Abstract
Background:
Oestrogen receptor-alpha (ERα) is highly expressed in diffuse-type gastric cancer and oestrogen increases the proliferation of ERα-positive gastric cancer. However, a detailed mechanism by which oestrogen increases the proliferation of these cells is still unclear.
Methods:
We used 17-β-oestradiol (E2) as a stimulator against the ERα pathway. Pure anti-oestrogen drug ICI 182 780 (ICI) and small interfering RNA against ERα (ERα siRNA) were used as inhibitors. Cyclopamine (Cyc) was used as the hedgehog (Hh) pathway inhibitor. Two human ERα-positive gastric cancer cells were used as target cells. Effects of the stimulator and inhibitor on E2-induced cell proliferation were also examined.
Results:
In ERα-positive cells, E2 increased not only cell proliferation but also one of the ligands of the Hh pathway, Shh expression. 17-β-Oestradiol-induced cell proliferation was suppressed by ICI, ERα siRNA or Cyc. The increased expression of Shh induced by E2 was suppressed by ICI and ERα siRNA but not by Cyc. Furthermore, recombinant Shh activated the Hh pathway and increased cell proliferation, whereas anti-Shh antibody suppressed E2-induced cell proliferation. When a relationship between ERα and Shh expressions was analysed using surgically resected gastric cancer specimens, a positive correlation was found, suggesting a linkage between the ERα and Hh pathways.
Conclusion:
Our data indicate that activation of the ERα pathway promotes cell proliferation by activating the Hh pathway in a ligand-dependent manner through Shh induction of ERα-positive gastric cancer.
Keywords: gastric cancer, hedgehog signalling pathway, Sonic hedgehog, oestrogen receptor-α, proliferation
Gastric cancer is one of the most lethal of all malignancies (Parkin, 2001). In particular, patients with unresectable, metastatic or recurrent gastric cancer have only few therapeutic options. Thus, it is urgent to develop novel therapeutics for gastric cancer.
Gastric cancers are classified into two major histological types using the criteria of Lauren, namely intestinal type and diffuse type (Lauren, 1965). The carcinogenic pathway of intestinal-type gastric cancer develops through several sequential stages with Helicobacter pylori infection, followed by chronic gastritis, atrophic gastritis and intestinal metaplasia (Yuasa, 2003), whereas the diffuse type is believed to be derived from hyperplastic stem or precursor cells (Ming, 1998). It is considered that diffuse-type gastric cancer has a higher malignant potential such as invasion and metastasis, compared with intestinal-type gastric cancer.
Oestrogen has various physiological functions, such as normal cell growth and differentiation in many target tissues. Oestrogen is produced not only from the ovary but also from extra-ovarian tissues, that is, from the skin, brain, testis, adipose tissues and vascular smooth muscle (Ackerman et al, 1981; Leshin et al, 1981; Brodie and Inkster, 1993; Lephart, 1996; Ueyama et al, 2002). The biological actions of oestrogen are mediated through two specific receptors (oestrogen receptor, ERs), ERα and ERβ, which belong to the nuclear receptor superfamily. Oestrogen-bound ERs bind as homodimers or heterodimers to a specific DNA sequence known as the oestrogen-responsive element (ERE), and regulate the transcription of target genes (Matthews and Gustafsson, 2003). As oestrogen is a stimulant for the initiation and promotion of breast cancer, and ERα can be expressed in gastric cancer cells, it has been suggested that the ERα pathway may have a role in the progression of gastric cancer (Harrison et al, 1989b; Wu et al, 1994; Karat et al, 1999; Takano et al, 2002; Chandanos et al, 2008). In gastric cancer, ERα expression is higher in the diffuse type than in the intestinal type (Kitaoka, 1983; Tokunaga et al, 1986; Matsui et al, 1992; Zhao et al, 2003), and oestradiol (E2) enhances gastric cancer cell proliferation in vitro (Matsui et al, 1992; Takano et al, 2002). On the basis of these observations, several clinical trials using a partial oestrogen antagonist, tamoxifen (TAM), have been conducted for the management of ERα-positive gastric cancer patients. However, the results have not been consistent and the utility of ERα for the treatment of gastric cancer is still controversial (Harrison et al, 1989a, 1989b; Koullias et al, 2003).
The hedgehog (Hh) signalling pathway has a crucial role in embryonic development, tissue regeneration and carcinogenesis. Of the three Hh ligands, namely Sonic Hh (Shh), Indian Hh (Ihh) and Desert Hh (Dhh) (Pasca di Magliano and Hebrok, 2003; Lum and Beachy, 2004; Briscoe and Therond, 2005; Hooper and Scott, 2005; Katoh and Katoh, 2005), Shh is exclusively expressed in the acid-producing parietal cells in both human and murine stomach, and is believed to be a regulator of gastric fundic gland differentiation and mutation (Ramalho-Santos et al, 2000; van den Brink et al, 2001, 2002; Dimmler et al, 2003). Pharmacological inhibition of Shh signalling in the adult stomach causes loss of parietal cells (gastric atrophy) and subsequent disruption of glandular differentiation (van den Brink et al, 2002). Furthermore, Shh is strongly implicated in maintaining stem cell niches in the adult stomach (Katoh and Katoh, 2006). Recently, ligand-dependent activation of the Hh pathway, especially due to an aberrant expression of Shh, has been detected in various cancers including gastric cancer (Berman et al, 2003; Watkins et al, 2003; Karhadkar et al, 2004; Sanchez et al, 2004; Sheng et al, 2004). Overexpression of Shh leads to carcinogenesis through the aberrant activation of the Hh pathway (Berman et al, 2003; Thayer et al, 2003; Cengel, 2004; Sanchez et al, 2004). It is also believed that Shh has an important role during the progression of gastric cancer, because Shh expression is much higher in the diffuse type than in the intestinal type in human gastric cancer (Ma et al, 2005, 2006).
It is noteworthy that our previous study demonstrated a positive correlation between Hh pathway activation and ERα status (Kubo et al, 2004), and suggested that ERα could regulate Hh pathway activation in ERα-positive breast cancer (Koga et al, 2008). It has also been shown that the Hh pathway can be a useful therapeutic target against breast cancer and gastric cancer (Kubo et al, 2004; Yanai et al, 2007). From these results, we hypothesised that stimulation of the ERα pathway induces Shh expression, activates the Hh pathway and consequently promotes cell proliferation in ERα-positive gastric cancer cells. The ERα pathway could be a possible therapeutic target for patients with ERα-positive gastric cancer.
