Abstract
The epithelium plays a key role in the spread of Lassa virus. Transmission from rodents to humans occurs mainly via inhalation or ingestion of droplets, dust, or food contaminated with rodent urine. Here, we investigated Lassa virus infection in cultured epithelial cells and subsequent release of progeny viruses. We show that Lassa virus enters polarized Madin-Darby canine kidney (MDCK) cells mainly via the basolateral route, consistent with the basolateral localization of the cellular Lassa virus receptor α-dystroglycan. In contrast, progeny virus was efficiently released from the apical cell surface. Further, we determined the roles of the glycoprotein, matrix protein, and nucleoprotein in directed release of nascent virus. To do this, a virus-like-particle assay was developed in polarized MDCK cells based on the finding that, when expressed individually, both the glycoprotein GP and matrix protein Z form virus-like particles. We show that GP determines the apical release of Lassa virus from epithelial cells, presumably by recruiting the matrix protein Z to the site of virus assembly, which is in turn essential for nucleocapsid incorporation into virions.
Lassa virus (LASV), a member of the family Arenaviridae, is a highly pathogenic agent causing hemorrhagic fever as a severe clinical manifestation. Arenaviruses are currently classified into more than 20 species, which are divided into the Old World and New World virus complexes (10). The Old World group includes the prototype lymphocytic choriomeningitis virus (LCMV) and the highly human-pathogenic viruses LASV and Lujo virus, as well as the nonpathogenic Ippy, Mobala, Mopeia, and Kodoko viruses (7, 21, 36). The New World virus complex contains among others, the hemorrhagic fever-associated Junín, Machupo, Guanarito, and Sabiá viruses and the recently discovered Chapare virus (14).
With the exception of the New World virus Tacaribe virus, which was isolated from fruit bats, all arenaviruses have specific rodent species as their natural reservoirs. Rodents of the Mastomys natalensis species complex were identified as the natural host of LASV in certain countries in West Africa, including Sierra Leone, Nigeria, Guinea, and Liberia (26, 35, 49). An estimated 100,000 to 300,000 human LASV infections occur annually, of which approximately 30% result in illness, which can range from mild, flu-like symptoms to fulminant hemorrhagic fever with a mortality rate of about 16% of hospitalized cases (47, 48). Due to the severe or even fatal outcome of disease, unavailability of vaccine prophylaxis, and inadequate therapeutic treatment options, LASV is classified as a biosafety level 4 agent.
The primary transmission route of LASV from its host to humans is by direct exposure to virus-containing urine, which may occur via the respiratory tract, through inhalation of infected particulates, or via ingestion of contaminated food (62). Moreover, hunting and preparation for consumption of rodents have also been identified as possible risk factors for rodent-to-human transmission of LASV (67). LASV is spread from human-to-human by contact with infectious body fluids or through nosocomial contaminations (22, 27). During the infection process, virus contacts the epithelial layers of the body and, after breaking through the epithelial tissue barrier, exploits dendritic cells for further dissemination (3, 15). It has been shown for LASV, as well as for other arenaviruses, that during the course of infection, infectious virus particles are released from epithelia into body fluids and urine (32, 45, 71).
As epithelial layers play a pivotal role not only in initial virus infection but also in release of virus progeny during the early stages of infection, virus spread within the organism and virus release for further transmission, the polarity of entry and release from polarized epithelia has been studied extensively with various viruses. Virus entry in polarized cells is correlated with the apical or basolateral localization of the responsible virus receptor (24, 34, 68). Viruses that are transmitted through aerosols or surface contact with body fluids are generally thought to enter the epithelial barrier from the apical side, whereas virus infections due to injuries or transmission from animals' bites and scratches enter epithelial cell layers from the basolateral side. Further, the spread of disease is also dependent on the directional release of the virus from epithelial cells. In general, basolateral virus budding is thought to cause systemic infections, whereas local infections are a result of viruses that are released predominantly from the apical side (69). Fitting with this model, budding of wild-type Sendai virus is restricted to the apical domain of polarized cells and causes a local respiratory infection, whereas systemic spread of a Sendai virus mutant could be attributed mainly to its bipolar virus release (66). The direction of entry and release can also be highly dependent on the type of tissue involved, as Sindbis and Semliki Forest viruses show differences in directed release in colon and thyroid gland cells (75). Similar differences in polarized virus release have also been shown for different members within a single virus family (59).
In order to understand virus dissemination within the organism, it is of interest to determine on which side viruses enter and leave polarized epithelial cell layers. Here, we present data on directional LASV invasion into polarized MDCK cell culture and demonstrate a directional release of LASV from these cells. Furthermore, we have elucidated how Lassa virus proteins interact to direct budding and release of LASV progeny from epithelial cell layers.
MATERIALS AND METHODS
Viruses and cell cultures.
Lassa virus (LASV; strain Josiah), vesicular stomatitis virus (VSV; strain Indiana), and influenza virus A/chicken/Germany/N/49 (H10N7; virus N) were used. Virus stocks were obtained by propagation of LASV in Chinese hamster ovary (CHO) cells (39), VSV in MDCK-II (Madin-Darby canine kidney cells, strain II) cells, and influenza virus in embryonated chicken eggs. Influenza virus and VSV stocks were plaque titrated, and the titers of LASV stocks were determined by 50% tissue culture infectious dose (TCID50); virus stocks were then stored at −80°C until further use. All experiments involving LASV-infected samples were performed under bio safety level 4 conditions at the Philipps University of Marburg.
MDCK-II cells were grown in minimal essential medium (MEM) (Invitrogen). Cos 7 cells (African green monkey kidney cells), Huh 7 cells (human hepatoma cell line 7), and 293 T cells (human kidney cells) were cultivated in Dulbecco's modified Eagle's medium (DMEM; Invitrogen). All cell cultures were grown under standard conditions (37°C, 5% CO2) in the presence of penicillin (100 U ml−1), streptomycin (100 μg ml−1), glutamine (2 mmol), and 10% fetal calf serum (FCS; Pan Biotech). Polarized MDCK-II cells were cultured on filters (Transwell filter devices; 2.5-cm diameter; pore sizes of 0.4 μm or 3.0 μm; Greiner) until confluence. Cell culture medium was exchanged daily until cell polarity was reached (3 to 5 days), which was measured using a Millicell-ERS volt-ohmmeter (Millipore). Independently, cell layers were analyzed for polar integrity by immunochemical staining of the tight-junction resident zonula occludens protein ZO-3.
Antibodies.
LASV glycoprotein was detected using either the monoclonal antibody, designated AC1, specific for the GP-1 subunit (kindly provided by M. C. Georges-Courbot, Unit of Biology of Viral Emerging Infections, Institute Pasteur, Lyon, France) or polyclonal antibodies raised in rabbits: α-GP-2-N, recognizing the N-terminal GP-2 ectodomain, and α-GP-2-C, detecting the cytoplasmic domain of GP-2 (38). Rabbit antisera against the LASV proteins Z and NP, designated α-Z and α-NP, respectively, were previously described (39, 63). Additional primary antibodies used included a monoclonal mouse antibody against NP (α-m-NP) (70) (kindly provided by I. S. Lukashevich, Institute of Human Virology, University of Maryland, Baltimore, MD), a rabbit VSV-G polyclonal antiserum (kindly provided by G. Herrler, Institut für Virologie, Stiftung Tierärztliche Hochschule Hannover, Germany), a chicken antibody directed against the hemagglutinin (HA) tag (Sigma-Aldrich), an antibody raised in rabbit against ZO-3 (Chemicon), and a monoclonal mouse antibody against the β subunit of dystroglycan (clone 46DAG1/8D5; Abcam). Rabbit antiserum was also raised against inactivated influenza virus (H10N7; virus N). Secondary antibodies labeled with IRDye 800 (Invitrogen) were used for immunoblotting (IB) and subsequently quantified using the Odyssey infrared quantification system (Li-Cor). Further secondary antibodies labeled with either fluorescein isothiocyanate (FITC), tetramethyl rhodamine isothiocyanate (TRITC), or cyanine dye 5 (Cy5) were used for immunofluorescence microscopy studies (IF). The following antibodies were used at the indicated dilutions: α-GP-1 (IB, 1:5,000; IF, 1:200), α-GP-2-N (immunoprecipitation [IP], 1:1,000; IB, 1:3,000; IF, 1:50), α-GP-2-C (IB, 1:5,000; IF, 1:100), α-Z (IP, 1:1,000; IB, 1:10,000; IF, 1:200), α-m-NP (IB, 1:5,000; IF, 1:200), α-NP (IP, 1:1,000; IB, 1:5,000; IF, 1:100), α-VSV-G (IB, 1:5,000), α-HA tag (IF, 1:100), α-β-dystroglycan (IF, 1:200), α-ZO-3 (IF, 1:20), and secondary antibodies (IF, 1:100; IB, 1:5,000).
Protein expression in mammalian cells.
