Abstract
Context:
The protective equipment worn during American football has been shown to increase thermal strain; however, the perception of this increased heat has not been examined.
Objective:
To evaluate perceptual responses of American football players while wearing different uniforms during exercise in the heat and to evaluate how these responses may be used to monitor athlete safety.
Design:
Randomized controlled trial.
Setting:
Human Performance Laboratory.
Patients or Other Participants:
Ten men with more than 3 years of competitive experience as football linemen (age = 23.8 ± 1.3 years, height = 183.9 ± 1.8 cm, mass = 117.4 ± 3.5 kg, body fat = 30.1% ± 1.7%) participated.
Intervention(s):
On 3 occasions in hot, humid (33°C, 48%–49% relative humidity) environmental conditions, participants completed 10 minutes of strenuous repetitive box lifting (RBL), 10 minutes of seated rest, and up to 60 minutes of treadmill walking. At each trial, they wore a different uniform condition: control (CON) clothing comprising shorts, socks, and sneakers; partial (PART) National Football League (NFL) uniform comprising the uniform without helmet or shoulder pads; or full (FULL) NFL uniform. Exercise, meals, and hydration status were controlled.
Main Outcome Measure(s):
Rectal temperature (Tre), skin temperature (Tsk), rating of perceived exertion (RPE), thermal perception (THM), perception of thirst (TST), and perception of muscle pain (MPN) were obtained for time points matched across trials.
Results:
Nineteen of the 30 trials ended before 60 minutes of treadmill walking as a result of participant exhaustion. Mean treadmill time was longer for the CON condition (51.7 ± 13.4 minutes) than for the PART (43.1 ± 15.6 minutes; t9 = 3.092, P = .01) or the FULL (36.2 ± 13.2 minutes; t9 = 4.393, P = .002) conditions. Neck and forearm Tsk increased between the initial time point and the end of exercise in the PART (33.6 ± 0.9°C and 35.0 ± 0.6°C, respectively; F2,18 = 9.034, P < .001) and the FULL (33.4 ± 0.9°C and 35.2 ± 0.6°C, respectively; F2,18 = 21.011, P = .002) conditions. Rate of Tre rise was greater in the FULL (0.042 ± 0.010°C/min) than in the PART (0.034 ± 0.006°C/min) condition (F2,27 = 10.69, P = .04). We found a relationship at the post-RBL and final time points between RPE and THM (r = 0.75, P < .001 and r = 0.59, P < .001, respectively), RPE and TST (r = 0.76, P < .001 and r = 0.61, P < .001, respectively), and RPE and MPN (r = 0.63, P < .001 and r = 0.64, P < .001, respectively). The RPE was greater at the end of exercise in the PART (17 ± 2) and FULL (18 ± 1) conditions than in the CON (15 ± 3) condition (F2,18 = 7.403, P = .005).
Conclusions:
Although no differences in perceptual scales existed between the PART and FULL conditions, the Tsk and rate of Tre increase differed, indicating that football athletes find it difficult to perceptually rate exercise conditions as potentially dangerous hyperthermia develops. In addition, correlations between the perceptual scales further defined perceptual responses during exercise in the heat.
Keywords: rectal temperature, rating of perceived exertion, thermal perception, thirst perception, muscle pain perception
Key Points.
The addition of a uniform, with or without pads, increased the rate of rectal temperature rise, skin temperature, and rating of perceived exertion at a given workload and decreased the amount of exercise an individual could safely perform.
Although exercise time was reduced in the partial and full uniform conditions compared with the control condition, perceptual ratings did not reflect increased thermal strain, with few perceptual differences between the control condition and the partial or the full uniform conditions.
Positive correlations of rating of perceived exertion with perception of thirst, thermal perception, and perception of muscle pain may indicate that all measured perceptions may be integrated and may influence ratings of perceived exertion.
Athletes push to the physical limits of the human body in the sport of American football, especially when exercising in the heat. Between 1995 and 2001, 21 athletes died as a result of exertional heat stroke that they sustained while practicing or playing football.1 The high incidence of heat-related deaths in football is explained in part by the heat balance equation2:
where S is heat storage, M is metabolic heat production, W is external work, K is conduction, R is radiation, C is convection, and E is evaporation. In this case, heat storage is a function of the endogenously created body heat minus any work that is done plus or minus the 4 methods of heat dissipation. Factors such as convection are commonly thought to allow an athlete to dissipate heat; however, when the air moving over the athlete's skin is warmer than the skin temperature (Tsk), convection will increase heat storage. Athletes who play football typically have large body and muscle masses, which result in great metabolic heat production that must be dissipated to maintain a safe body temperature. The uniform used by football players, including the shoulder pads and helmet, hinders heat loss via all avenues (conduction, radiation, convection, and evaporation) and increases metabolic heat production because of the weight of the equipment and clothing. Although an athlete may sweat at a greater rate while wearing a uniform,3,4 a large percentage of the sweat drips off the body and, thus, does not contribute to evaporative heat loss.5 Because of their large body sizes and intense levels of effort6 and the environment (both the ambient and the microenvironment created between the skin and uniform), football players encounter a high risk of hyperthermia, which may lead to heat illness or death due to heat stroke.
Heat stress has physiologic consequences that are associated with a decrease in exercise performance and an increase in the rating of perceived exertion (RPE).7–10 Similarly, this has been observed3,4,11–14 with exercise while wearing a football uniform. The RPE also increases in hypohydrated individuals who exercise in the heat.15 However, other psychophysiologic or perceptual scales, such as perception of thirst (TST),16 thermal perception (THM),17 and perception of muscle pain (MPN),18 or the modified Environmental Symptoms Questionnaire (ESQ)19–22 have not been examined in reference to uniformed athletes exercising in the heat. Greater understanding of the perceptual responses of uniformed athletes exercising in the heat may offer coaches and athletic trainers a field-applicable method by which to evaluate the health of their players so they can challenge their athletes while minimizing the risk of heat illness or death. Therefore, the purpose of our investigation was to evaluate the perceptual responses of American football players wearing different football uniforms during exercise in a hot environment and to determine if these responses may be used to monitor athlete safety. We hypothesized that (1) the addition of shoulder pads and a helmet would inhibit body heat loss, (2) THM ratings would be different among conditions at milestone time points, (3) the perceptual difference among conditions would be pronounced, and (4) the final RPE would be correlated with THM.