Materials and methods
Cell culture, reagents and antibodies
We prepared eight gastric cancer cell lines, KATOIII, NCI-N87, MK-1, AGS, MKN45, Hs746T, SNU-16 and MKN74. These were maintained at 37°C under a humidified atmosphere of 5% CO2 and 95% air in RPMI1640 medium (Life Technologies, Grand Island, NY, USA) supplemented with 10% fetal bovine serum (FBS; Life Technologies) and antibiotics (100 Units ml−1 penicillin and 100 μg ml−1 streptomycin; Meijiseika, Tokyo, Japan). Cells were incubated for 24 h in phenol-red-free minimum essential medium (MEM; Invitrogen, Carlsbad, CA, USA) without FBS before all experiments (termed oestrogen starvation). Thereafter, cells were principally cultured in MEM supplemented with 5% dextran-coated charcoal-treated FBS (DCC-FBS-MEM) in a humidified 95% air and 5% CO2 atmosphere. 17-β-Oestradiol was purchased from Sigma (Deisenhofen, Germany). The ER pathway antagonist, ICI 182 780 (ICI), was purchased from Tocris Cookson Ltd. (Ellisville, MO, USA). Cyclopamine (Cyc) was purchased from Toronto Research Chemicals (North York, ON, Canada). Both ICI and Cyc were diluted in 99.5% ethanol as a stock solution, and stored at −30°C. Recombinant human Shh N-terminal peptide (rhShh) was purchased from R&D Systems (Minneapolis, MN, USA). Rat anti-Shh NH2-terminal peptide antibody (αShh-Ab) was purchased from R&D Systems.
Expression vectors
cDNAs encoding human ERα were cloned into the pSG5 expression vector as described previously (Green et al, 1988; Kato et al, 2002). This cDNA and ERE-tk-luc, a single consensus ERE upstream of luciferase, were kindly provided by Dr Norio Wake (Kyushu University, Fukuoka, Japan). pRL-SV40 was purchased from Promega (Madison, WI, USA).
Reverse transcription–PCR
Total RNA was extracted from cultured cells by the guanidinium thiocyanate–phenol–chloroform single-step method. For the reverse transcription (RT) reaction, pd(N)6 Random Hexamer (GE Healthcare UK Ltd, Buckinghamshire, England) was used for priming. The ERα forward (5′-CAG GGG TGA GTG GGG TC-3′) and reverse (5′-ATG CGG AAC CGA GAT GAT-3′) primers yielded a 483-bp product. Gli1 forward (5′-TCT GCC CCC ATT GCC CAC TTG-3′) and reverse (5′-TAC ATA GCC CCC AGC TAC CTC-3′) primers yielded a 480-bp product. The Shh forward (5′-CGC ACG GGG ACA GCT CGG AAG T-3′) and reverse (5′-CTG CGC GGC CCT CGT AGT GC-3′) primers yielded a 477-bp product. The Ptch1 forward (5′-CGG CGT TCT CAA TGG GCT GGT TTT-3′) and reverse (5′-GTG GGG CTG CTG TCT CGG GTT CG-3′) primers yielded a 376-bp product. Glyceraldehyde-3-phosphate dehydrogenase (GAPDH) forward (5′-CCA CCC ATG GCA AAT TCC ATG GCA-3′) and reverse (5′-TCT AGA CGG CAG GTC AGG TCC ACC-3′) primers yielded a 593-bp product. The amplification conditions comprised an initial denaturation for 2 min at 95°C, followed by 35 cycles of 94°C for 30 s, 58°C for 30 s and 72°C for 1 min. The amplification of each gene was in the linear range. The RT–PCR products were separated on ethidium bromide-stained 2% agarose gels. Semi-quantitative analysis was carried out with a Molecular Imager FX Pro (Bio-Rad Laboratories, Hercules, CA, USA).
Real-time RT–PCR
Total RNA was extracted using the RNeasy mini kit (Qiagen, Valencia, CA, USA) and quantified by spectrophotometry (Ultrospec 2100 Pro; Amersham Pharmacia Biotech, Cambridge, UK). RNA (700 ng) was treated with DNase, and reverse transcribed to cDNA using the Quantitect Reverse Transcription Kit (Qiagen) according to the manufacturer's protocol. Reactions were run with SYBR Premix Ex Taq (Takara Bio Inc., Otsu, Japan) on a DNA Engine Opticon 2 System (MJ Research, Waltham, MA, USA). pShh-GFP or pGli1 was serially diluted in 10-fold increments and amplified with the primer pairs to generate a standard curve for Shh or Gli1. Standard curves for β-actin were generated using cDNA from MK-1 cells treated with E2 for 8 h. Each sample was run in triplicate. All primer sets amplified fragments <200 bp long. The sequences of the primers used were as follows: β-actin, forward, 5′-TTG CCG ACA GGA TGC AGA AGG A-3′, reverse, 5′-AGG TGG ACA GCG AGG CCA GGA T-3′ ERα, forward, 5′-GGA GGG CAG GGG TGA A-3′, reverse, 5′-GGC CAG GCT GTT CTT CTT AG-3′ pS2, forward, 5′-CAT GGA CGT CCC TCC AGA AGA G-3′, reverse, 5′-CTC TGG GAC TAA TCA CCG TGC TG-3′ Shh, forward, 5′-GTG TAC TAC GAG TCC AAG GCA C-3′, reverse, 5′-AGG AAG TCG CTG TAG AGC AGC-3′ and Gli1, forward, 5′-GGT TCA AGA GCC TGG GCT GTG T-3′, reverse, 5′-GGC AGC ATT CTC AGT GAT GCT G-3′. The amount of each target gene in a given sample was normalised to the level of β-actin in that sample.
