ABSTRACT
OBJECTIVE
To investigate what role family physicians currently play in the management of patients with nutrition-related issues and whether implementation of current nutrition counseling guidelines is feasible in primary care practices.
DESIGN
Mailed survey.
SETTING
Family practice offices in British Columbia.
PARTICIPANTS
A total of 451 Canadian-trained family physicians practising in British Columbia.
MAIN OUTCOME MEASURES
Respondents’ demographic characteristics; respondents’ attitudes about and perceived barriers to nutrition counseling, as well as their current practices and training in this area.
RESULTS
Among the 757 physicians surveyed, the response rate was 59.6%. Overall, respondents had positive attitudes about the role of nutrition in patient health, and most physicians (58.1%) believed that more than 60% of their patients would benefit from nutrition counseling. However, there was a considerable gap between the proportion of patients who respondents thought would benefit from nutrition counseling and the proportion of patients who received such counseling either in the family physicians’ offices or through referral to dietitians. Rural physicians referred patients to dietitian services more frequently than urban physicians did (41.7% vs 21.7% made more than 20 referrals to dietitians each year). Nearly all physicians identified lack of time and compensation as the strongest barriers to providing nutrition guidance. Training was not considered to be as strong a barrier to counseling, even though 82.3% of family physicians reported their formal nutrition training in medical school to be inadequate, and only 30% of family physicians reported currently using any nutrition-related resources.
CONCLUSION
For family physicians, successful implementation of the 2006 Canadian Clinical Practice Guidelines on the Management and Prevention of Obesity requires access to adequate training, compensation, and evidence-based interventions related to nutrition. This study highlights current nutrition counseling practices in family medicine and identifies several obstacles to integrating the current guidelines in primary care settings.
RÉSUMÉ
OBJECTIF
Examiner le rôle que jouent présentement les médecins de famille dans le traitement des patients présentant des problèmes d’ordre nutritionnel et déterminer si la mise en œuvre des directives actuelles sur le counseling nutritionnel est réalisable en médecine primaire.
TYPE D‘ÉTUDE
Enquête postale.
CONTEXTE
Établissements de médecine familiale de Colombie-Britannique.
PARTICIPANTS
Un total de 451 médecins de famille formés au Canada et pratiquant en Colombie-Britannique.
PRINCIPAUX PARAMÈTRES À L’ÉTUDE
Caractéristiques démographiques des répondants; leur attitude à l’égard du counseling nutritionnel et les facteurs qui s’y opposent, de même que leurs façons de faire actuelles et leur formation dans ce domaine.
RÉSULTATS
Sur les 757 médecins consultés, le taux de réponse était de 59,6 %. Globalement, les répondants avaient des attitudes positives concernant le rôle de la nutrition dans la santé des patients, et la plupart (58,1 %) estimaient que plus de 60 % de leurs patients bénéficieraient de conseils nutritionnels. Toutefois, il y avait un écart considérable entre la proportion de patients qui, selon les répondants, bénéficieraient de ces conseils et la proportion de ceux qui recevaient de tels conseils soit au bureau du médecin, soit par l’intermédiaire d’une consultation en diététique. Les médecines ruraux adressaient plus souvent leurs patients aux services diététiques que les médecins urbains (41,7 % contre 21,7 % ont demandé plus de 20 consultations en diététique par année). Presque tous les répondants indiquaient que le manque de temps et de rémunération étaient les principaux obstacles au counseling nutritionnel. La formation n’était pas considérée comme un obstacle aussi important, même si 82,3 % des médecins de famille mentionnaient avoir eu une formation insuffisante à la faculté et seulement 30 % d’entre eux disaient faire actuellement usage de ressources en lien avec la nutrition.
CONCLUSION
Pour les médecins de famille, le succès dans la mise en œuvre des directives canadiennes de pratique clinique de 2006 sur le traitement et la prévention de l’obésité requiert l’accès à une formation et une rémunération adéquates, et à des interventions nutritionnelles fondées sur des preuves. Cette étude décrit les modes actuels de counseling nutritionnel en médecine familiale et identifie plusieurs obstacles à la mise en œuvre des directives actuelles dans un contexte de soins primaires.
