Parent training has become a major focus of intervention efforts aimed at preventing or reducing conduct problems (including physically aggressive behavior) and preventing violence among children through the reduction of maladaptive parenting behaviors and an increase in the use of positive parenting strategies (Bor, Sanders, & Markie-Dadds, 2002; Brestan & Eyberg, 1998; Gross et al., 2003; Redmond & Shin, 1998; Reid, Webster-Stratton, & Baybar, 2004; Sanders, 1999; Sanders, Markie-Dadds, Tully, & Bor, 2000a; Sanders, Turner, & Markie-Dadds, 2002; Spoth, Redmond, & Shin, 1998; Taylor & Biglan, 1998; Webster-Stratton & Reid, 2003a; Webster-Stratton & Reid, 2003b; Webster-Stratton, Reid, & Hammond, 2001; Webster-Stratton & Taylor, 2001). Parenting interventions that include language promotion activities as well as parenting skills training may yield the most effective strategies for the prevention or reduction of physical aggression (Arnold, Lonigan, Whitehurst, & Epstein, 1994), through direct effects on physical aggression and indirect effects on physical aggression that are mediated by improved verbal abilities.
Deciding when to implement intervention programs so that they are successful is a challenging task, but crucial if we are to prevent individuals from developing into life-course persistent offenders (Moffitt, 1993; Moffitt, Caspi, Dickson, Silva, & Stanton, 1996). Evidence is accumulating that persistent physical aggression leading to adolescent and adult violence develops prior to a child entering school and that the best time to intervene is prior to age 8, before these behaviors become ingrained (Brestan & Eyberg, 1998; Gross et al., 2003; Moffitt, 1993; Reid et al., 2004; Spoth et al., 1998; Taylor & Biglan, 1998; Webster-Stratton & Reid, 2003a; Webster-Stratton & Taylor, 2001; Webster-Stratton et al., 2001;Yoshikawa, 1994). Tremblay (2000) posits that parent training programs during the preschool years which address discipline issues, use of physical punishment, and the regulation of physical aggression help prevent the trajectory towards further behavioral problems such as delinquency, truancy, and adolescent violence.
One challenge to implementing prevention/intervention programs is determining the format for delivering the intervention: group-based versus home-based programs or a combination of these two approaches. The majority of parent training programs are group-based. Brestan & Eyberg (1998) note in their review of 82 studies on psychosocial treatments for conduct disordered children that only 11% of the interventions took place in the home and over ½ were conducted in a group format. Sanders et al. have developed a group-based, comprehensive behavioral family intervention aimed at preventing severe behavioral and emotional disturbances in children through parenting skills training, improving parents’ sense of their competency regarding their parenting abilities, increasing parents’ communication about parenting issues, and reducing parenting stress (Sanders et al., 2002). This program, known as the Triple P-Positive Parenting Program, has been tested in a wide variety of settings with sample sizes ranging from 16–1615 (Sanders et al., 2002). A unique feature of the Triple P program is the multilevel concentration of the intervention. The intensity level of the intervention can be tailored to meet the needs of the child and family. This program has demonstrated consistent, sustained effects on reductions in children’s disruptive behaviors and increased parental confidence over time and across the age continuum from birth through age 12 years (Sanders et al., 2002).
The Incredible Years program is a comprehensive, multi-faceted, developmentally-based preventive intervention, delivered in a group setting, which contains training components for parents, teachers, and children (Webster-Stratton, 1998). This program has been identified as one of 11 model programs under the Blueprints for Violence Prevention initiative (http://www.colorado.edu/cspv/blueprints/model/overview.html). The parent training program focuses on teaching effective parenting skills, positive discipline strategies, and methods for parents to enhance their children’s social skills, emotional language building, and prosocial behaviors. The teacher training components are designed to reinforce the parent program as well as provide effective strategies for promoting social competence and managing misbehavior in the classroom. The child training program emphasizes skill-building in emotional literacy, empathy, anger management, and inter-personal problem-solving (Webster-Stratton, 1998; Bauer & Webster-Stratton, 2006). This program has demonstrated sustained long-term outcomes in families of children ages 2–10 who are at risk for conduct problems (http://www.colorado.edu/cspv/blueprints/model/overview.html).
While these two group-based parent training programs have demonstrated positive outcomes for parents and children, delivering the training program in the home may be more advantageous in that the parents do not have to arrange for transportation, child care or even time off from work which may improve retention in the program. Home visiting programs for first-time parents have garnered attention as effective parent training strategies which impact a host of parent and child outcomes (McNaughton, 2004; Kearney, York, & Deatrick, 2000; Austin & Lemon, 2005; Fetrick, Christensen, & Mitchell, 2003; Olds, Sadler, & Kitzman, 2007) and these programs are typically targeted to those parents at highest risk for poor outcomes. “Bringing the intervention into the home also provides opportunity for more whole family involvement, personalized service, individual attention, and rapport building” (Sweet & Applebaum, 2004, pg. 1435). A meta-analysis on the effectiveness of home visiting programs revealed that families who were targeted as being “at-risk”, visited by professionals, and who had a larger number of visits over a longer period of time demonstrated greater improvements in child cognition and child abuse outcomes (Sweet & Applebaum, 2004).
The Nurse-Family Partnership (NFP), an intensive nurse-home visiting program, targets first-time, low income mothers and begins during pregnancy and continues until the child is two years old. The NFP has demonstrated consistent program effects on parenting behaviors and children’s verbal ability, cognition, and executive function (Kitzman et al., 1997; Kitzman et al., 2000; Olds, Henderson, Tatelbaum, & Chamberlin, 1988; Olds et al., 2004a; Olds et al., 2002; Olds et al., 2004b). The NFP is one of 11 programs identified by the Center for the Study and Prevention of Violence as a model program in its Blueprints for Violence Prevention initiative (http://www.colorado.edu/cspv/blueprints/model/overview.html). Results from a 15 year follow-up of adolescents from the Elmira NFP trial revealed that there was a 59% reduction in arrests and a 90% reduction in adjudications as PINS (person in need of supervision) among the nurse-visited group (Olds et al., 1998), outcomes linked to early aggressive behavior during childhood (Broidy et al., 2003; Fergusson & Horwood, 2002; Moffitt & Caspi, 2001; Moffitt, Caspi, Rutter & Silva, 2001; Moffitt et al., 1996; Nagin & Tremblay, 1999, 2001; Reis & Roth, 1993; Tremblay, 2000; 2004).