Immunoblotting
Whole-cell extraction was performed with M-PER Reagents (Pierce Biotechnology, Rockford, IL, USA) according to the manufacturer's instructions. Protein concentration was determined using the Bio-Rad Protein Assay (Bio-Rad Laboratories), and whole-cell extract (80 μg) was separated by electrophoresis on a SDS-polyacrylamide gel, and transferred to Protran nitrocellulose membranes (Whatman, Dassel, Germany). Blots were then incubated overnight with GAPDH (1 : 1000), ERα (1 : 200) or Shh (1 : 200) primary antibody at 4°C. Blots were then incubated in HRP-linked secondary antibody (Amersham Biosciences, Piscataway, NJ, USA) at room temperature for 1 h. Immunocomplexes were detected using ECL together with the western blotting detection system (Amersham Biosciences) and visualised using a Molecular Imager FX (Bio-Rad Laboratories). Glyceraldehyde-3-phosphate dehydrogenase was used as a protein loading control.
Dual luciferase assay
KATOIII and NCI-N87 cells in 24-well plates were transfected with plasmids with TransFast transfection reagent according to the manufacturer's instructions. Cells on each well were co-transfected with 10 ng of pRL-SV40 (Promega) and 1 μg ERE-tk-Luc. After oestrogen starvation, E2 and ICI or Cyc were added to each well for 8 h, and luciferase assays were performed using the dual luciferase assay kit (Promega) according to the manufacturer's instructions. The luciferase activities were normalised to Renilla luciferase activity.
Small interfering RNA against ERα
KATOIII and NCI-N87 cells (1.0 × 106 cells) were transfected with small interfering RNA (siRNA) (100 nM) against ERα by lipofectamine as per the manufacturer’s instructions, and then plated in a 25-cm2 flask for 24 h in 10% FBS-RPMI. After oestrogen starvation, the cells were treated with E2 for 16 h, and then used for real-time RT–PCR. The following siRNAs were used: Validated Stealth RNAi against ERα and the Stealth RNAi-negative control (Invitrogen).
Proliferation assay
KATOIII (5 × 103 per well), NCI-N87 (1 × 104 per well) and MK-1 (5 × 103 per well) cells were seeded in 48-well plates in complete culture medium and were incubated overnight. After oestrogen starvation, the medium was changed to 5% DCC-FBS-MEM containing various concentrations of reagents. After 72 h of incubation, cells were harvested by trypsinisation, and viable cells were counted using a Coulter counter (Beckman Coulter, Fullerton, CA, USA).
Clinical samples
Surgical specimens were obtained from 20 patients with diffuse-type gastric cancer and from 20 patients with intestinal type. All of the patients underwent resection at the Department of Surgery and Oncology, Kyushu University (Fukuoka, Japan), between 1996 and 2004. All 40 patients gave informed consent before surgical treatment and were enrolled into this study. All surgical specimens were frozen at −80°C, examined histopathologically and classified using the tumour-node-metastasis classification. Total mRNA of these specimens was extracted using the RNeasy mini kit (Qiagen) as per the manufacturer’s recommendation.
Immunohistochemistry
Single-antibody detection was carried out as described previously (Kubo et al, 2004), with the following protocol modifications: Endogenous peroxidase activity was blocked using 3% H2O2 in methanol for 30 min at room temperature. Antigen retrieval was achieved by boiling tissue in 0.01 mol l−1 sodium citrate (pH 6.0) for 5 min. All primary antibodies were incubated overnight at 4°C. The primary antibodies used were Shh (1 : 50 H-160, sc-9024,) and ERα (1 : 50 F-10, sc-8002) (Santa Cruz Biotechnology, Santa Cruz, CA, USA). Secondary antibodies (Shh rabbit anti-IgG; ERα, mouse anti-IgG; Nichirei Co., Ltd, Tokyo, Japan) were applied for 1 h at room temperature. Protein was detected by brown pigmentation using the standard 3, 3′-diaminobenzidine (DAB) protocol. Slides were lightly counterstained with haematoxylin. Negative controls were obtained in all cases by omitting the first antibodies. All primary antibodies had been previously tested for immunohistostaining.
Statistical analysis
Student's t-test was used for statistical analysis, unless indicated otherwise. The correlation of clinicopathological features between the ERα and Shh expression was analysed by the Mann–Whitney U-test. All calculations were carried out using the StatView 5.0 J software (Abacus Concepts, Berkeley, CA, USA). Single asterisk denotes P<0.05; P-values <0.05 were considered significant.
Results
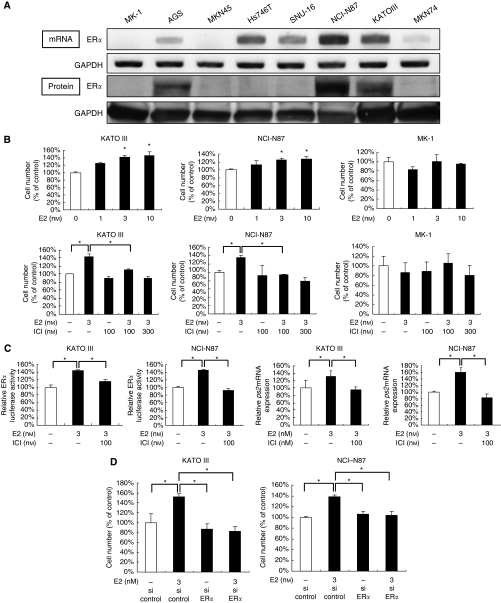
Oestrogen activates the ERα pathway and induces increased proliferation
We examined ERα expression in eight human gastric cancer cell lines. Five cell lines showed ERα expression at the mRNA level (Figure 1A), and three of the five cell lines, namely KATOIII, NCI-N87 and AGS cells, also showed detectable ERα expression at the protein level (Figure 1A). Thus, we selected KATOIII (diffuse type) and NCI-N87 (intestinal type) cells as ERα-positive cells, and selected MK-1 cells (diffuse type) as ERα-negative cells. We then examined whether the ERα pathway has a role in the proliferation of ERα-positive cells. As we expected, E2 increased the proliferation of ERα-positive but not negative cells in a dose-dependent manner (Figure 1B). This E2-induced cell proliferation was completely inhibited by ICI 182 780 (100 nM). ICI did not affect cell proliferation without supplementation of E2 (Figure 1B). On the basis of these preliminary data, E2 and ICI were used at a concentration of 3 and 100 nM, respectively, throughout the study. We further examined whether the ERα pathway is functional in these ERα-positive cells. Activation of the ERα pathway by E2 was determined with an ERα reporter assay and pS2 expression, a target gene of the ERα pathway (Campbell-Thompson, 1997; Singh et al, 1997). We found that E2 increased both ERα-responsive reporter activity (Figure 1C) and pS2 mRNA expression (Figure 1C) in these ERα-positive cells. This increased activation of the ERα pathway by E2 was almost completely inhibited by ICI. Finally, to confirm the contribution of the ERα pathway to E2-induced proliferation of ERα-positive cells, we silenced ERα mRNA expression of ERα-positive cells by RNA interference. Transfection of siRNA resulted in an 85% or greater knockdown of ERα mRNA expression (data not shown). Silencing of ERα did not affect cell proliferation without supplementation of E2. However, E2-induced cell proliferation was inhibited by ERα-siRNA (Figure 1D). These data indicate that E2 increases proliferation of ERα-positive gastric cancer cells through activation of the ERα pathway.
