Abstract
Objectives
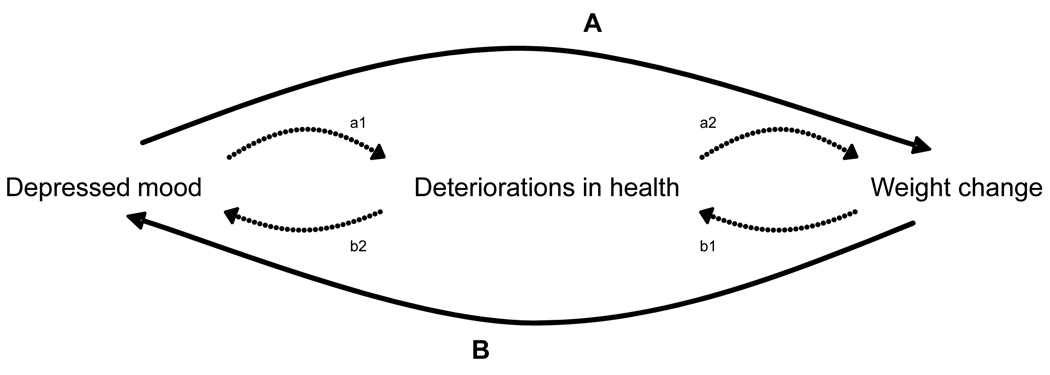
Weight change may be considered an effect of depression. In turn, depression may follow weight change. Deteriorations in health may mediate these associations. The objective was to examine reciprocal associations between depressed mood and weight change, and the potentially mediating role of deteriorations in health (interim hospitalizations and incident mobility imitation) in these associations.
Design
Prospective observational cohort study
Settings
Memphis, Tennessee and Pittsburgh, Pennsylvania
Participants
2406 black and white men and women, aged 70–79 participating in the Health, Aging and Body composition (Health ABC) study.
Measurements
Depressed mood at baseline (T1) and 3-year follow-up (T4) was measured with the CES-D scale. Three weight change groups (T1–T4) were created: loss (≥5% loss), stable (within ±5% loss or gain), and weight gain (≥5% gain).
Results
At T1 and T4, respectively 4.4% and 9.5% of the analysis sample had depressed mood. T1 depressed mood was associated with weight gain over the 3-year period (OR:1.91; 95%CI:1.13–3.22). Weight loss over the 3-year period was associated with T4 depressed mood (OR:1.51; 95%CI:1.05–2.16). Accounting for deteriorations in health in the reciprocal associations between weight change and depressed mood reduced effect sizes between 16–27%.
Conclusions
In this study, depressed mood predicted weight gain over three years, while weight loss over three years predicted depressed mood. These associations were partly mediated through deteriorations in health. Implications for clinical practice and prevention include increased awareness that depressed mood can cause weight change, but can also be preceded by deteriorations in health and weight change.
Keywords: depression, weight change, aging
OBJECTIVE
Late-life depression has been associated with both weight loss and weight gain (1–5). Depressive symptoms may affect weight change directly or indirectly through for example changes in appetite (6) or level of physical activity (7). Conversely, weight change may also lead to depressive symptoms. Alterations in body weight are associated with an array of unfavorable health outcomes, dependent upon initial body composition, intention, and extent of weight change. For example, weight gain is associated with an increased risk of coronary heart disease, type 2 diabetes, and the metabolic syndrome (8–10). Weight loss is associated with sarcopenia, cachexia, frailty, and mortality (11–13). These weight change-related deteriorations in health may gradually lead to eliciting or aggravating depressive symptoms (14–16).
Longitudinal studies that examined reciprocal relations between depression and weight change are very limited. A study among 53–63 year old adults showed that baseline depression was related to subsequent weight loss in both men and women and weight gain in women (5). Weight loss predicted increases in depressive symptoms only in men (5). More research is also needed to elucidate the mechanisms that underlie the relationships between depression and weight change. The link between depression and weight changes might be due to deteriorations in health.
Our study aims to examine reciprocal associations between depressed mood and weight change, and to assess the mediating role of deteriorations in health in these reciprocal associations as illustrated in Figure 1. First, we examined the association between depressed mood at baseline (T1) and 3-year (T1–T4) weight change (arrow ‘A’ in Figure 1), and to assess the potentially mediating role of deteriorations in health – represented by interim hospitalization and incident mobility limitation between T1 and T4 – on this association (arrows ‘a1’ and ‘a2’ in Figure 1). Second, we examined whether weight changes over a 3-year period predicted T4 depressed mood (arrow ‘B’ in Figure 1), and to assess the potentially mediating role of deteriorations in health on this association (arrows ‘b1’ and ‘b2’ in Figure 1).