Cells were transfected using Lipofectamine 2000 (Invitrogen) according to the manufacturer's instructions. The plasmids contained the following DNA inserts: cDNA of the LASV glycoprotein (preGP-C), preGP-C with a C-terminal HA tag (YPYDVPDYA) (GPHAtag), the matrix protein (Z), and the nucleoprotein (NP) (19, 20). For generation of MDCK-II cell lines that stably express LASV proteins in various combinations, cells were cotransfected with the selection plasmid pIG-1 at a ratio of 1:10 using Lipofectamine 2000. Cells were then cultured for 2 weeks under selective pressure in the presence of 50 μg ml−1 Geneticin (Invitrogen). Single cell clones were then selected and transferred to individual wells of a 96-well plate for further growth in selective medium. When grown to confluence, cells were transferred to larger flasks. Stable protein expression was analyzed by Western blotting. To confirm protein expression in all cells in the culture, immunofluorescence analyses were performed.
Isolation of virus-like particles (VLPs).
Cell culture medium of confluent layers of MDCK-II cells stably expressing various combinations of LASV proteins was replaced with fresh medium containing 2% FCS. After 48 h, the cell supernatants were precleared by low-speed centrifugation at 4,000 × g for 20 min. Supernatants were then layered onto a sucrose cushion (20%, wt/wt) and ultracentrifuged using either an SW32 or SW60 rotor (Beckman) at 125,000 × g or a TLA45 rotor (Beckman) at 91,000 × g for 2.5 h. Pellets from supernatants of a 75-cm2 cell culture were resuspended in 100 μl phosphate-buffered saline (PBS). The samples were used for either electron microscopic analyses, protease protection assay, immunoprecipitation, or immunoblotting.
Protease protection assay.
Protease protection assays were performed as described previously (39). Briefly, aliquots of purified VLP samples were incubated at 37°C for 30 min with either 0.1 μg μl−1 proteinase K (Fermentas) or 0.1 μg μl−1 proteinase K in the presence of 1% Triton X-100 or were left untreated. Proteinase K was inactivated by the addition of phenylmethylsulfonyl fluoride (PMSF; Serva; 1 μg μl−1 final concentration). Sample buffer was added, and aliquots were subjected to SDS-PAGE followed by immunoblotting.
Immunoprecipitation.
To study the molecular interaction of viral proteins in VLPs, we performed coimmunoprecipitation (CoIP) studies. Therefore, CoIP buffer (20 mM Tris-HCl [pH 7.4], 100 mM NaCl, 5 mM EDTA, 1% NP-40, 1 mM PMSF, and Complete protease inhibitor [one tablet in 50 ml lysis buffer; Calbiochem]) was added to purified VLPs. For immunoprecipitation from cell lysate, cells were washed in PBS and lysed in CoIP puffer. After incubation on ice for 30 min, samples were sonicated twice for 30 s each at 40 W (Branson Sonifier). Preparations were precleared by centrifugation at 20,000 × g for 30 min and incubated with protein A-Sepharose beads and primary antibodies at 4°C overnight. After several washes, precipitated proteins were analyzed by SDS-PAGE and immunoblotting.
Cell surface biotinylation.
MDCK-II cells stably expressing either the LASV glycoprotein or the VSV glycoprotein were grown on membrane filters (0.4-μm-pore-size Transwell filters) and washed twice with ice-cold PBS, and one side of each filter membrane was incubated twice for 20 min on ice with PBS containing 1 mg ml−1 sulfo-N-hydroxysuccinimido-biotin (sulfo-NHS-biotin; Pierce) while the opposite side of the membrane was incubated with 0.1 M glycine. Thereafter, cells were washed with PBS and further incubated with 0.1 M glycine for 5 min from both sides. After the cells were washed three times with PBS, filter membranes were cut out and transferred into 500 μl PBS containing 1% NP-40 and protease inhibitors as mentioned in the previous section. After incubation at 4°C for 2 h, samples were sonicated at 40 W for 2 min. Filters were removed, and cell lysates were clarified by centrifugation in a microcentrifuge at 20,000 × g at 4°C for 20 min. Biotinylated proteins present in the supernatant were bound to streptavidin-coupled Sepharose beads (Pierce) at 4°C overnight. After three washing steps, proteins were detached from beads by treatment with sample buffer (95°C, 10 min) and subjected to SDS-PAGE followed by immunoblotting using protein specific antibodies.
Virus entry and release assay in polarized cells.
MDCK-II cells were grown on Transwell filters with a pore size of 3.0 μm until a polarized phenotype was established. Cells were infected with LASV, influenza virus, or VSV at a multiplicity of infection (MOI) of 1 from either the apical or the basolateral cell surface. After infection for 1 h, cells were washed three times and further incubated in new cell culture medium containing 2% FCS. Virus samples from the upper and lower filter chambers were taken at the indicated time points after infection. Titers of LASV and VSV were determined using TCID50, while titers of influenza virus were titrated using a microplate format plaque assay with subsequent immunostaining, as described previously (46). Briefly, virus dilutions were incubated on MDCK-II cells in cell culture medium containing 2% FCS. After 5 h, cells were fixed with 4% paraformaldehyde (PFA) and permeabilized with 0.3% Triton X-100, and single infected cells were visualized using an influenza virus-specific antiserum (1:2,000) followed by incubation with a horseradish peroxidase-labeled secondary anti-rabbit antibody (Dako). Finally, cells were stained with True Blue peroxidase substrate (KPL).
Confocal immunofluorescence microscopy.
MDCK-II cell lines that stably expressed viral proteins were grown on Transwell filters (0.4-μm pore size), and Huh 7 cells that transiently expressed viral proteins were grown on glass coverslips. Cells were fixed with either methanol-acetone (1:1) at −20°C for 5 min or with 4% PFA at room temperature (RT) for 20 min. After methanol-acetone fixation, LASV-infected cells were additionally treated with 4% PFA for 48 h. Fixed cells were washed twice with PBS containing 0.2% bovine serum albumin, incubated with primary antibodies for 1 h (Huh 7 cells) or 2 h (MDCK-II cells), and subsequently stained with fluorescent dye-labeled secondary antibodies for 1 h or 2 h, respectively. After rinsing with PBS, samples were mounted with Mowiol (Hoechst). Confocal imaging was performed using a confocal Leica TCS-SP2 microscope and Leica confocal software.
Electron microscopy.
Transmission electron microscopy was performed with LASV and VLPs after fixation with 4% PFA for 48 h. Virus or VLP suspension was added to Formvar-carbon-coated copper grids and left for 10 min. After the grids were washed three times in PBS for 2 min, the samples were negatively stained with 2% phosphotungstate solution (pH 7) and visualized with a Zeiss 109 electron microscope using a charge-coupled device (CCD) camera (TRS) and the Image SP viewer software program (Sys-Prog).
RESULTS
Lassa virus preferentially enters polarized epithelium from the basolateral cell side.
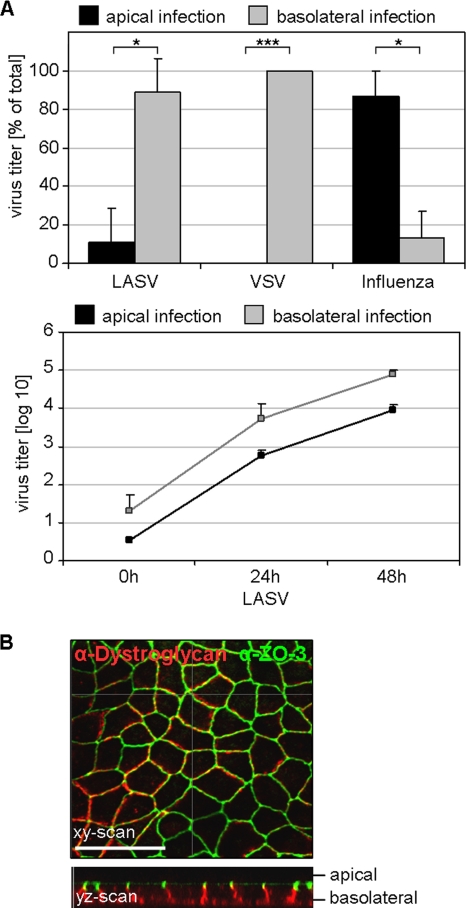
Until now there has been no detailed knowledge available regarding entry and release of LASV in polarized epithelial cells. In this study, we first wanted to determine the preferred side for virus entry in polarized cells. To this end, epithelial cells were grown on filter inserts and infected with LASV at an MOI of 1 from either the apical or basolateral cell surface. LASV titers were determined by TCID50 at indicated time points. To measure the infection efficiency for the cells on each filter, the virus titers of the apical and basolateral chambers were added together. As controls, we used influenza virus and VSV as well-established reference viruses known to enter polarized cells preferentially from the apical or basolateral side, respectively (57, 60). Analysis of viral titers revealed that entry of LASV into polarized cells occurs predominantly via the basolateral route (Fig. 1A, upper and lower panels), resulting in approximately 10-fold-greater virus yields compared to apical infection.
FIG. 1.
Entry of Lassa virus into polarized epithelial cells. (A) Polarized MDCK-II cells grown on Transwell filters with a pore size of 3.0 μm were infected with Lassa virus (LASV) at an MOI of 1 via either the apical (black) or basolateral (gray) route. After 48 h, total virus yield from the combined media of the lower and upper chambers was determined by TCID50 (upper panel). Influenza virus and VSV served as controls for apical and basolateral virus infection, respectively, and titers were determined at 8 h p.i. The virus titers of LASV at indicated time points are graphed in the lower panel. Average values were obtained from three independent experiments. The error bars denote standard deviations. ***, P < 0.001; *, P < 0.05 (t test). (B) Localization of the LASV receptor dystroglycan. MDCK-II cells grown to polarity on Transwell filters with a pore size of 0.4 μm were fixed with methanol-acetone and immunostained for expression of the LASV receptor dystroglycan (red) and the tight-junction-specific protein ZO-3 (green) and were subsequently analyzed by confocal microscopy. The optical section in the xy direction was scanned at the height of tight junctions. The yz scan shows distributions of dystroglycan and ZO-3 protein with respect to the apical and basolateral cell surfaces. The scale bar represents 20 μm.