Differential Effects of Intervention
Studies have shown that males consistently have higher rates of physically aggressive behaviors than females from early childhood to adolescence (Broidy et al., 2003), with early childhood-onset (prior to adolescence) physical aggression having a 10:1 male to female ratio (Moffitt, 1993; Moffitt et al., 2001; Moffitt et al., 1996). Moffitt et al., (2001) found that males scored significantly higher than females on every measure of physically aggressive or violent behavior between ages 5 and 21. Given these gender differences in physically aggressive behavior, surprisingly, few studies were found which examined the effectiveness of prevention/intervention programs for conduct disorder and aggression by gender, which begs the question, why not? In fact, our original analyses of the NFP revealed that the intervention did not significantly impact overall externalizing behaviors in either the Memphis or Denver trials at ages 2 and 4 years (Kitzman et al., 1997; Kitzman et al., 2000; Olds et al., 2002; Olds et al., 2004b). However, neither gender effects nor the subset of physically aggressive behaviors were examined. Webster-Stratton (1996), in her study of the predictors of treatment outcomes by gender, found that while externalizing behavior, as reported by mothers and teachers, differed by gender at baseline (males exhibited higher levels of hostile-aggressive behaviors than females), male and female responses to the intervention were very similar. Both groups demonstrated significant reductions in aggressive behavior and these results remained stable at 1 and 2 year follow-up assessments. Williams and colleagues (2004) found no gender differences in the treatment effects of a children’s temper-taming program, however, there were only 12 females included in the final sample of 56 children (Williams, Waymouth, Lipman, Mills, & Evans, 2004). Among a sample of adolescents (N=61, 34 males and 27 females), Campbell (2005) demonstrated that while males and females presented with similar symptoms and underlying difficulties upon entry to treatment, the females exhibited significantly more improvements due to treatment than the males. Given the few studies found which examined intervention effects by gender and the known developmental differences which exist in physical aggression between males and females, Webster-Stratton summarizes by stating “it is time to remedy this gap in the research to determine whether there are different behavioral symptoms, developmental pathways, etiological factors, and treatment outcomes for girls and boys” (1996, p. 541).
This study builds on our previous analyses of the control group from the Memphis NFP trial which demonstrated gender differences in the relationship between verbal ability and physical aggression (Anson, Sidora-Arcoleo, Cole, Kitzman, & Olds, 2007) by examining the differential effects of the NFP on verbal ability and the development of physically aggressive behavior in children from 2 through 12 years.
Theoretical Framework for Analytical Model
The theoretical framework used for the secondary analyses is known as the “language-aggression hypothesis”. Boone & Montare (1976) devised the language-aggression hypothesis which states that language is inversely related to aggression: low levels of language proficiency are associated with high levels of aggressive behavior. The language-aggression hypothesis was derived from Pavlov’s excitation-inhibition model. In this model, “it is proposed that excitatory and inhibitory processes operate on abstract language processes to direct and control behavioral activities” (Pavlov, 1927, 1955, as cited in Boone & Montare, 1976, p 851). The language-aggression hypothesis is theoretically centered on the premise that higher language proficiency leads to greater control of aggressive impulses, leading to a reduction in aggressive behavior. Many researchers have shown a link between language and aggressive behavior across the age continuum (Estrem, 2001; Dionne et al., 2003; Cohen et al., 1993; Gualtieri, et al., 1982; Stowe, Arnold & Ortiz, 2000; Cook, Greenberg & Kusche, 1994; Mack & Warr-Leeper, 1992; Cohen et al., 1993; Beitchman et al., 1985; Stevenson & Richman, 1978; Stattin & Klackenberg, 1993).
Dionne and colleagues posit that this language-aggression association usually falls under two developmental models. (Dionne, 2005; Dionne, et al., 2003). The first model, referred to as the shared etiological model, suggests that aggression and language problems share similar origins, including either biological origins or shared environmental origins (e.g., harsh, restrictive parenting and poverty). The second model focuses on a causal pathway from low language proficiency to increased aggression. It is theorized that children with language deficits may have difficultly with negotiation and problem-solving skills. Children with limited communication skills may be more easily frustrated and thus, social interactions may present more conflict episodes (Dionne, 2005).
Utilizing the language-aggression hypothesis, the specific study questions examined were:
Was the nurse home visiting intervention effective in reducing physically aggressive behaviors through age 12 years?
Did the intervention effects on the development of physical aggression over time differ by gender?
Did maternal psychological resources mediate the relationship between the intervention and physical aggression?
Were the effects of the intervention on physical aggression mediated by children’s verbal ability?
Methods
Design
The data for these secondary analyses were derived from a longitudinal randomized, controlled trial evaluating the impact of a nurse home visiting intervention (NFP) on pregnancy outcomes, parenting, and a wide array of maternal and child life course outcomes. A full description of the study design has been reported earlier but is summarized here (Kitzman et al, 1997). Office and home interviews and assessments were conducted at registration and post-partum when the target child was 6 months old, and 1, 2, 4, 6, 9 and 12 years of age. Data from the 2, 6, and 12 year assessment periods were used for these analyses since these were the only time periods when verbal ability and/or physical aggression was assessed. Data collection for the 12 year assessment period was conducted from 7/03–3/06. All women randomized to the post-partum intervention groups and who had a live birth were included in these analyses (N=721); 22 women did not have live births.
Sample
Women less than 29 weeks pregnant were recruited from the obstetrical clinic at the Regional Medical Center in Memphis, Tennessee if they had no previous live births, no specific chronic illnesses thought to contribute to fetal growth retardation or preterm delivery, and at least 2 of the following sociodemographic risk conditions: unmarried, less than 12 years of education, and unemployed. All women who were enrolled signed consent forms approved by the Research Subjects Review Board at The University of Rochester and the University of Tennessee.
Intervention Groups
Women were randomized to intervention groups by a computer program using methods that are extensions of those given by Soares and Wu (Soares & Wu, 1983). Randomization was conducted within strata from a model with 5 classification factors: maternal race, maternal age, gestational age at enrollment, head of household employment status, and geographic region of residence. Women assigned to the home visitation groups were subsequently randomly assigned to a nurse home visitor.
Women in intervention group 1 (N=166) were provided free-roundtrip taxicab transportation for scheduled prenatal care appointments; they did not receive any postpartum services or assessments. Women in intervention group 2 (N=515) were provided free transportation for scheduled prenatal care and developmental screening and referral services for the child at ages 6, 12, and 24 months. Women in intervention group 3 (N=230) were provided the free transportation and screening services offered in group 2 and also intensive nurse home visitation services during pregnancy, 1 postpartum visit in the hospital before discharge, and 1 postpartum visit in the home. Women in intervention group 4 (N=228) were provided the same services as those in group 3 but also were visited by nurses until the child’s second birthday. For the evaluation of postnatal outcomes, intervention group 2 was contrasted with intervention group 4, since only these groups were assessed after delivery of the child.
Nurse Home Visiting Intervention
The experimental home visitation program was carried out by the Memphis/Shelby County Health Department. The nurses completed an average of 7 home visits (range 0–18) during pregnancy and 26 home visits (range 0–71) during the first 2 years postpartum. The nurses followed a detailed visit-by-visit protocol to help women improve their health-related behaviors, care of their children, and life-course development (pregnancy planning, educational achievement, and participation in the workforce). The postpartum program protocols focused on helping mothers and other caregivers improve the physical and emotional care of their children. Specific curricula were integrated into the program to promote parent-child interaction by facilitating parents’ understanding of their infants’ and toddlers’ communicative signals (NCAST, 1994; Sumner, Barnard, Johnson-Crowley, & Spietz, 1990) and enhancing interest in playing with their children in ways that promoted emotional and cognitive development (Sparling & Lewis, 1984). A more detailed description of the nurse home visitation program can be found in Kitzman et al. (1997).