METHODS
Participants
Portions of the following methods and data are also presented in a companion paper.23 Ten men (age = 23.8 ± 1.3 years, height = 183.9 ± 1.8 cm, mass = 117.4 ± 3.5 kg, body fat = 30.1% ± 1.7%) volunteered for this study. All participants had a history of at least 3 years of competitive football experience. Participants revealed any use of supplements or medications, which was reviewed by a physician, and were excluded if any substance could have affected their thermoregulation or safety. They also were excluded from participation if they reported a history of exertional heat stroke, recurring exercise-associated muscle cramps, exercise-heat intolerance, lower back or other current musculoskeletal injury, body mass of less than 104.7 kg, age outside the range of 19 to 34 years, or syncope in the presence of needles or blood. Before participation in the study, all volunteers provided written informed consent. This protocol was approved by the University of Connecticut Institutional Review Board.
Familiarization
Uniforms
Participants reported to the Human Performance Laboratory at least 3 days before their first experimental test day to be familiarized with procedures and the following 3 uniforms: control (CON), which consisted of compression shorts, athletic shorts, ankle-length socks, and sneakers; a partial football uniform (PART), which consisted of over-the-calf socks, sneakers, gloves, T-shirt, jersey, compression shorts, pants, and pads on knees and thighs; and a full football uniform (FULL), which consisted of all equipment and clothing in the PART condition plus a helmet and shoulder pads. The uniform was an official issue of the National Football League and was manufactured from heavyweight nylon and Lycra (INVISTA, Wichita, KS).
Perceptual Scales
Participants were also familiarized with several psychophysiologic scales. We used a shortened and modified version of the ESQ.19 This 16-item version was modified to make it more applicable to the sensations associated with hot environments.20,22–24 The version contained statements, such as “I feel warm” and “I have a headache,” which the participants rated from 0 (not at all) to 5 (extreme) using pen and paper. Participants completed this questionnaire once during familiarization. We also administered the RPE,10 THM,9,17 TST,16 and MPN scales before exercise, during exercise, and postexercise during the familiarization session.25
The RPE scale is based on the theory that “man reacts to the world as he perceives it, and not as it ‘really is’”10; scores range from 6 (no exertion at all) to 20 (maximal exertion). The THM instrument subjectively rates an individual's thermal sensation; it ranges from 0 (unbearably cold) to 8 (unbearably hot), with the center point corresponding to a score of 4 (comfortable). The TST measures the thirst sensations that an exercising individual experiences; it ranges from 1 (not thirsty at all) to 9 (very, very thirsty). Each participant was instructed that TST is separate from THM, and an increase in THM does not assume an increase in TST. The MPN is used to rate muscle pain encountered during exercise; it is a 13-point incremental scale ranging from 0 (no pain at all) to 10 (extremely intense pain, almost unbearable), with additional values for 0.5 and an optional point placed outside point 10 to denote unbearable pain. Participants were informed that MPN is independent of RPE.25
Familiarization Session
At the familiarization session, we recorded each participant's age, height, and mass without the uniform. To familiarize participants with the exercise protocol, they donned the FULL condition in an environmental chamber (model 2000; Minus-Eleven Inc, Malden, MA) at 23°C (73.4°F). Each participant was taught proper lifting form (ie, keeping feet close to the box, bending knees, and holding head up to limit the stress placed on the lower back). They completed 5 minutes of repetitive box lifting (RBL)26 at the experimental pace (10 lifts/min). The RBL involved lifting a 20.4-kg (45-lb) metal box with handles, walking 2.4 m, and placing it on a platform 1.32 m from the floor. An investigator (E.C.J.) slid a second identical box down a ramp from the platform to the starting position as the participant carried the first box to the platform. Another investigator (M.S.G.) provided constant pacing feedback by counting “3, 2, 1, lift” before each box lift. Participants were informed as each minute milestone passed. The participants recovered by sitting for 5 minutes, and then they performed 10 minutes of treadmill (model 356i; Precor Inc, Woodinville, WA) walking at 5.63 km/h on a 5% grade.
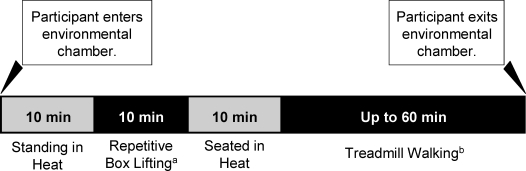
Experimental Trials
Three trials separated by at least 3 days and by no more than 7 days were completed in a randomized, counterbalanced order. Participants completed a 24-hour diet record before each trial and were instructed to consume the same foods at the same times before each trial. Upon arrival at the Human Performance Laboratory, participants consumed a small standardized breakfast (1 whole-wheat bagel, 1 oz [28 g] cream cheese, 2 medium bananas, and 250 mL of water) and were allowed 1 hour for digestion. Participants provided urine samples, which were analyzed using a refractometer (model A300CL; Spartan, Tokyo, Japan), to confirm euhydration via urine specific gravity (Usg).27 Participants were not tested if Usg was equal to or more than 1.028. Next, participants entered the environmental chamber that was maintained at 33°C (91.4°F) and 48% to 49% relative humidity and stood for 10 minutes to allow blood pressure to equilibrate. Participants completed 10 minutes of RBL, 10 minutes of seated rest, and up to 60 minutes of treadmill walking (5.63 km/h, 5% grade) (Figure 1).