The current generation of children is the first in recent history projected to have a shorter lifespan than that of their parents. This projection is based on the rising incidence of obesity, which is replacing undernutrition as the most prevalent nutrition-related disease in the world.1–3 Obesity is an important modifiable risk factor for chronic diseases such as heart disease, hypertension, stroke, and diabetes, which accounted for 32% of deaths worldwide in 2005.4–7 In Canada, an estimated 36% of adults and 18% of children are considered to be overweight (body mass index 25 to 30 kg/m2), and an additional 23% of adults and 8% of children are considered to be obese (body mass index > 30 kg/m2).8,9
The 2006 Canadian Clinical Practice Guidelines on the Management and Prevention of Obesity10 underscore the importance of nutritional assessment and dietary intervention as part of an integrated approach within the primary care setting. To date, there is little literature from Canada investigating the feasibility of these guidelines in the context of typical family practice visits. Literature from other countries demonstrates that family doctors provide or refer patients to others for dietary counseling for only a small proportion of patients, despite the belief that such counseling is important and can be effective in changing patient behaviour.11 Perceived barriers to counseling identified in other regions included time constraints, lack of payment, and inadequate training.11–14 This study aims to explore nutrition counseling in primary care in a Canadian setting by examining the attitudes about and perceived barriers to nutrition counseling, as well as current practices and training in this area, among family physicians in British Columbia.
METHODS
Design and participants
Based on a predicted response rate of 50% and allowing for a 5% margin of error, 800 general practitioners trained in Canada and family physicians certified by the College of Family Physicians of Canada were randomly selected from the British Columbia College of Physicians and Surgeon’s electronic medical directory. Those physicians who were not currently practising family medicine in British Columbia were excluded. Surveys were mailed in June 2006 with an introductory cover letter, a $1 incentive lottery ticket, and a stamped return envelope with a unique identifier to facilitate repeat mailings. To ensure the results were nonnominal, returned surveys were opened and unique identifiers removed by an independent third party. Nonrespondents were sent a reminder by repeat mailing and another by fax within 4 months of the initial mailing.
A literature review provided initial direction for survey content. Experts in nutrition and questionnaire design reviewed several drafts, and the resulting 4-page, 18-item questionnaire was pilot-tested on a group of family physicians based in Vancouver, BC, and modified accordingly.
Statistical analysis
Data analysis was performed using SPSS version 14.0. Statistical associations between continuous and categorical variables were identified using independent t tests and paired t tests. Associations between pairs of categorical variables relied on cross-tabulation with χ2 tests, while associations between pairs of continuous variables were explored using Pearson correlations. Results were deemed to be significant if P < .05. In order to reduce the number of statistical analyses performed, composite “comfort” and “attitude” scores were calculated for each physician. These continuous composite variables were the average of each physician’s responses to the individual component variables.
This study was approved by the Behavioural Research Ethics Board at the University of British Columbia.
RESULTS
Of the 800 surveys mailed, 23 respondents returned the survey indicating that they did not practise family medicine, 18 were returned to sender, and 2 were returned incomplete. Of the remaining 757 physicians surveyed, 59.6% responded (N = 451). Demographic characteristics of the respondents are outlined and compared with those of the general family physician population in British Columbia in Table 1.15–17
Table 1.
Demographic characteristics of respondents compared with those of family physicians and general practitioners in British Columbia
| CHARACTERISTICS | PROPORTION OF SURVEY RESPONDENTS | PROPORTION OF BC PHYSICIANS15,16 |
|---|---|---|
| Sex | ||
| • Male | 56.4 | 66.1 |
| • Female | 43.6 | 33.9 |
| Age, y | ||
| • ≤ 40 | 24.9 | 24.6 (35–44)* |
| • 41–50 | 37.2 | 33.3 (45–54)* |
| • > 50 | 37.9 | 35.0 (≥ 55)* |
| Practice location† | ||
| • Urban | 52.8 | NA |
| • Suburban | 37.2 | NA |
| • Rural | 24.8 | 20.9‡ |
NA—data not available.
Reference population ages indicated in parenthesis. Percentages do not add to 100 owing to incomplete data.
