Abstract
Context:
Previous research has indicated that despite awareness of the current literature on the recommended prevention and care of exertional heat stroke (EHS), certified athletic trainers (ATs) acknowledge failure to follow those recommendations.
Objective:
To investigate the current knowledge, attitudes, and practices of ATs regarding the recognition and treatment of EHS.
Design:
Cross-sectional study.
Setting:
Online survey.
Patients or Other Participants:
We obtained a random sample of e-mail addresses for 1000 high school and collegiate ATs and contacted these individuals with invitations to participate. A total of 498 usable responses were received, for a 25% response rate.
Main Outcome Measure(s):
The survey instrument evaluated ATs' knowledge and actual practice regarding EHS and included 29 closed-ended Likert scale questions (1 = strongly disagree, 7 = strongly agree), 2 closed-ended questions rated on a Likert scale (1 = lowest value, 9 = greatest value), 8 open-ended questions, and 7 demographic questions. We focused on the open-ended and demographic questions.
Results:
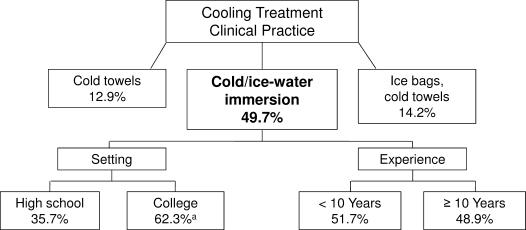
Although most ATs (77.1%) have read the current National Athletic Trainers' Association position statement on heat illness, only 18.6% used rectal thermometers to assess core body temperature to recognize EHS, and 49.7% used cold-water immersion to treat EHS. Athletic trainers perceived rectal thermometers as the most valid temperature assessment device when compared with other assessment devices (P ≤ .05), but they used oral thermometers as the primary assessment tool (49.1%). They identified cold-water immersion as the best cooling method (P ≤ .05), even though they used other means to cool a majority of the time (50.3%).
Conclusions:
The ATs surveyed have sound knowledge of the correct means of EHS recognition and treatment. However, a significant portion of these ATs reported using temperature assessment devices that are invalid with athletes exercising in the heat. Furthermore, they reported using cooling treatment methods that have inferior cooling rates.
Keywords: cooling methods, temperature assessment, evidence-based medicine, heat illnesses, whole-body cooling
Key Points.
Although most athletic trainers have read the current National Athletic Trainers' Association position statement on exertional heat illnesses, fewer than one-fifth used rectal thermometers to assess core body temperature, and only one-half used cold-water immersion to treat exertional heat stroke.
Athletic trainers identified lack of training and equipment and invasiveness as barriers to the use of rectal thermometry when evaluating a potential case of exertional heat stroke.
Limited resources, inducing shock and compromising the safety of the athlete, and success with other methods were documented as barriers to the implementation of cold-water immersion for the treatment of an athlete with an exertional heat stroke.
Exertional heat stroke (EHS) is a serious medical condition characterized by an elevated core body temperature (>104°F [40°C]) and central nervous system dysfunction1,2 that has a potentially tragic outcome if not properly recognized and rapidly treated.1,3,4 The condition occurs predominantly in settings in which athletes perform intense exercise in hot or humid environmental conditions, but it also can occur in a mild environment. Although numerous preventive measures can be adopted by coaches, sport administrators, and the medical staff to reduce the likelihood of EHS (eg, decrease performance intensity, change practice time, decrease or eliminate equipment, acclimatize properly to the heat, hydrate appropriately), the risk of EHS is ever present. Because of the potential for EHS when athletes exercise in the heat, the medical staff must be equipped with the best policies and procedures to recognize and treat the condition in the most efficacious manner.
Current literature1,5 supports rectal temperature as the most practical, reliable, and valid means for assessing hyperthermic body temperature in the field setting. Methods such as esophageal and ingestible thermistors are valid for assessing body temperature during outdoor exercise in the heat but are less practical than rectal thermometers. Sports medicine associations (National Athletic Trainers' Association [NATA],1 American College of Sports Medicine [ACSM],2 International Amateur Athletic Federation6) and military organizations (US7 and Israeli8 militaries) have strongly advocated the use of rectal temperature assessment when EHS is suspected.
For the treatment of EHS, cold-water or ice-water immersion or dousing has demonstrated superior cooling rates and is, therefore, recommended9–11 as the most efficient cooling treatment for hyperthermic individuals. The efficacy of combining rectal temperature assessment with cold-water or ice-water immersion or dousing is evident from the 100% survival rates reported at the Falmouth Road Race12,13; Marine Corps Marathon14; Marine Corps Recruit Depot at Parris Island, South Carolina15; Marine Corps Base at Quantico, Virginia (Bruce Adams, oral communication, October 2008); and many others. Temperature assessment via rectal measurement and rapid cooling via cold-water or ice-water immersion or dousing can account for the lack of fatalities in the more than 1000 cases of EHS during at least the past 20 years of these events (Bruce Adams, oral communication, October 2008).12–15 However, the care provided to EHS patients in youth, middle school, high school, college, and professional sport settings, as well as other sport venues, has not followed the aforementioned guidelines, and numerous fatalities have been reported.16 Exertional heat stroke is the second leading cause of death among athletes, followed only by sudden cardiac death,17 particularly during August preseason football. A recent NATA News16 article highlighted the sobering reality of sport fatalities, in which at least 3 of the 16 fatalities during the 2008 preseason were the result of EHS. The recent trial of a Kentucky high school football coach in the EHS death of an athlete confirms both the seriousness of EHS and the lack of understanding of potentially fatal environmental illness. Previous researchers18 have demonstrated that athletic trainers (ATs) have a strong knowledge base regarding EHS, particularly with respect to preventive measures and recognition of appropriate methods for evaluation and treatment, yet they choose to use other, invalid temperature devices and cooling methods. The dichotomy between knowledge of EHS and appropriate assessment and treatment may contribute to more adverse outcomes. Dombek et al18 investigated high school ATs' knowledge and behaviors regarding the prevention, recognition, and treatment of EHS. Although ATs were actively taking steps to prevent EHS and identified rectal temperature as the most valid assessment device for EHS (88%) and cold-water immersion as the most effective cooling method (60.7%), many acknowledged using oral thermometers (65%) to assess core temperature, treating EHS with methods other than cooling (eg, removal of clothing, finding shade), and using cold-water immersion sparingly (31%). Dombek et al18 were among the first to identify a gap between ATs' knowledge and clinical practices within a given domain of athletic training. Because of the potential mortality linked to EHS, we need to further investigate ATs' beliefs and practices regarding the condition.
