Abstract
The signaling lymphocytic activation molecule (SLAM; CD150) is the immune cell receptor for measles virus (MV). To assess the importance of the SLAM-MV interactions for virus spread and pathogenesis, we generated a wild-type IC-B MV selectively unable to recognize human SLAM (SLAM-blind). This virus differs from the fully virulent wild-type IC-B strain by a single arginine-to-alanine substitution at amino acid 533 of the attachment protein hemagglutinin and infects cells through SLAM about 40 times less efficiently than the isogenic wild-type strain. Ex vivo, this virus infects primary lymphocytes at low levels regardless of SLAM expression. When a group of six rhesus monkeys (Macaca mulatta) was inoculated intranasally with the SLAM-blind virus, no clinical symptoms were documented. Only one monkey had low-level viremia early after infection, whereas all the hosts in the control group had high viremia levels. Despite minimal, if any, viremia, all six hosts generated neutralizing antibody titers close to those of the control monkeys while MV-directed cellular immunity reached levels at least as high as in wild-type-infected monkeys. These findings prove formally that efficient SLAM recognition is necessary for MV virulence and pathogenesis. They also suggest that the selectively SLAM-blind wild-type MV can be developed into a vaccine vector.
Measles virus (MV) is an enveloped virus with a negative-sense RNA genome (2). It is still a major cause of death in children of developing countries, mainly due to opportunistic secondary infections facilitated by MV-induced immune suppression (12, 29). Transient but severe immune suppression is explained at least in part by the rapid spread of MV infection in immune cells (6, 37, 41). MV targets immune cells through its hemagglutinin (H) that binds cellular receptors and triggers the other glycoprotein F to fuse cellular membranes (22).
Two MV receptors have been identified. The first one was the membrane cofactor protein (MCP; CD46), a ubiquitously expressed regulator of complement activation sustaining infection by the MV vaccine strain (8, 21) but not by wild-type (WT) strains (24). Wild-type MV strains, as well as the vaccine strain, enter cells through the signaling lymphocytic activation molecule (SLAM; CD150) (10, 15, 35). SLAM is an immune cell-specific protein expressed on the surface of thymocytes, activated lymphocytes, mature dendritic cells, and activated macrophages (4, 31). The existence of another receptor on cells derived from human lung and bladder epithelium has been inferred (18, 33). While this epithelial receptor (EpR) has not been identified yet, it appears to be a basolateral protein expressed by cells forming tight junctions (18).
We are characterizing the mechanisms by which MV spreads in its host and the pathogenic consequences of the interactions with different receptors. We previously showed that an MV unable to recognize EpR remains virulent in rhesus monkeys but cannot cross the epithelium and is not shed (18). This result is consistent with the model of MV pathogenesis according to which immune cells in the airway lumen are initially infected, cross the epithelial barrier, and disseminate the infection to lymphatic tissues (18). Ultimately, infected immune cells may spread the infection to the respiratory epithelium (11, 18). This new model also predicts that an MV unable to recognize SLAM (SLAM-blind) would fail to spread efficiently and be attenuated.
To test this aspect of the new model, we generated a SLAM-blind MV, based on the previous identification of H protein residues necessary for productive SLAM interactions (23, 36). To assess whether the SLAM-relevant residues, originally identified in the CD46-binding background of the vaccine H protein, are neutral also for EpR-mediated cell entry, we used a wild-type H protein and a cell line expressing EpR. We found that only the arginine-to-alanine mutation at position 533 was completely neutral for EpR-dependent fusion. To investigate the role of SLAM in pathogenesis, we then generated in the wild-type IC-B strain a SLAM-blind MV with the arginine-to-alanine mutation at position 533 (34). After confirming the predicted receptor specificity of the recombinant virus, we inoculated six rhesus monkeys, and we document here that the SLAM-blind MV is attenuated and yet induces strong adaptive immune responses.
MATERIALS AND METHODS
Cells.
The human lung cell line H358 (catalog number CRL-5807; ATCC) was maintained in RPMI 1640 medium (Mediatech Inc., Herndon, VA) supplemented with 2 mM l-glutamine and adjusted to contain 1.5 g/liter sodium bicarbonate, 4.5 g/liter glucose, 10 mM HEPES, 1 mM sodium pyruvate, and 10% fetal calf serum (FCS). The MV rescue helper cell line 293-3-46 (26) was grown in Dulbecco's modified Eagle's medium (DMEM; Mediatech Inc.) with 10% FCS and 1.2 mg of G418/ml (Mediatech Inc.). Vero/human SLAM (hSLAM) cells (24), kindly provided by Y. Yanagi (Kyushu University, Fukuoka, Japan), were maintained in DMEM supplemented with 10% FCS and 0.5 mg of G418/ml.
Recombinant viruses.
Recombinant viruses were generated based on plasmid p(+)MV323 coding for the WT IC323 genome derived from strain IC-B (34). Recombinant MVwtIC323 (WT) and MVwtIC323-GFP ([WTgreen] where GFP is green fluorescent protein) were recovered as previously described (18). The SLAM-blind H protein mutant (HSLAMblind) was generated by importing the two nucleotide changes coding for mutation R533A in pCG-H323 (18) using a QuikChange mutagenesis kit (Stratagene, La Jolla, CA) and transferring the resulting PacI/SpeI fragment into two full-length MV genomes with or without the GFP reporter gene. After transfection with the full-length genomes, the rescue cells were overlaid on H358 cells expressing the EpR to amplify WT-HSLAMblind and WTgreen-HSLAMblind.
Virus titers.
Due to receptor usage restriction, the titers of WT-HSLAMblind and WTgreen-HSLAMblind can be determined only on EpR-expressing H358 cells. MV infection was detected after end-point dilution on H358 cells either directly by GFP fluorescence or indirectly by immunofluorescence using a mixture of two monoclonal antibodies (MAB8905; Chemicon, Billerica, MA) directed against the H protein and labeled with fluorescein isothiocyanate ([FITC] Millipore, Billerica, MA). The indirect method was used for MV titrations in monkey peripheral blood mononucleated cell (PBMC) samples.