Measures
Mediating Variable
Maternal Psychological Resources
A variable was created to index women’s psychological resources measured at registration. It was based upon the mean z-scores of their intelligence (Shipley, 1940), mental health (Ware, Veit, & Donald, 1985), sense of mastery (Pearlin & Schooler, 1967), plus self-efficacy (Bandura, 1977). Unpublished confirmatory factor analysis showed that the 4 components of the psychological resources variable form a single latent variable (α= 0.61). The psychological resource variable was standardized to a mean of 100 and standard deviation of 10 and then dichotomized at values ≤100 vs. >100, creating a median split. The dichotomous variable was created because in our previous analyses where maternal psychological resources was analyzed as a continuous variable, it was found that treatment differences occurred in the tails of the distribution. Thus, for ease of examination of interaction effects and interpretation of results, this classification variable based on a median split was used.
Covariates
Household Poverty
A single index of household poverty at registration was created based upon the averaged z-scores of the following variables: household discretionary income, whether the head of the household was employed, and household density (number of persons per room), standardized to a mean of 100 and a standard deviation of 10. It also formed a single latent variable (α= 0.54). This variable is included as a covariate in the analytical models because there were baseline differences between the intervention groups.
Negative Parenting Attitudes
At intake, mothers completed the Adult-Adolescent Parenting Inventory (Bavolek, 1984), a measure of parenting attitudes that indicate a high-risk for child maltreatment. The four scales derived from this measure are: parental lack of empathy, role reversal, unrealistic expectations for the child and a belief in physical punishment. Higher scores are indicative of negative parenting attitudes. This instrument has been widely utilized in a variety of settings and demonstrated good psychometric properties in this sample (α=.91). This variable is included as a covariate in the analytical models because previous research has demonstrated that harsh, restrictive parenting leads to increased aggressive behavior among children (Coté, Vaillancourt, LeBlanc, Nagin, & Tremblay, 2006; Loeber et al., 2005; Reid et al., 2004, Taylor & Biglan, 1998) and this was a targeted outcome of the intervention that we wanted to control for.
Dependent Variables
Child’s Verbal Ability – Age 2
The Mental Development Index (MDI) from the Bayley Scales of Infant Development (BSID) (Bayley, 1993) was used as a proxy for verbal ability at age 2 since we had no direct assessment of verbal ability at this age. The BSID measures the developmental functioning of infants ages 1 to 42 months and yields a mental development index (MDI) and a motor scale. The MDI measures a variety of abilities including vocalization and verbal communication, memory, sensory-perceptual acuities and discrimination, object constancy, learning and problem-solving abilities. Higher scores indicate better functioning. While the MDI subscale of the BSID is an overall measure of infant cognitive development and not a direct assessment of verbal ability, other researchers have shown significant correlations between the BSID and various language assessments during infancy and toddlerhood (Costarides & Shulman, 1998; Molfese & Acheson, 1997; Siegal, Cooper, Fitzhardinge, & Ash 1995). Scores on the MDI are standardized to M = 100 and SD = 15.
Child’s Verbal ability – Age 6
The Peabody Picture Vocabulary Test – Revised (PPVT-R; Dunn & Dunn, 1981) was used to assess verbal ability at age 6. The PPVT-R measures a child’s receptive vocabulary and is used as a screening tool for verbal ability. Higher scores indicate better verbal ability. Scores on the PPVT-R are standardized (M = 100, SD = 15), have large normative data sample, and demonstrate adequate reliability and validity (Dunn & Dunn, 1981).
Physical Aggression – Age 2
Three items from the aggression subscale of the Child Behavior Checklist (CBCL, ages 2–3; Achenbach, 1992) were selected as the measure of physical aggression: “physically attacks others;” “hits others;” and “gets into fights,” consistent with previous research (Broidy et al., 2003; Tremblay & Nagin, 1999). For each behavior, mothers were asked to think about the past 6 months and report how true or untrue each statement was about her child with response choices consisting of: 0 (not true), 1 (somewhat or sometimes true), and 2 (very true or often true). A latent variable for age 2 physical aggression was estimated as the shared variance among these three indicators. Standardized loadings ranged from .60 to .70, ps < .01.
Physical Aggression - Ages 6 and 12
Items from the CBCL (ages 4–16; Achenbach, 1991) aggression subscale were used as the measure of physical aggression at ages 6 and 12 years. “Physically attacks others” and “gets into many fights” were used for the measure of physical aggression, similar with the age 2 measure of physical aggression. The item “hits others” was not included in the CBCL for this age group. Latent variables for physical aggression at 6 and 12 years were estimated as the shared variance among these two indicators at each age. Standardized loadings ranged from .64 to .67 at age 6 and from .57 to .64 at age 12, ps < .01.
Statistical Analysis
All women randomized to intervention group (excluding cases where a miscarriage, abortion or stillbirth occurred) were included in these analyses. Descriptive statistics were computed for all study variables. Structural equation modeling was used to examine the influence of the intervention on children’s verbal ability and physically aggressive behaviors. Analyses were conducted simultaneously for all verbal ability and aggression measures. Research questions 1–3 were tested in four primary models, respectively focusing on: (1) intervention main effects, (2) intervention X child gender effects, (3) intervention X maternal psychological resources effects, and (4) intervention x gender x maternal psychological resources effects. Significant interactions were further probed to determine the nature of the interactions.
Mediation analyses (research question 4) were conducted independently for each outcome. Mediation tests examine whether the relationship between a predictor (X) and criterion (Y) can be explained by the effect of X on an interceding variable, the mediator (M). Mediation is tested through first showing that X (e.g., intervention) is associated with both M (e.g., verbal ability) and Y (e.g., physical aggression). Second, a path model is estimated by simultaneously regressing (a) Y on M and X, and (b) M on X. Mackinnon, Lockwood, Hoffman, West, and Sheets (2002) suggest that two criteria be met when using such tests for mediation in intervention research. The first criterion, known as the joint test, requires statistically significant paths from intervention to mediator and mediator to outcome. The second criterion is a statistically significant result of a test that takes each of these paths into account simultaneously, such as the asymmetric confidence limits test. Accordingly, both joint tests and asymmetric confidence limits tests were used for all tests of mediation.
Due to the skewed distributions for the physical aggression variables, two steps were taken in order to guard against misleading results due to violated statistical assumptions. First, all hypothesis tests were evaluated with adjusted standard errors and model fit indices computed using the Robust Maximum Likelihood (MLR) estimation method in Mplus version 4.0 (Muthén & Muthén, 2006). Second, we ran parallel analyses using bias-corrected bootstrapped estimates, which yielded highly similar results to the robust estimation method (available from the first author). Due to the exploratory nature of these simultaneous equations models, a p-value of .10 was selected as the cut-off for determining statistical significance.