To determine whether the observed preferential entry site of LASV at the basolateral domain correlates with an increased basolateral cell surface expression of the cellular LASV receptor, the N-terminal subunit of dystroglycan, confocal immunofluorescence microscopy was used. Images of yz scanning sections of polarized cell monolayers revealed localization of dystroglycan predominantly in the basolateral domain (Fig. 1B). This result is consistent with earlier observations showing that dystroglycan acts as a laminin receptor responsible for formation of basement membranes at the basal site of differentiated polarized cells of various tissues (17, 30), but it differs from examinations using human airway epithelia, where dystroglycan was found to be localized to both apical and basolateral membrane domains (18).
Apical release of Lassa virus from polarized epithelial cells.
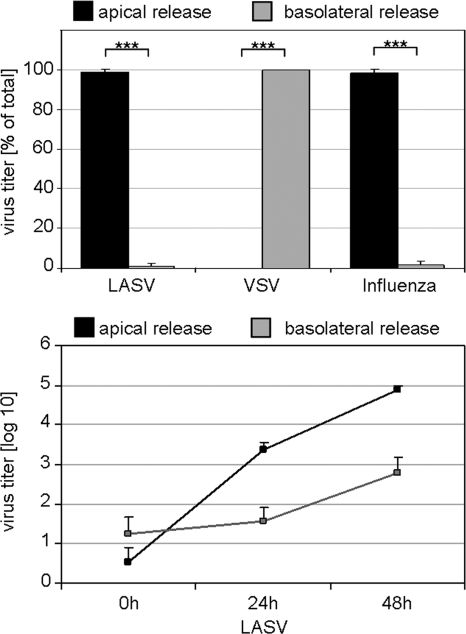
Next we wanted to determine the preferred site of LASV release. For this, confluent epithelial cell layers grown on permeable Transwell filters were infected basolaterally with LASV at an MOI of 1. At the indicated time points, infected supernatants from either the apical or the basolateral chambers were assessed for progeny virus production by TCID50. As controls, polarized epithelial cells were infected with either VSV, via the basolateral surface, or influenza virus, via the apical surface, respectively. Consistent with earlier reports (57) VSV exhibited basolateral virus release, while the release of influenza viruses occurred from the apical cell surface. The release of LASV from the apical membrane domain generated titers up to 200-fold higher than virus release into the basolateral medium (Fig. 2, upper and lower panels). It is notable, that the intact polarized epithelial cell layers survived even 72 h of LASV infection, as seen from the expression pattern of the tight-junction-associated protein ZO-3, which appears indistinguishable from that in mock-infected cells (Fig. 3A, inset). These results demonstrate that LASV is released from epithelial cells in a polarized manner through the apical domain without any significant destruction of the polarized cell layer.
FIG. 2.
Directional release of Lassa virus from polarized epithelium. MDCK-II cells grown to polarity on 3.0-μm-pore-size Transwell filters were infected with LASV from the basolateral cell surface at an MOI of 1. Virus released into the apical chambers and into the basolateral chambers were determined by TCID50 titration at 48 h after infection (upper panel). VSV and influenza virus were inoculated from the basolateral or apical side of the cell cultures, respectively, and progeny virus was titrated 8 h p.i., as described in Materials and Methods. Additionally, LASV titers from the cell culture media of the apical or basolateral chamber were measured at the indicated time points and graphed (lower panel). Statistical evaluation was performed as described for Fig. 1.
FIG. 3.
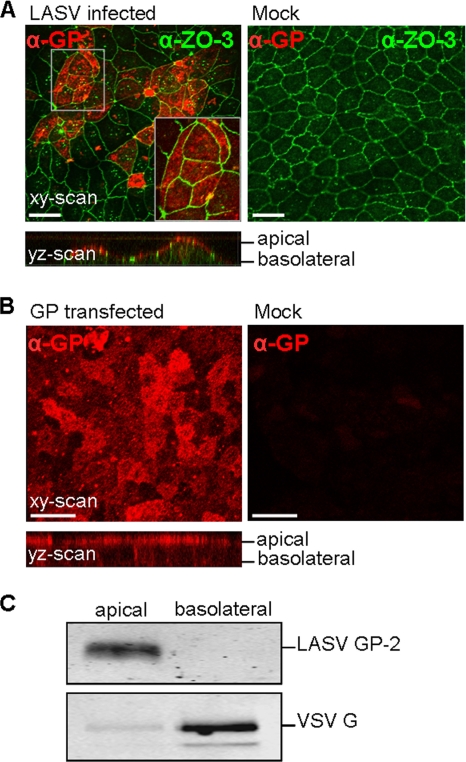
Localization of Lassa virus glycoprotein GP in polarized epithelial cells. (A) MDCK-II cells were infected with LASV at an MOI of 1 from the basolateral cell surface. At 72 h p.i. cells were fixed with methanol-acetone and subsequently treated with 4% PFA for 48 h. The LASV glycoprotein subunit GP-1 (red) and the tight-junction resident protein ZO-3 (green) were immunostained. Distributions of GP and ZO-3 were monitored by using confocal laser scanning microscopy in the xy and yz directions. The xy scan is a composite of several images from the apical and middle regions of the image stack because of the irregular height of the cells. The scale bars denote 20 μm. (B) Immunodetection of GP in a stably GP-expressing nonpermeabilized MDCK-II cell line. Cells were fixed with 4% paraformaldehyde and immunostained using an α-GP-2-N antibody (red). The scale bars denote 20 μm. (C) Proteins on the cell surface of stably LASV GP- and VSV G-expressing MDCK-II cells were labeled with sulfo-NHS-biotin on either the apical or basolateral side. After cell lysis, biotinylated proteins were precipitated using streptavidin-coupled Sepharose beads and subsequently subjected to SDS-PAGE and immunoblot analysis using α-GP-2-C or α-VSV G antiserum.
Lassa virus glycoprotein exhibits intrinsic apical localization.
It is not known which viral gene product is involved in the apical maturation of LASV. Investigations of several viruses showed that in addition to the matrix protein, the glycoprotein is also considered to be a major determinant for directed virus release from polarized epithelial cells. To investigate the possibility of an intrinsic polar distribution of GP, we compared the localization of the glycoprotein in cells infected with LASV to that in cells expressing only GP using confocal microscopy. Images of yz sections revealed an apical distribution of LASV GP in both LASV-infected and single-GP-expressing cells (Fig. 3A and B). Furthermore, cell surface localization of single-expressed GP at the apical cell surface was confirmed using cell surface biotinylation (Fig. 3C). Here, VSV glycoprotein served as a basolateral control. Taken together, these data indicate that GP transport occurs preferentially to the apical cell surface and does not require the presence of other viral proteins.
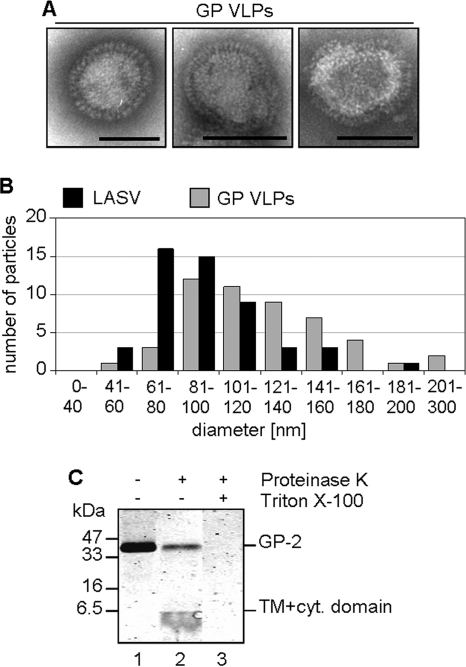
Lassa virus glycoprotein induces the formation of virus-like particles.