Virus stocks.
To prepare virus stocks, Vero/hSLAM or H358 cells were inoculated at a multiplicity of infection (MOI) of 0.03 with the relevant virus and incubated at 37°C. Cells were scraped in Opti-MEM I, and MV particles were released by one freeze-thaw cycle. Titers were determined by 50% end-point titration on Vero/hSLAM or H358 cells according to the Spearman-Kärber method (16). We note that WTgreen titers determined on H358 cells are about 10 times lower than those determined on Vero/hSLAM cells. For consistency, titers of both WTgreen and WTgreen-HSLAMblind were determined on H358 cells.
Standardization of the SLAM-blind virus titers for monkey infection.
Studies with wild-type virus are based on titers determined on Raji cells (7), which cannot be used to titrate the SLAM-blind virus. To be in the position of infecting monkeys with equivalent titers of the SLAM-blind and wild-type viruses, we redetermined the titer of the wild-type virus on H358 cells and found that the titer was similar to titers determined in Raji cells (but about 10 times lower than titers in Vero/hSLAM cells). Thus, we infected monkeys with 104.5 50% tissue culture infectious doses (TCID50) of WT-HSLAMblind based on titers in H358 cells.
Cell-to-cell fusion assay after transient expression.
Vero/hSLAM or H358 cells at 80% confluence in six-well tissue culture plates were transfected with equal amounts (2.4 μg) of the GFP expression plasmid pEGFP-N1 (Clontech, Mountain View, CA), the fusion protein expression plasmid pCG-IC323-F (18), and either pCG-IC323-H (18) or an H protein mutant using Lipofectamine 2000 (Invitrogen, Carlsbad, CA). Cells fusion was assessed at 24 h posttransfection. The field-of-view area was 1,200 by 900 μm and typically contained 2,000 Vero/hSLAM cells or 1,300 H358 cells at the time of assessment. In Vero/hSLAM cells, a syncytium was defined as a cell with five or more nuclei. The levels of fusion in Vero/hSLAM are reported (see Fig. 1) with the following notation: −, two or fewer syncytia per field of view; +, less than 50% of the nuclei located in syncytia; ++, between 50% and 90% of the nuclei located in syncytia; +++, more than 90% of the nuclei located in syncytia. The levels of fusion in H358 are reported (see Fig. 1) with the following notation: −, no syncytium formation; +, less than 8% of the nuclei located in syncytia; ++, 9% to 15% of the nuclei located in syncytia; and +++, 16% to 25% of the nuclei located in syncytia.
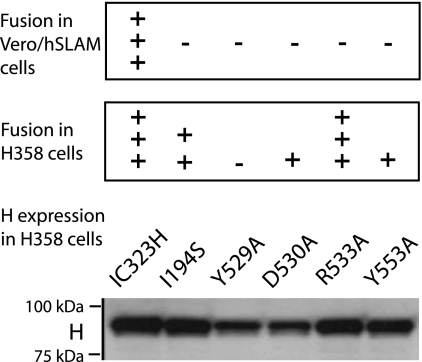
FIG. 1.
Impact of five single amino acid changes on wild-type H protein function. Vero/hSLAM and H358 cells were cotransfected with expression plasmids encoding GFP, IC323-F, and IC323-H or the corresponding mutants. (Top) SLAM-dependent fusion support on Vero/hSLAM cells. (Center) EpR-dependent fusion support on H358 cells. Fusion was graded as indicated in the Materials and Methods section, based on the average of three independent experiments; identification of syncytia was facilitated by the combination of phase-contrast analysis and observation of GFP expression. (Bottom) H protein expression levels in H358 cells at 24 h posttransfection of the corresponding plasmids. H protein was visualized by immunoblotting using an antibody directed against the cytoplasmic tail of H (3).
Virus-induced cell fusion assays.
To obtain clearly separated syncytia originating from single infection events, H358 cells were infected at the low MOI of 0.001. At 48 h postinfection 20 syncytia per virus were identified, and the number of nuclei per syncytium was counted.
Infection of cell lines expressing or not expressing SLAM.
Equal numbers of Vero and Vero/hSLAM cells were mixed and left for 4 h to attach to the bottom of a six-well plate before infection with WTgreen or WTgreen-HSLAMblind at an MOI of 1. After 12 h, the cells were detached using Versene (Gibco) and analyzed by flow cytometry using an anti-SLAM antibody (anti CD150-phycoerythrin; BD Biosciences, Bedford, MA) to quantify SLAM expression and GFP to detect viral infection. We note that Vero/hSLAM cells divide more rapidly then Vero cells, resulting in overrepresentation of the former cells in the fluorescence-activated cell sorter (FACS) analysis.
Ex vivo infection of PBMCs.
Ficoll-purified human PBMCs were seeded in 24-well plates at a density of 4 × 105 cells in 0.5 ml. Nonactivated PBMCs were infected with either WTgreen or WTgreen-HSLAMblind at an MOI of 1 for 24 h. T-cell activation was performed by the addition of 10 μg/ml phytohemagglutinin (PHA; Sigma-Aldrich, Saint-Louis, MO) for 12 h, followed by infection at an MOI of 1 for 12 h before analysis. The number of infected cells was quantified by flow cytometry after staining with phycoerythrin-conjugated anti-CD150 and an allophycocyanin (APC)-conjugated monoclonal mouse antibody directed against CD3 for T-cell staining (BD Biosciences). Acquisition of samples was performed on a flow cytometer (FacsCanto or LSRII; BD Biosciences) and analyzed using FlowJo software (Tree Star Inc., Asland, OR).
Infection of rhesus monkeys.
Colony-bred male and female juvenile rhesus monkeys (Macaca mulatta), seronegative for MV, were housed in accordance with guidelines of the American Association for Accreditation of Laboratory Animal Care. All animal experiments were approved by the UC Davis Chancellor's Animal Use and Care Administrative Advisory Committee.