Figure 1.
Protocol schematic. a Repetitive box lifting consisted of lifting a 20.4-kg metal box with handles and walking 2.4 m to place it on a platform 1.32 m from the floor at a rate of 10 lifts per minute for 10 minutes. b Treadmill walking occurred at a pace of 5.63 km/h at 5% grade for 60 minutes or until volitional fatigue occurred.
Participants completed the modified ESQ before and after completion of each experimental trial. The RPE, THM, TST, and MPN were administered before and after the RBL task, each 20 minutes throughout treadmill walking, and at cessation of exercise.
Body mass was measured with the participants wearing shorts only before RBL and at cessation of exercise, after they had exited the chamber and removed all components of the football uniform. We used a digital scale (model BWB-800S; Tanita Corporation, Tokyo, Japan), measuring to the nearest 50 g. This measurement was used to determine sweat rate.We measured rectal temperature (Tre) via a rectal thermistor (model 401; Yellow Springs Instruments, Yellow Springs, OH) inserted 10 cm past the anal sphincter, forearm and posterior neck Tsk via an infrared temperature scanner placed against the skin (Ototemp HTTS-3000; Exergen Corporation, Watertown, MA), and heart rate via telemetry (Polar Electro, Port Washington, NY) (for participant safety) before RBL and every 5 minutes until exhaustion or completion of treadmill walking. Participants were not tested if their resting Tre was equal to or more than 37.8°C. Rate of Tre rise (RTre) was calculated by first determining the net change in Tre from the initial to the final time point and then dividing that value by the total time of the trial. To calculate the estimated time to reach the Tre limit of 40°C, we used the RTre values and the mean observed initial Tre in the following equation:
where T is time to reach 40°C (minutes) and iTre is the mean initial Tre for the respective trial.
Internal uniform humidity was measured with a wand stylus (Digi-Sense Humidity Meter; Cole-Parmer Instrument Company, Vernon Hills, IL), which has a resolution of 0.1% and an accuracy of ±2% relative humidity. This humidity meter was calibrated by the manufacturer before shipment and was used soon after purchase. Uniform humidity measurements were taken by inserting the humidity probe under the back of the participant's jersey and T-shirt in the lumbar region of the lower back (being careful not to rest the probe against the skin) before RBL, at 5 minutes of RBL, after RBL, and every 20 minutes until exhaustion/completion. We administered the ESQ before RBL and immediately after exhaustion/completion. We recorded TST, THM, RPE, and MPN before RBL, after RBL, during the first minute of treadmill walking, every 20 minutes during treadmill walking, and at exhaustion/completion. After cessation of exercise, total heat exposure time was calculated by adding 20 minutes to each mean treadmill time to allow for RBL and the seated rest before treadmill walking via a digital chronograph (30-lap IRONMAN Triathlon; Timex, Middlebury, CT).
Exercise was terminated if (1) the participant demonstrated signs and symptoms of heat illness (nausea, mental disorientation, lack of coordination, dizziness); (2) the participant elected to stop volitionally because of physical exhaustion; or (3) Tre exceeded 40°C. Participants left the environmental chamber, sat quietly in a cool environment, and drank water ad libitum. Before leaving the Human Performance Laboratory, participants were advised to drink at least 150% of the lost water weight during the following 12 hours, preferably combined with a meal, to encourage their return to an euhydrated state within the next day.28,29
Statistical Analyses
All data were combined and analyzed using a 2-way repeated-measures (uniform × time) analysis of variance. Post hoc 2-tailed, paired-samples t tests were used to determine pairwise differences among uniform types and time. Initial and postexercise ESQ responses were summed to create 1 new scale score for the 16 statements for each condition. We used 2-tailed, paired-samples t tests to determine differences between the initial and postexercise new-scale variable. The internal consistency of the scale scores, as measured by the Cronbach α (α = 0.71), indicated that the variables were internally reliable in this study sample. Post hoc 2-tailed, paired-samples t tests were used to determine differences in individual statement responses. The Pearson product moment correlation with 2-tailed tests of significance was used to analyze the relationships within the perceptual scales and between the perceptual scales and the physiologic responses to exercise in the heat before and after RBL, as well as at exhaustion/completion. The final time point occurred either at physical exhaustion (10 minutes of RBL and less than 60 minutes of treadmill walking) or at completion of the exercise protocol (10 minutes of RBL and 60 minutes of treadmill walking). The α level was set at .05. We used SPSS (version 17.0; SPSS Inc, Chicago, IL) for all statistical analyses.
RESULTS
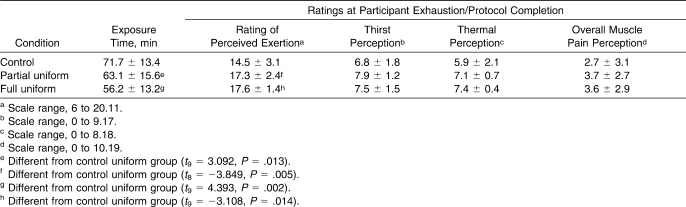
Mean exposure time and final time point RPE, TST, THM, and MPN are presented in Table 1. Mean treadmill time was 51.7 ± 13.42 minutes for the CON condition, 43.1 ± 15.61 minutes for the PART condition, and 36.2 ± 13.16 minutes for the FULL condition. Seven of 10 participants completed 60 minutes of treadmill walking in the CON condition; 3 of 10 completed 60 minutes of treadmill walking in the PART condition; and 1 of 10 completed 60 minutes of treadmill walking in the FULL condition. All participants who ceased exercise before completing the 60-minute treadmill walk cited physical exhaustion as the cause (ie, no participants reached the Tre limit of 40°C or displayed signs or symptoms of heat illness).