Definitions of urban, suburban, and rural were not provided to survey respondents.
Rural was defined as areas with populations of less than 10 000 persons.17
Physician comfort with nutrition topics
Using a 10-point Likert scale, physicians were asked to indicate their level of comfort discussing nutrition topics with their patients in 3 broad areas: general nutrition (eg, healthy eating for normal-weight individuals, nutrition for pregnant women and children, vitamin and mineral supplementation, and prevention of chronic disease); nutrition for chronic diseases (eg, heart disease, diabetes, hypercholesterolemia, hypertension, and cancer); and special topics in nutrition (eg, weight loss, vegetarian diets, herbal supplementation, and fad diets). Strong correlations existed within the responses of individual physicians, with those who were comfortable discussing one topic being generally comfortable with all topics. On average, physicians were more comfortable discussing general nutrition topics compared with nutrition topics related to chronic disease (7.77 vs 7.59, P < .0005) or special topics in nutrition (7.77 vs 6.59, P < .0005). Overall comfort scores did not differ significantly between urban and rural physicians.
Attitudes and current practices
Physicians were asked to what extent they agreed with 4 statements about nutrition, using a 5-point Likert scale (Table 2). Responses to the first 3 statements were averaged and used to generate a composite attitude score for each physician, with a higher score reflecting a more positive attitude toward nutrition in family practice. Attitude scores were not associated with sex or practice location, but were significantly associated with age: physicians younger than 50 years of age had more positive attitudes toward nutrition (P = .009).
Table 2.
Physician attitudes toward nutrition counseling in the family practice setting: Physicians were asked to what extent they agreed with the following statements, using a 5-point Likert scale.
| STATEMENTS | STRONGLY DISAGREE, % | SOMEWHAT DISAGREE, % | NEUTRAL, % | SOMEWHAT AGREE, % | STRONGLY AGREE, % |
|---|---|---|---|---|---|
| Counseling patients about nutrition is one of the responsibilities of the physician | 1.1 | 4.5 | 7.0 | 43.0 | 44.3 |
| Nutrition is a significant component of prevention and progression of many chronic diseases | 0.9 | 0.7 | 2.0 | 26.0 | 70.4 |
| Nutrition counseling in the family practice setting is effective at changing patients’ behaviour | 1.1 | 8.2 | 16.3 | 53.3 | 21.3 |
| I feel that patients want more information on nutrition than I am able to provide | 1.8 | 9.1 | 16.6 | 46.6 | 25.9 |
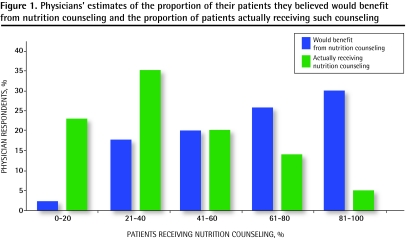
Physicians were asked to indicate what percentage of their patient populations they believed would benefit from and what percentage actually received nutrition counseling in the family practice setting (Figure 1). Most physicians (58.1%) reported that more than 60% of the patients in their practices would benefit from nutrition counseling; however, only 19.1% reported that more than 60% of their patients actually received such counseling. This discrepancy is underscored by the finding that 72.5% of physicians thought that their patients would like more nutrition information than they were able to provide (Table 2).
Figure 1.
Physicians’ estimates of the proportion of their patients they believed would benefit from nutrition counseling and the proportion of patients actually receiving such counseling
Nearly all physicians responding to the survey reported that they referred patients to dietitians (95.2%). However, the frequency of referrals was not associated with the proportion of patients that physicians believed would benefit from nutrition counseling (P = .460) or with the proportion of patients receiving nutrition counseling (P = .494). Similar numbers of physicians reported making fewer than 10 referrals, 10 to 20 referrals, or more than 20 referrals annually (36.9%, 35.6%, and 27.5%, respectively). However, rural physicians reported making significantly more referrals to dietitians than urban physicians did (41.7% of rural physicians made more than 20 referrals per year compared with 21.7% of urban physicians, P < .0005).