Following conventions outlined by Kline (1998), Byrne (2001), and Cudeck & Browne (1993), our criteria for assessing adequacy of fit were as follows: χ2 to df ratio of less than 2, comparative fit index (CFI) and Tucker-Lewis Index (TLI) at or above .90, and a root mean square error approximation (RMSEA) at or below .08. All models comfortably exceeded the fit criteria and specific fit index values are available from the first author upon request.
Results
Background characteristics of the sample at randomization are presented in Table 1. The intervention groups were equivalent on background characteristics with one exception: the composite household poverty variable. Women in the nurse-visited group resided in households with higher poverty. Therefore, as stated previously, this variable was included as a covariate in the model.
Table 1.
Background Characteristics of Sample at Randomization
| Treatment Group |
||
|---|---|---|
| Comparison | Nurse-visited | |
| % | % | |
| African-American | 92 | 89 |
| Married | 2 | 1 |
| % Male Children | 50 | 51 |
| Low Psychological Resources | 51 | 55 |
| Mean (SD) | Mean (SD) | |
|---|---|---|
| Age | 18.1 (3.2) | 18.1 (3.3) |
| Education (yrs. completed) | 10.3 (1.9) | 10.1 (2.0) |
| % Census tract below poverty | 34.5 (21.3) | 35.8 (20.5) |
| Household poverty | 99.5 (10.1) | 101.9 (10.0) |
| Negative Parenting Beliefs | 99.8 (7.6) | 100.7 (8.5) |
Model 1: Main Effects of Intervention
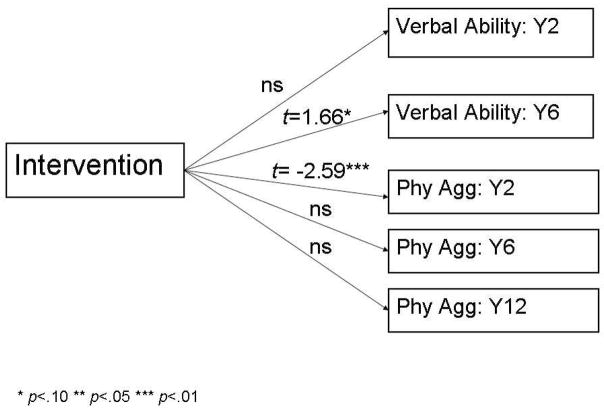
Figure 1 presents the results for the simultaneous equation model for the main effects of nurse home visitation on verbal ability and physical aggression measures, controlling for household poverty and negative parenting beliefs. There were no statistically significant effects of the intervention on cognitive development at age 2, but at age 6, there was a trend towards significance with the nurse-visited children demonstrating higher MDI scores than the comparison group children (t=1.66, p<.10). Additionally, nurse-visited children exhibited significantly lower physical aggression scores at age 2 than their comparison group counterparts (t=−2.59, p<.01). This finding, however, was attenuated by ages 6 and 12 years.
Figure 1.
Model 1- Main effects of intervention
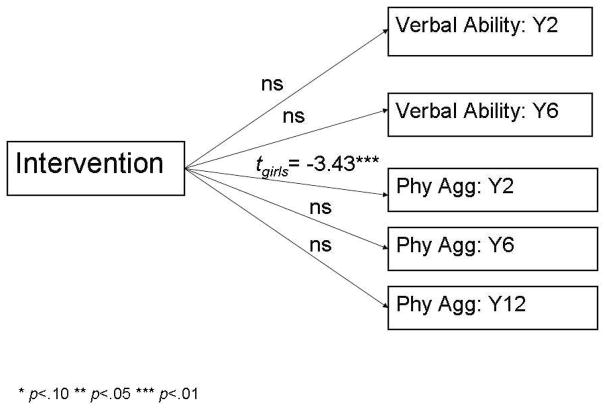
Model 2: Intervention x Gender Effects
Model 2 built on Model 1 by testing whether the effects of nurse home visitation differed for males and females. Gender and the interaction of intervention x gender were added as predictors of verbal ability and physical aggression (Figure 2). By and large, intervention effects did not significantly interact by child gender. The sole exception involved age 2 aggression, for which the intervention X gender interaction term was marginally significant (t=1.95, p < .10, not shown). Follow-up analyses of this interaction revealed that nurse home visitation significantly protected against age 2 aggression in females (t = −3.43, p < .01), but not males (t = −0.23, n.s.). As in Model 1, however, a significant reduction in aggression linked to nurse home visitation was not evident at ages 6 and 12 years for either gender.
Figure 2.
Model 2- Intervention x Gender
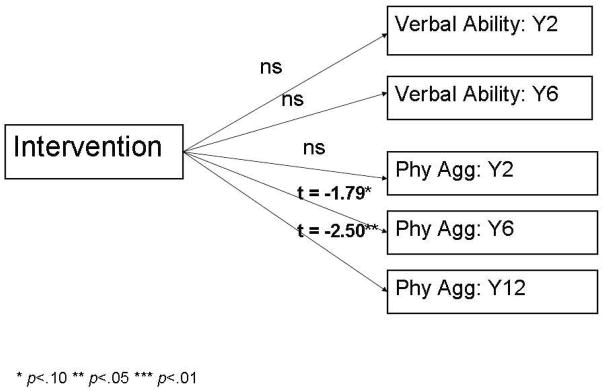
Model 3: Intervention x Maternal Psychological Resources
Model 3 also built on Model 1 by testing whether the effects of nurse home visitation differed for children of high vs. low psychological resource mothers. Maternal psychological resources and the interaction of intervention x maternal psychological resources were added as predictors of verbal ability and physical aggression (Figure 3). There were no statistically significant interactions of intervention x maternal psychological in predicting verbal ability at ages 2 or 6, or physical aggression at 2 years of age. By age 6, however, the intervention x maternal psychological resources interaction on physical aggression was significant (t=−2.49, p<.05, not shown) and was sustained through age 12 (t=−2.35, p<.05, not shown). Probing the interaction effect further, children of nurse-visited, high psychological resource mothers demonstrated significantly lower physical aggression scores compared to children of high psychological resource control mothers (age 6 years t = −1.79, p<.10 and age 12 years t = −2.50, p<.05). In contrast, the intervention had no significant effect on aggression among 6 and 12-year-old children of low psychological resource mothers.
Figure 3.
Model 3- Intervention x Psychological Resources
Model 4: Intervention x Gender x Maternal Psychological Resources
The presence of 2-way interactions of child gender and maternal psychological resources with intervention suggested the possibility of three-way interactions. Model 4 added gender and intervention x gender terms to Model 3, which enabled the testing of the three-way interaction involving intervention X gender x maternal psychological resources. There were no significant 3-way interactions in the prediction of verbal ability and physically aggressive behavior.