Table 1.
Perceptual Values (Mean ± SD) at Participant Exhaustion/Protocol Completion
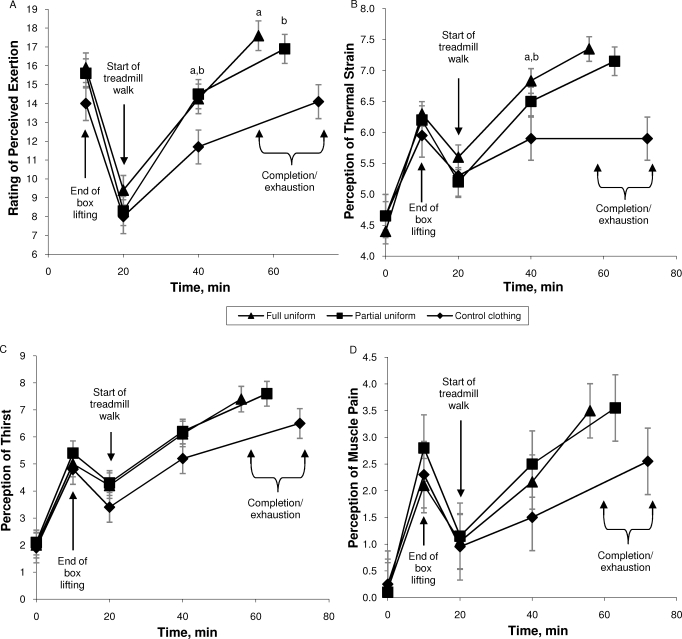
We found no difference between the PART and FULL conditions for any of the perceptual scale ratings immediately after treadmill walking. However, we found differences for RPE and THM between the CON and PART conditions and between the CON and FULL conditions (Figure 2).
Figure 2.
Perceptual scale responses (means ± SDs) over time (N = 10). A, Rating of perceived exertion; B, perception of thermal strain; C, perception of thirst; and D, perception of muscle pain. a Indicates difference between full uniform and control uniform conditions (P < .05). b Indicates difference between partial uniform and control uniform conditions (P < .05).
The Tre at initial, post-RBL, and final time points, respectively, for each condition were as follows: CON (37.2 ± 0.1°C, 37.8 ± 0.3°C, 38.8 ± 0.5°C), PART (37.2 ± 0.1°C, 37.7 ± 0.4°C, 39.2 ± 0.6°C), and FULL (37.2 ± 0.1°C, 37.7 ± 0.5°C, 39.2 ± 0.5°C). The Tre increased from the initial time point to the post-RBL time point, as well as between the post-RBL time point and the final time point, in all conditions (F2,18 = 108.012 to F2,16 = 167.434; P range, <.001). Skin temperatures at the neck and forearm sites at the initial, post-RBL, and final time points, respectively, were as follows: CON (33.0 ± 1.0°C and 33.0 ± 1.0°C, 32.8 ± 0.8°C and 33.7 ± 1.1°C, 34.5 ± 1.1°C and 34.5 ± 1.0°C), PART (33.5 ± 1.0°C and 33.6 ± 0.9°C, 33.7 ± 0.9°C and 33.7 ± 0.8°C, 35.3 ± 1.0°C and 35.0 ± 0.6°C), and FULL (33.5 ± 1.4°C and 33.4 ± 0.9°C, 34.2 ± 1.1°C and 33.7 ± 1.0°C, 35.6 ± 1.0°C and 35.2 ± 0.6°C). We found no changes in either neck or forearm Tsk in the CON condition. However, both neck and forearm Tsk in PART (F2,18 = 9.034, P < .001) and FULL (F2,18 = 21.011, P = .002) increased from the initial time point to the final time point.
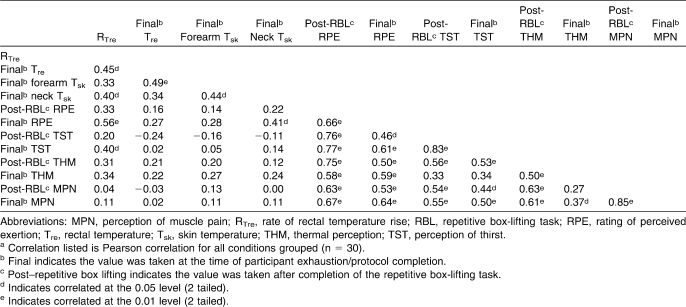
All uniform conditions were then combined at the post-RBL and final time points to analyze the relationships within the perceptual scales, as well as between the perceptual scales, and the physiologic responses to exercise in the heat. For each of the following variables, the values at the post-RBL and final times, respectively, are listed: Tre (37.7 ± 0.4°C, 39.0 ± 0.5°C), forearm Tsk (33.7 ± 0.9°C, 34.9 ± 0.9°C), neck Tsk (33.6 ± 1.1°C, 35.1 ± 1.0°C), RPE (15 ± 2, 16 ± 3), TST (5 ± 2, 7 ± 2), THM (6 ± 1, 7 ± 1), and MPN (2 ± 2, 3 ± 3). Pearson product moment correlations within these values are reported in Table 2.
Table 2.
Grouped Pearson Product Moment Correlationsa Between Physiologic and Perceptual Responses During Exercise in a 33°C Environment
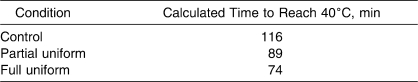
The rate of Tre rise was different among all conditions (CON = 0.026 ± 0.008, PART = 0.034 ± 0.006, FULL = 0.042 ± 0.010) (F2,27 = 10.69, P < .001). Using the experimental RTre values and the mean observed initial Tre (36.99 for CON, 36.98 for PART, and 36.89 for FULL), we calculated the estimated time to reach the limit of 40°C. We found a noteworthy reduction in the estimated time to reach a Tre of 40°C in the FULL versus the PART condition and in the PART versus the CON condition (Table 3).
