Abstract
Objective
To examine the impact of Medicare managed care (MMC) versus Medicare fee for service (MFFS) on stent patients' use of physicians with lower resource use and better outcomes.
Data Sources/Study Setting
Retrospective secondary data from 2003 through 2006 for 67,476 patients without acute myocardial infarction, staying 2 or more days in hospital, and treated by 486 physicians in Florida performing 10 or more cases per quarter.
Study Design
Analysis was at the patient level. Multivariate logistic models estimated the probability of an MMC patient using a physician with a particular risk-adjusted profile rank with respect to hospital peers.
Principal Findings
No differences were found in usage of physicians with shorter admissions. Compared with MFFS, MMC patients were significantly less likely to use physicians whose average mortality was the lowest/lowest quartiles/below median among facility peers, and more likely to use a physician ranked below median on live discharges directly home (not needing home health care, skilled nursing care, or a subacute hospital convalescence). Similar results were found with emergency admissions, and where physicians both attended and treated.
Conclusions
Florida percutaneous coronary interventions patients insured by MMC used physicians with worse outcome profiles than those of MFFS patients. Results were not consistent with hospital care differences, physician–patient, or payor–physician selection, but they were consistent with selection of unobservably sicker members into MMC and concentration of MMC among physicians.
Keywords: Managed care, quality, resource use, incentives, selection effects
Medicare Advantage managed care (MMC) plans face fixed administered payments at the county level and must balance cost containment and quality of delivered care objectives. A bipartisan goal since the inception of managed care plans has been the simultaneous achievement of both objectives. This may not be feasible, given evidence that more efficient hospitals do not generally provide better care (Saleh, Hannan, and Racz 2008; Jha et al. 2009;).
Could MMC plans procure both efficiency and high quality? De Parle (2002) argued MMC performed a little better than traditional Medicare fee for service (MFFS) in delivery quality and health status. Yet reported satisfaction of beneficiaries' does not differ between MFFS and MMC, and MMC quality of care may not justify these increased payments (Orszag 2007).
A very large literature has examined the degree to which managed care plans trade-off cost and quality, mostly at the hospital level. Results have been mixed, most likely due to unobserved between-hospital differences and to different features of the local hospital and insurance markets. Far less research exists on the extent to which the use of physicians differs across plans. Informed MMC plans may be able to selectively contract with more efficient, higher quality providers, guide enrollees to these, and positively influence care quality and resource consumption during the admission.
This study tests this hypothesis by examining whether managed care coronary stent patients in Florida used physicians that differed systematically from those used by fee-for-service patients over the period 2003–2006. Within-hospital analysis mitigates omitted variables biases (e.g., staffing and discharge policies) inherent in between-hospital analyses. Confounding due to unobserved patient health and decisions and provider preferences is also taken into account.
BACKGROUND
The provision of actuarially fair risk-bearing services by intermediaries in the market for medical care should be good for risk-averse consumers (Arrow 1963). However, insurers are exposed to financial risk since fixed revenues from members are realized before claims are paid out. Moral hazard, subscriber health status heterogeneity, and provider quality uncertainty further complicate the insurers' objectives.
Three broad categories of risk mitigation strategies exist. Selection of members with desirable health risks can be achieved through marketing, screening, and pricing. Selection of providers with “better” cost, utilization, and/or quality can be accomplished through selective contracting (Flynn, Smith, and Davis, 2002). Restriction of members' choices of physician, hospital, and treatment can result through financial incentives and policy restrictions (Cutler, McClellan, and Newhouse 2000; Bundorf et al. 2004;).
The consequences of such risk mitigation and managed care may be particular patterns of care and resource use by providers. For example, selective contracting on the basis of provider prices might reduce the feasible quantity and quality of care that providers are able to deliver.
How managed care impacts the trade-off between health care efficiency and quality remains unresolved (Enthoven 1978). Every, Cannon, and Granger (1992) showed that managed care patients with unstable angina were less likely to receive angiography, without apparent mortality cost. Using patient choice models, Escarce et al. (1999) showed that coronary bypass managed care patients were more likely to be seen at higher quality hospitals in California, but no more likely in Florida. The more mature managed care market in California was thought to allow better-informed plans.
Policy experiments such as RAND's Health Insurance Experiment (Newhouse 2004) or natural experiments in CHAMPUS (Goldman 1995) have been used to relate insurance status to health and cost outcomes. Generally these results have shown positive results: managed care contains costs, but apparently not at the cost of health status.
Luft (2003) found no differences between the treatment and outcomes of managed care insured and private heart attack patients in California. Erickson et al. (2000a) found that adult managed care patients were more likely to be admitted to lower quality cardiac hospitals in New York. Children with congenital heart defects were treated at higher mortality hospitals in California (Erickson et al. 2000b).
More recent studies have found mixed results in consumer responses to managed care access of care (Miller and Luft 2002), surveyed health status (Xu and Jensen 2006), measurable quality of care (Miller and Luft 2002; Zhan et al. 2004;), or measurable care expenditures (Chen and Escarce 2004).
Higher managed care penetration was shown to lead to better quality of care (Rogowski, Jain, and Escarce 2007) and lower mortality in California but higher mortality in New York (Escarce, Jain, and Rogowski 2006), and lower rates of use of expensive treatments in acute heart attack treatments in general (Bundorf et al. 2004).
Research Question and Hypotheses
This study's central question is whether managed care enrollees systematically use physicians with different resource use or quality profiles in the market for coronary stent procedures. Past research guides hypotheses on the direction of these differences.
Flynn et al. (2002) described managed care plans' use of economic credentialing to exclude physicians with high resource use and the use of higher volume coronary stent providers.1 Managed care payors may also elect to provide separate incentives to contracted providers to align their clinical practice to managed care objectives (Bundorf et al. 2004).
If negotiated prices with in-panel physician and hospital providers dominate contractual arrangements, the profiles of physicians treating MMC plan members may reflect lower resource use (e.g., shorter lengths of stay). Limited empirical evidence from hospitals suggests indeed that managed care payors contract more on convenience, geographical location, and negotiated prices than mortality and complication rates (Schulman et al. 1997; Hannan 1999; Gaskin et al. 2002; Rainwater and Romano 2003;). Accordingly it is hypothesized that:
MMC patients will use physicians with shorter average length of stays than physicians seen by MFFS patients.
Quality profiles could be similar because patients, referring physicians, and insurers cannot reliably distinguish between physicians on some outcomes. In this study's empirical setting mortality rates are relatively low, many physicians have zero panel average mortality, and no information was publicly available on mortality at the cardiologist level.
Outcome profiles could be better if insurers used other outcome measures with more stability and higher variation, and guided subscribers to these. For example, the rate of postadmission discharge to skilled nursing facility and short-term convalescent hospitals may be correlated with complications occurring before discharge. Physicians used by MMC patients may have better profiles if managed care payors use volume thresholds as de facto quality markers (Flynn et al, 2002).2 It is thus expected that:
MMC patients will use physicians with similar or more favorable average outcome profiles than physicians seen by MFFS patients.
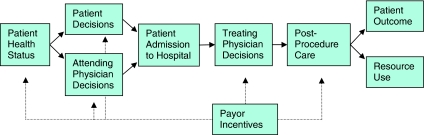
In Figure 1 the conceptual framework for this study is shown. A series of confounding biases due to selection or composition biases is highlighted. For example, managed care payors may have enrolled plan members with unobservably different ex ante health status. This bias cannot be signed with certainty, but anecdotal reports suggest that MMC plan members tend to be healthier (Rice and Desmond 2004).
