Abstract
Objective
To update research on Medicare payments in the last year of life.
Data Sources
Continuous Medicare History Sample, containing annual summaries of claims data on a 5 percent sample from 1978 to 2006.
Study Design
Analyses were based on elderly beneficiaries in fee for service. For each year, Medicare payments were assigned either to decedents (persons in their last year) or to survivors (all others).
Results
The share of Medicare payments going to persons in their last year of life declined slightly from 28.3 percent in 1978 to 25.1 percent in 2006. After adjustment for age, sex, and death rates, there was no significant trend.
Conclusions
Despite changes in the delivery of medical care over the last generation, the share of Medicare expenditures going to beneficiaries in their last year has not changed substantially.
Keywords: End-of-life care, Medicare, health care costs, elderly
End-of-life care comprises a large proportion of services funded by the Medicare program, accounting for over one-fourth of Medicare expenditures for the elderly (Lubitz and Riley 1993). The level, types, and intensity of such care have been topics of a considerable amount of research over the last 25 years, both in the United States and in other countries (Lubitz and Prihoda 1984; Riley et al. 1987; Scitovsky 1994; Garber, MaCurdy, and McClellan 1999; Felder, Meier, and Schmitt 2000; Hogan et al. 2001; Stooker et al. 2001; Buntin and Huskamp 2002; Hanratty et al. 2007; Calfo, Smith, and Zezza 2008; Kronman et al. 2008;). Some of the interest in this area comes from the perception that costs can be contained by targeting aggressive and expensive care at the end of life (Emanuel and Emanuel 1994; Scitovsky 1994; Garber, MaCurdy, and McClellan 1998;). Also, research has found problems with end-of-life care, leading many analysts to conclude that existing patterns of care do not meet the needs and preferences of terminally ill patients (The SUPPORT Principal Investigators 1995; Medicare Payment Advisory Commission 1999; Lynn et al. 2000; Teno et al. 2004; Shipman et al. 2008;).
Several developments in the last few decades may have altered patterns of care among dying patients, possibly reducing the percent of Medicare payments incurred in the last year of life. For example, the hospice benefit was introduced to Medicare in 1983 and provides care focusing on palliative and support services for terminally ill patients. Hospice use has increased rapidly in recent years, although evidence of its impact on costs in the last year of life is mixed (Medicare Payment Advisory Commission 2008). In addition, life expectancy has increased among the elderly (Federal Interagency Forum on Aging-Related Statistics 2008). Because acute care costs are lower among persons dying at older ages (Lubitz and Riley 1993; Levinsky et al. 2001;), the percentage of Medicare payments spent on the last 12 months of life may be gradually declining. Changes in medical care related to chronic disease may also have affected the share of Medicare payments going to end-of-life care, given that the highest increases in spending have been among beneficiaries in better health and with fewer functional limitations (Chernew et al. 2005; Thorpe and Howard 2006;).
The purpose of this study is to update research on payments for Medicare services in the last year of life. Previous studies have reported results through the late 1990s and found payments in the last year of life to comprise 26–30 percent of Medicare payments for the elderly (Lubitz and Riley 1993; Hogan et al. 2001; Hoover et al. 2002; Calfo, Smith, and Zezza 2008;). This study updates earlier findings through 2006, using the Continuous Medicare History Sample (CMHS). Use of the CMHS, which covers a 30-year period, also permits long-term trends in patterns of care to be more clearly identified.
DATA AND METHODS
The CMHS contains enrollment and claims data for a 5 percent random sample of the Medicare population (based on the last two digits of the Health Insurance Claim [HIC] number), covering the most recent 30-year period for which data are available. Medicare payment and utilization data are aggregated by type of claim by calendar year; claim-specific data such as diagnoses and procedures are not contained on the file. An indicator for managed care enrollment is included for each year and intensive care unit (ICU) and coronary care unit (CCU) charges from inpatient hospital stays have been aggregated for each year after 1982. Payments for prescription drugs, which Medicare began covering in 2006, are not included in this file. The CMHS is longitudinal, that is, beneficiaries remain on the file until death unless their HIC numbers change and cause them to drop out of the sample.