Building upon the work of Dombek et al,18 we studied both high school and collegiate settings; focused on the recognition and treatment of EHS; used a validated survey instrument to gain better insight into ATs' knowledge, attitudes, and practices regarding EHS; and explored potential barriers to implementing the recommended practices. Our purpose, therefore, was to determine ATs' knowledge, attitudes, and practices regarding the recognition and treatment of EHS. The research questions that guided this investigation were as follows:
Do ATs possess the knowledge to accurately diagnose and treat a suspected EHS?
Are ATs using the recommended practices for the recognition and treatment for an EHS, as outlined by the NATA1 position statement on exertional heat illnesses?
If ATs acknowledge not following recommended practices for the recognition and treatment of EHS, what barriers are preventing ATs from using those recommendations?
METHODS
Participants
A total of 2000 potential participants (1000 high school ATs, 1000 collegiate ATs) were identified by the NATA, and 498 ATs participated, yielding a 25% response rate. Volunteers were randomly selected for participation, regardless of previous exposure to athletes with EHS.
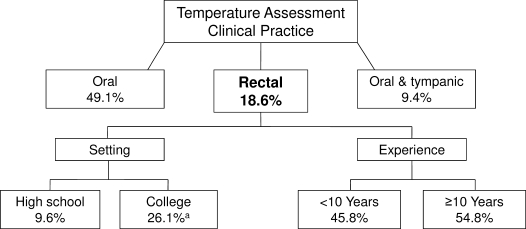
Instrument
To date, we are unaware of a validated instrument to investigate the clinical practice behaviors of ATs regarding EHS. Therefore, we developed a survey to investigate the current behaviors of ATs with regard to the recognition and treatment of EHS. To create the survey, we called on a group of heat and hydration experts (n = 8) to develop questions addressing the aforementioned research questions. In addition, content and face validity were established through pilot testing and exploratory factor analysis. The final instrument included 29 closed-ended questions rated on a Likert scale (1 = strongly disagree, 7 = strongly agree), 2 closed-ended questions rated on a different Likert scale (1 = lowest value, 9 = greatest value), 8 open-ended questions, and 7 demographic questions. The 8 open-ended questions investigated the respondent's actual clinical practice and reasons for such practice (eg, temperature assessment device, cooling methods). The purpose of this paper is to highlight the findings yielded by the respondents' rankings on the 2 closed-ended questions and the open-ended items, which addressed the actual clinical practices of ATs as well as the rationales behind the selection of those practice methods. Table 1 provides some of the questions used for analysis.
Table 1.
Sample Survey Questionsa
Procedures
The study received approval from the University of Connecticut institutional review board. We obtained 2000 e-mail addresses of male and female ATs (1000 high school and 1000 collegiate ATs) at random from the NATA membership office and e-mailed these individuals an invitation to participate in the survey, a description of the procedures required to participate, and an electronic link to the Internet site containing the survey. Confidentiality and the right to forego participation were ensured. Participants were asked to complete the survey 1 time only. To encourage completion of the survey, nonrespondents received reminder broadcast letters biweekly for 2 months.
Statistical Analyses
Closed-ended items (ranking questions for temperature assessment and treatment of EHS) were analyzed using 1-way analysis of variance, and follow-up independent-samples t tests were used to examine within-groups differences (clinical setting, experience, and previous experience with EHS). For this study, clinical setting was defined as either high school or college, experience was defined as less than 10 years or 10 years or more, and experience with EHS was defined as previous exposure to recognizing or treating an EHS. Paired-samples t tests were used for an overall comparison of 2 closed-ended items: views on temperature assessment device validity and efficacy of cooling treatment methods. Qualitative data were openly coded by 2 independent coders to ensure validity of the categories. The categories were created to demonstrate preference of temperature assessment device and cooling treatment as well as to summarize the overall opinions of the respondents based upon reasons for lack of implementation of rectal temperature assessment and cold-water immersion treatments. Frequencies were obtained for open-ended items (preference for temperature assessment and cooling) and analyzed using a Pearson χ2 test after the data were categorized and assigned a number code (eg, ice bag = 1). Significance was set at P ≤ .05 for all statistical analyses.
RESULTS
Demographics
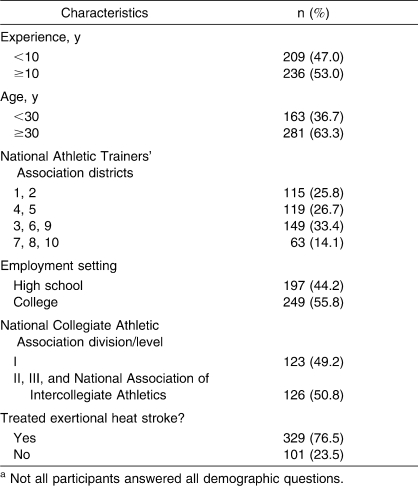
A total of 498 surveys were received and complete demographics were analyzed from 446 respondents (n = 197 high school, n = 249 college). Because the demographic questions were located at the end of the survey, some participants failed to complete this section, which resulted in discrepancies in reporting demographic data (Table 2). Although 77% (347/450) of the participants indicated that they had read the current NATA1 position statement on exertional heat illnesses, 63.6% (287/449) admitted to not having reading the ACSM position stand2 on exertional heat illnesses. Additionally, 76.5% (344/450) of the respondents indicated they had experience with treating EHS in the clinical setting.