To examine interdependence among the viral proteins GP, Z, and NP in directional virus release, we developed an assay that uses the formation of virus-like particles (VLPs). To establish this assay, we first analyzed supernatants of virus protein-expressing cells by pelleting them through a 20% sucrose cushion and then analyzing them for the presence of GP, Z, or NP. Surprisingly, GP and Z were found to be released from cells that expressed solely GP or Z (Fig. 4C, lane 1, and 5A, lanes 1 and 7). Until now, investigations of arenavirus proteins have described only the matrix protein Z as inducing the formation of VLPs (55, 63). To further demonstrate that solitary expression of the LASV glycoprotein facilitates the formation of virus-like particles, we examined the GP-containing sedimentable material under the electron microscope after negative staining. Virus-like particles were visualized that appeared similar to Lassa virions with respect to their shape and the presence of a typical corona of LASV glycoprotein spikes (Fig. 4A). In a parallel investigation of the supernatant of mock-infected cells no spike-containing vesicles could be detected (data not shown). The size distribution of GP-induced VLPs was similar to that of LASV particles (Fig. 4B). To confirm the existence of lipid vesicles that contain LASV glycoprotein spikes, we further performed a protease protection assay. Proteinase K treatment of VLPs revealed that GP-1 and the ectodomain of GP-2 were accessible to proteinase K and therefore were degraded (Fig. 4C). Both the transmembrane and the adjacent cytoplasmic domains of GP-2 were inaccessible to proteinase K digestion and thus appeared as a small protein band below 6.5 kDa in size on the immunoblot. A small proportion of the GP molecules were inaccessible to proteinase K digestion, most likely due to VLPs that clustered together. To exclude a strict cell type-dependent release in MDCK cells, we tested several mammalian cell lines during our studies and found that the release of GP-driven VLPs was also observed in various other mammalian cells, including Huh7 cells, 293T cells, and Cos-7 cells (data not shown). GP-VLP formation was independent of the protein expression level, as we observed VLPs released from stably transfected cells, with low expression levels, as well as from transiently expressing cells containing large amounts of GP (compare Fig. 4C, lane 1, and 5C, lower panel, lane 1).
FIG. 4.
Release of spike-containing virus-like particles due to solitary expression of Lassa virus glycoprotein GP. (A) Supernatants of stably LASV glycoprotein-expressing MDCK-II cells were collected and pelleted though a 20% sucrose cushion. The pellets were resuspended, fixed with 4% PFA, adsorbed on Formvar-coated copper grids, and negatively stained with 2% phosphotungstate acid before electron microscopic analysis. Scale bars denote 100 nm. (B) Size comparisons of LASV particles and GP-VLPs were performed by electron microscopy using 50 particles each. Particles were measured from the tips of glycoprotein spikes and sorted in size fractions differing by 20 nm. (C) A protease protection assay was performed with three aliquots of a VLP suspension harvested as described for panel A. One aliquot of GP-VLP suspension was left untreated (lane 1), and the second and third aliquots were incubated with proteinase K (lanes 2 and 3). The third aliquot (lane 3) was additionally treated with Triton X-100. The proteins of all three samples were subjected to SDS-PAGE and immunoblotting. LASV glycoprotein was identified by immune detection using the α-GP-2-C antibody.
Taken together, these results demonstrate a release of GP spike-containing VLPs by cells that express only the LASV glycoprotein. Thus, it is shown for the first time that LASV proteins can form two types of virus-like particles, i.e., GP-derived VLPs and Z-induced VLPs, which are both released into the cell culture supernatant as lipid-enveloped particles independent of other viral proteins.
Characterization of virus-like particles induced by Lassa virus proteins.
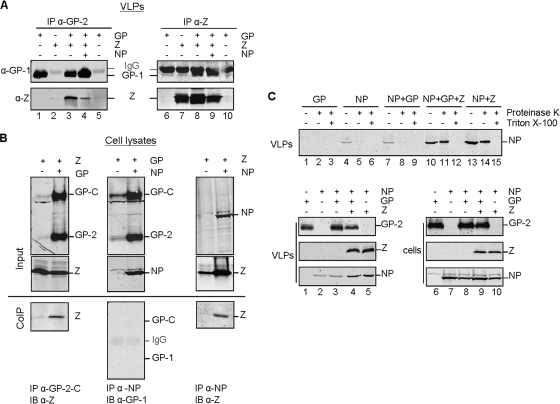
To study the influences of GP, Z and NP on directional VLP release, it is important to understand the interdependence of the three proteins. For this, we first determined whether GP and the matrix protein Z can interact and be incorporated into the same VLPs. Untagged GP and Z were stably coexpressed in mammalian cells, and the protein composition of isolated VLPs was analyzed by immunoprecipitation using antibodies specific for GP and Z, respectively. The glycoprotein GP and the matrix protein Z coprecipitated, independent of whether GP-specific or Z-specific antibodies were used (Fig. 5A, lanes 3 and 8). In triple-expression experiments NP was included but did not result in enhanced efficiency of the GP-Z interaction in VLPs (Fig. 5A, lanes 4 and 9). Rather, a decreased amount of Z was obtained by triple expression of GP, Z, and NP after precipitation with GP antibodies (Fig. 5A, lane 4), which was most likely due to the smaller amount of Z protein in the VLP preparation (Fig. 5A, lane 9). These pulldown experiments demonstrate an interaction between the matrix protein Z and GP within VLPs released from GP- and Z-expressing cells, independent of the presence of NP. The results obtained were confirmed by examining interaction of the proteins within mammalian cells following transfection with different combinations of untagged proteins and immunoprecipitation analysis. A pulldown of LASV GP resulted in coprecipitation of the matrix protein Z (Fig. 5B, right panel). Similarly, a pulldown of the matrix protein Z by NP was also possible (Fig. 5B, left panel). However, no interaction of GP and NP could be detected (Fig. 5B, middle panel).
FIG. 5.
Interaction of Lassa virus glycoprotein GP, matrix protein Z, and nucleoprotein NP. (A) VLPs from MDCK-II cells that stably express GP, Z, and NP in various combinations were obtained by pelleting cell culture supernatants through a 20% sucrose cushion. After resuspension and lysis of the VLPs, LASV proteins were coimmunoprecipitated using rabbit α-GP-2-C-specific (lanes 1 to 5) or rabbit α-Z-specific (lanes 6 to 10) antibodies. The precipitated proteins were separated by SDS-PAGE and transferred onto nitrocellulose membranes. LASV GP and Z were identified by immunoblot analyses using a mouse antibody for GP-1 detection and an α-Z rabbit serum. Weak (left panel) and strong (right panel) immunoglobulin (IgG) background bands were also detected. (B) 293 T cells were transfected with different combinations of GP, NP, and Z, as indicated. Cells were lysed, and proteins were immunoprecipitated (IP) using α-GP-2-C, α-NP, or α-Z antibodies. Precipitated proteins (CoIP) as well as cell lysates (Input) were separated by SDS-PAGE. Precipitated proteins were visualized by immunoblotting (IB) using mouse α-GP-1 and α-Z antibodies, whereas immunoblots of cell lysates were stained using rabbit α-GP-2-C, α-NP, and α-Z antibodies. (C) The supernatants of Cos 7 cells which transiently express either GP (lanes 1 to 3), NP (lanes 4 to 6), NP plus GP (lanes 7 to 9), NP plus GP plus Z (lanes 10 to 12), or NP plus Z (lanes 13 to 15) were examined for the presence of nucleoprotein within VLPs by protease protection assay (for the method, see Fig. 4C). Immunoblots of proteinase K-treated and nontreated samples were stained using the α-NP antibody (upper panel). Immunoblots of cell lysates of the various transfected cells (lower panel, lanes 6 to 10) and the corresponding VLPs (lower panel, lanes 1 to 5) are shown. The viral proteins were subjected to SDS-PAGE and subsequently to immunoblotting using α-GP-2-C, α-NP, and/or α-Z antibodies.
Further, we investigated whether GP and Z are able to incorporate NP into their VLPs. For this, we examined VLPs released from cells transiently expressing untagged versions of NP alone or NP in combination with either GP or matrix protein Z or from cells expressing the triple combination NP, GP, and Z (Fig. 5C, lower panel, lanes 6 to 10). Virus-like particles were isolated as described above (Fig. 5C, lower panel, lanes 1 to 5) and subjected to protease protection assay (Fig. 5C, upper panel). NP remained protected from protease digestion only in the presence of the matrix protein Z (Fig. 5C, upper panel, lanes 11 and 14), indicating that Z alone is sufficient for incorporation of NP into VLPs. Disruption of the lipid envelope of Z-derived VLPs with detergent resulted in proteolytic degradation of NP (Fig. 5C, upper panel, lanes 12 and 15). Some faint NP bands were detectable in lanes 4 and 7, which may represent proteinase K-sensitive aggregations of NP released from necrotic cells. No NP was detectable when VLPs induced by GP were analyzed (Fig. 5C, upper panel, lane 8). It is worth noting that coexpression of GP together with NP or with NP and Z did not significantly influence the efficiency of incorporation of GP into VLPs (compare Fig. 5C, lower panel, lanes 1, 3, and 4).
In conclusion, our data indicate that LASV NP interacts with the matrix protein Z but not with the viral glycoprotein and thus is incorporated into vesicles only in the presence of the matrix protein Z. Further, GP and Z are capable of interacting and are incorporated within the same VLPs. Thus, expression of GP, Z, and NP results in the release of vesicles that contain all three viral proteins.
Cellular colocalization of GP, NP, and Z protein.