Figure 1.
Conceptual Framework: Schematic Treatment Process and Points of Potential Payor Influence
Once insured, a member with private information on his or her health status may have preferences for a particular hospital and physician. Anthony et al. (2009) find that some preferences for care influence care-seeking decisions. Geweke, Gowrisankaran, and Town (2003) also found that unobserved illness severity is strongly correlated with admission to high-quality hospitals.
Patient heterogeneity in coronary stent admissions is substantial (Resnic 2007). Many inpatient stent admissions are emergent, complex medical emergencies precipitated by an acute myocardial infarction. These admissions span many days with substantial mortality risk due to the underlying medical condition and its complications. Many other inpatient admissions are scheduled and do not involve an overnight stay. While observed as inpatient admissions, their length of stay is 1 day, and mortality is negligible. The pronounced differences between these patient groups may bias risk-adjustment and physician profiles.
Whether a particular attending or treating physician has contracted with a payor, the physician may also have preferences for particular patient attributes (Werner, Asch, and Polsky 2005). For example, treatment of unobservably healthier private patients for the dilation of relatively minor coronary artery narrowing (the well-known “oculostenotic reflex”) would bias mortality downwards.
If this is more likely with MFFS than with MMC patients, then such physician-mediated effects may lead to omitted variables bias.3 This problem may be accentuated in elective, 1-day-only cases, where the attending physician is also the treating physician. It may be attenuated in emergency cases where selection is infeasible.
Finally, some physicians differ greatly from their peers in terms of workload or time observed. Those who perform only a few cases intermittently may see very sick or complex patients. Those who exit the panel after a short period of time may have unobservable and unrepresentative quality problems that warrant exclusion from the analysis.
ANALYTICAL STRATEGY
We obtained administrative data on all 246,044 discharges for percutaneous coronary interventions (PCI) in state-regulated hospitals in Florida from the first quarter of 2003 through the last quarter of 2006. The data were provided by the Florida Department of Health's Agency for Health Care Administration. After validation of records (described in the Web Appendix SA1) there remained 221,150 PCI discharges treated by 998 physicians in 114 hospitals.
Data Restrictions
Nearly 70 percent of the validated records were excluded from analysis, to mitigate the potential for confounding due to patient and physician heterogeneity. A total of 65,260 acute myocardial infarction (AMI) patients were excluded. Only records with a DRG code of 527 (until the last quarter of 2005, thereafter 557 and 558) and a code of 517 were included. This removes patients whose serious underlying and/or precipitating medical condition may be the chief driver of outcomes and length of stay.
Of the remaining 155,890 patient records, a further 85,055 records of patients spending 1 day or less in hospital were excluded. This “Winsorization” of the data in turn removed both the least sick patients with short, scheduled interventions (likely to do well with any physician) and the sickest patients who died on the first day (likely to succumb regardless of physician).
Of the remaining 70,835 patients without AMI who stayed at least 2 days, a further 3,359 records were removed based on physician characteristics. Using the original, unrestricted data, unrepresentative physicians who saw low volumes of patients were identified. Peer specialty societies recommend annual PCI volume of around 75–100 cases to preserve skills and ensure acceptable performance. In this study, 594 treating physicians who saw less than 40 cases per year were removed from analysis.
These restrictions resulted in an analysis set of 67,476 patients seen by 486 physicians in 97 facilities. Unaudited, self-reported physician characteristics publicly available from the Florida Department of Health were linked with treating physician license numbers. This study was approved by (the Duke University Health System) Institutional Review Board.
Econometric Specification
The central hypotheses of this study posit different use by differently insured patients of physicians with different profiles. To operationalize this, physicians were ranked within each facility based on their profile relative to peers practicing in that facility. If a patient i was observed to use, say, a physician of below-median quality, a binary indicator yi was set to 1. The outcome of interest was the probability of the event yi=1, and the focal variable was the payor status of the patient. A latent variable logistic approach was specified4:
The vector of patient-level controls coincided with those of the risk models (below). Other controls included dummy indicators for facility and calendar year of admission. Models were estimated using maximum likelihood and conventional standard errors throughout. Multivariate-adjusted odds ratios were computed for the focal variable of payor status, where an estimated odds ratio less than one implies that the event is less likely to happen and conversely. Medicare FFS was the referent category.5
Physician Ranking Method
Each patient admission at a particular hospital was observed to match to a treating physician. A set was constructed of all possible alternative matches to other physicians observed to work at that facility in that quarter.
There were 1,083 choice sets, each corresponding to a hospital*quarter dyad. The average admission faced a feasible choice set of approximately eight treating physicians who met the minimum caseload requirements above. Every physician in that choice set was initially ranked separately on average risk-adjusted in-hospital mortality (mortality) and average risk-adjusted length of stay (LOS).
In exploratory analysis, a large number of physicians (282 of 486) had zero mortality over the entire panel, resulting in 88 choice sets in which every treating physician had zero mortality. This lack of variation would tend to bias the results to the null (since in these choice sets there can be no difference in use among differently insured).
An alternative composite outcome measure was used to complement the mortality measure. “Home” was defined as live discharge directly to the patient's own home, neither requiring home health care nor transfer to a skilled nursing facility or subacute convalescent hospital.6 Figure SA2 and Figure SA3 document the median profile and the interquartile range of physician profiles across the choice sets. Substantial variation in physician profiles across and within choice sets is noted.7
In different specifications these measures were either risk-adjusted or crude unadjusted measures, and they were computed based on all the physician's patients in the analysis dataset or just the patients in the year of admission. No qualitative changes in the findings were observed across these different specifications; findings reported here are based on risk-adjusted measures for all of the included panel data.
Risk Models
Risk models were used to control for differences in case mix between physicians. The sensitivity of a physician's average mortality profile to his or her case mix has long been known. More recently, risk adjustment of LOS data has been used to benchmark hospital efficiency (Saleh, Hannan, and Racz 2008). Cowper et al. (2001) point out that economic profiles of interventional cardiologists may not be comparable if they are not adjusted for case mix.
The LOS model used in this study uses patient record data on race, age, median earnings in the zipcode, urgency of admission, source of admission, indicators for the facility, year, and DRG code. A limited number of medical comorbidity covariates are included, where these are more likely to be ex ante present on admission as opposed to complications arising ex interim (see Appendix SA1). An ordinary least-squares regression on actual patient LOS explained 21.2 percent of the variability in hospital stay lengths.
The fitted values from this model were used as expected values for each patient. The risk-adjusted LOS for each physician was computed by dividing the actual aggregate LOS by the aggregate expected LOS, normalized by multiplication with the average LOS in the data.
An analogous procedure was used to generate risk-adjusted mortality and risk-adjusted live discharges home for each physician, using a probit regression and including the same covariates as the LOS model. These risk models were also relatively robust, with pseudo R2 of 24.9 and 19.5 percent, respectively. No risk models contained payor status as a covariate.
FINDINGS
In Table 1 baseline characteristics of the analysis patient population are shown. The most obvious differences between patients insured by MFFS and MMC are in demographics. MMC patients come from a significantly more ethnically diverse background with 16 percent Hispanic and 9 percent black (cf. 6 and 6 percent, respectively, for MFFS).
Table 1.