Table 2.
Demographic Data of Survey Respondentsa
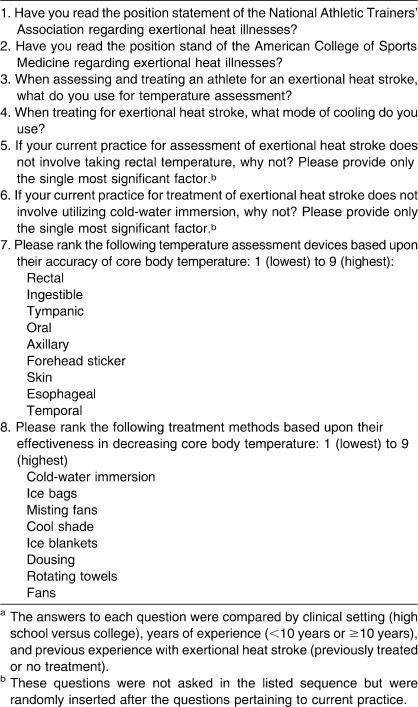
Temperature Assessment Devices: Validity of Instruments
The ATs surveyed perceived rectal and ingestible thermistors as the most valid temperature assessment devices when compared with other devices (P < .001), regardless of clinical setting, experience, or previous experience in treating EHS (Figure 1). When participants were compared by experience, ingestible temperature was rated as having greater validity by more experienced ATs (those with 10 or more years of experience) compared with less experienced ATs (those with fewer than 10 years of experience) (P = .042). Those ATs with less experience rated axillary temperature as a more valid measure than did more experienced ATs (P = .026). No differences were noted within NATA districts regarding views on the validity of temperature assessment devices. High school ATs rated oral (P = .022) and forehead sticker temperatures (P = .032) as more valid than did collegiate ATs. By collegiate setting, ATs at the National Collegiate Athletic Association Division II and III and National Association of Intercollegiate Athletics levels rated the validity of temporal (P = .012), tympanic (P = .005), oral (P = .047), forehead sticker (P = .001), and skin temperature (P = .028) higher than did Division I ATs. Those who had previously treated EHS rated temporal (P = .032) and skin temperatures (P = .026) as more valid than did ATs without experience in dealing with EHS treatment.
Figure 1.
Athletic trainers' views on validity of temperature assessment devices (n = 498). a Difference compared with rectal temperature (P < .05).
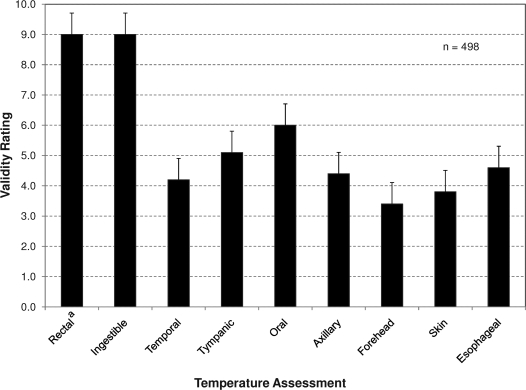
Temperature Assessment Devices: Actual Practice
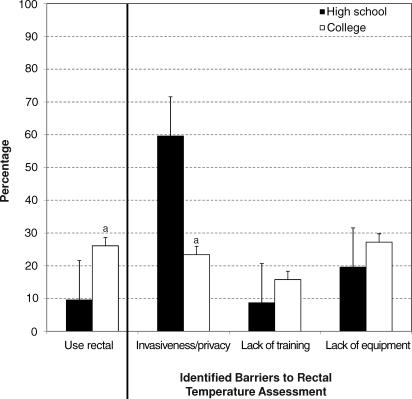
Rectal and ingestible thermometers were cited as the most valid temperature assessment devices. However, only 18.6% (93/456) of participants used these devices for core body temperature assessment in an athlete with possible EHS. Oral thermometers were the most commonly used assessment devices (49.1%, 224/456), followed by the combination of oral and tympanic devices (9.4%, 43/456) and tympanic devices alone (9%, 41/456). A total of 8% (40/456) of ATs did not use any device to assess body temperature in a potential case of EHS. High school ATs used a temperature assessment method other than rectal more often than did collegiate ATs (P < .001), who more frequently used rectal temperature assessment (P < .001). Figure 2 provides a breakdown of clinical practices by clinical setting and years of experience. Invasiveness, lack of training, and lack of equipment availability were major reasons cited for the use of temperature assessment devices other than rectal thermometers (Figure 3). Compared with collegiate ATs, high school ATs used other temperature devices, rather than rectal thermometers, reporting invasiveness and privacy as the most common barriers (P < .001) to using rectal thermometers. See Table 3 for identified barriers to the use of rectal thermometers.
Figure 2.
Athletic trainers' temperature assessment clinical practices, overall and within setting and experience groups (high school athletic trainers = 197, collegiate athletic trainers = 249, athletic trainers with fewer than 10 years of experience = 209, athletic trainers with 10 or more years of experience = 236). a P < .05.
Figure 3.
Percentage of athletic trainers who used rectal temperature assessment in the evaluation of possible exertional heat stroke and barriers identified by those who did not (high school athletic trainers = 197, collegiate athletic trainers = 249). a P < .05.