Mediated Effects of Intervention
It was hypothesized that the effects of nurse home visitation on child aggression would be mediated by the effect of nurse home visitation on child verbal ability. So as not to violate the temporal precedence criterion in establishing causality, this pattern of mediation was only evaluated for cases in which a measure of the child’s verbal ability was assessed at the same time as or before the measure of the child’s physical aggression. Mediation models were tested controlling for the possible effects of household poverty and negative parenting beliefs on both the mediator and outcome. Based on the results of Models 1 through 4, and their associated follow-up tests, we further restricted our analyses to the subgroup of the sample in which intervention effects on physical aggression were concentrated: 2-year-old females.
The hypothesized intervention→verbal ability→aggression mediated effect was not supported by the data. In the case of 2-year-old females’ physical aggression, the joint significance test criterion was not met because the intervention had no significant effect on age 2 verbal ability (t = 0.715).
An alternate direction of mediation was suggested by the data. There was a significant intervention effect on physical aggression at age 2 and a marginal effect on verbal ability at age 6 (see Figure 1). Accordingly, it seemed possible that the effect of nurse home visiting on age 6 verbal ability was mediated by the effect on toddler aggression. Tests of this alternate direction of mediation were limited to females, since the protective effect of nurse home visitation on age 2 physical aggression was concentrated in females. The joint significance criterion was met.
The path from intervention to age 2 aggression (t = −3.149, p < .01) was significant; the path from age 2 aggression to age 6 verbal ability was marginally significant (t = −1.826) (Figure 4). Moreover, the asymmetric 95% confidence interval around the unstandardized estimate of the indirect (i.e., mediated) effect of 0.301 did not include zero (95% CI=0.001, 0.786). Finally, the effect of nurse home visitation on age 6 verbal ability dropped to a non-significant level (t = 0.661), controlling for age 2 physical aggression. Thus, the positive effect of nurse home visitation on females’ verbal ability at age 6 appeared to have been mediated by a protective effect on their physical aggression at age 2.
Figure 4.
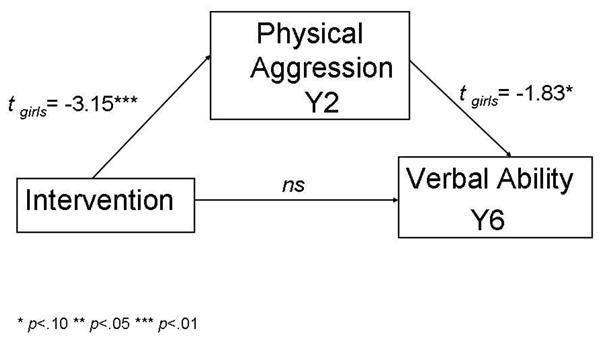
Mediational effects -alternative hypothesis
Discussion
Many of the effective parenting programs are based on social learning theories which stress the role that parenting style and discipline strategies play in shaping children’s social competence and reducing conduct problems such as physically aggressive behavior. Few studies found during the literature review examined the effectiveness of prevention/intervention programs for physical aggression by gender (or other sub-groups) or whether the observed effects were sustained over time. The findings from this study add to the literature in several important areas. While our previous analyses revealed no intervention effects when the general constellation of externalizing behaviors was examined, these analyses demonstrated that the nurse home visiting intervention significantly reduced the subset of physically aggressive behaviors among 2-year old children. Subsequent analyses demonstrated a differential impact of the nurse home visitation intervention by gender and mother’s psychological resources with the program’s effects concentrated among females and children of high psychological resource mothers. The nurse home visiting intervention successfully interrupted the early development of physically aggressive behavior in females, however, by age 6 and through age 12, the intervention effects were attenuated. In light of the fact that both intervention groups demonstrated decreases in physically aggressive behavior over time and were equivalent by 6 years of age, some might question the necessity of the intervention in the first place if, over time, the children ultimately end up in the same place. Our response to this challenge would be that the nurse-visited females exhibited a significantly lower peak value for physical aggression than the comparison group females at age 2 which may have inhibited the development of many of the negative outcomes which have been associated with early conduct problems (e.g., violence, school failure, substance abuse, and delinquency) (Webster-Stratton & Taylor, 2001) placing the nurse visited females on a different trajectory. Subsequent analyses are planned to examine these trajectories of physical aggression and their relationship to children’s academic and behavioral outcomes.
The lack of intervention impact among the males was unexpected. The results of these analyses suggest etiological factors other than verbal ability may be important in the prediction of physically aggressive behavior among males. Previous research has suggested that maternal characteristics (e.g., depression, harsh parenting) are important predictors of physical aggression among females (Keenan & Shaw, 1994, Webster-Stratton, 1996) while difficult temperament and non-compliance are key predictors for males (Keenan & Shaw, 1994), thus potentially requiring modification of current intervention programs. It may be that “one intervention does not fit all.”
Another key finding was that the nurse home visiting intervention had a significant and sustained impact on physically aggressive behaviors from age 6 through 12 years among children of mothers with high psychological resources. In previous publications (Kitzman et al., 1997; Kitzman et al., 2000; Olds et al, 2004a; Olds et al., 2002; Olds et al., 2004b), we demonstrated impacts on children’s cognitive and language development which we hypothesized to be a result of improvements in parental caregiving (e.g., quality of the home environment, reduction in harsh parenting beliefs) and maternal life course (e.g., increased birth interval between first and second child, less reliance on welfare). We theorize that these high psychological resource mothers were better able to handle the demands involved in providing sustained, competent care of their children due to the improvements noted above.
An interesting finding was that the verbal ability→aggression hypothesis was not supported by these data for either gender. An alternative hypothesis was tested based on Patterson’s theory of coercion (Patterson, DeBaryshe, & Ramsey, 1989) which was supported by our data for females. These findings suggest that the nurse home visiting intervention worked by reducing physical aggression at age 2 and this reduction in physical aggression led to increased verbal ability scores at age 6. Dionne (2005) posits that children’s disruptive behavior may interfere with linguistic stimulation creating language deficits. She states, however, that overt aggression is rarely assessed at the same time as, or prior to, language development indicating that we cannot rule out this pathway of influence.
Given these findings, additional analyses are planned utilizing more complex models which will include the known predictors for males and females in order to better understand whether there are different etiological pathways by gender which lead to physically aggressive behavior.
There are several limitations to these analyses. Due to the fact that these were secondary analyses and we did not have a specific verbal ability measure at 2 years, we used the Bayley Mental Developmental Index (Bayley 1993), a broader cognitive measure. It’s possible that since this measure included memory, sensory-perceptual acuities and discrimination, object constancy, learning and problem-solving abilities (in addition to vocalization and verbal communication) that any specific impact on verbal ability may have been masked. Another limitation concerns our measure of physically aggressive behaviors. There were three items that assessed physical aggression age at 2 but only two of these items were included in the 6 and 12 year CBCL. We ran the analyses using all three indicators at age 2 and then removed “Hits others” so that all three time periods had the same items as indicators of physical aggression and the results were essentially unchanged. Maternal reports were used to obtain assessments of children’s behavior. We did obtain CBCL data from children’s teachers at age 12 years but did not have corresponding measurements at the earlier data gathering periods to corroborate mothers’ reports and, therefore, were not able to include these data (another limitation of secondary data analyses). Previous research has demonstrated that parent’s reports of their children’s aggressive behavior are reliable and valid (Kingston & Prior, 1995; Soussignan et al., 1992).