Baseline Characteristics of the Study Population by Payor Status
| MFFS | MMC | FFS and PPO | HMO | Self-pay | All | |
|---|---|---|---|---|---|---|
| (n=33,840) | (n=6,626) | (n=11,043) | (n=7,856) | (n=2,520) | (n=67,476) | |
| Observed outcomes | ||||||
| Length of stay (days) | 4.2 | 4.1 | 3.3 | 3.2 | 3.5 | 3.9 |
| Discharged: home | 85 | 87*** | 97 | 97 | 97 | 90 |
| Home health care | 8 | 8 | 1 | 2 | 1 | 6 |
| Skilled nursing care | 4 | 3** | 0 | 0 | 0 | 3 |
| Subacute hospital | 2 | 1*** | 1 | 1 | 1 | 1 |
| Died in hospital | 0.6 | 0.7 | 0.2 | 0.1 | 0.5 | 0.5 |
| Expected outcomes | ||||||
| Length of stay | 3.9 | 4.0*** | 3.8 | 3.9 | 3.9 | 3.9 |
| Discharge home | 90 | 89** | 91 | 90 | 90 | 90 |
| In-hospital death | 0.58 | 0.63*** | 0.4 | 0.5 | 0.4 | 0.5 |
| Demographics | ||||||
| Male gender | 56 | 59*** | 72 | 73 | 72 | 62 |
| Ethnicity or race: white | 85 | 71*** | 83 | 76 | 68 | 80 |
| Hispanic | 6 | 16*** | 7 | 11 | 14 | 9 |
| Black | 6 | 9*** | 6 | 8 | 11 | 7 |
| Median zipcode earnings (1999 U.S.$) | 22,047 | 23,008*** | 22,600 | 23,709 | 21,827 | 22,353 |
| Aged: 55–64 years old | 8 | 8 | 51 | 47 | 38 | 24 |
| 65–74 years | 41 | 43** | 9 | 8 | 5 | 28 |
| >75 years | 48 | 46 | 2 | 3 | 3 | 29 |
| Encounter | ||||||
| Presentation: emergent | 44 | 51*** | 53 | 51 | 64 | 49 |
| Urgent | 35 | 30*** | 30 | 34 | 25 | 33 |
| Elective | 20 | 19*** | 17 | 16 | 11 | 18 |
| Referred by: Emerg. Dept. | 47 | 55*** | 56 | 57 | 68 | 53 |
| Hospital transfer | 12 | 12 | 12 | 10 | 14 | 12 |
| Physician | 38 | 28*** | 30 | 31 | 15 | 32 |
| Comorbidities | ||||||
| Chronic disease count | 6.3 | 6.1*** | 5.6 | 5.5 | 5.6 | 6.1 |
| Diabetes | 33 | 36*** | 29 | 32 | 28 | 33 |
| Hypertension | 62 | 67*** | 61 | 63 | 58 | 62 |
| COPD | 17 | 14*** | 8 | 7 | 10 | 14 |
| Liver disease | 1 | 1 | 2 | 2 | 2 | 1 |
| Fluid disorder | 8 | 8 | 6 | 5 | 7 | 7 |
| Coagulopathy | 3 | 3 | 2 | 2 | 1 | 2 |
| Prior neurological disease | 3 | 3 | 2 | 2 | 2 | 3 |
| Prior malignancies | 10 | 9 | 4 | 4 | 3 | 7 |
| Procedures | ||||||
| Pacemaker inserted | 1 | 1 | 1 | 1 | 1 | 1 |
| Catheterized | 85 | 90*** | 90 | 91 | 92 | 88 |
| Drug eluting stent | 85 | 89*** | 89 | 90 | 88 | 87 |
| DRG (all without AMI) | ||||||
| 517 (Stent, BMS) | 15 | 11*** | 11 | 10 | 12 | 13 |
| 527 (Stent, DES) | 46 | 43*** | 43 | 45 | 31 | 44 |
| 557 (DES, w. Maj. CV Diag.) | 23 | 28*** | 29 | 28 | 44 | 27 |
| 558 (DES, w/o Maj. CV Diag.) | 15 | 18*** | 17 | 17 | 14 | 16 |
Notes. Patient level means. Medicaid (1,842) and Medicaid MC (710 patients) suppressed. Excludes patients with<2 days stay, acute myocardial infarction (AMI) DRGs, patients of physicians performing less than 10 cases/quarter or observed less than two quarters.
BMS, bare-metal stent; COPD, chronic obstructive pulmonary disease; DES, drug-eluting stent; FFS, fee for service; HMO, health maintenance organization; MC, managed care; PPO, preferred provider organization.
p<.001
p<.01
*p<.05 indicate Wilcoxon's signed rank two-sided test of significance between MFFS and MMC.
Even after the aggressive winnowing of the data to exclude short-stay admissions and AMI presentations, MMC patients present emergently more often. They also tend to come more through the ER than via a physician's referral. Whether this is correlated with slower presentations or poorer preadmission care is unknown in this data.8 Expected outcomes by payor type are consistent with observably sicker MMC patients: longer expected admissions, lower expected discharge rate directly home, higher expected in-hospital death rate.
Physician Characteristics
This study's hypotheses imply that MMC payors select physicians with different profiles or such physicians self-select to MMC payors. This in turn makes a nonuniform distribution of MMC patients across physicians necessary, and it may also lead to differences in observable physician characteristics. While the former was supported, the latter was not.
Analysis of the physicians' patient bases showed that 76 of 486 physicians saw no MMC patients at all over the panel, while another 85 had more than 20 percent of their patients insured by MMC. Those physicians who saw a larger proportion of Medicare MC patients in their practice tended to also see larger proportions of Medicaid MC (Pearson correlation 0.22, p<.001) and commercial HMO insured patients (0.23, p<.001). They tended to see lower proportions of traditional Medicare (−0.69, p<.001) or commercial FFS and PPO patients (−0.42, p<.001). There was no significant association between overall caseload and the proportion of patients insured by different insurers.
Categorizing physicians by quintiles in Table 2 shows the nonuniform distribution of MMC patients across physicians. Quintile 1 represents physicians with negligible MMC patients, while physicians in quintile 5 have on average 28 percent of their total patients insured by MMC, and as much as 74 percent.
Table 2.