Table 3.
Barriers to Use of Rectal Thermometers
Treatment: Validity of Cooling Methods
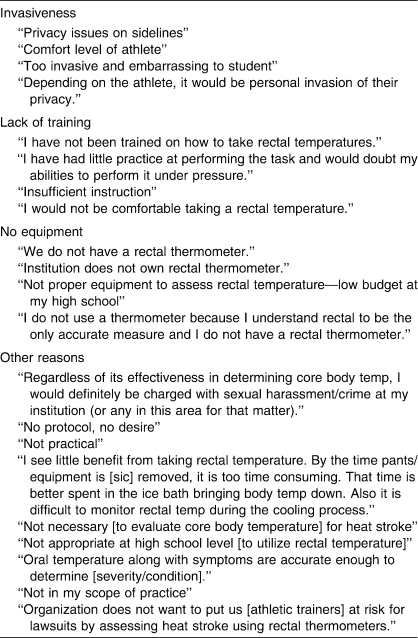
An overall comparison of cooling treatment methods was performed (Figure 4). Cold-water or ice-water immersion was rated as the most effective cooling treatment, followed by the ice vest and blankets (P < .001), regardless of clinical setting, experience, or previous experience in treating EHS. When compared with less experienced ATs (those with fewer than 10 years of experience), more experienced ATs (those with 10 or more years of experience) rated cold-water or ice-water immersion (P = .004), fans (P = .016), misting fans (P = .001), and rotating towels (P = .001) as the most effective cooling treatments. High school ATs rated misting fans as more effective in treating EHS than did collegiate ATs (P = .032). Within collegiate divisions and EHS treatment experience groups, we found no differences regarding views on cooling treatment efficacy.
Figure 4.
Athletic trainers' views on efficacy of cooling treatment methods for exertional heat stroke (n = 497). a Difference compared with cold-water or ice-water immersion (P < .05).
Treatment: Actual Practice
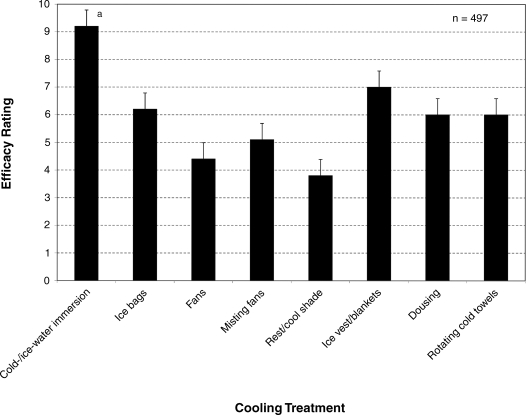
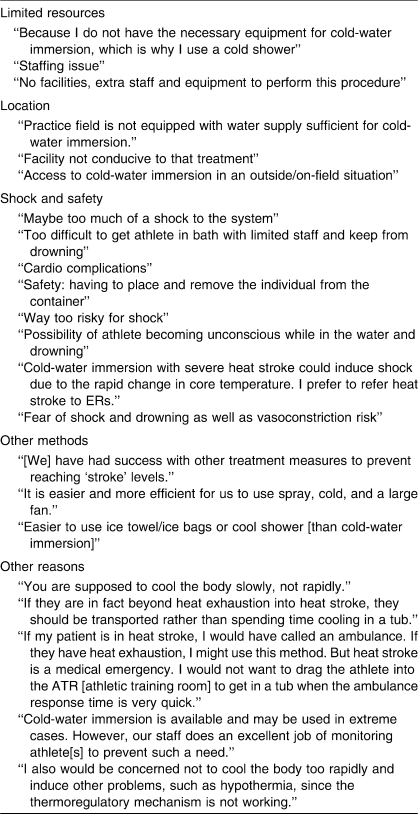
Although ATs identified cold-water or ice-water immersion as the most efficient cooling treatment when compared with other cooling methods (P < .001), only 49.7% (224/451) identified this as their EHS treatment of choice. The most commonly practiced cooling method was ice bags or towels (14.2%, 64/451), followed by cold towels (12.9%, 58/451) and ice bags (10%, 45/451). More collegiate ATs reported using cold-water or ice-water immersion for primary cooling treatment than did high school ATs (P < .001). Consequently, high school ATs more frequently reported using other methods for primary cooling (P < .001). Figure 5 provides a synopsis of actual clinical practice by clinical setting and years of experience. Limited resources and staffing, location, shock and safety, and use of other cooling methods were cited as reasons why cold-water and ice-water immersion were not implemented (Table 4). High school ATs more often reported limited resources as a primary reason for not using cold-water or ice-water immersion, compared with collegiate ATs (P < .001). Table 4 provides a list of reasons ATs chose other cooling methods.
Figure 5.
Athletic trainers' cooling treatment clinical practices, overall and within setting and experience groups (athletic trainers with fewer than 10 years of experience = 209, athletic trainers with 10 or more years of experience = 236). a P < .05.
Table 4.
Barriers to Implementation of Cold-Water or Ice-Water Immersion
DISCUSSION
Although death from EHS is preventable, every year athletes succumb to hyperthermic injury. The purpose of our investigation was to identify the level of knowledge of high school and collegiate ATs with regard to EHS; we also sought to identify their current practices for recognition and treatment of EHS. Because EHS is a frequent occurrence in military and athletic settings, many researchers have sought to understand the causes of EHS and to reduce or prevent the mortality linked to the condition. A connection between EHS deaths and improper practices and medical care has been suggested by previous authors18 and therefore served as the impetus for our research study.
