbilt University Developmental Stuttering Research Project.
Participants were between the ages of 3;0 and 5;2 (CWS: M = 45.53, SD = 8.32; CWNS: M = 47.67, SD = 6.69) with no statistically significant between-group difference (t [24] = −.664, p = .51) in chronological age. The CWS group consisted of 12 boys and 5 girls (all were Caucasian), and the CWNS group consisted of 5 boys and 4 girls (eight Caucasian participants and one Hispanic participant). For the CWS group, 14 parents of the 17 participants expressed concern about their child’s speech fluency, reporting an average time since initial onset of stuttering (TSO) of 12.07 months (SD = 11.28 months; range = 1 – 38 months). Time since onset was unavailable for the 3 parents who did not express concern about their child’s speech fluency. TSO was determined using the “bracketing” procedure (see Yairi & Ambrose, 1992 for a description; Anderson, Pellowski, Conture, & Kelly, 2003; Anderson, Wagovich & Hall, 2006; Anderson, 2007).
Each child’s social-economic status (SES) was calculated and described for the parents of all participants. SES was determined through application of the Four Factor Index of Social Position (Hollingshead, 1975), which involves the assessment of maternal and paternal occupation and education levels for each participant, with scores ranging from 8 to 66. A higher score suggests higher SES. There was no statistically significant between-group difference in SES, t [24] = .181, p = .86, in SES between CWS (M = 45.59, SD = 9.01) and CWNS (M = 44.94, SD = 7.85).
All participants were paid volunteers referred to the Vanderbilt Bill Wilkerson Center by their parents, speech-language pathologists, daycare, preschool, or school personnel. None of the 26 children had received formal/structured intervention for stuttering or any other communication disorder prior to participation in this study. Also, participants had no known or reported hearing, neurological, developmental, academic, intellectual, or emotional problems. This study’s protocol was approved by the Institutional Review Board at Vanderbilt University, Nashville, Tennessee. For each of the 26 participants, parents signed an informed consent, and their children assented.
Excluded participants
From an initial group of 25 CWS, 8 participants were excluded because they were missing one or more of the conversational samples (e.g., narrative with clinician in clinic, conversation with parent in home, etc.) analyzed in this study. From an initial group of 18 CWNS, 9 participants were excluded because they were missing one or more of the conversational samples analyzed in this study. All children that remained (i.e., 17 CWS and 9 CWNS) participated in all samples analyzed as part of the final data corpus.
Classification
Classification for CWS and CWNS was based on a typical 300-word conversational sample between the child and a clinician in a clinical setting as well as scores on the Stuttering Severity Instrument-3 (SSI-3; Riley, 1994). Table 1 depicts both talker groups divided by severity.
Table 1.
Number of children who stutter (CWS) (n=17) and children who do not stutter (CWNS) (n=9) exhibiting one of five Stuttering Severity Instrument-3 (SSI-3; Riley, 1994) ratings. For CWNS, 100% (n=9) of the participants had a rating of “Very Mild” (the lowest obtainable SSI-3 rating); for CWS, ≈53% (n=9) had a rating of “Mild”, ≈35% (n=6) rated as “Moderate”, and ≈12% (n=2) rated as “Severe” or “Very Severe”.
| Severity | CWS | CWNS | |
|---|---|---|---|
| Very Mild | 0-8 | 0 | 9 |
| 9-10 | 0 | 0 | |
|
| |||
|
| |||
| Mild | 11-12 | 2 | 0 |
| 13-16 | 7 | 0 | |
|
| |||
|
| |||
| Moderate | 17-23 | 5 | 0 |
| 24-26 | 1 | 0 | |
|
| |||
|
| |||
| Severe | 27-28 | 1 | 0 |
| 29-31 | 0 | 0 | |
|
| |||
|
| |||
| Very Severe | 32 + | 1 | 0 |
|
| |||
| Total | 17 | 9 | |
Children who stutter (CWS)
As used in previous studies (e.g., Pellowski, & Conture, 2002; Arnold, Conture, & Ohde, 2005; Hartfield & Conture, 2006; Karrass et al., 2006; Schwenk, Conture, & Walden, 2006), a child was considered a CWS if he or she (a) exhibited three or more stuttering-like disfluencies (SLD; i.e., sound/syllable repetitions, monosyllabic whole-word repetitions, sound prolongations, inaudible sound prolongations) per 100 words of conversational speech with a clinician in a clinical setting (based on a 300-word sample; Bloodstein, 1995; Conture, 2001; Yairi & Ambrose, 1992) and (b) received a total score of 11 or above (a severity equivalent of at least “mild”) on the SSI-3 (CWS had a mean score of 18.40, SD = 8.77).
Children who do not stutter (CWNS)
As used in previous studies (e.g., Arnold et al., 2005; Hartfield & Conture, 2006; Karrass et al., 2006; Pellowski, & Conture, 2002; Schwenk et al., 2006), a child was considered a CWNS if he or she (a) exhibited two or fewer SLD per 100 words of conversational speech with a clinician in a clinical setting (based on a 300-word sample) and (b) received an overall score of 10 or less (a severity equivalent of less than “mild”) on the SSI-3 (CWNS had a mean score of 5.00, SD = 3.30).
Typical Clinical Condition
As previously stated, a typical 300-word conversational sample between the child and a clinician in a clinical setting was elicited from each child. While a conversational sample obtained with the parent in the home environment is considered to be one of the more ideal settings within which to assess childhood stuttering, the present authors used the conversational sample in the clinic as the baseline measure. This was done because this type of setting (i.e., clinical setting between a child and a clinician) is most often used during the assessment of stuttering (Curlee, 2007), particularly in diagnostic environments where the parent or home environment may not be readily accessible. Therefore, this conversational sample from each child served as the typical clinical condition which was used to compare samples elicited from the experimental settings (a - Home with clinician, b - Home with parent, c - Clinic with parent, and d - Narrative with clinician).