Six animals were inoculated under the same conditions we previously used for the WT IC-B strain infections (7). Briefly, 104.5 TCID50s of WT-HSLAMblind in a volume of 1 ml were inoculated by a single drop onto the conjunctiva of each eye, and the remainder was divided into both nares (20, 42). The animals were monitored daily for clinical symptoms including anorexia, depression, coughing, diarrhea, and skin rash. They were bled under ketamine sedation on days 0, 3, 7, 14, 28, and 90 after inoculation.
Viremia levels in monkeys.
Viremia was quantified by end-point dilution coculture with H358 cells. Serial 10-fold dilutions of PBMCs were made in RPMI 1640 medium supplemented with 2 mM l-glutamine and adjusted to contain 1.5 g/liter sodium bicarbonate, 4.5 g/liter glucose, 10 mM HEPES, 1 mM sodium pyruvate, and 5% FCS. Four replicates of 101 to 105 PBMCs were cocultured with 4 × 104 H358 cells per well in 96-well plates (Fisher Scientific), and 106 PBMCs were cocultured with 106 H358 cells in T25 flasks. The cultures were maintained for 14 days, monitored for syncytia formation, and stained by immunofluorescence as described above for viral titration.
Humoral immune response.
MV neutralizing antibody titers were determined by plaque reduction assay by incubating complement-inactivated macaque serum dilutions with 50 PFU of MVvac(GFP)N expressing GFP (28), and titers were expressed as 90% plaque reduction fluorescence-forming units, as previously described (28).
Cell-mediated immunity.
MV-specific T cells were counted using a gamma interferon (IFN-γ) enzyme-linked immunospot (ELISPOT) assay as previously described (25). Briefly, PBMCs were resuspended at 5 × 106 cells/ml in a 48-well flat-bottom plate in AIM V medium (Gibco/Invitrogen Corp., Grand Island, NY), supplemented with 10% FCS, and stimulated overnight with live MV, Edmonston strain (American Type Culture Collection), at 103 TCID50s/100 μl. Positive-control stimulation was performed with 10 ng/ml phorbol 12-myristate 13-acetate and 1 μg/ml ionomycin (Sigma, St. Louis, MO).
Following overnight incubation, cells were transferred to a 96-well ELISPOT plate coated with antibody to rhesus IFN-γ (U-Cytech BV, Utrecht, The Netherlands) and developed as described by the manufacturer. Spot-forming cells (SFC) were counted under a dissecting microscope, and the numbers of spots in duplicate wells were averaged. A positive result was at least 10 spots per well and equal to or more than the mean plus 2 standard deviations of the medium control. The spot number in medium control wells was subtracted from the experimental spot count, and the number of SFC was adjusted to 106 PBMCs. Statistical analysis of the data was performed using one-way analysis of variance (ANOVA) tests with the software JMP7 (JMP, Cary, NC).
RESULTS
Identification of an H protein amino acid substitution interfering with SLAM-dependent fusion support while completely preserving EpR-dependent function.
The H protein amino acid substitutions Y529A, D530A, R533A, Y553A (36), and I194S (23) were originally identified as changes interfering with SLAM-dependent fusion while preserving CD46-dependent fusion. Here, we introduced these substitutions individually in the H protein of the wild-type prototypic virulent strain IC-B, a strain of MV unable to use CD46 as a receptor (34).
To assess the fusion support efficiency of the different mutant H proteins, we cotransfected the H-expressing plasmids with a plasmid coding for the F protein of the IC-B strain in cells expressing either SLAM (Vero/hSLAM) or EpR (H358). Figure 1 (top panel) indicates that all five mutants completely lost the SLAM-dependent fusion support function, as expected. In contrast, mutants had different levels of fusion activity on H358 cells (Fig. 1, center panel): the R533A mutant retained wild-type levels of fusion efficiency; the I194S mutant showed a slight reduction in EpR-dependent fusion support; and the Y529A, D530A, and Y553A mutants significantly or completely lost EpR-dependent fusion support. Since immunoblot analyses indicated that levels of expression for H proteins with Y529A and D530A mutations were lower than the level of the parental wild-type IC-B H protein (Fig. 1, bottom panel), we excluded these and the Y553A mutants from further analysis.
Generation of a SLAM-blind MV in the wild-type IC-B genetic background.
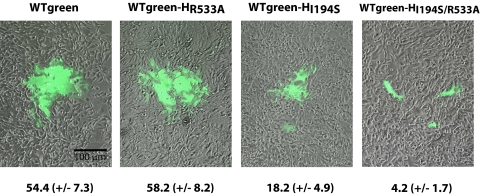
In order to generate a SLAM-blind MV, we focused on the two most promising amino acid substitutions, R533A and I194S. Substitution of arginine (codon AGG at position 533, but also CGN) to alanine (GCN) requires two nucleotide changes, whereas a change of isoleucine to serine is a single nucleotide mutation. Mutations coding for the two amino acid substitutions were imported individually and in combination in the genome of the GFP-expressing recombinant MV strain IC323 (18). Both single mutants and the double mutant were rescued by overlaying 293-3-46 MV rescue cells on H358 cells (26) and were amplified on H358 cells.
To analyze EpR-dependent fusion support efficiency of these three viruses compared to that of the isogenic wild-type virus, H358 cells were infected at a low MOI, and the number of nuclei per syncytium was counted 2 days postinoculation. The parental wild-type and the isogenic R533A mutant (Fig. 2, first and second panels, respectively) had similar fusion capacities, with an average of 54 and 58 nuclei per syncytia, respectively (numbers below the panels). Syncytia from the I194S mutant had an average of 18 nuclei (Fig. 2, third panel), whereas the double mutant I194S/R533A was minimally fusogenic, with 4 nuclei per syncytium (Fig. 2, fourth panel). We thus operated with the R533A mutant (WTgreen-HSLAMblind) for all subsequent experiments. The growth of this mutant and WTgreen was compared in H358 cells: both viruses reached similar peak titers of 2 × 104 TCID50s/ml at 60 h postinfection. Titers of WTgreen were also determined on Vero/hSLAM cells, where the virus reached a titer 10 times higher.
