Abstract
Neurodegenerative and infectious disorders including Alzheimer’s and Parkinson’s diseases, amyotrophic lateral sclerosis, and stroke are rapidly increasing as population’s age. Alzheimer’s disease alone currently affects 4.5 million Americans, and more than $100 billion is spent per year on medical and institutional care for affected people. Such numbers will double in the ensuing decades. Currently disease diagnosis for all disorders is made, in large measure, on clinical grounds as laboratory and neuroimaging tests confirm what is seen by more routine examination. Achieving early diagnosis would enable improved disease outcomes. Drugs, vaccines or regenerative proteins present “real” possibilities for positively affecting disease outcomes, but are limited in that their entry into the brain is commonly restricted across the blood–brain barrier. This review highlights how these obstacles can be overcome by polymer science and nanotechnology. Such approaches may improve diagnostic and therapeutic outcomes. New developments in polymer science coupled with cell-based delivery strategies support the notion that diseases that now have limited therapeutic options can show improved outcomes by advances in nanomedicine.
Keywords: Nanomedicine, Bioimaging, Neurodegenerative disorders, Magnetic resonance spectroscopy, Polymer chemistry, Blood-brain barrier
1. Introduction
Neurodegenerative disorders, Alzheimer’s and Parkinson’s diseases (AD and PD), stroke, amyotrophic lateral sclerosis (ALS), multiple sclerosis (MS), and HIV-1-associated dementia (HAD) are amongst the principal debilitating conditions of the 21st century [1–5]. The group of diseases is linked to advancing age, environmental cues and/or disordered immunity and less with host genetics [6]. As modern medicine can manage only symptoms, not the disease process, the stakes to find effective means for diagnosis and therapy are significant. The accumulation, aggregation and modification of normal host proteins, the effects of viral infections, disrupted blood flow, alterations in tissue homeostasis, and immunological damage underlie the pathogenesis of most neurodegenerative disorders [7–9]. How to slow or halt this process as well as to define the onset and progression of disease remains the focus of many research efforts [10,11]. Such works have met with mixed results in translating promising laboratory and animal study results to clinical practice. Indeed, disease treatments remain palliative [12]. Nonetheless, there remains considerable promise for new disease modalities if issues of untoward side effects and site-directed drug delivery can be overcome [13–16].
To best affect disease outcomes, drugs or immune modulators must enter the central nervous system (CNS) and thus penetrate the blood–brain barrier (BBB). This is not a simple task. Indeed, the BBB represents a significant impediment for drug delivery due to its structure and functional complexities [17]. Entry of low molecular weight compounds and biomacromolecules are significantly restricted in entering the brain and include imaging contrast agents, drugs, nucleic acids, and proteins representing a major bottleneck in the development of efficacious and safe treatment and diagnostic modalities. This is especially noteworthy at early stages of the disease when the BBB is intact. The limitation in BBB permeability is attributed to brain microvessel endothelial cells (BMVEC) forming brain capillaries. Tight intercellular junctions, low pinocytic potential, expression of outwardly drug efflux transporters and high levels of drug metabolizing enzymes, all contribute to barrier function and restricting passage of solutes from blood to brain. Overall, the ability to circumvent the BBB barrier to affect biological processes in brain will significantly impact the detection, treatment, and understanding of disease progression. Safe, site-specific, and efficient delivery of compounds to CNS disease sites remains a singular goal in achieving optimal therapeutic outcomes to combat neurodegenerative diseases.
Towards these goals, out laboratories have sought to join efforts to improve drug delivery for neurodegenerative disorders using nanomedicine and polymer techniques. The foundation for these works rests, in part, by both utilizing and combating neuroinflammatory processes. Indeed, epidemiologic, animal, human, and therapeutic studies strongly support the presence of a central neuroinflammatory cascade underlying the pathogenesis of neurodegenerative diseases regardless of etiology. Our own works seek to harness such inflammatory processes by using circulating immunocytes to attenuate microglial neurotoxic responses or as carriers of drugs packaged within nanoparticles [18]. Moreover, delivery of biologically active agents across the BBB has advanced through the discovery of drug nanocarriers, polymeric modulators of drug efflux transport, and polymeric conjugates [19]. The singular goal is in developing therapeutic interventions that positively affect the tempo and progression of human CNS disease. We believe that to achieve these goals, cross-disciplinary expertize in biomedical sciences (neuroscience, pathology, immunology, pharmacology, molecular imaging) and in material, biomaterial, and pharmaceutical sciences (polymers, nanomaterials, drug delivery, and gene delivery) are required.
Although extensive reviews on drug delivery to the brain have emerged in recent years [17,20–35] none describes the recent and significant works that employ cell and polymer-based nanomaterials in CNS delivery. In this regard, balanced discussions are made to describe disease processes and needs together with new research efforts made in nanomedicine. This was done towards what could be applied to better diagnosis and treatment of neurodegenerative disorders. The review is divided into several distinct parts. First, we provide a brief introduction to these disorders including the use of bioimaging in disease diagnosis. Second, we discuss barriers that need to be overcome for successful CNS disease treatment. Third, the major types of nanocarriers (liposomes, nanoparticles, polymeric micelles, nanogels, and others) that show promise for diagnostic and therapeutic agent delivery to the brain are described. Fourth, cell-mediated delivery of nanocarriers to affected brain regions is described. This is done along with their potential applications for improved pharmacokinetics in the body. Fifth, polymeric inhibitors of drug efflux systems are described as means to selectively increase permeability of therapeutic agents in BBB. Finally, we consider chemical modifications of proteins, in particular, conjugation with amphiphilic block copolymers, as novel strategies to increase protein delivery to the brain.
2. Neurodegenerative disorders
AD, the most prevalent of neurodegenerative diseases, is characterized by memory, cognition, and behavior impairments [6]. As time ensues, individuals develop profound memory loss that affects most daily activities and the lives of their loved ones. AD neuropathology shows two types of lesions, senile plaques and neurofibrillary tangles (NFT) composed of β-amyloid (Aβ). Although plaques and NFT appear to be the most prevailing features of AD pathology, they alone are not sufficient to generate the significant and profound neuronal loss during disease. Like in AD, PD symptoms appear gradually but are unique and dependent on the affected brain subregion. They include difficulties in maintaining balance and in ambulation; tremors; inflexibility/stiffness of the limbs and trunk; and bradykinesia (slowness of movement). PD is defined, pathologically, by the loss of dopaminergic neurons (dopamine producing neurons) of the substantia nigra pars compacta (SNpc) and subsequent loss of striatal dopamine projecting to the caudate-putamen [36]. Neuronal damage caused by neurotoxic factors initiated from inflammatory responses by immune activated glia are linked to cognitive and motor deterioration, which contribute to the breakdown of the BBB. This allows leukocytes entry into the brain serving to speed a neuroinflammatory cascade. Although the causes of both AD and PD remain unknown, patterns of familial inheritance suggest a possible connection involving abnormal protein processing (Aβ for AD and alpha synuclein for PD) and accumulation.
After heart disease and cancer within the developed world, stroke is the third largest killer, second most common cause of neurologic disability after AD [37]. There are over five million deaths a year from stroke and over nine million stroke survivors. Between the ages of 45 and 85, 20–25% of men and women, respectively, can expect to have at least one incident of stroke. Atherosclerosis, heart disease, hypertension, diabetes, and life-style habits are risk factors correlated with disease. Unlike AD and PD, many of the risk factors for developing this disease can be modified. The etiology of stroke is brain vascular occlusions (thrombotic stroke) or rupture (hemorrhagic stroke). The neuropathological hallmarks of stroke are necrotic infarcts of variable size with inflammatory gliosis.
ALS, also known as Lou Gehrig’s disease, is a devastating motor neuron disorder and is one of the most common adult-onset neurodegenerative diseases [38]. Muscle weakness is the hallmark sign of ALS, occurring in nearly 60% of patients. The symptoms include tripping, dropping items, abnormal fatigue of the arms and/or legs, slurred speech, muscle cramps, and twitches to towards complete neuromuscular failure and death (typically caused by compromised respiratory function) in three to five years. ALS affects about 5–7/100,000 adults throughout the world with 95% of cases sporadic [39]. ALS pathology is characterized by neuronal degeneration and atrophy confined almost entirely to the upper and lower motor neurons. Missense mutations on chromosome 21 encoding for a Cu/Zn binding protein called superoxide dismutase is linked to disease [40]. SOD is the most important enzyme in defense against oxidative stress.
A fifth neurodegenerative disorder occurs secondary to infection with the human immunodeficiency virus (HIV) and is called HIV-associated dementia (HAD) or more generally HIV-associated cognitive dysfunction. Today more than 40 million people are living with HIV disease and the representing death toll is in excess of 25 million people. Nearly half of HIV infected people display some form of neurological dysfunction; most likely due to early entry of HIV-1 into the CNS [4,5]. The virus enters the brain within CD4+ T lymphocytes and/or mononuclear phagocytes (MP: dendritic cells, monocytes, and macrophages) [41]. The pathology of HAD revolves around the formation of multi-nucleated giant cells of MP lineage that are also the main reservoirs for virus in the brain [42]. MP can yield a variety of disease outcomes as they function to present, phagocytize and clear microbial infections and tissue debris, and secrete a variety of bioactive molecules including those that affect immunity and tissue homeostasis [43].
Reactive MP responses predominate at the site of neuronal injury in HAD and may be amplified through paracrine and autocrine processes [44]. Specifically, microglial responses are likely to play a central role in the loss of neurons [45]. MP can secrete neurotoxins and induce neuronal injury leading to neurocognitive and motor impairments. Clear connections exist between inflammation and neurodegeneration [46,47]. Microglial cells rapidly respond to insults with hypertrophy, proliferation, and expression of proinflammatory cytokines [48]. Indeed, in neurodegenerative diseases, activated microglia affect neuronal injury through secretion of glutamate, proinflammatory factors, reactive oxygen species, quinolinic acid amongst others and by mobilization of adaptive immune responses and cell chemotaxis leading to transendothelial immune cell migration across the BBB and perpetuation of neural damage [49–52]. As disease progresses, inflammatory secretions engage neighboring glial cells, including astrocytes and endothelial cells, resulting in a vicious cycle of autocrine and paracrine amplification of inflammation resulting in significant tissue injury and deficits in neurogenesis [53]. Emphasizing the role of microglia more broadly in the pathogenesis of neurodegenerative diseases is the epidemiological data that has shown the use of non-steroidal anti-inflammatory drugs decreases the risk of disease [54,55].
The means to halt the neurotoxic potential of microglia as well as the overall pathogenic disease process are vaccines designed to clear deposits of aggregated and toxic proteins or prevent the later stages of neuronal damage regardless of inciting event. Drugs are also becoming available serving to stimulate neuronal repair and differentiation [12,15,55,56]. However, each of these therapeutic modalities shows limitations due to toxicity and BBB penetration.
Finally, lysosomal storage disorders (LSDs; Gaucher’s disease, Niemann-Pick disease, Tay-Sachs disease and Sandhoff’s disease, Krabbe’s disease, Fabry’s disease, metachromatic leukodystrophy amongst nearly 50 total disorders) are recessive genetic diseases that occur as a consequence of deficiencies in cellular enzymatic acid hydrolases (lysosomal enzymes) that catalyze the metabolism and clearance of glycoprotein metabolism and glycolipids [57]. The brain is particularly rich in gangliosides and is such particularly affected. Moreover, the presence of lysosomal enzymes in the reitculoendothelial system also makes the liver and spleen particularly vulnerable. Inherited deficiencies of lysosomal enzymes result in accumulation of undegraded proteins and metabolites including break down products of cell metabolism and macromolecules. They can also occur as a consequence of transporter protein defects. Such deficiencies lead to pathogenic accumulation of proteins within lysosomes. Current treatment modalities for LSDs are bone marrow transplantation together with enzyme replacements. These provide benefit to visceral manifestations but not address the CNS pathologies that are both a common and significant signature for disease [58]. These are limited as therapeutic agents cannot cross the BBB. Thus, the clinical severity including neuropsychiatric symptoms and the lack of efficient therapy led to trials of gene therapy (ex vivo and in vivo) and development of stem cell and encapsulation cell therapeutic approaches for disease [59–62]. Injections of recombinant virus vectors for systemic and CNS malfunctions directly into the brain have bypassed the BBB but the possibilities for tumor formation and toxicity could limit their development and use. Nonetheless, genes encoding the normal lysosomal enzymes with new vectors can modulate immunogenicity, transduction efficacy, tumor formation, and cell-targeting are fertile research areas. Improving the effectiveness of CNS treatment outcomes through targeted delivery of enzymes and genes into brain cells is just now being developed. This may be achieved through the CNS implantable biocapsules and micro-electro-mechanical system approaches or using nanomedicine approaches discussed in this paper.
3. Bioimaging of the CNS
Diagnostic decisions for neurologic and neurodegenerative disorders can often be clouded by concomitant depression, motor impairments, and lethargy that follow debilitating immune suppression and weight loss. In reality, cognitive, motor, and behavior abnormalities underlie a variety of neurological dysfunctions associated with neurodegenerative disorders and HIV-1 infection. Thus, combinations of clinical, laboratory, and neuroimaging tests, while not irrefutably conclusive, are essential to provide diagnostic support [63–66]. A wide range of neuroimaging techniques can aid in the diagnosis of neurological complications associated with neurodegenerative disorders. These techniques include nuclear medicine studies such as positron emission tomography (PET) and single photon emission computed tomography (SPECT). Morphological studies include magnetic resonance imaging (MRI) and computed tomography (CT). Studies of brain physiology and biochemistry consist of SPECT and MRI perfusion, magnetization transfer MRI (to assess myelin loss), 1H and 31P magnetic resonance spectroscopy (MRS) and magnetic resonance spectroscopic imaging (MRSI) [67–73].
These techniques have the potential to identify underlying neurological processes involved in disease progression. Thus, MRI, CT, or diffusion tensor imaging (DTI) is often used to supplement clinical and neurological examinations for diagnosis of a variety of degenerative disorders of the CNS including HIV-1 associated cognitive impairments [74–77]. These radiographic and functional imaging tests can delineate the structural and metabolic effects of diseases of the brain and differentiate them from other types of degenerative, infectious or cancerous lesions. CT, MRI, and DTI easily depict brain atrophy. Computerized tomography of the brain characteristically can show mass lesions or cerebral atrophy and is reflective of moderate to severe disease [70,78,79]. Indeed, MRI studies of patients can show changes in ventricular size, sulcal widening, diffuse white matter abnormalities and atrophy. On MRI these lesions appear as a fluffy, non-focal signal hyperintensity on T2-weighted images involving bilaterally the periventricular and centrum semiovale white matter [78]. The distribution and existence of such lesions does not necessarily correlate with clinical examination and a certain degree of parenchymal involvement, seen in MRI evaluations, may be visible in asymptomatic patients. However extensive white matter involvement is more likely to be symptomatic. These changes, however, usually appear in the later stages of neurodegenerative disease and thus are not useful for diagnosis. MRSI has emerged as an effective way to detect early brain dysfunction. MRSI is a non-invasive method of quantitating neuronal loss performed with conventional resonance imagers. Assessment of in vivo metabolism gives biochemical information that complements the structural information from the MRI examination in a quantitative fashion. MRSI has shown that in early stages of dementia in frontal white matter shows changes suggestive of glial proliferation and cell membrane injury evaluated using measurement of N-acetyl compounds. Reduction in N-acetylaspartate (NAA), a marker for neuronal loss, using in vivo proton MRSI in patients with advanced neurodegenerative disease has been proposed as a therapeutic monitoring system [80]. The ratio of NAA to creatine reflects neuronal density and correlates with cognitive impairment. MRSI has also demonstrated progressive neuronal loss over time [73,81,82]. As the precision of these technologies improve metabolic alterations and neuronal loss can be determined much earlier and with broader applicability to monitor disease.
All of the bioimaging techniques have the potential advantage of detecting early functional abnormalities before morphological changes occur. These provide a broad array of tests to pinpoint onset and degree of neural injury. Although structural imaging techniques are not sensitive indicators of neurological disease, functional imaging has greater value as it can reveal abnormalities before structural atrophy or focal CNS lesions are visible when subtle clinical abnormalities are seen on examination. All together, imaging tests afford conformation of what is seen on clinical and laboratory examination and cannot be used independently as a measure of disease diagnosis or staging. This all points to the need for better and earlier tests as these will certainly prove to be of critical importance to provide the most effective treatments. Such treatments need not only mean early intervention but means to effectively penetrate barriers so that CNS drug delivery can be optimized without secondary toxicities to the human host.
4. Barriers to CNS drug delivery
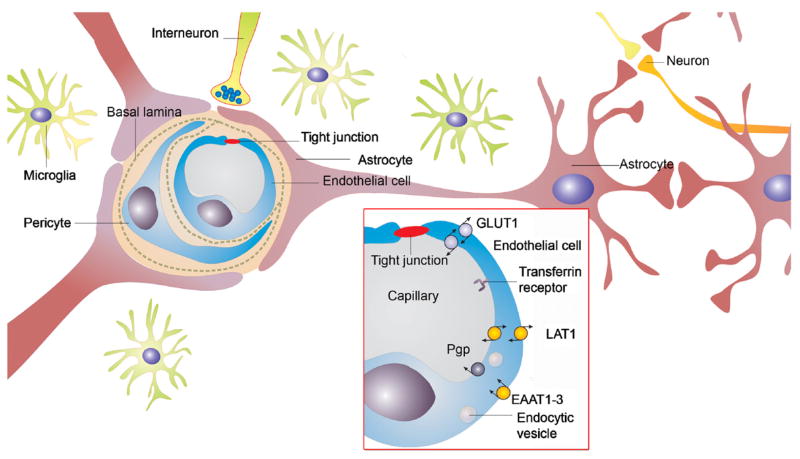
The brain is separated from the rest of the body by formidable barriers that hinder delivery of diagnostic and therapeutic agents to CNS. Understanding physiological features of these barriers is necessary for discovery of the means toward effective delivery of drugs and imaging agents. The BBB consists of walls of capillaries that separate brain from circulating blood (Fig. 1). In the human brain there are approximately 100 billion capillaries that have a net surface area of nearly 20 square meters. Despite its enormous surface area, the BBB lacks intercellular cleft and fenestrae and significantly restricts the entry of solutes to the brain from the periphery. Its low permeability is attributed, in large part, to BMVEC, which forms tight junctions and have low pinocytic activity [17,83,84]. Some relatively lipophilic and low molecular weight substances can transport across the BMVEC by passive diffusion. However, a large number of lipophilic compounds are rapidly effluxed from the brain into the blood by extremely effective drug efflux systems expressed in the BBB [85–88]. These efflux systems include P-glycoprotein (Pgp), multi-drug resistance proteins (MRPs), breast cancer resistance protein (BCRP), and the multi-specific organic anion transporter (MOAT). There is also an enzymatic barrier to drug transport in the BMVEC. Activity of many enzymes that participate in the metabolism and inactivation of endogenous compounds, such as γ-glutamyl transpeptidase, alkaline phosphatase, and aromatic acid decarboxylase is elevated in cerebral microvessels [89,90].
Fig. 1.
The BBB is formed by BMVEC (see insert) that form tight junctions and express different transport systems such as Pgp, glucose transporter (GLUT1), large amino acid transporter (LAT1), excitatory amino acid transporters (EAAT1-3), transferrin receptor and others.
Along with isolating brain with respect to entry of “unwanted” molecules, BBB provides for selective transport of small molecules, polypeptides and even cells to the CNS. In particular, nutrients and endogenous compounds required by CNS, such as amino acids, glucose, essential fatty acids, vitamins, minerals, electrolytes, are effectively carried to the brain by numerous saturable transport systems expressed at the BBB [91]. By first restricting and then selectively transporting circulating substances the BBB acts as a regulatory membrane, which largely defines the homeostatic and nutritive CNS environment. The BBB also has a role in brain and peripheral tissue communication by allowing some peptides and regulatory proteins into the CNS [85,91–94]. The polypeptides, such as wheatgerm agglutinin, leptin, and insulin cross the BBB by adsorptive transcytosis [95,96].