Physician Characteristics by Increasing Medicare Managed Care Payor Mix
| Categories of physicians by their payor mix (Quintiles of MMC cases/total cases) |
|||||
|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | Q5 | |
| Cutoffs for Medicare MC payor mix | (0%–0.7%) | (0.7%–3.2%) | (3.2%–7.7%) | (7.9%–17.1%) | (17.4%–74.0%) |
| Payor mix | |||||
| Medicare MC | 0 | 2 | 5 | 13 | 28*** |
| Medicare FFS | 62 | 59 | 55 | 44 | 33*** |
| Private FFS and PPO | 20 | 18 | 18 | 14 | 12*** |
| Private HMO | 7 | 9 | 12 | 15 | 15*** |
| Selfpay | 4 | 3 | 3 | 4 | 4*** |
| Medicaid | 3 | 3 | 2 | 3 | 3 |
| Medicaid MC | 0 | 1 | 1 | 2 | 2*** |
| Treating physician characteristics | |||||
| Trained overseas | 6 | 6 | 13 | 10 | 8*** |
| Last training (year) | 1990 | 1991 | 1993 | 1992 | 1990 |
| Trained as internist | 96 | 92 | 90 | 93 | 96 |
| Trained as cardiologist | 85 | 87 | 88 | 89 | 89*** |
| Trained as interventionalist | 33 | 28 | 34 | 35 | 14*** |
| IM certificates (number) | 2.0 | 1.8 | 1.9 | 1.8 | 1.7*** |
| Cardiology certificates (number) | 1.3 | 1.2 | 1.3 | 1.1 | 1.1*** |
| Interventionalist certificates (number) | 0.4 | 0.3 | 0.4 | 0.2 | 0.2*** |
| Group practice size (total partners) | 7 | 7 | 5 | 5 | 3*** |
| Holds staff privileges (number) | 2.2 | 2.2 | 2.7 | 3.1 | 3.2*** |
| Other state licenses (number) | 1.2 | 0.9 | 1.2 | 0.5 | 1.0*** |
| Holds faculty appointment | 7 | 9 | 13 | 25 | 15*** |
| Used DES in 2003 Q1 | 1 | 1 | 0 | 6 | 15*** |
| Patient demographics | |||||
| Male gender | 61 | 63 | 62 | 62 | 63*** |
| White | 89 | 85 | 83 | 73 | 68*** |
| Black | 7 | 7 | 7 | 8 | 8*** |
| Hispanic | 2 | 4 | 6 | 15 | 18*** |
| Aged 55–64 years | 24 | 24 | 25 | 25 | 22*** |
| 65–74 years | 29 | 28 | 27 | 27 | 28* |
| Older than 75 years | 29 | 29 | 30 | 28 | 32*** |
| Median earnings zipcode (1999 U.S.$) | 21,363 | 21,612 | 22,136 | 23,237 | 23,406*** |
| Presentation | |||||
| Emergent | 46 | 49 | 44 | 53 | 53*** |
| Urgent | 40 | 33 | 35 | 25 | 31*** |
| Referred by ER department | 51 | 53 | 50 | 55 | 55*** |
| Referred by physician | 36 | 34 | 35 | 32 | 27*** |
| Transferred from other hospital | 12 | 11 | 12 | 11 | 14*** |
| Selected comorbidities | |||||
| Chronic diseases (count) | 6.1 | 6.1 | 6.0 | 6.2 | 6.0*** |
| Diabetes | 31 | 33 | 31 | 34 | 34*** |
| COPD | 15 | 14 | 13 | 14 | 13*** |
| Chronic kidney disease | 3 | 3 | 3 | 4 | 4** |
| Any malignancies | 7 | 8 | 7 | 6 | 8*** |
| DRG (all without AMI) | |||||
| 517 (Stent, BMS) | 15 | 15 | 13 | 13 | 11*** |
| 527 (Stent, DES) | 45 | 46 | 42 | 43 | 44 |
| 557 (DES, w. Maj. CV Diag.) | 24 | 24 | 27 | 28 | 29*** |
| 558 (DES, w/o Maj. CV Diag.) | 16 | 15 | 17 | 16 | 15 |
Notes. Patient-weighted means (%, unless otherwise indicated). Quintiles are categories of physicians by increasing MMC payor mix computed over their patients in the restricted panel of 67,476 patients. Patients; physicians in each quintile: Q1 (13,184; 98), Q2 (14,186; 97), Q3 (12,927; 97), Q4 (12,508; 97) and Q5 (14,671; 97).
p<.001
p<.01
p<.05 indicate Wilcoxon signed rank two-sided test of significance between Q1 and Q5.
However, physicians who had a high proportion of MMC patients in their practice did not differ dramatically from their colleagues.9 The most important variables may be volume and experience. Counting all stent cases performed between 2003 and 2006 shows that the lowest (highest) quintile physicians averaged 392 (472) total cases. On average those seeing the fewest (most) MMC patients performed 30 (35) cases per quarter. Physicians who are more likely to see MMC insured patients thus have more stent experience and practice more frequently. In theory, the benefits of experience economies should accrue to their patients.
While many statistically significant differences in physician characteristics are found between the lowest and highest quintiles, these are unlikely to have substantial clinical meaning. Notably, physicians across the quintiles have similar training, while those with the highest MMC caseload in their practices tend to hold faculty appointments.
They had earlier access to the new DES stents, before marketing approval in the second quarter of 2003. This suggests close integration into the specialty and a propensity to adopt leading-edge technologies. On balance these differences did not support a contention that physicians who perform more MMC insured stent cases were of observably lower quality.
Use of Faster Discharging Physicians
The impact of payor type on the use of differently ranked physicians is shown in Table 3, where each row is a separately estimated model.
Table 3.
Odds of Use of Differently Profiled Physicians by Payor Status
| Payor Type |
|||||
|---|---|---|---|---|---|
| Rank of Physician Used and Ranking Criteria | Medicare FFS | Medicare MC | FFS & PPO | HMO | Self-pay |
| (n=33,840) | (n=6,626) | (n=11,043) | (n=7,856) | (n=2,520) | |
| By length of stay | |||||
| Lowest one | 1.00 (referent) | 1.03 (0.94–1.14) | 1.12 (1.01–1.23) * | 1.17 (1.05–1.30) ** | 0.92 (0.79–1.08) |
| Lowest quartile | 1.00 (referent) | 0.96 (0.90–1.02) | 0.98 (0.94–1.02) | 0.95 (0.91–0.99) | 0.90 (0.84–0.96) |
| Next quartile | 1.00 (referent) | 1.09 (1.03–1.16) ** | 1.05 (0.98–1.12) | 1.02 (0.95–1.09) | 0.98 (0.89–1.09) |
| Below median | 1.00 (referent) | 1.01 (0.95 –1.06) | 1.08 (1.02–1.15) ** | 1.03 (0.96–1.10) | 0.95 (0.86–1.04) |
| Next quartile | 1.00 (referent) | 1.01 (0.95–1.08) | 0.89 (0.83–0.94) *** | 1.00 (0.93–1.07) | 1.00 (0.91–1.01) |
| Highest quartile | 1.00 (referent) | 0.96 (0.91–1.03) | 0.98 (0.92–1.05) | 0.93 (0.87–1.00) | 1.06 (0.96–1.18) |
| Highest one | 1.00 (referent) | 0.92 (0.83–1.00) | 1.06 (0.96–1.15) | 0.96 (0.86–1.07) | 1.16 (1.01–1.13) * |
| By mortality | |||||
| Lowest one | 1.00 (referent) | 0.89 (0.84–0.95) *** | 1.01 (0.94–1.07) | 0.95 (0.89–1.02) | 0.96 (0.87–1.07) |
| Lowest quartile | 1.00 (referent) | 0.90 (0.84–0.95) ** | 1.02 (0.95–1.08) | 0.96 (0.89–1.03) | 0.97 (0.89–1.03) |
| Next quartile | 1.00 (referent) | 0.88 (0.83–0.93) *** | 1.02 (0.96–1.09) | 1.00 (0.96–1.09) | 0.96 (0.87–1.06) |
| Below median | 1.00 (referent) | 0.89 (0.84–0.94) *** | 1.01 (0.95–1.07) | 0.99 (0.93–1.06) | 0.96 (0.87–1.07) |
| Next quartile | 1.00 (referent) | 1.19 (1.12–1.27) *** | 1.07 (1.00–1.04) * | 1.11 (1.04–1.19) ** | 1.02 (0.92–1.12) ** |
| Highest quartile | 1.00 (referent) | 0.96 (0.91–1.03) | 1.01 (0.95–1.08) | 0.96 (0.89–1.03) | 1.04 (0.94–1.16) |
| Highest one | 1.00 (referent) | 1.12 (1.02–1.22) * | 1.06 (0.97–1.16) | 1.04 (0.94–1.15) | 0.96 (0.84–1.11) |
| By discharged home | |||||
| Lowest one | 1.00 (referent) | 0.88 (0.80–0.97) ** | 0.93 (0.85–1.02) | 0.96 (0.87–1.07) | 0.97 (0.85–1.12)) |
| Lowest quartile | 1.00 (referent) | 0.91 (0.86–0.97) ** | 0.94 (0.88–1.00) | 0.95 (0.88–1.02) | 0.95 (0.87–1.05) |
| Next quartile | 1.00 (referent) | 1.25 (1.18–1.33) *** | 0.99 (0.93–1.05) | 1.10 (1.02–1.18) | 1.03 (0.93–1.14) |
| Below median | 1.00 (referent) | 1.12 (1.06–1.19) *** | 0.93 (0.88–0.99) * | 1.02 (0.95–1.09) | 0.99 (0.90–1.09) |
| Next quartile | 1.00 (referent) | 0.96 (0.90–1.02) | 1.03 (0.96–1.11) | 1.03 (0.96–1.11) | 1.00 (0.90–1.11) |
| Highest quartile | 1.00 (referent) | 0.94 (0.88–1.00) | 1.07 (1.00–1.14) * | 0.95 (0.88–1.02) | 1.05 (0.95–1.17) |
| Highest one | 1.00 (referent) | 0.91 (0.82–1.00) * | 1.03 (0.93–1.13) | 0.93 (0.84–1.14) | 1.02 (0.88–1.18) |
Notes. Each row represents a separately estimated multivariate logistic regression model with dependent variable an indicator for the rank of the physician used within the facility peer group that period. Reported statistics are multivariate adjusted odds ratios and 95% confidence intervals using conventional standard errors. Physician measures of admission length and mortality are their panel averages, adjusted for risk and compared to facility peer group in quarter of admission. Other model covariates suppressed. Medicaid and Medicaid MC suppressed.