FIG. 2.
Extent of cell fusion elicited by four different SLAM-blind viruses on EpR-expressing H358 cells 2 days after infection. Phase-contrast pictures of the cells were overlaid with fluorescence microscopy images. Panels show representative pictures. Bottom numbers indicate the number of nuclei per syncytium (averages of nuclei count in 20 syncytia per virus); standard deviations are indicated in parenthesis.
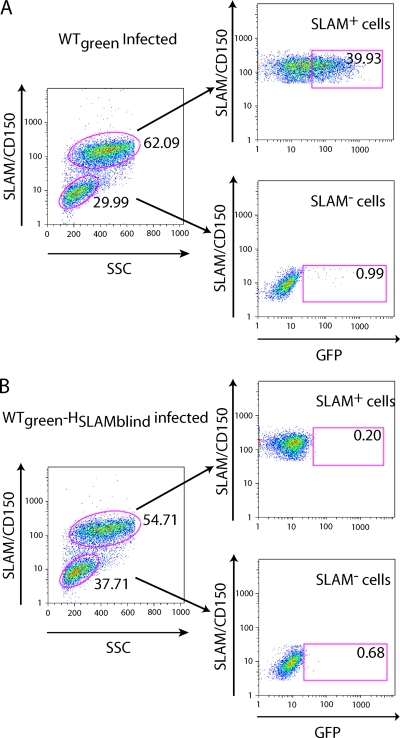
WTgreen-HSLAMblind infects cells through SLAM about 40 times less efficiently than the isogenic wild-type virus.
To assess the specificity of the SLAM-blind virus, we mixed two cell types, Vero/hSLAM cells, which express SLAM, and Vero cells, which do not. We then infected this cell mixture with either WTgreen or WTgreen-HSLAMblind at the same MOI and allowed the infections to develop for 12 h. Cells were then stained for SLAM expression and analyzed by flow cytometry to measure the percentage of GFP-expressing cells in the two populations. WTgreen infected about 40% of the SLAM-expressing cells (Fig. 3A, top right), and about 1% of SLAM-negative cells (Fig. 3A, bottom right). In contrast, WTgreen-HSLAMblind infected SLAM-positive and SLAM-negative cells at the background level, below 1% (Fig. 3B, right panels). Thus, WTgreen-HSLAMblind infects SLAM-expressing cells at least 40 times less efficiently than the isogenic WT.
FIG. 3.
Receptor specificity of WTgreen-HSLAMblind. Two cell populations, Vero/hSLAM expressing SLAM or Vero cells, were mixed and infected with either WTgreen (A) or WTgreen-HSLAMblind (B). After 12 h the mixed cells were analyzed by flow cytometry; an anti-SLAM antibody was used to quantify SLAM expression (vertical axis). In the left panels side scatter analysis (SSC) was used to differentiate the two cell populations (horizontal axis); in the right panels GFP expression analysis was used to identify infected cells (horizontal axis). Percentages report the number of cells in the red gate divided by the total number of cells in the plot, multiplied by 100.
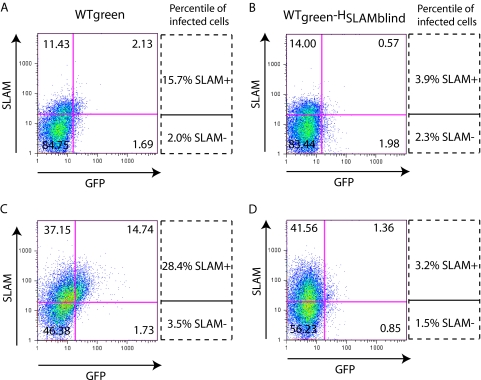
WTgreen-HSLAMblind does not efficiently infect primary T lymphocytes.
To assess the specificity of infection of the SLAM-blind virus in human PBMCs, these cells were infected, with or without stimulation by PHA, which preferentially activates T lymphocytes, and analyzed by flow cytometry to measure SLAM expression and GFP expression, a marker of infection. Figure 4 illustrates the specificity of infection of CD3 T cells. Without PHA stimulation, WTgreen infects about 16% of the SLAM-positive and 2% of the SLAM-negative CD3-positive cells (Fig. 4A). With PHA stimulation, the percentage of infected cells approximately doubled in both SLAM-positive and -negative cells, but an approximately 8-to-1 infection ratio remained constant (Fig. 4C). In contrast, WTgreen-HSLAMblind infected SLAM-positive and SLAM-negative CD3 cells with low efficiency and independently of PHA stimulation (Fig. 4B and Fig. D). Altogether, these data indicate that wild-type virus can enter T lymphocytes through a receptor other than SLAM but only with low efficiency.
FIG. 4.
WTgreen and WTgreen-HSLAMblind infection of CD3-positive human PBMCs. Human PBMCs, either nonactivated (A and B) or PHA activated (C and D), were infected with WTgreen (A and C) or WTgreen-HSLAMblind (B and D), and the level of infected SLAM-positive and SLAM-negative CD3+ T cells was determined by FACS analysis. The vertical axis shows SLAM expression levels. The threshold of positive SLAM expression was set using the corresponding isotype control. The horizontal axis shows GFP fluorescence. The percentage of infected cells was calculated by dividing the number of GFP-expressing cells (right quadrants, upper or lower) by the total number of cells in the corresponding pairs of upper or lower quadrants, respectively.
WT-HSLAMblind is attenuated in rhesus monkeys.