Figure 1.
Putative reciprocal associations between depressed mood and 3-year weight change.
METHODS
Study population
The Health, Aging and Body Composition (Health ABC) Study is an ongoing longitudinal cohort study designed to investigate the impact of body composition changes and weight-related health conditions on functional decline in older adults. The Health ABC Study enrolled 3075 well-functioning, 70- to 79-year old, black and white men and women. Participants were identified from a random sample of white Medicare beneficiaries and all age-eligible community-dwelling black residents in designated zip code areas surrounding Memphis, Tennessee, and Pittsburgh, Pennsylvania. Participants were eligible if they reported no difficulty in either walking one quarter of a mile, going up 10 steps without resting, or performing basic activities of daily living. Participants were excluded if they reported a history of active treatment for cancer in the prior three years, planned to move out of the study area in the next three years, or were currently participating in a randomized trial of a lifestyle intervention. Baseline data, collected between April 1997 and June 1998, included an in-person interview and a clinic-based examination, with evaluation of body composition, clinical and sub-clinical diseases, and physical functioning. From April 1997 onward, clinic visits were alternated with telephone interviews at 6-month intervals. Two-thousand-four hundred-thirty-nine people had full data on T1 (baseline) and T4 weight and depressed mood. Data on deteriorations in health and covariates were missing for 33 participants, leaving 2406 participants for the present analyses. All participants signed informed written consent forms approved by the institutional review boards of the clinical sites.
Measures
Depressed mood
Depressed mood was measured at T1 and T4 with the Center for Epidemiologic Studies Depression (CES-D) scale, a 20-item, self-report scale designed to measure depressive symptoms experienced during the previous week (17). The scale, with scores ranging from 0 to 60, has been shown to be a valid and reliable instrument in older populations with good psychometric properties (18, 19). To screen for participants with clinically relevant levels of depressive symptoms (no/yes), the commonly used CES-D cut-off score of ≥ 16 was applied, hereafter called depressed mood (14, 20).
Weight change
Body weight was measured to the nearest 0.1 kg with a standard balance beam scale. In conformity of literature that suggests that weight changes of ≥5% are potentially clinically relevant (21, 22). Body weight change over 3 years (T1–T4) was calculated and classified into 3 weight change groups: loss (≥5% of loss), stable (within ±5% loss or gain), and weight gain (≥5% of gain).
Deteriorations in health
Reported number of interim hospitalizations ≥ 24 hours and/or interim outpatient revascularization procedures (cardiac catheterization and percutaneous transluminal coronary angioplasty) occurring between T1 and T4, were considered a primary measure of deterioration in health. Incident mobility limitation (no/yes) was considered a second measure of deterioration in health. Incident implies newly reported difficulty walking one-quarter mile or climbing 10 steps at two consecutive semi-annual follow-up measurements between T1 and T4.
Covariates
Covariates –all measured at T1– included age, gender, race (white/black), marital status (married/was married/never married), study site (Memphis/Pittsburgh), body mass index (BMI) in kg/m2, intentionality of weight change during any of the three years of follow-up (no/yes), number of self-reported diseases (presence (no/yes) of arthritis, osteoporosis, acute myocardial infarction, angina pectoris, congestive heart failure, peripheral artery disease, transient ischaemic attack, cerebrovascular accident, hypertension, rheumatic heart disease, chronic obstructive pulmonary disease, cancer, diabetes, kidney disease, Parkinson’s disease, thyroid disease, gout, and other conditions for which participants saw a doctor), anti-depressant use (no/yes), smoking status (never/former/current), and alcohol use (current/former/never).
Statistical analyses
Chi square test for categorical variables and t-tests for continuous variables were used to examine differences in baseline characteristics between participants who were included in our analysis and those who were not. To examine patterns of interim hospitalizations and incident mobility limitation across categories of T1 depressed mood and 3-year weight change chi-square tests were used (arrow ‘a1’ and ‘a2’ in Figure 1). Chi-square tests were also used to we examine patterns of T4 depressed mood and 3-year weight change across categories of interim hospitalizations and incident mobility limitation (arrow ‘b1’ and ‘b2’ in Figure 1).