The file used for this study covered the years 1978–2007; results are presented through 2006, as explained below. Medicare payments for the years 1998–2000 were not accurately recorded in the CMHS because of a programming error. Consequently, the years 1998–2000 were excluded from all analyses. For each study year, the analysis was restricted to beneficiaries who were age 65 and older and were not enrolled in a managed care plan at any time during the year. Managed care enrollees were eliminated from the analysis because Medicare does not receive claims payment data for them. Within the study years, managed care enrollment peaked at 19.5 percent of the CMHS sample in 2006. Annual Medicare payments were inflation adjusted to 2006 using the Consumer Price Index (Bureau of Labor Statistics 2008).
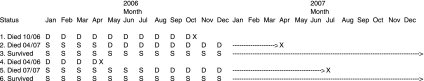
Our primary goal was to assign Medicare payments either to decedents (persons in their last year) or to survivors (all others) for each calendar year, following methods used in an earlier study (Lubitz and Riley 1993). In the case of calendar year 2006, for example, persons who survived through December 31, 2007 were identified as survivors for 2006 (see nos. 3 and 6 in Diagram 1). Their person-years of enrollment in 2006 and all their Medicare payments for services provided in 2006 were assigned to survivors. For persons who died in 2006, person-years of enrollment and payments in 2006 were assigned to decedents (nos. 1 and 4). For those dying in 2007 (nos. 2 and 5), a portion of the payments and person-years of enrollment for calendar 2006 was assigned to survivors and a portion to decedents. The portion assigned to decedents (with the exception of hospice payments, as described below) depended on the proportion of calendar 2006 that was spent within 365 days of death. Thus, if person no. 2 in Diagram 1 died on the 100th day of 2007, then 265/365 of their 2006 enrollment and nonhospice payments were assigned to decedents and 100/365 to survivors. This method differs from that used in the earlier study, where dates of discharge were used to assign inpatient hospital and skilled nursing facility services to decedent and survivor categories. In the current study, payments for all services were prorated because dates of discharge are no longer available on the CMHS database. Payments assigned to decedents may therefore be understated because service use tends to increase as death approaches; prorating payments by days may result in too few payments being assigned to the last year of life. A comparison of overlapping years (1980, 1985, and 1988) between this analysis and the earlier study suggests that the change in methodology reduced the estimated payments going to the last year of life by less than two percentage points. For hospice services, all 2006 payments for 2007 decedents were assigned to decedents rather than being prorated between decedents and survivors, because it was assumed that all hospice services were provided close to death. The same methodology was used to assign person-months and payments to decedents and survivors for all years of the study.
Diagram 1.
Examples of Allocation of 2006 Medicare Payments between Decedents and Survivors
Notes: These examples use person-months to illustrate the allocation principle. Actual allocations were made at the level of person-days. X, month of death; D, months allocated to decedents; S, months allocated to survivors.
The percents of payments going to decedents and survivors in each year were adjusted to the age, sex, and survival status of the 1978 sample to account for changes in the Medicare population over time. Adjustment for a given year was made by applying average payment amounts for each cell to the age, sex, and survival distribution of the 1978 sample. Both unadjusted and adjusted estimates are presented. Per capita payments for a given year were computed by dividing total dollars assigned to decedents (or survivors) by the total number of person-years for decedents (or survivors) in that year.
Hospitalization and use of ICU and CCU services near death represent two measures of the intensity of terminal care (Earle et al. 2004; Wennberg et al. 2004;). For beneficiaries dying in March of selected years, we determined the percent who were hospitalized and the percent using ICU/CCU services (measured as ICU/CCU charges greater than U.S.$0) in the calendar year of death. March decedents were chosen for this analysis to capture hospitalization and ICU/CCU use in the last 2–3 months of life, given the limitations of the CMHS file structure. Rates of hospitalization may be understated because hospital stays are counted from inpatient hospital claims files and Medicare does not receive inpatient hospital claims for some hospitalizations undergone by hospice enrollees. Those hospitalizations are billed as hospice services, provided that the hospitalization is for care related to the terminal illness. Undercounting of hospitalizations would be greater in the later years of the study when hospice use was highest.