Standardized Speech-Language Tests and Hearing Screening
To participate in this study, all participants scored at the 16th percentile or higher on the (a) Peabody Picture Vocabulary Test- Third Edition (PPVT-IIIA or B; Dunn & Dunn, 1997), (b) Expressive Vocabulary Test (EVT; Williams, 1997), (c) Test of Early Language Development-3 (TELD-3; Hresko, Reid, & Hamill, 1999) and (d) “Sounds in Words” subtest of the Goldman-Fristoe Test of Articulation-2 (GFTA-2; Goldman & Fristoe, 2000), standardized tests used to assess receptive and expressive vocabulary, receptive and expressive language skills, and articulation abilities, respectively. These tests were administered to each child during a visit to the child’s home approximately 1-2 weeks before the child’s visit to the clinic. Furthermore, each participant passed a bilateral pure tone hearing and tympanometric screening (ASHA, 1990) during their visit to the clinic.
Procedures
Each child participated in a series of speaking samples that varied by conversational partner (parent and clinician) and location (home visit and clinic visit) as well as one narrative sample. Samples taken at the home visit and the clinic visit were elicited 1-2 weeks apart. At each location, a parent conversational sample and clinician conversational sample were elicited during the same visit with the addition of a narrative sample during the clinic visit. Although all home samples were taken during a visit occurring before clinic samples, in both settings (home and clinic) all conversational samples were counterbalanced within each visit
Conversational Sample with the Parent and Clinician
Each child participated in a 300-word conversational sample with the parent, typically the mother, in both the (1) home and (2) clinical setting; each child also participated in a 300-word conversational sample with the clinician in both the (3) home and (4) clinical setting. In each setting (home with parent and clinician; clinical setting with parent and clinician), age-appropriate toys were provided to stimulate dialogue. Each of these 4 conversations was approximately 20 minutes in length to allow for a complete 300-word sample. Once 300-words were obtained, each conversational sample was finished.
Narrative Sample with the Clinician
Each child participated in a narrative sample with the clinician in a clinical setting using excerpts from a series of wordless picture books (Mayer, 1967, 1969, 1973) in a randomized design. For this preliminary study, it was not possible, given preschool children’s inattention, fatigue and/or lack of cooperation in the home, to reliably obtain a narrative sample with the clinician in the home. To elicit the narrative sample, the participant initially, viewed sequential story-book pages from wordless picture books. These pages were displayed, one-at-a-time, on a computer monitor and the child was instructed by the experimenter to “look at the pictures and think about a story”. After viewing the story book pages once, the experimenter returned to the beginning storybook page and prompted the participant to create a story while the experimenter advanced through the set of storybook pictures a second time for the participants viewing. During the narrative task, the clinician randomly provided vague prompts (e.g., “uh-huh”, “really”, “what else”, “what happened next”) throughout the sample in order to encourage speech from each participant. Narrative samples were approximately 200-300 words in length.
Definition/ Description of Main Dependent Measures
Speech disfluencies
The primary dependent measure for this study was the (a) %SLD/%nonSLD (for CWS the %SLD was used; for CWNS, the %nonSLDs were used since CWNS do not exhibit substantially amounts of SLDs) and (b) SLD/TD obtained from each 300-word conversational/narrative sample.
As previously stated, each child participated in a conversational sample that varied by partner (clinician vs. parent) and location (home vs. clinic). Each child also participated in a narrative sample with the clinician to compare to the conversational sample with the clinician, which allowed for variation of context. Therefore, the dependent measure, speech disfluencies, was analyzed accordingly.
Intrajudge and interjudge measurement reliability
Identification of stuttering-like and nonstuttering-like speech disfluencies
Intra- and interjudge measurement reliability was obtained for total disfluencies (stuttering-like + nonstuttering-like) and stuttering-like disfluencies. Three participants (18% of CWS group and ≈33% of CWNS group) per each of the two talker group (CWS and CWNS) were randomly selected (n=6) and the typical clinical diagnostic conversation (clinician-child conversation in clinical setting) for each participant was used for intra- and interjudge reliability. Intrajudge reliability was assessed by having the first author judge each sample for the mean frequency of total and (non) stuttering-like disfluencies for the first 100 words on two separate occasions. Interjudge reliability was assessed by having the first author and a doctoral student, blind to talker group classification judge each sample for the mean frequency of total and (non)stuttering-like disfluencies for the first 100 words on two separate occasions. Both the first author (Judge 1) and the doctoral student (Judge 2) were certified speech-language pathologists with experience assessing stuttering. Intra- and interjudge reliability for three speech disfluency measures (mean frequency of [1] total disfluencies per 100 words, [2] stuttering-like disfluencies per 100 words, and [3] nonstuttering-like disfluencies per 100 words) was based on the Kappa statistic (Cohen, 1960).
For CWS, intrajudge reliability for the mean frequency of total speech disfluencies, stuttering-like disfluencies, and nonstuttering-like disfluencies was .98, .96, and .89, respectively. Interjudge reliability for the overall mean frequency of total speech disfluencies, stuttering-like disfluencies, and nonstuttering-like disfluencies was .97, .97, and .94, respectively. For CWNS, intrajudge reliability for the mean frequency of total speech disfluencies, stuttering-like disfluencies and nonstuttering-like disfluencies was.81, 1.00, and .78 respectively. Interjudge reliability for the overall mean frequency of total speech disfluencies, stuttering-like disfluencies and nonstuttering-like disfluencies was.92, 1.00, and .91 respectively.
Results
Descriptive Information
Stuttering/Speech Disfluencies
Descriptive statistics for %SLD, %nonSLD, and SLD/TD, for CWS (n=17) and CWNS (n=9), are presented in Table 2.
Table 2.