Our most notable and disconcerting result was the discrepancy between current position statement recommendations and the behavior of ATs regarding the recognition and treatment of EHS, as documented in our open-ended survey questions. Although 77.1% had read the latest NATA1 position statement on exertional heat illness and could correctly identify the most valid temperature assessment devices and treatment options, many were not following these recommended guidelines, a finding comparable with the results generated by the pilot study of Dombek et al.18 More perplexing is that the ATs recognized that rectal temperature and cold-water or ice-water immersion were the “gold standards” for recognition and treatment, respectively, but opted to use other methods based upon personal beliefs or inaccurate information rather than evidence-supported recommendations. Moreover, the rationale (Tables 3 and 4) behind the ATs' selections of modalities for temperature assessment devices and treatment methods for EHS demonstrates a dichotomy between knowledge and appropriate clinical practice. The gap between evidence-based recommendations and actual clinical practice exists not only with the recognition and treatment of EHS but also within the overall health care system,19 because only 55% of physicians adhere to evidence-based medicine.20,21 Skill expertise, lack of familiarity, confidence in abilities,19 and practice style traits22 have all been documented as influencing a medical professional's use of evidence-based practice. Several of the factors found previously are similar to the barriers (Tables 3 and 4) cited by our participants with regard to EHS. However, more research is necessary to completely understand why the best practices are not being implemented. Additionally, more than three-quarters of those who completed the survey indicated treating an EHS, which calls into question whether the condition was properly diagnosed and treated, particularly in light of the respondents' preferences for nonrecommended practices and assessment devices.
Another explanation, one that necessitates future inquiry, is the role of clinical education and academic preparation of athletic training students as a potential reason for the discrepancy between knowledge and appropriate clinical practice in EHS treatment. Clinical education is a critical component for athletic training students as they integrate athletic training knowledge and skills,23 and although students use a variety of methods to learn,24–26 they must be afforded ample opportunities to practice and demonstrate their skill proficiency through authentic (observational and hands-on) experiences.27,28 Proficiency, a measure of “real-life” application,29(p3) may not always be plausible in clinical education but is still necessary for professional development.30 Perhaps a lack of EHS exposure (to both recognition and treatment) within the clinical setting is leading to the use of invalid temperature assessment devices and inappropriate treatment methods. In addition, athletic training educators may be providing students with accurate information regarding recommended practices for EHS but undermining their application within the clinical setting by failing to offer students structured, hands-on experience in the didactic portion of the curriculum so that the students gain proficiency. Under the current NATA educational competencies, athletic training students must only recognize that rectal temperature assessment and cold-water immersion are options for recognition and treatment of EHS, but these procedures are not documented as the gold standard by the NATA educational competencies.29 Yet the NATA1 and ACSM2 position stands do, indeed, recognize these practices as the gold standard. This is relevant given the fact that the NATA educational competencies specifically reference the NATA position statements as the gold standard for practice guidelines and encourage all program personnel to include evidence-based practice in a student's educational program.29 Also, once the student is in the clinical setting, a disregard for recommended practices is reinforced by the lack of exposure to actual cases of EHS, coupled with a clinical instructor's opinions and use of inappropriate assessment and treatment methods. Modeling professional behaviors and practices has been documented23 as the most beneficial strategy to promote learning for athletic training students; therefore, modeling may provide a plausible rationale for the dichotomy between understanding appropriate evaluation and treatment measures and using them when necessary. Based upon the responses provided by participants regarding choice and support of temperature assessment devices and cooling methods (Tables 3 and 4), inconsistencies are evident in the knowledge and practice demonstrated in the clinical education of ATs. Some of these participants may serve in the capacity of an Approved Clinical Instructor and are, as a result, charged with mentoring future clinicians; their practices greatly influence students' experiences. Finally, the athletic training student's decisions regarding EHS may be reinforced by a lack of supervision31 or limited clinical instruction time30 when working as an AT.
Temperature Assessment Devices and Clinical Practice
Many signs and symptoms are associated with EHS, including altered mental status, vomiting, and hypotension. However, the hallmark of the condition is an elevated core body temperature of 40°C (104°F). Therefore, temperature assessment is a key component in the recognition of EHS. Based on accuracy and practicality, rectal temperature assessment is recommended by the NATA,1 the Inter-Association Task Force on heat illness,6 and the ACSM.2 In its position stand on exertional heat illness during training and competition, the ACSM2 stated that
rectal temperature should be measured in any athlete who collapses or exhibits signs and symptoms consistent with EHS. Temporal, tympanic, oral, axillary, and skin temperature measurements should not be used to diagnose or distinguish EHS from exertional heat exhaustion.2(p561)
Esophageal and ingestible temperature assessments are also considered accurate, but because of the invasiveness of the former and drawbacks of the latter, rectal assessment is preferred. Despite criticisms and perceptions of impracticality, the NATA1 mirrors the ACSM2 recommendations for forehead skin temperatures. In support of the use of rectal temperature, Casa et al5 reported different body temperature measurements of hyperthermic participants exercising in the heat when rectal temperature was compared with oral, tympanic, axillary, temporal, and forehead temperatures. Evidence refuting the validity of these commonly used methods for body temperature assessment (oral, temporal, and axillary) indicates that ATs who fail to use rectal temperature as a means of assessment can miss or delay the diagnosis of EHS. Any delay in the initiation of rapid cooling increases the likelihood of an adverse outcome.9 Immediate rectal temperature measurement for a suspected EHS patient is a nearly foolproof method of properly assessing this condition. In the current study, we found that 71.4% (n = 330) of participants currently use temperature devices other than rectal thermometers. Also, 90% of high school ATs (n = 158) reported using temperature devices other than rectal thermometers; this was higher than the rate of their collegiate counterparts (67.9%, n = 167). Regardless of personal beliefs and current practices, tympanic and oral temperature devices should not be used in combination for clinical assessment because of their documented5 inaccuracy in those individuals who are exercising in the heat. Furthermore, as medical care providers, ATs must move past their own insecurities and trepidations regarding the use of the rectal thermometer in order to accurately diagnose a potential medical emergency and then appropriately apply the best treatment. Given the consistent, strong available evidence regarding the lack of validity of temporal, tympanic, oral, and axillary measures of core temperature for athletes performing intense exercise in the heat, it could easily be assumed that using these devices to assess for EHS might constitute medical malpractice, and legal implications could ensue.