Using multinomial logistic regression models, we determined the effect of T1 on 3-year weight change (arrow ‘A’ in Figure 1). Two models were fitted: model 1 adjusted for age, gender, race, site, marital status, smoking, alcohol use, body mass index, trying to change weight, number of chronic diseases, and anti-depressants use; model 2 additionally adjusted for interim hospitalizations and incident mobility limitation. Then we determined the effect of 3-year weight change on T4 depressed mood using logistic regression analyses (arrow B in figure 1). Model 1 adjusted for age, gender, race, site, marital status, baseline depressed mood, smoking, alcohol use, body mass index, trying to change weight, number of chronic diseases, and anti-depressants use and model 2 additionally adjusted for interim hospitalizations and incident mobility limitation. A percentage reduction in the odds ratio (OR) from model 1 was computed: (OR model 1 -OR model x)/(OR model 1 −1)*100%. When the decrease of the original effect exceeds 10%, the newly added variables can be regarded as mediating variables, provided that the predictor and outcome variable are associated significantly and the newly added variables are associated with both the predictor and outcome variable (23). All analyses are shown for men and women together because no significant interactions with gender were observed. Analyses were performed using SPSS, version 15.0 (SPSS Inc., Chicago, IL).
RESULTS
Compared to respondents who were included in our analysis sample (n=2406), those who were not (n=669) were significantly older (t=2.98, df=3073, p<0.01), less likely to be white (chi-square=48.20, df=1, p<0.01), less likely to be married (chi-square= 9.84, df=2, p<0.01), less likely to try to change their weight (chi-square=25.47, df=1, p<0.01), more likely to have ever smoked (chi-square=30.90, df=2, p<0.01), and had significantly higher CES-D scores (t=3.88, df=3047, p<0.01) (Table 1). Table 1 also shows that 4.4% of the persons in the analysis sample had depressed mood at T1 and 9.5% had depressed mood at T4. Also, 70.7% of the persons in the analysis sample remained weight stable over the 3-year period, while 18.1% lost weight and 11.2% gained weight over the 3-year period. Finally, 34.8% of the persons in the analysis sample reported interim hospitalization and 28.3% reported incident mobility limitation.
Table 1.
Main characteristics of the study population
| Characteristic | Attrition or loss to follow-up n=669 |
Included in the analysis sample n=2406 |
|---|---|---|
| Age, mean (SD) | 74.5 (2.9) | 74.1 (2.9) a |
| Gender,% female | 49.0 | 52.2 |
| Race,% white | 46.6 | 61.6 b |
| Study site,% Pittsburgh | 47.7 | 50.2 |
| Marital status,% married | 52.0 | 58.4 c |
| Smoking status,% never | 39.8 | 45.1 c |
| Alcohol use,% current | 47.0 | 50.4 |
| Body mass index, mean (SD) | 27.4 (5.1) | 27.4 (4.7) |
| Trying to change weight,% yes | 23.8 | 34.0 b |
| Number of chronic diseases,% [mt]2 |
45.0 | 42.0 |
| Antidepressant use,% yes | 2.7 | 2.4 |
| Depressed mood | ||
| T1 CES-D score, mean (SD) |
5.5 (5.5) | 4.5 (5.2) d |
| % T1 depressed mood | 5.9 | 4.4 |
| T4 CES-D score, mean (SD) |
6.5(6.4) | |
| % T4 depressed mood | 9.5 | |
| % T1 and T4 depressed mood |
2.3 | |
| Weight change over 3-year period,% |
||
| Stable | 70.7 | |
| Loss | 18.1 | |
| Gain | 11.2 | |
|
Number of interim hospitalizations,% |
||
| None | 65.2 | |
| 1–2 | 29.2 | |
| ≥3 | 5.6 | |
| Incident mobility limitation,% yes | 28.3 |
T-test significant, (df=3073, p<0.01);
Pearson chi-square significant (df=1);
Pearson chi-square significant (df=1)
T-test significant, (df=3047, p<0.01).
Table 2a shows that people with depressed mood at T1 were more likely to develop mobility limitations (chi-square=25.60, df=1, p<0.01). People who were weight stable were least likely to have hospitalizations (chi-square=27.33, df=4, p<0.01) and mobility limitations (chi-square=28.98, df=2, p<0.01). The weight loss and gain group did not significantly differ from each other regarding the number of hospitalization and mobility limitation. People with hospitalizations were less likely to be weight stable over 3 years (chi-square=27.23, df=4, p<0.01) and more likely to have depressed mood at T4 (chi-square=11.26, df=2, p<0.01) (Table 2b). All three hospitalization categories differed significantly from each other regarding the distribution over the weight change groups. People with one or two hospitalizations did not differ significantly from those without or 3 or more hospitalizations regarding the prevalence of depressed mood at T4. Further, people with mobility limitations were less likely to be weight stable (chi-square=28.98, df=2, p<0.01) and more likely to have depressed mood at T4 (chi-square=62.02, df=1, p<0.01).