Predictors of practice
Both physician comfort level with and physician attitude toward nutrition were strong predictors of a physician’s nutrition counseling practices. Physicians who were more comfortable providing nutrition counseling thought that more of their patients would benefit from such counseling (P = .034), were more likely to provide nutrition counseling to patients in their offices (P < .0005), and were more likely to spend more time discussing nutrition per visit (P < .0005). Physicians’ attitude scores were strongly associated with providing nutrition counseling (P < .0005). Specifically, family physicians who believed nutrition counseling was one of their roles, and those who believed it was effective for changing behaviour, reported that a significantly greater proportion of their patients received nutrition counseling in their offices (P < .0005 for both comparisons).
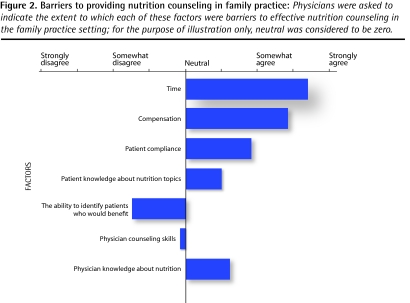
Barriers to nutrition counseling
Using a 5-point Likert scale, physicians were asked to indicate which factors were barriers to effective nutrition counseling (Figure 2). Inadequate time and compensation were the most consistently identified obstacles, while physician counseling skills and the ability to identify patients who would benefit were not considered to be barriers. Physicians working in rural areas were less likely than their nonrural counterparts to consider compensation (4.22 vs 4.45, P = .031) and physician counseling skills (2.66 vs 3.01, P = .024) to be barriers to providing nutrition counseling. There was no consistent association between the identified barriers and the frequency of dietitian referrals.
Figure 2.
Barriers to providing nutrition counseling in family practice: Physicians were asked to indicate the extent to which each of these factors were barriers to effective nutrition counseling in the family practice setting; for the purpose of illustration only, neutral was considered to be zero.
Knowledge and training
When questioned about the adequacy of their nutrition training in medical school, by far most (82.3%) physicians thought it was inadequate. This finding was independent of age (P = .198) and year of graduation (P = .681). Respondents who considered their training to be inadequate reported significantly lower levels of comfort with counseling patients about nutrition (P = .010), and these respondents were more likely to consider physician knowledge to be a barrier to providing counseling in their practices (17.4% vs 7.1%, P = .002). The perceived adequacy of nutrition training was not associated with a physician’s estimate of the proportion of patients who would benefit from nutrition counseling or with the proportion of patients who received such counseling.
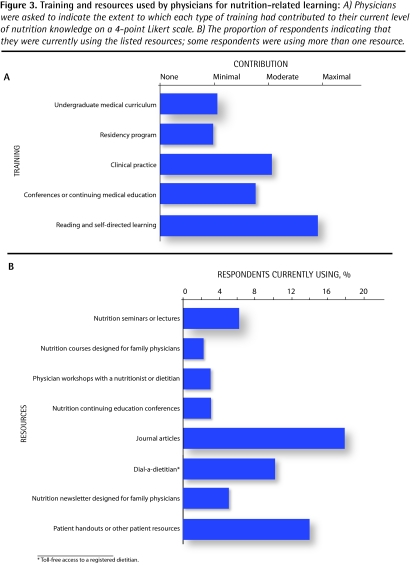
Physicians were also asked to indicate the extent to which various stages and types of training had contributed to their current level of nutrition-related knowledge (Figure 3A). Most indicated that reading and self-directed learning had made the largest contribution; however, only 30% of physicians reported currently using any nutrition-related resource (Figure 3B). When asked which resources they thought would be effective, physicians responded positively to all modalities with no statistically significant differences found among the resources listed.
Figure 3.
Training and resources used by physicians for nutrition-related learning: A) Physicians were asked to indicate the extent to which each type of training had contributed to their current level of nutrition knowledge on a 4-point Likert scale. B) The proportion of respondents indicating that they were currently using the listed resources; some respondents were using more than one resource.