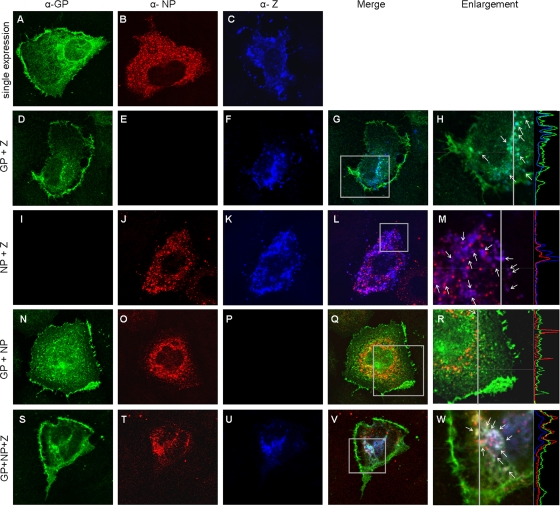
To further substantiate the results obtained and to visualize the interaction site of GP, Z, and NP, we performed colocalization analyses. For this, mammalian cells transiently expressing HA-tagged GP, untagged Z, and/or untagged NP in various combinations were examined by immunofluorescence. When expressed alone, GP is present in membranous structures in the cytoplasm, most likely representing endoplasmic reticulum (ER), as well as in vesicle-like structures and at the plasma membrane (Fig. 6A). The nucleoprotein NP exhibits a dot-like staining spread evenly throughout the cytoplasm (Fig. 6B). In contrast, the matrix protein Z is present in larger patches also distributed throughout the cytoplasm (Fig. 6C). Cells that express GP together with Z show a partial colocalization in vesicle-like structures near the nucleus (Fig. 6D to H). Also, the nucleoprotein and matrix protein Z colocalize (Fig. 6I to M). Here, the dot-like NP staining becomes more discrete. In addition, NP is also detectable in Z-positive patches (Fig. 6M). In contrast, the coexpression of GP and NP reveals no colocalization (Fig. 6N to R), supporting our immunoprecipitation data, which also indicated that no direct interaction exists between GP and NP. However, coexpression of GP, Z, and NP results in colocalization of these three proteins in vesicular structures in the perinuclear region similar to those observed for cells coexpressing only GP and Z (Fig. 6S to W). Interestingly, no colocalization of viral proteins at the plasma membrane could be observed. Similar results were obtained by coimmunofluorescence analysis using an HA-tagged version of the matrix protein Z (data not shown).
FIG. 6.
Intracellular colocalization of Lassa virus proteins GP, Z, and NP. Huh 7 cells transiently expressed LASV glycoprotein GPHAtag, NP, and/or Z. Cells were methanol-acetone fixed at 24 h after transfection, and LASV proteins were detected using chicken α-HA tag (green)-, mouse α-m-NP (red)-, and rabbit α-Z (blue)-specific antibodies. The immunofluorescence microscopic analyses were done by sequential scanning using confocal microscopy. Single expression of GP, NP, and Z (A to C); double expression of GP and Z (D to H), NP and Z (I to M), or GP and NP (N to R); and triple expression of GP, NP, and Z (S to W) are shown. Enlarged sections of merged images (H, M, R, and W) that contain fluorescence profile lines are additionally shown. Arrows indicate colocalization.
Together these confocal microscopic analyses of singly expressed and coexpressed viral proteins clearly demonstrate partial intracellular colocalization of GP and Z proteins, of NP and Z proteins, and of GP, NP, and Z proteins in vesicular structures that are located in the perinuclear region, indicating that these organelles represent an important platform for LASV assembly. The identification of these subcellular structures is currently in progress.
Lassa virus glycoprotein GP is the determining factor for apical VLP release.
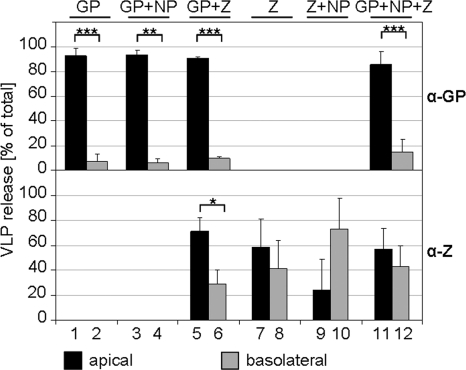
The insights obtained regarding the interdependence of GP, Z, and NP in VLP formation enabled us to investigate the role of each protein in directional release from polarized epithelial cells. For this examination, we used epithelial cells that stably expressed GP, Z, and NP either alone or in various combinations cultivated on Transwell filters. VLPs were harvested from the apical and basolateral chambers by pelleting supernatants through a 20% sucrose cushion. VLPs were then analyzed by immunoblotting and subsequent immunoblot quantification. All GP-containing VLPs, formed either from GP expressing cells or from cells expressing GP plus NP, GP plus Z, or GP plus Z plus NP, were released predominantly from the apical cell surface (Fig. 7, upper panel, bars 1 and 2, 3 and 4, 5 and 6, and 11 and 12), which indicates a dominant role of GP in apical VLP release. Coexpression of Z and/or NP had no or only a marginal influence on the apical release of GP-containing VLPs (Fig. 7, upper panel, bars 3 and 4, 5 and 6, and 11 and 12). Immunoblot analyses of matrix protein Z-containing VLPs revealed different results. Cells that express Z as the only viral protein showed a bipolar VLP release with an apical tendency (Fig. 7, lower panel, bars 7 and 8). Additional expression of GP resulted in enhanced apical release of Z (Fig. 7, lower panel, bars 5 and 6). Interestingly, expression of Z with NP resulted in a tendency toward VLP release from the basolateral side (Fig. 7, lower panel, bars 9 and 10). Triple expression of GP, Z, and NP again resulted in a bipolar release of Z-containing VLPs, with slightly more apically released VLPs (Fig. 7, lower panel, bars 11 and 12).
FIG. 7.
Viral determinants for directed virus-like particle release from polarized epithelial cells. MDCK-II cells that stably express GP, Z, and NP in various combinations were grown on Transwell filters (0.4-μm pore size) until polarization was achieved. After cell culture medium replacement with fresh medium containing 2% FCS, cells were further cultivated for 48 h. VLPs from the apical and basolateral chambers were harvested and concentrated by pelleting through a 20% sucrose cushion. The resuspended samples were subjected to SDS-PAGE and immunoblotting using the α-GP-2-C and α-Z antibodies. The viral proteins GP and Z were quantified using the Odyssey infrared quantification system. Average values from four to six independent experiments are expressed as percentage of VLP release. Error bars denote standard deviations. ***, P < 0.001; **, P < 0.01; *, P < 0.05 (t test).
In conclusion, these results indicate a dominant role of GP in directing VLP release at the apical cell surface of polarized epithelial cells, while Z-induced VLPs are released in a bipolar fashion.
DISCUSSION
Infection of the kidney in rodents plays a pivotal role in facilitating the transmission of LASV from its natural host to humans. In this study we investigated LASV entry and release using polarized kidney epithelium. We show that LASV entry occurs predominantly from the basolateral compartment. These data are consistent with recent observations for directional entry of Junin virus and LCMV in polarized human airway epithelia, which represents, in addition to the gastrointestinal tract, the natural gateway for arenavirus infections in humans (18). In contrast to these findings, earlier published work showed that Junin virus infection of polarized epithelial cell lines occurred preferentially through the apical surface (12). The observed discrepancy concerning Junin virus entry might be explained either by different experimental approaches or by the use of epithelial cell lines of different origins in these studies (12, 18). At present it is not known whether tissue-dependent variations in receptor expression, particularly in different epithelial cell types, may account for the described differences. However, similar to the basolateral surface expression of the LASV receptor dystroglycan (this study and references 17 and 29), transferrin 1, the cellular receptor for Junin virus and other New World arenaviruses, has also been shown to be expressed predominantly at the basolateral domain of epithelial cells (18, 28, 56).
In general, viruses that enter epithelial cells from the basolateral side are thought to be transmitted by infection via injured tissue or bites and scratches from animal vectors. However, exceptions have been noted; for example, canine parvovirus and human cytomegalovirus enter epithelial cells from the basolateral side despite being transmitted by dust or droplet infection (5, 23). In the cases of Junin virus and LCMV, it has been suggested that injuries to or destruction of the airway epithelium are required for infection (18). In this context, however, it is worth noting that similar infectious doses were described for subcutaneous and aerosol LASV infections for guinea pigs, indicating that damaged airway tissue, e.g., due to a secondary infection, is not necessary for robust LASV infection (62). Hence, it is still unclear how virions break through the epithelial barrier during initial host infection.
Investigating directional virus egress, we have found that LASV is released primarily from the apical compartment of polarized renal epithelial cells. We determined the relative release of infectious LASV and compared it with those of influenza virus and VSV as well established reference viruses (57, 60). In agreement with our observations, Junin virus and Tacaribe virus release from different polarized epithelial cell cultures has been shown to occur from the apical domain (12), while from human airway epithelial cells a basolateral virus release of LCMV and Junin virus has been suggested (18). Future work will have to identify the molecular determinants responsible for these cell type-dependent variations in arenavirus release.
Furthermore, in the present study we show that LASV infection did not cause significant cytopathic effects in epithelial cells and that no influence on tight junctions could be visualized, suggesting that there is no direct virus impact on tight-junction integrity. Studies of endothelial cells infected with various hemorrhagic fever viruses have demonstrated a redistribution of junction proteins resulting in increased paracellular permeability (25, 65). Examination of LASV-infected endothelial cells revealed no cellular damage (44); however, at present it is not known whether LASV influences the integrity of tight junctions in the endothelium during the course of infection.