Table 2.
| 2a Number of interim hospitalizations and incident mobility limitation across T1depression and 3-year weight change categories. | |||||||
|---|---|---|---|---|---|---|---|
| Number of interim hospitalizations, % | Incident mobility limitation, % | ||||||
| none | 1–2 | ≥3 | p-value | No | Yes | p-value | |
| T1 depressed mood | |||||||
| No depressed mood (n=2300) |
65.4 | 29.2 | 5.4 | 0.37 | 72.7 | 27.3 | <0.01 a |
| Depressed mood (n=106) |
61.3 | 30.2 | 8.5 | 50.0 | 50.0 | ||
| Weight change over 3- year period |
|||||||
| Stable (n=1701) | 58.2 | 32.4 | 9.4 | <0.01 b | 74.8 | 25.2 | <0.01 c |
| Loss (n=435) | 67.9 | 27.6 | 4.5 | 63.9 | 36.1 | ||
| Gain (n=270) | 59.6 | 34.1 | 6.3 | 64.1 | 35.9 | ||
| Table 2b Categories of 3-year weight change and depression at T4 across number of interim hospitalizations and incident mobility limitation. | |||||||
|---|---|---|---|---|---|---|---|
| Weight change over 3-year period,% | T4 depressed mood,% | ||||||
| Stable | Loss | Gain | p-value | No | Yes | p-value | |
| Number of interim hospitalizations |
|||||||
| None (n=1569) |
73.6 | 16.1 | 10.3 | <0.01 a | 91.7 | 8.3 | <0.01 b |
| 1–2 (n=703) | 66.9 | 20.1 | 13.1 | 89.2 | 10.8 | ||
| ≥3(n=134) | 56.7 | 30.6 | 12.7 | 83.6 | 16.4 | ||
| Incident mobility limitation |
|||||||
| No (n=1724) |
73.8 | 16.1 | 10.0 | <0.01 b | 93.4 | 6.6 | <0.01 c |
| Yes (n=682) | 62.8 | 23.0 | 14.2 | 83.0 | 17.0 | ||
Pearson chi-square significant (df=1)
Pearson chi-square significant (df=4)
Pearson chi-square significant (df=2)
Pearson chi-square significant (df=4)
Pearson chi-square significant (df=2)
Pearson chi-square significant (df=1)
The results of the multinomial logistic regression analyses demonstrating the effect of T1 depressed mood on 3-year weight change are presented in table 3. Persons with T1 depressed mood had an increased risk of 1.91 (Wald=5.78, df=1, p=0.02, 95% confidence interval (CI):1.13–3.22) to have a weight gain of ≥5% over the 3-year period, compared to those with T1 depressed mood with no weight change (Model 1), adjusted for baseline weight and other covariates. Compared to the relative risk from Model 1, the OR in Model 2 decreased 16% to 1.76 (Wald=4.31, df=1, p=0.04, 95%CI:1.03–3.00) when both interim hospitalization and incident mobility limitation between T1 and T4 were entered in the logistic regression analyses.
Table 3.
Effect of T1 depressed mood on 3-year weight change a
| Weight change over 3-year period | ||||||
|---|---|---|---|---|---|---|
| Loss | Gain | |||||
|
Wald statistic df=1 |
p | OR(95%CI) |
Wald statistic df=1 |
p | OR(95%CI) | |
| Model 1 b | ||||||
| No depressed mood |
Ref | Ref | ||||
| Depressed mood | 0.07 | 0.78 | 1.08(0.63– 1.83) |
5.78 | 0.02 | 1.91(1.13–3.22) |
| Model 2 c | ||||||
| No depressed mood |
Ref | Ref | ||||
| Depressed mood | 0.002 | 0.97 | 0.99(0.58– 1.70) |
4.31 | 0.04 | 1.76(1.03–3.00) |
| Percentage reduction d | -- | 16 | ||||
Multinomial logistic regression analysis. Values indicate odds ratios (OR) with 95% confidence intervals (CI) and p-values by Wald statistics with df=1.
Model 1 adjusted for age, gender, race, site, marital status, smoking, alcohol use, body mass index, trying to change weight, number of chronic diseases, and anti-depressants use.