Our model of MV pathogenesis postulates that primarily infected lymphatic cells carry MV to the respiratory epithelium and predicts that a SLAM-blind MV would fail to spread efficiently and be attenuated (18). To test this model, we infected rhesus monkeys, a primate species that develops the clinical signs of measles when infected with wild-type MV (20, 42). Since the wild-type virus IC-B that we previously used to establish standard values for viremia and clinical signs (7) does not express GFP, we generated an isogenic SLAM-blind virus not expressing GFP and named it WT-HSLAMblind. We inoculated six rhesus monkeys intranasally with this virus using the same procedure previously established for the isogenic WT virus and followed the development of clinical signs over 28 days.
Table 1 indicates that the six monkeys infected with WT-HSLAMblind developed no clinical signs of measles, including skin rash or anorexia. Viremia was detected in the PBMCs of only one macaque inoculated with WT-HSLAMblind early after inoculation (day 3) and at very low titers (101.38) (Table 1). At later time points (days 7 and 14 postinfection) no virus was detected. Absence of clinical signs in all six infected animals and low-level viremia in only one animal very early after inoculation indicate that WT-HSLAMblind is attenuated in rhesus monkeys.
TABLE 1.
Clinical signs and virulence of SLAM-blind MV in rhesus monkeys
| Virus strain | No. of monkeys with clinical symptom/no. of monkeys tested |
Viremia (TCID50/106 PBMCs) at: |
|||
|---|---|---|---|---|---|
| Rash | Anorexia | Day 3 | Day 7 | Day 14 | |
| WT-HSLAMblind | 0/5a | 0/5a | <1c | <1 | <1 |
| 0/1b | 0/1b | 101.38 | <1 | <1 | |
| WT | 2/6 | 3/6 | NDd | 103.76 | 101.08 |
Monkeys 099, 418, 426, 583, and 609.
Monkey 621.
The lower detection limit was 1 TCID50/106 PBMCs.
ND, not determined.
WT-HSLAMblind elicits robust adaptive immune responses.
To assess the strength of the adaptive immune responses elicited in rhesus monkeys by WT-HSLAMblind, we titrated anti-MV neutralizing antibodies in serum, and measured the number of MV-specific IFN-γ-secreting T cells. Figure 5A indicates that at 14 days postinoculation, the neutralizing antibody titers in hosts infected with WT-HSLAMblind ranged from 1:32 to 1:128. This is about half the range of the titers measured in hosts infected with WT virus (range, 1:72 to 1:176; the difference between the two groups is statistically significant, with a P value of 0.04). At day 28, the mean titers of neutralizing antibodies in hosts infected with WT-HSLAMblind were 1:152, and in hosts infected with WT virus 1:576, there was again a statistically significant difference (P = 0.002). Thus, WT-HSLAMblind elicited a humoral immune response with neutralizing antibody titers about four times lower than those of the isogenic WT virus 1 month after infection.
FIG. 5.
Analysis of the humoral and cellular immune responses elicited by WT-HSLAMblind. (A) Neutralizing antibody response of monkeys infected with WT or WT-HSLAMblind (SLAMb). Serum obtained before or 14 or 28 days postinoculation was assayed for MV neutralization. The vertical axis shows the reciprocals of the neutralization titers. Each dot represents an animal, and the short horizontal bar indicates the mean of the group. The interrupted line represents the limit of detection; all preinoculation sera had titers below this value. (B) MV-specific IFN-γ-secreting cells in monkeys infected with WT or WT-HSLAMblind. PBMCs were obtained 28 or 90 days postinoculation and stimulated with live MV Edmonston strain, and the number of spot-forming cells per 106 PBMCs was measured with an IFN-γ-specific ELISPOT assay. Each dot represents the number of spot-forming cells for an animal, and the horizontal bar indicates the mean of the group.
To assess the strength of the cell-mediated immune response, MV-specific IFN-γ-secreting T cells in PBMCs obtained at 1 or 3 months postinfection were counted with an ELISPOT assay (Fig. 5B). All animals infected with the WT developed a specific MV response with means of 57 and 74 SFC/106 PBMCs at days 28 and 90, respectively. Animals infected with WT-HSLAMblind developed a specific MV response with means of 128 and 165 SFC/106 PBMCs at days 28 and 90, respectively. Differences between the experimental groups were not statistically significant at day 28 (P = 0.14) but were significant at day 90 (P = 0.045). These results show that, despite attenuation, the WT-HSLAMblind virus elicits levels of cellular immunity as high as or greater than those induced by the isogenic WT strain.
DISCUSSION
SLAM-independent entry.
We generated a selectively SLAM-blind MV differing from the fully virulent wild-type IC-B strain by a single arginine-to-alanine substitution at amino acid 533 of the H protein. This virus entered SLAM-expressing Vero cells about 40 times less efficiently than the isogenic wild-type strain. On the other hand, both the SLAM-blind and the wild-type strains entered Vero cells not expressing SLAM with low efficiency and airway epithelial cells expressing EpR with high efficiency. Both the wild-type and the SLAM-blind virus entered SLAM-negative primary T lymphocytes 5 to 10 times less efficiently than the wild-type virus entered SLAM-positive primary T lymphocytes. An interpretation of these findings is that SLAM-independent wild-type MV entry accounts for a small but significant fraction of PBMC infection.
The alternative explanation for these observations is that SLAM may be expressed at levels undetectable with antibodies but sufficient to sustain efficient viral entry. Indeed, SLAM is downregulated from the cell surface upon MV infection (9, 40), and for wild-type MV infection our data do not exclude this possibility. However, the argument that the expression level is minimal but sufficient for entry is unlikely to explain cell entry of the SLAM-blind virus because the interaction of this virus with SLAM is very weak. We have measured the binding affinity of the R533A H protein mutant ectodomain and the SLAM ectodomain by Biacore analysis and found it to be close to 100 μM, or about 1,000 times lower than the 80 nM affinity we measured for the isogenic H protein with an arginine at position 533 (23; also C. Navaratnarajah and R. Cattaneo, unpublished) (these measurements were done in the NSe vaccine lineage H protein background). Since this weak interaction is unlikely to support cell entry through SLAM, we think that the SLAM-blind virus uses another unidentified lymphocytic protein as a receptor. Analogously, wild-type MV strains may also enter human PBMCs through this unidentified receptor. Indications for the existence of alternative MV receptors have been obtained in other cellular systems (14, 30).