DISCUSSION
Attitudes and current practice
Overall, family physicians had positive attitudes toward the potential effects of nutrition counseling on patient behaviour, and they believed that most of their patients would benefit from nutrition counseling. Nevertheless, there was a considerable gap between the number of patients that physicians thought would benefit from nutrition counseling and the number that received such counseling. Studies from other regions have demonstrated similar findings.11,12,18
Despite the perceived need for nutrition counseling identified in this study, there was no associated increase in the frequency of dietitian referrals, suggesting that many patients who might benefit from dietary counseling do not have access to it, either from their primary care providers or dietitians. Although this study did not explore why physicians are underusing dietitians, previous studies have identified concerns about effectiveness, lack of feedback to physicians, cost to patients, inaccessibility of services secondary to waiting lists, and geographic location.19,20 In our study there was an increased frequency of referral from rural physicians compared with their nonrural counterparts. This finding might be related to the nature of practice in smaller medical centres, where physicians might have more opportunity for interaction and direct communication with allied health professionals. Rural health workers might also collaborate more with other professionals, as they have less support from members of their own profession compared with those in urban areas.21 Creating more effective links between urban family physicians and dietitians might improve access to nutrition counseling for patients living in larger centres.
Barriers
In contrast to some studies,12–14 physician-related factors such as knowledge, counseling skills, and the ability to identify appropriate patients were not identified as important barriers, despite the fact that more than 80% of respondents thought their nutrition training had been inadequate. Rather, lack of time and compensation were identified as the strongest barriers, consistent with studies from other countries.11–13 The recent addition of a billing code in British Columbia for risk evaluation related to cardiovascular disease, which can include nutritional assessment,22 is a step toward addressing these identified barriers.
That more than 50% of respondents only “somewhat agreed” that “nutrition counseling in the family practice setting [was] effective at changing patients’ behaviour” might help explain some physicians’ unwillingness to provide nutrition counseling. Results from other studies are consistent with this perceived modest effectiveness of nutrition counseling, especially when compared with other preventive interventions, such as smoking cessation counseling and cervical and prostate cancer screening programs.12,18 It has also been shown that nutrition counseling by other health care professionals is more effective than that provided by family physicians.23 Although a systematic review showed that multiple visits of considerable length are required to change a patient’s behaviour,24 other literature suggests that interventions need not be so time-intensive for family physicians, and that they are effective when used in conjunction with tools and strategies such as dietary questionnaires and educational handouts, flagging high-risk patients, scheduling “well-care” visits, and follow-up telephone counseling.25–27 In addition, training family physicians in counseling techniques has been shown to be effective both for changing patient behaviour28–30 and for giving physicians the confidence to provide and follow-up on such interventions.31 Although the addition of a billing code might improve the provision of dietary counseling in primary care in British Columbia, it will likely take the addition of a number of these other strategies to improve patient outcomes.
Knowledge and training
Given that most respondents in this study reported that their nutrition training in medical school was inadequate, it might not be surprising that only 30% of family physicians currently use any nutrition-related resources. A poor base of nutrition knowledge and a lack of compensation for counseling in the office likely affect physicians’ motivation for continuing education on nutrition topics. Previous studies have identified patient pamphlets as the most useful aid in counseling and peer-reviewed nutrition journals as being the most commonly used resource for continuing education,32,33 although respondents in our study did not single out any particular resource as being more effective than another. Improving physicians’ nutrition knowledge and counseling skills requires a comprehensive approach, including sufficient nutrition curriculum in medical school and residency, incentives for physicians to engage in continuing education, and finally effective and practical tools to support counseling in family practice clinics.
Limitations
The physicians surveyed in our study were Canadian-trained and practising within a single province in the Canadian health care system, and the concerns and barriers identified might not be generalizable beyond this population. As with all self-administered surveys, this study was subject to a volunteer bias, although the effects of this are minimized by the nearly 60% response rate. Results might also have been subject to a social desirability response bias, whereby respondents give socially acceptable responses rather than reporting their actual opinions or practices. However, many physicians surveyed offered self-critical responses to various questionnaire items, suggesting that this bias did not have a strong effect on the results of this study.
Conclusion
The new Canadian guidelines on the management and prevention of obesity recommended initial assessment by a physician, a multidisciplinary approach to lifestyle modification, and regular follow-up. Findings from this study suggest that physicians recognize the importance of dietary intervention and demonstrate a willingness to provide nutrition counseling. However, inadequate training, time, and compensation; insufficient use of dietitian services; and a lack of evidence-based interventions remain obstacles in the primary care setting. Initiatives to reduce barriers to preventive counseling and further research around nutrition-related interventions in the primary care setting are urgently needed to mitigate the ever growing burden of preventable chronic diseases.