Again, similar to the findings reported by Dombek et al,18 ATs in our study were aware of the proper clinical practices for EHS, yet they failed to apply that understanding to their clinical practice. Prior to this investigation, we were unaware of any research conducted to better understand potential barriers or hindrances resulting in the inconsistency between recommended and actual care for EHS patients. As previously mentioned, many ATs indicated privacy and invasiveness issues (and possible legal issues), lack of training, and a lack of equipment as reasons why they did not implement rectal temperature measurements. In other words, the potential for saving a life by measuring rectal temperature was thwarted by the discomfort and adherence to social norms regarding a patient's privacy. This indicates a need for improved or continuing education (or both). A lack of training in rectal temperature assessment by ATs, and a similar barrier reported by physicians regarding adherence to practice guidelines,19 points toward an educational deficiency regarding EHS in AT education curricula. Classroom instruction and laboratory education on the nuances of rectal temperature assessment and the field application of this skill need to be integrated, so that clinicians develop a higher comfort level with implementing this skill during a time of stress. In addition, there is a clear need for seminars and workshops for ATs regarding best practices in EHS. As we move toward an evidence-based medical model and continue to secure our reputation in the medical field, it is imperative that educators and clinicians follow the guidelines recommended in the recognition and treatment of EHS. Yet, until ATs accept the use of rectal thermometers, take the steps necessary to feel comfortable using the device, and include rectal thermometers in medical equipment budgets, improper diagnosis of EHS will continue. Furthermore, complying with the NATA1 position statement regarding the use of rectal temperature assessment assures that the best available medical evidence is being used to diagnose and monitor EHS patients. An important step in assisting ATs to learn how to perform this important diagnostic test is to have the skill added to the NATA educational competencies and to offer continuing education opportunities for current practitioners. Lack of equipment may be the result of inadequate knowledge by athletic directors and others responsible for purchasing appropriate equipment for the AT.
Treatment and Clinical Practice
If performed properly and rapidly, treatment of EHS can be life saving. In conjunction with early recognition, the NATA1 position statement recommended rapid cooling of a person with suspected EHS: “Lower the body-core temperature as quickly as possible. The fastest way to decrease body temperature is to remove clothes and equipment and immerse the body (trunk and extremities) into a pool or tub of cold water.”1(p334) Only half of the participants within the current research study used cold-water or ice-water immersion for EHS treatment. When compared by clinical setting (Figure 4), 64.3% (n = 126) of high school ATs and 37.7% (n = 92) of collegiate ATs used other cooling treatments, indicating that high school ATs were more likely than collegiate ATs to rely on improper methods when treating EHS.
Rapid cooling treatment via cold-water or ice-water immersion, although strongly recommended by association position statements, has been occasionally criticized by professionals in the sports medicine community. In a review, Casa et al9 presented strong support for the use of cold-water or ice-water immersion as the gold standard for EHS treatment. Casa et al9 addressed and refuted the misconceptions regarding cold-water and ice-water immersion. Misconceptions associated with cold-water and ice-water immersion include peripheral vasoconstriction, which impedes heat loss; onset of shivering, which delays cooling; discomfort of cold water for patient and care providers; difficulty applying supplemental treatments; unsanitary conditions; hypothermic afterdrop; impracticality; and lack of cooling superiority. These misconceptions have been reported throughout the sports medicine literature and may be factors contributing to improper EHS treatment practices among ATs. In our study, collegiate and high school ATs cited a lack of resources (eg, cold-water immersion tub), field location, success using other methods, potential cardiovascular shock, and other safety issues of the patient as major reasons why cold-water immersion was not used. This finding is alarming, especially given that most participants acknowledged having read the NATA1 position statement regarding exertional heat illnesses and EHS. Again, those responsible for allocating funds to obtain adequate equipment may contribute to the failure to use cold-water immersion if such equipment is not available for treatment. The ATs also stated that the location of the equipment hindered their use of cold-water or ice-water immersion, which indicates poor organizational strategy or lack of resources (or both). Participants in our study preferred to use other, less effective methods of cooling, indicating a bias against cold-water or ice-water immersion, perhaps resulting from the many misconceptions reported in the sports medicine literature.
Preference for other cooling treatments is potentially linked to other issues. For example, ATs in the high school and collegiate setting differed in their knowledge of EHS treatment. Compared with collegiate ATs, high school ATs were more likely to agree that cold-water or ice-water immersion should not be used because of lack of staffing and difficulty placing an athlete in an immersion tub. However, these reasons do not appear to be valid, because coaches and other athletes can assist in this effort. Most high schools have only 1 AT; therefore, lack of staffing can be an issue when administering a cooling treatment. For high school ATs, using ice bags may be easier and may require less assistance than attempting to move the patient into an immersion tub. We interpret this as a preference for a more convenient, less effective treatment, as opposed to using a proven, rapid, life-saving treatment. When compared with collegiate ATs, high school ATs were less likely to use cold-water or ice-water immersion because of their inability to continuously monitor rectal temperature, even though they viewed rectal temperature assessment as the best method. When compared with Division I ATs, those in Divisions II and III and the National Association of Intercollegiate Athletics also hesitated to use cold-water immersion because of the inability to continuously monitor rectal temperature. Other cooling methods, although less efficient, are perceived to allow for continuous monitoring of core temperature, unlike rectal temperature measurement, yet this rationale is untrue. This incorrect assumption would explain the preference for cooling methods over cold-water or ice-water immersion in these settings. Despite the preference of some ATs for these cooling methods, the consequences may be catastrophic, and ATs must understand that the keys to treating EHS and preventing death are to “cool first” via cold-water or ice-water immersion and “transport second.”14(p148) The concept that treatment for EHS is more effective if they do not immediately transport to the hospital is tough for many medical professionals to grasp but is the most critical aspect of acute care for EHS. Aggressive cooling must begin onsite immediately to assure survival, and transportation could hinder this process, possibly to the extent of a fatal consequence. Thus, the AT needs to be ready to initiate aggressive cooling onsite. When the athlete is sufficiently cooled via cold-water immersion (usually to about 38.9–39.4°C [102–103°F], which typically takes 15–20 minutes in cold water), then he or she can be immediately transported to the hospital via an ambulance.