Even if SLAM-independent entry in PBMCs occurs, it does not cause disease: the SLAM-blind virus does not spread efficiently in rhesus monkeys. One week after inoculation, about 1 in 150 PBMCs were infected in the six monkeys inoculated with wild-type MV. In contrast, infectivity was detected only transiently at day 3 postinfection in a single host inoculated with the SLAM-blind virus. Virus titers in this monkey were just above the detection level of 1 in 100,000 cells and about 1,000 times lower than the titers in the control group. MV entry through SLAM, a signaling protein, may prime the host cell to support efficient viral replication, whereas entry though another protein may not. It was previously observed that replication of the MV vaccine Edmonston in certain cell types in tonsillar tissue was very inefficient, suggesting the existence of postentry blocks of viral replication that are relaxed only when SLAM sustains viral entry (5).
We are not in the position of analyzing the sequence of the SLAM-blind virus after monkey passage because our attempts to reisolate this virus were not successful. Initial titer determination from PBMCs of monkeys relied on overlaying cells on EpR-expressing cells, fixation, and staining with an MV-specific antibody, which resulted in virus inactivation. Titers were just above background, and subsequent attempts to isolate virus from frozen PBMC aliquots repeatedly failed. Since the virus also failed to grow when SLAM-expressing cells were used to overlay PBMCs, we think that it was not a revertant.
Attenuation by receptor detargeting and vaccine development.
No clinical evidence of disease was documented in the monkeys infected with the SLAM-blind MV. These findings prove formally that efficient SLAM recognition is necessary for MV virulence and are consistent with a mechanism of pathogenesis depending on efficient MV spread in SLAM-expressing cells and lymphatic tissue before infection of airway epithelial cells (18, 32).
A pathogenesis model postulating immune cell infection before respiratory epithelial cell infection has also been proposed for canine distemper virus (CDV), the MV-homologue virus that infects small carnivores (37). Indeed, a SLAM-blind CDV was generated and found to be completely attenuated in ferrets, a natural host (39). However, this SLAM-blind virus was based on an H protein in which six amino acid changes had been introduced, including four with slightly negative effects also on a SLAM-independent fusion support function (38). Therefore, attenuation of this CDV may not have been exclusively SLAM specific. In contrast, one single amino acid change was introduced in MV H that was completely neutral to its SLAM-independent fusion support function. We note that since two nucleotide mutations had to be introduced to change an arginine to alanine, two mutations would be necessary to generate a true revertant, and the probability of this occurring in the early phases or during replication is low. Consistently, in another monkey infection study based on recombinant MV with two mutations, no revertants were selected in 12 hosts (7).
These facts and the observation that detargeting from SLAM-dependent entry results in significant attenuation while still allowing a strong immune response suggest the possibility of using SLAM-blind viruses as vaccines. In particular, 1 month after inoculation the neutralizing antibody response and the number of IFN-γ-secreting cells specific for the SLAM-blind virus were slightly lower than or equivalent to the responses against the wild-type virus, respectively. However, 3 months after inoculation the number of virus-specific IFN-γ-secreting cells was significantly higher in hosts infected with the SLAM-blind MV than in hosts infected with the isogenic wild-type strain. It is possible that this late, stronger response reflects lack of immune suppression of hosts infected with the SLAM-blind virus, which implies that this virus may be an effective vaccine. In this perspective, it is interesting that the neutralizing antibody response, the numbers of virus-specific IFN-γ-secreting cells, and the levels of viremia are comparable between monkeys infected intranasally with the SLAM-blind virus and those inoculated subcutaneously with a vaccine MV (28).
Vectored MVs are currently being developed based on infectious genomic cDNAs of the traditional MV vaccine strain Edmonston, which was derived from a pathogenic wild-type precursor by repeated passages on mammalian and avian cell lines (17). These vectored MVs include those for divalent vaccination against MV and hepatitis B virus (27, 28), MV and HIV/simian immunodeficiency virus (SIV) (13, 19, 43), or against other important pathogens (1).
The Edmonston strain attenuation process resulted in selection of a few dozen mutations distributed in all the MV genes. On the other hand, we have started a systematic effort to characterize the effects of a few targeted mutations on virulence and the adaptive immune response of monkeys. These mutations include the mutation of arginine to alanine at H protein position 533 (SLAM-blind virus), other H protein mutations that ablate the EpR interaction (18), ablation of expression of the V and C host control proteins (7), and selective inactivation of the interaction with STAT1 (P. Devaux et al., personal communication). Thus, the foundations for rational engineering of vaccines with desirable attenuation characteristics through combinatorial genetics are being laid. It is now important to assess whether a SLAM-blind MV expressing foreign antigen can elicit protective immunity against other pathogens in vivo.
Acknowledgments
We thank P. Devaux, C. Navaratnarajah, and V. von Messling for insightful comments.
This work was supported by NIH grant R01 AI063476. J. R.-D.V. is a scholar of the National Researcher System, CONACyT (Mexico).
Footnotes
Published ahead of print on 13 January 2010.