Acknowledgments
We thank Heather Lovelace and Cheryl Taunton for their invaluable contributions. This study was funded by the Canadian Institutes of Health Research Institute of Nutrition, Metabolism, and Diabetes; the British Columbia College of Family Physicians; and the University of British Columbia Faculty of Medicine Summer Student Internship Program.
EDITOR’S KEY POINTS
The 2006 Canadian Clinical Practice Guidelines on the Management and Prevention of Obesity highlight nutritional assessment and dietary intervention by primary care providers (or through referral to dietitians) as key components. This study investigates what role family physicians currently play in the management of patients with nutrition-related issues and whether implementation of these guidelines is feasible in primary care practices.
Findings from this study suggest that physicians recognize the importance of dietary intervention and demonstrate a willingness to provide nutrition counseling. However, inadequate training, time, and compensation; insufficient use of dietitian services; and a lack of evidence-based interventions remain obstacles in the primary care setting. Initiatives to reduce barriers to preventive counseling and further research around nutrition-related interventions in the primary care setting are needed to mitigate the ever growing burden of preventable chronic diseases.
POINTS DE REPÈRE DU RÉDACTEUR
Les directives canadiennes de pratique clinique de 2006 sur le traitement et la prévention de l’obésité soulignent le rôle primordial de l’évaluation nutritionnelle et des interventions alimentaires effectuées par les soignants de première ligne (ou par l’intermédiaire de diététistes consultés). Cette étude voulait connaître le rôle que joue actuellement le médecin de famille dans le traitement des patients qui présentent des problèmes d’ordre nutritionnel et déterminer si ces directives sont applicables en médecine de première ligne.
D’après nos résultats, les médecins reconnaissent l’importance des interventions nutritionnelles et se disent prêts à prodiguer des conseils sur l’alimentation. Toutefois, le manque de formation, de temps et de rémunération; le recours insuffisant aux services de diététique; et l’absence d’interventions fondées sur des preuves demeurent des obstacles dans un contexte de soins primaires. Si on veut atténuer la montée incessante des maladies chroniques évitables, il faudra trouver des moyens de faciliter le counseling préventif et effectuer davantage de recherches sur les interventions d’ordre nutritionnel.
Footnotes
This article has been peer reviewed.
Contributors
Dr Scott is the principle investigator for this project and was involved with study design, analysis of data, and revision of the manuscript. Drs Wynn, Trudeau, and Taunton made equal contributions to study design, survey development, analysis of data, and manuscript composition. Ms Gowans was responsible for statistical analysis of the data and review of the manuscript.
Competing interests
None declared
References
- 1.Ludwig DS. Childhood obesity—the shape of things to come. N Engl J Med. 2007;357(23):2325–7. doi: 10.1056/NEJMp0706538. [DOI] [PubMed] [Google Scholar]
- 2.Olshansky SJ, Passaro DJ, Hershow RC, Layden J, Carnes BA, Brody J, et al. A potential decline in life expectancy in the United States in the 21st century. N Engl J Med. 2005;352(11):1138–45. doi: 10.1056/NEJMsr043743. [DOI] [PubMed] [Google Scholar]