Figure 1.
E2 activates the ERα pathway and induces increased proliferation in ERα-positive gastric cancer cells. (A) Both mRNA (upper panel) and protein (lower panel) expression of ERα were increased in KATOIII and NCI-N87, as shown by RT–PCR and western blotting. GAPDH was used as a loading control. (B) Cell proliferation in the presence of E2 alone (upper panel) or in combination with ICI (lower panel) in KATOIII, NCI-N87 and MK-1 cells. Cells were cultured in 5% DCC-FBS-MEM (DCC-FBS) for 72 h. (C) A dual luciferase assay was performed 8 h after treatment with the indicated reagents (left two panels). Relative pS2 mRNA expression in KATOIII and NCI-N87 was examined by real-time RT–PCR (right two panels). (D) Cell proliferation in KATOIII and NCI-N87 cells transfected with ERα-siRNAs or control siRNA. After transfection with ERα siRNA or control siRNA, KATOIII and NCI-N87 cells were treated with or without E2 for 72 h. Results are expressed as mean±s.d. *P<0.05.
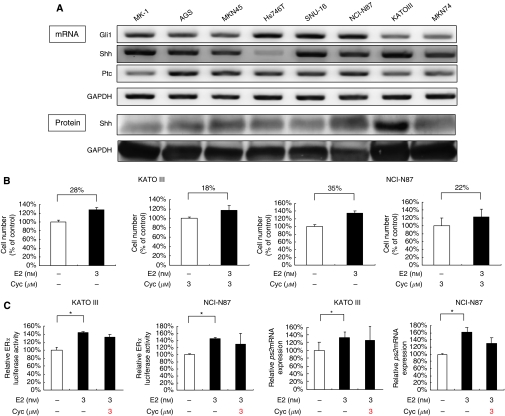
Oestrogen-induced cell proliferation is suppressed by inhibition of the Hh pathway
As our previous study indicated a crosstalk between the ERα and Hh pathways in ERα-positive breast cancer cells (Koga et al, 2008), we examined the expression of Hh-related molecules, including Shh, Ptched 1 (Ptc) and Gli1, in ERα-positive gastric cancer cells. Consistent with our previous report (Yanai et al, 2007), we found that these cells expressed Hh-related molecules at the mRNA level (Figure 2A). Gli1 expression indicates a constitutive activation of the Hh pathway in gastric cancer cells, because Gli1 is a target gene of the Hh pathway (Kubo et al, 2004). In our previous report, cyclopamine suppressed the proliferation of these cells (Yanai et al, 2007). To estimate a contribution of the Hh pathway to E2-induced increase in proliferation, we compared the increasing rate of proliferation induced by E2 between the presence and absence of Hh pathway activity (Figure 2B). In Kato III, the increasing rate was 28 and 18% in the presence and absence of Hh pathway activity, respectively. In NCI-N87, it was 35 and 22%, respectively. These data indicate that a block of the Hh pathway reduces the degree of E2-induced increase of proliferation. To determine the relationship between these two pathways, we examined how cyclopamine affects ERα pathway activation induced by E2. We found that cyclopamine did not affect E2-induced activation of the ERα pathway (Figure 2C). These data suggest that the Hh pathway contributes to E2-induced cell proliferation of ERα-positive gastric cancer cells.
Figure 2.
E2-induced cell proliferation is suppressed by inhibition of the Hh pathway in ERα-positive gastric cancer cells. (A) Both mRNA (upper panel) and protein (lower panel) expressions of Hh-related molecules were increased in KATOIII, NCI-N87 and MK-1 cells, as shown by RT–PCR and western blotting. GAPDH was used as a loading control. (B) The increasing rate of proliferation induced by E2 in the presence and absence of Hh pathway activity. (C) An ERα dual luciferase assay in KATOIII and NCI-N87 cells was performed 8 h after treatment with indicated reagents (left two panels). Relative pS2 mRNA expression in KATOIII and NCI-N87 cells was examined by real-time RT–PCR (right two panels). Results are expressed as mean±s.d. *P<0.05.
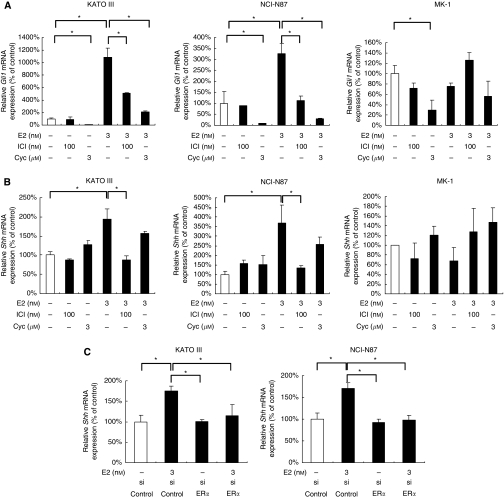
Oestrogen induces the increased Shh expression through activation of the ERα pathway
As contribution of the Hh pathway to E2-induced cell proliferation has been previously suggested, we examined whether E2 could induce Hh pathway activation in ERα-positive cells. Activation of the Hh pathway was determined by Gli1 mRNA expression. We found that E2 markedly increased Gli1 mRNA expression in ERα-positive cells, and that the increased Gli1 mRNA expression was significantly suppressed by ICI. ICI alone did not affect Gli1 mRNA expression without supplementation of E2 (Figure 3A). Cyclopamine suppressed this E2-induced Gli1 mRNA expression more strongly than did ICI. 17-β-Oestradiol-induced Gli1 mRNA expression was not found in ERα-negative cells. We then investigated the molecular mechanisms by which E2 activates the Hh pathway in ERα-positive cells. Ligand-dependent activation of the Hh pathway has been shown in gastric cancer (Berman et al, 2003). Therefore, we focused on an Hh pathway ligand, Shh. As expected, E2 increased Shh mRNA expression of ERα-positive cells, and this E2-induced increase was almost completely inhibited by ICI (Figure 3B). Cyclopamine did not affect E2-induced Shh expression. Neither ICI nor cyclopamine significantly affected Shh expression in ERα-negative cells. Finally, to confirm a contribution of the ERα pathway to E2-induced Shh mRNA expression in ERα-positive cells, we used ERα-silenced ERα-positive cells as target cells. Silencing of ERα alone did not affect Shh expression when there was no supplementation of E2. Importantly, E2-induced Shh expression was almost completely inhibited in ERα-silencing cells (Figure 3C). These data indicate that E2 increases Shh induction of ERα-positive gastric cancer cells through the activation of the ERα pathway.