REFERENCES
- 1.Billeter, M. A., H. Y. Naim, and S. A. Udem. 2009. Reverse genetics of measles virus and resulting multivalent recombinant vaccines: applications of recombinant measles viruses. Curr. Top. Microbiol. Immunol. 329:129-162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cattaneo, R., and M. B. Mc Chesney. 2008. Measles virus, p. 285-291. In B. Mahy and M. Van Regenmortel (ed.), In Encyclopedia of virology, 3rd ed., vol. 3. Academic Press, San Diego, CA. [Google Scholar]
- 3.Cattaneo, R., and J. K. Rose. 1993. Cell fusion by the envelope glycoproteins of persistent measles viruses which caused lethal human brain disease. J. Virol. 67:1493-1502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cocks, B. G., C. C. Chang, J. M. Carballido, H. Yssel, J. E. de Vries, and G. Aversa. 1995. A novel receptor involved in T-cell activation. Nature 376:260-263. [DOI] [PubMed] [Google Scholar]
- 5.Condack, C., J. C. Grivel, P. Devaux, L. Margolis, and R. Cattaneo. 2007. Measles virus vaccine attenuation: suboptimal infection of lymphatic tissue and tropism alteration. J. Infect. Dis. 196:541-549. [DOI] [PubMed] [Google Scholar]
- 6.de Swart, R. L., M. Ludlow, L. de Witte, Y. Yanagi, G. van Amerongen, S. McQuaid, S. Yuksel, T. B. H. Geijtenbeek, W. P. Duprex, and A. D. M. E. Osterhaus. 2007. Predominant infection of CD150+ lymphocytes and dendritic cells during measles virus infection of macaques. PLoS Pathogens. 3:1771-1781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Devaux, P., G. Hodge, M. B. McChesney, and R. Cattaneo. 2008. Attenuation of V- or C-defective measles viruses: infection control by the inflammatory and interferon responses of rhesus monkeys. J. Virol. 82:5359-5367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dorig, R. E., A. Marcil, A. Chopra, and C. D. Richardson. 1993. The human CD46 molecule is a receptor for measles virus (Edmonston strain). Cell 75:295-305. [DOI] [PubMed] [Google Scholar]
- 9.Erlenhoefer, C., W. J. Wurzer, S. Loffler, S. Schneider-Schaulies, V. ter Meulen, and J. Schneider-Schaulies. 2001. CD150 (SLAM) is a receptor for measles virus but is not involved in viral contact-mediated proliferation inhibition. J. Virol. 75:4499-4505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Erlenhofer, C., W. P. Duprex, B. K. Rima, V. ter Meulen, and J. Schneider-Schaulies. 2002. Analysis of receptor (CD46, CD150) usage by measles virus. J. Gen. Virol. 83:1431-1436. [DOI] [PubMed] [Google Scholar]
- 11.Ferreira, C. S. A., M. Frenzke, V. H. J. Leonard, G. G. Welstead, C. D. Richardson, and R. Cattaneo. 2009. Measles virus infection of alveolar macrophages and dendritic cells precedes spread to lymphatic organs in transgenic mice expressing human signaling lymphocytic activation molecule (SLAM, CD150). J. Virol. doi: 10.1128/JVI.01559-01509. [DOI] [PMC free article] [PubMed]
- 12.Griffin, D. E. 2007. Measles virus, p. 1551-1585. In D. M. Knipe, P. M. Howley, D. E. Griffin, R. A. Lamb, M. A. Martin, B. Roizman, and S. E. Straus (ed.), Fields virology, 5th ed. Lippincott Williams & Wilkins, Philadelphia, PA.
- 13.Guerbois, M., A. Moris, C. Combredet, V. Najburg, C. Ruffie, M. Fevrier, N. Cayet, S. Brandler, O. Schwartz, and F. Tangy. 2009. Live attenuated measles vaccine expressing HIV-1 Gag virus like particles covered with gp160DeltaV1V2 is strongly immunogenic. Virology 388:191-203. [DOI] [PubMed] [Google Scholar]
- 14.Hashimoto, K., N. Ono, H. Tatsuo, H. Minagawa, M. Takeda, K. Takeuchi, and Y. Yanagi. 2002. SLAM (CD150)-independent measles virus entry as revealed by recombinant virus expressing green fluorescent protein. J. Virol. 76:6743-6749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hsu, E. C., C. Iorio, F. Sarangi, A. A. Khine, and C. D. Richardson. 2001. CDw150(SLAM) is a receptor for a lymphotropic strain of measles virus and may account for the immunosuppressive properties of this virus. Virology 279:9-21. [DOI] [PubMed] [Google Scholar]
- 16.Kärber, G. 1931. Beitrag zur kollektiven Behandlung pharmakologischer Reihenversuche. Arch. Exp. Pathol. Pharmakol. 162:480-483. [Google Scholar]
- 17.Katz, S. L. 2009. John F. Enders and measles virus vaccine—a reminiscence. Curr. Top. Microbiol. Immunol. 329:3-11. [DOI] [PubMed] [Google Scholar]
- 18.Leonard, V. H. J., P. L. Sinn, G. Hodge, T. Miest, P. Devaux, N. Oezguen, W. Braun, P. B. McCray, Jr., M. B. McChesney, and R. Cattaneo. 2008. Measles virus blind to its epithelial cell receptor remains virulent in rhesus monkeys but cannot cross the airway epithelium and is not shed. J. Clin. Invest. 118:2448-2458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lorin, C., L. Mollet, F. Delebecque, C. Combredet, B. Hurtrel, P. Charneau, M. Brahic, and F. Tangy. 2004. A single injection of recombinant measles virus vaccines expressing human immunodeficiency virus (HIV) type 1 clade B envelope glycoproteins induces neutralizing antibodies and cellular immune responses to HIV. J. Virol. 78:146-157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McChesney, M. B., C. J. Miller, P. A. Rota, Y. D. Zhu, L. Antipa, N. W. Lerche, R. Ahmed, and W. J. Bellini. 1997. Experimental measles. I. Pathogenesis in the normal and the immunized host. Virology 233:74-84. [DOI] [PubMed] [Google Scholar]