These limitations notwithstanding, this study has highlighted the importance of examining various pathways for the development of physically aggressive behavior in children and suggests that these pathways may differ by gender and other maternal or child characteristics. It is critical that gender is included in future analytical models examining intervention effects on physically aggressive behavior. Had we just limited our analyses to intervention x time effects, we would have missed the fact that all of the program effects were concentrated among the females.
Future research efforts should focus on analyzing more complex models which include previously identified predictors and potentially important subgroups. Gaining a better understanding of differing etiological pathways and responses to prevention and intervention programs will allow us to tailor these interventions to improve effectiveness.
Implications for Nursing Practice
The findings from this study can help nurses working with mothers understand the developmental differences in physical aggression between males and females and that the effectiveness of education and intervention strategies may differ by child’s gender. Nurses who provide well-child care are in a position to screen and identify children and families who may be at risk for conduct problems and provide referral to a parenting skills training program, if available in the community in which the family lives. Even if no formal program exists, nurses can incorporate several key components of these parenting skills training programs in their face-to-face contacts with families. Teaching parents the use of positive discipline strategies (e.g., use of time out instead of spanking) and how to interact with their child in ways that promote the child’s social and emotional development will lead to positive sociobehavioral outcomes for the child. By providing parents these skills, nurses can enhance parents’ confidence in their ability to parent their child in ways that promote optimal social, emotional, and behavioral development.
Acknowledgments
Funding Support: The earlier phases of this research were supported by 5 federal agencies: The National Institute of Nursing Research (NR01-01691-05), the Bureau of Maternal and Child Health (MCJ 360579), the Administration for Children and Families (90PJ0003), the Office of the Assistant Secretary for Planning and Evaluation (Department of Health and Human Services), and the National Center for Child Abuse and Neglect, through a transfer of funds to the National Institute of Nursing Research. Support was also received from the 4 following private foundations: the Robert Wood Johnson Foundation (017934 and 11084); the Carnegie Corporation of New York (B5492); the Pew Charitable Trusts (88-0211-000 and 93-02363-000); and the William T. Grant Foundation (88-1246-88 and 91-1246-88). The six year phase of this research was supported by the Administration for Children and Families, Department of Health and Human Services (90PD0215/01), the Hearst Foundation, the Robert Wood Johnson Foundation (027901), and a Senior Research Scientist Award to Dr. David Olds (1-K05-MH01382-01).
Footnotes
Prior Presentation: The results of this manuscript were presented at the annual American Public Health Association Meeting on November 7, 2007 in Washington, DC.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Kimberly Sidora-Arcoleo, Arizona State University College of Nursing & Healthcare Innovation, Phoenix, Arizona.
Elizabeth Anson, Email: elizabeth_anson@urmc.rochester.edu, University of Rochester School of Nursing, Rochester, New York.
Michael Lorber, Email: mlorber@scrippscollege.edu, Scripps College, Claremont, California.
Robert Cole, Email: robert_cole@urmc.rochester.edu, University of Rochester School of Nursing, Rochester, New York.
David Olds, Email: david.olds@uchsc.edu, University of Colorado Department of Pediatrics, Denver, Colorado.
Harriet Kitzman, Email: harriet_kitzman@urmc.rochester.edu, University of Rochester School of Nursing and Department of Pediatrics, Rochester, New York.
References
- Achenbach T. Manual for the Child Behavior Checklist/2–3 and 1992 Profile. Burlington, VT: University of Vermont Department of Psychiatry; 1992. [Google Scholar]
- Anson E, Sidora-Arcoleo K, Cole R, Kitzman H, Olds DL. Development of physical aggression: exploring the relationship with language. Journal of Pediatric Nursing. 2007 (Under review) [Google Scholar]
- Arnold DH, Lonigan CJ, Whitehurst GJ, Epstein JN. Accelerating language development through picture book reading: replication and extension to a videotape training format. Journal of Educational Psychology. 1994;86:235–243. [Google Scholar]
- Austin MJ, Lemon K. Promising programs to serve low-income families in poverty neighborhoods. Journal of Health & Social Policy. 2005;21:65–94. doi: 10.1300/j045v21n01_03. [DOI] [PubMed] [Google Scholar]
- Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychology Review. 1977;84:191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- Bauer NS, Webster-Stratton C. Prevention of behavioral disorders in primary care. Current Opinion in Pediatrics. 2006;18:654–660. doi: 10.1097/MOP.0b013e3280106239. [DOI] [PubMed] [Google Scholar]
- Bavolek SJ. Handbook for the AAPI: Adult-Adolescent Parenting Inventory. Eau Claire, Wisconsin: Family Development Resources, Inc; 1984. [Google Scholar]
- Bayley N. Bayley scales of infant development. 2. San Antonio, TX: The Psychological Corporation, Harcourt Brace; 1993. [Google Scholar]
- Bor W, Sanders MR, Markie-Dadds C. The effects of the Triple P-Positive Parenting program on preschool children with co-occurring disruptive behavior and attentional/hyperactive difficulties. Journal of Abnormal Child Psychology. 2002;30:571–587. doi: 10.1023/a:1020807613155. [DOI] [PubMed] [Google Scholar]
- Brestan EV, Eyberg SM. Effective psychosocial treatments of conduct-disordered children and adolescents: 29 years, 82 studies, and 5,272 kids. Journal of Clinical Child Psychology. 1998;27:180–189. doi: 10.1207/s15374424jccp2702_5. [DOI] [PubMed] [Google Scholar]
- Broidy LM, Tremblay RE, Brame B, Fergusson D, Horwood JL, Laird R, et al. Developmental trajectories of childhood disruptive behaviors and adolescent delinquency: A six-site, cross-national study. Developmental Psychology. 2003;39 (2):222–245. doi: 10.1037//0012-1649.39.2.222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Byrne BM. Structural equation modeling with AMOS: basic concepts, applications, and programming. Mahwah, NJ: Lawrence Erlbaum Associates; 2001. [Google Scholar]
- Campbell A. Gender differences in adolescents with disruptive behavior disorders: a look at self-report, projective, and treatment outcome measures. (Doctoral dissertation, University of Tennessee, 2005) Dissertation Abstracts International: Section B: The Sciences and Engineering. 2005;65:4819. [Google Scholar]
- Center for the Study and Prevention of Violence. Blueprints for Violence Prevention. 2007 Retrieved October 12, 2007 from http://www.colorado.edu/cspv/blueprints/model/overview.html.