Means and standard deviations for %SLD, %nonSLD and SLD/TD by partner, context, and location for preschool CWS (n=17) and CWNS (n=9).
| CWS | CWNS | ||||
|---|---|---|---|---|---|
| M | SD | M | SD | ||
| %SLD | Home Clinician | 10.02 | 8.52 | .97 | .65 |
| Home Parent | 8.47 | 6.22 | .85 | .51 | |
| Clinic Clinician | 8.58 | 7.04 | .57 | .52 | |
| Clinic Parent | 8.14 | 6.51 | .72 | .59 | |
| Clinic Narrative | 7.72 | 9.47 | 1.00 | 1.16 | |
| %nonSLD | Home Clinician | 2.85 | 1.43 | 3.79 | 3.14 |
| Home Parent | 3.35 | 1.72 | 2.78 | 2.43 | |
| Clinic Clinician | 4.15 | 2.92 | 3.30 | 2.23 | |
| Clinic Parent | 2.86 | 1.20 | 3.27 | 2.51 | |
| Clinic Narrative | 5.11 | 3.10 | 3.66 | 4.51 | |
| SLD/TD | Home Clinician | 70.85 | 17.64 | 23.24 | 14.97 |
| Home Parent | 68.67 | 12.61 | 25.91 | 13.47 | |
| Clinic Clinician | 65.00 | 20.25 | 17.70 | 14.24 | |
| Clinic Parent | 68.39 | 17.20 | 18.87 | 21.46 | |
| Clinic Narrative | 55.59 | 19.25 | 14.50 | 13.47 | |
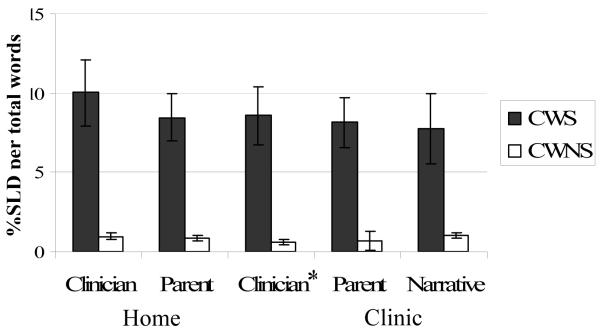
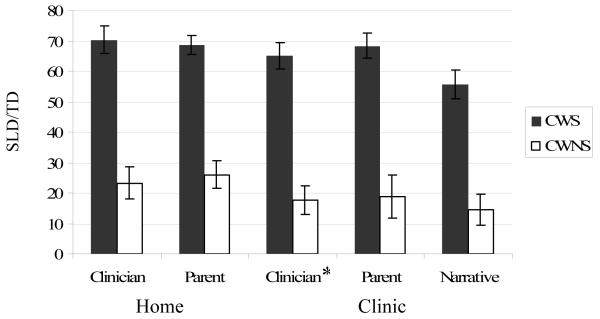
Based on the typical clinical condition only (i.e., clinician-child conversation in clinical setting), there was a statistically significant difference, t [24] = 3.38, p < .01, in frequency of stuttering-like disfluencies (see Figure 1) between CWS (M = 8.58, SD = 7.04) and CWNS (M = .57, SD = .52) as well as a significant difference, t [24] = 6.21, p < .001, in the ratio of SLD/TD (see Figure 2) between CWS (M = 65.00, SD = 20.25) and CWNS (M = 17.70, SD = 14.24).
Figure 1.
Mean %SLD for present study participants across location, conversational speaker and context from the present sample (± standard error); * Typical Clinical Conversation.
Figure 2.
Mean SLD/TD for present study participants across location, conversational speaker and context from the present sample (± standard error); * Typical Clinical Conversation.
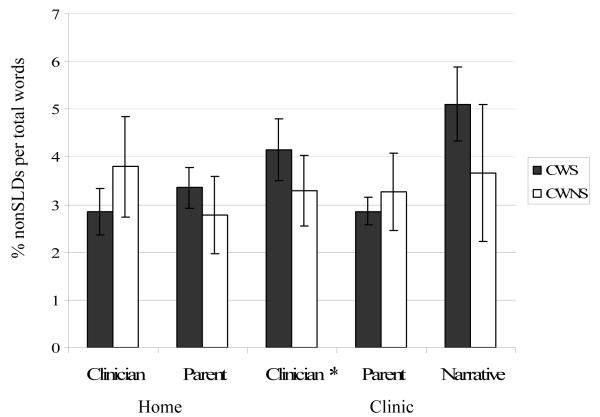
There was, however, no significant difference, t [24] = .77, p = .45, in nonstuttering-like disfluencies (see Figure 3) between CWS (M = 4.15, SD = 2.92) and CWNS (M = 3.30, SD = 2.23). Thus, as expected based on selection criteria, the two groups of children were significantly different in terms of basic measures of stuttering in the typical clinical condition (i.e., clinician-child conversation in clinical setting).
Figure 3.
Mean %nonSLD for present study participants across location, conversational speaker and context from the present sample (± standard error); * Typical Clinical Conversation.
Speech and Language Abilities
Based on participant inclusion/exclusion criteria described above, all 26 participants in this study had to exhibit scores at or above the 16th percentile (less than 1 SD below the mean) on a series of standardized speech-language tests (PPVT-III, EVT, TELD-3, and GFTA-2) in order to be included in the final sample. A multivariate analysis of variance (MANOVA) revealed no significant between-group differences on any of these five measures of speech and language: PPVT, F(1,24)= .00, p=.99; EVT, F(1,24)= 1.63, p=.21; TELD- Receptive Language, F(1,24)= 2.64, p=.12; TELD- Expressive Language, F(1,24)= .75, p=.40; and GFTA, F(1,24)= −.42, p=.68. See Table 3 for means and standard deviations for each standardized test per talker group.
Table 3.
Standard Scores (means, M, and standard deviation, SD) for children who stutter (CWS; n=17) and children who do not stutter (CWNS; n=9) for all standardized speech-language tests
| Speech-language test | CWS | CWNS | ||
|---|---|---|---|---|
| M | SD | M | SD | |
| PPVT-III | 108.65 | 13.61 | 108.56 | 8.17 |
| EVT | 114.18 | 9.85 | 109.33 | 7.75 |
| TELD-3 | ||||
| Expressive subtest | 116.06 | 11.24 | 107.78 | 14.35 |
| Receptive subtest | 107.29 | 14.53 | 102.78 | 7.77 |
| GFTA-2 | 108.59 | 11.26 | 110.44 | 9.94 |
Note: PPVT-III: Peabody Picture Vocabulary Test – III; EVT: Expressive Vocabulary Test; TELD-3: Test of Early Language Development -3; GFTA-2: Goldman-Fristoe Test of Articulation-2.
Influence of partner, location and context on stuttering and related measure
Paired-sample t-tests were used to determine whether there was significant variability depending on partner, location, and situation. For CWS, the frequency of stuttering (%SLD) and the ratio of stuttering-like to total disfluencies (SLD/TD) were used. However, since CWNS do not exhibit significant amounts of SLDs, only their frequency of nonstuttering disfluencies (%nonSLD) was used.