Finally, the endothelial cell monolayer of cerebral vessels and its basement membrane are covered by astrocyte endfeet, leptomeningeal cells, and a parenchymal membrane that contribute to the formation of the BBB. As a consequence of this morphology, leukocyte penetration into the brain involved several steps to complete. First, penetration of the endothelial cell monolayer and underlying basement membrane need occur and involves an integrin beta1-mediated process. Second, is penetration through the parenchymal basement membrane and glia limitans likely involving macrophage-derived gelatinase (matrix metalloproteinase MMP-2 and MMP-9 activity [97]).
Brain capillaries account for about 95% of brain vasculature. The circumventricular regions of the CNS do not express the classical brain capillary endothelial cells, but have microvessels similar to those of the periphery. Though such capillaries are more permeable to solutes, the epithelial cells of choroid plexus and tanycytes of other regions adjacent to the ventricles of the brain form tight junctions to prevent transport from blood to brain. Choroid plexus is a major site of cerebrospinal fluid (CSF) production. The epithelial cell barrier of choroid plexus restricting transport of solutes from blood to CSF is known as the blood–CSF barrier (BCB). This barrier is more “leaky” than BBB and its electric resistance is about 10 times less. Although, BCB surface area is much smaller than that of BBB, its leakiness may account for the small amount of albumin found in the CSF [98]. Furthermore, recent evidence shows that antibodies and erythropoietin exert their effects by entering the brain through CSF [99,100]. At the same time, penetration of solutes across BCB does not guarantee a solute’s transport into the brain due to tremendous diffusion distances between the CSF and brain interstitial fluid. All together, due to small surface area and diffusion limitations, BCB has not been considered as an option for delivery of diagnostic and therapeutic agents.
5. Nanocarriers for CNS drug delivery
The development of man-made polymers for controlled release of therapeutic agents was triggered by discoveries made by Folkman and Long who demonstrated that hydrophobic dyes diffuse through a silicone tubing wall at a constant rate [101,102]. Since then, numerous polymeric materials and devices for drug delivery have been developed, including films, tablets, gels, microspheres and others [103,104]. Many of these materials and devices are used clinically. Some, materials such as intracranial polymeric implants were explored for sustained delivery of therapeutic molecules to the brain, for example in treatment of tumors [105,106]. However, such localized delivery approaches have been hampered by their invasiveness, inflammatory responses to implants and limited distribution of therapeutic molecules around the implantation site [107–109].
Therefore development of polymer therapeutics and nanomedicines that can overcome barriers to CNS and can be delivered systemically would be a tremendous advancement in diagnosis and treatment of neurodegenerative disorders, brain cancer and trauma. A number of polymer therapeutics is on the market or undergoing clinical evaluation to treat cancer and other diseases [110,111]. These are mainly low molecular weight drugs or therapeutic proteins that are chemically linked to water-soluble polymers to increase drug solubility, drug stability, or enable site-specific transport of drugs to target tissues affected by disease. Separately, PEG-coated liposomes carrying chemotherapeutic drugs have been approved for clinical use [112,113]. They served as first examples of nanoscale materials that found practical application in medicine, called collectively nanomedicines. Another example of a nanomaterial-based drugs now available for disease treatment is albumin-bound paclitaxel [114]. In addition, nanoparticles made of poly(D,L,lactide-co-glycolide) (PLGA) and other biodegradables have the potential to enhance delivery of drugs, genes, and vaccines to combat disease [115].
A new generation of nanomedicines has emerged, which uses novel self-assembled nanomaterials for drug and gene delivery [116–122]. Examples include polymeric micelles [118,123–126], DNA/polycation complexes (“polyplexes”) [127–135], block ionomer complexes [116,136–139], nanogels [140–144] and others. Of these materials, polymeric micelles have been evaluated in human trials for the delivery of anti-cancer agents [145–149]. The promising results of these trials suggest that polymeric micelles are likely to find practical use in medicine. Moreover, further advances in polymer chemistry resulted in the development of novel nanomaterials with unique spatial orientation of molecular groups, including dendrimers [150], star-polymers [151], and cross-linked polymer micelles [152–155]. In parallel, advances in nanomanufacturing and nanofabrication led to the development of carbon nanotubes [156,157], and polymeric nanofibers [158,159]. In terms of delivery of bioactive molecules, these materials are at relatively early development stages. However, their unique structural and mechanical properties hold great promise for drug delivery, bioimaging and tissue engineering research [160,161].
All together, nanomedicines have emerged serving to improve delivery of drugs and diagnostic agents to disease target sites and to trigger release. Moreover, they can be targeted not only to an organ or tissue, but to a particular cell or even an intracellular compartment. These systems often exhibit similarity in their size and structure to natural carriers such as viruses and serum lipoproteins, and offer multi-faceted specific properties useful in applications for delivery of imaging and therapeutic agents to CNS. Some specific examples of the nanomaterials that were evaluated for brain delivery or have potential in such applications are considered below.
5.1. Liposomes
Liposomes are vesicular structures composed of unilamellar or multi-lamellar lipid bilayers surrounding internal aqueous compartments. Their sizes vary from several nanometers to several microns. Relatively large amounts of drug molecules can be incorporated into liposome aqueous compartments (water soluble compounds) or within lipid bilayers (lipophilic compounds). Conventional liposomes usually are rapidly cleared from circulation by reticuloendothelial system (RES). Extended circulation time can be accomplished with small-sized liposomes (< 10 nm) composed of neutral, saturated phospholipids and cholesterol. Furthermore, many modern studies use liposomes with a surface modified with polyethylene glycol (PEG) [162–164]. Such modification (“PEGylation”) reduces opsonisation of liposomes in plasma and decreases its recognition and removal by the MP system in liver and spleen. PEGylated (or “stealth”) liposomes have circulation half-life as long as 50 h in humans [165]. One example, a doxorubicin encapsulated in PEGylated liposome, Doxil®, was approved for treatment of ovarian cancer, AIDS-related Kaposi’s sarcoma SS [112] and metastatic breast cancer [166]. Overall, encapsulation of a drug into liposomes may prolong drug circulation time in blood stream, reduce drug side effects, and enhance drug therapeutic effects in CNS. Indeed, liposomes were evaluated for CNS drug delivery in a number of publications [162,167–179].
Liposomes are readily taken up by macrophages, microglia and astrocytes in the CNS. PEGylated liposomes accumulate more rapidly in brain when the BBB is compromised such as in experimental autoimmune encephalomyelitis (EAE) [174]. Interestingly, brain accumulation of liposomes labeled with radioactive isotope, 99mTc is increased during EAE [168]. PEGylated liposomes coupled with monoclonal antibodies to glial fibrillary acidic protein (GFAP), an antigen expressed in astrocytes show altered brain penetrance [178]. Incapable of penetrating a normal BBB, immunoliposomes used to treat glial brain tumors that express GFAP can reach their disease site when the BBB is partially permeabilized [178]. The mechanism(s) of brain accumulation in disease may involve enhanced permeability and retention (EPR) of circulating liposomes at sites of disease-induced BBB compromise. Alternatively liposomes may be captured by MP, which then cross the BBB. Liposomes have also been conjugated with mannose, transferrin and insulin receptors at the surface of brain capillaries [167,180]. In particular, transferrin receptor is necessary to deliver iron across BBB [181]. Expression of this receptor in BBB increases during certain pathologies, for instance after stroke. Hence, transferrin-conjugated liposomes successfully targeted post-ischemic brain endothelium in rats [175]. In addition considerable work was reported on antibodies to transferrin receptor, OX26, that were linked to the surface of PEGylated liposomes via PEG spacers. Such immunoliposome constructs were used to deliver small drugs, Daunomycin [162], and Digoxin [182] as well as plasmid DNA [169] to the brain. Notably, OX26-conjugated liposomes selectively distributed to BMVEC but avoided choroid plexus epithelium, neurons, and glia [177]. (In related work OX26 antibodies directly linked to oligonucleotides [183] or fibroblast growth factor [172] enhanced delivery of these molecules to the brain.) Another example of a brain targeting vector is a genetically engineered monoclonal antibody to human insulin receptor, 83-14 MAb [184]. This vector was also used for targeting liposomes with a reporter gene to the brain [173]. Furthermore, PEGylated immunoliposomes containing antibodies directed to insulin or transferrin receptors were used successfully as carriers for gene replacement therapy in PD model [179]. The mechanism by which immunoliposomes cross the BBB is not fully understood. It was hypothesized that it involves binding of immunoliposomes to capillary luminal membrane receptors, fusion of the liposomes with several vesicular pits into a large vesicle and transcytosis of this vesicle to the abluminal membrane border [23].
5.2. Nanoparticles
Nanoparticles can be used for drug and gene delivery [21,30,31,33,140,142,185–194]. They are often composed of insoluble polymer(s). During their formulation drug is captured within the precipitating polymer, forming nanoparticle, and then released upon degradation of a polymer in the biological environment. The methods for preparation of nanoparticles commonly employ the use of organic solvents that may result in degradation of immobilized drug agents, especially biomacromolecules. To allow for efficient cell uptake the nanoparticle size should not exceed ca. 100–200 nm. In addition, nanoparticle surface is often modified by PEG to increase its dispersion stability and extend its circulation times in the body [188–190]. For example, poly(butylcyanoacrylate) nanoparticles were evaluated for CNS delivery of several drugs [21,190,193,195–197]. These nanoparticles were coated with PEG-containing surfactants, such as Tween 80. After injection, they localized in the choroid plexus, via mater and ventricles, and, to a lower extent, in the capillary endothelial cells. Some evidence suggests that increased brain delivery with surfactant-coated poly(butylcyanoacrylate) nanoparticles may be associated with non-specific permeabilization of BBB and toxicity [198]. Drugs delivered to CNS in these constructs included, analgesics (Dalargin, Loperamide), anti-cancer agents (Doxorubicin), anti-convulsants (NMDA receptor antagonist, MRZ 2/576), and peptides (Ddalargin and Kytorphin) [196,197]. For example, nanoparticles prolonged anti-convulsive activity of MRZ 2/576 compared to the free drug [199]. In another study, Doxorubicin-laden nanoparticles increased survival in rats with aggressive glioblastoma [197]. More recently nanoparticles conjugated with metal chelators, Desferioxamine or D-Penicillamine, were shown to cross the BBB, chelate metals, and exit through the BBB with their complexed metal ions [33,194]. This method may prove to be useful for reducing the metal load in neural tissue thus mitigating harmful effects of oxidative damage during AD and other CNS diseases.
A subset of nanoparticles, nanospheres are hollow species prepared by microemulsion polymerization or covering colloidal templates with a thin layer of polymer material followed by template removal [200]. Carboxylated polystyrene nanospheres (20 nm) were evaluated for CNS drug delivery [201]. After intravenous injection such nanospheres remained in the vasculature under normal conditions. However, they extravasated into brain during cerebral ischemia-induced stress that partially opened the BBB [202]. Such nanospheres may have potential for CNS delivery of drugs and imaging agents during ischemia, stroke and other conditions that disrupt the BBB.
Drug nanosuspensions represent crystalline drug particles often stabilized by non-ionic PEG-containing surfactants or with mixtures of lipids [203,204]. They can be manufactured by a variety of techniques such as media milling, high-pressure homogenization or using emulsions and microemulsions as templates [205,206]. These procedures often result in irregular shaped, rather polydisperse materials of near micron or sub-micron particle size range. Major advantages of this technology include its simplicity, high drug loading capacity and applicability to many drugs including very hydrophobic compounds [206,207]. Similar to regular nanoparticles, nanosuspension surfaces can be modified to increase its delivery to brain after systemic administration [207]. One application of a nanosuspension for cell-mediated delivery to CNS is discussed in a subsequent section.
5.3. Polymeric micelles
Polymeric micelles (“micellar nanocontainers”) have also been developed as carriers of drugs [125,208–212] and diagnostic imaging agents [213]. They form spontaneously in aqueous solutions of amphiphilic block copolymers and have a core-shell architecture with a core of hydrophobic polymer blocks (e.g., poly(propylene glycol) (PPG), poly (D,L-lactide), poly(caprolactone), etc.) and a shell of hydrophilic polymer blocks (often PEG). The size of polymeric micelles usually varies from ca. 10 to 100 nm. Their core can incorporate considerable amounts (up to 20–30% wt) of water-insoluble drugs preventing premature drug release and degradation. The shell stabilizes micelles in dispersion and masks the drug from interactions with serum proteins and untargeted cells. After reaching target cells drug is released from the micelle via diffusion. Several clinical trials are completed or underway to evaluate polymeric micelles for delivery of anti-cancer drugs [145–149].
One early study used micelles of Pluronic® block copolymers (PEG-b-PPG-b-PEG) as carriers for CNS drug delivery [123,214]. These micelles were conjugated with either polyclonal antibodies against brain α2-glycoprotein or insulin as targeting moieties. Both antibody- and insulin-vectorized micelles were shown to deliver a drug or a fluorescent probe to brain in vivo [214]. Furthermore, there was a considerable increase in neuroleptic activity of a drug (haloperidol) solubilized in the targeted micelles compared to a free drug. Subsequent studies demonstrated that insulin-modified micelles undergo receptor-mediated transcytosis in BMVEC from luminal (blood) to abluminal (brain) side [215].
Polyion complex micelles (also termed “block ionomer complexes”) are novel nanosystems for incorporation of charged molecules. They are formed as a result of the reaction of double hydrophilic block copolymers containing ionic and non-ionic blocks with macromolecules of opposite charge including oligonucleotides, plasmid DNA and proteins [136,216–221] or surfactants of opposite charge [222–227]. For example, block ionomer complexes were prepared by reacting trypsin or lysozyme (that are positively charged under physiological conditions) with an anionic block copolymer, PEG-poly(α,β-aspartic acid) [218,219]. Such complexes spontaneously assemble into nanosized particles having core-shell architecture. The core contains polyion complexes of a biomacromolecule and ionic block of the copolymer. The shell is formed by the non-ionic block. In case of surfactant-based complexes the core is composed of mutually neutralized surfactant ions and polyion chains. It contains hydrophobic domains of surfactant tail groups and can additionally incorporate water-insoluble drugs [139,224]. Depending on surfactant and block copolymer architectures the complexes assume different morphologies including vesicles and micelles of different shapes [223,228]. These nanomaterials are versatile and can incorporate solutes of different structure with high loading capacity. Furthermore, they can release solutes upon change of environmental conditions such as pH (acidification), concentration and chemical structure of elementary salt [139,226]. These nanomaterials were shown to efficiently deliver DNA molecules in vitro and in vivo [216,229–231] although no study on their delivery to CNS was reported so far.
Advances were made to develop stable polymeric micelles that do not dissociate during circulation in the body. Examples include amphiphilic scorpion-like block copolymers with low critical micelle concentration (CMC) [151] as well as various types of unimolecular micelles based on amphiphilic star-like macromolecules with covalently bound hydrophobic cores [151,154,232,233]. Core-polymerization was employed to stabilize micelles of heterotelechelic amphiphilic block copolymers containing polymerizable groups at the ends of hydrophobic blocks [234]. Wooley et al. have developed cage-like nanostructures on the base of polymeric micelles with hydrophobic core and cross-linked anionic shell [155,235,236]. In addition micelles with cross-linked ionic cores were prepared by self-assembly of ionic blocks of double hydrophilic block copolymers with a condensing agent, followed by chemical cross-linking of ionic blocks [153]. The resulting micelles contain a hydrophilic PEO shell and a cross-linked hydrophilic ionic core, which is swollen in water and can incorporate hydrophilic drugs and imaging agents [237,238]. In another study to improve stability of polyion complex micelles with immobilized proteins, protein and block ionomer were additionally cross-linked with each other [218,220]. Similarly, in surfactant based block ionomer complexes surfactant molecules were chemically linked to each other (“dimerized”) forming stable vesicles [239]. All together polymeric micelles of various types is a versatile platform for delivery of imaging and therapeutic agents and one should expect further development of these systems for CNS drug delivery.
5.4. Nanogels
Nanogels are nanosized networks of cross-linked polymers that often combine ionic and non-ionic chains, such as polyethyleneimine (PEI) and PEG [140,142,240,241] or poly(acrylic acid) and Pluronic® [238]. Such networks swell in water and can incorporate through ionic interactions of oppositely charged molecules such as oligonucleotides, siRNA, DNA, proteins and low molecular mass drugs. Their loading proceeds with very high capacities (up to 40–60% wt) not achieved with conventional nanoparticles [140,191,237,238,240–242]. Because of solubility of PEG chains, individual collapsed nanogel particles do not phase separate and form stable dispersions. Transport of oligonucleotides incorporated in nanogel particles across an in vitro model of the BBB was recently reported [142]. Notably, nanogels decreased degradation of oligonucleotides during their transport in BMVEC. To further enhance delivery across the BBB the surface of nanogels was modified by either transferrin or insulin [142]. In vivo studies suggested that nanogel increased brain uptake of oligonucleotides while decreasing its uptake in liver and spleen. Overall, nanogels are promising carriers for CNS drug delivery, although they are in relatively early stages of development.
5.5. Other nanomaterials
Nanofibers and nanotubes are carbon vapor-grown [243], self-assembled from peptide amphiphiles [244,245] or electrospun from most polymer materials [158]. Carbon nanotubes have attracted attention in nanomedicine although there are also serious concerns regarding their safety [246,247]. Electrospun continuous nanofibers are unique since they represent nanostructures in two dimensions and macroscopic structures in another dimension [158,248]. They are safer to manufacture than carbon nanotubes and pose less risk of air pollution. Electrospun nanofibers of a degradable polymer, PLGA loaded with dexamethasone have been used for neural prosthetic applications [249]. A conducting polymer, poly(3,4-ethylenedioxythiophene), was deposited to the nanofiber surface and the coated nanofibers were then mounted on the microfabricated neural microelectrodes, which were implanted into brain. The drug was released by electrical stimulation that induced a local dilation of the coat and increased permeability. In future, nanotubes and nanofibers can be administered systemically, if the toxicity issues are addressed, for example, by appropriate polymer coating. Continuous nanofibers are more likely to be used in implants and tissue engineering applications.
Dendrimers, are regularly branched polymer molecules with branches growing from one or several centers. They can be formulated non-ocovalently with biological agents, such as DNA or conjugated with pro-drug or imaging agents and thus can be used as delivery vehicles for drug therapy or molecular imaging [250–255]. To the best of our knowledge dendrimers have not been evaluated so far for CNS delivery except for few studies on intratumoral delivery of dendrimer conjugates with anti-cancer agents to treat glioma [256,257]. However, transport of dendrimers in another barrier cell model, intestine epithelial cells (Caco-2) was studied recently [258]. Notably, the generation and surface properties of dendrimers were found to be very important. Cationic dendrimers were generally more toxic and disrupted the tight junctions. These effects increased as dendrimer generation and, consequently, net surface area increased. Surface modification of dendrimers with carboxylic groups greatly decreased the toxicity, although the modified dendrimers still opened tight junctions. In our opinion, it is a matter of time before various dendrimers are applied for CNS delivery of diagnostic and therapeutic agents.
6. Cell-mediated delivery of nanocarriers to the brain
A distinct case of the vehicle-mediated CNS drug delivery employs specific cell carriers that can incorporate micro- and nanocontainers loaded with drugs and act as perfect Trojan horses by migrating across the BBB and carrying drugs to the site of action [259–262]. It is documented that AD, PD, stroke, ALS and HAD, have in common an inflammatory component [263]. The process of inflammation is characterized by extensive leukocytes (neutrophils and monocytes) recruitment. Our knowledge of the function of MP has evolved considerably since Ilya Mechnikov, over a century ago, discovered an inflammatory cell type in starfish larvae capable of engulfing foreign objects. The past century has realized a great deal of progress in understanding the role MP plays in immunity and most notably in the CNS. Macrophages orchestrate intracellular killing of pathogenic microbes, antigen presentation, and secretion of biologically active factors, as well as mediation of pathological processes. Underlying such cellular functions is inflammation; the same response that often proves detrimental in localized and systemic diseases, including those operative in neurodegenerative disorders. Inflammatory processes are engaged in attempts to eliminate the invader along with clearance of damaged tissue. With regards to the nervous system neuroinflammation, perpetrated through activation of brain MP along with other glial elements, including astrocytes and endothelial cells, may act through paracrine pathways to accelerate neuronal injury in highly divergent diseases such as AD, PD, stroke, ALS, HAD and spongiform encephalopathies or prion-mediated neurodegeneration. The biological processes causing inflammatory responses into a neurotoxic state, thus, are common links to many other neurodegenerative diseases. As the role of the immune system is clarified, new opportunities for amelioration of the neurodegeneration from neurotoxins produced by the immune system will become critical for early treatment. In neurodegenerative diseases, CNS inflammatory infiltrates are complex and multi-faceted. The initial responders or the MP cell elements of innate immunity set up a cascade, which later involve the activation and recruitment of the adaptive immune system and ultimately tissue destruction. MP and T cells possess the unique property of migrating toward the site of inflammation through the processes known as diapedesis and chemataxis [264]. Their combat arsenal consists of uptake of the foreign particle, producing toxic compounds, and liberation of substances stored in intracellular vesicles via exocytosis. Therefore, these cells can be used for cell-mediated CNS drug delivery when loaded with a drug and administered into the blood stream.