RESULTS
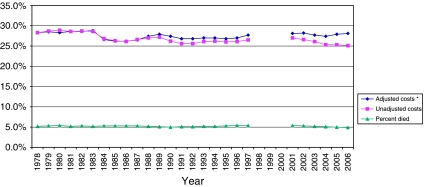
The crude death rate among elderly Medicare beneficiaries remained stable between 1978 and 2006 at about 5 percent (Figure 1). The percent of Medicare payments going to persons in their last year of life exhibited some variability, with an overall decrease during that time from 28.3 percent in 1978 to 25.1 percent in 2006 (p<.01 for linear trend). The largest 1-year change occurred between 1983 and 1984 (a decrease of 1.8 percentage points), when the Medicare prospective payment system for inpatient hospital care began. Following adjustment for age, sex, and death rates, the percent of payments going to the last year of life did not change significantly between 1978 and 2006. The adjusted trend reflects the fact that the average age of decedents rose from 78.7 in 1978 to 81.9 in 2006 (data not shown).
Figure 1.
Percent Dying and Percent of Medicare Payments Spent in the Last 12 Months of Life, among Medicare Beneficiaries Aged 65 and Older, 1978–2006
Notes: Figure excludes beneficiaries enrolled in managed care at any point during the year. Payment data were not available for years 1998–2000. *Adjusted to the age, sex, and survival status of the 1978 sample. For linear trends 1978–2006: p<.01 (unadjusted costs), p=.64 (adjusted costs), and p=.11 (death rates). Source: Medicare Continuous History Sample.
The percent of March decedents who were hospitalized in their last few months did not show a significant trend, remaining near 63 percent in most years (Table 1). The percent with multiple hospitalizations increased between 1978 and 2006, however, from 20.3 to 27.0 percent. The percent using ICU/CCU services increased both for decedents (from 26.1 percent in 1983 to 33.1 percent in 2006) and for survivors (from 4.0 to 6.3 percent). Survivors had much lower levels of hospitalization and there was no significant trend with respect to percent hospitalized or percent with multiple hospitalizations.
Table 1.
Measures of Inpatient Hospital Use among Medicare Beneficiaries Aged 65 and Older, by Survival Status, 1978–2006
| Year |
|||||||
|---|---|---|---|---|---|---|---|
| Utilization Measure and Survival Status | 1978 | 1983 | 1988 | 1993 | 1997 | 2002 | 2006 |
| Percent hospitalized | |||||||
| March decedents | 64.5 | 67.4 | 63.7 | 63.0 | 62.6 | 62.8 | 62.5 |
| Survivors | 18.5 | 20.1 | 16.1 | 16.0 | 16.5 | 17.0 | 16.7 |
| Percent undergoing multiple hospitalizations | |||||||
| March decedents | 20.3 | 23.0 | 22.2 | 22.0 | 24.5 | 25.6 | 27.0 |
| Survivors | 5.2 | 6.1 | 4.8 | 4.9 | 5.6 | 5.9 | 5.6 |
| Percent using ICU/CCU services | |||||||
| March decedents | N/A | 26.1 | 27.7 | 26.4 | 28.7 | 30.7 | 33.1 |
| Survivors | N/A | 4.0 | 4.6 | 5.1 | 5.6 | 6.1 | 6.3 |
Notes: p<.05 for positive linear trend in multiple hospitalizations for decedents and ICU use for both decedents and survivors.
Trends in multiple hospitalizations for survivors and percent hospitalized for decedents and survivors were not statistically significant.