Partner
Tests of the effects of the partner (parent versus clinician) were tested separately at the home and clinic locations. For CWS, there were no significant difference between the %SLD and SLD/TD ratios from the speech samples taken with the clinician and the samples taken with the parent when tested at home, %SLD: t (16) = 1.46, p=.16 and SLD/TD: t (16) = .48, p=.64. Likewise, there were no significant difference for CWS from speech samples taken with the clinician versus the parent when tested at the clinic, %SLD: t (16) = .65, p=.53 and SLD/TD: t (16) = −.85, p=.41. For CWNS, there were no significant differences between %nonSLD from the speech samples taken with the clinician and the samples taken with the parent when tested at home, t (8) = 1.80, p=.11, or at the clinic, t (8) = .05, p=.96.
Location
For CWS, tests of the effects of the location (i.e., home versus clinic) on %SLD and the SLD/TD ratios indicated no significant differences when tested with the parent, %SLD: t (16) = .51, p=.62 and SLD/TD: t (16) = .07, p=.95, or with the clinician %SLD: t (16) = 1.64, p=.12 and SLD/TD: t (16) = 1.36, p=.19. For the CWNS, there was no significant difference between %nonSLD from the speech samples taken at home versus the clinic with the parent t (8) = −.51, p=.62, and with the clinician t (8) =.67, p=.52.
Context
For CWS, tests of the effects of context (narrative versus conversation) on %SLD and SLD/TD ratio were assessed from the child’s conversation with the clinician at the clinic and the child’s narrative with the clinician at the clinic. The %SLD did not significantly differ between the two contexts, t (15) = .97, p=.35. However, when the two SLD/TD ratios were compared, for the CWS, the ratio from the conversational sample was significantly higher than the ratio from the narrative, t (15) = 2.58, p < .05. For CWNS, the %nonSLD did not significantly differ between the two contexts, t (7) = −.39, p=.71.
Influence of partner, context and location on talker group classification
After testing the data for variability, we next tested the main hypotheses of the study, Will conversational partner, context, or location impact talker group classification? Chi-square tests of independence were used to test whether children’s predicted talker group would be the same regardless of conversational partner (parent versus clinician), location (home versus clinic), or context (conversation versus narrative). Significant chi-square statistics would indicate that talker group based on one speech sample is related to the talker group based on the other speech sample (see Table 4 for comparisons of talker group classification derived from different conversational partner, location, and context).
Table 4.
Predicted talker group observed (obs) and expected by chance (exp) when comparing conversations with the clinician and the parent (n=26).
| Home | *Clinic | ||||
|---|---|---|---|---|---|
| Classified Talker Group with Parent |
Classified Talker Group with Parent |
||||
| Classified Talker Group with Clinician |
CWS Obs (Exp) |
CWNS Obs (Exp) |
Classified Talker Group with Clinician |
CWS Obs (Exp) |
CWNS Obs (Exp) |
| CWS | 14 (9) | 2 (7) | CWS | 14 (9) | 1 (6) |
| CWNS | 0 (5) | 10 (5) | CWNS | 0 (5) | 9 (4) |
| Clinician | *Parent | ||||
|---|---|---|---|---|---|
| Classified Talker Group in Home |
Classified Talker Group in Home |
||||
| Classified Talker Group in Clinic |
CWS Obs (Exp) |
CWNS Obs (Exp) |
Classified Talker Group in Clinic |
CWS Obs (Exp) |
CWNS Obs (Exp) |
| CWS | 16 (10) | 0 (6) | CWS | 13 (8) | 0 (5) |
| CWNS | 1 (6) | 9 (4) | CWNS | 1 (7) | 10 (5) |
| Clinician | ||
|---|---|---|
| Classified Talker Group from Narrative |
||
| Classified Talker Group from Conversation |
CWS Obs (Exp) |
CWNS Obs (Exp) |
| CWS | 13 (8) | 0 (5) |
| CWNS | 1 (7) | 10 (5) |
Note: Table 4 depicts data resulting from the Chi-Square Analyses conducted in the present study. Data listed as Expected (Exp) is based on chance alone, if the classification from one conversation was in no way related to the classification from the other conversation. Data listed as Observed (Obs) is based on the actual findings of the present study. Thus, as the result of changes to variables included in the present study (Location – Home v. Clinic, Conversational Partner – Parent v. Clinician, Context – Conversation v. Narrative), Table 4 illustrates the number of participants classified in each talker group. In each variable within the table, diagonal numbers represent individuals with identical diagnoses from components of each variable. In other words, based on changes in conversational partner within the home, there were 14 (of 17) participants with identical CWS diagnoses and 9 (of 9) participants with identical CWNS diagnoses.
Two children did not fit the criteria for either group based on the conversational sample with the parent in the clinic. One child was classified as CWS based on the clinician conversation, and the other was classified as CWNS.
Partner
Tests of the effects of the conversational partner (parent versus clinician) were tested separately for the home and clinic locations. Based on the speech samples taken at the child’s home, the predicted talker group from the conversation with the clinician was significantly related to the predicted talker group from the conversation with the parent, χ2 (1) = 18.96, p < .001. When examining the conversational samples taken at the clinic, again the predicted talker group from the conversation with the clinician was also significantly related to the predicted talker group from the conversation with the parent, χ2 (2) = 20.09, p < .001. In essence, whether speech was measured in the home or in the clinic, the conversational partner did not significantly impact into which talker group the child would be classified.
Location
Next, the effects of the location (home versus clinic) were tested separately for the parent and clinician conversations. When testing whether the location affected the talker group in conversation with the clinician, the talker group derived from the home sample was significantly related to the talker group derived from the clinic sample, χ2 (1) = 18.24, p < .001. When testing whether location impacted the talker group based on conversations with the parent, again the talker group derived from the home sample was significantly related to the talker group derived from the clinic sample, χ2 (2) = 20.25, p < .001. In other words, talker group classification was the same whether measured in the home or the clinic.