FFS, fee for service; HMO, health maintenance organization; MC, managed care; PPO, preferred provider organization.
p<.001
p<.01
p<.05, two-sided tests of significance.
The estimated odds ratios (with MFFS as the referent payor type) for the focal payor status variables are reported, while control covariates were suppressed.10 Charity patients were excluded from the multivariate logistic usage models since the focus was on the effects of the type of insurance as opposed to the presence of insurance. The small number of Workman's Compensation, CHAMPUS, and VA patients was also excluded. The factors determining choice sets for these payors were unlikely to be the same as for the Medicare and commercially insured populations.
The top panel of Table 3 shows that Hypothesis 1 was not supported. There were no consistent differences between MFFS and MMC in the use of physicians whose risk-adjusted average discharges were faster than others in the patient's choice set. The likelihood of using a physician whose LOS profile was below median compared with his or her peers appeared the same for MMC and MFFS patients (OR 1.01, p=.852).11
Use of Higher Mortality Physicians
Hypothesis 2 predicted that MMC patients would use physicians with no worse outcome profiles. In the middle panel of Table 3 analogous models show the use of physicians ranked in terms of their risk-adjusted mortality profile within the facility peer group. There were consistent and precisely estimated differences between MFFS and MMC stent patients.
MMC patients were significantly less likely to see a physician whose mortality profile was below median (OR 0.89, p<.001) or the absolute lowest mortality (OR 0.89, p<.001). On the other hand, the probability of seeing the absolute highest mortality stent physician was much higher for MMC than MFFS patients (OR 1.12, p<.05).
There is a large number of physicians with zero mortality. If the estimates of a physician's risk-adjusted mortality ratio (RAMR) are precise, this imparts a conservative bias to our tests for the use of lower mortality physicians (who are then “overrepresented” in the choice sets, reducing the possible differences among differently insured).
However, if they tended to have lower volumes, then higher sampling variation could bias rankings of estimated RAMR. Although there was no statistically persuasive relationship between volume and risk-adjusted mortality ratios (Pearson correlation 0.017, p=.718), we investigated this further with an alternative ranking approach.
For each physician we tested the difference between 1 and his or her ratio of observed to expected deaths (Liu et al. 2003). For example, a physician with unexpectedly low (but nonzero) mortality would have a negative z score in this approach. Since many RAMR are zero, we added a small positive fraction (0.25) to all observed deaths to avoid having a zero variance term in the z test calculation.12 We then reranked every physician in each choice set by their z scores, and the differences between this ranking and the original one is shown in Figure SA1. Those physicians with zero mortality had rankings closer to the middle of the distribution.13
There are no optimal ranking approaches, and this alternative method has a countervailing bias. Using statistical tests of the difference between observed and expected mortality rates can unfairly penalize high-volume physicians for whom such tests have greater power.14 However, using this alternative approach the estimated odds ratios for seeing differently ranked physicians by peer group mortality test z scores were qualitatively unchanged to those reported originally (see Appendix Table SA3). Since our results using the alternative ranking scheme were similar to those obtained using the original ranking scheme, we conclude that the mortality results are robust to both of the countervailing biases mentioned earlier.
Use of Physicians with Higher Direct Home Live Discharges
In the lower panel of Table 3 similar models show the use of physicians ranked in terms of their risk-adjusted home discharge profile within the facility peer group. This outcome represents live discharges that neither required a follow-on stay in a skilled nursing facility or subacute hospital nor required home health care support.
Higher quality profiles in this dimension are ones that are above median relative to other physicians and were predicted to be used by MMC patients under Hypothesis 2. However, MMC patients were significantly more likely to see a physician whose home discharge profile was below median (OR 1.12, p<.001) and significantly less likely to see one whose home discharge profile was the best in the choice set (OR 0.91, p<.05).15
Refutability Analyses: Selection and Composition Biases
In Figure 1 possible selection and composition biases were outlined. Of particular concern were physician selection of patients (and vice versa), patient self-selection into plans, and unobserved patient heterogeneity. To address the first, subpopulations within the data were reanalyzed (Angrist and Krueger 1999). To investigate the second, stratified analyses were conducted by propensity for having MMC payor status. To understand the third, separate risk models were computed by ethnicity, physicians were reranked, and usage reestimated.
Physician selection of patients or vice versa is less feasible when a patient presents both on an emergency basis and via the emergency department. The observed use of a particular physician is plausibly exogenous in this subpopulation, and patients should have similar likelihoods of seeing a physician whose profiles involve longer average stays or better average outcomes. However, essentially the same results were found in this smaller subsample (see Appendix Table SA1).
Similarly, physician selection of patients could be accentuated when the treating physician is also the attending physician. This subpopulation included plausibly endogenous cases where a physician has self-referred a patient for a stent procedure. Reanalysis in this subset of patients found, however, qualitatively similar results (see Appendix Table SA2). Despite the substantially decreased sample size, estimates remained precise.
Patient self-selection into plans is possible, and it is consistent with the differences in patient characteristics by payor type in Table 1. Such self-selection may be responsible for the obtained results. To investigate this, a propensity score stratified analysis was performed.16 A logistic model was specified with plausible determinants of payor status (e.g., gender, age, median zipcode earnings) and an indicator of MMC status as the dependent variable. The fitted values from this regression were used as propensity scores and 10 blocks were created with similar propensities and balanced covariates.