Limitations
Given the low response rate in the current study, our findings must be interpreted with caution. Applying findings from this study to ATs in other settings or to other sports medicine professionals may be inappropriate, because only high school and collegiate ATs participated in the survey. We took several steps to increase the overall response rate, including developing a shorter survey and sending reminder e-mails to nonrespondents; however, the low response rate (25%) was a limiting factor in the overall strength of the findings. Low response rates have been reported32 in Web-based surveys compared with mail surveys. Additionally, response rates have been less than optimal when studying random samples within the NATA.32
CONCLUSIONS
The ATs who participated in the current study, on average, rated rectal temperature assessment as the most valid method, compared with other commonly used temperature assessment devices. They also rated cold-water or ice-water immersion as providing faster cooling than other treatment methods. Because these findings are consistent with the literature, we believe that high school and collegiate ATs, in general, have sound knowledge of the correct means of EHS recognition and treatment. However, the ATs were still hesitant to adhere to or implement evidence-based recommendations as they pertain to EHS.
Several steps must be taken to continue to reduce the fatal consequences associated with EHS, including the use of rectal thermometry and cold-water or ice-water immersion in the recognition and treatment of EHS and the continued education of health care providers who diagnose and treat EHS.33,34 Finally, additional research is necessary to determine why ATs have not implemented the recommended practices and to determine what can be done to change this disconnect between knowledge and clinical practice.
Acknowledgments
We thank Angie West, MA, ATC; Rebecca Stearns, MA, ATC; and Rebecca Lopez, MS, ATC, for their tireless efforts toward survey and methods development. We also thank the initial panel of experts who participated in the development and validation of the survey instrument, as well as all the athletic trainers who took the time to complete the survey.
REFERENCES
- 1.Binkley H. M., Beckett J., Casa D. J., Kleiner D. M., Plummer P. E. National Athletic Trainers' Association position statement: exertional heat illnesses. J Athl Train. 2002;37(3):329–343. [PMC free article] [PubMed] [Google Scholar]
- 2.Armstrong L. E., Casa D. J., et al. American College of Sports Medicine. American College of Sports Medicine position stand: exertional heat illnesses during training and competition. Med Sci Sports Exerc. 2007;39(3):556–572. doi: 10.1249/MSS.0b013e31802fa199. [DOI] [PubMed] [Google Scholar]
- 3.Casa D. J., Armstrong L. E., Ganio M. S., Yeargin S. W. Exertional heat stroke in competitive athletes. Curr Sports Med Rep. 2005;4(6):309–317. doi: 10.1097/01.csmr.0000306292.64954.da. [DOI] [PubMed] [Google Scholar]
- 4.Rav-Acha M., Hada E., Epstein M., Heled Y., Moran D. S. Fatal exertional heat stroke: a case series. Am J Med Sci. 2004;328(2):84–87. doi: 10.1097/00000441-200408000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Casa D. J., Becker S. M., Ganio M. S., et al. Validity of devices that assess body temperature during outdoor exercise in the heat. J Athl Train. 2007;42(3):333–342. [PMC free article] [PubMed] [Google Scholar]
- 6.Roberts W. O. Part II: medical management and administration manual for long-distance road racing. In: Brown C. H., Gudjonsson B., editors. IAAF Medical Manual for Athletics and Road Racing Competitions: A Practical Guide. Monaco: International Amateur Athletic Federation Publications; 1998. pp. 39–76. [Google Scholar]
- 7.Heat Stress Control and Casualty Management. Bethesda, MD: Departments of the Army and Air Force; 2003. Headquarters Department of the Army and Air Force. Technical Bulletin MED 507/AFPAM 48-152(1). [Google Scholar]
- 8.Epstein Y., Moran D. S., Shapiro Y. Exertional heatstroke in the Israeli Defense Forces. In: Pandolf K. B., Burr R. E., editors. Medical Aspects of Harsh Environments. Vol 1. Bethesda, MD: US Army Medical Department; 2001. pp. 281–292. [Google Scholar]
- 9.Casa D. J., McDermott B. P., Lee E. C., Yeargin S. W., Armstrong L. E., Maresh C. M. Cold water immersion: the gold standard for exertional heatstroke treatment. Exerc Sport Sci Rev. 2007;35(3):141–149. doi: 10.1097/jes.0b013e3180a02bec. [DOI] [PubMed] [Google Scholar]
- 10.Clements J. M., Casa D. J., Knight J. C., et al. Ice-water immersion and cold-water immersion provide similar cooling rates in runners with exercise-induced hyperthermia. J Athl Train. 2002;37(2):146–150. [PMC free article] [PubMed] [Google Scholar]
- 11.Proulx C. I., Ducharme M. B., Kenny G. P. Effect of water temperature on cooling efficiency during hyperthermia in humans. J Appl Physiol. 2003;94(4):1317–1323. doi: 10.1152/japplphysiol.00541.2002. [DOI] [PubMed] [Google Scholar]
- 12.O'Malley D. E. Hyperthermia on a short race course: the Falmouth Road Race experience. Paper presented at: American Medical Athletic Association's 37th Annual Sports Medicine Symposium at the Boston Marathon; April 19, 2008; Boston, MA.