Our data, together with previous results observed with polarized epithelial cells, lead to a better understanding of both arenavirus dissemination within an infected organisms and virus transmission. The natural infection of arenaviruses begins at the epithelia of the respiratory and gastrointestinal tracts. Once they have overcome the epithelial barrier, arenaviruses infect primarily macrophages, dendritic cells, and the endothelium (2, 3, 15, 44). These cells then help the virus to spread into many other tissues, including kidneys (31). As a consequence, the epithelium becomes infected from the basolateral cell surface and, subsequently, efficient virus replication takes place. Postmortem examination of Lassa fever patients and studies of LASV-infected animal models demonstrated high viral content in kidneys (71, 72).
Directional budding and release of enveloped viruses from polarized epithelial cells are complex processes that are driven principally by one or several viral structural proteins. The analysis of virus-like particles is a valuable approach to obtain knowledge about the requirement of individual viral proteins in determining directional assembly and VLP release. For this, knowledge about the interdependence of the participating viral proteins, which we gained through coimmunoprecipitation and coimmunofluorescence analyses, is important. Previous investigations by us and others have revealed an interaction of the arenavirus matrix protein Z with the nucleoprotein NP (9, 20). Consistent with data for New World arenaviruses and LCMV (9, 37), we demonstrated that the LASV matrix protein is able to recruit the nucleoprotein into VLPs. This behavior is also a characteristic of matrix proteins of other negative-strand RNA viruses such as Ebola, Newcastle disease, and parainfluenza viruses (13, 41, 54). In our study we also confirmed interaction between LASV GP and the matrix protein Z (8). Surprisingly, although LASV is suggested to bud from the plasma membrane, colocalization was observed in vesicle-like structures within the cytoplasm, with no colocalization of GP and Z detectable on the plasma membrane of the cell. This observation is in line with a recent finding observed for the New World arenavirus Junin (1). Here, electron microscopic analyses of cells coexpressing GP and Z failed to detect plasma membrane areas in which the two proteins colocalize. Whether the final budding process occurs very rapidly, thus making partial association difficult to detect, or whether additional viral components are required for this process remains unclear. However, the latter explanation is rather unlikely, since we observed a direct interaction between GP and Z in purified VLPs as well as intracellularly.
Analysis of cells expressing GP and Z together with NP revealed similar results, showing a colocalization in vesicle-like structures near the nucleus. Additional investigations into the exact site of LASV assembly may provide interesting insights in the future. We further demonstrated that NP did not influence the interaction or incorporation efficiency of GP and Z, which differs from observations using chimeric New World arenavirus VLPs (9). An interaction of GP and NP, in the absence of Z, could not be detected using coimmunoprecipitation, colocalization, or VLP incorporation analyses, either by us or by others (9).
In the present study we demonstrate that solitary expression of the LASV glycoprotein GP results in the release of spike-containing virus-like particles. VLP formation by arenavirus proteins has, until now, been described only for the matrix protein Z (55, 63). As a characteristic of most other enveloped viruses, several virus proteins are needed to form VLPs; for example, in mumps virus the matrix, fusion, and nucleocapsid proteins are all required for an efficient production of VLPs (40). However, the induction of VLP release by expressed glycoproteins as the sole viral protein is not unusual. These kind of particles have been previously demonstrated for foamy virus, hepatitis B virus, influenza virus, VSV, and Ebola virus, as well as other viruses (11, 16, 52, 58, 61, 64, 73). At present it is not known whether GP-induced VLPs are also released during the course of LASV infection. If this is the case, one could speculate that noninfectious GP-derived VLPs may have some relevance for pathogenesis, for instance, through binding of LASV GP-specific antibodies, thus delaying immune detection of infected cells.
Our findings regarding GP-induced VLPs and the insights obtained on the interdependence of the three proteins GP, Z, and NP for budding provided the basis for identification of the direction-determining factors for the release of Lassa virions from a polarized epithelium. We observed that GP-driven VLPs are apically released and are not influenced by coexpression of Z or NP, while VLPs from cells expressing only the matrix protein Z are released in a largely bipolar fashion. Investigation of the directional release of GP-Z VLPs shows that GP leads to an apical budding tendency of Z, suggesting recruitment of Z by GP to the apical cell membrane. In contrast, NP redirects Z to the basolateral domain. Due to the almost exclusively apical release of GP-containing VLPs, VLPs containing GP, Z, and NP are also released predominantly from the apical membrane. This apical distribution of GP is supported by the finding that it is located at the apical cell membrane in solitary GP-expressing cells as well as in cells infected with LASV. The apical localization and budding of GP is independent of the presence of other viral proteins. As a result, GP acts as the determining factor for directional apical release of VLPs containing GP, Z, and NP, which suggests that the apical release of Lassa virions is also determined by the glycoprotein GP.
A viral glycoprotein as a determining factor for directed virus egress has so far been described only for members of the retrovirus family. However, the retroviral glycoproteins direct basolateral virus release by utilizing a basolateral sorting signal in their cytoplasmic domains (4, 42, 43, 53). In contrast, analyses using influenza virus, VSV, and human respiratory syncytial virus showed that while their glycoproteins are located at the site of virus budding, they are not the direction-determining factors (6, 50, 74). For Marburg virus and measles virus, the matrix protein was described to be the determining factor for directional virus release (33, 51).
In conclusion, this study shows that entry and release of LASV in epithelial cells occur from opposing cell surfaces. LASV enters the epithelium from the basolateral side and is apically released. This apical release provides new progeny virions for transmission to new hosts. The characterization of virus-like particles induced from cells expressing solely GP was the basis for an approach to investigate the roles of the individual viral proteins, i.e., glycoprotein, matrix protein, and nucleoprotein, in directional virus release. As a result of these studies, we defined the glycoprotein as the sole direction-determining factor for apical LASV release.
Acknowledgments
We thank M. C. Georges-Courbot (Institute Pasteur, Lyon, France), G. Herrler (Tiermedizinische Hochschule, Hannover), and I. S. Lukashevich (Institute of Human Virology, University of Maryland, Baltimore) for providing antibodies. We are grateful to F. Grolig for help with confocal microscopy and to S. Heck and L. Kolesnikova for electron microscopy. We thank H. D. Klenk and A. Maisner for helpful discussions and critical manuscript reviews. We also thank P. Neubauer-Rädel for expert technical assistance and G. Ludwig and M. Schmidt for technical support with biosafety level 4 procedures.
This work was supported by the DFG Schwerpunktprogramm 1175, Ga282/5, and the DFG Sonderforschungsbereich 593.
Footnotes
Published ahead of print on 13 January 2010.
REFERENCES
- 1.Agnihothram, S. S., B. Dancho, K. W. Grant, M. L. Grimes, D. S. Lyles, and J. H. Nunberg. 2009. Assembly of arenavirus envelope glycoprotein GPC in detergent-soluble membrane microdomains. J. Virol. 83:9890-9990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Andrews, B. S., A. N. Theofilopoulos, C. J. Peters, D. J. Loskutoff, W. E. Brandt, and F. J. Dixon. 1978. Replication of dengue and junin viruses in cultured rabbit and human endothelial cells. Infect. Immun. 20:776-781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baize, S., J. Kaplon, C. Faure, D. Pannetier, M. C. Georges-Courbot, and V. Deubel. 2004. Lassa virus infection of human dendritic cells and macrophages is productive but fails to activate cells. J. Immunol. 172:2861-2869. [DOI] [PubMed] [Google Scholar]
- 4.Ball, J. M., M. J. Mulligan, and R. W. Compans. 1997. Basolateral sorting of the HIV type 2 and SIV envelope glycoproteins in polarized epithelial cells: role of the cytoplasmic domain. AIDS Res. Hum. Retroviruses 13:665-675. [DOI] [PubMed] [Google Scholar]