The odds of seeing a below median mortality profile physician was estimated within each stratum (results available on request). The combined odds ratio for Medicare MC across the strata was computed by weighting each stratum's estimate by the inverse of its standard error. This result did not differ qualitatively from that obtained in Table 3. However, this approach maintains the very strong assumption that assignment of MMC status was random conditional on several observable covariates. If selection occurs—as is likely—on unobservables, use of a propensity score analysis is inappropriate.
Unobserved patient heterogeneity was also investigated, given the imbalance of ethnicities between MFFS and MMC. Individual risk models were estimated for white, Hispanic, and black patients. Appendix SA1 describes the substantial differences in the estimated risk models by ethnicity. Using these tailored risk models, physician risk-adjusted mortality was recomputed and the main usage equations were re-estimated. Point estimates for the odds of using different ranked physicians were directionally similar, but odds ratios were estimated substantially less precise at p<.01. When analysis was restricted to the Hispanic or black subpopulations, estimated odds ratios for MMC insured patients were statistically indistinguishable from 1. However, results for the white subpopulation were qualitatively similar to the main results in Table 3, suggesting that unobserved patient heterogeneity may remain.
DISCUSSION
This study's results were unexpected and did not confirm the hypotheses that managed care insurers are able to procure more efficient and (weakly) higher quality stent physicians for their members. No evidence was found that Medicare payor type significantly influenced the likelihood of using physicians with different admission length profiles. Instead, MMC subscribers had significantly worse odds of seeing those physicians with favorable outcome profiles.
What gave rise to these systematic differences? A process of elimination yields unobserved patient health status as the most likely cause. Consider the conceptual framework of Figure 1, from right to left. Differences in hospital and postprocedure care seem unlikely, given the same admission length profiles of physicians seeing MFFS and those seeing MMC patients.
Physician preferences or payor restrictions on physician type were not supported in subpopulation analyses. In emergency patients, payor restrictions are unlikely to bind and physician preferences are likely inoperative. Yet MMC patients had the same differences in use of physicians with less favorable outcome profiles.
Physician self-selection biases should have been accentuated in those patients where the physician is both treating and attending. These cases account for approximately half of all elective admissions, and plausibly include self-referral cases. Yet here, again, qualitatively similar systematic differences in physician use were found. Similar reasoning suggests that systematic patient decisions at the time of admission are unlikely to produce these results, and the consistency of results argues against chance as an explanation.
By this process of elimination, this study's findings are largely consistent with unobservable adverse MMC member health status leading to marginally worse outcomes. Put differently, observed outcome differences may just be a proxy for unobserved health status or illness severity. Nonuniform concentration of MMC patients among particular physicians then ensures that a typical MMC patient will see a physician whose profiles have become slightly worse over time than his or her peers in the same hospital.
Nothing in this conclusion requires that physicians be differently skilled or provide care differently. Indeed, the analysis of physician characteristics suggests that those seeing many MMC patients are arguably closer integrated into academic and specialist medicine.
The observed differences in patient characteristics across payor types lend support to this conclusion. While Park (2007) argued that MMC enrollees do not tend to be disproportionately from minority racial groups in national data, here significantly more Hispanic patients have opted for MMC.17 In this data, substantial between-ethnic group differences in the risk models were observed, making it more likely that patients differ on unobservables too. An open question is whether poorer, unobservably sicker minority individuals prefer MMC to MFFS because of higher foreseen out-of-pocket expenditures.
LIMITATIONS
This study's analysis had several limitations. Administrative and claims data have well-known data integrity and coding issues, and they provide few controls for demographics. Despite screening and validation, it is unknown to what degree the dataset contained residual systematic errors. Internal validity was limited since analysis focused on an aggressively restricted set of patients.18 Given the data from one state, one disease class, and one procedure, caution is also needed before assuming these conclusions hold more widely.
Outcomes were short term and limited to observing in-hospital mortality and discharge directly home. In-hospital mortality is in general a downwards-biased outcome, a bias in the opposite direction to that found here with MMC patients. For mortality, a standardized endpoint would be preferable to exclude “sick” discharges with mortality at home. The use of the discharge directly home outcome compensated for this somewhat, since it captured discharged patients too sick to return directly home.
CONCLUSIONS
These findings raise questions surrounding the screening, self-selection, and care management of MMC plan members. Such plans offer easily visible choice and cost benefits to potential members. But this is clearly at the expense of taxpayers: MMC plan overpayments now average ∼112 percent of the traditional MFFS costs at the county level (Orszag 2007).
One open policy question is whether MMC plans actually benefit their members from an individual cost-effectiveness perspective, compared with MFFS. Another question is whether such net benefits are fairly distributed across minorities and across different health status segments. This is especially relevant if care management under high-growth variants of MMC (such as “Medicare Advantage Private FFS”) does not address complex underlying health status differences.
These questions clearly matter from a broader societal perspective. MMC plans were once seen as test-beds for innovation, as prudent purchasers and promoters of quality health status improvement.19
Further research into minority and managed care member health status and impact of such factors on risk models and expected outcomes will help to address important individual health services questions such as these. Public policy on the appropriate level of cross-subsidies and the appropriate role of commercial managed care in health entitlement programs would also be informed by such research.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: I am grateful to Bob Kaplan, Michael Ong, Bill Zame, Kevin Schulman, two anonymous reviewers, and the editors for their valuable comments and advice.
Disclosures: None.
Disclaimers: None
NOTES
The assumption is maintained that length of stay proxies hospital resource uses and incurred costs. In this data, there was substantial and significant correlation between total billed hospital charges and length of stay (Pearson correlation=0.79, p<.001).
Lower mortality could also be an artifact for faster-discharging physicians from a competing risks perspective. Any decrease in admission length would tend to censor in-hospital mortality (Ho, Hamilton, and Roos 2000; Clark and Ryan 2002;).
Actual care may be identical across different patients, or become so. Glied and Zivin (2002) find that managed care practice patterns tend to “spillover” within a physician's practice across patients with different insurance status.
The use of naturally ordered outcomes (percentile ranks) suggests ordered logit regression approaches. Unfortunately, standard tests rejected the proportional odds assumption, and the monotonicity assumption a fortiori. Multinomial logit regression produced qualitatively similar results as shown; however, the strong assumption of irrelevance of independent alternatives failed to be validated in most of the specifications.
Reported odds ratios were not adjusted by approximating relative risk. Zhang and Yu (1998) recommend adjustment if both of the following conditions hold: unadjusted odds ratios are outside the range 0.5–2.0 (not met in the findings here) and the rate of the regression outcome exceeds 10 percent (holds by construction for all the quartile and median indicators, not met by the minimum and maximum indicators).
Block et al. (1998) propose same-stay CABG surgery as an alternative outcome measure. In the data used, the “treating physician” field contained the operating cardiac surgeon in those cases. This rendered identification of the treating cardiologist impossible, and thus conversion to CABG surgery was not used as an outcome.
If better physicians had substantively sorted to particular hospitals (lowering the variation within-choice sets but increasing it between-choice sets), this study's focus on relative differences among physicians within a hospital would miss the point.
Cohen et al. (2006) discuss evidence of longer pre-admission delays, and use of self-transportation to reach hospital in Hispanic American patients presenting with non-AMI acute coronary syndrome.
Physicians seeing the most MMC patients tended to see older, more emergent patients coming from an almost threefold higher minority background. This mirrors the observed patient differences by payor in Table 1.
Results were qualitatively similar when standard errors were clustered by payor type. Results reported here all use conventional errors.