It has been shown that cells capable of phagocytosis, such as macrophages or monocytes/neutrophils, can endocytose colloidal nanomaterials, for example, liposomes, and subsequently release them into the external media [259,261]. To accelerate the transport of monocytes/neutrophils to the brain site, the drug-containing liposomes were additionally loaded with magnetic particles [261]. Magnetic liposomes demonstrated about a 10-fold increase in brain levels compared to non-magnetic liposomes when local magnetic field was applied. It is noteworthy that both cell types showed preferential uptake of liposomes containing negatively charged lipids (such as phosphatidylserine), or liposomes modified with polyanion than liposomes containing only neutral lipids (such as phosphatidylcholine) [260]. This suggests that by engineering the surface of the nanomaterials one may modulate their uptake into and/or release from the cell carriers to optimize the therapeutic regimen. The phosphatidylserine-containing negatively charged liposomes were shown to increase therapeutic activity of an encapsulated anti-fungal agent, chloroquine, against C. neoformans infection in the mouse brain [262]. The chloroquine-loaded liposomes accumulated inside macrophage phagolysosomes and resulted in a remarkable reduction in fungal load in the brain even at low doses compared to the free drug at high doses, thus increasing the anti-fungal activity of macrophages.
T lymphocytes were also proposed as potential therapeutic drug carriers for cancer treatment [265]. The kinetics of loading and release of nanoparticles coated with cytotoxic antibiotic Doxorubicin into the cells were examined. It was suggested that the immune cells can accomplish target-specific and sheltered transport to the diseased site.
Ability of host cells to home diseased sites after ex vivo manipulation is a fundamental requirement and a major problem for their use as vehicles to target locally acting gene therapy to specific diseased sites. It was demonstrated that in the short term, up to 2 h after re-implantation, macrophages accumulate primarily in the lungs and, to a lesser extent, in the liver and spleen rather than in the target diseased tissue. A small proportion of manipulated macrophages (ranging from 0.2% to 28.8%) homes to the diseased site of interest following systemic administration. However, the presence of labeled macrophages in these sites was found to persist for at least 6–7 days [266]. Therefore, increasing the amount of cell carriers reaching the target site appears to be a crucial point in this type of drug delivery system.
Nonetheless, once the drug delivery vehicle has reached the site, subsequent drug release can occur within the extracellular space, or following internalization of the carrier into the target cell. Drugs with intracellular action, incapable of crossing cell membranes, can be assisted in reaching their cellular or tissue target. Cellular uptake mechanisms vary according to cell type, physicochemical properties of the internalized compound and the mechanisms of activation of the drug or cell carrier [267,268]. Intracellular targeting is feasible through the use of ligands that trigger receptor-mediated endocytosis or, perhaps, by modifying the surface of nanocarriers to induce or enhance cell uptake. Localized delivery of plasmid DNA, proteins and peptides and small molecular weight drugs can now be achieved using nanoparticles where nanoparticles uptake is both concentration- and time-dependent. For example, PLGA nanoparticles are transported into primary endosomes and sorted to either recycling endosomes or secondary endosomes [269]. In the acidic environment of the secondary endosome, the nanoparticle surface changes from anionic to cationic leading to the escape of the nanoparticles into the cytoplasm. While intracellular nanoparticle levels fall, extracellular nanoparticle levels may not fall rapidly. It was shown previously that when nanoparticles are delivered locally, drug levels in tissues can be sustained for up to 7–14 days [270,271]. Pentamidine-laden nanoparticles were studied in Leishmania infected mice [272]. Ultra-structural studies showed drug-loaded nanoparticles trafficking inside Leishmania-infected Kupffer cells. Within these Kupffer cells, the nanoparticles were located within vacuoles and primary lysosomes to form secondary lysosomes. Secondary lysosomes containing nanoparticle with parasitophorous vacuoles were observed. Of clinical significance, liposomal Amphotericin B has been shown to enhance cure rates of fungal infection, with limited side effects and show significantly reduced treatment length [273]. This therapy has replaced antimony and Amphotericin B deoxycholate as the drug of choice for this parasite.
Studies done in our laboratory using indinavir (IDV) nanosuspensions highlighted the importance of cell-based drug delivery for treatment of HIV disease [275–277]. When in an alkaline environment, IDV can be fabricated into nanosuspensions and remain stable. In vitro experiments revealed internalization of the nanosuspensions into macrophage lysosomes. Within the lysosomes, the acidic environment allowed Indinavir to be released from the nanosuspensions. The extracellular release of IDV was dependent on steady-state drug equilibrium within and outside the macrophages. Multiple washings of cells with media allowed for continued release of the drug in cell culture. Results of these experiments also revealed that IDV nanosuspension laden bone marrow derived macrophages (BMM) have the ability to carry and release the drug in tissue. After a single administration, robust lung, liver, and spleen BMM and drug distribution was observed (Fig. 2).
Fig. 2.
Tracking of BBM in mice. MRI and SPECT tests were used to track BMM in tissue after intravenous injection of labeled cells. Top: Time series of weighted MRI after super paramagnetic iron oxide (Feridex) labeled BMM. This demonstrates visible signal (in blue) due to signal loss caused by labeled cell accumulation in the spleen (upper) and liver (lower). The series of photomicrographs shows preinjection (time 0), and 1, 3, and 5 days after injection of the Feridex-labeled BMM. Bottom: Co-registration of 111In/Feridex-labeled BMM by MRI and SPECT. BMM were dual-labeled with Feridex and 111In and transferred to recipient mice. Recipients were anesthetized, positioned in custom built, MRI/SPECT compatible holders with attached fiducial markers and serial acquisitions of MRI and SPECT scans were performed on day 1 after transfer. SPECT data were interpolated to the resolution of the MRI data and fiducial markers were used for scaling and alignment. Reconstructed SPECT images (green) were co-registered and overlaid to MRI scans (red). Displayed co-registered images are 390 μm slices containing spleen (Spl) and kidney (Kid) (left panel) and liver (Liv) (right panel), and show areas of radioactive intensities of 111In-labeled BMM in SPECT images (green) that correspond to loss of MRI signal.
After intravenous injection of nanoparticle IDV laden BMM tissue and sera IDV levels were greater than or equal to 50 μM for 2 weeks. IDV nanosuspension BMM administered to HIV-1-challenged humanized mice revealed reduced numbers of virus-infected cells in plasma, lymph nodes, spleen, liver, and lung, as well as, CD4+ T-cell protection. These data demonstrate that a single dose of IDV nanosuspension, using BMM as a carrier, is effective and leads the way towards consideration for human testing. Although proof of concept for this cell-based delivery system was seen for ART parallel efforts in our laboratory are using the same system for delivery of growth factors and anti-inflammatory medicines in divergent neurodegenerative diseases. These diseases would collectively benefit from immunomodulation (drugs that deactivate microglial responses or affect anti-inflammatory activities in the CNS), neurotrophic factors such as glial derived neurotrophic factor or brain derived neurotrophic factor, and in the case of HIV-1 disease, ART (Fig. 3).
Fig. 3.
Proposed scheme for how macrophage-based nanoparticle drug delivery could affect disease outcomes in neurodegenerative disorders. BMM would enter the brain in significant numbers carried to sites of neuroinflammation through the establishment of a chemokine gradient. Once across the BBB macrophages would release drug to neighboring cells including other macrophages, microglia, astrocytes or neurons. The nanoparticles would dissolve and release drug that would subsequently affect neuronal viability and function, deactivation of neurotoxic inflammatory microglia, anti-retroviral responses and astrocyte neurotrophic activities. (Transport of cells across BBB (“diapedesis”) involving opening of endothelial tight junctions shown in the figure may be an oversimplification. There is evidence that mononuclear cells can traverse cerebral microvessels by a transcellular pathway, leaving the endothelial tight junctions intact [274]).
7. Polymeric inhibitors of drug efflux systems in BBB
An alternative to using nanocarriers or cells capable of crossing into brain is altering permeability of brain capillaries to solutes. Some studies used liposomes for temporal disruption of the BBB allowing passage of solutes to the brain [278]. An endogenetic bioactive peptide, RMP-7 (“Cereport®”) known to open tight junctions in BBB via effect on bradykinin 2 receptors, was linked to conventional liposomes. Transport of such modified liposomes loaded with horseradish peroxidase (HRP) increased in an in vitro model of the BBB compared to the unmodified liposomes [278]. However, potential toxicological implications of such intervention are a major concern. Therefore, more selective and less toxic approaches to altering permeability of BBB with respect to solutes are needed.
Solute transport from blood to CNS is hindered by drug efflux systems expressed within the brain capillary endothelium. Recently, much attention focused on multi-drug efflux transporters, Pgp, MRP1,4,5, and BCRP, MOAT that belong to the ABC cassette (ATP-binding cassette) family [86,279,280]. These transporters utilize ATP as energy source to actively remove drug molecules before they cross into brain parenchyma. Pgp is a most thoroughly studied transport protein with broad specificity to structurally diverse lipophilic and amphiphilic compounds [281]. It restricts CNS entry of many drugs, such as HIV-1 protease inhibitors (ritonavir, nalfinavir, and indinavir) [282], anti-inflammatory agents (prednesolone, dexamethasone and indomethacin) [281,283], neuroleptics (amitriptyline and haloperidol) [284], analgesics (morphine, beta-endorphin, and asimadoline) [285], anti-epileptic agents (carbamazepine, phenobarbital, phenytoin, and lamotrigine) [286], and anti-fungal agents (itraconazole and ketoconazole) [287]. Moreover, delivery of many anti-cancer agents (doxorubicin, vinblastine, paclitaxel, etc.) for treatment of brain tumors is also restricted by Pgp [288].
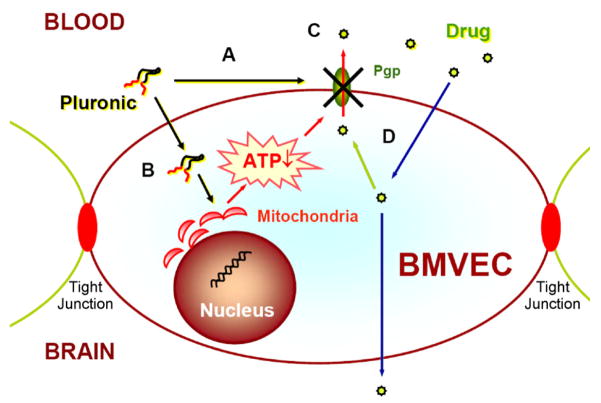
An emerging strategy for enhanced CNS delivery is co-administration of such compounds with inhibitors of drug efflux transporters [289–291]. First generation Pgp inhibitors include Pgp substrates, such as cyclosporine A and verapamil. Unfortunately, they have relatively low affinity to Pgp and high toxicity. Second generation include competitive inhibitors (valspodar, biricodar and others) that are more potent and less toxic than the first generation. However, they also interact with non-targeted proteins and exhibit unfavorable drug interactions, impeding their use. Third generation includes potent non-competitive inhibitors (Laniquidar (R101933), Tariquidar (XR9576); Zosuquidar (LY335979), etc.) that are currently under clinical development. Separately, non-ionic polymeric surfactants were identified as Pgp inhibitors [292–296]. These compounds have AB or ABA structure, where A block is a PEG chain, and B block is either a lipid group (e.g. Chremophor EL, Solutol HS 15, Polysorbate 80, and fatty acid PEG esters), or a PPG chain (Pluronic®). Of these compounds ABA triblock copolymers, Pluronic® were shown to be most active and useful in increasing CNS drug delivery.
Studies using polarized BMVEC monolayers as in vitro model of BBB, and in vivo animal models provided compelling evidence that Pluronic® block copolymers can inhibit Pgp and increase CNS delivery of a broad range of compounds [215,297,299–301]. Some representative examples are shown in Table 1. Maximal activity was observed with copolymers having intermediate lengths of PPG blocks and relatively hydrophobic such as Pluronic® P85 or L61 [302,303]. Mechanism of inhibition is very different compared to conventional low molecular weight inhibitors [303,304]. Pluronic® PPG chains immerse into cell membrane, resulting in local alterations of membrane structure and decrease in net membrane microviscosity (“membrane fluidization”) [304]. This is accompanied by inhibition of Pgp ATPase activity, possibly due to conformational changes in the transport protein, which in absence of copolymer is associated with lipid rafts [305]. Kinetics of Pluronic® effects is similar to that of a mixed type inhibitor-decreasing maximal reaction rate (Vmax) and increasing Michaelis–Menthen constant (Km) [306]. The magnitude of these effects for Vinblasine was as high as over 200-fold change in Vmax/Km. In addition to such a drastic effect at the level of a plasma membrane, copolymers also translocate into cells, inhibit respiration in mitochondria and deplete ATP necessary to sustain efflux and metabolic detoxification functions in barrier cells [304,307]. Remarkably, ATP depletion induced by Pluronic® is linked to multi-drug resistance (MDR) cell phenotype, since this effect is observed selectively in cells that overexpress Pgp (as well as MRPs) [307–309]. The “molecular” targets for Pluronic® in mitochondria isolated from DRM cancer cells include respiratory chain Complexes I and IV (D. Alakhova et al., in preparation). The latter, cytochrome C oxidase, is inhibited selectively in MDR cells, which may be due to differences in mitochondria membrane composition and structure in Pgp overexpressing and non-Pgp cells.
Table 1.
Effect of Pluronic® P85 on luminal to abluminal permeability of Pgp dependent compounds in bovine BMVEC monolayers
| Compound | Drug transporter | Papp × 106 (cm/s)a |
Effecta | |
|---|---|---|---|---|
| Assay buffer | Pluronic® P85 | |||
| Rhodamine 123b | Pgp | 2.8±0.2 | 4.5±0.3 | 1.6 (*) |
| Ziduvidinb | MRP | 16.5±1.8 | 31.1±9.1 | 2.0 (*) |
| Doxorubicinb | Pgp, MRP1 | 13.2±0.2 | 31.5±7.3 | 2.4 (*) |
| Digoxinc | Pgp, oatp2d | 3.8±0.4 | 15.5±1.0 | 4.1 (*) |
| Ritonavirc | Pgp | 0.9±0.1 | 6.5±0.6 | 7.7 (*) |
| Taxolb | Pgp | 1.5±0.1 | 16.5±2.1 | 11.2 (*) |
| Vinblastinec | Pgp, MRP1 | 0.6±0.1 | 12.2±2.0 | 19.0 (*) |
All together Pluronic® block copolymers exhibit double punch effect in BMVEC-first, by inhibiting Pgp and second by depleting energy, which combined results in shut down of the Pgp efflux system (Fig. 4). However, these effects are transient-initial Pgp activity and ATP levels were restored after removal of the block copolymer [304]. Furthermore, even during peak depletion of ATP tight junctions in BMVEC monolayers were not compromised [215,300]. Moreover, Pluronic® had little if any effect on other transport systems in BBB, such as glucose transporter (GLUT1), monocarboxylate transporter (MCT1) and amino acid transporters (LAT1, CAT1, and SAT1) [310,311]. Histochemical examination of tissue sections from Pluronic®-treated animals revealed no pathological changes in brain capillaries [310]. Importantly, no cerebral toxicity of any kind was observed in human Phase I and Phase II trials of SP1049C, a Pluronic®-based formulation of Doxorubicin to treat MDR tumors [145,149,312]. All together, it is likely, that this formulation, already validated in human trials, can be adopted to enhance CNS drug delivery.
Fig. 4.
A scheme illustrating mechanism of Pluronic® action in BBB: (A) inhibiting PgpATPase function in cell plasma membrane; (B) inhibiting respiration in mitochondria resulting in ATP depletion. Both effects combined result in (C) inhibition of the Pgp drug efflux system and (D) transport of the drug to the brain [304].
Several combinations of CNS drugs with Pluronic® block copolymer were evaluated in animal models. For example, Davis et al. have shown that Pluronic® P85 enhances opioid peptide analgesia [313]. Two opioid peptides, [D-Pen(2),D-Pen(5)]-enkephalin (DPDPE) and biphalin, were examined, with morphine as a non-peptide control. Pluronic® P85 co-administration with DPDPE and biphalin showed increased analgesia with both 0.01% and 1.0% Pluronic® P85. Morphine showed increased analgesia with 0.01% Pluronic® P85 only. This increase in analgesia was due to both an increase in peak effect, as well as a prolongation of the effect. All three analgesic compounds were likely to have increases in circulation time attributable to Pluronic® P85 co-administration as a major contributor to the enhanced analgesia. DPDPE and morphine further exhibited an enhanced uptake in bovine BMVEC in vitro indicative of Pgp (and possibly MRP) inhibition. In another study, ability of a Pluronic® P85 to increase efficacy of anti-retroviral therapy (ART) was evaluated using a severe combined immunodeficiency (SCID) mouse model of HIV-1 encephalitis (HIVE) [314]. The SCID mice inoculated with HIV-1 infected human monocyte-derived macrophages into the basal ganglia were treated with Pluronic® P85 and ART (zidovudine, lamivudine and nelfinavir) combination, or Pluronic® P85 and ART alone. Pluronic® P85 alone and combined ART–Pluronic® P85 groups showed the most significant reductions in percentage of HIV-1 p24 expressing MDM (8–22% of control) that were superior to the ART alone group (38% of control). The findings suggest major anti-retroviral effects of Pluronic® P85 and enhanced in vivo efficacy of anti-retroviral drugs when combined with the block copolymer.
8. Chemical modification of proteins for CNS delivery
CNS delivery of therapeutic proteins is greatly hampered by BBB [315]. Several attempts to modify proteins to increase BBB permeability were described. Protein conjugations with wheatgerm agglutinin [95,96] or cationic moieties (“cationization”) [316–318] were shown to enhance CNS delivery of these proteins through adsorptive endocytosis. However, toxicity and antigenicity of such modified proteins restricts their medical use [319]. Alternatively, protein conjugates with antibodies to insulin or transferrin receptors were also considered [319–322]. For example, basic fibroblast growth factor and brain-derived neurotrophic factor each were conjugated with OX26 antibody, resulting in an increased entry of these proteins to the brain and an increased neuroprotective effects in cerebral trauma models [323–325].
One significant technology uses protein-transduction domains (PTDs) for cellular delivery of polypeptides, polynucleotides and even nanoparticles [326,327]. Such PTDs are derived from HIV-1 transcriptional activator Tat protein, herpes-simplex-virus-1 (HSV) DNA-binding protein VP22, Drosophila Antennapedia (Antp) homeotic transcription factor as well as some other proteins. The PTDs can be (i) introduced into a protein (or any other compound) by chemical conjugation, (ii) genetically fused to the protein cDNA and then expressed in the host mammalian cells via transfection or (iii) produced in large amounts in bacteria. As a result of modifications with PTDs many proteins acquire ability to rapidly cross biological membranes and enter cells [328,329]. Until now mechanism of PTD transduction remains unclear [327]. It is possible that different PTDs exploit different routes of entry into cells. Except for high content of cationic aminoacids, Lys and Arg, there is little if any structural similarity between different PTDs. Tat transduction is critically dependent on the presence of the basic residues [330], and may involve binding of a cationic peptide with heparin sulfate proteoglycans at the cell surface [331], followed by internalization via lipid-raft dependent macropinocytosis [332]. Notably, the delivery process with PTD is stringent and may result in inactivation or denaturing of some PTD fusion proteins [326].