- 5.Basak, S., and R. W. Compans. 1989. Polarized entry of canine parvovirus in an epithelial cell line. J. Virol. 63:3164-3167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Batonick, M., A. G. Oomens, and G. W. Wertz. 2008. Human respiratory syncytial virus glycoproteins are not required for apical targeting and release from polarized epithelial cells. J. Virol. 82:8664-8672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Briese, T., J. T. Paweska, L. K. McMullan, S. K. Hutchison, C. Street, G. Palacios, M. L. Khristova, J. Weyer, R. Swanepoel, M. Egholm, S. T. Nichol, and W. I. Lipkin. 2009. Genetic detection and characterization of Lujo virus, a new hemorrhagic fever-associated arenavirus from southern Africa. PLoS Pathog. 5:e1000455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Capul, A. A., M. Perez, E. Burke, S. Kunz, M. J. Buchmeier, and J. C. de la Torre. 2007. Arenavirus Z-glycoprotein association requires Z myristoylation but not functional RING or late domains. J. Virol. 81:9451-9460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Casabona, J. C., J. M. Levingston Macleod, M. E. Loureiro, G. A. Gomez, and N. Lopez. 2009. The RING domain and the L79 residue of Z protein are involved in both the rescue of nucleocapsids and the incorporation of glycoproteins into infectious chimeric arenavirus-like particles. J. Virol. 83:7029-7039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Charrel, R. N., X. de Lamballerie, and S. Emonet. 2008. Phylogeny of the genus Arenavirus. Curr. Opin. Microbiol. 11:362-368. [DOI] [PubMed] [Google Scholar]
- 11.Chen, B. J., G. P. Leser, E. Morita, and R. A. Lamb. 2007. Influenza virus hemagglutinin and neuraminidase, but not the matrix protein, are required for assembly and budding of plasmid-derived virus-like particles. J. Virol. 81:7111-7123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cordo, S. M., M. Cesio y Acuna, and N. A. Candurra. 2005. Polarized entry and release of Junin virus, a New World arenavirus. J. Gen. Virol. 86:1475-1479. [DOI] [PubMed] [Google Scholar]
- 13.Coronel, E. C., K. G. Murti, T. Takimoto, and A. Portner. 1999. Human parainfluenza virus type 1 matrix and nucleoprotein genes transiently expressed in mammalian cells induce the release of virus-like particles containing nucleocapsid-like structures. J. Virol. 73:7035-7038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Delgado, S., B. R. Erickson, R. Agudo, P. J. Blair, E. Vallejo, C. G. Albarino, J. Vargas, J. A. Comer, P. E. Rollin, T. G. Ksiazek, J. G. Olson, and S. T. Nichol. 2008. Chapare virus, a newly discovered arenavirus isolated from a fatal hemorrhagic fever case in Bolivia. PLoS Pathog. 4:e1000047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Doyle, M. V., and M. B. Oldstone. 1978. Interactions between viruses and lymphocytes. I. In vivo replication of lymphocytic choriomeningitis virus in mononuclear cells during both chronic and acute viral infections. J. Immunol. 121:1262-1269. [PubMed] [Google Scholar]
- 16.Dubois, M. F., C. Pourcel, S. Rousset, C. Chany, and P. Tiollais. 1980. Excretion of hepatitis B surface antigen particles from mouse cells transformed with cloned viral DNA. Proc. Natl. Acad. Sci. U. S. A. 77:4549-4553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Durbeej, M., M. D. Henry, M. Ferletta, K. P. Campbell, and P. Ekblom. 1998. Distribution of dystroglycan in normal adult mouse tissues. J. Histochem. Cytochem. 46:449-457. [DOI] [PubMed] [Google Scholar]
- 18.Dylla, D. E., D. E. Michele, K. P. Campbell, and P. B. McCray, Jr. 2008. Basolateral entry and release of new and old world arenaviruses from human airway epithelia. J. Virol. 82:6034-6038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Eichler, R., O. Lenz, T. Strecker, and W. Garten. 2003. Signal peptide of Lassa virus glycoprotein GP-C exhibits an unusual length. FEBS Lett. 538:203-206. [DOI] [PubMed] [Google Scholar]
- 20.Eichler, R., T. Strecker, L. Kolesnikova, J. ter Meulen, W. Weissenhorn, S. Becker, H. D. Klenk, W. Garten, and O. Lenz. 2004. Characterization of the Lassa virus matrix protein Z: electron microscopic study of virus-like particles and interaction with the nucleoprotein (NP). Virus Res. 100:249-255. [DOI] [PubMed] [Google Scholar]
- 21.Emonet, S., J. J. Lemasson, J. P. Gonzalez, X. de Lamballerie, and R. N. Charrel. 2006. Phylogeny and evolution of old world arenaviruses. Virology 350:251-257. [DOI] [PubMed] [Google Scholar]
- 22.Enria, D., J. Mills, R. Flick, M. Bowen, D. Bausch, W. Shieh, and C. Peters. 2006. Arenavirus infections, p. 734-755. In R. L. Guerranat, D. H. Walker, and P. F. Weller (ed.), Tropical infectious diseases: principles, pathogens, and practice, 2nd ed., vol. 1. Elsevier, Philadelphia, PA. [Google Scholar]
- 23.Esclatine, A., M. Lemullois, A. L. Servin, A. M. Quero, and M. Geniteau-Legendre. 2000. Human cytomegalovirus infects Caco-2 intestinal epithelial cells basolaterally regardless of the differentiation state. J. Virol. 74:513-517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Excoffon, K. J., K. M. Guglielmi, J. D. Wetzel, N. D. Gansemer, J. A. Campbell, T. S. Dermody, and J. Zabner. 2008. Reovirus preferentially infects the basolateral surface and is released from the apical surface of polarized human respiratory epithelial cells. J. Infect. Dis. 197:1189-1197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Feldmann, H., H. Bugany, F. Mahner, H. D. Klenk, D. Drenckhahn, and H. J. Schnittler. 1996. Filovirus-induced endothelial leakage triggered by infected monocytes/macrophages. J. Virol. 70:2208-2214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fichet-Calvet, E., E. Lecompte, L. Koivogui, B. Soropogui, A. Dore, F. Kourouma, O. Sylla, S. Daffis, K. Koulemou, and J. Ter Meulen. 2007. Fluctuation of abundance and Lassa virus prevalence in Mastomys natalensis in Guinea, West Africa. Vector Borne Zoonotic Dis. 7:119-128. [DOI] [PubMed] [Google Scholar]
- 27.Fisher-Hoch, S. P., O. Tomori, A. Nasidi, G. I. Perez-Oronoz, Y. Fakile, L. Hutwagner, and J. B. McCormick. 1995. Review of cases of nosocomial Lassa fever in Nigeria: the high price of poor medical practice. BMJ 311:857-859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fuller, S. D., and K. Simons. 1986. Transferrin receptor polarity and recycling accuracy in “tight” and “leaky” strains of Madin-Darby canine kidney cells. J. Cell Biol. 103:1767-1779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Han, R., M. Kanagawa, T. Yoshida-Moriguchi, E. P. Rader, R. A. Ng, D. E. Michele, D. E. Muirhead, S. Kunz, S. A. Moore, S. T. Iannaccone, K. Miyake, P. L. McNeil, U. Mayer, M. B. Oldstone, J. A. Faulkner, and K. P. Campbell. 2009. Basal lamina strengthens cell membrane integrity via the laminin G domain-binding motif of alpha-dystroglycan. Proc. Natl. Acad. Sci. U. S. A. 106:12573-12579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Henry, M. D., and K. P. Campbell. 1998. A role for dystroglycan in basement membrane assembly. Cell 95:859-870. [DOI] [PubMed] [Google Scholar]
- 31.John, R., and P. J. Nelson. 2007. Dendritic cells in the kidney. J. Am. Soc Nephrol. 18:2628-2635. [DOI] [PubMed] [Google Scholar]
- 32.Khan, S. H., A. Goba, M. Chu, C. Roth, T. Healing, A. Marx, J. Fair, M. C. Guttieri, P. Ferro, T. Imes, C. Monagin, R. F. Garry, and D. G. Bausch. 2008. New opportunities for field research on the pathogenesis and treatment of Lassa fever. Antiviral Res. 78:103-115. [DOI] [PubMed] [Google Scholar]
- 33.Kolesnikova, L., E. Ryabchikova, A. Shestopalov, and S. Becker. 2007. Basolateral budding of Marburg virus: VP40 retargets viral glycoprotein GP to the basolateral surface. J. Infect. Dis. 196(Suppl. 2):S232-S236. [DOI] [PubMed] [Google Scholar]
- 34.Krautkrämer, E., and M. Zeier. 2008. Hantavirus causing hemorrhagic fever with renal syndrome enters from the apical surface and requires decay-accelerating factor (DAF/CD55). J. Virol. 82:4257-4264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lecompte, E., E. Fichet-Calvet, S. Daffis, K. Koulemou, O. Sylla, F. Kourouma, A. Dore, B. Soropogui, V. Aniskin, B. Allali, S. Kouassi Kan, A. Lalis, L. Koivogui, S. Günther, C. Denys, and J. ter Meulen. 2006. Mastomys natalensis and Lassa fever, West Africa. Emerg. Infect. Dis. 12:1971-1974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lecompte, E., J. ter Meulen, S. Emonet, S. Daffis, and R. N. Charrel. 2007. Genetic identification of Kodoko virus, a novel arenavirus of the African pigmy mouse (Mus Nannomys minutoides) in West Africa. Virology 364:178-183. [DOI] [PubMed] [Google Scholar]