Although not the main focus of this study, private FFS and commercial PPO patients had significantly higher odds of using a stent physician with a below median average length of stay or the absolute fastest discharging physician available at their hospital the quarter of their admission.
One could use a Bayesian model for the posterior mean of RAMR to shrink a zero mortality (or a low volume) physician “up” toward a RAMR of 1, but this assumes the conclusion that physicians are all similar after risk adjustment.
We are grateful to a referee for suggesting this approach.
Liu et al. (2003) show this using a Poisson process for mortality that simplifies the algebra. Our risk model is Bernoulli; we sketch the analogous result as follows. Let the count of observed deaths≡X be a binomial process with parameters n and p. Assume the count of expected deaths is exogenously given by Y=ns from an independent population binomial process with parameters n and s. We are interested in whether RAMR≡X/Y=1 ⇔ RAMR–1=0. The variance of X is np(1−p), so variance of RAMR will be np(1−p)/(n2s2). Hence, the z-test statistic will be (X/Y−1)(s√n/(√p√(1−p))). Replacing p with its sample analog, and s with its observed value, it is evident that the lower the variance of the RAMR estimates, ceteris paribus, the larger are the z test statistics.
A bidimensional ranking was also used in robustness tests. Here, the odds of seeing a physician with below median length of stay and better than median outcomes were investigated. Results were qualitatively unchanged from those reported in the one-dimensional specifications.
In a similar vein, a linearized “treatment regression” model was specified. One equation estimates the likelihood of the binary “treatment” variable (MMC payor status) as a function of one set of independent variables, while another estimates the outcome of interest as a function of the treatment and a separate subset of covariates. Equations were assumed linked by bivariate normal distributed errors. Estimation by maximum likelihood failed to converge.
Research by Cohen et al. (2006) found that Hispanic patients presenting with non-ST segment elevation acute coronary syndromes had a different risk profile than non-Hispanic whites, with for example significantly higher admission systolic blood pressure. Jha et al. (2008) find between-hospital differences in elderly Hispanic treatment, but this is washed out by this study's within-hospital analysis.
In earlier, unreported analyses on the entire 221,090 records qualitatively similar results were obtained for the mortality outcome. However, MMC patients also had significantly higher odds of seeing faster-discharging physicians than MFFS patients.
Nancy Ann De Parle, currently director of the White House Office of Health Reform, has commented (2002, pp. 510–11) that MMC plans “… can teach us important things that we need to understand.” The private Medicare Advantage plans were claimed to have “done a slightly better job of promoting quality in service delivery and in improving the health status of beneficiaries. … [They] arguably have more leeway to engage in these activities than [Medicare] will ever have.”
Supporting Information
Additional supporting information may be found in the online version of this article:
Appendix SA1: Data and Risk Model Validation.
Table SA1: Subpopulation Analysis. Odds of Use of Differently Profiled Physicians—Admitted via ER as Emergency.
Table SA2: Subpopulation Analysis: Odds of Use of Differently Profiled Physicians—Treating Physician Was Also Attending.
Table SA3: Odds of Use of Physicians Ranked by Z Scores of the Hypothesis That Observed Deaths = Expected Deaths.
Figure SA1: Relationship between Overall Panel Rankings by RAMR and by Z Score.
Figure SA2: Distribution of Physician Profiles across Choice Sets—Medians.
Figure SA3: Distribution of Physician Profiles across Choice Sets—IQRs.
Please note: Wiley-Blackwell is not responsible for the content or functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
REFERENCES
- Angrist JD, Krueger AB. Empirical Strategies in Labor Economics. In: Ashenfelter O, Card D, editors. Handbook of Labor Economics Volume 3. Amsterdam: Elsevier; 1999. pp. 1277–366. [Google Scholar]
- Anthony DL, Herndon MB, Gallagher PM, Barnato AE, Bynum JPW, Gottlieb DJ, Fisher ES, Skinner JS. How Much Do Patients' Preferences Contribute to Resource Use? Health Affairs. 2009;28(3):864–73. doi: 10.1377/hlthaff.28.3.864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arrow K. Uncertainty and the Welfare Economics of Medical Care. American Economic Review. 1963;53:941–73. [Google Scholar]
- Block PC, Peterson ED, Krone R, et al. Identification of Variables Needed to Risk Adjust Outcomes of Coronary Interventions: Evidence-based Guidelines for Efficient Data Collection. Journal of the American College of Cardiology. 1998;32:275–82. doi: 10.1016/s0735-1097(98)00208-3. [DOI] [PubMed] [Google Scholar]
- Bundorf MK, Schulman KA, Stafford JA, Gaskin D, Jollis JG, Escarce JJ. Impact of Managed Care on the Treatment, Costs, and Outcomes of Fee-for-Service Medicare Patients with Acute Myocardial Infarction. Health Services Research. 2004;39(1):131–52. doi: 10.1111/j.1475-6773.2004.00219.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen AY, Escarce JJ. Quantifying Income-related Inequality in Healthcare Delivery in the United States. Medical Care. 2004;42(1):38–47. doi: 10.1097/01.mlr.0000103526.13935.b5. [DOI] [PubMed] [Google Scholar]
- Clark DE, Ryan LM. Concurrent Prediction of Hospital Mortality and Length of Stay from Risk Factors on Admission. Health Services Research. 2002;37(3):631–45. doi: 10.1111/1475-6773.00041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen M, Roe M, Mulgund J, Peterson E, Sonel A, Menon V, Smith S, Jr., Saucedo J, Lytle B, Pollack C. Clinical Characteristics, Process of Care, and Outcomes of Hispanic Patients Presenting with Non–ST-Segment Elevation Acute Coronary Syndromes: Results From Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes with Early Implementation of the ACC/AHA Guidelines (CRUSADE) American Heart Journal. 2006;152(1):110–7. doi: 10.1016/j.ahj.2005.09.003. [DOI] [PubMed] [Google Scholar]
- Cowper PA, Peterson ED, DeLong ER, Wightman MB, Wawrzynski RP, Muhlbaier LH, Sketch Jr MH. The Impact of Statistical Adjustment on Economic Profiles of Interventional Cardiologists. Journal of the American College of Cardiology. 2001;38(5):1416–23. doi: 10.1016/s0735-1097(01)01538-8. [DOI] [PubMed] [Google Scholar]
- Cutler DM, McClellan M, Newhouse JP. How Does Managed Care Do It? The RAND Journal of Economics. 2000;31(3):526–48. [PubMed] [Google Scholar]
- De Parle NA. As Good as It Gets? The Future of Medicare+Choice. Journal of Health Politics, Policy, and Law. 2002;27(3):495–512. doi: 10.1215/03616878-27-3-495. [DOI] [PubMed] [Google Scholar]
- Enthoven AC. Shattuck Lecture—Cutting Cost without Cutting the Quality of Care. New England Journal of Medicine. 1978;298(22):1229–38. doi: 10.1056/NEJM197806012982204. [DOI] [PubMed] [Google Scholar]