Context
Finally, the predicted talker group based on the child’s conversation in the clinic with the clinician was compared to the predicted talker group based on the child’s narrative production in the clinic with the clinician. The predicted talker groups from the conversations and narratives were significantly related, χ2 (1) = 13.21, p < .001.
Type I error control
The False Discovery Rate (FDR; Benjamini & Hochberg, 1995) was used to control Type I error in preceding chi-square analyses. FDR is preferable to the standard Bonferroni procedure or Hochberg’s (1988) step-up Bonferroni procedure because it adequately controls for Type I error without the resultant increase in Type II error seen with Bonferroni and related procedures (Keselman, Cribbie, & Holland, 1999). After adjusting for the FDR, all five of the chi-square results remained statistically significant.
Influence of partner, context and location on talker group classification of borderline participants
We want to qualify the subsequent findings by noting that the sample size studied was insufficient for definitive use of inferential statistics. Be that as it may, we wanted to descriptively achieve some sense of how the variations (i.e., changes in partner, context, and location) in our measures would impact children at or near the borderline for talker group classification. To examine the influence of partner, context and location on talker group classification for those children on the borderline between CWS and CWNS (based on the typical clinical condition), the percentages of borderline participants consistently classified were reported.
Based on the %SLD yielded from the typical clinical condition, 9 participants (CWS n=5; CWNS n=4) from the present sample were identified as borderline based on, for CWS, a %SLD ranging from 3-4% and, for CWNS, a %SLD ranging from 1-2%. Again, the percentages of borderline participants consistently classified regardless of variations to location, partner and context were reported (see Table 5 for comparisons of talker group classification).
Table 5.
Predicted talker group, based on participants on the borderline between CWS and CWNS, observed (obs) and expected by chance (exp) when comparing conversations with the clinician and the parent (n=9; CWS =5, CWNS =4).
| Home | *Clinic | ||||
|---|---|---|---|---|---|
| Classified Talker Group with Parent |
Classified Talker Group with Parent |
||||
| Classified Talker Group with Clinician |
CWS Obs (Exp) |
CWNS Obs (Exp) |
Classified Talker Group with Clinician |
CWS Obs (Exp) |
CWNS Obs (Exp) |
| CWS | 2 (1) | 2 (3) | CWS | 3 (1) | 1 (2) |
| CWNS | 0 (1) | 5 (4) | CWNS | 0 (2) | 4 (3) |
| Clinician | *Parent | ||||
|---|---|---|---|---|---|
| Classified Talker Group in Home |
Classified Talker Group in Home |
||||
| Classified Talker Group in Clinic |
CWS Obs (Exp) |
CWNS Obs (Exp) |
Classified Talker Group in Clinic |
CWS Obs (Exp) |
CWNS Obs (Exp) |
| CWS | 3 (2) | 1 (2) | CWS | 2 (1) | 0 (1) |
| CWNS | 1 (2) | 4 (3) | CWNS | 1 (2) | 5 (4) |
| Clinician | ||
|---|---|---|
| Classified Talker Group from Narrative |
||
| Classified Talker Group from Conversation |
CWS Obs (Exp) |
CWNS Obs (Exp) |
| CWS | 2 (1) | 2 (3) |
| CWNS | 1 (2) | 4 (3) |
Note: Table 5 depicts data resulting from descriptive analyses of borderline participants included in the present study. Data listed as Expected (Exp) is based on chance alone, if the classification from one conversation was in no way related to the classification from the other conversation. Data listed as Observed (Obs) is based on the actual findings of the present study. Thus, as the result of changes to variables included in the present study (Location – Home v. Clinic, Conversational Partner – Parent v. Clinician, Context – Conversation v. Narrative), Table 5 illustrates the number of participants classified in each talker group. In each variable within the table, diagonal numbers represent individuals with identical diagnoses from components of each variable. In other words, based on changes in conversational partner within the home, there were 2 (of 5) participants with identical CWS diagnoses and 5 (of 5) participants with identical CWNS diagnoses.
One child did not fit the criteria for either group based on the conversational sample with the parent in the clinic.
Partner
Based on the speech samples taken from conversation with the clinician in the home versus the clinic, 77.8% (7 out of 9) borderline participants were consistently classified. Based on speech samples taken from conversation with the parents in the home versus the clinic, 87.5% (7 out of 8) borderline participants were consistently classified. In essence, for borderline CWS and CWNS, when measured in the home or clinic, the majority of participants were consistently classified regardless of partner.
Location
Based on the speech samples taken from conversations in the home with the parent versus the clinician, 77.8% (7 out of 9) borderline participants were consistently classified. Based on speech samples taken from conversations in the clinic with the parent versus the clinician, 87.5% (7 out of 8) borderline participants were consistently classified. Again, the majority of participants were consistently classified regardless of location.
Context
Finally, 66.7% (6 out of 9) borderline participants were consistently classified based on conversational and narrative samples taken in the clinic with the clinician. This finding suggests that the nature or context of communication (i.e., conversational versus narrative samples) has the greatest influence of the three conditions – partner, location and context – on determining talker group classification among those on the classification borderline.
Results of the present study lead to 3 main findings. The first main finding was that, changes in conversational partner, location, and context were not significantly related to changes in the %SLD, %nonSLD and the SLD/TD, with the exception of SLD/TD which differed in CWS (but not CWNS) between conversation and narrative. The second main finding was that these variations, although theoretically and empirically meaningful, were not found to significantly influence the diagnosis of CWS and CWNS, as a whole. The third main finding, based on descriptive analyses for participants on the borderline between CWS and CWNS, indicated that neither the conversational partner nor location had substantial influence on talker group classification, but that conversational context did have some influence. The general implications of each of these three findings will be discussed immediately below.
Influence of Conversational and Contextual Changes on Stuttering Frequency
The first main finding indicated that the %SLD (for CWS), the %nonSLD (for CWNS), and SLD/TD did not vary significantly for either talker group as a result of changes in conversational partner (parent – clinician) and location (home – clinic). However, with changes to context, significant variation in the SLD/TD was seen in CWS, but not in CWNS. Based on these findings, a sample of a preschool-age CWS’s stuttering frequency of stuttering, obtained from a typical clinical situation (e.g., child talking to clinician in a clinical setting) would not vary substantially from the frequency of stuttering obtained from a sample of the same child in the home or from conversational samples with the parent in either setting. This does not mean that evaluating fluency in various settings is not helpful and informative during both the evaluation and treatment of stuttering. However, many clinicians are often faced with the need to make a reasonably confident decision based solely on their conversational sample with the child in a clinical or school-based setting. Thus, a clinician could make a relatively informed decision - from their assessment in a clinical or school-based setting – about the diagnosis of stuttering in settings different from theirs or with other conversational partners.