Model 2: adjusted for all variables of model 1+hospitalizations and incident mobility limitation.
Percentage reduction in odds ratio from model 1 computed by (ORmodel1−ORmodel2)/ORmodel1−1)*100%.
Table 4 presents results from multivariate logistic regression analyses demonstrating the effect of 3-year weight change on T4 depressed mood. Persons who showed a weight loss of ≥5% over the 3-year period had a significantly increased risk of depressed mood at T4 (Wald=4.95, df=1, p=0.03, OR:1.51; 95%CI:1.05–2.16) compared to those with no weight change over the 3-year period (Model 1), adjusted for T1 BMI, T1 depressed mood, and other covariates. Compared to the relative risk from Model 1, the OR decreased 27% to 1.37 (Wald=2.89, df=1, p=0.09, 95%CI:0.95–1.98) when both interim hospitalization and incident mobility limitation between T1 and T4 were additionally entered in the logistic regression analyses (Model 2). When we excluded participant with depressed mood at T1, results remained very similar (data not shown)
Table 4.
Effect of 3-year weight change on T4 depressed mood a
| T4 depressed mood | |||||||
|---|---|---|---|---|---|---|---|
| Model 1 b | Model 2 c | Percentage | |||||
|
Wald statistic df=1 |
p | OR(95%CI) |
Wald statistic df=1 |
p | OR(95%CI) | Reduction d | |
| Weight change over 3-year period |
|||||||
| Stable | Ref | Ref | |||||
| Loss | 4.95 | 0.03 | 1.51(1.05–2.16) | 2.89 | 0.09 | 1.37(0.95–1.98) | 27 |
| Gain | 3.01 | 0.08 | 1.46(0.95–2.25) | 1.83 | 0.18 | 1.35(0.87–2.09) | -- |
Logistic regression analysis. Values indicate odds ratios (OR) with 95% confidence intervals (CI) and p-values by Wald statistics with df=1.
Model 1 adjusted for age, gender, race, site, marital status, baseline depressed mood, smoking, alcohol use, body mass index, trying to change weight, number of chronic diseases, and anti-depressants use.
Model 2: adjusted for all variables of model 1+hospitalizations and incident mobility limitation.
Percentage reduction in odds ratio from model 1 computed by (ORmodel1−ORmodel2)/ORmodel1−1)*100%.
In additional analysis, we examined the large group of weight stable people and defined ‘true’ weight stable people as people who did not gain or lose more than 5% of their baseline weight at every follow-up measurement (including T2, T3, and T4). Eighty-three percent of the weight stable group was truly weight stable. Those who gained or lost more than 5% of their weight but were considered weight stable based on their T4 weight were not at higher risk of depressed mood than the truly weight stable people (data not shown).
Depressive symptoms were measured with the full 20-item CES-D scale. A number of these items capture somatic symptoms which could be associated with body weight or change therein. Therefore, we performed a sensitivity analysis where we excluded the somatic items in calculation the CES-D score. The reciprocal associations between depressed mood and weight change remained very similar with this new CES-D score (data not shown).
DISCUSSION
Our study objective was to examine reciprocal associations between depressed mood and weight change over time using the conceptual model in Figure 1. On the basis of results from our analyses, we can conclude that baseline depressed mood predicted 3-year weight gain. However, 3-year weight loss predicted depressed mood at T4. Both of these associations were partly mediated through interim hospitalizations or revascularization procedures and incident mobility limitation. Accounting for these measures representing deteriorations in health in the regression models reduced original effect sizes between 16–27%.
Similar to our study, Haukkala, Uutela, and Salomaa (2) found that higher baseline scores on the Beck Depression Inventory predicted weight gain during a 3-year follow-up in a cardiovascular risk factor survey among 285 men and women aged 45 to 64 years at baseline. Their definition, though, of weight gain over the 3-year period was a gain of more than two BMI units. Thus –and under constancy of body height–, participants in lower BMI ranges achieved weight gain relatively less easy than participants in higher BMI ranges, whereas participants in our study were all at the same opportunity to achieve weight gain or loss. Contrary to our results, Haukkala, Uutela, and Salomaa also reported significant associations between higher depression scores and weight loss. A recent study that examined the reciprocal relations between depressed symptoms and changes in weight shows that baseline depression was related to subsequent weight loss in both men and women and weight gain in women (5). In the latter study, weight loss predicted increases in depressive symptoms only in men.