- Erickson LC, Torchiana DF, Schneider EC, Newburger JW, Hannan EL. The Relationship between Managed Care Insurance and Use of Lower-mortality Hospitals for CABG Surgery. Journal of the American Medical Association. 2000a;283(15):1976–82. doi: 10.1001/jama.283.15.1976. [DOI] [PubMed] [Google Scholar]
- Erickson LC, Wise PH, Cook EF, Beiser A, Newburger JW. The Impact of Managed Care Insurance on Use of Lower-mortality Hospitals by Children Undergoing Cardiac Surgery in California. Pediatrics. 2000b;105:1271–8. doi: 10.1542/peds.105.6.1271. [DOI] [PubMed] [Google Scholar]
- Escarce JJ, Jain AK, Rogowski J. Hospital Competition, Managed Care, and Mortality after Hospitalization for Medical Conditions: Evidence from Three States. Medical Care Research Review. 2006;63:112–40. doi: 10.1177/1077558706293839. [DOI] [PubMed] [Google Scholar]
- Escarce JJ, Van Horn RL, Pauly MV, Williams SV, Shea JA, Chen W. Health Maintenance Organizations and Hospital Quality for Coronary Artery Bypass Surgery. Medical Care Research Review. 1999;56:340–62. doi: 10.1177/107755879905600304. [DOI] [PubMed] [Google Scholar]
- Every NR, Cannon CP, Granger C. Influence of Insurance Type on the Use of Procedures, Medications and Hospital Outcome in Patients with Unstable Angina: Results from the GUARANTEE Registry. Journal of the American College Cardiology. 1992;32:387–92. doi: 10.1016/s0735-1097(98)00254-x. [DOI] [PubMed] [Google Scholar]
- Flynn KE, Smith MA, Davis MK. From Physician to Consumer: The Effectiveness of Strategies to Manage Health Care Utilization. Medical Care Research Review. 2002;59:455–81. doi: 10.1177/107755802237811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaskin DJ, Escarce JJ, Schulman KA, Hadley J. The Determinants of HMOs' Contracting with Hospitals for Bypass Surgery. Health Services Research. 2002;37(4):963–84. doi: 10.1034/j.1600-0560.2002.61.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geweke J, Gowrisankaran G, Town RJ. Bayesian Inference for Hospital Quality in a Selection Model. Econometrica. 2003;71(4):1215–38. [Google Scholar]
- Glied S, Zivin JG. How Do Doctors Behave When Some (But Not All) of Their Patients Are in Managed Care? Journal of Health Economics. 2002;21(2):337–53. doi: 10.1016/s0167-6296(01)00131-x. [DOI] [PubMed] [Google Scholar]
- Goldman DP. Managed Care as a Public Cost-containment Mechanism. The RAND Journal of Economics. 1995;26(2):277–95. [PubMed] [Google Scholar]
- Hannan EL. Commentary. Medical Care Research Review. 1999;56:363–72. [Google Scholar]
- Ho V, Hamilton BH, Roos LL. Multiple Approaches to Assessing the Effects of Delays for Hip Fracture Patients in the United States and Canada. Health Services Research. 2000;34(7):1499–518. [PMC free article] [PubMed] [Google Scholar]
- Jha AK, Orav EJ, Dobson A, Book RA, Epstein AM. Measuring Efficiency: The Association of Hospital Costs and Quality of Care. Health Affairs. 2009;28(3):897–906. doi: 10.1377/hlthaff.28.3.897. [DOI] [PubMed] [Google Scholar]
- Jha AK, Orav EJ, Zheng J, Epstein AM. The Characteristics and Performance of Hospitals that Care for Elderly Hispanic Americans. Health Affairs. 2008;27(2):528–37. doi: 10.1377/hlthaff.27.2.528. [DOI] [PubMed] [Google Scholar]
- Liu J, Louis TA, Pan W, Ma JZ, Collins AJ. Methods for Estimating and Interpreting Provider-specific Standardized Mortality Ratios. Health Services Outcomes Research Methodologies. 2003;4(3):135–49. doi: 10.1023/B:HSOR.0000031400.77979.b6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luft HS. Variations in Patterns of Care and Outcomes after Acute Myocardial Infarction for Medicare Beneficiaries in Fee-for-service and HMO Settings. Health Services Research. 2003;38(4):1065–79. doi: 10.1111/1475-6773.00163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller RH, Luft HS. HMO Plan Performance. Update: An Analysis of the Literature, 1997–2001. Health Affairs. 2002;21(4):63–86. doi: 10.1377/hlthaff.21.4.63. [DOI] [PubMed] [Google Scholar]
- Newhouse JP. Consumer-directed Health Plans and the RAND Health Insurance Experiment. Health Affairs. 2004;23(6):107–13. doi: 10.1377/hlthaff.23.6.107. [DOI] [PubMed] [Google Scholar]
- Orszag P. 2007. “CBO Testimony before the House Budget Committee, June 28, 2007: The Medicare Advantage Program” [accessed on December 9, 2009]. Congressional Budget Office. Available at http://www.cbo.gov/ftpdocs/82xx/doc8265/06-28-MedicareAdvantage.pdf.
- Park E. 2007. Informing the Debate about Curbing Medicare Advantage Overpayments.” [accessed on December 9, 2009]. Center on Budget and Policy Priorities. Report. Available at http://www.cbpp.org/7-19-07health.pdf.
- Rainwater JA, Romano PS. What Data Do California HMOs Use to Select Hospitals for Contracting? American Journal of Managed Care. 2003;9:553–61. [PubMed] [Google Scholar]
- Resnic FS. The Case for Outpatient Coronary Intervention: Balancing Charges and Discharges. Circulation. 2007;115:2248–50. doi: 10.1161/CIRCULATIONAHA.107.696286. [DOI] [PubMed] [Google Scholar]
- Rice T, Desmond KA. The Distributional Consequences of a Medicare Premium Support Proposal. Journal of Health Politics Policy and Law. 2004;29:1187–226. doi: 10.1215/03616878-29-6-1187. [DOI] [PubMed] [Google Scholar]
- Rogowski J, Jain AK, Escarce JJ. Hospital Competition, Managed Care, and Mortality after Hospitalization for Medical Conditions in California. Health Services Research. 2007;42(2):682–705. doi: 10.1111/j.1475-6773.2006.00631.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saleh SS, Hannan E, Racz M. Identifying Centers of Excellence in Efficiency and Quality in Coronary Revascularization: An Exploratory Approach for Procedure-specific Value-based Purchasing Program Design. Journal of Health Care Finance. 2008;34(4):42–51. [PubMed] [Google Scholar]
- Schulman KA, Rubenstein LE, Seils DM, Harris M, Hadley J, Escarce JJ. Quality Assessment in Contracting for Tertiary Care Services by HMOs: A Case Study of Three Markets. Joint Commission Journal on Quality Improvement. 1997;23(2):117–27. doi: 10.1016/s1070-3241(16)30304-2. [DOI] [PubMed] [Google Scholar]
- Werner RM, Asch DA, Polsky D. Racial Profiling: The Unintended Consequences of Coronary Artery Bypass Graft Report Cards. Circulation. 2005;111:1257–63. doi: 10.1161/01.CIR.0000157729.59754.09. [DOI] [PubMed] [Google Scholar]
- Xu X, Jensen GA. Health Effects of Managed Care among the Near-elderly. Journal of Aging Health. 2006;18:507–33. doi: 10.1177/0898264306289626. [DOI] [PubMed] [Google Scholar]
- Zhan C, Miller MR, Wong H, Meyer GS. The Effects of HMO Penetration on Preventable Hospitalizations. Health Services Research. 2004;39(2):345–61. doi: 10.1111/j.1475-6773.2004.00231.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J, Yu KF. What's the Relative Risk? A Method of Correcting the Odds Ratio in Cohort Studies of Common Outcomes. Journal of the American Medical Association. 1998;280(19):1690–1. doi: 10.1001/jama.280.19.1690. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.