Table excludes beneficiaries enrolled in managed care at any point during the year.
ICU/CCU data are not available in the Continuous Medicare History Sample file before 1983.
CCU, coronary care unit; ICU, intensive care unit; NA, not applicable
Source: Medicare Continuous History Sample file.
Throughout the study period, a higher proportion of spending for decedents was for inpatient hospital and skilled nursing facility care and less was for physician and outpatient care, compared to survivors (Table 2). The mix of services changed substantially over time for both decedents and survivors. Despite increases in multiple hospitalizations and ICU use, inpatient hospital services accounted for a declining percentage of payments, whereas outpatient, skilled nursing facility, and hospice care accounted for an increasing percentage. The decline in home health payments from 1997 to 2006 followed the tightening of Medicare payment rules for this service resulting from the Balanced Budget Act of 1997. Hospice services increased from 0.6 percent of payments for decedents in 1988 (it was not a covered service before 1983) to 9.7 percent of decedent payments in 2006. Thirty-one percent of sample persons dying in December 2006 incurred hospice payments that year (data not in tables).
Table 2.
Percent Distribution of Medicare Payments among Types of Service for Beneficiaries Aged 65 and Older, by Survival Status, for Selected Years, 1978–2006
| 1978 |
1988 |
1997 |
2006 |
|||||
|---|---|---|---|---|---|---|---|---|
| Decedents | Survivors | Decedents | Survivors | Decedents | Survivors | Decedents | Survivors | |
| Payments per person-year | U.S.$13,401 | U.S.$1,858 | U.S.$21,941 | U.S.$3,259 | U.S.$33,234 | U.S.$5,103 | U.S.$38,975 | U.S.$5,993 |
| Type of service (percent distribution) | ||||||||
| Total | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 |
| Inpatient hospital | 76.3 | 64.7 | 69.8 | 53.3 | 56.4 | 44.2 | 50.2 | 37.7 |
| Physician and other medical | 17.3 | 27.9 | 20.5 | 34.0 | 17.3 | 28.5 | 18.8 | 5.3 |
| Outpatient | 2.6 | 4.3 | 4.8 | 9.1 | 5.4 | 10.1 | 6.8 | 13.0 |
| Hospice | 0.0 | 0.0 | 0.6 | 0.0 | 3.4 | 0.2 | 9.7 | 1.0 |
| Skilled nursing facility | 1.9 | 1.2 | 1.8 | 1.2 | 9.4 | 6.3 | 10.4 | 7.4 |
| Home health | 1.8 | 1.9 | 2.6 | 2.4 | 8.2 | 10.7 | 4.1 | 5.6 |
Notes: p<.05 for differences between decedents and survivors in the mix of services for each year. Standard errors for the comparison were determined by the method of random groups.
Table excludes beneficiaries enrolled in managed care at any point during the year.
Dollars are inflation adjusted to 2006 using the Consumer Price Index (Series CPI-U-RS).
For hospice enrollees, hospital, physician, and other services related to the terminal illness (except services by an attending physician not employed by the hospice) are billed and paid as hospice services.
Source: Medicare Continuous History Sample file.
DISCUSSION
Medical care services in the last year of life continue to have a large impact on Medicare expenditures. The percent of Medicare dollars going to end-of-life care has declined slightly, but still accounts for a quarter of Medicare payments for the elderly. This is the case despite substantial changes in the types of services received by both decedents and survivors. Technological advances and other factors driving medical care use and costs have apparently increased the amount of care received by survivors and decedents in a similar manner. Although medical technology has changed remarkably during our 29-year study period, the basic payment approach of Medicare has not. It remains, especially for physicians, largely a fee-for-service system, with financial incentives to produce more services (Wilensky 2009).