- Costarides AH, Shulman BB. Norm-referenced language measures: Implications for assessment of infants and toddlers. Topics in Language Disorders. 1998;18:26–33. [Google Scholar]
- Coté SM, Vaillancourt T, LeBlanc JC, Nagin D, Tremblay RE. The development of physical aggression from toddlerhood to pre-adolescence: a nation wide longitudinal study of Canadian children. Journal of Abnormal Child Psychology. 2006;34:71–85. doi: 10.1007/s10802-005-9001-z. [DOI] [PubMed] [Google Scholar]
- Cudeck R, Browne MW. Constructing a covariance matrix that yields a specified minimizer and a specified minimum discrepancy function value. Psychometrika. 1992;57:357–369. [Google Scholar]
- Dunn LM, Dunn LM. Peabody Picture Vocabulary Test-Revised. Circle Pines, MN: American Guidance Service; 1981. [Google Scholar]
- Fergusson DM, Horwood LJ. Male and female offending trajectories. Development & Psychopathology. 2002;14:159–177. doi: 10.1017/s0954579402001098. [DOI] [PubMed] [Google Scholar]
- Fetrick A, Christensen M, Mitchell C. Does public health nurse home visitation make a difference in the health outcomes of pregnant clients and their offspring? Public Health Nursing. 2003;20:184–189. doi: 10.1046/j.0737-1209.2003.20305.x. [DOI] [PubMed] [Google Scholar]
- Gross D, Fogg L, Webster-Stratton C, Garvey C, Julion W, Grady J. Parent training of toddlers in day care in low-income urban communities. Journal of Consulting and Clinical Psychology. 2003;71:261–278. doi: 10.1037/0022-006x.71.2.261. [DOI] [PubMed] [Google Scholar]
- Kearney MH, York R, Deatrick JA. Effects of home visits to vulnerable young families. Journal of Nursing Scholarship. 2000;32:369–376. doi: 10.1111/j.1547-5069.2000.00369.x. [DOI] [PubMed] [Google Scholar]
- Keenan K, Shaw DS. The development of aggression in toddlers: A study of low-income families. Journal of Abnormal Child Psychology. 1994;33:53–77. doi: 10.1007/BF02169256. [DOI] [PubMed] [Google Scholar]
- Kingston L, Prior M. The development of patterns of stable, transient, and school-age onset aggressive behavior in young children. Journal of the American Academy of Child & Adolescent Psychiatry. 1995;34:348–358. doi: 10.1097/00004583-199503000-00021. [DOI] [PubMed] [Google Scholar]
- Kitzman H, Olds DL, Henderson CR, Jr, Hanks C, Cole R, Tatelbaum R, et al. Effect of prenatal and infancy home visitation by nurses on pregnancy outcomes, childhood injuries, and repeated childbearing: a randomized controlled trial. JAMA. 1997;278:644–652. [PubMed] [Google Scholar]
- Kitzman H, Olds DL, Sidora K, Henderson CR, Jr, Hanks C, Cole R, et al. Enduring effects of nurse home visitation on maternal life course: a 3-year follow-up of a randomized trial. JAMA. 2000;283:1983–1989. doi: 10.1001/jama.283.15.1983. [DOI] [PubMed] [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. New York, NY: Guilford Press; 1998. [Google Scholar]
- Loeber R, Pardini D, Homish DL, Wei EH, Crawford AM, Farrington DP, et al. The Prediction of Violence and Homicide in Young Men. Journal of Consulting and Clinical Psychology. 2005;73:1074–1088. doi: 10.1037/0022-006X.73.6.1074. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychological Methods. 2002;7:83–104. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McNaughton DB. Nurse home visits to maternal-child clients: a review of intervention research. Public Health Nursing. 2004;21:207–219. doi: 10.1111/j.0737-1209.2004.021303.x. [DOI] [PubMed] [Google Scholar]
- Moffitt TE. Adolescence-Limited and Life-Course-Persistent Antisocial Behavior: A developmental taxonomy. Psychological Review. 1993;100 (4):674–701. [PubMed] [Google Scholar]
- Moffitt TE, Caspi A. Childhood predictors differentiate life-course persistent and adolescence-limited antisocial pathways among males and females. Development & Psychopathology. 2001;13:355–375. doi: 10.1017/s0954579401002097. [DOI] [PubMed] [Google Scholar]
- Moffitt TE, Caspi A, Rutter M, Silva PA. Sex Differences in Antisocial Behavior: Conduct Disorder, Delinquency, and Violence in the Dunedin Longitudinal Study. New York: Cambridge University Press; 2001. [Google Scholar]
- Moffitt TE, Caspi A, Dickson N, Silva P, Stanton W. Childhood-onset versus adolescent conduct problems in males: Natural history from ages 3–18. Development and Psychopathology. 1996;8:399–424. [Google Scholar]
- Molfese VJ, Acheson S. Infant and preschool mental and verbal abilities: how are infant scores related to preschool scores? International Journal of Behavioral Development. 1997;20:595–607. [Google Scholar]
- Muthén LK, Muthén BO. MPLUS User’s Guide. 4. Los Angeles, CA: Muthen & Muthen; 1998–2006. [Google Scholar]
- Nagin D, Tremblay RE. Trajectories of males’ physical aggression, opposition, and hyperactivity on the path to physically violent and nonviolent juvenile delinquency. Child Development. 1999;70 (5):1181–1196. doi: 10.1111/1467-8624.00086. [DOI] [PubMed] [Google Scholar]
- Nagin D, Tremblay R. Parental and early childhood predictors of persistent physical aggression in males from kindergarten to high school. Archives of General Psychiatry. 2001;58 (4):389–394. doi: 10.1001/archpsyc.58.4.389. [DOI] [PubMed] [Google Scholar]
- NCAST Caregiver/Parent-Child Interaction Teaching Manual. Seattle: NCAST Publications, University of Washington, School of Nursing; 1994. [Google Scholar]
- Olds DL, Henderson CR, Jr, Tatelbaum R, Chamberlin R. Improving the life-course development of socially disadvantaged mothers: a randomized trial of nurse home visitation. American Journal Public Health. 1988;78:1436–1445. doi: 10.2105/ajph.78.11.1436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olds DL, Henderson CR, Jr, Cole R, Eckenrode J, Kitzman H, Luckey D, et al. Long-term effects of nurse home visitation on children’s criminal and antisocial behavior: 15-year follow-up of a randomized controlled trial. JAMA. 1998;280:1238–1244. doi: 10.1001/jama.280.14.1238. [DOI] [PubMed] [Google Scholar]
- Olds DL, Kitzman H, Cole R, Robinson J, Sidora K, Luckey D, et al. Effects of nurse home visiting on maternal life-course and child development: age-six follow-up of a randomized trial. Pediatrics. 2004;114:1550–1559. doi: 10.1542/peds.2004-0962. [DOI] [PubMed] [Google Scholar]
- Olds DL, Robinson J, O’Brien R, Luckey DW, Pettitt LM, Henderson CR, Jr, et al. Home visiting by paraprofessionals and by nurses: a randomized, controlled trial. Pediatrics. 2002;110:486–496. doi: 10.1542/peds.110.3.486. [DOI] [PubMed] [Google Scholar]