Tat is likely to play a role in development of neuroAIDS [333–337]. It is released from HIV-1 infected cells and has various effects on different cells in the brain including activating microglia and inducing oxidative stress in endothelial cells. All together it increases permeability of BBB and facilitates entry of HIV-1 into the CNS. Furthermore, circulating Tat peptide alone crosses the BBB by a non-saturable mechanism with a unidirectional influx rate of 0.490 microl/g/min and enters CNS almost as fast as many centrally active proteins [338]. It can also carry various compounds to the brain. For example, Tat-conjugated CdSratioMn/ZnS quantum dots (Qdots), intra-arterially delivered to a rat labeled brain tissue within a few minutes [339]. Histological data clearly showed that Tat-conjugated Qdots migrated beyond endothelial cells and reached the brain parenchyma. Several Tat fusion proteins were evaluated for treatment of neurodegenerative disorders [340]. In particular, intravenous delivery of Tat peptide linked with anti-apoptotic factor Bcl-XL and glial cell line-derived neurotrophic factor (GDNF) resulted in a rapid transduction of the brain tissue [341,342]. When administered after focal cerebral ischemia, intravenous Tat-Bcl-XL and Tat-GDNF significantly reduced brain injury, both when applied after severe and mild ischemic insults. In another study Tat-GDNF fusion protein was evaluated in a subchronic scheme of 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP) model for PD [343]. Although the fusion protein did indeed reach the dopaminergic neurons the in vivo application of Tat-GDNF did not provide neuroprotection of dopaminergic neurons. However, a fusion protein containing tyrosine hydroxylase (TH) was therapeutically effective on 6-hydroxydopamine (6-OHDA)-induced PD model rats [344]. Further studies evaluated Tat-PTD fused to cystatin B in therapy of Unverricht–Lundborg epilepsy [345], BH4 domain of Bcl-XL to counteract Abeta toxicity on capillary endothelium [346] and glucocerebrosidase in Gaucher disease [347]. All together the PTD protein modification technology has attracted considerable attention in CNS drug delivery. However, biological activity of PTDs, including potential immunogenecity and long-term side effects can impose considerable limitations on development of therapeutic modalities for the treatment of neurodegenerative disorders [340].
A different approach to CNS delivery of proteins, involves point modification of proteins with a small number of fatty acid residues (e.g. stearate or palmitate) [348,349]. As a result of such modification, protein molecule remains water-soluble but also acquires hydrophobic anchors that can target even very hydrophilic proteins to cell surfaces and increase cell uptake [130,349–356]. Over a dozen water-soluble polypeptides (enzymes, antibodies, toxins, cytokines) were modified by this method [130,348,351,357–360]. Such modification of protein does not inhibit its specific activity. To the contrary, in selected cases when protein acts through cell surface receptor fatty acylation can result in drastic enhancement of its activity, likely due to protein concentration at a cell membrane [351,361]. Furthermore, insulin modified with a palmitic acid residue produced a prolonged hypoglycemic effect and was shown to be less immunoreactive compared to native insulin [350].
The relevance of this technology to CNS delivery was first demonstrated by Chekhonin et al. [358,362]. Stearoylation of Fab fragments of antibodies against GFAP and brain specific α2-glycoprotein increased its brain accumulation in a rat. Furthermore, a neuroleptic drug conjugated with stearoylated Fab fragments was more potent compared to the free drug. Notably, stearoylated Fab fragments of non-specific immunoglobulins did not accumulate in brain but instead accumulated in liver [358]. It was not clear at that time whether proteins actually crossed BBB or remained associated with luminal surface of brain capillaries. Subsequent studies demonstrated that stearoylation of ribonuclease A (ca. 13.6 kDa) [355] or horseradish peroxidase (HRP) (ca. 40 kDa) [363] greatly increased passage of these proteins across in vitro BBB. Of three fatty acid derivatives-myristic, palmitic and stearic, the latter was the most active [355]. Furthermore, stearoylation of HRP improved its penetration to brain in vivo by about 2.4-fold but also increased its volume distribution suggesting peripheral binding [363]. Transport of stearoylated HRP across the brain capillaries was validated by capillary depletion method. A possible mechanism for entry of fatty acylated proteins to brain is adsorptive endocytosis in BBB.
Another promising approach to CNS delivery is protein conjugation with Pluronic® block copolymers [363]. In particular, HRP modified with Pluronic® P85 and L121 displayed increased BBB permeability compared to native HRP. Best results were achieved when the protein and Pluronic® were linked via cleavable disulfide links. Such modification also enhanced translocation of HRP into BMVEC and led to accumulation of this protein in cytoplasm, nuclei, and other cellular organelles. This result was remarkable since unmodified HRP is impermeable and remains sequestered in endocytic vesicles after its fluid phase endocytosis. Furthermore, in vivo studies demonstrated that rates of modified HRP entry into brain increased by ca. 4-times compared to unmodified protein. Overall, modification of HRP resulted in almost two-fold increase in its brain accumulation. All together, this technology is promising for improving delivery of protein-based diagnostic and therapeutic agents to the brain.
9. Conclusion
Tremendous efforts in the last several decades have resulted in numerous inventions to improve CNS drug delivery. Many of the systems have significant potential for clinical applications. Nonetheless, the wide variety of strategies reflects the inherent difficulty in therapeutic and imaging agent transport across the BBB. In fact, the effective combination of several approaches, such as encapsulation of drugs into nanoparticles conjugated with vector moieties or using micelles of Pluronic block copolymers along with Pluronic “unimers” for drug efflux transporter inhibition in brain capillaries, may yield promising outcomes. Recently, the abilities to package a variety of drugs in cells to affect neuroregeneration, anti-inflammatory activities, or prevent microbial infections within the CNS has received significant attention. All together these works lay an important foundation for future studies into improving pharmacokinetics, reducing system drug toxicity and enabling earlier diagnosis of human disease. With the threat of significant increases in the prevalence and incidence of human neurodegenerative disorders, these advances cannot come soon enough.
Acknowledgments
We thank Dr. Elena Batrakova and Dr. Huanyu Dou for providing valuable assistance in research and analysis of literature in this manuscript and Dr. Michael Boska, Zagit Gaimalov and Robin Taylor for help with the figure illustrations. This work was supported by the National Institutes of Health grants NS36229, NS051335, CA89225, and CA116591 (to AVK) and 2R37 NS36126, P01 NS31492, P01 NS43985, U54 NS43011-01, 2 R01 NS034239, P20 RR15635 (to HEG), National Science Foundation DMR 0513699 (to AVK) and the Francine and Louis Blumkin Foundation and the Community Pride Neuroscience Initiative (to HEG).
Abbreviations
- Aβ
β-amyloid
- AD
Alzheimer’s disease
- ALS
amyotrophic lateral sclerosis
- ART
antiretroviral therapy
- BBB
blood–brain barrier
- BCB
blood–CSF barrier
- BCRP
breast cancer resistance protein
- BMM
bone marrow derived macrophages
- BMVEC
brain microvessel endothelial cells
- CMC
critical micelle concentration
- CNS
central nervous system
- CSF
cerebrospinal fluid
- CT
computed tomography
- DPDPE
D-Pen(2), D-Pen(5)]-enkephalin
- DTI
diffusion tensor imaging
- EAE
experimental autoimmune encephalomyelitis
- EAAT1-3
excitatory amino acid transporters 1–3
- EPR
permeability and retention
- HAD
HIV-1-associated dementia
- HIV-1
human immunodeficiency virus type 1
- HIVE
HIV-1 encephalitis
- HSV
Herpes-simplex-virus-1
- IDV
Indinavir
- GDNF
glial cell line-derived neurotrophic factor
- GFAP
glial fibrillary acidic protein
- LSD
lysosomal storage disorders
- MDR
multi-drug resistance
- MOAT
multi-specific organic anion transporter
- MP
mononuclear phagocytes
- MPTP
1-methyl-4-phenyl-1, 2, 3, 6-tetrahydropyridine
- MRI
magnetic resonance imaging
- MRP
multi-drug resistance protein
- MRS
magnetic resonance spectroscopy
- MRSI
magnetic resonance spectroscopic imaging
- MS
multiple sclerosis
- NAA
N-acetylaspartate
- Oatp2
organic anion transporting polypeptide subtype 2
- 6-OHDA
6-hydroxydopamine
- PD
Parkinson’s disease
- PEG
polyethylene glycol
- PET
positron emission tomography
- Pgp
P-glycoprotein
- PLGA
poly(D, L, lactide-co-glycolide)
- Pluronic®
poly(ethylene glycol)-b-poly(ethylene glycol)-b-poly(ethylene glycol)
- PTD
protein-transduction domain
- RES
reticuloendothelial system
- Qdots
quantum dots
- SCID
severe combined immunodeficiency (mouse)
- SNpc
substantia nigra pars compacta
- SPECT
single photon emission computed tomography
- TH
tyrosine hydroxylase
Footnotes
This article was published in an Elsevier journal. The attached copy is furnished to the author for non-commercial research and education use, including for instruction at the author’s institution, sharing with colleagues and providing to institution administration.
Other uses, including reproduction and distribution, or selling or licensing copies, or posting to personal, institutional or third party websites are prohibited.
In most cases authors are permitted to post their version of the article (e.g. in Word or Tex form) to their personal website or institutional repository. Authors requiring further information regarding Elsevier’s archiving and manuscript policies are encouraged to visit:http://www.elsevier.com/copyright
References
- 1.Schrag A, Quinn NP, Ben-Shlomo Y. Heterogeneity of Parkinson’s disease. J Neurol Neurosurg Psychiatry. 2006;77:275–6. [PMC free article] [PubMed] [Google Scholar]
- 2.Kantarci O, Wingerchuk D. Epidemiology and natural history of multiple sclerosis: new insights. Curr Opin Neurol. 2006;19:248–54. doi: 10.1097/01.wco.0000227033.47458.82. [DOI] [PubMed] [Google Scholar]
- 3.Flachenecker P. Epidemiology of neuroimmunological diseases. J Neurol. 2006;253:v2–8. doi: 10.1007/s00415-006-5001-3. [DOI] [PubMed] [Google Scholar]
- 4.Valcour V, Paul R. HIV infection and dementia in older adults. Clin Infect Dis. 2006;42:1449–54. doi: 10.1086/503565. [DOI] [PubMed] [Google Scholar]
- 5.McArthur JC. HIV dementia: an evolving disease. J Neuroimmunol. 2004;157:3–10. doi: 10.1016/j.jneuroim.2004.08.042. [DOI] [PubMed] [Google Scholar]
- 6.Mayeux R. Epidemiology of neurodegeneration. Annu Rev Neurosci. 2003;26:81–104. doi: 10.1146/annurev.neuro.26.043002.094919. [DOI] [PubMed] [Google Scholar]
- 7.Liu B, Hong JS. Role of microglia in inflammation-mediated neurodegenerative diseases: mechanisms and strategies for therapeutic intervention. J Pharmacol Exp Ther. 2003;304:1–7. doi: 10.1124/jpet.102.035048. [DOI] [PubMed] [Google Scholar]
- 8.Corti O, et al. Parkinson’s disease: from causes to mechanisms. C R Biol. 2005;328:131–42. doi: 10.1016/j.crvi.2004.10.009. [DOI] [PubMed] [Google Scholar]
- 9.Gendelman HE. Neural immunity: friend or foe? J Neurovirol. 2002;8:474–9. doi: 10.1080/13550280290168631. [DOI] [PubMed] [Google Scholar]
- 10.Bhanu Prakash K, et al. Identification, segmentation, and image property study of acute infarcts in diffusion-weighted images by using a probabilistic neural network and adaptive gaussian mixture model. Acad Radiol. 2006;13:1474–84. doi: 10.1016/j.acra.2006.09.045. [DOI] [PubMed] [Google Scholar]
- 11.Prinster A, et al. Grey matter loss in relapsing-remitting multiple sclerosis: a voxel-based morphometry study. Neuroimage. 2006;29:859–67. doi: 10.1016/j.neuroimage.2005.08.034. [DOI] [PubMed] [Google Scholar]
- 12.Robichaud AJ. Approaches to palliative therapies for Alzheimer’s disease. Curr Top Med Chem. 2006;6:553–68. doi: 10.2174/156802606776743039. [DOI] [PubMed] [Google Scholar]
- 13.Weissig V, et al. Liposomes and liposome-like vesicles for drug and DNA delivery to mitochondria. J Liposome Res. 2006;16:249–64. doi: 10.1080/08982100600851169. [DOI] [PubMed] [Google Scholar]
- 14.Collister KA, Albensi BC. Potential therapeutic targets in the NF-kappaB pathway for Alzheimer’s disease. Drug News Perspect. 2005;18:623–9. doi: 10.1358/dnp.2005.18.10.959576. [DOI] [PubMed] [Google Scholar]
- 15.Bruijn LI, Cudkowicz M. Therapeutic targets for amyotrophic lateral sclerosis: current treatments and prospects for more effective therapies. Expert Rev Neurother. 2006;6:417–28. doi: 10.1586/14737175.6.3.417. [DOI] [PubMed] [Google Scholar]
- 16.Tyler CM, Federoff HJ. CNS gene therapy and a nexus of complexity: systems and biology at a crossroads. Cell Transplant. 2006;15:267–73. doi: 10.3727/000000006783982007. [DOI] [PubMed] [Google Scholar]
- 17.Pardridge W. The blood–brain barrier: bottleneck in brain drug development. NeuroRx. 2005;2:3–14. doi: 10.1602/neurorx.2.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kingsley JD, et al. Nanotechnology: A focus on nanoparticles as a drug delivery system. J Neuroimmunol Pharmacol. 2006;1:340–50. doi: 10.1007/s11481-006-9032-4. [DOI] [PubMed] [Google Scholar]
- 19.Kabanov AV, Batrakova EV. New technologies for drug delivery across the blood brain barrier. Curr Pharm Des. 2004;10:1355–63. doi: 10.2174/1381612043384826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Spector R. Drug transport in the mammalian central nervous system: multiple complex systems. A critical analysis and commentary. Pharmacology. 2000;60:58–73. doi: 10.1159/000028349. [DOI] [PubMed] [Google Scholar]
- 21.Alyaudtin RN, et al. Interaction of poly(butylcyanoacrylate) nanoparticles with the blood–brain barrier in vivo and in vitro. J Drug Target. 2001;9:209–21. doi: 10.3109/10611860108997929. [DOI] [PubMed] [Google Scholar]
- 22.Pardridge W. Targeting neurotherapeutic agents through the blood–brain barrier. Arch Neurol. 2002;59:35–40. doi: 10.1001/archneur.59.1.35. [DOI] [PubMed] [Google Scholar]
- 23.Cornford EM, Cornford ME. New systems for delivery of drugs to the brain in neurological disease. Lancet Neurol. 2002;1:306–15. doi: 10.1016/s1474-4422(02)00136-9. [DOI] [PubMed] [Google Scholar]
- 24.Pardridge W. Drug and gene delivery to the brain: the vascular route. Neuron. 2002;36:555–8. doi: 10.1016/s0896-6273(02)01054-1. [DOI] [PubMed] [Google Scholar]
- 25.Misra A, et al. Drug delivery to the central nervous system: a review. J Pharm Pharm Sci. 2003;6:252–73. [PubMed] [Google Scholar]
- 26.Begley DJ. Delivery of therapeutic agents to the central nervous system: the problems and the possibilities. Pharmacol Ther. 2004;104:29–45. doi: 10.1016/j.pharmthera.2004.08.001. [DOI] [PubMed] [Google Scholar]
- 27.Kas HS. Drug delivery to brain by microparticulate systems. Adv Exp Med Biol. 2004;553:221–30. doi: 10.1007/978-0-306-48584-8_17. [DOI] [PubMed] [Google Scholar]
- 28.Banks W, Lebel C. Strategies for the delivery of leptin to the CNS. J Drug Target. 2002;10:297–308. doi: 10.1080/10611860290031895. [DOI] [PubMed] [Google Scholar]
- 29.Loscher W, Potschka H. Drug resistance in brain diseases and the role of drug efflux transporters. Nat Rev Neurosci. 2005;6:591–602. doi: 10.1038/nrn1728. [DOI] [PubMed] [Google Scholar]
- 30.Roney C, et al. Targeted nanoparticles for drug delivery through the blood–brain barrier for Alzheimer’s disease. J Control Release. 2005;108:193–214. doi: 10.1016/j.jconrel.2005.07.024. [DOI] [PubMed] [Google Scholar]
- 31.Liu X, Chen C. Strategies to optimize brain penetration in drug discovery. Curr Opin Drug Discovery Dev. 2005;8:505–12. [PubMed] [Google Scholar]
- 32.Gaillard PJ, Visser CC, de Boer AG. Targeted delivery across the blood–brain barrier. Expert Opin Drug Deliv. 2005;2:299–309. doi: 10.1517/17425247.2.2.299. [DOI] [PubMed] [Google Scholar]
- 33.Liu G, et al. Nanoparticle and other metal chelation therapeutics in Alzheimer disease. Biochim Biophys Acta. 2005;1741:246–52. doi: 10.1016/j.bbadis.2005.06.006. [DOI] [PubMed] [Google Scholar]
- 34.Garcia-Garcia E, et al. Colloidal carriers and blood–brain barrier (BBB) translocation: a way to deliver drugs to the brain? Int J Pharm. 2005;298:274–92. doi: 10.1016/j.ijpharm.2005.03.031. [DOI] [PubMed] [Google Scholar]
- 35.Silva GA. Neuroscience nanotechnology: progress, opportunities and challenges. Nat Rev Neurosci. 2006;7:65–74. doi: 10.1038/nrn1827. [DOI] [PubMed] [Google Scholar]
- 36.Dauer W, Przedborski S. Parkinson’s disease: mechanisms and models. Neuron. 2003;39:889–909. doi: 10.1016/s0896-6273(03)00568-3. [DOI] [PubMed] [Google Scholar]
- 37.Ohira T, et al. Risk factors for ischemic stroke subtypes: the atherosclerosis risk in communities study. Stroke. 2006;37:2493–8. doi: 10.1161/01.STR.0000239694.19359.88. [DOI] [PubMed] [Google Scholar]
- 38.Zoccolella S, et al. Signs and symptoms at diagnosis of amyotrophic lateral sclerosis: a population-based study in southern Italy. Eur J Neurol. 2006;13:789–92. doi: 10.1111/j.1468-1331.2006.01384.x. [DOI] [PubMed] [Google Scholar]
- 39.Qureshi MM, et al. Analysis of factors that modify susceptibility and rate of progression in amyotrophic lateral sclerosis (ALS) Amyotroph Lateral Scler. 2006;7:173–82. doi: 10.1080/14660820600640596. [DOI] [PubMed] [Google Scholar]