Our findings suggest there have been increases in both aggressive care and nonaggressive care at the end of life among the elderly. Multiple hospitalizations increased in the last few months of life, as did the use of ICU/CCU services, suggesting a general increase in intensity of care. Other studies have also found an increase in the aggressiveness of care at the end of life (Barnato et al. 2004; Earle et al. 2004;). On the other hand, the substantial growth in hospice payments indicates that palliative and supportive care is becoming more common. Some patients receive both styles of care, undergoing aggressive treatment for some time, then enrolling in hospice a short time before death (Earle et al. 2004). The relationship between hospice utilization and other services is not clear; in some cases hospice may substitute for other types of care, and in others it may be used in addition to conventional care services.
Some important limitations apply to the findings presented here. First, this study does not address quality or appropriateness of care, but only provides a descriptive analysis of trends in Medicare-covered services in the last year of life. Second, care received in the last year is not synonymous with care rendered during terminal illness. The categorization of individuals into “decedents” and “survivors” is based on retrospective knowledge of vital status and many services are provided to seriously ill patients when the outcome of care is still in doubt (Bach, Schrag, and Begg 2004). Third, this analysis was restricted to acute care services covered by Medicare, not including prescription drugs. Importantly, most nursing home services were not included because they are not usually covered by Medicare. Nursing home use is high near the end of life and, unlike acute care services, nursing home costs increase with age at death (Spillman and Lubitz 2000; Hoover et al. 2002; Liu, Wiener, and Niefeld 2006;). Lastly, the analysis excluded managed care enrollees, who now make up over 20 percent of Medicare beneficiaries. There are no data available on costs of Medicare-covered services for decedents and survivors in managed care. To estimate the impact of excluding managed care enrollees, we repeated our analysis separately for states with high and low managed care penetration. There was no difference in percent of payments going to decedents in the two groups of states, or in trends in the two groups, suggesting that the exclusion of the managed care population did not strongly affect our findings.
Despite changes in the delivery of medical care over the last generation, the share of Medicare expenditures going to beneficiaries in their last year of life has not changed substantially. Factors that drive increases in health care costs have apparently affected the care of decedents and survivors in similar ways.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: The authors thank Charles Herboldsheimer for his valuable assistance in preparing data files for the analysis, and Joanne Lynn for her helpful comments on an earlier draft of the manuscript.
Findings from this study were presented at the annual meeting of AcademyHealth on June 28, 2009 in Chicago, IL. The statements contained in this article are those of the authors and do not necessarily reflect the views or policies of the Centers for Medicare and Medicaid Services or the National Center for Health Statistics.
Disclaimers: None.
Disclosures: None.
Supporting Information
Additional supporting information may be found in the online version of this article:
Appendix SA1: Author Matrix.
Please note: Wiley-Blackwell is not responsible for the content or functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
REFERENCES
- Bach PB, Schrag D, Begg CB. Resurrecting Treatment Histories of Dead Patients: A Study Design That Should Be Laid to Rest. Journal of the American Medical Association. 2004;292(22):2765–70. doi: 10.1001/jama.292.22.2765. [DOI] [PubMed] [Google Scholar]
- Barnato AE, McClellan MB, Kagay CR, Garber AM. Trends in Inpatient Treatment Intensity among Medicare Beneficiaries at the End-of-Life. Health Services Research. 2004;39(2):363–75. doi: 10.1111/j.1475-6773.2004.00232.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buntin MB, Huskamp H. What Is Known about the Economics of End-of-Life Care for Medicare Beneficiaries? Gerontologist. 2002;42(Special issue III):40–8. doi: 10.1093/geront/42.suppl_3.40. [DOI] [PubMed] [Google Scholar]
- Bureau of Labor Statistics. Updated CPI-U-RS, All Items and All Items Less Food and Energy, 1978–2007. 2008. [accessed on August 12, 2008]. Available at http://stats.bls.gov/cpi/cpiurs1978_2007.pdf.
- Calfo S, Smith J, Zezza M. Last Year of Life Study. 2008. [accessed on August 11, 2008]. Available at http://www.cms.hhs.gov/ActuarialStudies/downloads/Last_Year_of_Life.pdf.