Figure 3.
E2 upregulates Shh expression through ERα activation in ERα-positive gastric cancer cells. (A) Gli1 mRNA in KATOIII, NCI-N87 and MK-1 cells treated with the indicated reagents for 8 h was examined by real-time RT-PCR. (B) Shh mRNA in KATOIII, NCI-N87 and MK-1 cells treated with the indicated reagents for 8 h was examined by real-time RT-PCR. (C) After transfection with ERα siRNA or control siRNA, KATOIII and NCI-N87 cells were treated with E2 for 8 h and then Shh mRNA was examined by real-time RT–PCR. Results are expressed as mean±s.d. *P<0.05.
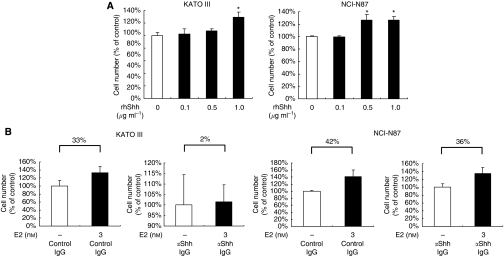
Oestrogen increases cell proliferation through Shh induction, followed by increased Hh pathway activation
We next examined whether Shh induced by E2 could cause the proliferation of ERα-positive cells in a ligand-dependent manner. As mentioned above, the Hh pathway is constitutively activated in these cells. Therefore, we first investigated whether exogenous Shh could further increase the proliferation of these cells. We found that rhShh increased Gli1 mRNA expression (data not shown) and the proliferation of these ERα-positive cells in a dose-dependent manner (Figure 4A). We investigated whether a neutralising antibody against Shh could suppress E2-induced proliferation of ERα-positive cells. Anti-Shh antibody decreased Gli1 mRNA expression (data not shown). Anti-Shh antibody reduced the increasing rate of proliferation induced by E2 (Figure 4B). In KATO III, the increasing rate was 2 and 33% in the presence and absence of the anti-Shh antibody, respectively. In NCI-N87, it was 36 and 42%, respectively. These data indicate that the anti-Shh antibody reduces the degree of E2-induced increase of proliferation, suggesting a contribution of Shh to E2-induced proliferation. Taken together, these results suggest that Shh induced by E2 is functional and increases cell proliferation by activating the Hh pathway in a ligand-dependent manner.
Figure 4.
E2 increases cell proliferation through Shh induction, followed by increased Hh pathway activation. (A) KATOIII and NCI-N87 cells were treated with rhShh at the indicated concentrations for 72 h. rhShh was resolved in PBS containing 0.1% bovine serum albumin (BSA) as per the manufacturer's recommendation. Each control contained the same amount of BSA. Results are expressed as percentage (%) cell number to each control. (B) Cells were treated with anti-Shh antibody (αShh-Ab, 30 μg ml−1) or isotype-matched control IgG (Control IgG, 30 μg ml−1) in the presence of E2 in KATOIII and NCI-N87 cells for 72 h. αShh-Ab or control IgG was added to the medium at the same time as E2. The increasing rate of proliferation induced by E2 in the presence and absence of αShh antibody is expressed as mean±s.d. *P<0.05.
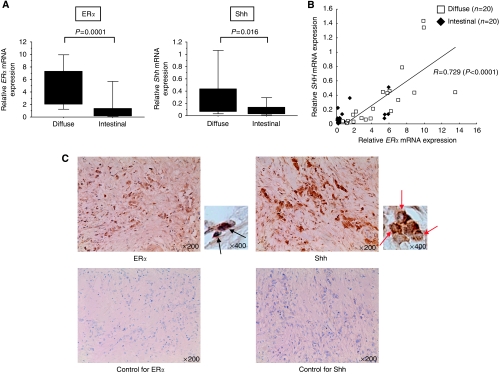
ERα mRNA expression positively correlates with Shh mRNA expression in gastric cancer tissues
We investigated the possibility that a correlation between the ERα and Hh pathways exists in vivo using 40 surgically resected gastric cancer tissues. When 40 gastric cancer tissues were histologically divided into two groups, that is, 20 diffuse type and 20 intestinal type, no significant correlation between histological type and UICC stage was found (data not shown). The ERα mRNA expression was significantly higher in diffuse-type gastric cancer tissues than in intestinal-type gastric cancer tissues (P<0.0001; Figure 5A). Similarly, Shh mRNA expression was significantly higher in diffuse-type gastric cancer tissues than in intestinal-type gastric cancer tissues (P<0.016; Figure 5A). As expected, mRNA expression levels of ERα and Shh were tightly correlated (P<0.0001; Figure 5B). The correlation between ERα and Shh is significantly stronger in diffuse-type (P<0.0001; Supplementary Figure 1A) gastric cancer tissues than in intestinal-type gastric cancer tissues (P<0.0226; Supplementary Figure 1B). Expression of ERα and Shh was also examined immunohistochemically. Consistent with mRNA expression, both ERα and Shh were also highly expressed in diffuse-type gastric cancer cells (Figure 5C). In addition, histochemical analysis showed that Shh is mainly expressed by cancer cells themselves. In this study, however, we did not perform correlation analysis between these molecules at the protein level, because it was difficult to accurately estimate the expression intensity. Nevertheless, our data suggest that a novel link between the ERα and Hh pathways is present even in gastric cancer tissues.
Figure 5.