Our finding of weight loss prompting to depressed mood, partly through deteriorations in health, is consistent with several other studies (3, 24). Chapman and Nelson described that (involuntary) weight loss could lead to decreased immunocompetence and muscle wasting (24). In turn, decreased immunocompetence and muscle wasting were found to predispose to hospitalizations and incident mobility problems, respectively (25–27), but also to depressed mood (16, 28, 29), putatively through inflammatory and hormonal responses (19, 28, 29). Other studies demonstrated the association between mobility problems and hospitalizations, and between mobility problems and depressed mood (20, 30–32). The constellation of weight loss, hospitalization, mobility change, and depressed mood could also signal a process of failure to thrive, which is a syndrome in late life manifested by weight loss ≥5%, decreased appetite, poor nutrition, and inactivity, often accompanied by dehydration, impaired immune function, and low cholesterol levels (33). Also, Robertson and Montagnini described that depressive symptoms can be a cause and a consequence of failure to thrive (34).
In this study we focused on deteriorations in health that may mediate the reciprocal association between depressed mood and weight change. There are, however, other factors that may mediate these relations, for example stress. The association between stress and stressful life events and depressive symptoms has been well-established (35). Stress has also been related to under- and overeating and subsequent weight changes (36).
Our findings of depressed mood being more likely to result in weight gain as compared to nondepressed mood, and weight loss being more likely to result in depressed mood as compared to weight stability may seem contradictory. It is possible that participants who were detected with depressed mood at baseline were referred to their local health care provider. The resultant treatment might have led to weight gain in these individuals. However, participants with feelings of depression that went undetected at baseline might have wound up in a reciprocal process in which weight loss and feelings of depression reinforce each other. These individuals were being detected with depressed mood at T4.
We did not adjust for physical activity in any of our analyses. Since alterations in physical activity can be considered characteristic of depressed mood (6), and since physical activity facilitates weight loss and weight maintenance (37), adjustment for physical activity in the analyses would have constituted statistical overcorrection and, theoretically, attenuation of true effects of depressed mood on weight change and vice versa.
Some limitations of the study need to be considered. First, participants in our study represent the higher functioning segment of the older population since they were all without mobility limitation at study baseline. This is also seen in the low prevalence of depressed mood at baseline in our study population. The extrapolation of these findings to younger individuals or frailer older adults may therefore not be appropriate. Moreover, we only included participants with valid data at baseline and follow-up in our analyses. People in our analysis sample, for example, had a significantly lower CES-D score at baseline than people that were not included in our analyses. Selection bias effect may have caused an attenuation of true effects of depressed mood on weight change and vice versa. Another limitation is that deteriorations in health were conceptualized as a mediating factor in our study, while the concept was defined as a relatively distal determinant of health. Second, the deterioration in health, theoretically, could have long started off subclinically, while clinically –in terms of our definition of deterioration in health– no deterioration is noticeable. This would argue for future research using a design in which deterioration in health can be conceptualized as a shared determinant of depression and weight change, and in which deterioration in health can be assessed using more proximal parameters of health as well, such as bloodserum levels. Third, in our analyses we examined depressed mood at T1 and T4 and we do no know the exact moment someone got depressed mood. Further studies should investigate the effect of weight change on time to depressed mood.
The cardinal finding is that the pathogenetic pathway as we hypothesized it (Figure 1) was validated in this relatively healthy, older study population; depressed mood was more likely to result in weight gain as compared to nondepressed mood, while weight loss was more likely to result in depressed mood as compared to weight stability. Both associations were partly mediated through deteriorations in health. Implications for clinical practice and prevention include increased awareness that depressed mood can result in weight changes, but can also be preceded by deteriorations in health and weight change. Also, the pathogenetic pathway may be elaborated upon in future research. For now, opportunities should be sought for intervention upon the reciprocal process of depression and weight change in community-dwelling older populations.
Acknowledgment
Funding: This study was supported by National Institute on Aging contracts N01-AG-6-2101, N01-AG-6-2103, and N01-AG-6-2106. This research was supported (in part) by the Intramural Research Program of the NIH, National Institute on Aging.