Table 3.
Estimated Time Needed to Reach a Rectal Temperature of 40°C
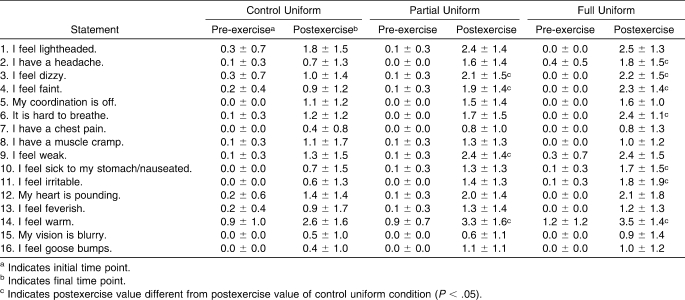
At first, the scaled score for initial and final time point ESQ responses was compiled for each condition. Initial responses were not different between the CON and the PART conditions (t9 = 0.768, P = .46), between the PART and FULL conditions (t9 = −1.048, P = .32), or between the CON and FULL conditions (t9 = 0.293, P = .78). Within each condition, the scaled score increased (from the initial to the final time point) for the CON (t9 = −2.371, P = .04), PART (t9 = −4.583, P = .001), and FULL (t9 = −5.103, P = .001) conditions. The scaled score final time point responses were greater in the PART than in the CON (t9 = −2.363, P = .04) condition and were greater in the FULL than in the CON (t9 = −2.569, P = .03) condition. However, we found no difference between the PART and FULL conditions.
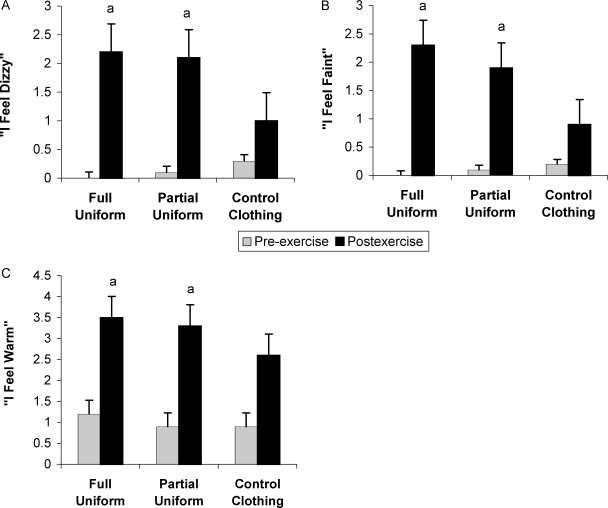
Finally, to examine which questions were most sensitive to the perceived differences while wearing a football uniform, individual t tests were performed. In 3 of 16 statements, the final time point mean responses were lower in the CON than in the PART or FULL conditions (Table 4): “I feel dizzy” (t9 = −2.905, P = .02 and t9 = −2.571, P = .03, respectively); “I feel faint” (t9 = −2.739, P = .02 and t9 = −2.806, P = .02, respectively); and “I feel warm” (t9 = −4.431, P = .002 and t9 = −5.461, P < .001, respectively) (Figure 3). The final time point mean values were lower in the CON than in the FULL condition only for 4 additional statements: “I have a headache” (t9 = −3.498, P = .007); “It is hard to breathe” (t9 = −2.882, P = .02); “I feel sick/nauseated” (t9 = −2.535, P = .03); and “I feel irritable” (t9 = −2.449, P = .04). Final time point responses to the statement “I feel weak” were greater only in the PART condition (compared with the CON [t9 = −4.714, P = .001] condition).
Table 4.
Environmental Symptoms Questionnaire Ratings (Mean ± SD) Before Exercise and Immediately Postexercise
Figure 3.
Modified Environmental Symptoms Questionnaire responses (mean ± SD) before and immediately after exercise, n = 10. A, “I feel dizzy;” B, “I feel faint;” C, “I feel warm.” a Indicates different from control uniform condition final time point value (P < .05).
Humidity between the skin and uniform for the PART and FULL conditions was similarly near maximum at the end of exercise (90.41% ± 4.43% and 89.03% ± 3.57%, respectively; t9 = −0.953, P = .37). The uniform humidity data for the PART condition, the FULL condition, and the 2 uniform conditions combined were then plotted against each participant's THM rating matched at specific times. The resulting Pearson product moment correlation coefficients for THM versus uniform humidity in the PART condition (n = 10), the FULL condition (n = 10), and combined uniform conditions (n = 20) were r = 0.475 (P = .002), r = 0.756 (P < .001), and r = 0.585 (P < .001), respectively.
DISCUSSION
The purpose of our study was to evaluate the perceptual responses of American football linemen exercising in different modes (eg, RBL and treadmill walking) in the heat while wearing 3 different clothing ensembles and to see if these responses could be used to monitor athlete safety. Previous investigators3,4,11–14 have evaluated the effects of a protective uniform on Tre, sweat rate, macronutrient use, and blood lactate levels; however, the effects of uniforms on perception have not been studied. Our main finding demonstrated no differences between the PART and FULL conditions in terms of mean exposure time, RPE, TST, THM, MPN, and most final time point ESQ responses; few perceptual differences between the CON and PART conditions and between the CON and FULL conditions; significant correlations within the perceptual scales; a significant correlation between RTre and RPE; and a difference in RTre among all conditions.
During the 30 experiments (10 per uniform condition), 19 ended before completion of 60 minutes of treadmill walking because the participants were physically exhausted. In these 19 trials, no participant reached the predetermined Tre limit of 40°C or displayed signs or symptoms of heat illness. Although the mean exposure time was lower in the FULL condition than in the PART condition, this value was not different because of the variability and range of exposure times in each trial. We attributed these differences in exposure time to the cardiovascular physical fitness and heat tolerance levels of participants.