- 40.Shaw PJ. Molecular and cellular pathways of neurodegeneration in motor neurone disease. J Neurol Neurosurg Psychiatry. 2005;76:1046–57. doi: 10.1136/jnnp.2004.048652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Meltzer MS, Gendelman HE. Mononuclear phagocytes as targets, tissue reservoirs, and immunoregulatory cells in human immunodeficiency virus disease. Curr Top Microbiol Immunol. 1992;181:239–63. doi: 10.1007/978-3-642-77377-8_9. [DOI] [PubMed] [Google Scholar]
- 42.Luo X, et al. Macrophage proteomic fingerprinting predicts HIV-1-associated cognitive impairment. Neurology. 2003;60:1931–7. doi: 10.1212/01.wnl.0000064396.54554.26. [DOI] [PubMed] [Google Scholar]
- 43.Zheng J, et al. HIV-1 infected and immune competent mononuclear phagocytes induce quantitative alterations in neuronal dendritic arbor: relevance for HIV-1-associated dementia. Neurotox Res. 2001;3:443–59. doi: 10.1007/BF03033203. [DOI] [PubMed] [Google Scholar]
- 44.Kadiu I, et al. Mononuclear phagocytes in the pathogenesis of neurodegenerative diseases. Neurotox Res. 2005;8:25–50. doi: 10.1007/BF03033818. [DOI] [PubMed] [Google Scholar]
- 45.Anderson E, et al. HIV-1-associated dementia: a metabolic encephalopathy perpetrated by virus-infected and immune-competent mononuclear phagocytes. J Acquired Immune Defic Syndr. 2002;31(Suppl 2):S43–54. doi: 10.1097/00126334-200210012-00004. [DOI] [PubMed] [Google Scholar]
- 46.Gendelman HE, et al. The neuropathogenesis of the AIDS dementia complex. Aids. 1997;11(Suppl A):S35–45. [PubMed] [Google Scholar]
- 47.Cotter RL, et al. Insights into the neurodegenerative process of Alzheimer’s disease: a role for mononuclear phagocyte-associated inflammation and neurotoxicity. J Leukoc Biol. 1999;65:416–27. doi: 10.1002/jlb.65.4.416. [DOI] [PubMed] [Google Scholar]
- 48.Ciborowski P, Gendelman HE. Human immunodeficiency virus-mononuclear phagocyte interactions: emerging avenues of biomarker discovery, modes of viral persistence and disease pathogenesis. Curr HIV Res. 2006;4:279–91. doi: 10.2174/157016206777709474. [DOI] [PubMed] [Google Scholar]
- 49.Lipton SA, Gendelman HE. Seminars in medicine of the Beth Israel Hospital, Boston. Dementia associated with the acquired immunodeficiency syndrome. N Engl J Med. 1995;332:934–40. doi: 10.1056/NEJM199504063321407. [DOI] [PubMed] [Google Scholar]
- 50.Gendelman HE, et al. The macrophage in the persistence and pathogenesis of HIV infection. Aids. 1989;3:475–95. doi: 10.1097/00002030-198908000-00001. [DOI] [PubMed] [Google Scholar]
- 51.Ghorpade A, et al. Mononuclear phagocyte differentiation, activation, and viral infection regulate matrix metalloproteinase expression: implications for human immunodeficiency virus type 1-associated dementia. J Virol. 2001;75:6572–83. doi: 10.1128/JVI.75.14.6572-6583.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Jiang ZG, et al. Glutamate is a mediator of neurotoxicity in secretions of activated HIV-1-infected macrophages. J Neuroimmunol. 2001;117:97–107. doi: 10.1016/s0165-5728(01)00315-0. [DOI] [PubMed] [Google Scholar]
- 53.Poluektova L, et al. Macrophage-induced inflammation affects hippocampal plasticity and neuronal development in a murine model of HIV-1 encephalitis. Glia. 2005;52:344–53. doi: 10.1002/glia.20253. [DOI] [PubMed] [Google Scholar]
- 54.Cole GM, et al. NSAID and antioxidant prevention of Alzheimer’s disease: lessons from in vitro and animal models. Ann N Y Acad Sci. 2004;1035:68–84. doi: 10.1196/annals.1332.005. [DOI] [PubMed] [Google Scholar]
- 55.Moreira PI, et al. Therapeutic options in Alzheimer’s disease. Expert Rev Neurother. 2006;6:897–910. doi: 10.1586/14737175.6.6.897. [DOI] [PubMed] [Google Scholar]
- 56.Dou H, et al. Neuroprotective strategies for HIV-1 associated dementia. Neurotox Res. 2004;6:503–21. doi: 10.1007/BF03033447. [DOI] [PubMed] [Google Scholar]
- 57.Fellgiebel A, Muller MJ, Ginsberg L. CNS manifestations of Fabry’s disease. Lancet Neurol. 2006;5:791–5. doi: 10.1016/S1474-4422(06)70548-8. [DOI] [PubMed] [Google Scholar]
- 58.Jeyakumar M, et al. Storage solutions: treating lysosomal disorders of the brain. Nat Rev Neurosci. 2005;6:713–25. doi: 10.1038/nrn1725. [DOI] [PubMed] [Google Scholar]
- 59.Neumann H. Microglia: a cellular vehicle for CNS gene therapy. J Clin Invest. 2006;116:2857–60. doi: 10.1172/JCI30230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Watson G, et al. Intrathecal administration of AAV vectors for the treatment of lysosomal storage in the brains of MPS I mice. Gene Ther. 2006;13:917–25. doi: 10.1038/sj.gt.3302735. [DOI] [PubMed] [Google Scholar]
- 61.Liu G, et al. Adeno-associated virus type 5 reduces learning deficits and restores glutamate receptor subunit levels in MPS VII mice CNS. Mol Ther. 2007;15:242–7. doi: 10.1038/sj.mt.6300016. [DOI] [PubMed] [Google Scholar]
- 62.Kim SU. Genetically engineered human neural stem cells for brain repair in neurological diseases. Brain Dev. 2007;29:193–201. doi: 10.1016/j.braindev.2006.07.012. [DOI] [PubMed] [Google Scholar]
- 63.Au WL, et al. Neuroimaging in Parkinson’s disease. J Neural Transm Suppl. 2006:241–8. [PubMed] [Google Scholar]
- 64.Mosconi L. Brain glucose metabolism in the early and specific diagnosis of Alzheimer’s disease. FDG-PET studies in MCI and AD. Eur J Nucl Med Mol Imaging. 2005;32:486–510. doi: 10.1007/s00259-005-1762-7. [DOI] [PubMed] [Google Scholar]
- 65.Boska MD, et al. Advances in neuroimaging for HIV-1 associated neurological dysfunction: clues to the diagnosis, pathogenesis and therapeutic monitoring. Curr HIV Res. 2004;2:61–78. doi: 10.2174/1570162043485095. [DOI] [PubMed] [Google Scholar]
- 66.Tucker K, Robertson KR, Lin W, Smith JK, An H, Chen Y, et al. Neuroimaging in human immunodeficiency virus infection. J Neuroimmunol. 2004;157:153–62. doi: 10.1016/j.jneuroim.2004.08.036. [DOI] [PubMed] [Google Scholar]
- 67.Dhib-Jalbut S, et al. Neurodegeneration and neuroprotection in multiple sclerosis and other neurodegenerative diseases. J Neuroimmunol. 2006;176:198–215. doi: 10.1016/j.jneuroim.2006.03.027. [DOI] [PubMed] [Google Scholar]
- 68.Bocti C, et al. Topographical patterns of lobar atrophy in frontotemporal dementia and Alzheimer’s disease. Dement Geriatr Cogn Disord. 2006;21:364–72. doi: 10.1159/000091838. [DOI] [PubMed] [Google Scholar]
- 69.Kuwabara Y. Advance of SPECT: differential diagnosis and evaluation of pathophysiology of neurodegenerative disorders. Rinsho Shinkeigaku. 2004;44:894–6. [PubMed] [Google Scholar]
- 70.Silverman DH, Alavi A. PET imaging in the assessment of normal and impaired cognitive function. Radiol Clin North Am. 2005;43:67–77. doi: 10.1016/j.rcl.2004.09.012. [DOI] [PubMed] [Google Scholar]
- 71.Wearne SL, et al. New techniques for imaging, digitization and analysis of three-dimensional neural morphology on multiple scales. Neuroscience. 2005;136:661–80. doi: 10.1016/j.neuroscience.2005.05.053. [DOI] [PubMed] [Google Scholar]
- 72.Machulda MM, et al. Comparison of memory fMRI response among normal, MCI, and Alzheimer’s patients. Neurology. 2003;61:500–6. doi: 10.1212/01.wnl.0000079052.01016.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Kantarci K, et al. 1H magnetic resonance spectroscopy, cognitive function, and apolipoprotein E genotype in normal aging, mild cognitive impairment and Alzheimer’s disease. J Int Neuropsychol Soc. 2002;8:934–42. doi: 10.1017/s1355617702870084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Burn DJ, O’Brien JT. Use of functional imaging in Parkinsonism and dementia. Mov Disord. 2003;18(Suppl 6):S88–95. doi: 10.1002/mds.10568. [DOI] [PubMed] [Google Scholar]
- 75.Khachaturian ZS. Diagnosis of Alzheimer’s disease: two-decades of progress. J Alzheimers Dis. 2006;9:409–15. doi: 10.3233/jad-2006-9s346. [DOI] [PubMed] [Google Scholar]
- 76.Thompson PM, et al. Thinning of the cerebral cortex visualized in HIV/AIDS reflects CD4+ T lymphocyte decline. Proc Natl Acad Sci USA. 2005;102:15647–52. doi: 10.1073/pnas.0502548102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Thurnher MM, et al. Diffusion-tensor MR imaging of the brain in human immunodeficiency virus-positive patients. AJNR Am J Neuroradiol. 2005;26:2275–81. [PMC free article] [PubMed] [Google Scholar]
- 78.Walker Z, Walker RW. Imaging in neurodegenerative disorders: recent studies. Curr Opin Psychiatry. 2005;18:640–6. doi: 10.1097/01.yco.0000184417.29082.ea. [DOI] [PubMed] [Google Scholar]
- 79.Lehericy S, et al. Magnetic resonance imaging of Alzheimer’s disease. Eur Radiol. 2007;17:347–62. doi: 10.1007/s00330-006-0341-z. [DOI] [PubMed] [Google Scholar]
- 80.Boska MD, et al. Quantitative 1H magnetic resonance spectroscopic imaging determines therapeutic immunization efficacy in an animal model of Parkinson’s disease. J Neurosci. 2005;25:1691–700. doi: 10.1523/JNEUROSCI.4364-04.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Block W, et al. In-vivo proton MR-spectroscopy of the human brain: assessment of N-acetylaspartate (NAA) reduction as a marker for neurodegeneration. Amino Acids. 2002;23:317–23. doi: 10.1007/s00726-001-0144-0. [DOI] [PubMed] [Google Scholar]
- 82.Ackl N, et al. Hippocampal metabolic abnormalities in mild cognitive impairment and Alzheimer’s disease. Neurosci Lett. 2005;384:23–8. doi: 10.1016/j.neulet.2005.04.035. [DOI] [PubMed] [Google Scholar]
- 83.Mayhan W. Regulation of blood–brain barrier permeability. Microcirculation. 2001;8:89–104. doi: 10.1111/j.1549-8719.2001.tb00160.x. [DOI] [PubMed] [Google Scholar]
- 84.Smith MW, Gumbleton M. Endocytosis at the blood–brain barrier: from basic understanding to drug delivery strategies. J Drug Target. 2006;14:191–214. doi: 10.1080/10611860600650086. [DOI] [PubMed] [Google Scholar]
- 85.Begley D. The blood–brain barrier: principles for targeting peptides and drugs to the central nervous system. J Pharm Pharmacol. 1996;48:136–46. doi: 10.1111/j.2042-7158.1996.tb07112.x. [DOI] [PubMed] [Google Scholar]
- 86.Tamai I, Tsuji A. Transporter-mediated permeation of drugs across the blood–brain barrier. J Pharm Sci. 2000;89:1371–88. doi: 10.1002/1520-6017(200011)89:11<1371::aid-jps1>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- 87.Fromm M. P-glycoprotein: a defense mechanism limiting oral bioavailability and CNS accumulation of drugs. Int J Clin Pharmacol Ther. 2000;38:69–74. doi: 10.5414/cpp38069. [DOI] [PubMed] [Google Scholar]
- 88.Loscher W, Potschka H. Role of drug efflux transporters in the brain for drug disposition and treatment of brain diseases. Prog Neurobiol. 2005;76:22–76. doi: 10.1016/j.pneurobio.2005.04.006. [DOI] [PubMed] [Google Scholar]
- 89.Minn A, et al. Drug metabolizing enzymes in the brain and cerebral microvessels. Brain Res Brain Res Rev. 1991;16:65–82. doi: 10.1016/0165-0173(91)90020-9. [DOI] [PubMed] [Google Scholar]
- 90.Abbott N, Romero I. Transporting therapeutics across the blood–brain barrier. Mol Med Today. 1996;2:106–13. doi: 10.1016/1357-4310(96)88720-x. [DOI] [PubMed] [Google Scholar]
- 91.Davson H, Segal MB. Physiology of the CSF and blood–brain barriers. Boca Raton: CRC Press; 1996. Special aspects of the blood–brain barrier; pp. 303–485. [Google Scholar]
- 92.Banks WA, Kastin AJ. Passage of peptides across the blood–brain barrier: pathophysiological perspectives. Life Sci. 1996;59:1923–43. doi: 10.1016/s0024-3205(96)00380-3. [DOI] [PubMed] [Google Scholar]
- 93.Banks WA, et al. Transport of insulin across the blood–brain barrier: saturability at euglycemic doses of insulin. Peptides. 1997;18:1423–9. doi: 10.1016/s0196-9781(97)00231-3. [DOI] [PubMed] [Google Scholar]
- 94.Woods SC, et al. Insulin and the blood–brain barrier. Curr Pharm Des. 2003;9:795–800. doi: 10.2174/1381612033455323. [DOI] [PubMed] [Google Scholar]
- 95.Raub TJ, Audus KL. Adsorptive endocytosis and membrane recycling by cultured primary bovine brain microvessel endothelial cell monolayers. J Cell Sci. 1990;97(Part 1):127–38. doi: 10.1242/jcs.97.1.127. [DOI] [PubMed] [Google Scholar]
- 96.Banks WA, Broadwell RD. Blood to brain and brain to blood passage of native horseradish peroxidase, wheat germ agglutinin, and albumin: pharmacokinetic and morphological assessments. J Neurochem. 1994;62:2404–19. doi: 10.1046/j.1471-4159.1994.62062404.x. [DOI] [PubMed] [Google Scholar]
- 97.Agrawal S, et al. Dystroglycan is selectively cleaved at the parenchymal basement membrane at sites of leukocyte extravasation in experimental autoimmune encephalomyelitis. J Exp Med. 2006;203:1007–19. doi: 10.1084/jem.20051342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Broadwell RD, Sofroniew MV. Serum proteins bypass the blood–brain fluid barriers for extracellular entry to the central nervous system. Exp Neurol. 1993;120:245–63. doi: 10.1006/exnr.1993.1059. [DOI] [PubMed] [Google Scholar]
- 99.Banks WA, et al. Passage of amyloid beta protein antibody across the blood–brain barrier in a mouse model of Alzheimer’s disease. Peptides. 2002;23:2223–6. doi: 10.1016/s0196-9781(02)00261-9. [DOI] [PubMed] [Google Scholar]
- 100.Kozlowski GP, Sterzl I, Nilaver G. Localization patterns for immunoglobulins and albumins in the brain suggest diverse mechanisms for their transport across the blood–brain barrier (BBB) In: Ermisch A, Landgraf R, Rühle HJ, editors. Progress in brain research. Amsterdam: Elsevier; 1992. pp. 149–54. [DOI] [PubMed] [Google Scholar]
- 101.Folkman J, Long DM. The use of silicone rubber as a carrier for prolonged drug therapy. J Surg Res. 1964;71:139–42. doi: 10.1016/s0022-4804(64)80040-8. [DOI] [PubMed] [Google Scholar]
- 102.Folkman J, Long DM, Jr, Rosenbaum R. Silicone rubber: a new diffusion property useful for general anesthesia. Science. 1966;154:148–9. doi: 10.1126/science.154.3745.148. [DOI] [PubMed] [Google Scholar]
- 103.Langer R. Drug delivery. Drugs on target. Science. 2001;293:58–9. doi: 10.1126/science.1063273. [DOI] [PubMed] [Google Scholar]
- 104.Richards Grayson AC, et al. Multi-pulse drug delivery from a resorbable polymeric microchip device. Nat Mater. 2003;2:767–72. doi: 10.1038/nmat998. [DOI] [PubMed] [Google Scholar]
- 105.Wu MP, et al. In vivo versus in vitro degradation of controlled release polymers for intracranial surgical therapy. J Biomed Mater Res. 1994;28:387–95. doi: 10.1002/jbm.820280314. [DOI] [PubMed] [Google Scholar]
- 106.Lesniak MS, Langer R, Brem H. Drug delivery to tumors of the central nervous system. Curr Neurol Neurosci Rep. 2001;1:210–6. doi: 10.1007/s11910-001-0020-z. [DOI] [PubMed] [Google Scholar]
- 107.Saltzman WM, et al. Intracranial delivery of recombinant nerve growth factor: release kinetics and protein distribution for three delivery systems. Pharm Res. 1999;16:232–40. doi: 10.1023/a:1018824324275. [DOI] [PubMed] [Google Scholar]
- 108.Stroh M, et al. Diffusion of nerve growth factor in rat striatum as determined by multiphoton microscopy. Biophys J. 2003;85:581–8. doi: 10.1016/S0006-3495(03)74502-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Siepmann J, Siepmann F, Florence AT. Local controlled drug delivery to the brain: mathematical modeling of the underlying mass transport mechanisms. Int J Pharm. 2006;314:101–19. doi: 10.1016/j.ijpharm.2005.07.027. [DOI] [PubMed] [Google Scholar]
- 110.Duncan R. The dawning era of polymer therapeutics. Nat Rev Drug Discov. 2003;2:347–60. doi: 10.1038/nrd1088. [DOI] [PubMed] [Google Scholar]
- 111.Duncan R. Polymer conjugates as anticancer nanomedicines. Nat Rev Cancer. 2006;6:688–701. doi: 10.1038/nrc1958. [DOI] [PubMed] [Google Scholar]
- 112.Gabizon A, Shmeeda H, Barenholz Y. Pharmacokinetics of pegylated liposomal doxorubicin: review of animal and human studies. Clin Pharmacokinet. 2003;42:419–36. doi: 10.2165/00003088-200342050-00002. [DOI] [PubMed] [Google Scholar]
- 113.Sharpe M, et al. Polyethylene glycol-liposomal doxorubicin: a review of its use in the management of solid and haematological malignancies and AIDS-related Kaposi’s sarcoma. Drugs. 2002;62:2089–126. doi: 10.2165/00003495-200262140-00012. [DOI] [PubMed] [Google Scholar]
- 114.Gradishar WJ. Albumin-bound paclitaxel: a next-generation taxane. Expert Opin Pharmacother. 2006;7:1041–53. doi: 10.1517/14656566.7.8.1041. [DOI] [PubMed] [Google Scholar]
- 115.Feng SS, et al. Nanoparticles of biodegradable polymers for clinical administration of paclitaxel. Curr Med Chem. 2004;11:413–24. doi: 10.2174/0929867043455909. [DOI] [PubMed] [Google Scholar]
- 116.Kakizawa Y, Kataoka K. Block copolymer micelles for delivery of gene and related compounds. Adv Drug Deliv Rev. 2002;54:203–22. doi: 10.1016/s0169-409x(02)00017-0. [DOI] [PubMed] [Google Scholar]
- 117.Kabanov A, Batrakova E, Alakhov V. Pluronic block copolymers as novel polymer therapeutics for drug and gene delivery. J Control Release. 2002;82:189–212. doi: 10.1016/s0168-3659(02)00009-3. [DOI] [PubMed] [Google Scholar]
- 118.Savic R, et al. Micellar nanocontainers distribute to defined cytoplasmic organelles. Science. 2003;300:615–8. doi: 10.1126/science.1078192. [DOI] [PubMed] [Google Scholar]
- 119.Trentin D, Hubbell J, Hall H. Non-viral gene delivery for local and controlled DNA release. J Control Release. 2005;102:263–75. doi: 10.1016/j.jconrel.2004.09.029. [DOI] [PubMed] [Google Scholar]
- 120.Missirlis D, Tirelli N, Hubbell JA. Amphiphilic hydrogel nanoparticles. Preparation, characterization, and preliminary assessment as new colloidal drug carriers. Langmuir. 2005;21:2605–13. doi: 10.1021/la047367s. [DOI] [PubMed] [Google Scholar]