- Olds DL, Robinson J, Pettitt L, Luckey D, Holmberg J, Ng RK, et al. Effects of home visits by paraprofessionals and by nurses: age 4 follow-up results of a randomized trial. Pediatrics. 2004;114:1560–8. doi: 10.1542/peds.2004-0961. [DOI] [PubMed] [Google Scholar]
- Olds DL, Sadler L, Kitzman H. Programs for parents of infants and toddlers: recent evidence from randomized trials. Journal of Child Psychology & Psychiatry & Allied Disciplines. 2007;48:355–91. doi: 10.1111/j.1469-7610.2006.01702.x. [DOI] [PubMed] [Google Scholar]
- Patterson GR, DeBaryshe BD, Ramsey E. A developmental perspective on antisocial behavior. American Psychologist. 1989;44:329–335. doi: 10.1037//0003-066x.44.2.329. [DOI] [PubMed] [Google Scholar]
- Pearlin LI, Schooler C. The structure of coping. Journal of Health and Social Behavior. 1967;19:2–21. [PubMed] [Google Scholar]
- Reid MJ, Webster-Stratton C, Baydar N. Halting the development of conduct problems in Head Start children: the effects of parent training. Journal of Clinical Child and Adolescent Psychology. 2004;33:279–291. doi: 10.1207/s15374424jccp3302_10. [DOI] [PubMed] [Google Scholar]
- Reiss AJ, Roth JA. Perspectives on Violence. In: Reiss AJ, Roth JA, editors. Understanding and Preventing Violence. Washington, DC: National Academy Press; 1993. [Google Scholar]
- Sanders MR. The Triple P-Positive Parenting Program: towards an empirically validated multilevel parenting and family support strategy for the prevention of behavior and emotional problems in children. Clinical Child and Family Psychology Review. 1999;2:71–90. doi: 10.1023/a:1021843613840. [DOI] [PubMed] [Google Scholar]
- Sanders MR, Markie-Dadds C, Tully LA, Bor W. The Triple P-Positive Parenting Program: a comparison of enhanced, standard, and self-directed behavioral family intervention for parents of children with early onset conduct problems. Journal of Consulting and Clinical Psychology. 2000;68:624–640. [PubMed] [Google Scholar]
- Sanders MR, Turner KM, Markie-Dadds C. The development and dissemination of the Triple P_Positive Parenting Program: a multilevel, evidence-based system of parenting and family support. Prevention Science. 2002;3:173–189. doi: 10.1023/a:1019942516231. [DOI] [PubMed] [Google Scholar]
- Shipley W. A self-administered scale for measuring intellectual impairment and deterioration. Journal of Psychology. 1940;9:371–377. [Google Scholar]
- Siegel LS, Cooper DC, Fitzhardinge PM, Ash AJ. The use of the mental development index of the Bayley scale to diagnosis language delay in 2-year-old high-risk infants. Infant Behavior & Development. 1995;18:483–486. [Google Scholar]
- Soares JF, Wu CF. Some restricted randomization rules in sequential designs. Communications in Statistical Theory and Methods. 1983;12:2017–2034. [Google Scholar]
- Soussignan R, Tremblay RE, Schaal B, Laurent D, Larivée S, Gagnon C, et al. Behavioural and cognitive characteristics of conduct disordered-hyperactive males from age 6 to 11: a multiple informant perspective. Journal of Child Psychology and Psychiatry. 1992;33:1333–1346. doi: 10.1111/j.1469-7610.1992.tb00953.x. [DOI] [PubMed] [Google Scholar]
- Sparling J, Lewis I. Partners for Learning. Lewisville, NC: Kaplan Press; 1984. [Google Scholar]
- Spoth R, Redmond C, Shin C. Direct and indirect latent variable parenting outcomes of two universal family-focused preventive interventions: extending a public health-oriented research base. Journal of Consulting and Clinical Psychology. 1998;66:385–399. doi: 10.1037//0022-006x.66.2.385. [DOI] [PubMed] [Google Scholar]
- Sumner GA, Barnard KE, Johnson-Crowley N, Spietz A. NCAST Keys to Caregiving. Seattle: NCAST Publications, University of Washington, School of Nursing; 1990. [Google Scholar]
- Taylor TK, Biglan A. Behavioral family interventions for improving childrearing: a review of the literature for clinicians and policymakers. Clinical Child and Family Psychology Review. 1998;1:41–59. doi: 10.1023/a:1021848315541. [DOI] [PubMed] [Google Scholar]
- Tremblay RE. The development of physically aggressive behavior during childhood: What have we learned in the past century? International Journal of Behavioral Development. 2000;24:129–141. [Google Scholar]
- Tremblay RE. Decade of behavior distinguished lecture: Development of physical aggression during infancy. Infant Mental Health Journal. 2004;25:399–407. [Google Scholar]
- Ware JE, Veit CT, Donald CA. Refinements in the measurement of mental health for adults in the Health Insurance Study. Santa Monica, CA: RAND Corporation; 1985. [Google Scholar]
- Webster-Stratton C. Early-onset conduct problems: does gender make a difference? Journal of Consulting and Clinical Psychology. 1996;64:540–551. doi: 10.1037//0022-006x.64.3.540. [DOI] [PubMed] [Google Scholar]
- Webster-Stratton C. Preventing conduct problems in Head Start children: strengthening parent competencies. Journal of Consulting and Clinical Psychology. 1998;66:715–730. doi: 10.1037//0022-006x.66.5.715. [DOI] [PubMed] [Google Scholar]
- Webster-Stratton C, Reid MJ. The incredible years, parent, teacher, and child intervention: targeting multiple areas of risk for a young child with pervasive conduct problems using a flexible, manualized treatment program. Cognitive and Behavioral Practice. 2003;8:377–386. [Google Scholar]
- Webster-Stratton C, Reid MJ. Treating conduct problems and strengthening social and emotional competence in young children: the dina dinosaur treatment program. Journal of Emotional and Behavioral Disorders. 2003;11:130–143. [Google Scholar]
- Webster-Stratton C, Reid MJ, Hammond M. Preventing conduct problems, promoting social competence: a parent and teacher training partnership in Head Start. Journal of Clinical Child Psychology. 2001;30:283–302. doi: 10.1207/S15374424JCCP3003_2. [DOI] [PubMed] [Google Scholar]
- Webster-Stratton C, Taylor T. Nipping early risk factors in the bud: preventing substance abuse, delinquency, and violence in adolescence through interventions targeted at young children (0–8 years) Prevention Science. 2001;2:165–192. doi: 10.1023/a:1011510923900. [DOI] [PubMed] [Google Scholar]
- Williams S, Waymouth M, Lipman E, Mills B, Evans P. Evaluation of a children’s temper-taming program. Canadian Journal of Psychiatry. 2004;49:607–612. doi: 10.1177/070674370404900906. [DOI] [PubMed] [Google Scholar]
- Yoshikawa H. Prevention as cumulative protection: effects of early family support and education on chronic delinquency and its risks. Psychological Bulletin. 1994;115:28–54. doi: 10.1037/0033-2909.115.1.28. [DOI] [PubMed] [Google Scholar]