Footnotes
Conflict of interest: No disclosures to report
Finanancial disclosures: none
REFERENCES
- 1.French SA, Jeffery RW, Folsom AR, et al. History of intentional and unintentional weight loss in a population-based sample of women aged 55 to 69 years. Obesity research. 1995;3:163–170. doi: 10.1002/j.1550-8528.1995.tb00132.x. [DOI] [PubMed] [Google Scholar]
- 2.Haukkala A, Uutela A, Salomaa V. Depressive symptoms, cynical hostility and weight change: A 3-year follow-up among middle aged men and women. Int J Beh Med. 2001;8:116–133. [Google Scholar]
- 3.Huffman G. Evaluating and treating unintentional weight loss in the elderly. Am Fam Physician. 2002;65:640–650. [PubMed] [Google Scholar]
- 4.Thompson MP, Morris LK. Unexplained weight loss in the ambulatory elderly. Journal of the American Geriatrics Society. 1991;39:497–500. doi: 10.1111/j.1532-5415.1991.tb02496.x. [DOI] [PubMed] [Google Scholar]
- 5.Forman-Hoffman VL, Yankey JW, Hillis SL, et al. Weight and depressive symptoms in older adults: direction of influence? J Gerontol B Psychol Sci Soc Sci. 2007;62:S43–S51. doi: 10.1093/geronb/62.1.s43. [DOI] [PubMed] [Google Scholar]
- 6.Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR®) Washington, DC: American Psychiatric Association; 2003. [Google Scholar]
- 7.Van Gool CH, Kempen GI, Penninx BW, et al. Relationship between changes in depressive symptoms and unhealthy lifestyles in late middle aged and older persons: results from the Longitudinal Aging Study Amsterdam. Age and ageing. 2003;32:81–87. doi: 10.1093/ageing/32.1.81. [DOI] [PubMed] [Google Scholar]
- 8.Field AE, Manson JE, Laird N, et al. Weight cycling and the risk of developing type 2 diabetes among adult women in the United States. Obesity research. 2004;12:267–274. doi: 10.1038/oby.2004.34. [DOI] [PubMed] [Google Scholar]
- 9.Harris TB. Invited commentary: body composition in studies of aging: new opportunities to better understand health risks associated with weight. American journal of epidemiology. 2002;156:122–124. doi: 10.1093/aje/kwf024. discussion 125-126. [DOI] [PubMed] [Google Scholar]
- 10.Harris TB, Launer LJ, Madans J, et al. Cohort study of effect of being overweight and change in weight on risk of coronary heart disease in old age. BMJ (Clinical research ed. 1997;314:1791–1794. doi: 10.1136/bmj.314.7097.1791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bales CW, Ritchie CS. Sarcopenia, weight loss, and nutritional frailty in the elderly. Annual review of nutrition. 2002;22:309–323. doi: 10.1146/annurev.nutr.22.010402.102715. [DOI] [PubMed] [Google Scholar]
- 12.Bortz WM., 2nd A conceptual framework of frailty: a review. The journals of gerontology. 2002;57:M283–M288. doi: 10.1093/gerona/57.5.m283. [DOI] [PubMed] [Google Scholar]
- 13.Kotler DP. Cachexia. Annals of internal medicine. 2000;133:622–634. doi: 10.7326/0003-4819-133-8-200010170-00015. [DOI] [PubMed] [Google Scholar]
- 14.Beekman AT, Penninx BW, Deeg DJ, et al. Depression and physical health in later life: results from the Longitudinal Aging Study Amsterdam (LASA) Journal of affective disorders. 1997;46:219–231. doi: 10.1016/s0165-0327(97)00145-6. [DOI] [PubMed] [Google Scholar]
- 15.Bisschop MI, Kriegsman DM, Deeg DJ, et al. The longitudinal relation between chronic diseases and depression in older persons in the community: the Longitudinal Aging Study Amsterdam. Journal of clinical epidemiology. 2004;57:187–194. doi: 10.1016/j.jclinepi.2003.01.001. [DOI] [PubMed] [Google Scholar]
- 16.Vanitallie TB. Frailty in the elderly: contributions of sarcopenia and visceral protein depletion. Metabolism: clinical and experimental. 2003;52:22–26. doi: 10.1016/s0026-0495(03)00297-x. [DOI] [PubMed] [Google Scholar]
- 17.Radloff L. The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 18.Beekman AT, Deeg DJ, Van Limbeek J, et al. Criterion validity of the Center for Epidemiologic Studies Depression scale (CES-D): results from a community-based sample of older subjects in The Netherlands. Psychological medicine. 1997;27:231–235. doi: 10.1017/s0033291796003510. [DOI] [PubMed] [Google Scholar]