- 121.Salem AK, Searson PC, Leong KW. Multifunctional nanorods for gene delivery. Nat Mater. 2003;2:668–71. doi: 10.1038/nmat974. [DOI] [PubMed] [Google Scholar]
- 122.Nayak S, Lyon LA. Soft nanotechnology with soft nanoparticles. Angew Chem Int Ed Engl. 2005;44:7686–708. doi: 10.1002/anie.200501321. [DOI] [PubMed] [Google Scholar]
- 123.Kabanov AV, et al. The neuroleptic activity of haloperidol increases after its solubilization in surfactant micelles. Micelles as microcontainers for drug targeting. FEBS Lett. 1989;258:343–5. doi: 10.1016/0014-5793(89)81689-8. [DOI] [PubMed] [Google Scholar]
- 124.Yokoyama M, et al. Characterization and anticancer activity of the micelle-forming polymeric anticancer drug adriamycin-conjugated poly(ethylene glycol)-poly(aspartic acid) block copolymer. Cancer Res. 1990;50:1693–700. [PubMed] [Google Scholar]
- 125.Kwon GS. Polymeric micelles for delivery of poorly water-soluble compounds. Crit Rev Ther Drug Carrier Syst. 2003;20:357–403. doi: 10.1615/critrevtherdrugcarriersyst.v20.i5.20. [DOI] [PubMed] [Google Scholar]
- 126.Torchilin VP. Micellar nanocarriers: pharmaceutical perspectives. Pharm Res. 2007;24:1–16. doi: 10.1007/s11095-006-9132-0. [DOI] [PubMed] [Google Scholar]
- 127.Wu GY, Wu CH. Receptor-mediated in vitro gene transformation by a soluble DNA carrier system. J Biol Chem. 1987;262:4429–32. [PubMed] [Google Scholar]
- 128.Kabanov AV, et al. Increase in the transforming activity of plasmid DNA by means of its inclusion in the interpolyelectrolytic complex with a carbon-chain cation. Dokl Biochem (Dokl Akad Nauk SSSR) 1989;306:133–6. [PubMed] [Google Scholar]
- 129.Cotten M, et al. Transferrin-polycation-mediated introduction of DNA into human leukemic cells: stimulation by agents that affect the survival of transfected DNA or modulate transferrin receptor levels. Proc Natl Acad Sci USA. 1990;87:4033–7. doi: 10.1073/pnas.87.11.4033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Slepnev V, et al. Fatty acid acylated peroxidase as a model for the study of interactions of hydrophobically-modified proteins with mammalian cells. Bioconjug Chem. 1995;6:608–15. doi: 10.1021/bc00035a016. [DOI] [PubMed] [Google Scholar]
- 131.Boussif O, et al. A versatile vector for gene and oligonucleotide transfer into cells in culture and in vivo: polyethylenimine. Proc Natl Acad Sci USA. 1995;92:7297–301. doi: 10.1073/pnas.92.16.7297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Read ML, Logan A, Seymour LW. Barriers to gene delivery using synthetic vectors. Adv Genet. 2005;53:19–46. [PubMed] [Google Scholar]
- 133.Wagner E, Culmsee C, Boeckle S. Targeting of polyplexes: toward synthetic virus vector systems. Adv Genet. 2005;53:333–54. [PubMed] [Google Scholar]
- 134.Kabanov A, Zhu J, Alakhov V. Pluronic block copolymers for gene delivery. Adv Genet. 2005;53:231–61. [PubMed] [Google Scholar]
- 135.Ogris M, Wagner E. Tumor-targeted gene transfer with DNA polyplexes. Somat Cell Mol Genet. 2002;27:85–95. doi: 10.1023/a:1022988008131. [DOI] [PubMed] [Google Scholar]
- 136.Kabanov AV, et al. Water-soluble block polycations as carriers for oligonucleotide delivery. Bioconjug Chem. 1995;6:639–43. doi: 10.1021/bc00036a001. [DOI] [PubMed] [Google Scholar]
- 137.Harada A, Kataoka K. Formation of polyion complex micelles in an aqueous milieu from a pair of oppositely-charged block copolymers with poly(ethylene glycol) segments. Macromolecules. 1995;28:5294–9. [Google Scholar]
- 138.van Nostrum CF. Polymeric micelles to deliver photosensitizers for photodynamic therapy. Adv Drug Deliv Rev. 2004;56:9–16. doi: 10.1016/j.addr.2003.07.013. [DOI] [PubMed] [Google Scholar]
- 139.Oh KT, et al. Block ionomer complexes as prospective nanocontainers for drug delivery. J Control Release. 2006;115:9–17. doi: 10.1016/j.jconrel.2006.06.030. [DOI] [PubMed] [Google Scholar]
- 140.Vinogradov S, Batrakova E, Kabanov A. Poly(ethylene glycol)-polyethyleneimine nanogel particles: novel drug delivery systems for antisense oligonucleotides. Coll Surf B Biointerfaces. 1999;16:291–304. [Google Scholar]
- 141.McAllister K, et al. Polymeric nanogels produced via inverse microemulsion polymerization as potential gene and antisense delivery agents. J Am Chem Soc. 2002;124:15198–207. doi: 10.1021/ja027759q. [DOI] [PubMed] [Google Scholar]
- 142.Vinogradov SV, Batrakova EV, Kabanov AV. Nanogels for oligonucleotide delivery to the brain. Bioconjug Chem. 2004;15:50–60. doi: 10.1021/bc034164r. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Kazakov S, et al. Ion concentration of external solution as a characteristic of micro- and nanogel ionic reservoirs. J Phys Chem B Condens Matter Mater Surf Interfaces Biophys. 2006;110:15107–16. doi: 10.1021/jp061044i. [DOI] [PubMed] [Google Scholar]
- 144.Soni S, et al. Delivery of hydrophobised 5-fluorouracil derivative to brain tissue through intravenous route using surface modified nanogels. J Drug Target. 2006;14:87–95. doi: 10.1080/10611860600635608. [DOI] [PubMed] [Google Scholar]
- 145.Danson S, et al. Phase I dose escalation and pharmacokinetic study of Pluronic polymer-bound doxorubicin (SP1049C) in patients with advanced cancer. Br J Cancer. 2004;90:2085–91. doi: 10.1038/sj.bjc.6601856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Matsumura Y, et al. Phase I clinical trial and pharmacokinetic evaluation of NK911, a micelle-encapsulated doxorubicin. Br J Cancer. 2004;91:1775–81. doi: 10.1038/sj.bjc.6602204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Kim TY, et al. Phase I and pharmacokinetic study of Genexol-PM, a cremophor-free, polymeric micelle-formulated paclitaxel, in patients with advanced malignancies. Clin Cancer Res. 2004;10:3708–16. doi: 10.1158/1078-0432.CCR-03-0655. [DOI] [PubMed] [Google Scholar]
- 148.Matsumura Y. Micelle carrier system in clinical trial. Nippon Rinsho. 2006;64:316–21. [PubMed] [Google Scholar]
- 149.Armstrong A, et al. SP1049C as first-line therapy in advanced (inoperable or metastatic) adenocarcinoma of the oesophagus: a phase II window study. Journal of Clinical Oncology; ASCO annual meeting proceedings, Part I; 2006. p. 4080. [Google Scholar]
- 150.Helms B, Meijer EW. Chemistry. Dendrimers at work. Science. 2006;313:929–30. doi: 10.1126/science.1130639. [DOI] [PubMed] [Google Scholar]
- 151.Tao L, Uhrich KE. Novel amphiphilic macromolecules and their in vitro characterization as stabilized micellar drug delivery systems. J Colloid Interface Sci. 2006;298:102–10. doi: 10.1016/j.jcis.2005.12.018. [DOI] [PubMed] [Google Scholar]
- 152.Pochan DJ, et al. Toroidal triblock copolymer assemblies. Science. 2004;306:94–7. doi: 10.1126/science.1102866. [DOI] [PubMed] [Google Scholar]
- 153.Bronich TK, et al. Polymer micelle with cross-linked ionic core. J Am Chem Soc. 2005;127:8236–7. doi: 10.1021/ja043042m. [DOI] [PubMed] [Google Scholar]
- 154.Wang F, et al. Synthesis and evaluation of a star amphiphilic block copolymer from poly(epsilon-caprolactone) and poly(ethylene glycol) as a potential drug delivery carrier. Bioconjug Chem. 2005;16:397–405. doi: 10.1021/bc049784m. [DOI] [PubMed] [Google Scholar]
- 155.O’Reilly RK, Hawker CJ, Wooley KL. Cross-linked block copolymer micelles: functional nanostructures of great potential and versatility. Chem Soc Rev. 2006;35:1068–83. doi: 10.1039/b514858h. [DOI] [PubMed] [Google Scholar]
- 156.in het Panhuis M. Vaccine delivery by carbon nanotubes. Chem Biol. 2003;10:897–8. doi: 10.1016/j.chembiol.2003.10.005. [DOI] [PubMed] [Google Scholar]
- 157.Cai D, et al. Highly efficient molecular delivery into mammalian cells using carbon nanotube spearing. Nat Methods. 2005;2:449–54. doi: 10.1038/nmeth761. [DOI] [PubMed] [Google Scholar]
- 158.Dzenis Y. Material science. Spinning continuous fibers for nanotechnology. Science. 2004;304:1917–9. doi: 10.1126/science.1099074. [DOI] [PubMed] [Google Scholar]
- 159.Chua KN, et al. Surface-aminated electrospun nanofibers enhance adhesion and expansion of human umbilical cord blood hematopoietic stem/progenitor cells. Biomaterials. 2006;27:6043–51. doi: 10.1016/j.biomaterials.2006.06.017. [DOI] [PubMed] [Google Scholar]
- 160.Brewster ME, et al. The use of polymer-based electrospun nanofibers containing amorphous drug dispersions for the delivery of poorly water-soluble pharmaceuticals. Pharmazie. 2004;59:387–91. [PubMed] [Google Scholar]
- 161.Xu C, et al. Electrospun nanofiber fabrication as synthetic extracellular matrix and its potential for vascular tissue engineering. Tissue Eng. 2004;10:1160–8. doi: 10.1089/ten.2004.10.1160. [DOI] [PubMed] [Google Scholar]
- 162.Huwyler J, Wu D, Pardridge WM. Brain drug delivery of small molecules using immunoliposomes. Proc Natl Acad Sci USA. 1996;93:14164–9. doi: 10.1073/pnas.93.24.14164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Kozubek A, et al. Liposomal drug delivery, a novel approach: PLARosomes. Acta Biochim Pol. 2000;47:639–49. [PubMed] [Google Scholar]
- 164.Voinea M, Simionescu M. Designing of ‘intelligent’ liposomes for efficient delivery of drugs. J Cell Mol Med. 2002;6:465–74. doi: 10.1111/j.1582-4934.2002.tb00450.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Gabizon A, et al. Prolonged circulation time and enhanced accumulation in malignant exudates of doxorubicin encapsulated in polyethylene-glycol coated liposomes. Cancer Res. 1994;54:987–92. [PubMed] [Google Scholar]
- 166.Papaldo P, et al. A phase II study on metastatic breast cancer patients treated with weekly vinorelbine with or without trastuzumab according to HER2 expression: changing the natural history of HER2-positive disease. Ann Oncol. 2006;17:630–6. doi: 10.1093/annonc/mdj110. [DOI] [PubMed] [Google Scholar]
- 167.Umezawa F, Eto Y. Liposome targeting to mouse brain: mannose as a recognition marker. Biochem Biophys Res Commun. 1988;153:1038–44. doi: 10.1016/s0006-291x(88)81333-0. [DOI] [PubMed] [Google Scholar]
- 168.Rousseau V, et al. Early detection of liposome brain localization in rat experimental allergic encephalomyelitis. Exp Brain Res. 1999;125:255–64. doi: 10.1007/s002210050681. [DOI] [PubMed] [Google Scholar]
- 169.Shi N, et al. Brain-specific expression of an exogenous gene after i.v. administration. Proc Natl Acad Sci USA. 2001;98:12754–9. doi: 10.1073/pnas.221450098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Mora M, et al. Design and characterization of liposomes containing long-chain N-acylPEs for brain delivery: penetration of liposomes incorporating GM1 into the rat brain. Pharm Res. 2002;19:1430–8. doi: 10.1023/a:1020440229102. [DOI] [PubMed] [Google Scholar]
- 171.Thole M, et al. Uptake of cationzied albumin coupled liposomes by cultured porcine brain microvessel endothelial cells and intact brain capillaries. J Drug Target. 2002;10:337–44. doi: 10.1080/10611860290031840. [DOI] [PubMed] [Google Scholar]
- 172.Wu D, et al. Pharmacokinetics and brain uptake of biotinylated basic fibroblast growth factor conjugated to a blood–brain barrier drug delivery system. J Drug Target. 2002;10:239–45. doi: 10.1080/10611860290022679. [DOI] [PubMed] [Google Scholar]
- 173.Zhang Y, Boado R, Pardridge W. Marked enhancement in gene expression by targeting the human insulin receptor. J Gene Med. 2003;5:157–63. doi: 10.1002/jgm.333. [DOI] [PubMed] [Google Scholar]
- 174.Schmidt J, et al. Drug targeting by long-circulating liposomal glucocorticosteroids increases therapeutic efficacy in a model of multiple sclerosis. Brain. 2003;126:1895–904. doi: 10.1093/brain/awg176. [DOI] [PubMed] [Google Scholar]
- 175.Omori N, et al. Targeting of post-ischemic cerebral endothelium in rat by liposomes bearing polyethylene glycol-coupled transferrin. Neurol Res. 2003;25:275–9. doi: 10.1179/016164103101201508. [DOI] [PubMed] [Google Scholar]
- 176.Aoki H, et al. Therapeutic efficacy of targeting chemotherapy using local hyperthermia and thermosensitive liposome: evaluation of drug distribution in a rat glioma model. Int J Hyperthermia. 2004;20:595–605. doi: 10.1080/02656730410001703186. [DOI] [PubMed] [Google Scholar]
- 177.Gosk S, et al. Targeting anti-transferrin receptor antibody (OX26) and OX26-conjugated liposomes to brain capillary endothelial cells using in situ perfusion. J Cereb Blood Flow Metab. 2004;24:1193–204. doi: 10.1097/01.WCB.0000135592.28823.47. [DOI] [PubMed] [Google Scholar]
- 178.Chekhonin VP, et al. PEGylated immunoliposomes directed against brain astrocytes. Drug Deliv. 2005;12:1–6. doi: 10.1080/10717540590889556. [DOI] [PubMed] [Google Scholar]
- 179.Pardridge WM. Tyrosine hydroxylase replacement in experimental Parkinson’s disease with transvascular gene therapy. NeuroRx. 2005;2:129–38. doi: 10.1602/neurorx.2.1.129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Pardridge WM. Vector-mediated drug delivery to the brain. Adv Drug Deliv Rev. 1999;36:299–321. doi: 10.1016/s0169-409x(98)00087-8. [DOI] [PubMed] [Google Scholar]
- 181.Pardridge WM, Eisenberg J, Yang J. Human blood–brain barrier transferrin receptor. Metabolism. 1987;36:892–5. doi: 10.1016/0026-0495(87)90099-0. [DOI] [PubMed] [Google Scholar]
- 182.Huwyler J, et al. By-passing of P-glycoprotein using immunoliposomes. J Drug Target. 2002;10:73–9. doi: 10.1080/10611860290007559. [DOI] [PubMed] [Google Scholar]
- 183.Wu D, Boado R, Pardridge W. Pharmacokinetics and blood–brain barrier transport of [3H]-biotinylated phosphorothioate oligodeoxynucleotide conjugated to a vector-mediated drug delivery system. J Pharmacol Exp Ther. 1996;276:206–11. [PubMed] [Google Scholar]
- 184.Coloma MJ, et al. Transport across the primate blood–brain barrier of a genetically engineered chimeric monoclonal antibody to the human insulin receptor. Pharm Res. 2000;17:266–74. doi: 10.1023/a:1007592720793. [DOI] [PubMed] [Google Scholar]
- 185.Moghimi S, Illum L, Davis S. Physiopathological and physicochemical considerations in targeting of colloids and drug carriers to the bone marrow. Crit Rev Ther Drug Carrier Syst. 1990;7:187–209. [PubMed] [Google Scholar]
- 186.Moghimi SM, Szebeni J. Stealth liposomes and long circulating nanoparticles: critical issues in pharmacokinetics, opsonization and protein-binding properties. Prog Lipid Res. 2003;42:463–78. doi: 10.1016/s0163-7827(03)00033-x. [DOI] [PubMed] [Google Scholar]
- 187.Gref R, et al. Biodegradable long-circulating polymeric nanospheres. Science. 1994;263:1600–3. doi: 10.1126/science.8128245. [DOI] [PubMed] [Google Scholar]
- 188.Peracchia M, et al. Pegylated nanoparticles from a novel methoxypolyethylene glycol cyanoacrylate-hexadecyl cyanoacrylate amphiphilic copolymer. Pharm Res. 1998;15:550–6. doi: 10.1023/a:1011973625803. [DOI] [PubMed] [Google Scholar]
- 189.Torchilin V. Polymer-coated long-circulating microparticulate pharmaceuticals. J Microencapsul. 1998;15:1–19. doi: 10.3109/02652049809006831. [DOI] [PubMed] [Google Scholar]
- 190.Calvo P, et al. Quantification and localization of PEGy-lated polycyanoacrylate nanoparticles in brain and spinal cord during experimental allergic encephalomyelitis in the rat. Eur J Neurosci. 2002;15:1317–26. doi: 10.1046/j.1460-9568.2002.01967.x. [DOI] [PubMed] [Google Scholar]
- 191.Lemieux P, et al. Block and graft copolymers and NanoGel copolymer networks for DNA delivery into cell. J Drug Target. 2000;8:91–105. doi: 10.3109/10611860008996855. [DOI] [PubMed] [Google Scholar]
- 192.Gupta AK, et al. Receptor-mediated targeting of magnetic nanoparticles using insulin as a surface ligand to prevent endocytosis. IEEE Trans Nanobiosci. 2003;2:255–61. doi: 10.1109/tnb.2003.820279. [DOI] [PubMed] [Google Scholar]
- 193.Kreuter J. Influence of the surface properties on nanoparticle-mediated transport of drugs to the brain. J Nanosci Nanotechnol. 2004;4:484–8. doi: 10.1166/jnn.2003.077. [DOI] [PubMed] [Google Scholar]
- 194.Cui Z, et al. Novel D-penicillamine carrying nanoparticles for metal chelation therapy in Alzheimer’s and other CNS diseases. Eur J Pharm Biopharm. 2005;59:263–72. doi: 10.1016/j.ejpb.2004.07.009. [DOI] [PubMed] [Google Scholar]
- 195.Calvo P, et al. Long-circulating PEGylated polycyanoacrylate nanoparticles as new drug carrier for brain delivery. Pharm Res. 2001;18:1157–66. doi: 10.1023/a:1010931127745. [DOI] [PubMed] [Google Scholar]
- 196.Kreuter J, et al. Direct evidence that polysorbate-80-coated poly(butylcyanoacrylate) nanoparticles deliver drugs to the CNS via specific mechanisms requiring prior binding of drug to the nanoparticles. Pharm Res. 2003;20:409–16. doi: 10.1023/a:1022604120952. [DOI] [PubMed] [Google Scholar]
- 197.Steiniger SC, et al. Chemotherapy of glioblastoma in rats using doxorubicin-loaded nanoparticles. Int J Cancer. 2004;109:759–67. doi: 10.1002/ijc.20048. [DOI] [PubMed] [Google Scholar]
- 198.Olivier JC, et al. Indirect evidence that drug brain targeting using polysorbate 80-coated polybutylcyanoacrylate nanoparticles is related to toxicity. Pharm Res. 1999;16:1836–42. doi: 10.1023/a:1018947208597. [DOI] [PubMed] [Google Scholar]
- 199.Friese A, et al. Increase of the duration of the anticonvulsive activity of a novel NMDA receptor antagonist using poly(butylcyanoacrylate) nanoparticles as a parenteral controlled release system. Eur J Pharm Biopharm. 2000;49:103–9. doi: 10.1016/s0939-6411(99)00073-9. [DOI] [PubMed] [Google Scholar]
- 200.Hyuk Im S, Jeong U, Xia Y. Polymer hollow particles with controllable holes in their surfaces. Nat Mater. 2005;4:671–5. doi: 10.1038/nmat1448. [DOI] [PubMed] [Google Scholar]