- Chernew ME, Goldman DP, Pan F, Shang B. Disability and Health Care Spending among Medicare Beneficiaries. Health Affairs. 2005:W5-R42–W5-R52. doi: 10.1377/hlthaff.w5.r42. Published online on September 26, 2005 10.1377/hlthaffW5.R42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earle CC, Neville BA, Landrum MB, Ayanian JZ, Block SD, Weeks JC. Trends in the Aggressiveness of Cancer Care near the End-of-Life. Journal of Clinical Oncology. 2004;22(2):315–21. doi: 10.1200/JCO.2004.08.136. [DOI] [PubMed] [Google Scholar]
- Emanuel EJ, Emanuel LL. The Economics of Dying: The Illusion of Cost Savings at the End-of-Life. New England Journal of Medicine. 1994;330(8):540–4. doi: 10.1056/NEJM199402243300806. [DOI] [PubMed] [Google Scholar]
- Federal Interagency Forum on Aging-Related Statistics. Older Americans 2008: Key Indicators of Well-Being. Federal Interagency Forum on Aging-Related Statistics. Washington, DC: US Government Printing Office; 2008. [Google Scholar]
- Felder S, Meier M, Schmitt H. Health Care Expenditures in the Last Months of Life. Journal of Health Economics. 2000;19:679–95. doi: 10.1016/s0167-6296(00)00039-4. [DOI] [PubMed] [Google Scholar]
- Garber AM, MaCurdy T, McClellan M. Diagnosis and Medicare Expenditures at the End-of-Life. In: Wise DA, editor. Frontiers in the Economics of Aging. Chicago: University of Chicago Press; 1998. pp. 247–74. [Google Scholar]
- Garber AM, MaCurdy T. Medical Care at the End-of-Life: Diseases, Treatment Patterns, and Costs. In: Garber AM, editor. Frontiers in Health Policy Research. Vol. 2. Cambridge, MA: MIT Press; 1999. pp. 77–98. [Google Scholar]
- Hanratty B, Burstrom B, Walander A, Whitehead M. Inequality in the Face of Death? Public Expenditures on Health Care for Different Socioeconomic Groups in the Last Year of Life. Journal of Health Services Research and Policy. 2007;12(2):90–4. doi: 10.1258/135581907780279585. [DOI] [PubMed] [Google Scholar]
- Hogan C, Lunney J, Gabel J, Lynn J. Medicare Beneficiaries' Costs of Care in the Last Year of Life. Health Affairs. 2001;20(4):188–95. doi: 10.1377/hlthaff.20.4.188. [DOI] [PubMed] [Google Scholar]
- Hoover DR, Crystal S, Kumar R, Sambamoorthi U, Cantor JC. Medical Expenditures in the Last Year of Life: Findings from the 1992–1996 Medicare Current Beneficiary Survey. Health Services Research. 2002;37(6):1625–42. doi: 10.1111/1475-6773.01113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kronman AC, Ash AS, Freund KM, Hanchate A, Emanuel EJ. Can Primary Care Visits Reduce Hospital Utilization among Medicare Beneficiaries at the End-of-Life? Journal of General Internal Medicine. 2008;23(9):1330–5. doi: 10.1007/s11606-008-0638-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levinsky NG, Yu W, Ash A, Moskowitz M, Gazelle G, Saynina O, Emanuel EJ. Influence of Age on Medicare Expenditures and Medical Care in the Last Year of Life. Journal of the American Medical Association. 2001;286(11):1349–55. doi: 10.1001/jama.286.11.1349. [DOI] [PubMed] [Google Scholar]
- Liu K, Wiener JM, Niefeld MR. End-of-Life Medicare and Medicaid Expenditures for Dually Eligible Beneficiaries. Health Care Financing Review. 2006;27(4):95–110. [PMC free article] [PubMed] [Google Scholar]
- Lubitz J, Prihoda R. The Use and Costs of Medicare Services in the Last 2 Years of Life. Health Care Financing Review. 1984;5(3):117–31. [PMC free article] [PubMed] [Google Scholar]
- Lubitz JD, Riley GF. Trends in Medicare Payments in the Last Year of Life. New England Journal of Medicine. 1993;328(15):1092–6. doi: 10.1056/NEJM199304153281506. [DOI] [PubMed] [Google Scholar]
- Lynn J, Schall MW, Milne C, Nolan KM, Kabcenell A. Quality Improvements in End-of-Life Care: Insights from Two Collaboratives. Joint Commission Journal on Quality Improvement. 2000;26(5):254–67. doi: 10.1016/s1070-3241(00)26020-3. [DOI] [PubMed] [Google Scholar]
- Medicare Payment Advisory Commission. 1999. Improving Care at the End-of-Life. Report to the Congress: Selected Medicare issues. Washington, DC, pp. 117–32.