ERα mRNA expression positively correlates with Shh mRNA expression in gastric cancer tissues. (A) Relative ERα and Shh mRNA expressions in histological diffuse-type or intestinal-type gastric cancer are shown after normalisation to the corresponding β-actin mRNA expression. (B) Correlation with ERα and Shh mRNA expression in gastric cancer tissues. These were significantly correlated (R=0.729, P<0.0001). (C) The representative photographs of immunohistochemistry for ERα and Shh in a diffuse-type gastric cancer tissue. ERα expression (arrows) was observed in gastric cancer cells (upper left panels). Shh expression (arrow heads) was also observed in gastric cancer cells (upper right panels). The photographs stained with secondary antibody alone are shown as control (lower panels).
Discussion
We have shown, for the first time, a biologically significant linkage between the ERα and Hh pathways in ERα-positive gastric cancer cells. Briefly, oestrogen activates the ERα pathway, induces Shh production, activates Hh activation in an Shh-dependent manner and consequently increases cell proliferation in ERα-positive gastric cancer cells. Our data suggest that the ERα pathway could be a possible therapeutic target for patients with ERα-positive gastric cancer.
Consistent with our present data, it has already been shown that both ERα (Kitaoka, 1983; Tokunaga et al, 1986; Matsui et al, 1992; Zhao et al, 2003) and Shh (Ma et al, 2005; Yanai et al, 2007) are frequently expressed in diffuse-type gastric cancer, compared with intestinal type. Recently, it was shown that the Hh pathway might be linked to other proliferation-related signalling pathways. We have shown a crosstalk of the Hh pathway with the nuclear factor κ-B pathway in pancreatic cancer (Nakashima et al, 2006), the Wnt pathway in colonic and gastric cancer (Akiyoshi et al, 2008; Yanai et al, 2008) and the ERα pathway in breast cancer (Koga et al, 2008). Thus, we speculated that there was a linkage between the ERα and Hh pathways in diffuse-type gastric cancer. Our present data showed two key points in the linkage between the two pathways. One finding is that the ERα pathway affects the Hh pathway, because E2 induces both ERα pathway activation and Shh induction, followed by Hh pathway activation, and all of these phenomena were almost completely suppressed by blockade of the ERα pathway. The other finding is that the Hh pathway does not affect the ERα pathway, because neither blockade nor stimulation of the Hh pathway affected ERα pathway activation. A key molecule linking the ERα pathway with the Hh pathway is Shh, which is induced by ERα pathway activation. Thus, we speculate that a crosstalk between the two pathways is a one-way link from the ERα to the Hh pathway. The molecular mechanisms by which ERα pathway activation induces Shh production remain unclear.
Ligand-dependent Hh pathway activation participates in the increased proliferation of gastric cancer (Berman et al, 2003; Yanai et al, 2007). Therefore, in our study, it is not surprising that oestrogen-induced Shh induction increased the proliferation of ERα-positive gastric cancer cells. Our data indicate that blockade of the ERα pathway, such as using anti-oestrogens, may be valuable therapeutic tools for patients with ERα-positive gastric cancer. Interestingly, several clinical randomised controlled studies have already been performed using the selective ER modulator, TAM. Although ER status is an independent poor prognostic factor in gastric cancer (Harrison et al, 1989b; Matsui et al, 1992), the results of clinical randomised controlled studies disappointed us (Harrison et al, 1989a, 1989b). Nevertheless, our present data still indicate a possibility of an ERα pathway blocker as a therapeutic tool for patients with ERα-positive gastric cancer. When TAM was used at concentrations (1 μM) that do not affect cell proliferation of ERα-negative MK-1 cells (Supplementary Figure 2B), TAM did not significantly suppress both E2-induced Hh activation and E2-induced cell proliferation of ERα-positive gastric cancer cells (Supplementary Figure 2A). In contrast, ICI, at a concentration (100 nM) that does not affect cell proliferation of MK-1cells, almost completely suppressed both E2-induced Hh activation and E2-induced cell proliferation. It is well known that TAM can block only one domain, that is, activating function 2 (AF-2), among two distinct ERα activation domains (Ali and Coombes, 2002), whereas ICI can block both of the activation domains. In addition, it has been reported that TAM seems to function as a partial agonist in uterine tissues (Kedar et al, 1994). These findings indicate a possibility that different anti-oestrogens may display different tissue-specific actions. Our data indicate that the development of clinically available antagonists that can sufficiently block oestrogen-induced cell proliferation is promising for management of patients with aggressive diffuse-type gastric cancer. Our data also indicate that a combination of Hh inhibitors and anti-oestrogens may be more effective against ERα-positive gastric cancer. Furthermore, molecules contributing to E2-induced Shh induction may be novel therapeutic candidate molecules for the management of gastric cancer patients.
Conflict of interest
The authors declare no conflict of interest.
Acknowledgments
We thank Dr Kiyoko Kato (Kyushu University, Fukuoka, Japan), Kaori Nomiyama, Nobuhiro Torata and Miyuki Omori for their skilful technical assistance. This study was supported by General Scientific Research Grants (19591511, 19390337 and 21390363) from the Ministry of Education, Culture, Sports and Technology of Japan.