- 201.Yang C, et al. Nanoparticle-based in vivo investigation on blood–brain barrier permeability following ischemia and reperfusion. Anal Chem. 2004;76:4465–71. doi: 10.1021/ac035491v. [DOI] [PubMed] [Google Scholar]
- 202.Kreuter J. Nanoparticulate systems for brain delivery of drugs. Adv Drug Deliv Rev. 2001;47:65–81. doi: 10.1016/s0169-409x(00)00122-8. [DOI] [PubMed] [Google Scholar]
- 203.Jacobs C, Kayser O, Muller RH. Nanosuspensions as a new approach for the formulation for the poorly soluble drug tarazepide. Int J Pharm. 2000;196:161–4. doi: 10.1016/s0378-5173(99)00412-3. [DOI] [PubMed] [Google Scholar]
- 204.Rabinow BE. Nanosuspensions in drug delivery. Nat Rev Drug Discov. 2004;3:785–96. doi: 10.1038/nrd1494. [DOI] [PubMed] [Google Scholar]
- 205.Friedrich I, Muller-Goymann CC. Characterization of solidified reverse micellar solutions (SRMS) and production development of SRMS-based nanosuspensions. Eur J Pharm Biopharm. 2003;56:111–9. doi: 10.1016/s0939-6411(03)00043-2. [DOI] [PubMed] [Google Scholar]
- 206.Friedrich I, Reichl S, Muller-Goymann CC. Drug release and permeation studies of nanosuspensions based on solidified reverse micellar solutions (SRMS) Int J Pharm. 2005;305:167–75. doi: 10.1016/j.ijpharm.2005.09.007. [DOI] [PubMed] [Google Scholar]
- 207.Muller RH, Jacobs C, Kayser O. Nanosuspensions as particulate drug formulations in therapy. Rationale for development and what we can expect for the future. Adv Drug Deliv Rev. 2001;47:3–19. doi: 10.1016/s0169-409x(00)00118-6. [DOI] [PubMed] [Google Scholar]
- 208.Kataoka K, Harada A, Nagasaki Y. Block copolymer micelles for drug delivery: design, characterization and biological significance. Adv Drug Deliv Rev. 2001;47:113–31. doi: 10.1016/s0169-409x(00)00124-1. [DOI] [PubMed] [Google Scholar]
- 209.Kabanov AV, Alakhov VY. Pluronic block copolymers in drug delivery: from micellar nanocontainers to biological response modifiers. Crit Rev Ther Drug Carrier Syst. 2002;19:1–72. doi: 10.1615/critrevtherdrugcarriersyst.v19.i1.10. [DOI] [PubMed] [Google Scholar]
- 210.Torchilin VP. Targeted polymeric micelles for delivery of poorly soluble drugs. Cell Mol Life Sci. 2004;61:2549–59. doi: 10.1007/s00018-004-4153-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Allen TM, Cullis PR. Drug delivery systems: entering the mainstream. Science. 2004;303:1818–22. doi: 10.1126/science.1095833. [DOI] [PubMed] [Google Scholar]
- 212.Aliabadi HM, Lavasanifar A. Polymeric micelles for drug delivery. Expert Opin Drug Deliv. 2006;3:139–62. doi: 10.1517/17425247.3.1.139. [DOI] [PubMed] [Google Scholar]
- 213.Torchilin VP. PEG-based micelles as carriers of contrast agents for different imaging modalities. Adv Drug Deliv Rev. 2002;54:235–52. doi: 10.1016/s0169-409x(02)00019-4. [DOI] [PubMed] [Google Scholar]
- 214.Kabanov A, et al. A new class of drug carriers: micelles of poly(oxyethilene)-poly(oxupropilene) block copolymers as microcontainers for drug targeting from blood in brain. J Contr Release. 1992;22:141–58. [Google Scholar]
- 215.Batrakova E, et al. Effects of Pluronic P85 unimers and micelles on drug permeability in polarized BBMEC and Caco-2 cells. Pharm Res. 1998;15:1525–32. doi: 10.1023/a:1011942814300. [DOI] [PubMed] [Google Scholar]
- 216.Nguyen HK, et al. Evaluation of polyether-polyethyleneimine graft copolymers as gene transfer agents. Gene Ther. 2000;7:126–38. doi: 10.1038/sj.gt.3301052. [DOI] [PubMed] [Google Scholar]
- 217.Zhang GD, et al. Polyion complex micelles entrapping cationic dendrimer porphyrin: effective photosensitizer for photodynamic therapy of cancer. J Control Release. 2003;93:141–50. doi: 10.1016/j.jconrel.2003.05.002. [DOI] [PubMed] [Google Scholar]
- 218.Jaturanpinyo M, et al. Preparation of bionanoreactor based on core-shell structured polyion complex micelles entrapping trypsin in the core cross-linked with glutar-aldehyde. Bioconjug Chem. 2004;15:344–8. doi: 10.1021/bc034149m. [DOI] [PubMed] [Google Scholar]
- 219.Harada A, Kataoka K. Novel polyion complex micelles entrapping enzyme molecules in the core. 2. Characterization of the micelles prepared at nonstoichiometric mixing ratios. Langmuir. 1999;15:4208–12. [Google Scholar]
- 220.Harada A, Kataoka K. Switching by pulse electric field of the elevated enzymatic reaction in the core of polyion complex micelles. J Am Chem Soc. 2003;125:15306–7. doi: 10.1021/ja038572h. [DOI] [PubMed] [Google Scholar]
- 221.Harada A, Kataoka K. Chain length recognition: core-shell supramolecular assembly from oppositely charged block copolymers. Science. 1999;283:65–7. doi: 10.1126/science.283.5398.65. [DOI] [PubMed] [Google Scholar]
- 222.Bronich TK, et al. Soluble complexes from poly(ethylene oxide)-block-polymethacrylate anions and N-alkylpyridinium cations. Macromolecules. 1997;30:3519–25. [Google Scholar]
- 223.Bronich TK, et al. Self-assembly in mixtures of poly (ethylene oxide)-graft-poly(ethyleneimine) and alkyl sulfates. Langmuir. 1998;14:6101–6. [Google Scholar]
- 224.Bronich TK, et al. Novel drug delivery systems based on the complexes of block ionomers and surfactants of opposite charge. Colloids Surf B. 1999;16:243–51. [Google Scholar]
- 225.Bronich TK, et al. Effects of block length and structure of surfactant on self-assembly and solution behavior of block ionomer complexes. Langmuir. 2000;16:481–9. [Google Scholar]
- 226.Solomatin SV, et al. Environmentally responsive nanoparticles from block ionomer complexes: effect of pH and ionic strength. Langmuir. 2003;19:8069–76. [Google Scholar]
- 227.Solomatin SV, et al. Colloidal stability of aqueous dispersions of block ionomer complexes: effects of temperature and salt. Langmuir. 2004;20:2066–8. doi: 10.1021/la034895f. [DOI] [PubMed] [Google Scholar]
- 228.Solomatin SV, et al. Nanomaterials from ionic blockcopolymers and single-, double- and triple-tail surfactants. Langmuir. 2007;23:2838–42. doi: 10.1021/la062693o. [DOI] [PubMed] [Google Scholar]
- 229.Roy S, et al. Reduction of fibronectin expression by intravitreal administration of antisense oligonucleotides. Nat Biotechnol. 1999;17:476–9. doi: 10.1038/8654. [DOI] [PubMed] [Google Scholar]
- 230.Harada-Shiba M, et al. Polyion complex micelles as vectors in gene therapy—pharmacokinetics and in vivo gene transfer. Gene Ther. 2002;9:407–14. doi: 10.1038/sj.gt.3301665. [DOI] [PubMed] [Google Scholar]
- 231.Junghans M, et al. Cationic lipid-protamine-DNA (LPD) complexes for delivery of antisense c-myc oligonucleotides. Eur J Pharm Biopharm. 2005;60:287–94. doi: 10.1016/j.ejpb.2005.01.006. [DOI] [PubMed] [Google Scholar]
- 232.Liu H, et al. Unimolecular micelles: synthesis and characterization of amphiphilic polymer systems. J Polym Sci Part A Polym Chem. 1999;37:703. [Google Scholar]
- 233.Liu M, Kono K, Frechet JMJ. Water-soluble dendritic unimolecular micelles: their potential as drug delivery agents. J Control Release. 2000;65:121. doi: 10.1016/s0168-3659(99)00245-x. [DOI] [PubMed] [Google Scholar]
- 234.Iijima M, et al. Core-polymerized reactive micelles from heterotelechelic amphiphilic block copolymers. Macromolecules. 1999;32:1140. [Google Scholar]
- 235.Turner J, Wooley K. Nanoscale cage-like structures derived from polyisoprene-containing shell cross-linked nanoparticle templates. Nano Lett. 2004;4:683–8. [Google Scholar]
- 236.Ma Q, et al. Two-dimensional, shell-cross-linked nanoparticle arrays. J Am Chem Soc. 2001;123:4627–8. doi: 10.1021/ja0156542. [DOI] [PubMed] [Google Scholar]
- 237.Bontha S, Kabanov AV, Bronich TK. Polymer micelles with cross-linked ionic cores for delivery of anticancer drugs. J Control Release. 2006;114:163–74. doi: 10.1016/j.jconrel.2006.06.015. [DOI] [PubMed] [Google Scholar]
- 238.Bronich TK, et al. Template-assisted synthesis of nanogels from Pluronic-modified poly(acrylic acid) J Drug Targeting. 2006;14:357–66. doi: 10.1080/10611860600833781. [DOI] [PubMed] [Google Scholar]
- 239.Bronich TK, et al. Synthesis of vesicles on polymer template. J Am Chem Soc. 2002;124:11872–3. doi: 10.1021/ja020509p. [DOI] [PubMed] [Google Scholar]
- 240.Vinogradov SV, et al. Polyplex nanogel formulations for drug delivery of cytotoxic nucleoside analogs. J Control Release. 2005;107:143–57. doi: 10.1016/j.jconrel.2005.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Vinogradov SV, Kohli E, Zeman AD. Cross-linked polymeric nanogel formulations of 5′-triphosphates of nucleoside analogues: role of the cellular membrane in drug release. Mol Pharm. 2005;2:449–61. doi: 10.1021/mp0500364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Vinogradov SV, Bronich TK, Kabanov AV. Nanosized cationic hydrogels for drug delivery: preparation, properties and interactions with cells. Adv Drug Deliv Rev. 2002;54:135–47. doi: 10.1016/s0169-409x(01)00245-9. [DOI] [PubMed] [Google Scholar]
- 243.Che G, et al. Chemical vapor deposition based synthesis of carbon nanotubes and nanofibers using a template method. Chem Mater. 1998;10:260–7. [Google Scholar]
- 244.Guler MO, et al. Enhanced oligonucleotide binding to self-assembled nanofibers. Bioconjug Chem. 2005;16:501–3. doi: 10.1021/bc050053b. [DOI] [PubMed] [Google Scholar]
- 245.Bull SR, et al. Self-assembled peptide amphiphile nanofibers conjugated to MRI contrast agents. Nano Lett. 2005;5:1–4. doi: 10.1021/nl0484898. [DOI] [PubMed] [Google Scholar]
- 246.Muller J, et al. Respiratory toxicity of multi-wall carbon nanotubes. Toxicol Appl Pharmacol. 2005;207:221–31. doi: 10.1016/j.taap.2005.01.008. [DOI] [PubMed] [Google Scholar]
- 247.Lange H, et al. Carbon arc plasma as a source of nanotubes: emission spectroscopy and formation mechanism. J Nanosci Nanotechnol. 2003;3:51–62. doi: 10.1166/jnn.2003.191. [DOI] [PubMed] [Google Scholar]
- 248.Fong H, Chun I, Reneker D. Beaded nanofibers formed during electrospinning. Polymer. 1999;40:4585–92. [Google Scholar]
- 249.Abidian M, Martin D. Controlled release of an anti-inflammatory drug using conducting polymer nanotubes for neural prosthetic applications. MRS symposium; San Francisco. 2005. p. 1. [Google Scholar]
- 250.Haensler J, Szoka FC., Jr Polyamidoamine cascade polymers mediate efficient transfection of cells in culture. Bioconjug Chem. 1993;4:372–9. doi: 10.1021/bc00023a012. [DOI] [PubMed] [Google Scholar]
- 251.Kukowska-Latallo JF, et al. Efficient transfer of genetic material into mammalian cells using starburst polyamidoamine dendrimers. Proc Natl Acad Sci USA. 1996;93:4897–902. doi: 10.1073/pnas.93.10.4897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Nishiyama N, et al. Light-induced gene transfer from packaged DNA enveloped in a dendrimeric photosensitizer. Nat Mater. 2005;4:934–41. doi: 10.1038/nmat1524. [DOI] [PubMed] [Google Scholar]
- 253.Kobayashi H, Brechbiel MW. Nano-sized MRI contrast agents with dendrimer cores. Adv Drug Deliv Rev. 2005;57:2271–86. doi: 10.1016/j.addr.2005.09.016. [DOI] [PubMed] [Google Scholar]
- 254.Lee CC, et al. A single dose of doxorubicin-functionalized bow-tie dendrimer cures mice bearing C-26 colon carcinomas. Proc Natl Acad Sci USA. 2006;103:16649–54. doi: 10.1073/pnas.0607705103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Talanov VS, et al. Dendrimer-based nanoprobe for dual modality magnetic resonance and fluorescence imaging. Nano Lett. 2006;6:1459–63. doi: 10.1021/nl060765q. [DOI] [PubMed] [Google Scholar]
- 256.Yang W, et al. Molecular targeting and treatment of EGFRvIII-positive gliomas using boronated monoclonal antibody L8A4. Clin Cancer Res. 2006;12:3792–802. doi: 10.1158/1078-0432.CCR-06-0141. [DOI] [PubMed] [Google Scholar]
- 257.Wu G, et al. Targeted delivery of methotrexate to epidermal growth factor receptor-positive brain tumors by means of cetuximab (IMC-C225) dendrimer bioconjugates. Mol Cancer Ther. 2006;5:52–9. doi: 10.1158/1535-7163.MCT-05-0325. [DOI] [PubMed] [Google Scholar]
- 258.Kitchens KM, El-Sayed ME, Ghandehari H. Transepithelial and endothelial transport of poly (amidoamine) dendrimers. Adv Drug Deliv Rev. 2005;57:2163–76. doi: 10.1016/j.addr.2005.09.013. [DOI] [PubMed] [Google Scholar]
- 259.Daleke DL, Hong K, Papahadjopoulos D. Endocytosis of liposomes by macrophages: binding, acidification and leakage of liposomes monitored by a new fluorescence assay. Biochim Biophys Acta. 1990;1024:352–66. doi: 10.1016/0005-2736(90)90365-u. [DOI] [PubMed] [Google Scholar]
- 260.Fujiwara M, Baldeschwieler JD, Grubbs RH. Receptor-mediated endocytosis of poly(acrylic acid)-conjugated liposomes by macrophages. Biochim Biophys Acta. 1996;1278:59–67. doi: 10.1016/0005-2736(95)00183-2. [DOI] [PubMed] [Google Scholar]
- 261.Jain S, et al. RGD-anchored magnetic liposomes for monocytes/neutrophils-mediated brain targeting. Int J Pharm. 2003;261:43–55. doi: 10.1016/s0378-5173(03)00269-2. [DOI] [PubMed] [Google Scholar]
- 262.Khan MA, et al. Enhanced anticryptococcal activity of chloroquine in phosphatidylserine-containing liposomes in a murine model. J Antimicrob Chemother. 2005;55:223–8. doi: 10.1093/jac/dkh522. [DOI] [PubMed] [Google Scholar]
- 263.Perry VH, et al. Inflammation in the nervous system. Curr Opin Neurobiol. 1995;5:636–41. doi: 10.1016/0959-4388(95)80069-7. [DOI] [PubMed] [Google Scholar]
- 264.Kuby J. In: Immunology. Goldsby R, editor. New York: Freeman W.H. and Co; 1994. [Google Scholar]
- 265.Steinfeld U, et al. T lymphocytes as potential therapeutic drug carrier for cancer treatment. Int J Pharm. 2006;311:229–36. doi: 10.1016/j.ijpharm.2005.12.040. [DOI] [PubMed] [Google Scholar]
- 266.Audran R, et al. Fate of mouse macrophages radiolabelled with PKH-95 and injected intravenously. Nucl Med Biol. 1995;22:817–21. doi: 10.1016/0969-8051(95)00013-n. [DOI] [PubMed] [Google Scholar]
- 267.Carver LA, Schnitzer JE. Caveolae: mining little caves for new cancer targets. Nat Rev Cancer. 2003;3:571–81. doi: 10.1038/nrc1146. [DOI] [PubMed] [Google Scholar]
- 268.Owens DE, 3rd, Peppas NA. Opsonization, biodistribution, and pharmacokinetics of polymeric nanoparticles. Int J Pharm. 2006;307:93–102. doi: 10.1016/j.ijpharm.2005.10.010. [DOI] [PubMed] [Google Scholar]
- 269.Panyam J, et al. Rapid endolysosomal escape of poly (DL-lactide-co-glycolide) nanoparticles: implications for drug and gene delivery. Faseb J. 2002;16:1217–26. doi: 10.1096/fj.02-0088com. [DOI] [PubMed] [Google Scholar]
- 270.Manjunath K, Venkateswarlu V. Pharmacokinetics, tissue distribution and bioavailability of nitrendipine solid lipid nanoparticles after intravenous and intraduodenal administration. J Drug Target. 2006;14:632–45. doi: 10.1080/10611860600888850. [DOI] [PubMed] [Google Scholar]
- 271.Campbell RB. Tumor physiology and delivery of nano-pharmaceuticals. Anticancer Agents Med Chem. 2006;6:503–12. doi: 10.2174/187152006778699077. [DOI] [PubMed] [Google Scholar]
- 272.Paul M, et al. Physicochemical characteristics of pentamidine-loaded polymethacrylate nanoparticles: implication in the intracellular drug release in Leishmania major infected mice. J Drug Target. 1998;5:481–90. doi: 10.3109/10611869808997874. [DOI] [PubMed] [Google Scholar]
- 273.Gibbs WJ, Drew RH, Perfect JR. Liposomal amphotericin B: clinical experience and perspectives. Expert Rev Anti Infect Ther. 2005;2:167–81. doi: 10.1586/14787210.3.2.167. [DOI] [PubMed] [Google Scholar]
- 274.Wolburg H, Wolburg-Buchholz K, Engelhardt B. Diapedesis of mononuclear cells across cerebral venules during experimental autoimmune encephalomyelitis leaves tight junctions intact. Acta Neuropathol (Berlin) 2005;109:181–90. doi: 10.1007/s00401-004-0928-x. [DOI] [PubMed] [Google Scholar]
- 275.Gorantla S, et al. Quantitative magnetic resonance and SPECT imaging for macrophage tissue migration and nanoformulated drug delivery. J Leukoc Biol. 2006;80:1165–74. doi: 10.1189/jlb.0206110. [DOI] [PubMed] [Google Scholar]
- 276.Dou H, et al. Development of a macrophage-based nanoparticle platform for antiretroviral drug delivery. Blood. 2006;108:2827–35. doi: 10.1182/blood-2006-03-012534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Dou H, et al. Laboratory investigations for the morphologic, pharmacokinetic, and anti-retroviral properties of indinavir nanoparticles in human monocyte-derived macrophages. Virology. 2007;358:148–58. doi: 10.1016/j.virol.2006.08.012. [DOI] [PubMed] [Google Scholar]
- 278.Zhang X, et al. The effect of RMP-7 and its derivative on transporting evens blue liposomes into the brain. Drug Deliv. 2004;11:301–19. doi: 10.1080/10717540490494078. [DOI] [PubMed] [Google Scholar]
- 279.Pardridge W. Methodology, biology and pathology. Cambridge: Cambridge University Press; 1998. Introduction to the blood–brain barrier; p. 486. [Google Scholar]
- 280.Begley DJ. ABC transporters and the blood–brain barrier. Curr Pharm Des. 2004;10:1295–312. doi: 10.2174/1381612043384844. [DOI] [PubMed] [Google Scholar]
- 281.Tsuji A, Tamai I. Blood–brain barrier function of P-glycoprotein. Adv Drug Deliv Rev. 1997;25:287–98. [Google Scholar]
- 282.Kim RB, et al. The drug transporter P-glycoprotein limits oral absorption and brain entry of HIV-1 protease inhibitors. J Clin Invest. 1998;101:289–94. doi: 10.1172/JCI1269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Perloff MD, von Moltke LL, Greenblatt DJ. Ritonavir and dexamethasone induce expression of CYP3A and P-glycoprotein in rats. Xenobiotica. 2004;34:133–50. doi: 10.1080/00498250310001630215. [DOI] [PubMed] [Google Scholar]
- 284.Uhr M, et al. Penetration of amitriptyline, but not of fluoxetine, into brain is enhanced in mice with blood–brain barrier deficiency due to mdr1a P-glycoprotein gene disruption. Neuropsychopharmacology. 2000;22:380–7. doi: 10.1016/S0893-133X(99)00095-0. [DOI] [PubMed] [Google Scholar]