One caveat to the above relates to differences in SLD/TD ratio, for CWS, in conversational versus narrative samples. To the extent that the SLS/TD ratio is used by clinicians to help classify a child as CWS and CWNS, then the nature of sample employed to make that decision, based on present findings, needs careful consideration. For CWS, based on present findings, this ratio appears higher during conversation than narration. It is unclear whether this reflects the fact that different speech-language processes, those for conversation versus those for narration, influence childhood stuttering differently. These and related issues have been previously explored (e.g., Ingham & Riley, 1998; Johnson, 1961; Sawyer & Yairi, 2006); indeed, present findings, although involving preschool-age children, are consistent with Yaruss (1997) who studied school-age children. Indeed, it would appear that such differences in stuttering related to conversational versus narrative communication deserve further empirical investigation.
Influence of Stuttering Variation on Talker Group Classification
The second main finding indicated that variations in stuttering, for both talker groups as a whole, had no significant influence on the diagnosis of CWS versus CWNS. From a clinical perspective, this finding suggests that for most children, despite known variability in stuttering, reasonably accurate talker group classification can be made regardless of the conversational partner, location or context. Again, as stated above, present data suggest that a diagnosis of stuttering or nonstuttering based on a typical clinical sample involving a clinician – child conversation would be similar to a diagnosis based on data from a more naturalistic environment for example, in the home conversing with a parent. Specifically, of the present sample, 92% (at home) and 88% (in clinic) of children were correctly classified despite different partners (mother versus clinician), 92% (with clinician) and 88% (with parent) despite different locations (home versus clinic), and 89% despite different contexts (conversation versus narrative). Thus, although variation in stuttering occurred between partners, location and contexts as other studies have shown (e.g., Yaruss, 1997), these differences were not sufficient to change talker group assignment for the vast majority of preschool-age children in the present study.
Influence of Stuttering Variation on Talker Group Classification in Borderline Sample
The third main finding, based on descriptive analyses with the borderline sample (n = 9), indicated that changes in conversation partner and location had minimal influence on talker group classification with 77.8 – 87.5% of borderline participants consistently classified. However, talker group classification based on context (i.e., narrative vs. conversation) appeared to be less consistent with 67.7% of borderline participants consistently classified. As alluded to above, this latter finding is consistent with other studies (e.g., Yaruss, 1997) who report changes in stuttering across various communicative contexts. In other words, at least for borderline children, these changes in stuttering due to changes in context appear to have potential for influencing talker group classification and need to be carefully considered. One good thing to note for clinicians, however, is that it should be possible to use conversational and narrative samples during a routine clinical assessment, even if not possible to assess the child in both the home and clinic.
Although these findings should be cautiously interpreted due to the small sample of borderline participants used, preliminarily, findings appear to suggest that a conversational sample a more stable determinant of talker group classification than a narrative sample. But this speculation awaits further empirical exploration. Perhaps, present findings that speech disfluencies elicited from a conversational sample with the clinician in a clinical setting consistently predicts what one would see in conversational sample in the home would seem to provide some support for at least an initial diagnosis.
Caveat and Conclusions
Sample size
The participant sample size is relatively small for both talker groups (CWS: n = 17 and CWNS: n=9). Even though some of the contexts (e.g., narratives) and location (e.g., home) used in the present study do not appear to have been widely used in other studies, findings from other studies examining variations in stuttering involved larger sample sizes (n = 45; Yaruss, 1997). Therefore, the reader should be cautioned that the present results are preliminary and should be conservatively interpreted as such. Replication of the present findings using a larger sample size would allow for a more confident generalization to the overall population of preschool CWS.
Lack of counterbalancing
One methodological weakness of the study was that the order of the location (home versus clinic) was not counterbalanced. All participants participated in the home conversation approximately 2 weeks before the clinic conversation. However, samples were counterbalanced within each location. In other words, samples elicited in the home were counterbalanced separate from samples elicited in a clinical setting which were also counterbalanced. It is unclear whether this issue resulted in an order effect and whether that order effect might have meaningfully affected the accuracy and reliability of the observed diagnoses, a potential limitation to present findings. Future studies should attempt to counterbalance all aspects under investigation in order to rule out any possible order effects, no matter how unlikely.
Talker Group Classification
For the present study, talker group classification for CWS and CWNS was based on a typical 300-word conversational sample between the child and a clinician in a clinical setting as well as scores on the Stuttering Severity Instrument-3 (SSI-3; Riley, 1994). Although judgment of speech disfluencies, as used in this study, were based on listener perceptions, no other perceptual measure or rating system was included (for a review of perceptual rating instruments, see Franken, Boves, Peters & Webster, 1995). The criteria used in the present study, however, has been used in other studies (e.g., (Arnold, Conture, & Ohde, 2005; Hartfield & Conture, 2006; Karrass et al., 2006; Pellowski, & Conture, 2002) as one seemingly valid and reliable means to classify participants as either CWS or CWNS.
Conclusions
Variations in stuttering frequency in children are and will continue to be studied because such variations have important clinical as well as research implications. This is especially true when the diagnosis of childhood stuttering is based on stuttering frequency or when stuttering frequency is an important dependent variable in a research study. While there can be no question that such variation exists (e.g., Ingham & Riley, 1998; Johnson, 1961; Sawyer & Yairi, 2006; Yaruss, 1997), there also can be no question that we presently lack a full understanding of the implications this has for clinical as well as research endeavors. Thus, in the present study we attempt to empirically asses whether this variation is significant enough to influence or change talker group classification for young CWS and CWNS.