Previous researchers have demonstrated that shoulder pads and helmets increase both the insulation11,13 and the amount of energy needed to perform exercise because of added weight and altered biomechanics.3 For example, Hitchcock et al14 found that adding shoulder pads to a football uniform increased gastrointestinal temperature at the end of exercise. We did not find a difference between uniform types for either Tre or Tsk at the end of exercise. This discrepancy may be due to differences in experimental design (ie, our exercise protocol resulted in participants ending exercise as a result of exhaustion, whereas this was not the case in the study by Hitchcock et al14). In addition, we took the Tsk readings at sites that were not covered by the uniform. Chest and thigh Tsk might have yielded a more accurate portrayal of the Tsk response to a uniform.
Because of the differences in heat exposure time and the limitations of the Tsk readings, the RTre may be a more descriptive variable of the participant's response to exercise in the heat while wearing the different uniforms. Although no final Tre differences were seen between the PART and FULL conditions, the RTre values supported the hypothesis that the addition of shoulder pads and a helmet inhibits body heat loss. Based on the RTre for each uniform, prolonged exercise resulted in a Tre of 40°C in a shorter time in the FULL condition than in the PART condition.
The similar THM ratings in the PART and FULL conditions are contrary to the research of Cotter et al,30 who reported that the head was the most sensitive part of the body and strongly influenced the perception of total-body THM. In our study, we found no change in THM when a helmet was added. This dissimilarity was not surprising given the environmental conditions and metabolic requirements of our protocol. The extreme drive for cooling via skin blood flow may be reflected by near-maximal and similar Tsk being measured throughout the protocol. Gagge et al31 reported that Tsk must differ by at least 2°C to be perceived as being different. The Tsk in our study ranged from 33.0 ± 1.0°C to 34.5 ± 1.1°C in the CON condition, from 33.5 ± 1.0°C to 35.0 ± 1.0°C in the PART condition, and from 33.4 ± 0.9°C to 35.6 ± 1.0°C in the FULL condition. Therefore, a between-conditions difference in THM ratings at milestone time points was not hypothetically anticipated.
The thermoregulatory theory of fatigue32 postulates that a critical Tre (approximately 40°C) results in voluntary exhaustion. In our study, exercise time was reduced in the PART and FULL conditions compared with the CON condition. However, THM responses were not different among conditions at exhaustion. Before reaching the Tre threshold and concurrent with exercise cessation, a participant's THM was almost maximally rated in the PART and FULL conditions and remained close to maximum until the end of exercise, despite a rising Tre.
At the end of exercise, no correlation existed between THM and either Tre or Tsk (ie, maximal perceptual scores were perceived before participants reached the critical Tre). The lack of agreement between the perceptual ratings and the physiologic responses to cessation of exercise may have been due to the high humidity inside the uniform, which decreased each participant's ability to dissipate heat, because both skin and air within the microenvironment were virtually saturated. Increased humidity within the uniform may have increased THM at the skin, resulting in elevated perceptual ratings before increased heat storage and elevated Tre. A second plausible explanation for the inability of THM to predict exercise cessation involves the difference between peripheral and deep-tissue thermosensors. Thermosensors located near the skin surface are responsible for behavioral modifications,33 which play a large role in perception of heat. Deep-tissue thermosensors are different because their input results in the body's autonomic responses to high internal body temperatures.33 Afferent impulses from both areas are relayed to the hypothalamus, are integrated, and influence efferent responses.33,34 However, in the PART and FULL conditions, the skin was insulated, except where the Tsk readings were taken. This may have resulted in high activation of skin thermosensors, which superseded the input from deep-tissue thermosensors and may have resulted in the elevated perceptual ratings that were observed before reaching a critical Tre.
The THM and MPN were positively correlated at both the post-RBL and final time points. This result may reflect the opening of specific ion channels that are associated with thermal nociception (ie, thermal pain that occurs under high levels of THM).35 Theoretically, it would be useful to have a THM scale similar to MPN, which contains a point beyond the maximal number rating. The participant then could rate perceived pain that is due to THM. We recommend combining the MPN and THM ratings and evaluating the resulting scale in future studies.
As environmental humidity increases, the ability of the body to dissipate heat via evaporation decreases as a result of the increased partial pressure of water in the air surrounding the body; this, in turn, results in greater heat storage. Therefore, an increase in environmental humidity should result in an increased THM rating. Indeed, increased microenvironmental humidity between the uniform and skin (PART and FULL conditions) correlated positively with THM. Compared with the CON condition, the FULL and PART conditions also contained an increased microenvironmental humidity between the skin and uniform. Thus, increased THM due to uniform humidity, regardless of environmental humidity, can reflect limited heat loss and, in turn, can contribute to decreased performance.
The only significant ESQ perceptual difference appeared in final time point ESQ responses. Interestingly, 2 of the 4 ratings that were higher in the FULL than in the CON condition but were not higher in the PART than in the CON condition were related to specific equipment items. When the helmet was worn (FULL condition), responses to “I have a headache” were greater relative to the CON condition. In addition, when the shoulder pads were worn, applying pressure to the chest and upper back (FULL condition), responses to “It is hard to breathe” were greater relative to the CON condition.
Finally, based on past football heat studies,7–10,14 we expected to observe a more pronounced perceptual difference among conditions, but this did not occur. However, the correlations among different perceptual scales and between the perceptual scales and physiologic responses yielded novel information. The RPE was positively correlated with TST, THM, and MPN after RBL and at exhaustion/completion. These correlations indicated that all measured perceptions may be integrated and may influence RPE ratings. Finally, although the correlation between final RPE and final Tre that was expected based on past studies7–10,14 was not present, a positive correlation between RTre and final RPE was observed.