- 285.Moriki Y, et al. Involvement of P-glycoprotein in blood–brain barrier transport of pentazocine in rats using brain uptake index method. Biol Pharm Bull. 2004;27:932–5. doi: 10.1248/bpb.27.932. [DOI] [PubMed] [Google Scholar]
- 286.Potschka H, Fedrowitz M, Loscher W. P-Glycoprotein-mediated efflux of phenobarbital, lamotrigine, and felbamate at the blood–brain barrier: evidence from microdialysis experiments in rats. Neurosci Lett. 2002;327:173–6. doi: 10.1016/s0304-3940(02)00423-8. [DOI] [PubMed] [Google Scholar]
- 287.Miyama T, et al. P-glycoprotein-mediated transport of itraconazole across the blood–brain barrier. Antimicrob Agents Chemother. 1998;42:1738–44. doi: 10.1128/aac.42.7.1738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Tsuji A. P-glycoprotein-mediated efflux transport of anticancer drugs at the blood–brain barrier. Ther Drug Monit. 1998;20:588–90. doi: 10.1097/00007691-199810000-00024. [DOI] [PubMed] [Google Scholar]
- 289.Gottesman MM, Fojo T, Bates SE. Multidrug resistance in cancer: role of ATP-dependent transporters. Nat Rev Cancer. 2002;2:48–58. doi: 10.1038/nrc706. [DOI] [PubMed] [Google Scholar]
- 290.Kemper EM, et al. Increased penetration of paclitaxel into the brain by inhibition of P-Glycoprotein. Clin Cancer Res. 2003;9:2849–55. [PubMed] [Google Scholar]
- 291.Kemper EM, et al. The influence of the P-glycoprotein inhibitor zosuquidar trihydrochloride ( LY335979) on the brain penetration of paclitaxel in mice. Cancer Chemother Pharmacol. 2004;53:173–8. doi: 10.1007/s00280-003-0720-y. [DOI] [PubMed] [Google Scholar]
- 292.Woodcock DM, et al. Reversal of the multidrug resistance phenotype with cremophor EL, a common vehicle for water-insoluble vitamins and drugs. Cancer Res. 1990;50:4199–203. [PubMed] [Google Scholar]
- 293.Woodcock DM, et al. Reversal of multidrug resistance by surfactants. Br J Cancer. 1992;66:62–8. doi: 10.1038/bjc.1992.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 294.Nerurkar MM, Burton PS, Borchardt RT. The use of surfactants to enhance the permeability of peptides through Caco-2 cells by inhibition of an apically polarized efflux system. Pharm Res. 1996;13:528–34. doi: 10.1023/a:1016033702220. [DOI] [PubMed] [Google Scholar]
- 295.Buckingham LE, et al. Reversal of multi-drug resistance in vitro by fatty acid-PEG-fatty acid diesters. Int J Cancer. 1996;65:74–9. doi: 10.1002/(SICI)1097-0215(19960103)65:1<74::AID-IJC13>3.0.CO;2-I. [DOI] [PubMed] [Google Scholar]
- 296.Alakhov VY, et al. Hypersensitization of multidrug resistant human ovarian carcinoma cells by Pluronic P85 block copolymer. Bioconjug Chem. 1996;7:209–16. doi: 10.1021/bc950093n. [DOI] [PubMed] [Google Scholar]
- 297.Batrakova E, et al. Pluronic P85 increases permeability of a broad spectrum of drugs in polarized BBMEC and Caco-2 cell monolayers. Pharm Res. 1999;16:1366–72. doi: 10.1023/a:1018990706838. [DOI] [PubMed] [Google Scholar]
- 298.Kabanov AV, Batrakova EV, Miller DW. Pluronic block copolymers as modulators of drug efflux transporter activity in the blood–brain barrier. Adv Drug Deliv Rev. 2003;55:151–64. doi: 10.1016/s0169-409x(02)00176-x. [DOI] [PubMed] [Google Scholar]
- 299.Miller D, et al. Interactions of Pluronic block copolymers with brain microvessel endothelial cells: evidence of two potential pathways for drug absorption. Bioconjugate Chem. 1997;8:649–57. doi: 10.1021/bc970118d. [DOI] [PubMed] [Google Scholar]
- 300.Batrakova E, et al. Pluronic P85 enhances the delivery of digoxin to the brain: in vitro and in vivo studies. J Pharmacol Exp Ther. 2001;296:551–7. [PubMed] [Google Scholar]
- 301.Witt KA, et al. Pluronic p85 block copolymer enhances opioid peptide analgesia. J Pharmacol Exp Ther. 2002;303:760–7. doi: 10.1124/jpet.102.039545. [DOI] [PubMed] [Google Scholar]
- 302.Batrakova E, et al. Fundamental relationships between the composition of Pluronic block copolymers and their hypersensitization effect in MDR cancer cells. Pharm Res. 1999;16:1373–9. doi: 10.1023/a:1018942823676. [DOI] [PubMed] [Google Scholar]
- 303.Batrakova E, et al. Optimal structure requirements for Pluronic block copolymers in modifying P-glycoprotein drug efflux transporter activity in bovine brain microvessel endothelial cells. J Pharmacol Exp Ther. 2003;304:845–54. doi: 10.1124/jpet.102.043307. [DOI] [PubMed] [Google Scholar]
- 304.Batrakova EV, et al. Mechanism of Pluronic effect on P-glycoprotein efflux system in blood–brain barrier: contributions of energy depletion and membrane fluidization. J Pharmacol Exp Ther. 2001;299:483–93. [PubMed] [Google Scholar]
- 305.Bacso Z, et al. Raft and cytoskeleton associations of an ABC transporter: P-glycoprotein. Cytometry A. 2004;61:105–16. doi: 10.1002/cyto.a.20081. [DOI] [PubMed] [Google Scholar]
- 306.Batrakova EV, et al. Effect of Pluronic P85 on ATPase activity of drug efflux transporters. Pharm Res. 2004;21:2226–33. doi: 10.1007/s11095-004-7675-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 307.Batrakova EV, et al. Mechanism of sensitization of MDR cancer cells by Pluronic block copolymers: selective energy depletion. Br J Cancer. 2001;85:1987–97. doi: 10.1054/bjoc.2001.2165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 308.Kabanov AV, Batrakova EV, Alakhov VY. An essential relationship between ATP depletion and chemosensitizing activity of Pluronic block copolymers. J Control Release. 2003;91:75–83. doi: 10.1016/s0168-3659(03)00211-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 309.Batrakova EV, et al. Sensitization of cells overexpressing multidrug-resistant proteins by Pluronic P85. Pharm Res. 2003;20:1581–90. doi: 10.1023/a:1026179132599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 310.Batrakova EV, et al. Effects of Pluronic P85 on GLUT1 and MCT1 transporters in the blood–brain barrier. Pharm Res. 2004;21:1993–2000. doi: 10.1023/b:pham.0000048189.79606.6e. [DOI] [PubMed] [Google Scholar]
- 311.Zhang X, et al. Effect of Pluronic P85 on amino acid transporters in the blood brain barrier. Pharm Res. 2007 doi: 10.1023/b:pham.0000048189.79606.6e. in press. [DOI] [PubMed] [Google Scholar]
- 312.Valle JW, et al. A phase II, window study of SP1049C as first-line therapy in inoperable metastatic adenocarcinoma of the oesophagus. Journal of Clinical Oncology; ASCO annual meeting proceedings (post-meeting edition); 2004. p. 4195. [Google Scholar]
- 313.Witt KA, et al. Pluronic p85 block copolymer enhances opioid peptide analgesia. J Pharmacol Exp Ther. 2002;303:760–7. doi: 10.1124/jpet.102.039545. [DOI] [PubMed] [Google Scholar]
- 314.Spitzenberger TJ, et al. Novel delivery system enhances efficacy of antiretroviral therapy in animal model for HIV-1 encephalitis. J Cereb Blood Flow Metab. 2006;27:1033–42. doi: 10.1038/sj.jcbfm.9600414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 315.Lee V. Peptide and protein drug delivery. New York: Dekker; 1991. [Google Scholar]
- 316.Kumagai AK, Eisenberg JB, Pardridge WM. Absorptive-mediated endocytosis of cationized albumin and a beta-endorphin-cationized albumin chimeric peptide by isolated brain capillaries. Model system of blood–brain barrier transport. J Biol Chem. 1987;262:15214–9. [PubMed] [Google Scholar]
- 317.Triguero D, et al. Blood–brain barrier transport of cationized immunoglobulin G: enhanced delivery compared to native protein. Proc Natl Acad Sci USA. 1989;86:4761–5. doi: 10.1073/pnas.86.12.4761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 318.Triguero D, Buciak JL, Pardridge WM. Cationization of immunoglobulin G results in enhanced organ uptake of the protein after intravenous administration in rats and primate. J Pharmacol Exp Ther. 1991;258:186–92. [PubMed] [Google Scholar]
- 319.Bickel U, Yoshikawa T, Pardridge WM. Delivery of peptides and proteins through the blood–brain barrier. Adv Drug Deliv Rev. 2001;46:247–79. doi: 10.1016/s0169-409x(00)00139-3. [DOI] [PubMed] [Google Scholar]
- 320.Frank HJ, et al. Insulin binding to the blood–brain barrier in the streptozotocin diabetic rat. J Neurochem. 1986;47:405–11. doi: 10.1111/j.1471-4159.1986.tb04516.x. [DOI] [PubMed] [Google Scholar]
- 321.Duffy KR, Pardridge WM. Blood–brain barrier transcytosis of insulin in developing rabbits. Brain Res. 1987;420:32–8. doi: 10.1016/0006-8993(87)90236-8. [DOI] [PubMed] [Google Scholar]
- 322.Friden PM, et al. Anti-transferrin receptor antibody and antibody-drug conjugates cross the blood–brain barrier. Proc Natl Acad Sci USA. 1991;88:4771–5. doi: 10.1073/pnas.88.11.4771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 323.Zhang Y, Pardridge WM. Conjugation of brain-derived neurotrophic factor to a blood–brain barrier drug targeting system enables neuroprotection in regional brain ischemia following intravenous injection of the neurotrophin. Brain Res. 2001;889:49–56. doi: 10.1016/s0006-8993(00)03108-5. [DOI] [PubMed] [Google Scholar]
- 324.Zhang Y, Pardridge WM. Neuroprotection in transient focal brain ischemia after delayed intravenous administration of brain-derived neurotrophic factor conjugated to a blood–brain barrier drug targeting system. Stroke. 2001;32:1378–84. doi: 10.1161/01.str.32.6.1378. [DOI] [PubMed] [Google Scholar]
- 325.Song BW, et al. Enhanced neuroprotective effects of basic fibroblast growth factor in regional brain ischemia after conjugation to a blood–brain barrier delivery vector. J Pharmacol Exp Ther. 2002;301:605–10. doi: 10.1124/jpet.301.2.605. [DOI] [PubMed] [Google Scholar]
- 326.Schwarze SR, Hruska KA, Dowdy SF. Protein transduction: unrestricted delivery into all cells? Trends Cell Biol. 2000;10:290–5. doi: 10.1016/s0962-8924(00)01771-2. [DOI] [PubMed] [Google Scholar]
- 327.Wadia JS, Dowdy SF. Transmembrane delivery of protein and peptide drugs by TAT-mediated transduction in the treatment of cancer. Adv Drug Deliv Rev. 2005;57:579–96. doi: 10.1016/j.addr.2004.10.005. [DOI] [PubMed] [Google Scholar]
- 328.Derossi D, et al. The third helix of the Antennapedia homeodomain translocates through biological membranes. J Biol Chem. 1994;269:10444–50. [PubMed] [Google Scholar]
- 329.Vives E, Brodin P, Lebleu B. A truncated HIV-1 Tat protein basic domain rapidly translocates through the plasma membrane and accumulates in the cell nucleus. J Biol Chem. 1997;272:16010–7. doi: 10.1074/jbc.272.25.16010. [DOI] [PubMed] [Google Scholar]
- 330.Wender PA, et al. The design, synthesis, and evaluation of molecules that enable or enhance cellular uptake: peptoid molecular transporters. Proc Natl Acad Sci USA. 2000;97:13003–8. doi: 10.1073/pnas.97.24.13003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 331.Tyagi M, et al. Internalization of HIV-1 tat requires cell surface heparan sulfate proteoglycans. J Biol Chem. 2001;276:3254–61. doi: 10.1074/jbc.M006701200. [DOI] [PubMed] [Google Scholar]
- 332.Wadia JS, Stan RV, Dowdy SF. Transducible TAT-HA fusogenic peptide enhances escape of TAT-fusion proteins after lipid raft macropinocytosis. Nat Med. 2004;10:310–5. doi: 10.1038/nm996. [DOI] [PubMed] [Google Scholar]
- 333.Toborek M, et al. HIV-Tat protein induces oxidative and inflammatory pathways in brain endothelium. J Neurochem. 2003;84:169–79. doi: 10.1046/j.1471-4159.2003.01543.x. [DOI] [PubMed] [Google Scholar]
- 334.Toborek M, et al. Mechanisms of the blood–brain barrier disruption in HIV-1 infection. Cell Mol Neurobiol. 2005;25:181–99. doi: 10.1007/s10571-004-1383-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 335.Price TO, et al. HIV-1 viral proteins gp120 and Tat induce oxidative stress in brain endothelial cells. Brain Res. 2005;1045:57–63. doi: 10.1016/j.brainres.2005.03.031. [DOI] [PubMed] [Google Scholar]
- 336.D’Aversa TG, Eugenin EA, Berman JW. NeuroAIDS: contributions of the human immunodeficiency virus-1 proteins Tat and gp120 as well as CD40 to microglial activation. J Neurosci Res. 2005;81:436–46. doi: 10.1002/jnr.20486. [DOI] [PubMed] [Google Scholar]
- 337.Banks WA, Ercal N, Price TO. The blood–brain barrier in neuroAIDS. Curr HIV Res. 2006;4:259–66. doi: 10.2174/157016206777709447. [DOI] [PubMed] [Google Scholar]
- 338.Banks WA, Robinson SM, Nath A. Permeability of the blood–brain barrier to HIV-1 Tat. Exp Neurol. 2005;193:218–27. doi: 10.1016/j.expneurol.2004.11.019. [DOI] [PubMed] [Google Scholar]
- 339.Santra S, et al. Rapid and effective labeling of brain tissue using TAT-conjugated CdS:Mn/ZnS quantum dots. Chem Commun (Camb) 2005:3144–6. doi: 10.1039/b503234b. [DOI] [PubMed] [Google Scholar]
- 340.Snyder EL, Dowdy SF. Cell penetrating peptides in drug delivery. Pharm Res. 2004;21:389–93. doi: 10.1023/B:PHAM.0000019289.61978.f5. [DOI] [PubMed] [Google Scholar]
- 341.Kilic U, et al. Intravenous TAT-GDNF is protective after focal cerebral ischemia in mice. Stroke. 2003;34:1304–10. doi: 10.1161/01.STR.0000066869.45310.50. [DOI] [PubMed] [Google Scholar]
- 342.Kilic E, Kilic U, Hermann DM. TAT fusion proteins against ischemic stroke: current status and future perspectives. Front Biosci. 2006;11:1716–21. doi: 10.2741/1917. [DOI] [PubMed] [Google Scholar]
- 343.Dietz GP, et al. Application of a blood–brain-barrier-penetrating form of GDNF in a mouse model for Parkinson’s disease. Brain Res. 2006;1082:61–6. doi: 10.1016/j.brainres.2006.01.083. [DOI] [PubMed] [Google Scholar]
- 344.Wu SP, et al. A novel therapeutic approach to 6-OHDA-induced Parkinson’s disease in rats via supplementation of PTD-conjugated tyrosine hydroxylase. Biochem Biophys Res Commun. 2006;346:1–6. doi: 10.1016/j.bbrc.2006.03.247. [DOI] [PubMed] [Google Scholar]
- 345.Andrade DM, Scherer SW, Minassian BA. Protein therapy for Unverricht–Lundborg disease using cystatin B transduction by TAT-PTD. Is it that simple? Epilepsy Res. 2006;72:75–9. doi: 10.1016/j.eplepsyres.2006.07.009. [DOI] [PubMed] [Google Scholar]
- 346.Cantara S, et al. TAT-BH4 counteracts Abeta toxicity on capillary endothelium. FEBS Lett. 2007;581:702–6. doi: 10.1016/j.febslet.2007.01.037. [DOI] [PubMed] [Google Scholar]
- 347.Vaags AK, Campbell TN, Choy FY. HIV TAT variants differentially influence the production of glucocerebrosidase in Sf9 cells. Genet Mol Res. 2005;4:491–5. [PubMed] [Google Scholar]
- 348.Kabanov A, Levashov A, Martinek K. Transformation of water-soluble enzymes into membrane active form by chemical modification. Ann N Y Acad Sci. 1987;501:63–6. doi: 10.1111/j.1749-6632.1987.tb45685.x. [DOI] [PubMed] [Google Scholar]
- 349.Kabanov A, Levashov A, Alakhov V. Lipid modification of proteins and their membrane transport. Protein Eng. 1989;3:39–42. doi: 10.1093/protein/3.1.39. [DOI] [PubMed] [Google Scholar]
- 350.Hashimoto M, et al. Synthesis of palmitoyl derivatives of insulin and their biological activities. Pharm Res. 1989;6:171–6. doi: 10.1023/a:1015992828666. [DOI] [PubMed] [Google Scholar]
- 351.Alakhov V, et al. Increasing cytostatic effects of ricin A chain and Staphylococcus aureus enterotoxin A through in vitro hydrophobization with fatty acid residues. Biotechnol Appl Biochem. 1990;12:94–8. [PubMed] [Google Scholar]
- 352.Colsky A, Peacock J. Palmitate-derivatized antibodies can specifically “arm” macrophage effector cells for ADCC. J Leukoc Biol. 1991;49:1–7. doi: 10.1002/jlb.49.1.1. [DOI] [PubMed] [Google Scholar]
- 353.Melik-Nubarov NS, et al. Interaction of hydrophobized antiviral antibodies with influenza virus infected MDCK cells. Biochem Mol Biol Int. 1993;29:939–47. [PubMed] [Google Scholar]
- 354.Ekrami H, Kennedy A, Shen W. Water-soluble fatty acid derivatives as acylating agents for reversible lipidization of polypeptides. FEBS Lett. 1995;371:283–6. doi: 10.1016/0014-5793(95)00910-2. [DOI] [PubMed] [Google Scholar]
- 355.Chopineau J, et al. Monoacylation of ribonuclease A enables its transport across an in vitro model of the blood–brain barrier. J Control Release. 1998;56:231–7. doi: 10.1016/s0168-3659(98)00091-1. [DOI] [PubMed] [Google Scholar]
- 356.Kozlova N, et al. Catalytic properties and conformation of hydrophobized alpha-chymotrypsin incorporated into a bilayer lipid membrane. FEBS Lett. 1999;461:141–4. doi: 10.1016/s0014-5793(99)01449-0. [DOI] [PubMed] [Google Scholar]
- 357.Kabanov AV, et al. Fatty acid acylated antibodies against virus suppress its reproduction in cells. FEBS Lett. 1989;250:238–40. doi: 10.1016/0014-5793(89)80729-x. [DOI] [PubMed] [Google Scholar]
- 358.Chekhonin V, et al. Fatty acid acylated FAB-fragments of antibodies to neurospecific proteins as carriers for neuroleptic targeted delivery in brain. FEBS Lett. 1991;287:149–52. doi: 10.1016/0014-5793(91)80037-4. [DOI] [PubMed] [Google Scholar]
- 359.Robert S, et al. Fatty acid acylation of RNase A using reversed micelles as microreactors. Biochem Biophys Res Commun. 1993;196:447–54. doi: 10.1006/bbrc.1993.2270. [DOI] [PubMed] [Google Scholar]
- 360.Robert S, et al. Optimization of RNase A artificial hydrophobization in AOT reversed micelles. Ann N Y Acad Sci. 1995;750:121–4. doi: 10.1111/j.1749-6632.1995.tb19939.x. [DOI] [PubMed] [Google Scholar]
- 361.Kabanov AV, Alakhov VY, Chekhonin VP. Enhancement of macromolecule penetration into cells and nontraditional drug delivery systems. Sov Sci Rev Ser D Physicochem Biol. 1992;11:1–7. [Google Scholar]
- 362.Chekhonin V, et al. Transport of hydrophobized fragments of antibodies through the blood–brain barrier. Neuroreport. 1995;7:129–32. [PubMed] [Google Scholar]
- 363.Batrakova EV, et al. Polypeptide point modifications with fatty acid and amphiphilic block copolymers for enhanced brain delivery. Bioconjug Chem. 2005;16:793–802. doi: 10.1021/bc049730c. [DOI] [PMC free article] [PubMed] [Google Scholar]