- Medicare Payment Advisory Commission. 2008. Report to the Congress: Reforming the Delivery System. Washington, DC, pp. 203–40.
- Riley G, Lubitz J, Prihoda R, Rabey E. The Use and Costs of Medicare Services by Cause of Death. Inquiry. 1987;24:233–44. [PubMed] [Google Scholar]
- Scitovsky AA. ‘The High Cost of Dying’ Revisited. Milbank Quarterly. 1994;72(4):561–91. [PubMed] [Google Scholar]
- Shipman C, Gysels M, White P, Worth A, Murray SA, Barclay S, Forrest S, Shepherd J, Dale J, Dewar S, Peters M, White S, Richardson A, Lorenz K, Koffman J, Higginson IJ. Improving Generalist End of Life Care: National Consultation with Practitioners, Commissioners, Academics, and Service User Groups. British Medical Journal. 2008;337:a1720. doi: 10.1136/bmj.a1720. doi 10.1136/bmj.a1720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spillman BC, Lubitz J. The Effect of Longevity on Spending for Acute and Long-Term Care. New England Journal of Medicine. 2000;342(19):1409–15. doi: 10.1056/NEJM200005113421906. [DOI] [PubMed] [Google Scholar]
- Stooker T, van Acht JW, van Barneveld EM, van Vliet RC, van Hout BA, Hessing DJ, Busschbach JJ. Costs in the Last Year of Life in the Netherlands. Inquiry. 2001;38(1):73–80. doi: 10.5034/inquiryjrnl_38.1.73. [DOI] [PubMed] [Google Scholar]
- The SUPPORT Principal Investigators. A Controlled Trial to Improve Care for Seriously Ill Hospitalized Patients. Journal of the American Medical Association. 1995;274(20):1591–8. [PubMed] [Google Scholar]
- Teno JM, Clarridge BR, Casey V, Welch LC, Wetle T, Shield R, Mor V. Family Perspectives on End-of-Life Care at the Last Place of Care. Journal of the American Medical Association. 2004;291(1):88–93. doi: 10.1001/jama.291.1.88. [DOI] [PubMed] [Google Scholar]
- Thorpe KE, Howard DH. The Rise in Spending among Medicare Beneficiaries: The Role of Chronic Disease Prevalence and Changes in Treatment Intensity. Health Affairs. 2006:w378–w388. doi: 10.1377/hlthaff.25.w378. Published online on August 22, 2006 10.1377/hlthaff.25.w378. [DOI] [PubMed] [Google Scholar]
- Wennberg JE, Fisher ES, Stukel TA, Skinner JS, Sharp SM, Bronner KK. Use of Hospitals, Physician Visits, and Hospice Care during Last Six Months of Life among Cohorts Loyal to Highly Respected Hospitals in the United States. British Medical Journal. 2004;328:607–10. doi: 10.1136/bmj.328.7440.607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilensky GR. Reforming Medicare's Physician Payment System. New England Journal of Medicine. 2009;360(7):653–5. doi: 10.1056/NEJMp0808003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.