Footnotes
Supplementary Information accompanies the paper on British Journal of Cancer website (http://www.nature.com/bjc)
Supplementary Material
References
- Ackerman GE, Smith ME, Mendelson CR, MacDonald PC, Simpson ER (1981) Aromatization of androstenedione by human adipose tissue stromal cells in monolayer culture. J Clin Endocrinol Metab 53: 412–417 [DOI] [PubMed] [Google Scholar]
- Akiyoshi T, Nakamura M, Yanai K, Nagai S, Wada J, Koga K, Nakashima H, Sato N, Tanaka M, Katano M (2008) Gamma-secretase inhibitors enhance taxane-induced mitotic arrest and apoptosis in colon cancer cells. Gastroenterology 134: 131–144 [DOI] [PubMed] [Google Scholar]
- Ali S, Coombes RC (2002) Endocrine-responsive breast cancer and strategies for combating resistance. Nat Rev Cancer 2: 101–112 [DOI] [PubMed] [Google Scholar]
- Berman DM, Karhadkar SS, Maitra A, Montes De Oca R, Gerstenblith MR, Briggs K, Parker AR, Shimada Y, Eshleman JR, Watkins DN, Beachy PA (2003) Widespread requirement for hedgehog ligand stimulation in growth of digestive tract tumours. Nature 425: 846–851 [DOI] [PubMed] [Google Scholar]
- Briscoe J, Therond P (2005) Hedgehog signaling: from the Drosophila cuticle to anti-cancer drugs. Dev Cell 8: 143–151 [DOI] [PubMed] [Google Scholar]
- Brodie A, Inkster S (1993) Aromatase in the human testis. J Steroid Biochem Mol Biol 44: 549–555 [DOI] [PubMed] [Google Scholar]
- Campbell-Thompson ML (1997) Estrogen receptor alpha and beta expression in upper gastrointestinal tract with regulation of trefoil factor family 2 mRNA levels in ovariectomized rats. Biochem Biophys Res Commun 240: 478–483 [DOI] [PubMed] [Google Scholar]
- Cengel KA (2004) Targeting sonic hedgehog: a new way to mow down pancreatic cancer? Cancer Biol Ther 3: 165–166 [DOI] [PubMed] [Google Scholar]
- Chandanos E, Rubio CA, Lindblad M, Jia C, Tsolakis AV, Warner M, Gustafsson JA, Lagergren J (2008) Endogenous estrogen exposure in relation to distribution of histological type and estrogen receptors in gastric adenocarcinoma. Gastric Cancer 11: 168–174 [DOI] [PubMed] [Google Scholar]
- Dimmler A, Brabletz T, Hlubek F, Häfner M, Rau T, Kirchner T, Faller G (2003) Transcription of sonic hedgehog, a potential factor for gastric morphogenesis and gastric mucosa maintenance, is up-regulated in acidic conditions. Lab Invest 83: 1829–1837 [DOI] [PubMed] [Google Scholar]
- Green S, Issemann I, Sheer E (1988) A versatile in vivo and in vitro eukaryotic expression vector for protein engineering. Nucleic Acids Res 16: 369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrison JD, Morris DL, Ellis IO, Jones JA, Jackson I (1989a) The effect of tamoxifen and estrogen receptor status on survival in gastric carcinoma. Cancer 64: 1007–1010 [DOI] [PubMed] [Google Scholar]
- Harrison JD, Watson S, Morris DL (1989b) The effect of sex hormones and tamoxifen on the growth of human gastric and colorectal cancer cell lines. Cancer 63: 2148–2151 [DOI] [PubMed] [Google Scholar]
- Hooper JE, Scott MP (2005) Communicating with hedgehogs. Nat Rev Mol Cell Biol 6: 306–317 [DOI] [PubMed] [Google Scholar]
- Karat D, Brotherick I, Shenton BK, Scott D, Raimes SA, Griffin SM (1999) Expression of oestrogen and progesterone receptors in gastric cancer: a flow cytometric study. Br J Cancer 80: 1271–1274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karhadkar SS, Bova GS, Abdallah N, Dhara S, Gardner D, Maitra A, Isaacs JT, Berman DM, Beachy PA (2004) Hedgehog signalling in prostate regeneration, neoplasia and metastasis. Nature 431: 707–712 [DOI] [PubMed] [Google Scholar]
- Kato K, Horiuchi S, Takahashi A, Ueoka Y, Arima T, Matsuda T, Kato H, Nishida Ji J, Nakabeppu Y, Wake N (2002) Contribution of estrogen receptor alpha to oncogenic K-Ras-mediated NIH3T3 cell transformation and its implication for escape from senescence by modulating the p53 pathway. J Biol Chem 277: 11217–11224 [DOI] [PubMed] [Google Scholar]
- Katoh Y, Katoh M (2005) Hedgehog signaling pathway and gastric cancer. Cancer Biol Ther 4: 1050–1054 [DOI] [PubMed] [Google Scholar]
- Katoh Y, Katoh M (2006) Hedgehog signaling pathway and gastrointestinal stem cell signaling network (review). Int J Mol Med 18: 1019–1023 [PubMed] [Google Scholar]
- Kedar RP, Bourne TH, Powles TJ, Collins WP, Ashley SE, Cosgrove DO, Campbell S (1994) Effects of tamoxifen on uterus and ovaries of postmenopausal women in a randomised breast cancer prevention trial. Lancet 343: 1318–1321 [DOI] [PubMed] [Google Scholar]
- Kitaoka H (1983) [Sex hormone dependency and endocrine therapy in diffuse carcinoma of the stomach]. Gan To Kagaku Ryoho 10: 2453–2460 [PubMed] [Google Scholar]
- Koga K, Nakamura M, Nakashima H, Akiyoshi T, Kubo M, Sato N, Kuroki S, Nomura M, Tanaka M, Katano M (2008) Novel link between estrogen receptor alpha and hedgehog pathway in breast cancer. Anticancer Res 28: 731–740 [PubMed] [Google Scholar]
- Koullias GJ, Pratsinis CI, Korkolis DP, Kouraklis G, Papadopoulos SA, Davaris PS, Golematis BCh (2003) Brief tamoxifen pretreatment enhances the chemosensitivity of gastric carcinoma cells to 5-fluorouracil in vitro. Anticancer Res 23: 1575–1580 [PubMed] [Google Scholar]
- Kubo M, Nakamura M, Tasaki A, Yamanaka N, Nakashima H, Nomura M, Kuroki S, Katano M (2004) Hedgehog signaling pathway is a new therapeutic target for patients with breast cancer. Cancer Res 64: 6071–6074 [DOI] [PubMed] [Google Scholar]
- Lauren P (1965) The two histological main types of gastric carcinoma: diffuse and so-called intestinal-type carcinoma. An attempt at a histo-clinical classification. Acta Pathol Microbiol Scand 64: 31–49 [DOI] [PubMed] [Google Scholar]
- Lephart ED (1996) A review of brain aromatase cytochrome P450. Brain Res Brain Res Rev 22: 1–26 [PubMed] [Google Scholar]