- 3.Tanumihardjo SA, Anderson C, Kaufer-Horwitz M, Bode L, Emenaker NJ, Haqq AM, et al. Poverty, obesity, and malnutrition: an international perspective recognizing the paradox. J Am Diet Assoc. 2007;107(11):1966–72. doi: 10.1016/j.jada.2007.08.007. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization . Preventing chronic diseases: a vital investment. Geneva, Switz: World Health Organization; 2005. Available from: www.who.int/chp/chronic_disease_report/full_report.pdf. Accessed 2008 Sep 18. [Google Scholar]
- 5.Smith SC., Jr Multiple risk factors for cardiovascular disease and diabetes mellitus. Am J Med. 2007;120(3 Suppl 1):S3–11. doi: 10.1016/j.amjmed.2007.01.002. [DOI] [PubMed] [Google Scholar]
- 6.Sowers JR. Obesity as a cardiovascular risk factor. Am J Med. 2003;115(Suppl 8A):37S–41S. doi: 10.1016/j.amjmed.2003.08.012. [DOI] [PubMed] [Google Scholar]
- 7.Zarraga IG, Schwarz ER. Impact of dietary patterns and interventions on cardiovascular health. Circulation. 2006;114(9):961–73. doi: 10.1161/CIRCULATIONAHA.105.603910. Erratum in: Circulation 2006;114(19):e577. [DOI] [PubMed] [Google Scholar]
- 8.Shields M. Overweight and obesity among children and youth. Health Rep. 2006;17(3):27–42. [PubMed] [Google Scholar]
- 9.Tjepkema M. Nutrition: findings from the Canadian Community Health Survey. Ottawa, ON: Statistics Canada; 2005. Measured obesity. Adult obesity in Canada: measured height and weight. Issue No. 1. Catalogue No. 82-620-MWE2005001. Available from: www.statcan.ca/english/research/82-620-MIE/2005001/pdf/aobesity.pdf. Accessed 2008 Sep 15. [Google Scholar]
- 10.Lau DC, Douketis JD, Morrison KM, Hramiak IM, Sharma AM, Ur E, et al. 2006 Canadian clinical practice guidelines on the management and prevention of obesity in adults and children [summary] CMAJ. 2007;176(8):S1–13. doi: 10.1503/cmaj.061409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kushner RF. Barriers to providing nutrition counseling by physicians: a survey of primary care practitioners. Prev Med. 1995;24(6):546–52. doi: 10.1006/pmed.1995.1087. [DOI] [PubMed] [Google Scholar]
- 12.Cornuz J, Ghali WA, Di Carlantonio D, Pecoud A, Paccaud F. Physicians’ attitudes towards prevention: importance of intervention-specific barriers and physicians’ health habits. Fam Pract. 2000;17(6):535–40. doi: 10.1093/fampra/17.6.535. [DOI] [PubMed] [Google Scholar]
- 13.Hiddink GJ, Hautvast JG, van Woerkum CM, Fieren CJ, van ‘t Hof MA. Nutrition guidance by primary-care physicians: perceived barriers and low involvement. Eur J Clin Nutr. 1995;49(11):842–51. [PubMed] [Google Scholar]
- 14.Nicholas LG, Pond CD, Roberts DC. Dietitian–general practitioner interface: a pilot study on what influences the provision of effective nutrition management. Am J Clin Nutr. 2003;77(4 Suppl):1039S–42S. doi: 10.1093/ajcn/77.4.1039S. [DOI] [PubMed] [Google Scholar]
- 15.Canadian Medical Association . Statistical information on Canadian physicians: physician demographics. Ottawa, ON: Canadian Medical Association; 2006. Available from: www.cma.ca/index.cfm/ci_id/16959/la_id/1.htm#1. Accessed 2008 Sep 18. [Google Scholar]
- 16.Canadian Institute for Health Information . Supply, distribution and migration of Canadian physicians. Ottawa, ON: Canadian Institute for Health Information; 2005. Available from: http://secure.cihi.ca/cihiweb/products/supply_distribution_migration_canadian_physicians_2005_e.pdf. Accessed 2008 Sep 18. [Google Scholar]
- 17.Society of Rural Physicians of Canada . Comparative regional statistics. Shawville, QC: Society of Rural Physicians of Canada; 2005. Available from: www.srpc.ca. Accessed 2008 Sep 18. [Google Scholar]
- 18.Litaker D, Flocke SA, Frolkis JP, Stange KC. Physicians’ attitudes and preventive care delivery: insights from the DOPC study. Prev Med. 2005;40(5):556–63. doi: 10.1016/j.ypmed.2004.07.015. [DOI] [PubMed] [Google Scholar]