- 19.Penninx BW, Kritchevsky SB, Yaffe K, et al. Inflammatory markers and depressed mood in older persons: results from the Health, Aging and Body Composition study. Biological psychiatry. 2003;54:566–572. doi: 10.1016/s0006-3223(02)01811-5. [DOI] [PubMed] [Google Scholar]
- 20.Van Gool CH, Kempen GI, Penninx BW, et al. Impact of depression on disablement in late middle aged and older persons: results from the Longitudinal Aging Study Amsterdam. Social science & medicine (1982) 2005;60:25–36. doi: 10.1016/j.socscimed.2004.04.021. [DOI] [PubMed] [Google Scholar]
- 21.Newman AB, Yanez D, Harris T, et al. Weight change in old age and its association with mortality. Journal of the American Geriatrics Society. 2001;49:1309–1318. doi: 10.1046/j.1532-5415.2001.49258.x. [DOI] [PubMed] [Google Scholar]
- 22.Stevens J, Truesdale KP, McClain JE, et al. The definition of weight maintenance. International journal of obesity (2005) 2006;30:391–399. doi: 10.1038/sj.ijo.0803175. [DOI] [PubMed] [Google Scholar]
- 23.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. Journal of personality and social psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 24.Chapman KM, Nelson RA. Loss of appetite: managing unwanted weight loss in the older patient. Geriatrics. 1994;49:54–59. [PubMed] [Google Scholar]
- 25.Crighton MH, Puppione A. Geriatric neutrophils: implications for older adults. Semin Oncol Nurs. 2006;22:3–9. doi: 10.1016/j.soncn.2005.10.002. [DOI] [PubMed] [Google Scholar]
- 26.Holloszy JO. The biology of aging. Mayo Clinic proceedings. 2000;75 Suppl:S3–S8. discussion S8-9. [PubMed] [Google Scholar]
- 27.Visser M, Goodpaster BH, Kritchevsky SB, et al. Muscle mass, muscle strength, and muscle fat infiltration as predictors of incident mobility limitations in well-functioning older persons. The journals of gerontology. 2005;60:324–333. doi: 10.1093/gerona/60.3.324. [DOI] [PubMed] [Google Scholar]
- 28.Lyness JMCE. Vascular disease and depression. Models of the interplay between psychopathology and medical comorbidity, in Physical illness and depression in older aldults. In: Williamson DS GM, Parmelee PA, editors. A handbook of theory, research, and practice. New York: Kluwer Academic / Plenum Publishers; 2000. pp. 33–49. [Google Scholar]
- 29.Tsigos C, Chrousos GP. Hypothalamic-pituitary-adrenal axis, neuroendocrine factors and stress. Journal of psychosomatic research. 2002;53:865–871. doi: 10.1016/s0022-3999(02)00429-4. [DOI] [PubMed] [Google Scholar]
- 30.Yang Y, George LK. Functional disability, disability transitions, and depressive symptoms in late life. Journal of aging and health. 2005;17:263–292. doi: 10.1177/0898264305276295. [DOI] [PubMed] [Google Scholar]
- 31.Bruce ML. Depression and disability in late life: directions for future research. Am J Geriatr Psychiatry. 2001;9:102–112. [PubMed] [Google Scholar]
- 32.Vink D, Aartsen MJ, Comijs HC, et al. Onset of anxiety and depression in the aging population: comparison of risk factors in a 9-year prospective study. Am J Geriatr Psychiatry. 2009;17:642–652. doi: 10.1097/jgp.0b013e3181a65228. [DOI] [PubMed] [Google Scholar]
- 33.Extending life, enhancing life: a national research agenda on aging Washington, D.C, Institute of Medicine (U.S.)Committee on a National Research Agenda on Aging. Lonergan ET: National Academy Press; 1991. [PubMed] [Google Scholar]
- 34.Robertson RG, Montagnini M. Geriatric failure to thrive. Am Fam Physician. 2004;70:343–350. [PubMed] [Google Scholar]
- 35.Hammen C. Stress and depression. Annual review of clinical psychology. 2005;1:293–319. doi: 10.1146/annurev.clinpsy.1.102803.143938. [DOI] [PubMed] [Google Scholar]
- 36.Torres SJ, Nowson CA. Relationship between stress, eating behavior, and obesity. Nutrition (Burbank, Los Angeles County, Calif. 2007;23:887–894. doi: 10.1016/j.nut.2007.08.008. [DOI] [PubMed] [Google Scholar]
- 37.Blair SN. Evidence for success of exercise in weight loss and control. Annals of internal medicine. 1993;119:702–706. doi: 10.7326/0003-4819-119-7_part_2-199310011-00015. [DOI] [PubMed] [Google Scholar]