Present findings suggest that these variations are, on the whole, not sufficiently robust to significantly influence talker group classification (i.e., CWS vs. CWNS). In other words, despite the presence of stuttering variation, present results appear to support the notion that the diagnosis of CWS or CWNS would not significantly change as a result to the changes in conversational partner, context or location. Thus, a clinician could, with some degree of confidence, predict whether a diagnosis of stutterer or nonstutterer based on a typical clinician-child conversation in a clinical setting would hold true in other environments.
However, as findings also suggest changes in these variables (i.e., conversational partner, context, or location) would have their greatest impact on children on or around the borderline between classifying stutterer or nonstutterer. Maybe variation in stuttering could push such “borderline” children into or out of a stuttering diagnosis based on simple environmental or contextual changes. However, current findings suggest that even for the majority of these borderline children, changes to conversational partner and location would not significantly impact or change talker group classification. Talker group predictability, however, based on changes in context (i.e., conversational sample vs. narrative sample) was less reliable, certainly resulting in part from the small sample size.
Although a naturalistic environment (i.e., in the home with the parent) is considered the most ideal setting to evaluate stuttering in a young child (Martin et al., 1972), often times the diagnosis of stutterer or non-stutterer is made perforce using a clinician – child conversational sample collected in a clinical setting. The findings from the present study, although preliminary and awaiting further empirical assessment, provide a basis for comparison and suggest a need to continue investigating this empirical question. As with any empirical study, ours warrants replication with different participants, larger sample sizes and possibly different controls. However, there would seem to be reason to believe, based on present findings, that the diagnosis of CWS versus CWNS would not appreciably differ – despite variations in stuttering frequency between conversational partner and location - at least for children not on the diagnostic borderline between CWS and CWNS.
Acknowledgments
Author Note The authors would like to sincerely thank the following for aiding with the data collection process: Drs. Hayley S. Arnold and Corrin Richels, as well as Geoff Coalson, Katerina Ntouro and Krista Schwenk. Last, but not least, the authors extend their appreciation to the many children and their families who participated in this study.
This research was funded in part by grants from NIH/NICHD (5T32HD007226-29), NIH/NIDCD (3R01DC000523-13; 1R01EC006477-01A2) and a Discovery Grant from Vanderbilt University to the second and fourth authors.
Footnotes
Although very little is known about the variability of stuttering during a narrative task, there is a fair amount of research investigating the linguistic composition and language abilities of children who stutter during narrative story-telling speech (for a review of this literature, see Scott, Healey & Norris, 1995; Nippold, 1991; Trautman et al., 1999; Weiss & Zebrowski, 1994).
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Ambrose N, Yairi E. Normative disfluency data for early childhood stuttering. Journal of Speech, Language, and Hearing Research. 1999;42(4):895–909. doi: 10.1044/jslhr.4204.895. [DOI] [PubMed] [Google Scholar]
- American Speech-Language-Hearing Association Guidelines for screening for hearing impairment and middle-ear disorders. ASHA. 1990;32(Suppl 2):17–24. [PubMed] [Google Scholar]
- Anderson J. Phonological neighborhood and word frequency effects in the stuttered disfluencies of children who stutter. Journal of Speech, Language, and Hearing Research. 2007;50:229–247. doi: 10.1044/1092-4388(2007/018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson J, Pellowski M, Conture E, Kelly E. Temperamental characteristics of children who stutter. Journal of Speech, Language, and Hearing Research. 2003;46:1221–1233. doi: 10.1044/1092-4388(2003/095). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson J, Wagovich S, Hall N. Nonword repetition skills in young children who do and do not stutter. Journal of Fluency Disorders. 2006;31:177–199. doi: 10.1016/j.jfludis.2006.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnold H, Conture E, Ohde R. Phonological neighborhood density in the picture naming of young children who stutter: Preliminary study. Journal of Fluency Disorders. 2005;30(2):125–148. doi: 10.1016/j.jfludis.2005.01.001. [DOI] [PubMed] [Google Scholar]
- Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. Journal of the Royal Statistical Society. Series B (Methodological) 1995;57:289–300. [Google Scholar]
- Bloodstein O. A handbook on stuttering. 5th ed Singular; San Diego, CA: 1995. [Google Scholar]
- Byrd C, Conture E, Ohde R. Phonological priming of young children who stutter: Holistic versus Incremental. American Journal of Speech Language Pathology. 2007;16:43–53. doi: 10.1044/1058-0360(2007/006). [DOI] [PubMed] [Google Scholar]
- Cohen J. A coefficient of agreement for nominal scales. Educational and Psychological Measurement. 1960;20:37–46. [Google Scholar]
- Conture E. Stuttering: Its nature, diagnosis, and treatment. [3rd ] ed Allyn and Bacon; Boston: 2001. [Google Scholar]
- Conture E. Stuttering: Its Nature, Diagnosis and Treatment. Allyn & Bacon; Needham Heights, MA: 2001. [Google Scholar]
- Cordes A, Ingham R. The reliability of observational data: II. Issues in the identification and measurement of stuttering events. Journal of Speech and Hearing Research. 1994;37(2):279–294. [PubMed] [Google Scholar]
- Curlee R. Stuttering and related disorders of fluency. 3rd ed Thieme; New York: 2007. [Google Scholar]
- Dunn L, Dunn L. Peabody Picture Vocabulary Test. 3rd ed American Guidance Service; Circle Pines, MN: 1997. [Google Scholar]
- Franken M, Boves L, Peters H, Webster R. Perceptual evaluation of the speech before and after fluency shaping therapy. Journal of Fluency Disorders. 1992;17:223–242. [Google Scholar]