- 19.Nicholas L, Roberts DC, Pond D. The role of the general practitioner and the dietitian in patient nutrition management. Asia Pac J Clin Nutr. 2003;12(1):3–8. [PubMed] [Google Scholar]
- 20.Kuppersmith NC, Wheeler SF. Communication between family physicians and registered dietitians in the outpatient setting. J Am Diet Assoc. 2002;102(12):1756–63. doi: 10.1016/s0002-8223(02)90378-0. [DOI] [PubMed] [Google Scholar]
- 21.Medves J, Paterson M, Chapman CY, Young JH, Tata E, Bowes D, et al. A new inter-professional course preparing learners for life in rural communities. Rural Remote Health. 2008;8(1):836. Epub 2008 Feb 21. [PubMed] [Google Scholar]
- 22.Medical Services Commission . Preventing the onset of chronic diseases: cardiovascular risk assessment fee. Victoria, BC: Ministry of Health Services; 2008. Available from: www.primaryhealthcarebc.ca. Accessed 2008 Sep 15. [Google Scholar]
- 23.Thompson RL, Summerbell CD, Hooper L, Higgins JP, Little PS, Talbot D, et al. Dietary advice given by a dietitian versus other health professional or self-help resources to reduce blood cholesterol. Cochrane Database Syst Rev. 2003;(3):CD001366. doi: 10.1002/14651858.CD001366. [DOI] [PubMed] [Google Scholar]
- 24.Pignone MP, Ammerman A, Fernandez L, Orleans CT, Pender N, Woolf S, et al. Counseling to promote a healthy diet in adults: a summary of the evidence for the U.S Preventive Services Task Force. Am J Prev Med. 2003;24(1):75–92. doi: 10.1016/s0749-3797(02)00580-9. [DOI] [PubMed] [Google Scholar]
- 25.Delichatsios HK, Hunt MK, Lobb R, Emmons K, Gillman MW. EatSmart: efficacy of a multifaceted preventive nutrition intervention in clinical practice. Prev Med. 2001;33(2 Pt 1):91–8. doi: 10.1006/pmed.2001.0848. [DOI] [PubMed] [Google Scholar]
- 26.Ockene IS, Hebert JR, Ockene JK, Saperia GM, Stanek E, Nicolosi R, et al. Effect of physician-delivered nutrition counseling training and an office-support program on saturated fat intake, weight, and serum lipid measurements in a hyperlipidemic population: Worcester Area Trial for Counseling in Hyperlipidemia (WATCH) Arch Intern Med. 1999;159(7):725–31. doi: 10.1001/archinte.159.7.725. [DOI] [PubMed] [Google Scholar]
- 27.Eaton CB, Goodwin MA, Stange KC. Direct observation of nutrition counseling in community family practice. Am J Prev Med. 2002;23(3):174–9. doi: 10.1016/s0749-3797(02)00494-4. [DOI] [PubMed] [Google Scholar]
- 28.Kahan M, Wilson L, Becker L. Effectiveness of physician-based interventions with problem drinkers: a review. CMAJ. 1995;152(6):851–9. [PMC free article] [PubMed] [Google Scholar]
- 29.Lancaster T, Stead L, Silagy C, Sowden A. Effectiveness of interventions to help people stop smoking: findings from the Cochrane Library. BMJ. 2000;321(7257):355–8. doi: 10.1136/bmj.321.7257.355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bertholet N, Daeppen JB, Wietlisbach V, Fleming M, Burnand B. Reduction of alcohol consumption by brief alcohol intervention in primary care: systematic review and meta-analysis. Arch Intern Med. 2005;165(9):986–95. doi: 10.1001/archinte.165.9.986. [DOI] [PubMed] [Google Scholar]
- 31.Richmond R, Mendelsohn C, Kehoe L. Family physicians’ utilization of a brief smoking cessation program following reinforcement contact after training: a randomized trial. Prev Med. 1998;27(1):77–83. doi: 10.1006/pmed.1997.0240. [DOI] [PubMed] [Google Scholar]
- 32.Kelly A, Joffres MR. A survey of physicians’ uses/opinions regarding nutrition education resources. J Can Diet Assoc. 1990;51(3):409–12. [PubMed] [Google Scholar]
- 33.Mihalynuk TV, Knopp RH, Scott CS, Coombs JB. Physician informational needs in providing nutritional guidance to patients. Fam Med. 2004;36(10):722–6. [PubMed] [Google Scholar]