- 37.Lee, K. J., M. Perez, D. D. Pinschewer, and J. C. de la Torre. 2002. Identification of the lymphocytic choriomeningitis virus (LCMV) proteins required to rescue LCMV RNA analogs into LCMV-like particles. J. Virol. 76:6393-6397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lenz, O., J. ter Meulen, H. Feldmann, H. D. Klenk, and W. Garten. 2000. Identification of a novel consensus sequence at the cleavage site of the Lassa virus glycoprotein. J. Virol. 74:11418-11421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lenz, O., J. ter Meulen, H. D. Klenk, N. G. Seidah, and W. Garten. 2001. The Lassa virus glycoprotein precursor GP-C is proteolytically processed by subtilase SKI-1/S1P. Proc. Natl. Acad. Sci. U. S. A. 98:12701-12705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Li, M., P. T. Schmitt, Z. Li, T. S. McCrory, B. He, and A. P. Schmitt. 2009. Mumps virus matrix, fusion, and nucleocapsid proteins cooperate for efficient production of virus-like particles. J. Virol. 83:7261-7272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Licata, J. M., R. F. Johnson, Z. Han, and R. N. Harty. 2004. Contribution of Ebola virus glycoprotein, nucleoprotein, and VP24 to budding of VP40 virus-like particles. J. Virol. 78:7344-7351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lodge, R., L. Delamarre, J. P. Lalonde, J. Alvarado, D. A. Sanders, M. C. Dokhelar, E. A. Cohen, and G. Lemay. 1997. Two distinct oncornaviruses harbor an intracytoplasmic tyrosine-based basolateral targeting signal in their viral envelope glycoprotein. J. Virol. 71:5696-5702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lodge, R., J. P. Lalonde, G. Lemay, and E. A. Cohen. 1997. The membrane-proximal intracytoplasmic tyrosine residue of HIV-1 envelope glycoprotein is critical for basolateral targeting of viral budding in MDCK cells. EMBO J. 16:695-705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lukashevich, I. S., R. Maryankova, A. S. Vladyko, N. Nashkevich, S. Koleda, M. Djavani, D. Horejsh, N. N. Voitenok, and M. S. Salvato. 1999. Lassa and Mopeia virus replication in human monocytes/macrophages and in endothelial cells: different effects on IL-8 and TNF-alpha gene expression. J. Med. Virol. 59:552-560. [PMC free article] [PubMed] [Google Scholar]
- 45.Lunkenheimer, K., F. T. Hufert, and H. Schmitz. 1990. Detection of Lassa virus RNA in specimens from patients with Lassa fever by using the polymerase chain reaction. J. Clin. Microbiol. 28:2689-2692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Matrosovich, M., T. Matrosovich, W. Garten, and H. D. Klenk. 2006. New low-viscosity overlay medium for viral plaque assays. Virol. J. 3:63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.McCormick, J. B., I. J. King, P. A. Webb, K. M. Johnson, R. O'Sullivan, E. S. Smith, S. Trippel, and T. C. Tong. 1987. A case-control study of the clinical diagnosis and course of Lassa fever. J. Infect. Dis. 155:445-455. [DOI] [PubMed] [Google Scholar]
- 48.McCormick, J. B., P. A. Webb, J. W. Krebs, K. M. Johnson, and E. S. Smith. 1987. A prospective study of the epidemiology and ecology of Lassa fever. J. Infect. Dis. 155:437-444. [DOI] [PubMed] [Google Scholar]
- 49.Monath, T. P., V. F. Newhouse, G. E. Kemp, H. W. Setzer, and A. Cacciapuoti. 1974. Lassa virus isolation from Mastomys natalensis rodents during an epidemic in Sierra Leone. Science 185:263-265. [DOI] [PubMed] [Google Scholar]
- 50.Mora, R., E. Rodriguez-Boulan, P. Palese, and A. Garcia-Sastre. 2002. Apical budding of a recombinant influenza A virus expressing a hemagglutinin protein with a basolateral localization signal. J. Virol. 76:3544-3553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Naim, H. Y., E. Ehler, and M. A. Billeter. 2000. Measles virus matrix protein specifies apical virus release and glycoprotein sorting in epithelial cells. EMBO J. 19:3576-3585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Noda, T., H. Sagara, E. Suzuki, A. Takada, H. Kida, and Y. Kawaoka. 2002. Ebola virus VP40 drives the formation of virus-like filamentous particles along with GP. J. Virol. 76:4855-4865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Owens, R. J., and R. W. Compans. 1989. Expression of the human immunodeficiency virus envelope glycoprotein is restricted to basolateral surfaces of polarized epithelial cells. J. Virol. 63:978-982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Pantua, H. D., L. W. McGinnes, M. E. Peeples, and T. G. Morrison. 2006. Requirements for the assembly and release of Newcastle disease virus-like particles. J. Virol. 80:11062-11073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Perez, M., R. C. Craven, and J. C. de la Torre. 2003. The small RING finger protein Z drives arenavirus budding: implications for antiviral strategies. Proc. Natl. Acad. Sci. U. S. A. 100:12978-12983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Radoshitzky, S. R., J. Abraham, C. F. Spiropoulou, J. H. Kuhn, D. Nguyen, W. Li, J. Nagel, P. J. Schmidt, J. H. Nunberg, N. C. Andrews, M. Farzan, and H. Choe. 2007. Transferrin receptor 1 is a cellular receptor for New World haemorrhagic fever arenaviruses. Nature 446:92-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Rodriguez Boulan, E., and D. D. Sabatini. 1978. Asymmetric budding of viruses in epithelial monlayers: a model system for study of epithelial polarity. Proc. Natl. Acad. Sci. U. S. A. 75:5071-5075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Rolls, M. M., P. Webster, N. H. Balba, and J. K. Rose. 1994. Novel infectious particles generated by expression of the vesicular stomatitis virus glycoprotein from a self-replicating RNA. Cell 79:497-506. [DOI] [PubMed] [Google Scholar]
- 59.Rossen, J. W., C. P. Bekker, G. J. Strous, M. C. Horzinek, G. S. Dveksler, K. V. Holmes, and P. J. Rottier. 1996. A murine and a porcine coronavirus are released from opposite surfaces of the same epithelial cells. Virology 224:345-351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Roth, M. G., J. P. Fitzpatrick, and R. W. Compans. 1979. Polarity of influenza and vesicular stomatitis virus maturation in MDCK cells: lack of a requirement for glycosylation of viral glycoproteins. Proc. Natl. Acad. Sci. U. S. A. 76:6430-6434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Shaw, K. L., D. Lindemann, M. J. Mulligan, and P. A. Goepfert. 2003. Foamy virus envelope glycoprotein is sufficient for particle budding and release. J. Virol. 77:2338-2348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Stephenson, E. H., E. W. Larson, and J. W. Dominik. 1984. Effect of environmental factors on aerosol-induced Lassa virus infection. J. Med. Virol. 14:295-303. [DOI] [PubMed] [Google Scholar]
- 63.Strecker, T., R. Eichler, J. Meulen, W. Weissenhorn, H.-D. Klenk, W. Garten, and O. Lenz. 2003. Lassa virus Z protein is a matrix protein and sufficient for the release of virus-like particles. J. Virol. 77:10700-10705. [DOI] [PMC free article] [PubMed]
- 64.Takimoto, T., K. G. Murti, T. Bousse, R. A. Scroggs, and A. Portner. 2001. Role of matrix and fusion proteins in budding of Sendai virus. J. Virol. 75:11384-11391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Talavera, D., A. M. Castillo, M. C. Dominguez, A. E. Gutierrez, and I. Meza. 2004. IL8 release, tight junction and cytoskeleton dynamic reorganization conducive to permeability increase are induced by dengue virus infection of microvascular endothelial monolayers. J. Gen. Virol. 85:1801-1813. [DOI] [PubMed] [Google Scholar]
- 66.Tashiro, M., I. James, S. Karri, K. Wahn, K. Tobita, H. D. Klenk, R. Rott, and J. T. Seto. 1991. Pneumotropic revertants derived from a pantropic mutant, F1-R, of Sendai virus. Virology 184:227-234. [DOI] [PubMed] [Google Scholar]
- 67.Ter Meulen, J., I. Lukashevich, K. Sidibe, A. Inapogui, M. Marx, A. Dorlemann, M. L. Yansane, K. Koulemou, J. Chang-Claude, and H. Schmitz. 1996. Hunting of peridomestic rodents and consumption of their meat as possible risk factors for rodent-to-human transmission of Lassa virus in the Republic of Guinea. Am. J. Trop. Med. Hyg. 55:661-666. [DOI] [PubMed] [Google Scholar]
- 68.Tseng, C. T., J. Tseng, L. Perrone, M. Worthy, V. Popov, and C. J. Peters. 2005. Apical entry and release of severe acute respiratory syndrome-associated coronavirus in polarized Calu-3 lung epithelial cells. J. Virol. 79:9470-9479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Tucker, S. P., and R. W. Compans. 1993. Virus infection of polarized epithelial cells. Adv. Virus Res. 42:187-247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Vladyko, A. S., S. I. Bystrova, N. N. Lemeshko, and I. S. Lukashevich. 1987. Characteristics of monoclonal antibodies against Lassa virus. Mol. Gen. Mikrobiol. Virusol. 1987:37-40. [PubMed] [Google Scholar]
- 71.Walker, D. H., J. B. McCormick, K. M. Johnson, P. A. Webb, G. Komba-Kono, L. H. Elliott, and J. J. Gardner. 1982. Pathologic and virologic study of fatal Lassa fever in man. Am. J. Pathol. 107:349-356. [PMC free article] [PubMed] [Google Scholar]
- 72.Walker, D. H., H. Wulff, and F. A. Murphy. 1975. Experimental Lassa virus infection in the squirrel monkey. Am. J. Pathol. 80:261-278. [PMC free article] [PubMed] [Google Scholar]
- 73.Whitt, M. A., L. Chong, and J. K. Rose. 1989. Glycoprotein cytoplasmic domain sequences required for rescue of a vesicular stomatitis virus glycoprotein mutant. J. Virol. 63:3569-3578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Zimmer, G., K. P. Zimmer, I. Trotz, and G. Herrler. 2002. Vesicular stomatitis virus glycoprotein does not determine the site of virus release in polarized epithelial cells. J. Virol. 76:4103-4107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Zurzolo, C., C. Polistina, M. Saini, R. Gentile, L. Aloj, G. Migliaccio, S. Bonatti, and L. Nitsch. 1992. Opposite polarity of virus budding and of viral envelope glycoprotein distribution in epithelial cells derived from different tissues. J. Cell Biol. 117:551-564. [DOI] [PMC free article] [PubMed] [Google Scholar]