- 13.Brodeur V. B., Dennett S. R., Griffin L. S. Exertional hyperthermia, ice baths, and emergency care at the Falmouth Road Race. J Emerg Nurs. 1989;15(4):304–312. [PubMed] [Google Scholar]
- 14.McDermott B. P., Casa D. J., O'Connor F. G., et al. Examination of cold water-ice massage therapy for exertional heat stroke. Aviat Space Environ Med. 2009;80(8):720–722. doi: 10.3357/asem.2498.2009. [DOI] [PubMed] [Google Scholar]
- 15.Costrini A. Emergency treatment of exertional heatstroke and comparison of whole body cooling techniques. Med Sci Sports Exerc. 1990;22(1):15–18. [PubMed] [Google Scholar]
- 16.Bostic J., Hunt V. Sobering season: sports fatalities put medical care in spotlight. NATA News. 2008. pp. 16–17. October.
- 17.National Center for Catastrophic Injury Research. Catastrophic sport injury 25th annual report. http://www.unc.edu/depts/nccsi/index.htm. Accessed January 1, 2009.
- 18.Dombek P. M., Casa D. J., Yeargin S. W., et al. Athletic trainers' knowledge and behavior regarding the prevention, recognition, and treatment of exertional heat stroke at the high school level [abstract] J Athl Train. 2006;41(suppl 2):S47. [Google Scholar]
- 19.Cochrane L. J., Olson C. A., Murray S., Dupis M., Tooman T., Hayes S. Gaps between knowing and doing: understanding and assessing the barriers to optimal health care. J Contin Educ Health Prof. 2007;27(2):94–102. doi: 10.1002/chp.106. [DOI] [PubMed] [Google Scholar]
- 20.McGlynn E. A., Asch S. M., Adams J., et al. The quality of health care delivered to adults in the United States. N Engl J Med. 2003;348(26):2635–2645. doi: 10.1056/NEJMsa022615. [DOI] [PubMed] [Google Scholar]
- 21.Asch S. M., Kerr E. A., Keesey J., et al. Who is at greatest risk for receiving poor-quality health care? N Engl J Med. 2006;354(11):1147–1156. doi: 10.1056/NEJMsa044464. [DOI] [PubMed] [Google Scholar]
- 22.Korner-Bitensky N., Menon-Nair A., Thomas A., Boutin E., Arafah A. M. Practice style traits: do they help explain practice behaviors of stroke rehabilitation professionals? J Rehabil Med. 2007;39:685–692. doi: 10.2340/16501977-0106. [DOI] [PubMed] [Google Scholar]
- 23.Laurent T., Weidner T. G. Clinical instructors' and student athletic trainers' perceptions of helpful clinical instructor characteristics. J Athl Train. 2001;36(1):58–61. [PMC free article] [PubMed] [Google Scholar]
- 24.Brower K. A., Stemmans C. L., Ingersoll C. D., Langley D. J. An investigation of undergraduate athletic training students learning styles and program admission success. J Athl Train. 2001;36(2):130–135. [PMC free article] [PubMed] [Google Scholar]
- 25.Stradley S. L., Buckley B. D., Kaminski T. W., Horodyski M., Fleming D., Janelle C. M. A nationwide learning-style assessment of undergraduate athletic training students in CAAHEP-accredited athletic training programs. J Athl Train. 2002;37(suppl 4):S141–S146. [PMC free article] [PubMed] [Google Scholar]
- 26.Harrelson G. L., Leaver-Dunn D., Wright K. E. An assessment of learning styles among undergraduate athletic training students. J Athl Train. 1998;33(1):50–53. [PMC free article] [PubMed] [Google Scholar]
- 27.Mensch J. M., Ennis C. D. Pedagogic strategies perceived to enhance student learning in athletic training. J Athl Train. 2002;37(suppl 4):S199–S207. [PMC free article] [PubMed] [Google Scholar]
- 28.Middlemas D. A., Grant Ford M. L. Teaching high-risk clinical competencies: simulations to protect students and models. Athl Ther Today. 2005;10(11):23–25. [Google Scholar]
- 29.National Athletic Trainers' Association. Athletic Training Educational Competencies. 4th ed. Dallas, TX: National Athletic Trainers' Association; 2006. [Google Scholar]
- 30.Walker S. E., Weidner T. G., Armstrong K. J. Evaluation of athletic training students' clinical proficiencies. J Athl Train. 2008;43(4):386–395. doi: 10.4085/1062-6050-43.4.386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Weidner T. G., Noble G. L., Pipkin J. B. Athletic training students in the college/university setting and the scope of clinical education. J Athl Train. 2006;41(4):422–426. [PMC free article] [PubMed] [Google Scholar]
- 32.Fiala K. A. A Comparison of Characteristics and Responses for Non-Responding and Responding Certified Athletic Trainers to Mail and Web-Based Surveys on Continuing Education [doctoral dissertation] Storrs: University of Connecticut; 2004. [Google Scholar]
- 33.Mazerolle S. M., Yeargin S. W., Casa T. M., Casa D. J. Heat and hydration curriculum issues: part 3 of 4, rectal thermometry. Athl Ther Today. 2009;14(4):25–31. [Google Scholar]
- 34.Mazerolle S. M., Casa T. M., Casa D. J., Lopez R. L. Heat and hydration curriculum issues: part 4 of 4, cold water immersion. Athl Ther Today. 2009;14(5):15–20. [Google Scholar]