CONCLUSIONS
Although American football uniforms, including shoulder pads and helmets, protect players from impact, they reduce heat dissipation, increasing the risk of heat illness secondary to dehydration and hyperthermia. Our study confirmed that the addition of a uniform with or without pads increases RTre, Tsk, and RPE at a given workload and decreases the amount of exercise an individual can safely perform. These findings should be considered by coaches who design practices, particularly if players are not heat acclimatized or if they are unfit in the early season, when most heat illnesses occur. Increased strain was not reflected by any of the perceptual ratings. This may be an important risk factor for hyperthermia or heat stroke, because football athletes commonly exercise 2 to 3 hours during practice sessions. Our data indicated that vigilance on the part of the coaching and athletic training staffs is imperative, because a football athlete may not be aware that he is experiencing life-threatening hyperthermia.
Our results advanced our understanding of perceptual scales. The RPE scale may not be as simple as a perceived reflection of heart rate and ventilatory rate. Other factors, such as TST, THM, and MPN, are strongly associated with RPE. In addition, great THM sensation may affect an athlete's MPN. Furthermore, our study clarified how the human body perceives, integrates, and responds during exercise in the heat.
Acknowledgments
This investigation was funded in part by Waite, Schneider, Bayless & Chesley (Cincinnati, OH).
REFERENCES
- 1.Mueller F. O. Catastrophic sports injuries: who is at risk? Curr Sports Med Rep. 2003;2(2):57–58. doi: 10.1249/00149619-200304000-00001. [DOI] [PubMed] [Google Scholar]
- 2.Burton A. C. The application of the theory of heat flow to the study of energy metabolism. J Nutr. 1934;7:497–507. [Google Scholar]
- 3.Fox E. L., Mathews D. K., Kaufman W. S., Bowers R. W. Effects of football equipment on thermal balance and energy cost during exercise. Res Q. 1966;37(3):332–339. [PubMed] [Google Scholar]
- 4.Mathews D. K., Fox E. L., Tanzi D. Physiological responses during exercise and recovery in a football uniform. J Appl Physiol. 1969;26(5):611–615. doi: 10.1152/jappl.1969.26.5.611. [DOI] [PubMed] [Google Scholar]
- 5.Stitt J. T. Central regulation of body temperature. In: Gisolfi C. V., Lamb D. R., Nadel E. R., editors. Exercise, Heat, and Thermoregulation. Traverse City, MI: Cooper Publishing Group; 1993. pp. 1–47. Perspectives in Exercise Science and Sports Medicine; vol 6. [Google Scholar]
- 6.Montain S. J., Sawka M. N., Cadarette B. S., Quigley M. D., McKay J. M. Physiological tolerance to uncompensable heat stress: effects of exercise intensity, protective clothing, and climate. J Appl Physiol. 1994;77(1):216–222. doi: 10.1152/jappl.1994.77.1.216. [DOI] [PubMed] [Google Scholar]
- 7.Galloway S. D., Maughan R. J. Effects of ambient temperature on the capacity to perform prolonged cycle exercise in man. Med Sci Sports Exerc. 1997;29(9):1240–1249. doi: 10.1097/00005768-199709000-00018. [DOI] [PubMed] [Google Scholar]
- 8.Armada-da-Silva P. A., Woods J., Jones D. A. The effect of passive heating and face cooling on perceived exertion during exercise in the heat. Eur J Appl Physiol. 2004;91(5–6):563–571. doi: 10.1007/s00421-003-1006-0. [DOI] [PubMed] [Google Scholar]
- 9.Toner M. M., Drolet L. L., Pandolf K. B. Perceptual and physiological responses during exercise in cool and cold water. Percept Mot Skills. 1986;62(1):211–220. doi: 10.2466/pms.1986.62.1.211. [DOI] [PubMed] [Google Scholar]
- 10.Borg G. Perceived exertion as an indicator of somatic stress. Scand J Rehabil Med. 1970;2(2):92–98. [PubMed] [Google Scholar]
- 11.McCullough E. A., Kenney W. L. Thermal insulation and evaporative resistance of football uniforms. Med Sci Sports Exerc. 2003;35(5):832–837. doi: 10.1249/01.MSS.0000064998.48130.22. [DOI] [PubMed] [Google Scholar]
- 12.Noonan B., Mack G., Stachenfeld N. The effects of hockey protective equipment on high-intensity intermittent exercise. Med Sci Sports Exerc. 2007;39(8):1327–1335. doi: 10.1249/mss.0b013e3180619644. [DOI] [PubMed] [Google Scholar]
- 13.Kulka T. J., Kenney L. W. Heat balance limits in football uniforms: how different uniform ensembles alter the equation. Physician Sportsmed. 2002;30(7):29–39. doi: 10.3810/psm.2002.07.377. [DOI] [PubMed] [Google Scholar]
- 14.Hitchcock K. M., Millard-Stafford M. L., Phillips J. M., Snow T. K. Metabolic and thermoregulatory responses to a simulated American football practice in the heat. J Strength Cond Res. 2007;21(3):710–717. doi: 10.1519/R-20916.1. [DOI] [PubMed] [Google Scholar]
- 15.Maresh C. M., Herrera-Soto J. A., Armstrong E., et al. Perceptual responses in the heat after brief intravenous versus oral rehydration. Med Sci Sports Exerc. 2001;33(6):1039–1045. doi: 10.1097/00005768-200106000-00025. [DOI] [PubMed] [Google Scholar]