- Leshin M, Baron J, George FW, Wilson JD (1981) Increased estrogen formation and aromatase activity in fibroblasts cultured from the skin of chickens with the Henny feathering trait. J Biol Chem 256: 4341–4344 [PubMed] [Google Scholar]
- Lum L, Beachy PA (2004) The Hedgehog response network: sensors, switches, and routers. Science 304: 1755–1759 [DOI] [PubMed] [Google Scholar]
- Ma X, Chen K, Huang S, Zhang X, Adegboyega PA, Evers BM, Zhang H, Xie J (2005) Frequent activation of the hedgehog pathway in advanced gastric adenocarcinomas. Carcinogenesis 26: 1698–1705 [DOI] [PubMed] [Google Scholar]
- Ma XL, Sun HJ, Wang YS, Huang SH, Xie JW, Zhang HW (2006) Study of Sonic hedgehog signaling pathway related molecules in gastric carcinoma. World J Gastroenterol 12: 3965–3969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsui M, Kojima O, Kawakami S, Uehara Y, Takahashi T (1992) The prognosis of patients with gastric cancer possessing sex hormone receptors. Surg Today 22: 421–425 [DOI] [PubMed] [Google Scholar]
- Matthews J, Gustafsson JA (2003) Estrogen signaling: a subtle balance between ER alpha and ER beta. Mol Interv 3: 281–292 [DOI] [PubMed] [Google Scholar]
- Ming SC (1998) Cellular and molecular pathology of gastric carcinoma and precursor lesions: a critical review. Gastric Cancer 1: 31–50 [DOI] [PubMed] [Google Scholar]
- Nakashima H, Nakamura M, Yamaguchi H, Yamanaka N, Akiyoshi T, Koga K, Yamaguchi K, Tsuneyoshi M, Tanaka M, Katano M (2006) Nuclear factor-kappaB contributes to hedgehog signaling pathway activation through sonic hedgehog induction in pancreatic cancer. Cancer Res 66: 7041–7049 [DOI] [PubMed] [Google Scholar]
- Parkin DM (2001) Global cancer statistics in the year 2000. Lancet Oncol 2: 533–543 [DOI] [PubMed] [Google Scholar]
- Pasca di Magliano M, Hebrok M (2003) Hedgehog signalling in cancer formation and maintenance. Nat Rev Cancer 3: 903–911 [DOI] [PubMed] [Google Scholar]
- Ramalho-Santos M, Melton DA, McMahon AP (2000) Hedgehog signals regulate multiple aspects of gastrointestinal development. Development 127: 2763–2772 [DOI] [PubMed] [Google Scholar]
- Sanchez P, Hernández AM, Stecca B, Kahler AJ, DeGueme AM, Barrett A, Beyna M, Datta MW, Datta S, Ruiz i Altaba A (2004) Inhibition of prostate cancer proliferation by interference with SONIC HEDGEHOG-GLI1 signaling. Proc Natl Acad Sci USA 101: 12561–12566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheng T, Li C, Zhang X, Chi S, He N, Chen K, McCormick F, Gatalica Z, Xie J (2004) Activation of the hedgehog pathway in advanced prostate cancer. Mol Cancer 3: 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh S, Poulsom R, Wright NA, Sheppard MC, Langman MJ (1997) Differential expression of oestrogen receptor and oestrogen inducible genes in gastric mucosa and cancer. Gut 40: 516–520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takano N, Iizuka N, Hazama S, Yoshino S, Tangoku A, Oka M (2002) Expression of estrogen receptor-alpha and -beta mRNAs in human gastric cancer. Cancer Lett 176: 129–135 [DOI] [PubMed] [Google Scholar]
- Thayer SP, di Magliano MP, Heiser PW, Nielsen CM, Roberts DJ, Lauwers GY, Qi YP, Gysin S, Fernández-del Castillo C, Yajnik V, Antoniu B, McMahon M, Warshaw AL, Hebrok M (2003) Hedgehog is an early and late mediator of pancreatic cancer tumorigenesis. Nature 425: 851–856 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tokunaga A, Nishi K, Matsukura N, Tanaka N, Onda M, Shirota A, Asano G, Hayashi K (1986) Estrogen and progesterone receptors in gastric cancer. Cancer 57: 1376–1379 [DOI] [PubMed] [Google Scholar]
- Ueyama T, Shirasawa N, Numazawa M, Yamada K, Shelangouski M, Ito T, Tsuruo Y (2002) Gastric parietal cells: potent endocrine role in secreting estrogen as a possible regulator of gastro-hepatic axis. Endocrinology 143: 3162–3170 [DOI] [PubMed] [Google Scholar]
- van den Brink GR, Hardwick JC, Tytgat GN, Brink MA, Ten Kate FJ, Van Deventer SJ, Peppelenbosch MP (2001) Sonic hedgehog regulates gastric gland morphogenesis in man and mouse. Gastroenterology 121: 317–328 [DOI] [PubMed] [Google Scholar]
- van den Brink GR, Hardwick JC, Nielsen C, Xu C, ten Kate FJ, Glickman J, van Deventer SJ, Roberts DJ, Peppelenbosch MP (2002) Sonic hedgehog expression correlates with fundic gland differentiation in the adult gastrointestinal tract. Gut 51: 628–633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watkins DN, Berman DM, Burkholder SG, Wang B, Beachy PA, Baylin SB (2003) Hedgehog signalling within airway epithelial progenitors and in small-cell lung cancer. Nature 422: 313–317 [DOI] [PubMed] [Google Scholar]
- Wu CW, Chang YF, Yeh TH, Chang TJ, Lui WY, P’Eng FK, Chi CW (1994) Steroid hormone receptors in three human gastric cancer cell lines. Dig Dis Sci 39: 2689–2694 [DOI] [PubMed] [Google Scholar]
- Yanai K, Nagai S, Wada J, Yamanaka N, Nakamura M, Torata N, Noshiro H, Tsuneyoshi M, Tanaka M, Katano M (2007) Hedgehog signaling pathway is a possible therapeutic target for gastric cancer. J Surg Oncol 95: 55–62 [DOI] [PubMed] [Google Scholar]
- Yanai K, Nakamura M, Akiyoshi T, Nagai S, Wada J, Koga K, Noshiro H, Nagai E, Tsuneyoshi M, Tanaka M, Katano M (2008) Crosstalk of hedgehog and Wnt pathways in gastric cancer. Cancer Lett 263: 145–156 [DOI] [PubMed] [Google Scholar]
- Yuasa Y (2003) Control of gut differentiation and intestinal-type gastric carcinogenesis. Nat Rev Cancer 3: 592–600 [DOI] [PubMed] [Google Scholar]
- Zhao XH, Gu SZ, Liu SX, Pan BR (2003) Expression of estrogen receptor and estrogen receptor messenger RNA in gastric carcinoma tissues. World J Gastroenterol 9: 665–669 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.