- 21.Naniche, D., G. Varior-Krishnan, F. Cervoni, T. F. Wild, B. Rossi, C. Rabourdin-Combe, and D. Gerlier. 1993. Human membrane cofactor protein (CD46) acts as a cellular receptor for measles virus. J. Virol. 67:6025-6032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Navaratnarajah, C. K., V. H. Leonard, and R. Cattaneo. 2009. Measles virus glycoprotein complex assembly, receptor attachment, and cell entry. Curr. Top. Microbiol. Immunol. 329:59-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Navaratnarajah, C. K., S. Vongpunsawad, N. Oezguen, T. Stehle, W. Braun, T. Hashiguchi, K. Maenaka, Y. Yanagi, and R. Cattaneo. 2008. Dynamic interaction of the measles virus hemagglutinin with its receptor signaling lymphocytic activation molecule (SLAM, CD150). J. Biol. Chem. 283:11763-11771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ono, N., H. Tatsuo, Y. Hidaka, T. Aoki, H. Minagawa, and Y. Yanagi. 2001. Measles viruses on throat swabs from measles patients use signaling lymphocytic activation molecule (CDw150) but not CD46 as a cellular receptor. J. Virol. 75:4399-4401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Premenko-Lanier, M., P. A. Rota, G. H. Rhodes, W. J. Bellini, and M. B. McChesney. 2004. Protection against challenge with measles virus (MV) in infant macaques by an MV DNA vaccine administered in the presence of neutralizing antibody. J. Infect. Dis. 189:2064-2071. [DOI] [PubMed] [Google Scholar]
- 26.Radecke, F., P. Spielhofer, H. Schneider, K. Kaelin, M. Huber, C. Dotsch, G. Christiansen, and M. A. Billeter. 1995. Rescue of measles viruses from cloned DNA. EMBO J. 14:5773-5784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Reyes-del Valle, J., G. Hodge, M. B. McChesney, and R. Cattaneo. 2009. Protective anti-hepatitis B virus responses in rhesus monkeys primed with a vectored measles virus and boosted with a single dose of hepatitis B surface antigen. J. Virol. 83:9013-9017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Reyes del Valle, J., P. Devaux, G. Hodge, N. J. Wegner, M. B. McChesney, and R. Cattaneo. 2007. A vectored measles virus induces hepatitis B surface antigen antibodies while protecting macaques against measles virus challenge. J. Virol. 81:10597-10605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schneider-Schaulies, S., and J. Schneider-Schaulies. 2009. Measles virus-induced immunosuppression. Curr. Top. Microbiol. Immunol. 330:243-269. [DOI] [PubMed] [Google Scholar]
- 30.Shingai, M., M. Ayata, H. Ishida, I. Matsunaga, Y. Katayama, T. Seya, H. Tatsuo, Y. Yanagi, and H. Ogura. 2003. Receptor use by vesicular stomatitis virus pseudotypes with glycoproteins of defective variants of measles virus isolated from brains of patients with subacute sclerosing panencephalitis. J. Gen. Virol. 84:2133-2143. [DOI] [PubMed] [Google Scholar]
- 31.Sidorenko, S. P., and E. A. Clark. 1993. Characterization of a cell surface glycoprotein IPO-3, expressed on activated human B and T lymphocytes. J. Immunol. 151:4614-4624. [PubMed] [Google Scholar]
- 32.Takeda, M. 2008. Measles virus breaks through epithelial cell barriers to achieve transmission. J. Clin. Invest. 118:2386-2389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Takeda, M., M. Tahara, T. Hashiguchi, T. A. Sato, F. Jinnouchi, S. Ueki, S. Ohno, and Y. Yanagi. 2007. A human lung carcinoma cell line supports efficient measles virus growth and syncytium formation via SLAM- and CD46-independent mechanism. J. Virol. 81:12091-12096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Takeda, M., K. Takeuchi, N. Miyajima, F. Kobune, Y. Ami, N. Nagata, Y. Suzaki, Y. Nagai, and M. Tashiro. 2000. Recovery of pathogenic measles virus from cloned cDNA. J. Virol. 74:6643-6647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tatsuo, H., N. Ono, K. Tanaka, and Y. Yanagi. 2000. SLAM (CDw150) is a cellular receptor for measles virus. Nature 406:893-897. [DOI] [PubMed] [Google Scholar]
- 36.Vongpunsawad, S., N. Oezgun, W. Braun, and R. Cattaneo. 2004. Selectively receptor-blind measles viruses: identification of residues necessary for SLAM- or CD46-induced fusion and their localization on a new hemagglutinin structural model. J. Virol. 78:302-313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.von Messling, V., D. Milosevic, and R. Cattaneo. 2004. Tropism illuminated: lymphocyte-based pathways blazed by lethal morbillivirus through the host immune system. Proc. Natl. Acad. Sci. U. S. A. 101:14216-14221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.von Messling, V., N. Oezguen, Q. Zheng, S. Vongpunsawad, W. Braun, and R. Cattaneo. 2005. Nearby clusters of hemagglutinin residues sustain SLAM-dependent canine distemper virus entry in peripheral blood mononuclear cells. J. Virol. 79:5857-5862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.von Messling, V., N. Svitek, and R. Cattaneo. 2006. Receptor (SLAM [CD150]) recognition and the V protein sustain swift lymphocyte-based invasion of mucosal tissue and lymphatic organs by a morbillivirus. J. Virol. 80:6084-6092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Welstead, G. G., E. C. Hsu, C. Iorio, S. Bolotin, and C. D. Richardson. 2004. Mechanism of CD150 (SLAM) down regulation from the host cell surface by measles virus hemagglutinin protein. J. Virol. 78:9666-9674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yanagi, Y., M. Takeda, and S. Ohno. 2006. Measles virus: cellular receptors, tropism and pathogenesis. J. Gen. Virol. 87:2767-2779. [DOI] [PubMed] [Google Scholar]
- 42.Zhu, Y. D., J. Heath, J. Collins, T. Greene, L. Antipa, P. Rota, W. Bellini, and M. McChesney. 1997. Experimental measles. II. Infection and immunity in the rhesus macaque. Virology 233:85-92. [DOI] [PubMed] [Google Scholar]
- 43.Zuniga, A., Z. Wang, M. Liniger, L. Hangartner, M. Caballero, J. Pavlovic, P. Wild, J. F. Viret, R. Glueck, M. A. Billeter, and H. Y. Naim. 2007. Attenuated measles virus as a vaccine vector. Vaccine 25:2974-2983. [DOI] [PMC free article] [PubMed] [Google Scholar]