- 16.Engell D. B., Maller O., Sawka M. N., Francesconi R. N., Drolet L., Young A. J. Thirst and fluid intake following graded hypohydration levels in humans. Physiol Behav. 1987;40(2):229–236. doi: 10.1016/0031-9384(87)90212-5. [DOI] [PubMed] [Google Scholar]
- 17.Young A. J., Sawka M. N., Epstein Y., Decristofano B., Pandolf K. B. Cooling different body surfaces during upper and lower body exercise. J Appl Physiol. 1987;63(3):1218–1223. doi: 10.1152/jappl.1987.63.3.1218. [DOI] [PubMed] [Google Scholar]
- 18.Motl R. W., O'Connor P. J., Tubandt L., Puetz T., Ely M. R. Effect of caffeine on leg muscle pain during cycling exercise among females. Med Sci Sports Exerc. 2006;38(3):598–604. doi: 10.1249/01.mss.0000193558.70995.03. [DOI] [PubMed] [Google Scholar]
- 19.Kobrick J. L., Sampson J. B. New inventory for the assessment of symptom occurrence and severity at high altitude. Aviat Space Environ Med. 1979;50(9):925–929. [PubMed] [Google Scholar]
- 20.Armstrong L. E., Hubbard R. W., Kraemer W. J., DeLuca J. P., Christensen E. L. Signs and symptoms of heat exhaustion during strenuous exercise. Ann Sports Med. 1987;3(3):182–189. [Google Scholar]
- 21.Beidleman B. A., Muza S. R., Fulco C. S., Rock P. B., Cymerman A. Validation of a shortened electronic version of the Environmental Symptoms Questionnaire. High Alt Med Biol. 2007;8(3):192–199. doi: 10.1089/ham.2007.1016. [DOI] [PubMed] [Google Scholar]
- 22.Yamamoto L. M., Casa D. J., Stearns R. L., et al. Validation of a modified Environmental Symptoms Questionnaire for exercise in the heat. Med Sci Sports Exerc. 2008;40(5):S190. [Google Scholar]
- 23.Armstrong L. E., Johnson E. C., Casa D. J., et al. The American football uniform: uncompensable heat stress and hyperthermic exhaustion. J Athl Train. 2010;45(2):117–127. doi: 10.4085/1062-6050-45.2.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Johnson R. F., Merullo D. J. Nutritional Needs in Hot Environments: Applications for Military Personnel in Field Operations. Washington, DC: National Academy Press; 1993. Subjective reports of heat illness; pp. 277–293. In: Marriott BM, Committee on Military Nutrition of the Food and Nutrition Board of the Institute of Medicine, eds. [PubMed] [Google Scholar]
- 25.Cook D. B., O'Connor P. J., Eubanks S. A., Smith J. C., Lee M. Naturally occurring muscle pain during exercise: assessment and experimental evidence. Med Sci Sports Exerc. 1997;29(8):999–1012. doi: 10.1097/00005768-199708000-00004. [DOI] [PubMed] [Google Scholar]
- 26.Nindl B. C., Sharp M. A., Mello R. P., Rice V. J., Murphy M. M., Patton J. F. Gender comparison of peak oxygen uptake: repetitive box lifting versus treadmill running. Eur J Appl Physiol Occup Physiol. 1998;77(1–2):112–117. doi: 10.1007/s004210050308. [DOI] [PubMed] [Google Scholar]
- 27.Armstrong L. E. Assessing hydration status: the elusive gold standard. J Am Coll Nutr. 2007;26(suppl 5):575S–584S. doi: 10.1080/07315724.2007.10719661. [DOI] [PubMed] [Google Scholar]
- 28.Shirreffs S. M., Taylor A. J., Leiper J. B., Maughan R. J. Post-exercise rehydration in man: effects of volume consumed and drink sodium content. Med Sci Sports Exerc. 1996;28(10):1260–1271. doi: 10.1097/00005768-199610000-00009. [DOI] [PubMed] [Google Scholar]
- 29.Maughan R. J., Leiper J. B., Shirreffs S. M. Restoration of fluid balance after exercise-induced dehydration: effects of food and fluid intake. Eur J Appl Physiol Occup Physiol. 1996;73(3–4):317–325. doi: 10.1007/BF02425493. [DOI] [PubMed] [Google Scholar]
- 30.Cotter J. D., Zeyl A., Keizer E., Taylor N. A. S. The role of local skin temperature in determining the perception of local and whole-body thermal state. In: Shapiro Y. M., Epstein D. S., Jarusalem Y., editors. Environmental Ergonomics Recent Progress and New Frontiers. Tel Aviv, Israel: Freund Publishing House Ltd; 1996. pp. 85–88. [Google Scholar]
- 31.Gagge A. P., Stolwijk J. A., Hardy J. D. Comfort and thermal sensations and associated physiological responses at various ambient temperatures. Environ Res. 1967;1(1):1–20. doi: 10.1016/0013-9351(67)90002-3. [DOI] [PubMed] [Google Scholar]
- 32.Tatterson A. J., Hahn A. G., Martin D. T., Febbraio M. A. Effects of heat stress on physiological responses and exercise performance in elite cyclists. J Sci Med Sport. 2000;3(2):186–193. doi: 10.1016/s1440-2440(00)80080-8. [DOI] [PubMed] [Google Scholar]
- 33.Romanovsky A. A. Thermoregulation: some concepts have changed. Functional architecture of the thermoregulatory system. Am J Physiol Regul Integr Comp Physiol. 2007;292(1):R37–R46. doi: 10.1152/ajpregu.00668.2006. [DOI] [PubMed] [Google Scholar]
- 34.Egan G. F., Johnson J., Farrell M., et al. Cortical, thalamic, and hypothalamic responses to cooling and warming the skin in awake humans: a positron-emission tomography study. Proc Natl Acad Sci U S A. 2005;102(14):5262–5267. doi: 10.1073/pnas.0409753102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tominaga M., Caterina M. J. Thermosensation and pain. J Neurobiol. 2004;61(1):3–12. doi: 10.1002/neu.20079. [DOI] [PubMed] [Google Scholar]