- Goldman R, Fristoe M. Goldman--Fristoe Test of Articulation--2. American Guidance Service; Circle Pines, MN: 2000. [Google Scholar]
- Guitar B. Stuttering: An integrated approach to its nature and treatment. Lippincott Williams & Wilkins; Baltimore, MD: 1998. [Google Scholar]
- Hall K, Amir O, Yairi E. A longitudinal investigation of speaking rate children who stutter. Journal of Speech, Language, and Hearing Research. 1999;42:1367–1377. doi: 10.1044/jslhr.4206.1367. [DOI] [PubMed] [Google Scholar]
- Hartfield K, Conture E. Effects of perceptual and conceptual similarity in lexical priming of young children who stutter: preliminary findings. Journal of Fluency Disorders. 2006;31:303–324. doi: 10.1016/j.jfludis.2006.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hochberg Y. A sharper Bonferroni procedure for multiple tests of significance. Biometrika. 1988;75:800–803. [Google Scholar]
- Hollingshead A. Four factor index of social position. Yale University; 1975. Unpublished manuscript. [Google Scholar]
- Hresko W, Reid D, Hamill D. Test of Early Language Development-3. PRO-ED; Austin, TX: 1999. [Google Scholar]
- Ingham J, Riley G. Guidelines for documentation of treatment efficacy for young children who stutter. Journal of Speech, Language, and Hearing Research. 1998;41(4):753–770. doi: 10.1044/jslhr.4104.753. [DOI] [PubMed] [Google Scholar]
- Johnson W. Measurements of oral reading and speaking rate and disfluency of adult male and female stutterers and nonstutterers. Journal of Speech and Hearing Disorders. Monograph Supplement. 1961;7:1–20. [PubMed] [Google Scholar]
- Karrass J, Walden T, Conture E, Graham C, Arnold H, Hartfield K, Schwenk K. Relation of emotional activity and regulation to childhood stuttering. Journal of Communication Disorders. 2006;39(6):402–423. doi: 10.1016/j.jcomdis.2005.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keselman H, Cribbie R, Holland B. The pairwise multiple comparison multiplicity problem: An alternative approach to familywise and comparison wise Type I error control. Psychological Methods. 1999;4(1):58–69. [Google Scholar]
- Martin R, Haroldson S, Kuhl P. Disfluencies in child-child and child-mother speaking situations. Journal of Speech and Hearing Research. 1972;15(4):753–756. doi: 10.1044/jshr.1504.753. [DOI] [PubMed] [Google Scholar]
- Martin R, Kuhl P, Haroldson S. An experimental treatment with two preschool stuttering children. Journal of Speech, Language, and Hearing Research. 1972;15:743–752. doi: 10.1044/jshr.1504.743. [DOI] [PubMed] [Google Scholar]
- Mayer M. A boy, a dog, and a frog. Dial Books for Young Readers; New York: 1967. [Google Scholar]
- Mayer M. Frog, where are you? Dial Books for Young Readers; New York: 1969. [Google Scholar]
- Mayer M. Frog on his own. Dial Books for Young Readers; New York: 1973. [Google Scholar]
- Meyers S. Qualitative and quantitative differences and patterns of variability in disfluencies emitted by preschool stutterers and nonstutterers during dyadic conversations. Journal of Fluency Disorders. 1986;11:293–306. [Google Scholar]
- Nippold MA. Evaluating and enhancing idiom comprehension in language-disordered students. Language, Speech, and Hearing Services in Schools. 1991;22:100–106. [Google Scholar]
- Onslow M, Costa L, Rue S. Direct early intervention with stuttering: Some preliminary data. Journal of Speech and Hearing Disorders. 1990;55(3):405–416. doi: 10.1044/jshd.5503.405. [DOI] [PubMed] [Google Scholar]
- Pellowski MW, Conture EG. Characteristics of speech disfluency and stuttering behaviors in 3- and 4-year-old children. Journal of Speech, Language, and Hearing Research. 2002;45(1):20–34. doi: 10.1044/1092-4388(2002/002). [DOI] [PubMed] [Google Scholar]
- Riley GD. Stuttering Severity Instrument for Children and Adults. 3rd ed. PRO-ED; Austin TX: 1994. [DOI] [PubMed] [Google Scholar]
- Sawyer J, Yairi E. The effect of sample size on the assessment of stuttering severity. American Journal of Speech Language Pathology. 2006;15(1):36–44. doi: 10.1044/1058-0360(2006/005). [DOI] [PubMed] [Google Scholar]
- Silverman E, Silverman M. Situational variability of preschoolers’ disfluency: Preliminary study. Perceptual and Motor Skills. 1971;33:1021–22. doi: 10.2466/pms.1971.33.3.1021. [DOI] [PubMed] [Google Scholar]
- Scott LA, Healey EC, Norris JA. A comparison between children who stutter and their normally-fluent peers on a story retelling task. Journal of Fluency Disorders. 1995;20:279–292. [Google Scholar]; Silverman EM. Situational variability of preschoolers’ disfluency: Preliminary study. Perceptual and Motor Skills. 1971;33(3 Pt 1):1021–1022. doi: 10.2466/pms.1971.33.3.1021. [DOI] [PubMed] [Google Scholar]
- Schwenk KA, Conture EG, Walden TA. Reaction of background stimulation of preschool children who do and do not stutter. Journal of Communication Disorders. 2007;40(2):129–141. doi: 10.1016/j.jcomdis.2006.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trautman LS, Healey EC, Brown TA, Brown P, Jermano S. A further analysis of narrative skills of children who stutter. Journal of Communication Disorders. 1999;32:297–315. doi: 10.1016/s0021-9924(99)00005-2. [DOI] [PubMed] [Google Scholar]
- Weiss AL, Zebrowski PM. The narrative productions of children who stutter: A preliminary view. Journal of Fluency Disorders. 1994;19:39–63. [Google Scholar]
- Williams K. Expressive Vocabulary Test. American Guidance Service; Circle Pines, MN: 1997. [Google Scholar]
- Yairi E. Speech characteristics of early childhood stuttering. In: Curlee R, Siegel G, editors. Speech characteristics of early childhood stuttering. Allyn and Bacon; Needham Heights, MA: 1997. [Google Scholar]
- Yairi E, Ambrose N. A longitudinal study of stuttering in children: A preliminary report. Journal of Speech and Hearing Research. 1992;36:771–778. doi: 10.1044/jshr.3504.755. [DOI] [PubMed] [Google Scholar]
- Yairi E, Ambrose N. Early Childhood Stuttering: For clinicians by clinicians. Pro-Ed; Austin, TX: 2005. [Google Scholar]
- Yaruss JS. Clinical implications of situational variability in preschool children who stutter. Journal of Fluency Disorders. 1997;22(3):187–203. [Google Scholar]
- Yaruss JS. Real-time analysis of speech fluency: Procedures and reliability training. American Journal of Speech-Language Pathology. 1998;7:25–37. [Google Scholar]